Abstract
Against the background of the worldwide spread of the COVID-19 pandemic, due to the lack of effective collaborative incentive mechanisms, issues of dislocation and incoordination have emerged in the public health emergency management system (PES) globally. Nevertheless, the available research rarely touches upon the incentive mechanism design for the collaborative management of PES. To alleviate these inefficiency operations problems with PES, three game-theoretical decision models, including a decentralized decision model without public governance policy incentive (GPI), a decentralized decision model with GPI, and a collaborative decision model with GPI, were developed and analyzed to explore and design the incentive mechanism of PES. Furthermore, the corresponding numerical and sensitivity analyses were conducted to validate the modelling results in the article. The research results show that: (1) the collaborative decision scenario with GPI performs best, and the decentralized decision scenario with GPI performs second-best regarding the equilibrium emergency management efforts (EMEs) and utilities in all the decision scenarios; (2) an incentive mechanism of the “carrot + Stick” can effectively enhance the collaborative management of public health emergencies and its governance-driven operational performance/efficiency; (3) strengthening the performance assessment of emergency management for relevant government departments is beneficial in improving the overall emergency management efficiency of the PES; (4) reducing the cost of EMEs and enhancing the effectiveness of EMEs are conducive to improving the overall emergency management efficiency of the PES. This research provides a novel framework for designing an effective incentive mechanism to overcome the incoordination impacts and achieve collaborative operations across the PES.
1. Introduction
At the end of 2019, an epidemic of COVID-19, an infectious disease mainly transmitted through the respiratory tract, was caused by novel coronavirus infection named “SARS-CoV-2” by the International Classification Committee. Up to now (9 June 2022), the total number of confirmed cases of COVID-19 is more than 530 million, and the cumulative death toll has exceeded 6.3 million [1]. In recent years, many public health emergencies represented by COVID-19, SARS, and the Ebola virus in West Africa not only seriously endanger people’s health and safety, but also have a more serious impact on the global economy. In particular, in order to curb the spread of novel coronavirus, most countries and states have implemented a blockade policy, which has seriously affected the global production supply chain system resulting in a serious shortage of personal protection and medical emergency materials, so that many patients and healthcare personnel are in a high-risk state [2,3].
As Chinese President Xi Jinping said, the COVID-19 epidemic has been a major test of the country’s emergency response capacity and can expose the shortcomings of the emergency response system [4]. In Nigeria, for example, policy makers used the co-production model to establish a presidential working group (PTF) to make scientific and effective decisions to better respond to COVID-19. However, the lack of coordination among the multiple levels responsible for implementation and the obstacles to the implementation of political developments and interests in some states have led to a small and diminishing number of resources available for COVID-19 responses [5]. Although the United States has many impressive public and private laboratories, innovative pharmaceutical and technology companies, and highly capable national public health institutions, the United States ultimately depends on a significantly decentralized health care system. Each state finances and operates its own public health and surveillance system, and the country has been reluctant to establish a unified health system. The lack of clear coordination hindered the country’s ability to accurately estimate and predict the impact of COVID-19, resulting in delays in response activities, including detection and contact tracking. In addition, the lack of centralized funds leads to the long-term misuse and underutilization of human and financial resources [6]. Ultimately, high underinsurance rates may inhibit the use of health care and prevent citizens from seeking emergency care, leaving them untreated for chronic diseases, reducing the capacity of the health system to monitor symptoms, and undermining citizens’ overall trust in public services, thereby further exacerbating the harmful effects of COVID-19 [7]. Therefore, it can be seen that in response to such public health emergencies, a major key problem in the health systems of most countries is the lack of coordination in health emergency management.
In the face of public health emergencies such as the COVID-19 outbreak, numerous sources have highlighted the importance of incentive mechanisms for the collaborative operations management of public health emergency management systems (PES). As shown by many examples, the realization of collaborative operations management in the PES has encountered major challenges at many levels—such as in the early days of the outbreak in Wuhan where community grass-roots workers fought at the frontlines of the pandemic—played an important role in protecting public health and reducing social panic, but at the same time suffered from insufficient resources, a shortage of necessary personal protective equipment and materials, and a lack of timely coordination and the corresponding incentive mechanism [8,9]. In the early days of the COVID-19 pandemic in the United States, beyond federal and state policy protections, there were no governance-driven collaborative incentive mechanisms to support healthcare workers coping with the risks during this pandemic [10]. For example, a severe shortage of personal protective equipment has led to a number of healthcare workers being infected with COVID-19. Besides, this shortage also has prompted the Centers for Disease Control and Prevention (CDC) to issue instructions to health care workers to improvise and develop masks using the materials at hand. In this case, hospital leaders reportedly encouraged medical staff to use homemade masks for protection, as if nothing had changed; that is, they did not admit that homemade masks provide less protection than surgical masks and Nmur95 masks [10]. Furthermore, the lack of a governance-driven collaborative incentive mechanism for the PES also has triggered mass resignations of healthcare workers and weakened the emergency management capacity of health care institutions, thus also greatly reducing the effectiveness of emergency management in response to public health emergencies [6,11]. As a result, an effective collaborative incentive mechanism for collaborative emergency management of public health emergencies is urgently necessary to be designed to fully mobilize the enthusiasm of medical staff and medical institutions and improve the efficiency of collaborative emergency management of public health emergencies. It is an important issue that needs to be solved urgently in public health emergency management all over the world.
Hence, it would be of vital importance to investigate the impact of incoordination on the governance-driven operational performance of PES, and design an effective collaborative incentive mechanism to improve operational decisions and outcomes of PES under the public governance policy incentive (GPI), but it is still an area rarely studied in the available research literature. The following key research questions need to be addressed in this study: what operational strategies and incentive mechanisms should the PES take to enhance collaborative management and improve their governance-driven operational performance/efficiency? What degrees of emergency management effort (EME) should the medical institutions make to improve their governance-driven operational performance/efficiency? What intensities of transfer payment should the government department use to improve their governance-driven operational performance/efficiency? What is the impact of performance factor of government department on the governance-driven operational performance/efficiency of PES? These research questions will be solved through game-theoretical decision models and corresponding numerical and sensitivity analyses.
In terms of theoretical contribution, the available research rarely touches upon the incentive mechanism design for the collaborative management of public health emergencies. We address the literature gap by cross-fertilizing the areas of public governance, emergency management, game theory, and mechanism design. This paper proposes a novel and useful approach toward the incentive mechanism design for the collaborative management of public health emergencies with game-theoretical modeling and comparative numerical analysis. With regards to our practical contribution, our study sheds new light on studies of collaborative management of public health emergencies. This paper provides a framework for understanding the incoordination issue and its consequences in the public health emergency management system (PES) and designing the incentive mechanisms to overcome the incoordination impacts and achieve collaborative operations across the PES. The modelling and numerical results can be effectively used to help the PES make sensible operational decisions/strategies and improve the governance-driven operational performance and efficiency of the PES.
In the following sections, the corresponding literature review is first conducted in Section 2; the modelling notations and assumptions for public health emergency management system (PES) are defined in the beginning of Section 3; then, the game theoretical decision models for PES under three different decision scenarios are formulated and analyzed in Section 3, including the decentralized decision model without GPI (Section 3.1), decentralized decision model with GPI (Section 3.2), and collaborative decision model with GPI (Section 3.3); the numerical and sensitivity analyses for all game-theoretical decision models are implemented and discussed in Section 4; the managerial insights and policy implications are discussed and summarized in Section 5; and the research contributions and foresights from this study are summarized and concluded in Section 6.
