Electromyography: A Simple and Accessible Tool to Assess Physical Performance and Health during Hypoxia Training. A Systematic Review
Abstract
1. Introduction
2. Material and Methods
2.1. Search Strategy
2.2. Selection of Articles: Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Selection of Studies
3.2. Results of the Quality Assessment
3.3. Descriptive Information of the Selected Articles Included in the Systematic Review
3.4. Performance Measures
4. Discussion
4.1. Study Design and Participants
4.2. Additional Stimuli
4.3. Hypoxia
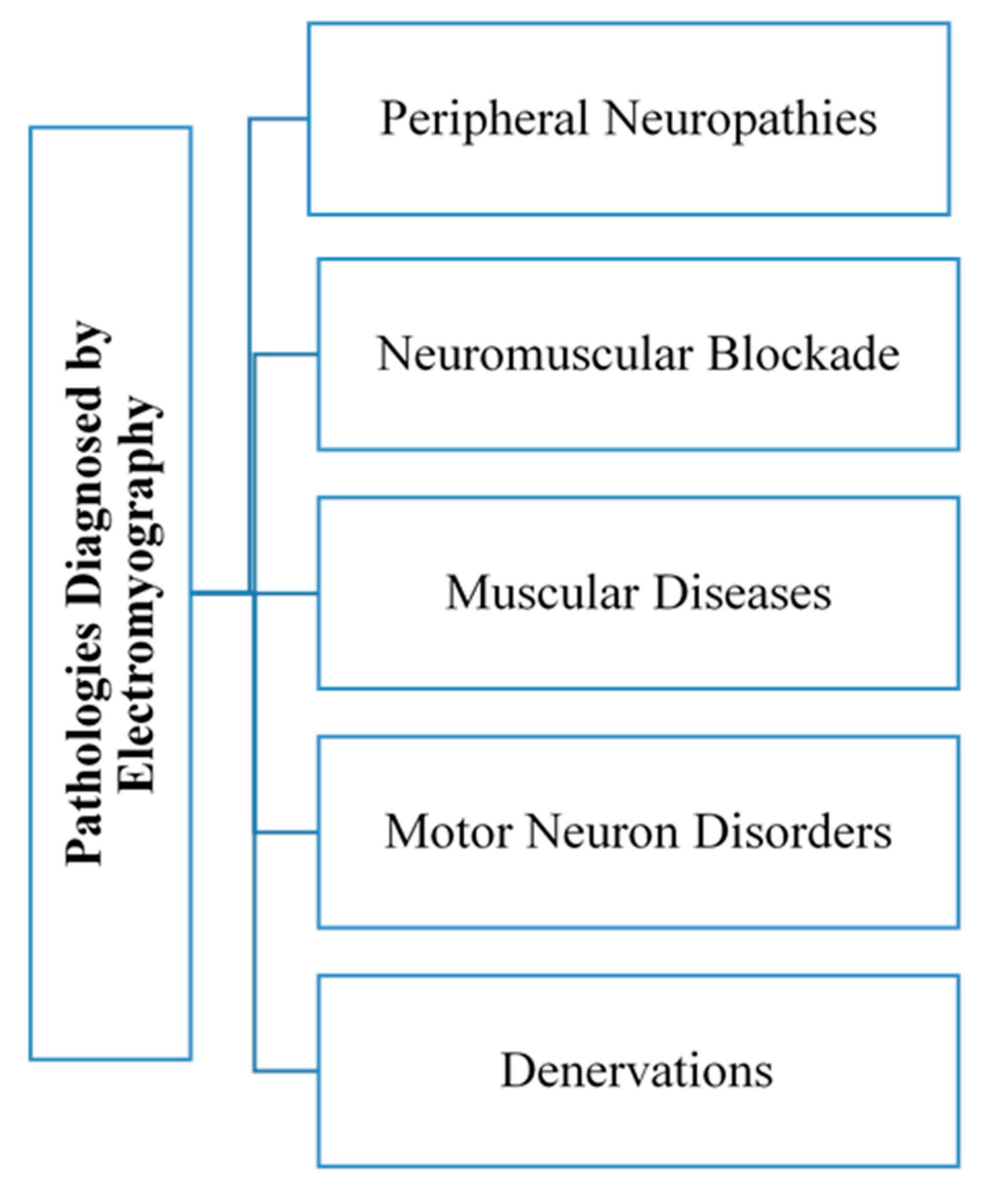
4.4. Electromyography
4.5. Muscles
4.6. Physical Activity
4.7. Electromyographic Evaluation of Muscle Activity by Electromyography
4.7.1. Muscular Activity
4.7.2. Muscle Fatigue
4.7.3. Muscle Activation
5. Application of Electromyography for a Sustainable Lifestyle
5.1. Quality of Health and Quality of Life
5.2. Physical Performance
6. Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fernandez-Lazaro, D.; Diaz, J.; Caballero, A.; Cordova, A. Strength and endurance training in hypoxia: Effect on muscular hypertrophy. Biomedica 2019, 39, 212–220. [Google Scholar]
- Millet, G.P.; Roels, B.; Schmitt, L.; Woorons, X.; Richalet, J.P. Combining hypoxic methods for peak performance. Sports Med. 2010, 40, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Cordova Martinez, A.; Pascual Fernandez, J.; Fernandez Lazaro, D.; Alvarez Mon, M. Muscular and heart adaptations of execise in hypoxia. Is training in slow hypoxy healthy? Med. Clin. 2017, 148, 469–474. [Google Scholar]
