A Refined Evaluation Analysis of Global Healthcare Accessibility Based on the Healthcare Accessibility Index Model and Coupling Coordination Degree Model
Abstract
:1. Introduction
2. Materials and methods
2.1. Construction of an Evaluation Index System
2.2. Determination of the Index Weight
2.3. HCA Index Model
2.4. Coupling Coordination Degree Model
2.5. Data Source and Processing
3. Results
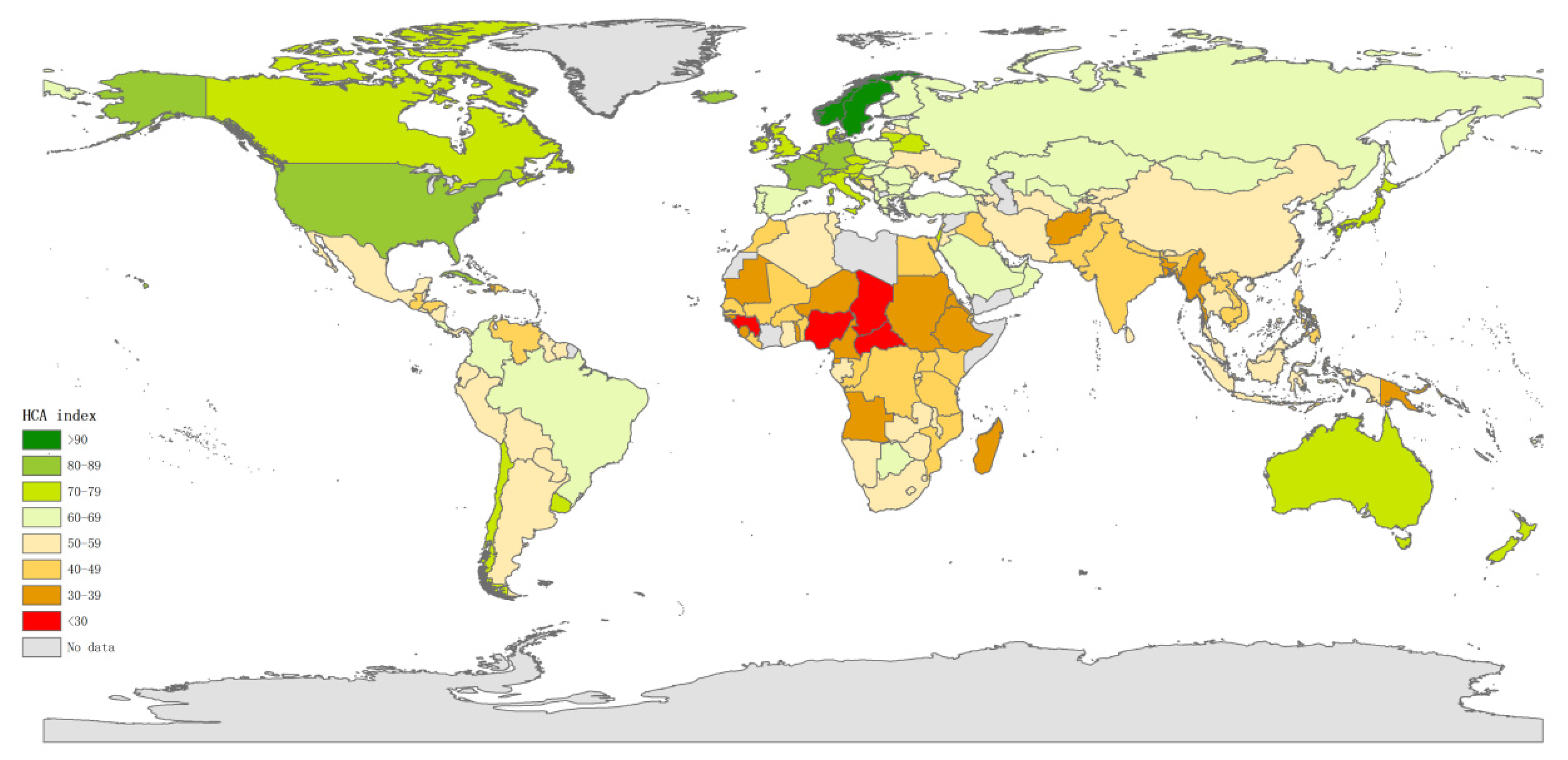
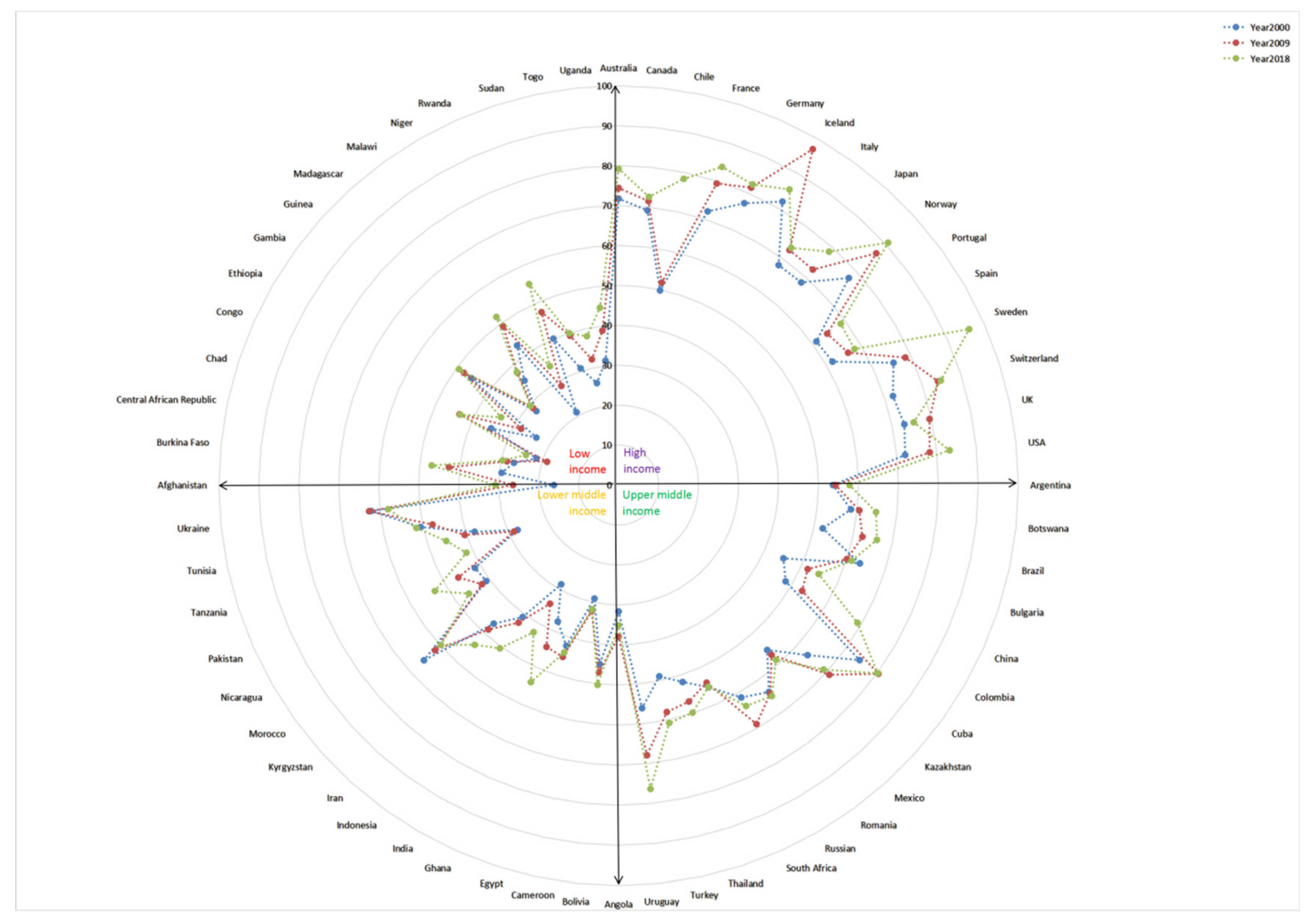
3.1. HCA Index Analysis
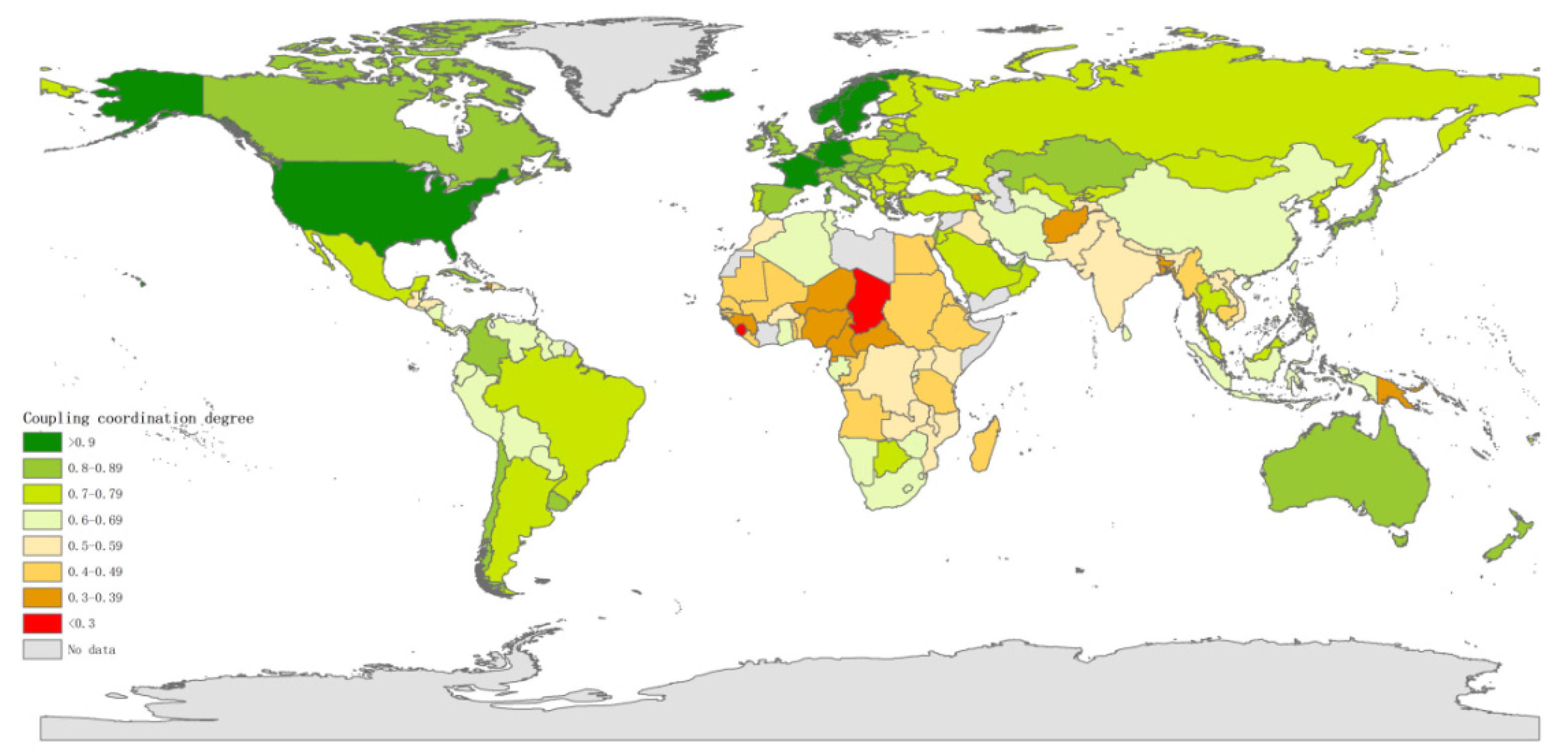
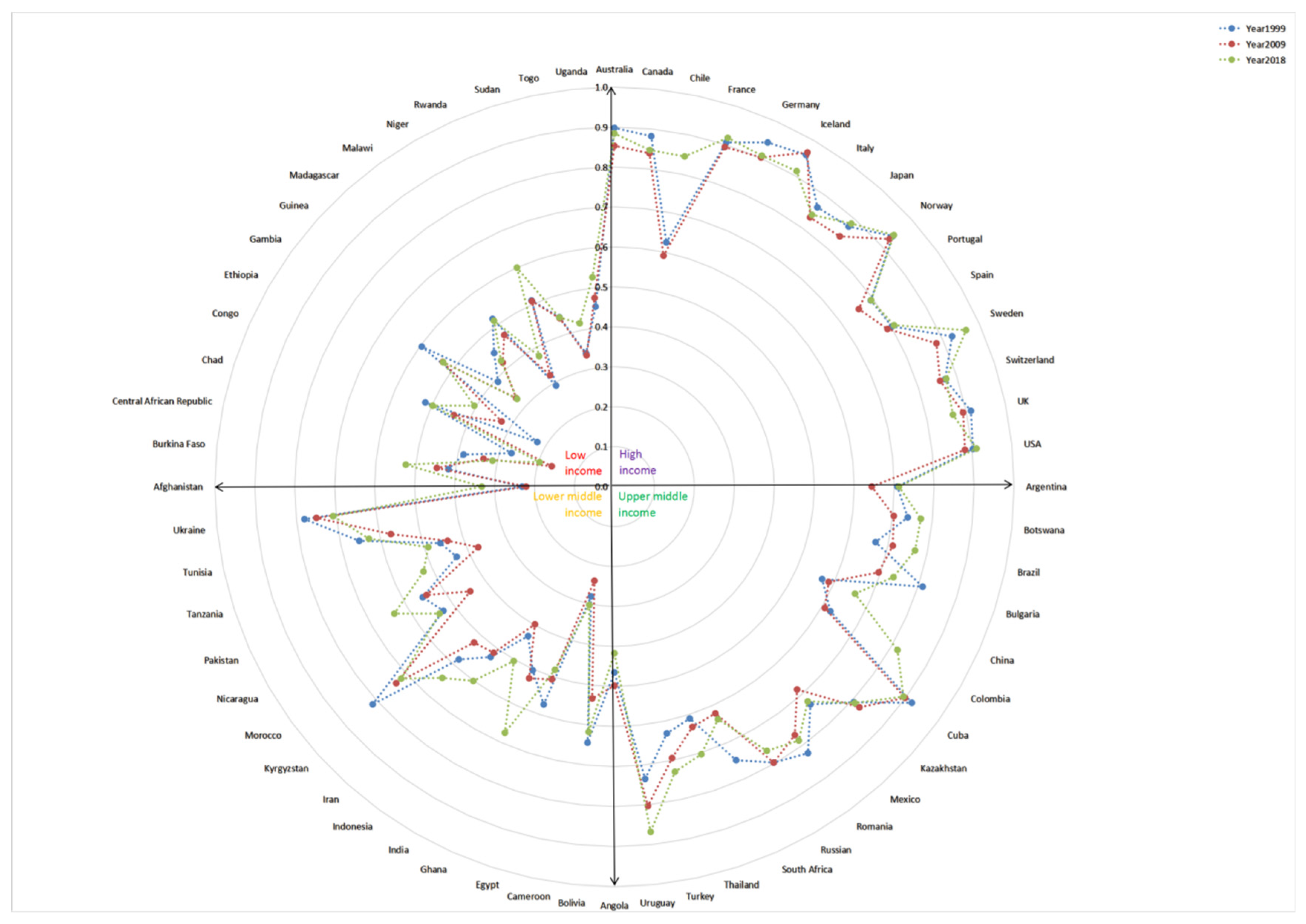
3.2. Coupling Coordination Degree Analysis
3.3. Refined Classification Analysis
4. Discussion
4.1. HCA Index
4.2. Coupling Coordination Degree
4.3. The role of HCA in Refining Classification Evaluation
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pu, Q.; Yoo, E.; Rothstein, D.H.; Cairo, S.; Malemo, L. Improving the spatial accessibility of healthcare in North Kivu, Democratic Republic of Congo. Appl. Geogr. 2020, 121, 102262. [Google Scholar] [CrossRef]
- Polo, G.; Acosta, C.M.; Ferreira, F.; Dias, R.A. Location-Allocation and Accessibility Models for Improving the Spatial Planning of Public Health Services. PLoS ONE 2015, 10, e119190. [Google Scholar] [CrossRef] [PubMed]
- Penchansky, R.; Thomas, J.W. The Concept of Access: Definition and Relationship to Consumer Satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Wang, L. Immigration, ethnicity, and accessibility to culturally diverse family physicians. Health Place 2007, 13, 656–671. [Google Scholar] [CrossRef]
- Delamater, P.L.; Messina, J.P.; Shortridge, A.M.; Grady, S.C. Measuring geographic access to health care: Raster and network-based methods. Int. J. Health Geogr. 2012, 11, 15. [Google Scholar] [CrossRef]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef]
- Ono, T.; Lafortune, G.; Schoenstein, M. Health Workforce Planning in OECD Countries: A Review of 26 Projection Models from 18 Countries; OECD Publishing: Paris, France, 2013. [Google Scholar]
- Ono, T.; Schoenstein, M.; Buchan, J. Geographic Imbalances in Doctor Supply and Policy Responses; OECD Publishing: Paris, France, 2014. [Google Scholar]
- OECD. Health for Everyone?: Social Inequalities in Health and Health Systems; OECD Publishing: Paris, France, 2019. [Google Scholar]
- Ouko, J.J.O.; Gachari, M.K.; Sichangi, A.W.; Alegana, V. Geographic information system-based evaluation of spatial accessibility to maternal health facilities in Siaya County, Kenya. Geogr. Res.-Aust. 2019, 57, 286–298. [Google Scholar] [CrossRef]