2. Literature Review
2.1. Emergency Management
The earliest definition for emergency management appeared in the discussion of the emotional responses of disaster victims caused by natural disasters [12]. Subsequently, the Federal Emergency Management Agency (FEMA) has defined emergency management as the management function responsible for establishing a framework within which communities are less vulnerable to hazards and better prepared to respond to disasters, stating that its guiding principles are comprehensive, progressive, risk-driven, integrated, collaborative, coordinated, flexible and professional [13]. In the practical measures and related research of emergency management, we found that the research mainly focuses on the prediction evaluation and countermeasure research of emergency management.
The prediction and evaluation of emergency management is the prediction and evaluation of the occurrence and impact of emergency events, and its accuracy has an important impact on the efficiency of resource allocation, scheduling, and evacuation [14]. Therefore, a comparative selection of forecasting techniques is necessary [14]. In addition, evaluating the operational problems of the existing emergency supply chain can look for the influencing factors of management failure [15], helping us to discover the resilience and effectiveness characteristics that a good emergency network should have [16].
The countermeasure research of emergency management can be divided into two branches: management innovation and technology innovation. In terms of management activities, a combination of static game and dynamic game network-embedded theory was used to carry out the behavior selection and mechanism research of the main body in emergency management activities [17,18]. It also used the suitable supply chain elasticity of the integrated supply chain structure to solve the logistics interruption problem in the retail industry [19]. In addition, the application of technical means to assist emergency management has also become popular. Scholars designed an intelligent urban emergency management system to improve urban emergency response and management capabilities [20], established an intelligent evaluation system for government emergency management based on the Internet of Things [21], used group decision support system for emergency management and recovery in coastal cities [22], and applied the scheduling theory and method to solve the patient admission scheduling problem under different scenarios [23,24,25].
The existing literature on emergency management is mostly focused on the research and technical attempts on the factors affecting the improvement of emergency management response capabilities, but not enough attention has been paid to the research on the characteristics of different stakeholders in emergency management activities. As such, it has not been able to combine different stakeholders’ interactions from the perspective of the governance-driven operations management and carry out a better incentive mechanism design and implementation.
2.2. Public Health Emergencies
2.2.1. Impact of Public Health Emergencies
The COVID-19 epidemic is a public health emergency that the world must face. Compared with previous public health emergencies, the spread of COVID-19 is faster due to increased globalization, longer incubation periods, and less symptoms. Clearly, a massive increase in the number of infections could overwhelm the healthcare system [26]. Therefore, it has a significant impact on the management of medical supplies and all aspects of people’s lives.
Faced with the severe shortage of medical supplies, scholars have emphasized the necessity of improving the emergency medical supplies reserve system [27]. The rational allocation of vaccines as medical products in short supply has also become an important research issue. [28] studied the meeting of vaccine needs in developing countries through advance market commitments (AMCs), later models that maximize utility and are outcome-constrained by decision makers on general convex sets help limit the impact of priorities in vaccine allocation [29].
In addition to its impact on the management of medical products, the pandemic can also affect people’s consumption activities and the speed at which emergency times occur. Pandemics could exacerbate the extent of impulsive consumption [30], so the role of mental accounting and loss aversion could be used to achieve research on stimulating consumption with low budgets [31]. Other public health emergencies in the early stage will allow individuals and governments to have an early response in the early stage of the outbreak [32].
2.2.2. Emergency Management of Public Health Emergencies
The emergency management of public health emergencies is an important research field of emergency management. The research mainly focuses on the prediction and evaluation of emergency management of public health emergencies and the research on specific management countermeasures.
The predictive evaluation of emergency management of public health emergencies includes evaluation of public health emergency preparedness and emergency public health management level. Ref. [33] evaluated the current public health emergency preparedness; Ref. [34] based on the emergency management life cycle theory, combined said theory with big data technology for the emergency management application of the 2003 SARS epidemic in China; Ref. [35] studied the evaluation indicators and indicator system of emergency management of public health emergencies in China; and Ref. [36] compared the emergency management strategies under the epidemic situation in two regions of Italy through the method of empirical research to find out the better response strategies.
The research on management countermeasures of public health emergencies can be divided into two branches: attempts to assist management by technical means and the design of management mechanisms. Based on spatial computing, a key issue in public health emergency management, OSCAR (an open space computing and data resource platform) was designed based on spatial computing [37], the use of IoT technology to establish remote public health emergency management system [38], and the construction of a deep learning-based medical material inventory management model [39] were all attempts to use technical means to improve management.
The design of the management mechanism is mainly a multi-agent management structure, including the design of the multi-agent network structure, the adaptive system, and the use of games to realize the multi-agent collaboration.
Ref. [40] defined a framework for the coordination of activities, actors, and resources to achieve emergency management of epidemics; Ref. [41] emphasized the importance of inter-agency communication in an emergency management study on MERS in South Korea; Ref. [42] constructed an analytical framework with five information dimensions for the emergency management of public health emergencies in China to guide the establishment of a multi-agent society Collaborative Network; and Ref. [43] studied the role of integrating the U.S. emergency planning system and local emergency management and public health departments in the context of the COVID-19 pandemic.
Recently, research on the management system of public health emergencies as an adaptive system has also become a hot topic. Ref. [44] found that an adaptive system approach utilizing the principle of complexity can better prepare for the upstream of public health emergency preparedness, and Ref. [45] pointed out that the establishment of a Public Health Emergency Operations Center (PHEOC) enables the optimization of PHEOC activities and their intended objectives.
Considering that the behavioral decisions of multiple subjects often affect each other in the management process, game theory has also been applied to the analysis and management of the behavior of each subject. Ref. [46] used a combination of evolutionary games and system dynamics to study the behavior–strategy interaction of three types of participants: government, community, and residents. Ref. [47] used game theory to develop a framework of the public–private emergency cooperation to meet the need to establish supply chains immediately after an emergency arises.
The available related researches on emergency management of public health emergencies point out the importance of multi-agent collaborative management. Most of the research is carried out from the perspective of systems and networks, and most of them focus on organizational cooperation of different natures. However, the research on the incentive mechanism design in the collaborative management of the healthcare system is not sufficient.
2.3. Collaborative Management
In the development of new products, innovation activities, and emergency management, collaborative management often occurs in activities involving the participation of multiple subjects. While utilizing the advantageous resources of each subject, it often brings about problems related to the coordination of decision-making and incentive measures [48]. This multi-agent collaborative management is often achieved through game models [46,47], supply chain models [48,49,50], and the construction of the system network model [51,52]. Game theory has also become an important method for collaborative management of public health emergencies.
The emergency management of public health emergencies is often characterized by a short timeframe and a large number of tasks. As such, there are often multiple subjects, including behavioral collaborative management [17,18,43] and collaborative communication on information [42].
In the existing literature on the collaborative management of public health emergencies, the application of game theory to the decision-making and coordination research of multiple subjects has emerged. Nevertheless, research on the incentive mechanism design in the collaborative management of the public health emergencies is not sufficient.
