Physical Activity and Healthy Habits Influence Mood Profile Clusters in a Lithuanian Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Data Screening and Descriptive Statistics
3.2. Cluster Analysis
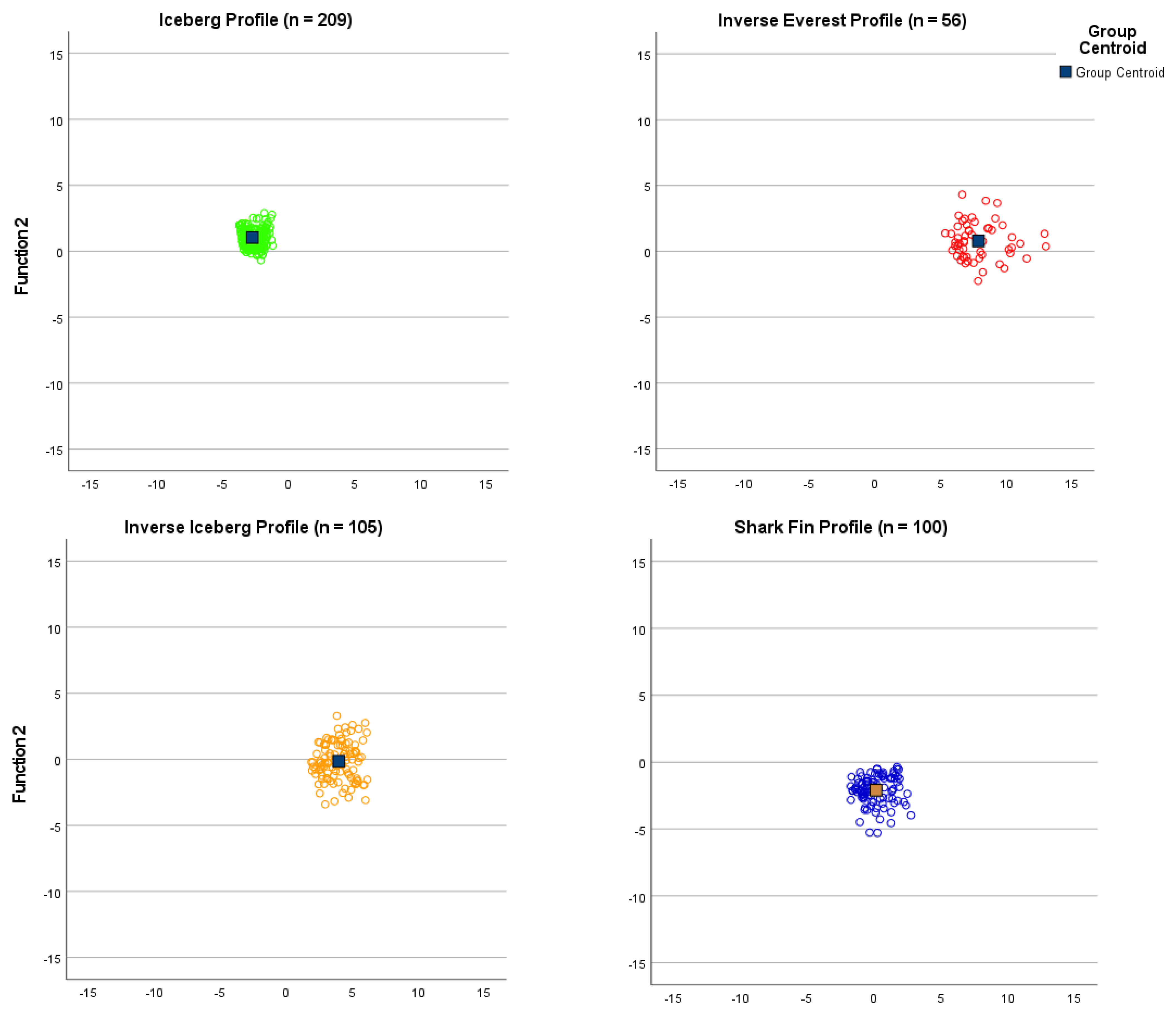
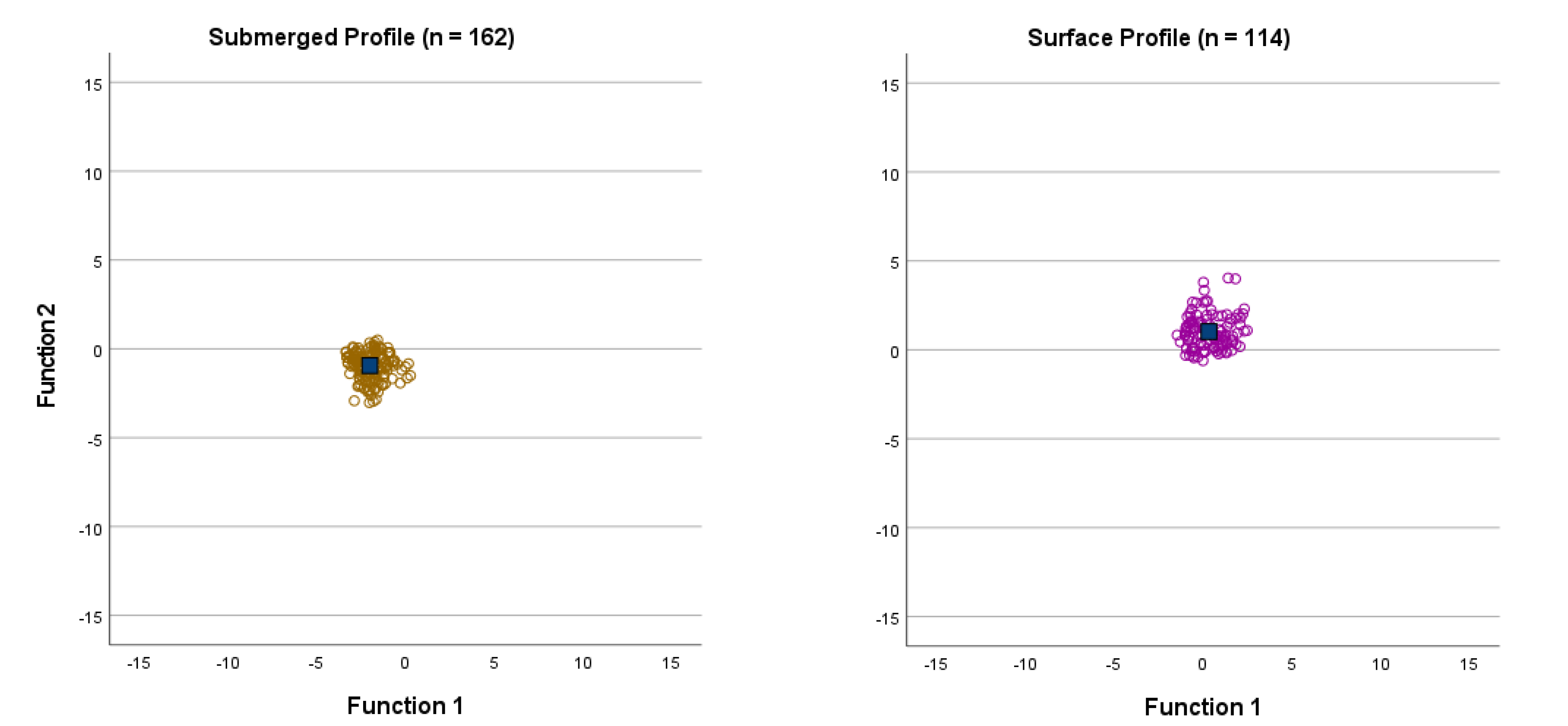
3.3. Cluster Strength
3.4. Cluster Prevalence
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gross, J.J.; Uusberg, H.; Uusberg, A. Mental illness and well-being: An affect regulation perspective. World Psychiat. 2019, 18, 130–139. [Google Scholar] [CrossRef]
- Ritchie, H.; Roser, M. Mental Health. 2018. Available online: https://ourworldindata.org/mental-health (accessed on 6 January 2022).
- Ammar, A.; Chtourou, H.; Boukhris, O.; Trabelsi, K.; Masmoudi, L.; Brach, M.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. COVID-19 home confinement negatively impacts social participation and life satisfaction: A worldwide multicenter study. Int. J. Environ. Res. Public Health 2020, 17, e6237. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of Depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Terry, P.C.; Parsons-Smith, R.L.; Terry, V.R. Mood responses associated with COVID-19 restrictions. Front. Psychol. 2020, 11, e589598. [Google Scholar] [CrossRef] [PubMed]
- Gataūlinas, A. Subjective well-being of Lithuanian society in the context of European Union countries. Vilniaus Univ. 2013, 1, 1–36. Available online: https://epublications.vu.lt/object/elaba:1822140/index/html (accessed on 8 August 2022).
- Puras, D.; Germanavicius, A.; Povilaitis, R.; Veniute, M.; Jasilionis, D. Lithuania mental health country profile. Int. Rev. Psychiat. 2004, 16, 117–125. [Google Scholar] [CrossRef]
- Puras, D.; Kolaitis, G.; Tsiantis, J. Child and adolescent mental health in the enlarged European Union: Overview of the CAMHEE project. Int. J. Ment. Health Prom. 2010, 12, 3–9. [Google Scholar] [CrossRef]
- Terry, P.C.; Lane, A.M.; Lane, H.J.; Keohane, L. Development and validation of a mood measure for adolescents. J. Sport Sci. 1999, 17, 861–872. [Google Scholar] [CrossRef]
- Terry, P.C.; Lane, A.M.; Fogarty, G.J. Construct validity of the Profile of Mood States–Adolescents for use with adults. Psychol. Sport Exerc. 2003, 4, 125–139. [Google Scholar] [CrossRef]
- Terry, P.C.; Skurvydas, A.; Lisinskiene, A.; Majauskiene, D.; Valanciene, D.; Cooper, S.; Lochbaum, M. Validation of a Lithuanian-language version of the Brunel Mood Scale: The BRUMS-LTU. Int. J. Environ. Res. Public Health 2022, 19, e4867. [Google Scholar] [CrossRef]
- Morgan, W.P. Selected psychological factors limiting performance: A mental health model. In Limits of Human Performance; Clarke, D.H., Eckert, H.M., Eds.; Human Kinetics: Champaign, IL, USA, 1985; pp. 70–80. [Google Scholar]