- Shah, T.I.; Bell, S.; Wilson, K. Spatial Accessibility to Health Care Services: Identifying under-Serviced Neighbourhoods in Canadian Urban Areas. PLoS ONE 2016, 11, e168208. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Zhang, Z.; Lan, X. Impact of China’s referral reform on the equity and spatial accessibility of healthcare resources: A case study of Beijing. Soc. Sci. Med. 2019, 235, 112386. [Google Scholar] [CrossRef]
- Bitton, A.; Fifield, J.; Ratcliffe, H.; Karlage, A.; Wang, H.; Veillard, J.H.; Schwarz, D.; Hirschhorn, L.R. Primary healthcare system performance in low-income and middle-income countries: A scoping review of the evidence from 2010 to 2017. BMJ Glob. Health 2019, 4, e1551. [Google Scholar] [CrossRef]
- Xu, Z.; Gahr, M.; Xiang, Y.; Kingdon, D.; Rüsch, N.; Wang, G. The state of mental health care in China. Asian J. Psychiatry 2022, 69, 102975. [Google Scholar] [CrossRef] [PubMed]
- OECD. Health at a Glance 2019: OECD Indicators; OECD Publishing: Paris, France, 2019. [Google Scholar]
- Matthews, K.A.; Gaglioti, A.H.; Holt, J.B.; Wheaton, A.G.; Croft, J.B. Using spatially adaptive floating catchments to measure the geographic availability of a health care service: Pulmonary rehabilitation in the southeastern United States. Health Place 2019, 56, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Di, X.; Wang, L.; Dai, X.; Yang, L. Assessing the Accessibility of Home-Based Healthcare Services for the Elderly: A Case from Shaanxi Province, China. Int. J. Environ. Res. Public Health 2020, 17, 7168. [Google Scholar] [CrossRef] [PubMed]
- Barber, R.M.; Fullman, N.; Sorensen, R.J.D.; Bollyky, T.; McKee, M.; Nolte, E.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; et al. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: A novel analysis from the Global Burden of Disease Study 2015. Lancet 2017, 390, 231–266. [Google Scholar] [CrossRef]
- Cabrera-Barona, P.; Blaschke, T.; Kienberger, S. Explaining Accessibility and Satisfaction Related to Healthcare: A Mixed-Methods Approach. Soc. Indic. Res. 2017, 133, 719–739. [Google Scholar] [CrossRef]
- Wagstaff, A.; Neelsen, S. A comprehensive assessment of universal health coverage in 111 countries: A retrospective observational study. Lancet Glob. Health 2020, 8, 39–49. [Google Scholar] [CrossRef]