2.4. Summary
To intuitively display the differences between our paper and the existing related literature, the contributions to the related literature are summarized in Table 1 to highlight our research opportunities and contributions. Obviously, the available literature rarely touches upon the following critical issues for the public health emergency management system (PES): (1) the optimal operational strategy of enhancing collaborative management and improving governance-driven operational performance/efficiency for the PES; (2) the best incentive mechanism of enhancing collaborative management and improving governance-driven operational performance and efficiency for the PES; (3) the optimal operational decisions of EME and transfer payment intensity for the PES; (4) the impact of performance factor of government department on the governance-driven operational performance and efficiency of the PES. This paper intends to explore the impact of incoordination on the governance-driven operational performance of public health emergency management system (PES) and design an effective collaborative incentive mechanism to improve operational decisions and outcomes of the PES.

Table 1.
Contributions to the related literature.
3. Model Formulation and Analysis
A public health emergency management system (PES) is composed of a government department (e.g., health commission), a center for disease control (CDC), and n medical institutions (e.g., hospitals). Since the CDC is also a special kind of medical institution, the PES can also be regarded as consisting of a government department and medical institutions.
For modeling needs, we mark the serial number of any medical institution as , , where the serial number of CDC is 0. The EME level of the ith medical institution is . The comprehensive EME level of all medical institutions is . Without loss of generality, the effect of unit EME can be set as , where is the fixed effect of unit EME and is the variable effect coefficient of the unit EME. Hence, the comprehensive emergency management effect of all medical institutions is . Since the governance performance of government departments is positively related to the effect of comprehensive emergency management, the governance performance of government department is , where is a governance performance factor of government department and meets . Generally, the cost of EME of the ith medical institution is a quadratic cost structure as , where is the unit cost of the EME level of the ith medical institution, and is the cost factor of the EME level of the ith medical institution.
Based on the above parameter settings, the utility of the ith medical institution equals to the total EME effect of the ith medical institution minus the EME cost of the ith medical institution. Then, the utility functions of the ith medical institution can be expressed as follows:
In order to encourage medical institutions to strengthen the level of EMEs and improve the effect of emergency management, the government department would set the threshold of EMEs for the ith medical institution to build an incentive mechanism of “carrot + Stick”. When the EME level of the ith medical institution exceeds the threshold, the part exceeding the threshold will be rewarded with “carrot”—, respectively. On the contrary, when the EME level of the ith medical institution is lower than the threshold, the part lower than the threshold will be punished with “Stick”—, respectively. Hereinto, is the transfer payment coefficient for the EMS exceeding/below the threshold. For the convenience of modeling, we define the transfer payment coefficient vector . With this setting, the utility of the ith medical institution equals to the total EME effect of the ith medical institution minus the EME cost of the ith medical institution plus the transfer payment from the government department. The utility of the government department equals to the governance performance of the government department minus the total transfer payment to multiple medical institution. Therefore, the utility functions of the ith medical institution and the government department can be respectively expressed as follows:
On this basis, the total utility function of the PES equals to all the medical institutions’ utilities plus the government department’s utility. Then, the total utility function of the PES can be expressed as follows:
Based on the above parameters and model settings, this section will build and analyze the equilibrium decision models under three scenarios: a decentralized decision model without GPI, a decentralized decision model with GPI, and a collaborative decision model with GPI. In order to distinguish different decision scenarios, superscripts/subscripts are introduced: represents the decentralized decision scenario without GPI, represents the decentralized decision scenario with GPI, and represents the collaborative decision scenario with GPI.
3.1. Decentralized Decision Model without GPI ()
In the decentralized decision scenario without GPI, all medical institutions independently make decisions to maximize their own utility, and the government department does not take “carrot + Stick” incentive measures for the emergency management of medical institutions. The decision sequence of the model is as follows: medical institutions make their decisions on their EMEs independently and simultaneously.
Based on the above settings, the optimization problems of the ith medical institution are:
Solving this optimal problem, we can obtain the equilibrium EME of the ith medical institution as follows:
Then, we can obtain the equilibrium comprehensive EME of PES and the effect of unit EME as follows:
Apparently, the equilibrium EME decreases as the costs of the EME levels increase, the equilibrium comprehensive EME of PES decreases as the costs of the EME levels increase, and the equilibrium effect of unit EME deceases as the costs of the EME levels increase.
Then, we can get the equilibrium utility of the ith medical institution and the equilibrium utility of the government department as follows:
Then, the total equilibrium utility of PES is as follows:
Under the decentralized decision scenario without GPI, the equilibrium utilities of medical institutions, government department and the PES decreases as the costs of the EME levels increase.
3.2. Decentralized Decision Model with GPI ()
In the decentralized decision scenario with GPI, all medical institutions independently make decisions to maximize their own utility, and the government department takes “carrot + Stick” incentive measures for the emergency management of medical institutions. The decision sequence of the model is as follows: the government department first decides the threshold of EMEs and the transfer payment coefficient , then medical institutions make their decisions on their EMEs independently and simultaneously.
Based on the above settings, the optimization problems of the ith medical institution are:
Likewise, solving this optimal problem, we can get the equilibrium reaction function of EME of the ith medical institution w.r.t. as follows:
Then, we can obtain the equilibrium reaction function of comprehensive EME of PES and the effect of unit EMEs w.r.t. as follows:
Plugging , and into the utility function of the government department, we can get the optimal problem of the government department as follows:
Solving this optimal problem, we can obtain the equilibrium transfer payment coefficient as follows:
Plugging into , and , we can get the equilibrium EME of the ith medical institution , the equilibrium comprehensive EME of PES and the equilibrium effect of unit EME as follows:
Obviously, the equilibrium EME decreases as the costs of the EME levels increase and increases as the transfer payment coefficient increases. Besides, the equilibrium comprehensive EME of the PES decreases as the costs of the EME levels increase and increases as the transfer payment coefficient increases. Furthermore, the equilibrium effect of unit EME deceases as the costs of the EME levels increase and increases as the transfer payment coefficient increases.
On this basis, we can obtain the equilibrium utility function of the ith medical institution and the equilibrium utility function of the government department w.r.t. as follows:
In order to make the ith medical institution have economic motivation to enhance the level of EME and improve the effect of emergency management, the utility of the ith medical institution under the scenario with GPI should be higher than that without GPI, i.e., the following conditions should be met:
Therefore, the optimal thresholds of EMEs with incentive effect must meet the following conditions:
On this basis, the equilibrium utility of the ith medical institution and the equilibrium utility of the government department are as follows:
Then, the total equilibrium utility of PES is as follows:
Under the decentralized decision scenario with GPI, the equilibrium utilities of medical institutions, government department and the PES decreases as the costs of the EME levels increase.
3.3. Collaborative Decision Model with GPI ()
In the collaborative decision scenario with GPI, all medical institutions collaboratively make decisions to maximize the utility of PES, and the government department takes “carrot + Stick” incentive measures for the emergency management of medical institutions. The decision sequence of the model is as follows: facing the goal of maximizing the utility of emergency management system and Pareto improvement of all the stakeholders’ utility, the government department first decides the threshold of EMEs and the transfer payment coefficient , then medical institutions make their decisions on their EMEs collaboratively and simultaneously.
3.3.1. Centralized Decision Model of PES
Firstly, the optimal problem of PES is as follows:
Solving this optimal problem, we can get the optimal EME of the ith medical institution as follows:
Then, we can obtain the optimal comprehensive EME of PES and the effect of unit EMEs as follows:
Apparently, the equilibrium EME decreases as the costs of the EME levels increases, the equilibrium comprehensive EME of PES decreases as the costs of the EME levels increases, and the equilibrium effect of unit EME deceases as the costs of the EME levels increases.