- Córdova Martínez, A.; Nuin, I.; Fernández-Lázaro, D.; Latasa Zudaire, I.A.; Rodríguez Falces, J. Electromyographic activity (EMG) during pedaling, its usefulness in the diagnosis of fatigue in cyclists. Arch. Med. Dep. 2017, 34, 217–223. [Google Scholar]
- Massó, N.; Rey, F.; Romero, D.; Gual, G.; Costa, L.; Germán, A. Applications of surface electromyography in sport. Apunt. Med. Esport. 2010, 45, 127–136. [Google Scholar] [CrossRef]
- Caballero, K.; Duque, L.M.; Ceballos, S.; Ramírez, J.C.; Peláez, A. Basic concepts for electromyographic analysis. Ces. Odontol. 2002, 15, 41–50. [Google Scholar]
- Tankisi, H.; Burke, D.; Cui, L.; de Carvalho, M.; Kuwabara, S.; Nandedkar, S.D.; Rutkove, S.B.; Stålberg, E.; Van Putten, M.J.; Fuglsang-Frederiksen, A. Standards of instrumentation of EMG. Clin. Neurophysiol. 2020, 131, 243–258. [Google Scholar] [CrossRef]
- Rojas Martínez, M.; Mañanas Villanueva, M.Á. Multichannel surface electromyography as a non-invasive tool in neuromuscular rehabilitation. In Proceedings of the 4th CEA Bioengineering Symposium 2012: Brain Computer Interface and Rehabilitation Technologies, Valladolid, Spain, 29 May 2012; University of Valladolid: Valladolid, Spain, 2012; pp. 73–79. Available online: https://upcommons.upc.edu/handle/2117/17970 (accessed on 2 September 2020).