- Hogan, D.R.; Stevens, G.A.; Hosseinpoor, A.R.; Boerma, T. Monitoring universal health coverage within the Sustainable Development Goals: Development and baseline data for an index of essential health services. Lancet Glob. Health 2018, 6, e152–e168. [Google Scholar] [CrossRef]
- McPake, B.I. Crunching health expenditure numbers: Important but treacherous terrain. Lancet Glob. Health 2018, 6, e124–e125. [Google Scholar] [CrossRef]
- Qi, Y.; Farnoosh, A.; Lin, L.; Liu, H. Coupling coordination analysis of China’s provincial water-energy-food nexus. Environ. Sci. Pollut. R. 2022, 29, 23303–23313. [Google Scholar] [CrossRef]
- Cheng, X.; Long, R.; Chen, H.; Li, Q. Coupling coordination degree and spatial dynamic evolution of a regional green competitiveness system—A case study from China. Ecol. Indic. 2019, 104, 489–500. [Google Scholar] [CrossRef]
- Shi, T.; Yang, S.; Zhang, W.; Zhou, Q. Coupling coordination degree measurement and spatiotemporal heterogeneity between economic development and ecological environment—Empirical evidence from tropical and subtropical regions of China. J. Clean. Prod. 2020, 244, 118739. [Google Scholar] [CrossRef]
- Janse van Rensburg, B.; Kotzé, C.; Moxley, K.; Subramaney, U.; Zingela, Z.; Seedat, S. Profile of the current psychiatrist workforce in South Africa: Establishing a baseline for human resource planning and strategy. Health Policy Plan. 2022, 37, 492–504. [Google Scholar] [CrossRef] [PubMed]
- Vardell, E. Global Health Observatory Data Repository. Med. Ref. Serv. Q. 2020, 39, 67–74. [Google Scholar] [CrossRef]
- Ampofo, A.G.; Boateng, E.B. Beyond 2020: Modelling obesity and diabetes prevalence. Diabetes Res. Clin. Pract. 2020, 167, 108362. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows, Version 25.0; IBM Corp.: Armonk, NY, USA, 2017. [Google Scholar]
- Parvin, F.; Ali, S.A.; Hashmi, S.N.I.; Khatoon, A. Accessibility and site suitability for healthcare services using GIS-based hybrid decision-making approach: A study in Murshidabad, India. Spat. Inf. Res. 2021, 29, 1–18. [Google Scholar] [CrossRef]
- De Mello-Sampayo, F. Spatial Interaction Model for Healthcare Accessibility: What Scale Has to Do with It. Sustainability 2020, 12, 4324. [Google Scholar] [CrossRef]
- Cortés, Y. Spatial Accessibility to Local Public Services in an Unequal Place: An Analysis from Patterns of Residential Segregation in the Metropolitan Area of Santiago, Chile. Sustainability 2021, 13, 442. [Google Scholar] [CrossRef]