- Lane, A.M.; Terry, P.C. The nature of mood: Development of a conceptual model with a focus on depression. J. Appl. Sport Psychol. 2000, 12, 16–33. [Google Scholar] [CrossRef]
- Beedie, C.J.; Terry, P.C.; Lane, A.M. Distinctions between emotion and mood. Cogn. Emot. 2005, 19, 847–878. [Google Scholar] [CrossRef]
- Siemer, M. Mood experience: Implications of a dispositional theory of moods. Emot Rev. 2009, 1, 256–263. [Google Scholar] [CrossRef]
- McNair, D.M.; Lorr, M.; Droppelman, L.F. Manual for the Profile of Mood States; Educational and Industrial Testing Services: San Diego CA, USA, 1971. [Google Scholar]
- McNair, D.M.; Lorr, M.; Droppelman, L.F. Revised Manual for the Profile of Mood States; Educational and Industrial Testing Services: San Diego CA, USA, 1992. [Google Scholar]
- Ekkekakis, P. The Measurement of Affect, Mood, and Emotion: A Guide for Health-Behavioral Research; Cambridge University Press: New York, NY, USA, 2013. [Google Scholar]
- Morgan, W.P.; Brown, D.R.; Raglin, J.S.; O’Connor, P.J.; Ellickson, K.A. Psychological monitoring of overtraining and staleness. Br. J. Sports Med. 1987, 21, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Beedie, C.J.; Terry, P.C.; Lane, A.M. The Profile of Mood States and athletic performance: Two meta-analyses. J. Appl. Sport. Psychol. 2000, 12, 49–68. [Google Scholar] [CrossRef]
- Lochbaum, M.; Zanatta, T.; Kirschling, D.; May, E. The Profile of Moods States and athletic performance: A meta-analysis of published studies. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 50–70. [Google Scholar] [CrossRef]
- Budgett, R. Fatigue and underperformance in athletes: The overtraining syndrome. Br. J. Sports Med. 1988, 32, 107–110. [Google Scholar] [CrossRef]
- Terry, P.C. The efficacy of mood state profiling with elite performers: A review and synthesis. Sport Psychol. 1995, 9, 309–324. [Google Scholar] [CrossRef]
- Parsons-Smith, R.L.; Terry, P.C.; Machin, M.A. Identification and description of novel mood profile clusters. Front. Psychol. 2017, 8, e1958. [Google Scholar] [CrossRef]
- Terry, P.C.; Parsons-Smith, R.L. Identification and incidence of mood profile clusters among sport participants. J. Sci. Med. Sport. 2019, 22, S100. [Google Scholar] [CrossRef]
- Van Wijk, C.H.; Martin, J.H.; Hans-Arendse, C. Clinical utility of the Brunel Mood Scale in screening for post-traumatic stress risk in a military population. Mil. Med. 2013, 178, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Galambos, S.A.; Terry, P.C.; Moyle, G.M.; Locke, S.A. Psychological predictors of injury among elite athletes. Br. J. Sports Med. 2005, 39, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Parsons-Smith, R.L. In the Mood: Online Mood Profiling, Mood Response Clusters and Mood-Performance Relationships in High-Risk Vocations. Ph.D. Thesis, University of Southern Queensland, Darling Heights, QLD, Australia, 2015. Unpublished. [Google Scholar]