3.3.2. Decentralized Decision Model of PES
The optimization problem of the ith medical institution under the “carrot + Stick” incentive measures is as follows:
Likewise, solving this optimal problem, we can get the equilibrium reaction function of EME of the ith medical institution w.r.t. as follows:
3.3.3. Collaborative Decision Model of PES
In order to achieve collaborative operations, it is necessary to meet the condition that the EME level under the centralized decision scenario should be consistent with that under the decentralized decision scenario, i.e., . That is,
Solving this equation, we can get the equilibrium transfer payment coefficient as follows:
On this basis, we can obtain the equilibrium utility function of the ith medical institution and the equilibrium utility function of the government department w.r.t. as follows:
In order to make the ith medical institution have economic motivation to enhance the levels of EMEs and improve the effect of emergency management, the utility of the ith medical institution under the scenario with GPI should be higher than that without GPI, i.e., the following conditions should be met:
Therefore, the optimal threshold of EMEs with incentive effect must meet the following conditions:
On this basis, the equilibrium utility of the ith medical institution , the equilibrium utility of the government department and the total equilibrium utility of PES are as follows:
Under the collaborative decision scenario with GPI, the equilibrium utilities of medical institutions, government department and the PES decreases as the costs of the EME levels increase.
3.4. Discussions and Comparisons of Analytical Results
The analytical results of three game-theoretical decision models in this section are summarized and compared in Table 2. Comparing the analytical results of the decentralized decision model without GPI, decentralized decision model with GPI, and collaborative decision model with GPI in Table 2, the key findings are identified below:

Table 2.
Analytical Results of Three Game-Theoretical Decision Models.
- (1)
- the equilibrium EMEs under the decentralized decision model with GPI are higher than those under the decentralized decision model without GPI, and the equilibrium EMEs under the collaborative decision model with GPI are higher than those under the decentralized decision model without GPI when condition 1 holds. Hereinto, condition 1 is the following inequality: .
- (2)
- the equilibrium comprehensive EME of the PES under the decentralized decision model with GPI are higher than those under the decentralized decision model without GPI, and the equilibrium comprehensive EME of the PES under the collaborative decision model with GPI are higher than those under the decentralized decision model without GPI when condition 1 holds.
- (3)
- the equilibrium effect of unit EME under the decentralized decision model with GPI are higher than those under the decentralized decision model without GPI, and the equilibrium effect of unit EME under the collaborative decision model with GPI are higher than those under the decentralized decision model without GPI when condition 1 holds.
4. Numerical and Sensitivity Analyses
Based on the game-theoretical decision models developed and analyzed in Section 4, a hypothetical PES within a large-sized county/small-sized city was selected for numerical and sensitivity analyses. Generally, this PES may be composed of one government department, one CDC, and several large and medium-sized hospitals; for instance, it is assumed that there are five large and medium-sized hospitals () in the county/city. Without losing generality, the fixed effect of unit EME is set at 1000, the variable effect coefficient of unit EME is set at 3, and the performance factor of government departments is set at 0.3, and the cost factor of the EME level of the ith medical institution is set at 100. The unit cost of the EME level of the ith medical institution , and the threshold of EME for the ith medical institution under decentralized decision and collaborative decision scenarios and are shown in Table 3. In the following Section 4.1 and Section 4.2, numerical and sensitivity analyses were conducted based on Matlab R2017b.

Table 3.
Parameter Value Setting.
4.1. Numerical Analysis
Based on the parameter value setting, the numerical analysis results of the decentralized decision model without GPI, the decentralized decision model without GPI, and the collaborative decision model with GPI are shown and compared in Table 4. The numerical analysis results show that:

Table 4.
Numerical Analysis Results.
- (1)
- Comparing the decentralized decision scenario without GPI and that with GPI, the equilibrium EMEs of all medical institutions under the decentralized decision scenario with GPI were higher than those without GPI; the equilibrium utilities of all medical institutions, government departments, and PES under the decentralized decision scenario with GPI, were higher than those without GPI.
- (2)
- Comparing the collaborative decision scenario with GPI and decentralized decision scenario with GPI, the equilibrium EMEs of all medical institutions under the collaborative decision scenario with GPI were higher than those under the decentralized decision scenario with GPI; the equilibrium utilities of all medical institutions, government departments, and PES under the collaborative decision scenario with GPI were higher than those under the decentralized decision scenario with GPI.
- (3)
- Comparing the collaborative decision scenario with GPI and decentralized decision scenario with GPI, the transfer payment coefficients of government department under the collaborative decision scenario with GPI were higher than those under the decentralized decision scenario with GPI.
4.2. Sensitivity Analysis
Based on the above numerical analysis results, the collaborative decision scenario with GPI outperformed the other scenarios regarding the operational decisions and outcomes. Therefore, the sensitivity analysis focused on how the changes of three key parameters of the collaborative decision scenario with GPI impacted the operational decisions and outcomes. These key parameters and their varying range were set as follows: (i) the performance factor of government department (). Taking the original value 0.3 as the baseline value, the upper and lower bound of the interval were set to the baseline value ± 0.2; (ii) the cost factor of EME of the ith medical institution (). Taking the original value 100 as the baseline value, the upper and lower bound of the interval were set to the baseline value ± 5; (iii) the variable effect coefficient of unit EME (). Taking the original value 3.0 as the baseline value, the upper and lower bound of the interval were set to the baseline value ± 2.0. The ± incremental scale and range of the change of each parameter are listed in Table 5, which is followed by the discussion of the sensitivity analysis results for each parameter.

Table 5.
Range of key parameter of sensitivity analysis.
The results of the sensitivity analysis show that:
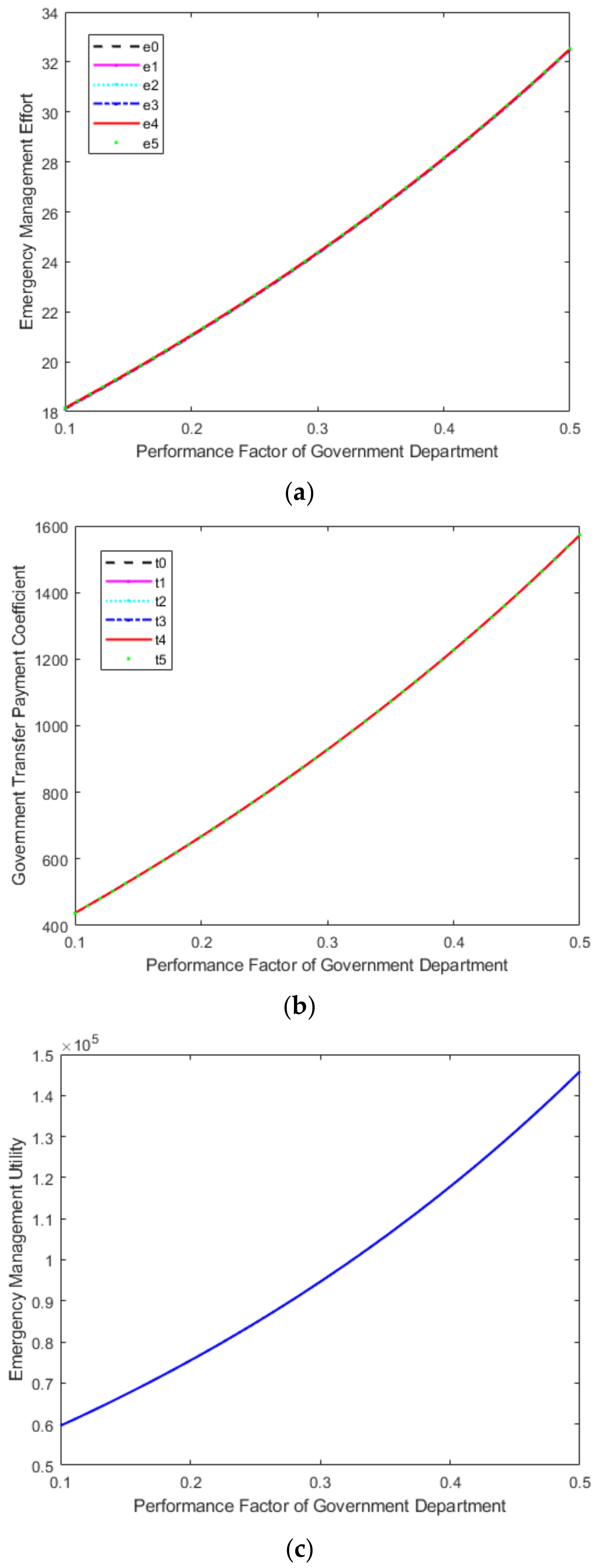
- (1)
- the sensitivity analysis results of performance factor of government department () are shown in Figure 1. As the performance factor of government department increased, the equilibrium EMEs of all medical institutions increased, the equilibrium transfer payment coefficients of the government department for medical institutions increased, and the equilibrium utility of PES increased.