- World Health Organization. World Health Statistics 2021: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Pandian, J.D.; Kalkonde, Y.; Sebastian, I.A.; Felix, C.; Urimubenshi, G.; Bosch, J. Stroke systems of care in low-income and middle-income countries: Challenges and opportunities. Lancet 2020, 396, 1443–1451. [Google Scholar] [CrossRef]
- Lantz, A.; Holmer, H.; Finlayson, S.R.G.; Ricketts, T.C.; Watters, D.A.; Gruen, R.L.; Johnson, W.D.; Hagander, L. Measuring the migration of surgical specialists. Surgery 2020, 168, 550–557. [Google Scholar] [CrossRef]
- Visconti, R.M.; Larocca, A.; Marconi, M. Accessibility to First-Mile health services: A time-cost model for rural Uganda. Soc. Sci. Med. 2020, 265, 113410. [Google Scholar] [CrossRef]
- McBain, R.K.; Jerome, G.; Warsh, J.; Browning, M.; Mistry, B.; Faure, P.A.I.; Pierre, C.; Fang, A.P.; Mugunga, J.C.; Rhatigan, J.; et al. Rethinking the cost of healthcare in low-resource settings: The value of time-driven activity-based costing. BMJ Glob. Health 2016, 1, e134. [Google Scholar] [CrossRef] [PubMed]
- Abdu, M.; Wilson, A.; Mhango, C.; Taki, F.; Coomarasamy, A.; Lissauer, D. Resource availability for the management of maternal sepsis in Malawi, other low-income countries, and lower-middle-income countries. Int. J. Gynecol. Obstet. 2018, 140, 175–183. [Google Scholar] [CrossRef]
- Núñez, A.; Manzano, C.A.; Chi, C. Health outcomes, utilization, and equity in Chile: An evolution from 1990 to 2015 and the effects of the last health reform. Public Health 2020, 178, 38–48. [Google Scholar] [CrossRef] [PubMed]
- De Vos, P. Cuba’s Strategy Toward Universal Health. Int. J. Health Serv. 2019, 49, 186–192. [Google Scholar] [CrossRef]
- Bhardwaj, N.; Skinner, D. Primary Care in Cuba: Considerations for the U.S. J. Health Care Poor Underserved 2019, 30, 456–467. [Google Scholar] [CrossRef] [PubMed]
| Dimensions | Evaluation Indicators | Unit | Property | Data Resources | References |
|---|---|---|---|---|---|
| Workforce | Medical doctors density | Per 10,000 population | Positive | The GHO database | Health at a Glance 2019: OECD Indicators |
| Nursing and midwifery personnel density | Per 10,000 population | Positive | The GHO database | Health at a Glance 2019: OECD Indicators | |
| Financial | OOP expenditure as percentage of CHE | % | Negative | The GHO database | Health at a Glance 2019: OECD Indicators |
| Catastrophic spending on health (at 10% threshold) | % | Negative | The GHO database | Health at a Glance 2019: OECD Indicators | |