- Sobhani, V.; Rostamizadeh, M.; Hosseini, S.; Hashemi, S.; Refoyo Román, I.; Mon-López, D. Anthropometric, physiological, and psychological variables that determine the elite pistol performance of women. Int. J. Environ. Res. Public Health 2022, 19, 1102. [Google Scholar] [CrossRef]
- Brandão, R.F.; Correa, M.; Sermarine, M.; Angelo, D.L.; Parsons-Smith, R.L.; Terry, P.C. Psychometric re-evaluation of the Brazil Mood Scale and evidence of mood profile clusters among youth athletes in Brazil. In Proceedings of the International Society of Sport Psychology (ISSP) 15th World Congress Proceedings, Taipei, Taiwan, 30 September–4 October 2021; pp. S183–S184. [Google Scholar] [CrossRef]
- Terry, P.C.; Parsons-Smith, R.L.; Zhang, C.Q.; Si, G.; Chung, P.K. Mood profile clusters among Chinese athletes and nonathletes. In Proceedings of the International Society of Sport Psychology (ISSP) 15th World Congress Proceedings, Taipei, Taiwan, 30 September–4 October 2021; pp. S182–S183. [Google Scholar] [CrossRef]
- Terry, P.C.; Parsons-Smith, R.L.; King, R.; Terry, V.R. Influence of sex, age, and education on mood profile clusters. PLoS ONE 2021, 16, e0245341. [Google Scholar] [CrossRef]
- Quartiroli, A.; Parsons-Smith, R.L.; Fogarty, G.J.; Kuan, G.; Terry, P.C. Cross-cultural validation of mood profile clusters in a sport and exercise context. Front. Psychol. 2018, 9, e1949. [Google Scholar] [CrossRef]
- Han, C.; Parsons-Smith, R.L.; Terry, P.C. Mood profiling in Singapore: Cross-cultural validation and potential applications of mood profile clusters. Front. Psychol. 2020, 11, e665. [Google Scholar] [CrossRef]
- Brandt, R.; Herrero, D.; Massetti, T.; Crocetta, T.B.; Guarnieri, R.; Monteiro, C.B.D.M.; Viana, M.D.S.; Bevilacqua, G.G.; de Abreu, L.C.; Andrade, A. The Brunel Mood Scale rating in mental health for physically active and apparently healthy populations. Health 2016, 8, 125–132. [Google Scholar] [CrossRef]
- Sties, S.W.; Gonzáles, A.I.; Netto, A.S.; Wittkopf, P.G.; Lima, D.P.; Carvalho, T. Validation of the Brunel Mood Scale for cardiac rehabilitation program. Br. J. Sports Med. 2014, 20, 281–284. [Google Scholar] [CrossRef]
- Yatabe, K.; Yui, N.; Kasuya, S.; Fujiya, H.; Tateishi, K.; Terawaki, F.; Yoshida, A.; Yoshioka, H.; Terauchi, K.; Miyano, H.; et al. Anxiety and Mood among Ballet Dancers: A Pilot Study on Effects of a Medical Approach Involving Periodic Intervention. 2014. Available online: https://www.researchgate.net/publication/272791152 (accessed on 6 January 2021).