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- O’Connor, D.; Green, S.; Higgins, J.P. Defining the review question and developing criteria for including studies. In Cochrane Handbook for Systematic Reviews of Interventions, 1st ed.; Higgins, J.P., Green, S., Eds.; Wiley Online Library: Chichester, UK, 2008; p. 83. [Google Scholar]
- Gallo Flórez, R. Physiological changes in sports women. Educ. Fis. Sports 1995, 17, 1–7. [Google Scholar]
- Córdova Martínez, A. Sports Physiology, 1st ed.; Síntesis: Madrid, Spain, 2013. [Google Scholar]
- París, C.L. Influence of sex in the practice of sports. Biol. Sportswom. Arbor. 2000, 165, 249–263. [Google Scholar]
- Law, M.; Stewart, D.; Letts, L.; Pollock, N.; Bosch, J.; Westmorland, M. Guidelines for Critical Review of Qualitative Studies; McMaster University Occupational Therapy Evidence-Based Practice Research Group: Hamilton, ON, Canada, 1998; pp. 1–9. [Google Scholar]
- Taylor, A.; Bronks, R. Effect of acute normobaric hypoxia on quadriceps integrated electromyogram and blood metabolites during incremental exercise to exhaustion. Eur. J. Appl. Physiol. Occup. Physiol. 1996, 73, 121–129. [Google Scholar] [CrossRef]
- Scott, B.R.; Slattery, K.M.; Sculley, D.V.; Lockhart, C.; Dascombe, B.J. Acute physiological responses to moderate-load resistance exercise in hypoxia. J. Strength Cond. Res. 2017, 31, 1973–1981. [Google Scholar] [CrossRef] [PubMed]
- Scott, B.R.; Slattery, K.M.; Sculley, D.V.; Smith, S.M.; Peiffer, J.; Dascombe, B.J. Acute physiological and perceptual responses to high-load resistance exercise in hypoxia. Clin. Physiol. Funct. Imaging 2018, 38, 595–602. [Google Scholar] [CrossRef]
- Fulco, C.S.; Lewis, S.F.; Frykman, P.N.; Boushel, R.; Smith, S.; Harman, E.A.; Cymerman, A.; Pandolf, K.B. Muscle fatigue and exhaustion during dynamic leg exercise in normoxia and hypobaric hypoxia. Eur. J. Appl. Physiol. 1996, 81, 1891–1900. [Google Scholar] [CrossRef]
- Osawa, T.; Kime, R.; Hamaoka, T.; Katsumura, T.; Yamamoto, M. Attenuation of muscle deoxygenation precedes EMG threshold in normoxia and hypoxia. Med. Sci. Sports Exerc. 2011, 43, 1406–1413. [Google Scholar] [CrossRef]
- Torres-Peralta, R.; Losa-Reyna, J.; Gonzalez-Izal, M.; Pérez-Suárez, I.; Calle-Herrero, J.; Izquierdo, M.; Calbet, J.A.L. Muscle activation during exercise in severe acute hypoxia: Role of absolute and relative intensity. High Alt. Med. Biol. 2014, 15, 472–482. [Google Scholar] [CrossRef]
- Girard, O.; Racinais, S. Combining heat stress and moderate hypoxia reduces cycling time to exhaustion without modifying neuromuscular fatigue characteristics. Eur. J. Appl. Physiol. 2014, 114, 1521–1532. [Google Scholar] [CrossRef]
- Girard, O.; Brocherie, F.; Morin, J.-B.; Millet, G.P. Neuro-mechanical determinants of repeated treadmill sprints-Usefulness of an “hypoxic to normoxic recovery” approach. Front. Physiol. 2015, 6, 260. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, A.; Hodder, S.; Havenith, G. The interactive effect of cooling and hypoxia on forearm fatigue development. Eur. J. Appl. Physiol. 2015, 115, 2007–2018. [Google Scholar] [CrossRef][Green Version]
- Lockhart, C.; Scott, B.R.; Thoseby, B.; Dascombe, B.J. Acute effects of interset rest duration on physiological and perceptual responses to resistance exercise in hypoxia. J. Strength Cond. Res. 2020, 34, 2241. [Google Scholar] [CrossRef] [PubMed]
- Hulley, S.B.; Cummings, S.R.; Browner, W.S.; Grady, D.G.; Newman, T.B. Designing Clinical Research: An Epidemiologic Approach, 2nd ed.; Lippincott, Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Mitchell, J.B.; Rogers, M.M.; Basset, J.T.; Hubing, K.A. Fatigue during high-intensity endurance exercise: The interaction between metabolic factors and thermal stress. J. Strength Cond. Res. 2014, 28, 1906–1914. [Google Scholar] [CrossRef] [PubMed]