| Services | DTP3 vaccination rates | % | Positive | The GHO database | Health at a Glance 2019: OECD Indicators |
| Skilled birth attendance | % | Positive | The GHO database | Health at a Glance 2019: OECD Indicators |
| Income Groups | Count | Countries |
|---|---|---|
| High-income | 56 | Andorra, Antigua and Barbuda, Australia, Austria, Bahamas, Bahrain, Barbados, Belgium, Brunei Darussalam, Canada, Chile, Cook Islands, Croatia, Cyprus, Czechia, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Latvia, Lithuania, Luxembourg, Malta, Nauru, Netherlands, New Zealand, Niue, Norway, Oman, Palau, Poland, Portugal, Qatar, Republic of Korea, Saint Kitts and Nevis, Saudi Arabia, Seychelles, Singapore, Slovakia, Slovenia, Spain, Sweden, Switzerland, Trinidad and Tobago, UK, United Arab Emirates, USA |
| Upper-middle-income | 53 | Albania, Argentina, Armenia, Azerbaijan, Belarus, Bosnia and Herzegovina, Botswana, Brazil, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, Equatorial Guinea, Fiji, Gabon, Georgia, Grenada, Guatemala, Guyana, Iraq, Jamaica, Jordan, Kazakhstan, Lebanon, Malaysia, Maldives, Marshall Islands, Mauritius, Mexico, Montenegro, Namibia, Panama, Paraguay, Peru, Republic of Moldova, Romania, Russia, Saint Lucia, Saint Vincent and the Grenadines, Serbia, South Africa, Suriname, Thailand, Tonga, Turkey, Turkmenistan, Tuvalu, Uruguay, Venezuela |
| Lower-middle-income | 54 | Algeria, Angola, Bangladesh, Belize, Benin, Bhutan, Bolivia, Cabo Verde, Cambodia, Cameroon, Comoros, Côte d’Ivoire, Djibouti, Egypt, El Salvador, Eswatini, Ghana, Haiti, Honduras, India, Indonesia, Iran, Kenya, Kiribati, Kyrgyzstan, Lesotho, Mauritania, Micronesia, Mongolia, Morocco, Myanmar, Nepal, Nicaragua, Nigeria, Pakistan, Papua New Guinea, Philippines, Samoa, Sao Tome and Principe, Senegal, Solomon Islands, Sri Lanka, Tajikistan, Tanzania, The Lao People’s Democratic Republic, The Republic of the Congo, Timor-Leste, Tunisia, Ukraine, Uzbekistan, Vanuatu, Viet Nam, Zambia, Zimbabwe |
| Low-income | 23 | Afghanistan, Burkina Faso, Burundi, Central African Republic, Chad, Democratic People’s Republic of Korea, Democratic Republic of the Congo, Eritrea, Ethiopia, Gambia, Guinea, Guinea-Bissau, Liberia, Madagascar, Malawi, Mali, Mozambique, Niger, Rwanda, Sierra Leone, Sudan, Togo, Uganda |
| Year | Low | Antagonism | High | Count |
|---|---|---|---|---|