- Gould, M.S.; Marrocco, F.A.; Kleinman, M.; Thomas, J.G.; Mostkoff, K.; Côté, J.; Davies, M. Evaluating iatrogenic risk of youth suicide screening programs: A randomized controlled trial. JAMA 2005, 29, 1635–1643. [Google Scholar] [CrossRef]
- European Institute for Gender Equality. Gender Equality Index 2021—Lithuania. Available online: https://eige.europa.eu/gender-equality-index/2021/country/LT (accessed on 1 February 2022).
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiat. 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef] [PubMed]
- Remmers, C.; Topolinski, S.; Koole, S.L. Why being mindful may have more benefits than you realize: Mindfulness improves both explicit and implicit mood regulation. Mindfulness 2016, 7, 829–837. [Google Scholar] [CrossRef]
- Bravo, A.J.; Boothe, L.G.; Pearson, M.R. Getting personal with mindfulness: A latent profile analysis of mindfulness and psychological outcomes. Mindfulness 2016, 7, 420–432. [Google Scholar] [CrossRef]
- Ford, C.G.; Wilson, J.M.; Altman, N.; Strough, J.; Shook, N.J. Profiles of mindfulness across adulthood. Mindfulness 2020, 11, 1557–1569. [Google Scholar] [CrossRef]
- Khantzian, E.J. The self medication hypothesis of substance use disorders: A reconsideration and recent applications. Harv. Rev. Psychiatry 1997, 4, 231–244. [Google Scholar] [CrossRef]
- Turner, S.; Mota, N.; Bolton, J.; Sareen, J. Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depress. Anxiety 2018, 35, 851–860. [Google Scholar] [CrossRef]
- Mojtabai, R.; Crum, R.M. Cigarette smoking and onset of mood and anxiety disorders. Am. J. Public Health 2013, 103, 1656–1665. [Google Scholar] [CrossRef]
- Lawrence, D.; Mitrou, F.; Zubrick, S.R. Smoking and mental illness: Results from population surveys in Australia and the United States. BMC Public Health 2009, 9, 285. [Google Scholar] [CrossRef]
- Baum-Baicker, C. The psychological benefits of moderate alcohol consumption: A review of the literature. Drug Alcohol. Depend. 1985, 15, 305–322. [Google Scholar] [CrossRef]
- Crum, R.M.; Mojtabai, R.; Lazareck, S.; Bolton, J.M.; Robinson, J.; Sareen, J.; Green, K.M.; Stuart, E.A.; La Flair, L.; Alvanzo, A.A.H.; et al. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry 2013, 70, 178–726. [Google Scholar] [CrossRef]
- Mäkelä, P.; Raitasalo, K.; Wahlbeck, K. Mental health and alcohol use: A cross-sectional study of the Finnish general population. Eur. J. Public Health. 2015, 25, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Stein, R.I.; Kenardy, J.; Wiseman, C.V.; Dounchis, J.Z.; Arnow, B.A.; Wilfley, D.E. What’s driving the binge in binge eating disorder? A prospective examination of precursors and consequences. Int. J. Eat. Disord. 2007, 40, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Razzoli, M.; Pearson, C.; Crow, S.; Bartolomucci, A. Stress, overeating, and obesity: Insights from human studies and preclinical models. Neurosci. Biobehav. Rev. 2017, 76 Pt A, 154–162. [Google Scholar] [CrossRef]
- Bradshaw, T.; Mairs, H. Obesity and serious mental ill health: A critical review of the literature. Healthcare 2014, 2, 166–182. [Google Scholar] [CrossRef]
- Chekroud, S.R.; Gueorguieva, R.; Zheutlin, A.B.; Paulus, M.; Krumholz, H.M.; Krystal, J.H.; Chekroud, A.M. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: A cross-sectional study. Lancet Psychiatry 2018, 5, 739–746. [Google Scholar] [CrossRef]
- de Rezende, L.F.; Rodrigues Lopes, M.; Rey-López, J.P.; Matsudo, V.K.; Luiz, O. Sedentary behavior and health outcomes: An overview of systematic reviews. PLoS ONE 2014, 9, e105620. [Google Scholar] [CrossRef]
- Karageorghis, C.I.; Bird, J.M.; Hutchinson, J.C.; Hamer, M.; Delevoye-Turrell, Y.N.; Guérin, S.M.R.; Mullin, E.M.; Mellano, K.T.; Parsons-Smith, R.L.; Terry, V.R.; et al. Physical activity and mental well-being under COVID-19 lockdown: A cross-sectional multination study. BMC Public Health 2021, 21, 988. [Google Scholar] [CrossRef]
- Terry, P.C.; Potgieter, J.R.; Fogarty, G.J. The Stellenbosch Mood Scale: A dual-language measure of mood. Int. J. Sport Exerc. Psychol. 2003, 1, 231–245. [Google Scholar] [CrossRef]
- Hasan, M.M.; Khan, M.H.A. Bangla version of the Brunel Mood Scale (BRUMS): Validity, measurement invariance and normative data in non-clinical sample. Heliyon 2022, 8, e09666. [Google Scholar] [CrossRef]
- Rohlfs, I.C.P.M.; Rotta, T.M.; Luft, C.B.; Andrade, A.; Krebs, R.J.; Carvalho, T. Brunel Mood Scale (BRUMS): An instrument for early detection of overtraining syndrome. Rev. Br. Med. Esporte 2008, 14, 176–181. [Google Scholar] [CrossRef]