 Figure 1. Impact of performance factor of government department () change on emergency management decisions and outcomes. (a) Effort. (b) Transfer Payment. (c) Utility.
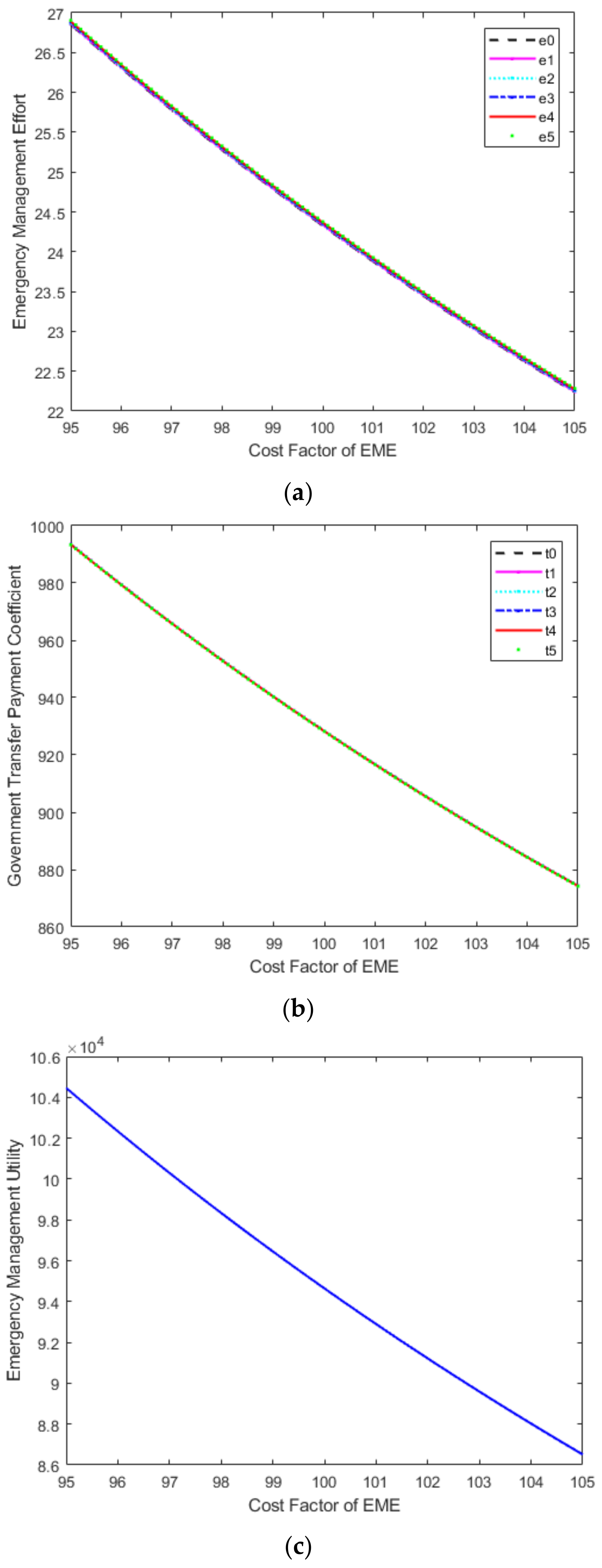
Figure 1. Impact of performance factor of government department () change on emergency management decisions and outcomes. (a) Effort. (b) Transfer Payment. (c) Utility. - (2)
- the sensitivity analysis results of the cost factor of the EME level () are shown in Figure 2. As the cost factor of the EME level increased, the equilibrium EMEs of all medical institutions decreased, the equilibrium transfer payment coefficients of the government department for medical institutions decreased, and the equilibrium utility of PES decreased.
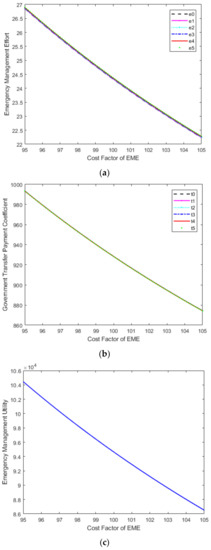 Figure 2. Impact of cost factor of EME () change on emergency management decisions and outcomes. (a) Effort. (b) Transfer Payment. (c) Utility.
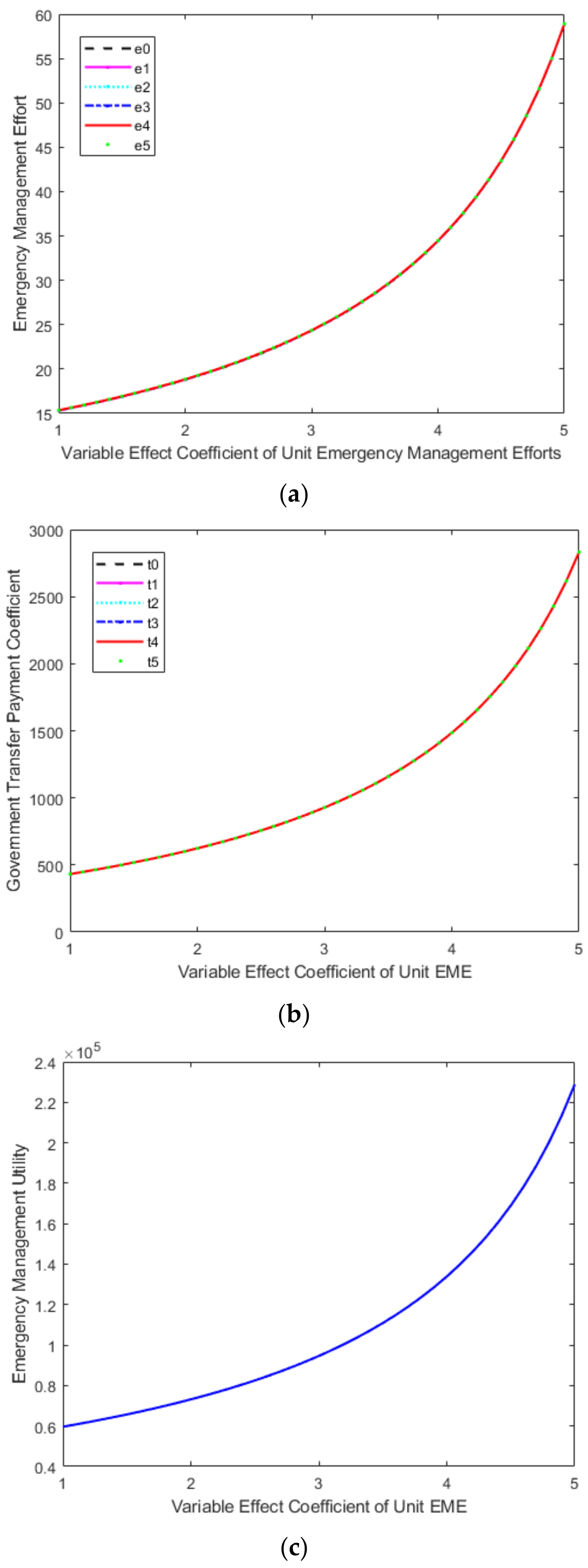
Figure 2. Impact of cost factor of EME () change on emergency management decisions and outcomes. (a) Effort. (b) Transfer Payment. (c) Utility. - (3)
- the sensitivity analysis results of variable effect coefficient of unit EME () are shown in Figure 3. As the variable effect coefficient of unit emergency management increased, the equilibrium EMEs of all medical institutions increased, the equilibrium transfer payment coefficients of the government department for medical institutions increased, and the equilibrium utility of PES increased.