| 2000 | Turkey, Colombia, Iran, Gambia, China, Bolivia, Malawi, Egypt, Nicaragua, Morocco, Indonesia, Rwanda, Tanzania, Ghana, Madagascar, Congo, Angola, Uganda, Sudan, Burkina Faso, Cameroon, India, Guinea, Pakistan, Central African Republic, Togo, Ethiopia, Chad, Niger, Afghanistan | Canada, Japan, Italy, Kyrgyzstan, Romania, Kazakhstan, Bulgaria, Ukraine, Spain, Russia, Portugal, Botswana, Uruguay, Mexico, South Africa, Argentina, Brazil, Thailand, Tunisia, Chile | Iceland, Norway, Germany, Sweden, Cuba, UK, Switzerland, USA, France, Australia | 60 |
| 2009 | Malawi, Iran, Gambia, Tunisia, Rwanda, Bolivia, Nicaragua, Egypt, Ghana, Congo, Burkina Faso, Indonesia, Morocco, Tanzania, Sudan, Uganda, Angola, Madagascar, India, Cameroon, Togo, Guinea, Niger, Pakistan, Central African Republic, Ethiopia, Afghanistan, Chad | Russia, Uruguay, Spain, Portugal, Romania, Ukraine, Brazil, Kyrgyzstan, Botswana, Bulgaria, Turkey, Mexico, Thailand, Argentina, South Africa, Colombia, Chile, China | Iceland, Norway, Switzerland, Germany, Cuba, UK, France, Sweden, USA, Australia, Italy, Japan, Canada, Kazakhstan | 60 |
| 2018 | Gambia, Burkina Faso, Morocco, Tanzania, Uganda, Egypt, Congo, India, Pakistan, Sudan, Togo, Madagascar, Angola, Niger, Ethiopia, Cameroon, Afghanistan, Central African Republic, Guinea, Chad | Colombia, Kazakhstan, Portugal, Spain, Brazil, Romania, Botswana, Russia, Bulgaria, Turkey, Thailand, Kyrgyzstan, Mexico, Ukraine, Argentina, South Africa, Rwanda, China, Ghana, Iran, Nicaragua, Malawi, Tunisia, Indonesia, Bolivia | Sweden, Norway, Iceland, Switzerland, France, USA, Germany, Cuba, Australia, Japan, Chile, Uruguay, UK, Italy, Canada | 60 |
| Distribution | Lower-middle-income (35%); Low-income (65%) | High-income (8%); Upper-middle-income (52%); Lower-middle-income (32%); Low-income (8%) | High-income (86.7%); Upper-middle-income (13.3%) | High-income (25%); Upper-middle-income (25%); Lower-middle-income (25%); Low-income (25%) |
| Year | Maladjustment | Sub Coordination | Coordination | Count |
|---|---|---|---|---|
| 2000 | Guinea, Central African Republic, Togo, Niger, Cameroon, Chad, Afghanistan, Ethiopia | Brazil, Tunisia, Bolivia, Turkey, Chile, Colombia, Thailand, Gambia, Iran, Egypt, China, Nicaragua, Morocco, Indonesia, Malawi, Congo, Rwanda, Ghana, Angola, Tanzania, Uganda, Madagascar, Sudan, India, Pakistan, Burkina Faso | Iceland, Germany, Norway, Sweden, Cuba, UK, France, USA, Australia, Canada, Japan, Switzerland, Italy, Romania, Kyrgyzstan, Bulgaria, Kazakhstan, Spain, Russia, Portugal, Ukraine, South Africa, Botswana, Uruguay, Mexico, Argentina | 60 |