- Zhang, C.Q.; Si, G.; Chung, P.K.; Du, M.; Terry, P.C. Psychometric properties of the Brunel Mood Scale in Chinese adolescents and adults. J. Sport Sci. 2014, 32, 1465–1476. [Google Scholar] [CrossRef] [PubMed]
- Květon, P.; Jelínek, M.; Burešová, I.; Bartošová, K. Czech adaptation of the Brunel Mood States for adolescent athletes. Studia Sport. 2020, 14, 47–57. Available online: https://journals.muni.cz/studiasportiva/article/viewFile/12758/11609 (accessed on 6 January 2021). [CrossRef]
- Rouveix, M.; Duclos, M.; Gouarne, C.; Beauvieux, M.C.; Filaire, E. The 24h urinary cortisol/cortisone ratio and epinephrine/norepinephrine ratio for monitoring training in young female tennis players. Int. J. Sport Med. 2006, 27, 856–863. [Google Scholar] [CrossRef]
- Lane, A.M.; Soos, I.; Leibinger, E.; Karsai, I.; Hamar, P. Validity of the Brunel Mood Scale for use with UK, Italian and Hungarian athletes. In Mood and Human Performance: Conceptual, Measurement, and Applied Issues; Lane, A.M., Ed.; Nova Science: Hauppauge, NY, USA, 2007; pp. 119–130. [Google Scholar]
- Quartiroli, A.; Terry, P.C.; Fogarty, G.J. Development and initial validation of the Italian Mood Scale (ITAMS) for use in sport and exercise contexts. Front. Psychol. 2017, 8, e1483. [Google Scholar] [CrossRef] [PubMed]
- Yatabe, K.; Oyama, T.; Fujiya, H.; Kato, H.; Seki, H.; Kohno, T. Development and validation of the preliminary Japanese version of the Profile of Mood States for adolescents. St. Marian. Med. J. 2006, 32, 539–547. [Google Scholar]
- Hashim, H.A.; Zulkifli, E.Z.; Yusof, H.A. Factorial validation of Malaysian adapted Brunel Mood Scale in an adolescent sample. Asian J. Sport Med. 2010, 1, 185. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3289187/ (accessed on 6 January 2021).
- Lan, M.F.; Lane, A.M.; Roy, J.; Hanin, N.A. Validity of the Brunel Mood Scale for use with Malaysian athletes. J. Sport Sci. Med. 2012, 11, 131. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3737843/ (accessed on 6 January 2021).
- Terry, P.C.; Malekshahi, M.; Delva, H.A. Development and initial validation of the Farsi Mood Scale. Int. J. Sport Exerc. Psychol. 2012, 10, 112–122. [Google Scholar] [CrossRef]
- Rajkovic, I. Translation and Validation of Brunel Mood Scale for Serbian Athlete Population. Master’s Thesis, University of Jyväskylä, Jyväskylä, Finland, 2014. Available online: https://www.semanticscholar.org/paper/Translation-and-validation-of-Brunel-Mood-Scale-for-Rajkovic/a483f94ab78daad71eb070e336079b756b8dc35f (accessed on 1 February 2022).
- Han, C.; Parsons-Smith, R.L.; Fogarty, G.J.; Terry, P.C. Psychometric properties of the Brunel Mood Scale in a Singaporean sporting context. Int. J. Sport Exerc. Psychol. 2022, 20, 698–714. [Google Scholar] [CrossRef]
- Cañadas, E.; Monleón, C.; Sanchis, C.; Fargueta, M.; Blasco, E. Spanish validation of BRUMS in sporting and non-sporting populations. Eur. J. Hum. Move. 2017, 38, 105–117. Available online: http://www.eurjhm.com/index.php/eurjhm/article/view/413/608 (accessed on 6 January 2021).
- Çakiroğlu1, A.A.; Demir, E.; Güçlü, M. The validity and reliability study of the Brunel Mood Scale with the adult athletes (Turkish Adaptation). Int. J. Appl. Exerc. Physiol. 2020, 9, 126–140. Available online: http://www.ijaep.com/index.php/IJAE/issue/view/36 (accessed on 1 February 2022).
- Malinauskas, R.; Malinauskiene, V.; Dumciene, A. Burnout and perceived stress among university coaches in Lithuania. J. Occup. Health 2010, 52, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Bunevičius, A.; Birbilaitė, I.; Katkutė, A. Validity of Lithuanian version of the Modern Personality Assessment based on the Big-Five Personality Dimensions Questionnaire. Biol. Psychiat. Psychopharm. 2008, 10, 27–30. Available online: https://www.researchgate.net/publication/274137424_Validity_of_Lithuanian_version_of_the_Modern_Personality_Assesment_based_on_the_Big-Five_personality_dimensions_questionnaire (accessed on 1 February 2022).
- Tabachnick, B.L.; Fidell, L.S. Using Multivariate Statistics, 7th ed.; Pearson Education: Boston, MA, USA, 2019. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 27.0; IBM Corp: Armonk, NY, USA, 2020. [Google Scholar]
- Wagstaff, K.; Cardie, C.; Rogers, S.; Schroedl, S. Constrained k-means clustering with background knowledge. Int. Conf. Mach. Learn. 2001, 1, 577–584. Available online: http://www.cs.cmu.edu/~./dgovinda/pdf/icml-2001.pdf (accessed on 1 February 2022).