- Cè, E.; Rampichini, S.; Agnello, L.; Limonta, E.; Veicsteinas, A.; Esposito, F. Combined effects of fatigue and temperature manipulation on skeletal muscle electrical and mechanical characteristics during isometric contraction. J. Electromyogr. Kinesiol. 2012, 22, 348–355. [Google Scholar] [CrossRef]
- Urdampilleta, A.; León-Guereño, P.; Calleja-González, J.; Roche, E.; Mielgo-Ayuso, J. Inclusion of resistance routines in a hypoxia training program does not interfere with prevention of acute mountain sickness. Phys. Sportsmed. 2020, 1–7. Available online: https://www.tandfonline.com/doi/abs/10.1080/00913847.2020.1786344 (accessed on 20 August 2020). [CrossRef]
- Fernández, J.M.; Acevedo, R.C.; Tabernig, C.B. Influencia de la fatiga muscular en la señal electromiográfica de músculos estimulados eléctricamente. Rev. EIA Esc. Ing. Antioq. 2007, 7, 111–119. [Google Scholar]
- Boyas, S.; Guével, A. Neuromuscular fatigue in healthy muscle: Underlying factors and adaptation mechanisms. Ann. Phys. Rehabil. Med. 2011, 54, 88–108. [Google Scholar] [CrossRef]
- Aparicio, M.V. Kinesiological electromyography. Rehabilitation 2005, 39, 255–264. [Google Scholar]
- Benedetti, M. Muscle activation intervals and EMG envelope in clinical gait analysis. IEEE Eng. Med. Biol. Mag. 2001, 20, 33–44. [Google Scholar] [CrossRef]
- Benedetti, M.G.; Catani, F.; Bilotta, T.; Marcacci, M.; Mariani, E.; Giannini, S. Muscle activation pattern and gait biomechanics after total knee replacement. Clin. Biomech. 2003, 18, 871–876. [Google Scholar] [CrossRef]
- Benoit, D.L.; Lamontagne, M.; Cerulli, G.; Liti, A. The clinical significance of electromyography normalisation techniques in subjects with anterior cruciate ligament injury during treadmill walking. Gait Posture 2003, 18, 56–63. [Google Scholar] [CrossRef]
- Frigo, C.; Crenna, P. Multichannel SEMG in clinical gait analysis: A review and state-of-the-art. Clin. Biomech. 2009, 24, 236–245. [Google Scholar] [CrossRef]
- Meekins, G.D.; So, Y.; Quan, D. American Association of Neuromuscular & Electrodiagnostic Medicine evidenced-based review: Use of surface electromyography in the diagnosis and study of neuromuscular disorders. Muscle Nerve 2008, 38, 1219–1224. [Google Scholar]
- Balestra, G.; Frassinelli, S.; Knaflitz, M.; Molinari, F. Time-frequency analysis of surface myoelectric signals during athletic movement. IEEE Eng. Med. Biol. Mag. 2001, 20, 106–115. [Google Scholar] [CrossRef]
- Nordander, C.; Hansson, G.-Å.; Rylander, L.; Asterland, P.; BystrÖm, J.U.; Ohlsson, K.; Balogh, I.; Skerfving, S. Muscular rest and gap frequency as EMG measures of physical exposure: The impact of work tasks and individual related. Ergonomics 2000, 43, 1904–1919. [Google Scholar] [CrossRef] [PubMed]
- So, R.; Ng, J.; Lam, R.; Lo, C.; Ng, G. EMG wavelet analysis of quadriceps muscle during repeated knee extension movement. Med. Sci. Sports Exerc. 2009, 41, 788–796. [Google Scholar] [CrossRef]


| Body System | Adaptive Physiological Response by Hypoxia |
|---|---|
| Respiratory |
|
| Cardiovascular |
|
| Endocrine |
|
| Metabolic |
|
| Hematological |
|
| Immune |
|
| Muscle |
|
| Author/s | Items | T1 | % | MQ | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||||
| Taylor et al. [15] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 13 | 81.25 | VG |
| Scott et al. [16] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 15 | 93.75 | E |
| Scott et al. [17] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 13 | 81.25 | VG |
| Fulco et al. [18] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 13 | 81.25 | VG |
| Osawa et al. [19] | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 11 | 68.75 | G |
| Torres et al. [20] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 13 | 81.25 | VG |