| 2009 | Pakistan, Togo, Central African Republic, Guinea, Ethiopia, Niger, Cameroon, Afghanistan, Chad | Turkey, Mexico, Argentina, Thailand, South Africa, Colombia, Chile, China, Tunisia, Nicaragua, Bolivia, Gambia, Iran, Ghana, Indonesia, Rwanda, Egypt, Angola, Uganda, Malawi, Burkina Faso, Morocco, Sudan, Congo, Tanzania, Madagascar, India | Iceland, Norway, Germany, Cuba, France, UK, Sweden, USA, Switzerland, Australia, Japan, Canada, Italy, Kazakhstan, Uruguay, Russia, Spain, Romania, Portugal, Ukraine, Kyrgyzstan, Brazil, Botswana, Bulgaria | 60 |
| 2018 | Niger, Afghanistan, Guinea, Central African Republic, Cameroon, Chad | Ghana, China, Iran, South Africa, Nicaragua, Tunisia, Bolivia, Indonesia, Rwanda, Morocco, Gambia, Uganda, Burkina Faso, Pakistan, Malawi, India, Congo, Tanzania, Egypt, Sudan, Madagascar, Togo, Angola, Ethiopia | Sweden, Norway, France, Iceland, USA, Germany, Cuba, Japan, Australia, Switzerland, Uruguay, UK, Canada, Chile, Italy, Colombia, Kazakhstan, Spain, Portugal, Romania, Botswana, Brazil, Russia, Bulgaria, Turkey, Mexico, Kyrgyzstan, Argentina, Ukraine, Thailand | 60 |
| Distribution | Lower-middle-income (16.7%); Low-income (83.3%) | Upper-middle-income (8.3%); Lower-middle-income (50%); Low-income (41.7%) | High-income (50%); Upper-middle-income (43.3%); Lower-middle-income (6.7%) | High-income (25%); Upper-middle-income (25%); Lower-middle-income (25%); Low-income (25%) |
| Type | Stage | 2000 | 2009 | 2018 | Count |
|---|---|---|---|---|---|
| Optimum | High-Coordination | Australia, Cuba, France, Germany, Iceland, Norway, Sweden, Switzerland, UK, USA | Australia, Canada, Cuba, France, Germany, Iceland, Italy, Japan, Kazakhstan, Norway, Sweden, Switzerland, UK, USA | Australia, Canada, Chile, Cuba, France, Germany, Iceland, Italy, Japan, Norway, Sweden, Switzerland, UK, Uruguay, USA | High-income (86.7%); Upper-middle-income (13.3%) |
| Suboptimum | High-Sub-Coordination | ||||
| Transition | High-Maladjustment | ||||
| Antagonism-Coordination | Argentina, Botswana, Bulgaria, Canada, Italy, Japan, Kazakhstan, Kyrgyzstan, Mexico, Portugal, Romania, Russia, South Africa, Spain, Ukraine, Uruguay | Botswana, Brazil, Bulgaria, Kyrgyzstan, Portugal, Romania, Russia, Spain, Ukraine, Uruguay | Argentina, Botswana, Brazil, Bulgaria, Colombia, Kazakhstan, Kyrgyzstan, Mexico, Portugal, Romania, Russia, Spain, Thailand, Turkey, Ukraine | High-income (13.3%); Upper-middle-income (73.4%); Lower-middle-income (13.3%) | |