- Bair, E. Semi-supervised clustering methods. Wiley Interdisc. Rev. Computat. Stat. 2013, 5, 349–361. [Google Scholar] [CrossRef]
- Jain, A.K. Data clustering: 50 years beyond k-means. Pattern Recog. Lett. 2010, 31, 651–666. [Google Scholar] [CrossRef]
- Leiner, D.J. Too fast, too straight, too weird: Non-reactive indicators for meaningless data in internet surveys. Surv. Res. Meth. 2019, 13, e7403. [Google Scholar] [CrossRef]
- Meisenberg, G.; Williams, A. Are acquiescent and extreme response styles related to low intelligence and education? Pers. Indiv. Diff. 2008, 44, 1539–1550. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using SPSS, 3rd ed.; Sage: London, UK, 2009. [Google Scholar]
- Amin, Z.; Canli, T.; Epperson, C.N. Effect of estrogen-serotonin interactions on mood and cognition. Behav. Cog. Neuro. Rev. 2005, 4, 43–58. [Google Scholar] [CrossRef]
- Ruigrok, A.N.V.; Salimi-Khorshidi, G.; Lai, M.C.; Baron-Cohen, S.; Lombardo, M.V.; Tait, R.J.; Suckling, J. A meta-analysis of sex differences in human brain structure. Neurosci. Biobehav. Rev. 2014, 39, 34–50. [Google Scholar] [CrossRef]
- Dorius, S.F.; Firebaugh, G. Trends in global gender inequality. Soc. Force. 2010, 88, 1941–1968. [Google Scholar] [CrossRef]
- Stamarski, C.S.; Son Hing, L.S. Gender inequalities in the workplace: The effects of organizational structures, processes, practices, and decision makers’ sexism. Front. Psychol. 2015, 6, e1400. [Google Scholar] [CrossRef] [PubMed]
- UN Women. Whose Time to Care? Unpaid Care and Domestic Work during COVID-19; UN Women: New York, NY, USA; Available online: https://data.unwomen.org/sites/default/files/inline-files/Whose-time-to-care-brief_0.pdf (accessed on 17 June 2022).
- Fluharty, M.; Taylor, A.E.; Grabski, M.; Munafò, M.R. The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine Tob. Res. 2017, 19, 3–13. [Google Scholar] [CrossRef]
- Rubin, L.F.; Haaga, D.A.F.; Pearson, J.L.; Gunthert, K.C. Depression as a moderator of the prospective relationship between mood and smoking. Health Psychol. 2020, 39, 99–106. [Google Scholar] [CrossRef]
- Fucito, L.M.; Juliano, L.M. Depression moderates smoking behavior in response to a sad mood induction. Psychol. Addict. Behav. 2009, 23, 546–551. [Google Scholar] [CrossRef]
- Sharma, A.; Madaan, V.; Petty, F.D. Exercise for mental health. Prim. Care Companion J. Clin. Psychiatry 2006, 8, 106. [Google Scholar] [CrossRef]
- Peluso, M.A.; Andrade, L.H. Physical activity and mental health: The association between exercise and mood. Clinics 2005, 60, 61–70. [Google Scholar] [CrossRef]
- Prentice, A.M. Overeating: The health risks. Obes. Res. 2001, 9 (Suppl. 4), 234S–238S. [Google Scholar] [CrossRef]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2021, 156, 104853. [Google Scholar] [CrossRef]
- Striegel-Moore, R.H.; Dohm, F.A.; Kraemer, H.C.; Schreiber, G.B.; Taylor, C.B.; Daniels, S.R. Risk factors for binge-eating disorders: An exploratory study. Int. J. Eat. Disord. 2007, 40, 481–487. [Google Scholar] [CrossRef]
- Behr, D.; Shishido, K. The translation of measurement instruments for cross-cultural surveys. In The SAGE Handbook of Survey Methodology; Wolf, C., Joye, D., Smith, T.W., Fu, Y., Eds.; Sage: London, UK, 2016; pp. 269–287. [Google Scholar]
- Sha, M.; Immerwahr, S. Survey translation: Why and how should researchers and managers be engaged? Surv. Pract. 2018, 11, e0016. [Google Scholar] [CrossRef]
- Robinson, L.; Cotten, S.R.; Ono, H.; Quan-Haase, A. Digital inequalities and why they matter. Information 2015, 18, 569–582. [Google Scholar] [CrossRef]
- Kimalainen, S. 13 Countries with the Highest Percentage of College Graduates in 2018. Available online: https://www.insidermonkey.com/blog/13-countries-with-the-highest-percentage-of-college-graduates-in-2018-658240/?singlepage=1 (accessed on 29 September 2021).
- Index Mundi. Lithuania Median Age—Demographics. Available online: https://www.indexmundi.com/lithuania/median_age.html (accessed on 29 September 2021).
- Statista. Population of Lithuania from 1950 to 2020, by Gender. Available online: https://www.statista.com/statistics/1016406/male-female-population-lithuania-1950-2020/ (accessed on 3 August 2022).
- Statista. Share of Individuals Who Currently Smoke Cigarettes, Cigars, Cigarillos or a Pipe in Selected European Countries in 2020. Available online: www.statista.com/statistics/433390/individuals-who-currently-smoke-cigarettes-in-european-countries/ (accessed on 3 August 2022).