| Girard et al. [21] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 13 | 81.25 | VG |
| Girard et al. [22] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 15 | 93.75 | E |
| Lloyd et al. [23] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 14 | 87.50 | VG |
| T2 | 9 | 9 | 9 | 9 | 4 | 9 | 7 | 7 | 9 | 9 | 9 | 2 | 9 | 9 | 9 | 1 | |||
| Characteristics | Type | Study Reference |
|---|---|---|
| Additional stimuli | Heat | [21] |
| Cold | [23] | |
| Hypoxia training | Normobaric hypoxia | [15,16,17,19,20,21,22,23] |
| Hypobaric hypoxia | [18] | |
| Electromyography | Integrated electromyography (iEMG) | [15] |
| Surface electromyography (sEMG) | [19,20,22] | |
| Both integrated and surface electromyography (iEMG & sEMG) | [16,17,18] | |
| Muscles | Lower limb | [15,16,17,18,19,20,21,22] |
| Forearm | [23] | |
| Physical activation | Cycling | [15,19,20,21] |
| Squat exercise plan | [16,17] | |
| Exercises of submaximum extension of the knee | [18] | |
| Sprints | [22] | |
| Exercises of voluntary isometric contraction | [23] | |
| Muscular activity | Integrated electromyography (iEMG) | [16,17,18] |
| Surface electromyography (sEMG) | [16,17,18] | |
| Muscle fatigue (exhaustion time) | Integrated electromyography (iEMG) | [15,18] |
| Surface electromyography (sEMG) | [18,21] | |
| Muscle activation | Integrated electromyography (iEMG) | [16,17,19,20] |
| Surface electromyography (sEMG) | [16,17] |
| Author/s–Year | Study Design | Population | Hypoxia | EMG | Muscle | Physical Activity |
|---|---|---|---|---|---|---|
| Taylor et al. (1996) [15] | One normoxia test and one HE test was performed in random order. A unique blind experiment design was used. The tests were separated by 24 h. | 14 healthy trained men 20.9 ± 2.7 years | HE (FiO2 13.5%) | iEMG. | Vastus lateralis, vastus internalis, and femoral rectum | The tests were carried out on a cycle ergometer. Each test began at 60 W and continued with exercise increments of 30 W ∙ 4 min−1. |
| Scott et al. (2017) [16] | The subjects went to the lab 3 times, each separated by at least 1 week. A blind and counterbalanced crossover design was used. They visited the lab 2 more times to complete an exercise protocol. | 14 healthy untrained men 21–29 years | HM (FiO2 16%) | iEMG and sEMG | Gluteus major, femoral biceps, vastus lateralis, and vastus internalis | Two sets of warm-up squats (10 repetitions at 40 and 50% of 1RM) before doing the first of 3 sets of 10 repetitions at 60% of 1RM, with a 60 s break between sets. They rested 8 min before doing the same warm-up and exercise protocol for dead weight. |
| Scott et al. (2018) [17] | The subjects went to the lab 4 times, each separated by at least 1 week. A randomized single-blind crossover design was used. They went 3 times more to complete an exercise protocol. | 12 healthy trained men 25.3 ± 4.3 years | HM (FiO2 16%) and high hypoxia (FiO2 13%) | iEMG and sEMG | Middle gluteus, femoral biceps, external and internal vastus | Two sets of squats (10 repetitions at 50% of 1RM and 7 repetitions at 65% of 1RM) separated by 90 s. They rested 180 s before the first 5 sets of 5 repetitions at 80% of 1RM, with a 180 s break. Then they rested 180 s before starting the same dead-weight protocol. |
| Fulco et al. (1996) [18] | Each subject was evaluated in 4 days, each separated by 2 to 5 days. The order of exercise days in normoxia or hypoxia was randomized. | 8 healthy untrained men 19.0 ± 1.0 years | HH (FiO2 13% and 464 Torr) | iEMG and sEMG | Vastus lateralis, vastus internalis, femoral rectum, and femoral biceps | On two of the trial days, the maximum rate of knee extension work was determined on one leg, and on the other two days a submaximal knee extension exercise was performed on one leg until exhaustion. |