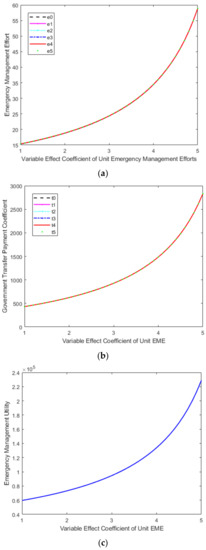 Figure 3. Impact of variable effect coefficient of unit EME () change on emergency management decisions and outcomes. (a) Effort. (b) Transfer Payment. (c) Utility.
Figure 3. Impact of variable effect coefficient of unit EME () change on emergency management decisions and outcomes. (a) Effort. (b) Transfer Payment. (c) Utility.
5. Managerial Insights and Policy Implications
Based on the modelling and numerical analyses, the corresponding managerial insights and policy implications for the public health emergency management system (PES) can be summarized as follows:
- (1)
- The government departments should use the “carrot + stick” type of public governance policy to incentivize medical institutions to strengthen their individual emergency management capabilities, thereby ultimately improving the overall emergency management effectiveness of the PES. For instance, the central government of China and the local government of Hunan province successively introduced a series of incentive policies and measures since February 2020, such as “Notice on several measures to improve the working conditions of frontline medical personnel and effectively care for the physical and mental health of medical personnel”; “Notice on several measures to further stimulate and care for the frontline staff of epidemic prevention and control”; and “Notice on the implementation of personnel and talent inclination policy measures for the frontline professionals and technicians of the prevention and control of the COVID-19 epidemic”, etc. These detailed incentive policies and measures include rapid promotion and advancement, rapid entry into the party for recognition and merit, rapid entry into the cadre (from contract workers to regular workers), and material incentives and subsidies among others. At the same time, incentive and accountability complement each other. Medical personnel who neglect their duties during the war against the epidemic should be strictly held accountable in accordance with relevant regulations, mainly including dismissal, warning, demerit, and other types of accountability measures.
- (2)
- Under the government’s public governance policy incentive, the collaborative decision mode should be adopted by the PES, which would help to improve the overall emergency management efficiency of the PES. In order to integrate the national epidemic and policy information resources, the national government should establish and improve the information sharing platform of the national public health system. This one-stop information service platform could maximize the linked emergency management capabilities of the government and medical institutions and promote the flattening of the organizational structure of the PES. After a public health emergency occurs, information can be directly transmitted and communicated within the PES based on this platform. This will enable medical institutions to provide timely and accurate information for research and judgment, rapidly transfer it to government departments, and quickly and efficiently formulate emergency policies based on the information.
- (3)
- In the PES, the superior government should enhance the performance assessment of emergency management for relevant government departments (i.e., improve the performance factor of government department), which would help to improve the transfer payment of the government department for medical institutions, enhance the emergency management efforts of medical institutions, and improve the overall emergency management efficiency of the PES. In order to improve the enthusiasm and initiative of relevant government departments in emergency management of public health emergencies, the assessment of public health, medical care, and other regular livelihood indicators could be added to the regular performance assessment mechanism of the relevant government. Furthermore, the emergency management of public health emergencies and other relevant indicators that show the responsibility and commitment of the government should be included in the “one vote veto” system, so as to curb the relevant government department’s various inaction behaviors in preventing and responding to public health emergencies and enhance their motivations to implement the policies from the higher government.
- (4)
- In the PES, medical institutions should reduce the costs of emergency management efforts (i.e., the cost factor of the emergency management effort level), which would help to improve the transfer payment of the government department for medical institutions, enhance the emergency management efforts of medical institutions, and improve the overall emergency management efficiency of the PES. In this COVID-19 pandemic, the medical institutions should flexibly adjust the medical materials procurement process in conjunction with the epidemic control situation, reasonably control procurement sources, dynamically manage procurement funds, strictly supervise procurement processes, reasonably use epidemic prevention and control resources, and effectively avoid the waste of medical resources. Furthermore, in large-scale, high-volume, population-based screening, the PES can use mixed-sample nucleic acid testing instead of single-sample nucleic acid testing according to the instructions of the epidemic prevention headquarters. This will improve the detection efficiency and achieve multi-screening, early detection, early isolation, early treatment and timely infection control, and thus effectively reducing emergency management costs.
- (5)
- In the PES, the government department and medical institutions should enhance the effectiveness of emergency management effort (i.e., the variable effect coefficient of unit emergency management effort), which would help to enhance the emergency management efforts of medical institutions and improve the overall emergency management efficiency of the PES. In the epidemiological investigation, the government department should make full use of technical means and big data information support to identify all close contacts, sub-close contacts, and general contacts of infected persons and other key populations quickly and accurately and catch the source of epidemic transmission precisely. Furthermore, based on the number of infected persons and trajectory investigation, medical institutions should propose the delineation of sealing control areas, control areas and prevention areas, report to the epidemic prevention and control command for approval and announcement, and propose dynamic adjustments according to the progress of epidemic prevention and control. Besides, the government department should delineate prevention and control areas scientifically, implement classification management measures more precisely, and curb the spread of the epidemic in the community effectively. These measures would effectively achieve the maximum prevention and control effect at the minimum cost and minimize the impact of the epidemic on economic and social development. Moreover, the government department should change the scope of nucleic acid testing from “full personnel” to “regional personnel” and scientifically define the size of the region according to the objective needs of epidemic prevention and control. Medical institutions could use nucleic acid testing in conjunction with antigen testing to enhance the quality control of nucleic acid testing, improve the effectiveness of accurate testing, and achieve the accurate prevention and control of epidemics.