- Jamieson, S. Likert scales: How to (ab)use them. Med. Educ. 2004, 38, 1217–1218. [Google Scholar] [CrossRef] [PubMed]
- Carifio, L.; Perla, R. Resolving the 50-year debate around using and misusing Likert scales. Med. Educ. 2008, 42, 1150–1152. [Google Scholar] [CrossRef]
- Gaito, J. Measurement scales and statistics: Resurgence of an old misconception. Psychol. Bull. 1980, 87, 564–567. [Google Scholar] [CrossRef]
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. 2010, 15, 625–632. [Google Scholar] [CrossRef]
- Pereira, M.A.; Marques, R.C.; Ferreira, D.C. An incentive-based framework for analyzing the alignment of institutional interventions in the public primary healthcare sector: The Portuguese case. Healthcare 2021, 9, 904. [Google Scholar] [CrossRef]
- Health and Wellbeing Queensland. Making Healthy Happen. 2020. Available online: https://hw.qld.gov.au/make-healthy-happen/health-wellbeing-initiatives/ (accessed on 3 August 2022).
- Victoria Department of Health. Public Health and Wellbeing Planning. 2021. Available online: https://www.health.vic.gov.au/health-strategies/public-health-and-wellbeing-planning (accessed on 3 August 2022).
- World Health Organization. Promoting Well-being. 2021. Available online: https://www.who.int/activities/promoting-well-being (accessed on 3 August 2022).
- Terry, P.C.; Lim, J.; Parsons-Smith, R.L. In The Mood: An Online Mood Assessment Based on the Brunel Mood Scale. 2013. Available online: www.moodprofling.com (accessed on 6 January 2021).

| Variable | M | SD | SEM | Min | Max | Skewness | Kurtosis | α |
|---|---|---|---|---|---|---|---|---|
| Tension | 3.43 | 3.56 | 0.13 | 0 | 15 | 1.10 | 0.51 | 0.83 |
| Depression | 2.62 | 3.53 | 0.13 | 0 | 16 | 1.54 | 1.75 | 0.88 |
| Anger | 2.35 | 3.20 | 0.12 | 0 | 16 | 1.70 | 2.70 | 0.86 |
| Vigor | 9.13 | 3.70 | 0.14 | 0 | 16 | −0.20 | −0.50 | 0.88 |
| Fatigue | 5.12 | 4.22 | 0.15 | 0 | 16 | 0.59 | −0.59 | 0.89 |
| Confusion | 2.84 | 3.46 | 0.13 | 0 | 16 | 1.41 | 1.55 | 0.85 |
| Source | Iceberg (n = 209; 28.0%) | Inverse Everest (n = 56; 7.5%) | Inverse Iceberg (n = 105; 14.1%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | 95% CI | M | SD | 95% CI | M | SD | 95% CI | |
| Tension | 43.22 | 3.75 | [42.56, 43.88] | 70.98 | 6.29 | [69.70, 72.26] | 61.64 | 6.29 | [60.71, 62.58] |
| Depression | 43.67 | 2.40 | [43.02, 44.32] | 72.98 | 8.29 | [71.73, 74.24] | 61.44 | 6.85 | [60.52, 62.35] |
| Anger | 44.14 | 3.10 | [43.40, 44.89] | 73.01 | 10.32 | [71.57, 74.46] | 58.88 | 8.30 | [57.83, 59.93] |
| Vigor | 60.22 | 4.93 | [59.35, 61.10] | 39.47 | 8.14 | [37.79, 41.16] | 43.55 | 8.60 | [42.32, 44.78] |
| Fatigue | 40.84 | 3.78 | [40.12, 41.56] | 65.24 | 7.23 | [63.84, 66.63] | 60.20 | 7.16 | [59.18, 61.22] |
| Confusion | 43.98 | 6.63 | [43.23, 44.73] | 72.25 | 8.27 | [70.80, 73.70] | 59.16 | 7.67 | [58.10, 60.22] |
| Source | Shark Fin(n = 100; 13.4%) | Submerged(n = 162; 21.7%) | Surface(n = 114; 15.3%) | ||||||
| M | SD | 95% CI | M | SD | 95% CI | M | SD | 95% CI | |
| Tension | 47.65 | 5.29 | [46.69, 48.60] | 43.44 | 3.85 | [42.69, 44.19] | 52.79 | 5.35 | [51.90, 53.69] |
| Depression | 47.87 | 5.29 | [46.93, 48.81] | 44.18 | 2.77 | [43.44, 44.92] | 49.93 | 5.14 | [49.05, 50.81] |
| Anger | 46.57 | 4.45 | [45.49, 47.65] | 44.30 | 2.94 | [43.46, 45.15] | 52.36 | 5.91 | [51.36, 53.37] |
| Vigor | 42.33 | 7.25 | [41.07, 43.59] | 45.83 | 5.53 | [44.84, 46.82] | 55.02 | 5.94 | [53.84, 56.20] |
| Fatigue | 59.19 | 5.46 | [58.14, 60.23] | 45.39 | 4.57 | [44.57, 46.21] | 48.40 | 5.47 | [47.42, 49.38] |
| Confusion | 46.61 | 5.18 | [45.53, 47.70] | 44.12 | 3.64 | [43.27, 44.97] | 52.99 | 6.81 | [51.98, 54.01] |