| Osawa et al. (2011) [19] | In random order, with an interval of 48 h between each exercise session | 9 healthy and physically 23.0 ± 2.0 years | HN (FiO2 12%) | sEMG | Vastus lateralis | The exercises were of incremental cycling on a ramp. A cycle ergometer was used and the frequency of pedaling was maintained at 60 rpm. It started at 10 W for 4 min and increased to a ramp speed of 20 W/min. |
| Torres et al. (2014) [20] | Subjects came to the laboratory on 2 different test days, at least 1 week apart. On each test day, the exercises were performed in random order. | 11 healthy and physically active men 21.0 ± 2.0 years | HN (FiO2 10.8%) | sEMG | Femoral rectum, vastus internalis, vastus externalis, and femoral biceps | Two series of exercises with an incremental cycle ergometer, with a rest of 90 min. The load was at 60 W (hypoxia) or 80 W (normoxia), and after 2 min the intensity increased by 20–30 W (hypoxia) or 30–40 W (normoxia) every 2 min until exhaustion. They were asked to maintain a pedal speed of 80 rpm. Burnout was defined as the inability to maintain a pedal speed greater than 50 rpm despite verbal stimulation for 5 s. |
| Girard et al. (2014) [21] | Trials were randomized, separated by at least 5–7 days and conducted at the same time of day | 11 healthy and physically active men | Moderate hypoxia (FiO2 15%) with heat 35 °C and 40% humidity and room temperature 22 °C | sEMG | Anterior soleus and tibialis | 10-min warm-up on an ergometer at 75 W (pedal speed 70–80 rpm); 5-min rest; up to the exhaustion limit with a fixed workload, 66% of the output power associated with VO2 (pedal speed 80–90 rpm); 5-min recovery, including 90 s of pedaling at 50 W, 60–70 rpm, with a rest of 3 min. It was over when the pedal cadence dropped from 60 rpm to more than 5 s. |
| Girard et al. (2015) [22] | During 3 experimental sessions (random crossover counterbalanced in double blind mode), at least 3–4 days apart. The protocols were executed in double-blind mode. | 13 healthy recreational team and racket sport players (31.2 ± 4.8 years) | Moderate HN (FiO2 16%) and Severe HN (FiO2 13%) | sEMG | Femoral rectum, vastus lateralis, femoral biceps, anterior tibialis, internal calves, and external calves | The first 8, 5 s of sprints with 25 s of rest. Followed by 6 min of rest and 4, 5 s of sprints with 25 s of rest. Before 10 min of race to 10 km∙h−1, with 15 min of specific muscle warm-up [3× (high knee, high heels, full kicks, jumping 10 s with 30 s walking), 3× (accelerations of 3 steps in a sense of subjective effort in 7, 8, and 9), 2× (sprints of 3 s with a sense of subjective effort in 8 and 9). A total of 3 sprints of 5 s, with 2 min rest. And 5 min of cooling was left before the repeated sprint protocol. |
| Lloyd et al. (2015) [23] | They were blinded and exposed once to the 4 conditions. The order was random and the exposures were separated by at least 4 days. | 8 healthy untrained men (21.9 ± 0.8 years) | HN (FiO2 16%) with cold 5 °C and room temperature 22 °C | sEMG | Extensor and flexor (radial, common, fingers) | After 15 min of rest, they performed intermittent dynamic exercises of the forearm at a maximum voluntary isometric contraction of 15% during 8 work sessions of 5 consecutive minutes. Each test was separated with a 110 s break. |
| Author/s–Year | Results | Conclusions |
|---|---|---|
| Taylor et al. (1996) [15] | HE increased quadriceps iEMG during ergometry, although these responses were not significant. | iEMG showed that HE reduced the time to exhaustion. |
| Scott et al. (2017) [16] | iEMG was significantly higher at HM, p ≤ 0.032. | HM with moderate load increased muscle activation. HM can increase muscle development. |