6. Conclusions
Due to the lack of a coordination mechanism in public health emergency management, the emergency management ability of medical institutions is weakened, and the emergency management efficiency of the PES is reduced. This paper tries to investigate the impact of incoordination on the governance-driven operational performance of public health emergency management system (PES) and design an effective collaborative incentive mechanism to improve operational decisions and outcomes of PES. Three different game-theoretical decision models, including a decentralized decision model without GPI, a decentralized decision model with GPI, and a collaborative decision model with GPI, are developed, analyzed, and compared for the PES, and then the corresponding numerical and sensitivity analyses are implemented and compared. On this basis, the corresponding managerial insights and policy implications are discussed and summarized. The research results show that: (1) the collaborative decision scenario with GPI performs best, and the decentralized decision scenario with GPI performs second-best regarding the equilibrium of EMEs and utilities in all the decision scenarios; (2) an incentive mechanism of “carrot + Stick” can effectively enhance the collaborative management of public health emergencies and its governance-driven operational performance and efficiency; (3) strengthening the performance assessment of emergency management for relevant government departments is beneficial in improving the overall emergency management efficiency of the PES; (4) reducing the cost of EMEs and enhancing the effectiveness of EME are conducive to improving the overall emergency management efficiency of the PES.
For lack of relevant literature, limited research funds, and difficulty in collecting empirical data, this study focuses mainly on the theoretical exploration of the incentive mechanism design for the collaborative management of public health emergencies. Even though insightful findings are discovered, some important research issues are still worthy of further exploration in the future. First, the impact of different decision structures on the operational decisions and outcomes in the PES can be further studied. Second, the screening game can be formulated and analyzed to investigate the impact of asymmetric information of all medical institutions’ cost type on the operational decisions and outcomes in the PES in future research. Third, more incentive structures can be further developed via different contracts based on different governance practices of public health emergencies in different countries and regions. Finally, empirical studies of specific sample PES cases from different countries and regions may be conducted in our future research.
Author Contributions
Investigation, X.L.; Supervision, C.W.; Writing–original draft, Y.H.; Writing—review & editing, Z.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Humanities and Social Science Youth Fund of Ministry of Education of P.R. China (Grant No. 21YJC790017), Excellent project of Jiangsu Social Science Application Research (Grant Nos. 21SYA-012, 22SKB-10), Jiangsu Provincial Hospital Association (Grant No. JSYGY-3-2021-533), Humanities and social sciences fund project of Jiangsu Provincial Department of Education (Grant No. SJCX20-0473), National Natural Science Foundation of China (Grant No. 71603125), China Scholarship Council (Grant No. 201706865020), and Young Leading Talent Program of Nanjing Normal University.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 13 April 2022).
- Wei, X.; Li, L.; Zhang, F. The impact of the COVID-19 pandemic on socio-economic and sustainability. Environ. Sci. Pollut. Res. 2021, 28, 68251–68260. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Liu, G.; Mai, T.H.T.; Li, T.T. Research on the Allocation of 3D Printing Emergency Supplies in Public Health Emergencies. Front. Public Health 2021, 9, 657276. [Google Scholar] [CrossRef] [PubMed]
- Cao, D. Xi Urges Redoubling Contagion Fight. 2020. Available online: https://www.chinadaily.com.cn/a/202002/11/WS5e41adefa31012821727670d.html (accessed on 11 April 2020).
- Abubakar, I.; Dalglish, S.L.; Ihekweazu, A.C.; Bolu, O.; Aliyu, S.H. Lessons from co-production of evidence and policy in Nigeria’s COVID-19 response. BMJ Glob. Health 2021, 6, e004793. [Google Scholar] [CrossRef] [PubMed]
- Dalglish, S.L. COVID-19 gives the lie to global health expertise. Lancet 2020, 395, 1189. [Google Scholar] [CrossRef]
- Lal, A.; Erondu, N.A.; Heymann, D.L.; Gitahi, G.; Yates, R. Fragmented health systems in COVID-19: Rectifying the misalignment between global health security and universal health coverage. Lancet 2021, 397, 61–67. [Google Scholar] [CrossRef]
- Kang, L.; Li, Y.; Hu, S.; Chen, M.; Yang, C.; Yang, B.X.; Wang, Y.; Hu, J.; Lai, J.; Ma, X.; et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020, 7, e14. [Google Scholar] [CrossRef]
- Zhang, X.; Yang, S. “A community system”: A critical foundation for the epidemic prevention and control of SARS-CoV-2. Int. J. Health Plan. Manag. 2020, 35, 1246–1249. [Google Scholar] [CrossRef]
- Rangachari, P.; Woods, J.L. Preserving Organizational Resilience, Patient Safety, and Staff Retention during COVID-19 Requires a Holistic Consideration of the Psychological Safety of Healthcare Workers. Int. J. Environ. Res. Public Health 2020, 17, 4267. [Google Scholar] [CrossRef]
- Sheather, J.; Slattery, D. The great resignation—How do we support and retain staff already stretched to their limit? BMJ 2021, 375, n2533. [Google Scholar] [CrossRef]
- Shader, R.I.; Schwartz, A.J. Management of Reactions to Disaster. Soc. Work 1966, 11, 99–104. [Google Scholar] [CrossRef]
- Blanchard, B.W.; Canton, L.C.; Cwiak, C.L.; Goss, K.C.; McEntire, D.A.; Newsome, L.; Selves, M.D.; Sorchik, E.A.; Stenson, K.; Turner, J.E.; et al. Principles of Emergency Management Supplement; Federal Emergency Management Agency: Washington, DC, USA, 2007. [CrossRef]
- Huang, D.; Wang, S.; Liu, Z. A systematic review of prediction methods for emergency management. Int. J. Disaster Risk Reduct. 2021, 62, 102412. [Google Scholar] [CrossRef]
- Shareef, M.A.; Dwivedi, Y.K.; Mahmud, R.; Wright, A.; Rahman, M.M.; Kizgin, H.; Rana, N.P. Disaster management in Bangladesh: Developing an effective emergency supply chain network. Ann. Oper. Res. 2019, 283, 1463–1487. [Google Scholar] [CrossRef]
- Resodihardjo, S.L.; Van Genugten, M.; Ruiter, M.N. A theoretical exploration of resilience and effectiveness requirements’ compatibility in formal and permanent emergency networks. Saf. Sci. 2018, 101, 164–172. [Google Scholar] [CrossRef]
- Huang, H.-C.; Gao, H.-F. Game Analysis of Behavior Choice on Construction of the Social Emergency Rescue System Between Government and Enterprises. IEEE Access 2020, 8, 149595–149601. [Google Scholar] [CrossRef]
- Fan, B.; Liu, R.; Huang, K.; Zhu, Y. Embeddedness in cross-agency collaboration and emergency management capability: Evidence from Shanghai’s urban contingency plans. Gov. Inf. Q. 2019, 36, 101395. [Google Scholar] [CrossRef]
- Shen, Z.M.; Sun, Y. Strengthening supply chain resilience during COVID-19: A case study of JD.com. J. Oper. Manag. 2021, 1–25. [Google Scholar] [CrossRef]