| Cluster | Predicted Group Membership | n | % | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| 1 | 209 | 0 | 0 | 0 | 0 | 0 | 209 | 100 |
| 2 | 0 | 48 | 8 | 0 | 0 | 0 | 56 | 85.7 |
| 3 | 0 | 1 | 102 | 1 | 0 | 1 | 105 | 97.1 |
| 4 | 0 | 0 | 1 | 86 | 11 | 2 | 100 | 86.0 |
| 5 | 9 | 0 | 0 | 0 | 153 | 0 | 162 | 94.4 |
| 6 | 5 | 0 | 1 | 1 | 1 | 106 | 114 | 93.0 |
| Source | Cluster | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | % | 2 | % | 3 | % | 4 | % | 5 | % | 6 | % | |
| Sex χ2(5) = 16.58 § | ||||||||||||
| Male (n = 199) | 73 §+ | 36.7 | 15 | 7.5 | 19 *− | 9.5 | 18 *− | 9.0 | 39 | 19.6 | 35 | 17.6 |
| Female (n = 547) | 136 §− | 24.9 | 41 | 7.5 | 86 *+ | 15.7 | 82 *+ | 15.0 | 123 | 22.5 | 79 | 14.4 |
| Age group (year) χ2(15) = 47.62 † | ||||||||||||
| 17–30 (n = 243) | 27 *− | 19.7 | 14 | 10.2 | 22 | 16.1 | 16 | 11.7 | 26 | 19.0 | 32 §+ | 23.4 |
| 31–40 (n = 263) | 45 *− | 22.4 | 21 | 10.4 | 40 §+ | 19.9 | 33 | 16.4 | 35 | 17.4 | 27 | 13.4 |
| 41–50 (n = 236) | 80 *+ | 33.9 | 15 | 6.4 | 29 | 12.3 | 32 | 13.6 | 47 | 19.9 | 33 | 14.0 |
| 51+ (n = 172) | 57 | 33.1 | 6 *− | 3.5 | 14 §− | 8.1 | 19 | 11.0 | 54 †+ | 31.4 | 22 | 12.8 |
| Smoking χ2(5) = 15.78 § | ||||||||||||
| No (n = 604) | 177 | 29.3 | 43 | 7.1 | 84 | 13.9 | 81 | 13.4 | 140 *+ | 23.2 | 79 †− | 13.1 |
| Yes (n = 142) | 32 | 22.5 | 13 | 9.2 | 21 | 14.8 | 19 | 13.4 | 22 *− | 15.5 | 35 †+ | 24.6 |
| Exercise χ2(5) = 59.17 † | ||||||||||||
| No (n = 202) | 25 †− | 12.4 | 25 §+ | 12.4 | 40 §+ | 19.8 | 41 †+ | 20.3 | 53 | 26.2 | 18 §− | 8.9 |
| Yes (n = 544) | 184 †+ | 33.8 | 31 §− | 5.7 | 65 §− | 11.9 | 59 †− | 10.8 | 109 | 20.0 | 96 §+ | 17.6 |
| Overeating χ2(10) = 43.83 † | ||||||||||||
| Never (n = 117) | 40 | 34.2 | 4 | 3.4 | 16 | 13.7 | 12 | 10.3 | 29 | 24.8 | 16 | 13.7 |
| Rarely (n = 495) | 156 §+ | 31.5 | 33 | 6.7 | 59 *− | 11.9 | 68 | 13.7 | 108 | 21.8 | 71 | 14.3 |
| Often (n = 134) | 13 †− | 9.7 | 19 §+ | 14.2 | 30 §+ | 22.4 | 20 | 14.9 | 25 | 18.7 | 27 | 20.1 |
| Health Status χ2(15) = 117.65 † | ||||||||||||
| Bad (n = 20) | 0 §− | 0.0 | 3 | 15.0 | 9 †+ | 45.0 | 4 | 20.0 | 3 | 15.0 | 1 | 5.0 |
| Satisfactory (n = 173) | 19 †− | 11.0 | 30 †+ | 17.3 | 38 †+ | 22.0 | 25 | 14.5 | 41 | 23.7 | 20 | 11.6 |
| Good (n = 420) | 124 | 29.5 | 22 §− | 5.2 | 51 | 12.1 | 57 | 13.6 | 92 | 21.9 | 74 *+ | 17.6 |
| Great (n = 133) | 66 †+ | 49.6 | 1 †− | 0.8 | 7 §− | 5.3 | 14 | 10.5 | 26 | 19.5 | 19 | 14.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terry, P.C.; Parsons-Smith, R.L.; Skurvydas, A.; Lisinskienė, A.; Majauskienė, D.; Valančienė, D.; Cooper, S.; Lochbaum, M. Physical Activity and Healthy Habits Influence Mood Profile Clusters in a Lithuanian Population. Sustainability 2022, 14, 10006. https://doi.org/10.3390/su141610006
Terry PC, Parsons-Smith RL, Skurvydas A, Lisinskienė A, Majauskienė D, Valančienė D, Cooper S, Lochbaum M. Physical Activity and Healthy Habits Influence Mood Profile Clusters in a Lithuanian Population. Sustainability. 2022; 14(16):10006. https://doi.org/10.3390/su141610006
Chicago/Turabian StyleTerry, Peter C., Renée L. Parsons-Smith, Albertas Skurvydas, Aušra Lisinskienė, Daiva Majauskienė, Dovilė Valančienė, Sydney Cooper, and Marc Lochbaum. 2022. "Physical Activity and Healthy Habits Influence Mood Profile Clusters in a Lithuanian Population" Sustainability 14, no. 16: 10006. https://doi.org/10.3390/su141610006
APA StyleTerry, P. C., Parsons-Smith, R. L., Skurvydas, A., Lisinskienė, A., Majauskienė, D., Valančienė, D., Cooper, S., & Lochbaum, M. (2022). Physical Activity and Healthy Habits Influence Mood Profile Clusters in a Lithuanian Population. Sustainability, 14(16), 10006. https://doi.org/10.3390/su141610006