| Scott et al. (2018) [17] | For squatting backwards, MH gave a higher iEMG result than in normoxia and high hypoxia, but the differences were not significant. But for dead weight, significant differences were observed, with high hypoxia being the one with the greatest results. | No significant differences were observed in iEMG during motor unit recruitment in MH, high hypoxia, or normoxia. |
| Fulco et al. (1996) [18] | The activity of the iEMG during maximum voluntary contraction decreased significantly when the duration of dynamic exercise was increased in both normoxia and HH. | Exhaustion was more related to the reduced speed of shortening than to the failure to generate force. |
| Osawa et al. (2011) [19] | EMG activity was not significantly higher in hypoxia at the same absolute exercise intensity and peak VO2. | Muscle deoxygenation was related to changes in muscle activity in both normoxia and hypoxia. |
| Torres et al. (2014) [20] | RMS increased with exercise intensity in the femoral rectum, vastus lateralis, vastus internalis, and femoral biceps, with greater effect in hypoxia, and the same relative intensity was greater in normoxia than in hypoxia. | Muscle activation during exercise increases almost linearly with exercise intensity following a specific muscle pattern, which is adjusted depending on FiO2 and the relative intensity of the exercise. |
| Girard et al. (2014) [21] | M-wave amplitude and mean quadratic activity were reduced in warm conditions compared to temperate conditions, while maximum EMG activity did not change. | The altitude had no effect on any measured parameter, but hypoxia combined with heat reduced the time to exhaustion. |
| Girard et al. (2015) [22] | Mean quadriceps root quadratic activity in severe HN was superior. During the first sprint of the subsequent normoxic set the electromyogram had no significant difference. | The sprint and neural alterations were influenced by hypoxia. However, hypoxia had no residual effect during a subsequent set performed in normoxia. |
| Lloyd et al. (2015) [23] | Electromyographic activity in relation to the force produced during MVC increased for cold and hypoxia. When stressors were combined, the effect was additive. | Both cold and hypoxia significantly reduced the production of brief CVS force. This appeared to be of mechanical origin, not a failure to recruit muscle fibers. In addition, the reduction |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Lázaro, D.; Mielgo-Ayuso, J.; Adams, D.P.; González-Bernal, J.J.; Fernández Araque, A.; Cano García, A.; Fernández-Lázaro, C.I. Electromyography: A Simple and Accessible Tool to Assess Physical Performance and Health during Hypoxia Training. A Systematic Review. Sustainability 2020, 12, 9137. https://doi.org/10.3390/su12219137
Fernández-Lázaro D, Mielgo-Ayuso J, Adams DP, González-Bernal JJ, Fernández Araque A, Cano García A, Fernández-Lázaro CI. Electromyography: A Simple and Accessible Tool to Assess Physical Performance and Health during Hypoxia Training. A Systematic Review. Sustainability. 2020; 12(21):9137. https://doi.org/10.3390/su12219137
Chicago/Turabian StyleFernández-Lázaro, Diego, Juan Mielgo-Ayuso, David P. Adams, Jerónimo J. González-Bernal, Ana Fernández Araque, Alicia Cano García, and Cesar I. Fernández-Lázaro. 2020. "Electromyography: A Simple and Accessible Tool to Assess Physical Performance and Health during Hypoxia Training. A Systematic Review" Sustainability 12, no. 21: 9137. https://doi.org/10.3390/su12219137
APA StyleFernández-Lázaro, D., Mielgo-Ayuso, J., Adams, D. P., González-Bernal, J. J., Fernández Araque, A., Cano García, A., & Fernández-Lázaro, C. I. (2020). Electromyography: A Simple and Accessible Tool to Assess Physical Performance and Health during Hypoxia Training. A Systematic Review. Sustainability, 12(21), 9137. https://doi.org/10.3390/su12219137