- Meng, Q. A Study on the Urban Emergency Management System Based on the Internet of Things. In Proceedings of the International Conference on Management Science and Engineering Management, Ontario, ON, Canada, 5–8 August 2019; Springer: Cham, Switzerland, 2019; pp. 645–655. [Google Scholar]
- Jia, D.; Wu, Z. Intelligent Evaluation System of Government Emergency Management Based on BP Neural Network. IEEE Access 2020, 8, 199646–199653. [Google Scholar] [CrossRef]
- Chen, Y.; Zhao, X.; Rich, E.; Luna-Reyes, L.F. Decision Models and Group Decision Support Systems for Emergency Management and City Resilience. In Research Anthology on Decision Support Systems and Decision Management in Healthcare, Business, and Engineering; IGI Global: Hershey, PA, USA, 2021; pp. 723–740. [Google Scholar]
- Ceschia, S.; Schaerf, A. Modeling and solving the dynamic patient admission scheduling problem under uncertainty. Artif. Intell. Med. 2012, 56, 199–205. [Google Scholar] [CrossRef]
- Guido, R.; Solina, V.; Mirabelli, G.; Conforti, D. Offline Patient Admission, Room and Surgery Scheduling Problems. In New Trends in Emerging Complex Real Life Problems; Daniele, P., Scrimali, L., Eds.; AIRO Springer Series; Springer: Cham, Switzerland, 2018; Volume 1, pp. 275–283. [Google Scholar] [CrossRef]
- Bastos, L.S.; Marchesi, J.F.; Hamacher, S.; Fleck, J.L. A mixed integer programming approach to the patient admission scheduling problem. Eur. J. Oper. Res. 2019, 273, 831–840. [Google Scholar] [CrossRef]
- Ye, J. The Role of Health Technology and Informatics in a Global Public Health Emergency: Practices and Implications From the COVID-19 Pandemic. JMIR Med. Inform. 2020, 8, e19866. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, X.; He, J. Challenges to the system of reserve medical supplies for public health emergencies: Reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Biosci. Trends 2020, 14, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Kremer, M.; Levin, J.; Snyder, C.M. Designing Advance Market Commitments for New Vaccines. Manag. Sci. 2022, 1–29. [Google Scholar] [CrossRef]
- Breugem, T.; Van Wassenhove, L.N. The Price of Imposing Vertical Equity Through Asymmetric Outcome Constraints. Manag. Sci. 2022, 1–17. [Google Scholar] [CrossRef]
- Li, M.; Zhao, T.; Huang, E.; Li, J. How does a public health emergency motivate People’s impulsive consumption? An empirical study during the COVID-19 outbreak in China. Int. J. Environ. Res. Public Health 2020, 17, 5019. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Shen, Q.; Li, Z.; Chen, S. Stimulating Consumption at Low Budget: Evidence from a Large-Scale Policy Experiment Amid the COVID-19 Pandemic. Manag. Sci. 2021, 67, 7291–7307. [Google Scholar] [CrossRef]
- Ru, H.; Yang, E.; Zou, K. Combating the COVID-19 Pandemic: The Role of the SARS Imprint. Manag. Sci. 2021, 67, 5606–5615. [Google Scholar] [CrossRef]
- Chiossi, S.; Tsolova, S.; Ciotti, M. Assessing public health emergency preparedness: A scoping review on recent tools and methods. Int. J. Disaster Risk Reduct. 2021, 56, 102104. [Google Scholar] [CrossRef]
- Mao, Z.; Zou, Q.; Yao, H.; Wu, J. The application framework of big data technology in the COVID-19 epidemic emergency management in local government—A case study of Hainan Province, China. BMC Public Health 2021, 21, 147. [Google Scholar] [CrossRef]
- Wang, J.; Yuan, B.; Li, Z. Evaluation of Public Health Emergency Management in China: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 3478. [Google Scholar] [CrossRef]
- Troisi, R.; Alfano, G. Is regional emergency management key to containing COVID-19? A comparison between the regional Italian models of Emilia-Romagna and Veneto. Int. J. Public Sect. Manag. 2021, 35, 195–210. [Google Scholar] [CrossRef]
- Guo, D.; Zhu, Y.; Yin, W. OSCAR: A framework to integrate spatial computing ability and data aggregation for emergency management of public health. GeoInformatica 2018, 22, 383–410. [Google Scholar] [CrossRef]
- Feng, Y.; Pan, Z. Optimization of Remote Public Medical Emergency Management System with Low Delay Based on Internet of Things. J. Health Eng. 2021, 2021, 5570500. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Gan, W.; Li, Z. Application of Medical Material Inventory Model Under Deep Learning in Supply Planning of Public Emergency. IEEE Access 2021, 9, 44128–44138. [Google Scholar] [CrossRef]
- Margherita, A.; Elia, G.; Klein, M. Managing the COVID-19 emergency: A coordination framework to enhance response practices and actions. Technol. Forecast. Soc. Chang. 2021, 166, 120656. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Jung, K. Dynamics of Interorganizational Public Health Emergency Management Networks: Following the 2015 MERS Response in South Korea. Asia Pac. J. Public Health 2018, 30, 207–216. [Google Scholar] [CrossRef]
- Huang, H.; Peng, Z.; Wu, H.; Xie, Q. A big data analysis on the five dimensions of emergency management information in the early stage of COVID-19 in China. J. Chin. Gov. 2020, 5, 213–233. [Google Scholar] [CrossRef]
- Wolf-Fordham, S. Integrating Government Silos: Local Emergency Management and Public Health Department Collaboration for Emergency Planning and Response. Am. Rev. Public Adm. 2020, 50, 560–567. [Google Scholar] [CrossRef]
- Khan, Y.; O’Sullivan, T.; Brown, A.; Tracey, S.; Gibson, J.; Généreux, M.; Schwartz, B. Public health emergency prepared-ness: A framework to promote resilience. BMC Public Health 2018, 18, 1344. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Huang, Y.; Zheng, Z.-J. Leveraging the Public Health Emergency Operation Center (PHEOC) for pandemic response: Opportunities and challenges. Glob. Health J. 2020, 4, 118–120. [Google Scholar] [CrossRef]
- Fan, R.; Wang, Y.; Lin, J. Study on Multi-Agent Evolutionary Game of Emergency Management of Public Health Emergencies Based on Dynamic Rewards and Punishments. Int. J. Environ. Res. Public Health 2021, 18, 8278. [Google Scholar] [CrossRef] [PubMed]
- Diehlmann, F.; Lüttenberg, M.; Verdonck, L.; Wiens, M.; Zienau, A.; Schultmann, F. Public-private collaborations in emergency logistics: A framework based on logistical and game-theoretical concepts. Saf. Sci. 2021, 141, 105301. [Google Scholar] [CrossRef]
- Bhaskaran, S.; Krishnan, V. Effort, Revenue, and Cost Sharing Mechanisms for Collaborative New Product Development. Manag. Sci. 2009, 55, 1152–1169. [Google Scholar] [CrossRef]
- Nip, K.; Wang, C.; Wang, Z. Competitive and Cooperative Assortment Games under Markov Chain Choice Model. Prod. Oper. Manag. 2021, 31, 1033–1051. [Google Scholar] [CrossRef]
- Chen, Y.; Özer, Ö. Supply Chain Contracts That Prevent Information Leakage. Manag. Sci. 2019, 65, 5449–5956. [Google Scholar] [CrossRef]
- Balcik, B.; Silvestri, S.; Rancourt, M.È.; Laporte, G. Collaborative prepositioning network design for regional disaster response. Prod. Oper. Manag. 2019, 28, 2431–2455. [Google Scholar] [CrossRef]
- Qiu, Y.; Shi, M.; Zhao, X.; Jing, Y. System dynamics mechanism of cross-regional collaborative dispatch of emergency supplies based on multi-agent game. Complex Intell. Syst. 2021, 1–12. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).