| Antagonism-Sub-Coordination | Brazil, Chile, Thailand, Tunisia | Argentina, Chile, China, Colombia, Mexico, South Africa, Thailand, Turkey | Bolivia, China, Ghana, Indonesia, Iran, Malawi, Nicaragua, Rwanda, South Africa, Tunisia | Upper-middle-income (20%); Lower-middle-income (60%); Low-income (20%) | |
| Antagonism-Maladjustment | |||||
| Low-Coordination | |||||
| Inferior | Low-Sub Coordination | Angola, Bolivia, Burkina Faso, China, Colombia, Congo, Egypt, Gambia, Ghana, India, Indonesia, Iran, Madagascar, Malawi, Morocco, Nicaragua, Pakistan, Rwanda, Sudan, Tanzania, Turkey, Uganda | Angola, Bolivia, Burkina Faso, Congo, Egypt, Gambia, Ghana, India, Indonesia, Iran, Madagascar, Malawi, Morocco, Nicaragua, Rwanda, Sudan, Tanzania, Tunisia, Uganda | Angola, Burkina Faso, Congo, Egypt, Ethiopia, Gambia, India, Madagascar, Morocco, Pakistan, Sudan, Tanzania, Togo, Uganda | Lower-middle-income (42.9%); Low-income (57.1%) |
| Worst | Low-Maladjustment | Afghanistan, Cameroon, Central African Republic, Chad, Ethiopia, Guinea, Niger, Togo | Afghanistan, Cameroon, Central African Republic, Chad, Ethiopia, Guinea, Niger, Pakistan, Togo | Afghanistan, Cameroon, Central African Republic, Chad, Guinea, Niger | Lower-middle-income (16.7%); Low-income (83.3%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, Z.; Sun, Y.; Liu, X.; Tu, Y.; Chen, S.; Qian, D. A Refined Evaluation Analysis of Global Healthcare Accessibility Based on the Healthcare Accessibility Index Model and Coupling Coordination Degree Model. Sustainability 2022, 14, 10280. https://doi.org/10.3390/su141610280
Sun Z, Sun Y, Liu X, Tu Y, Chen S, Qian D. A Refined Evaluation Analysis of Global Healthcare Accessibility Based on the Healthcare Accessibility Index Model and Coupling Coordination Degree Model. Sustainability. 2022; 14(16):10280. https://doi.org/10.3390/su141610280
Chicago/Turabian StyleSun, Zhenyu, Ying Sun, Xueyi Liu, Yixue Tu, Shaofan Chen, and Dongfu Qian. 2022. "A Refined Evaluation Analysis of Global Healthcare Accessibility Based on the Healthcare Accessibility Index Model and Coupling Coordination Degree Model" Sustainability 14, no. 16: 10280. https://doi.org/10.3390/su141610280
APA StyleSun, Z., Sun, Y., Liu, X., Tu, Y., Chen, S., & Qian, D. (2022). A Refined Evaluation Analysis of Global Healthcare Accessibility Based on the Healthcare Accessibility Index Model and Coupling Coordination Degree Model. Sustainability, 14(16), 10280. https://doi.org/10.3390/su141610280






