Abstract
Physicians that pursue postgraduate studies must simultaneously manage activities related to their academic training and their duties as specialized in a hospital. The aim of this study was to determine the challenges that affect the professional development and growth of 142 first-year medical residents from a private university in Peru, during the COVID-19 pandemic. The residents responded to an online questionnaire with eight open-ended questions soliciting the identification of two difficulties or challenges per question. Descriptive analysis of the challenges that were detected was carried out and two binomial logistic regression models were tested to evaluate the effect of academic and personal factors on professional development. A structural regression model with three predicting factors (Academic training, Mentorship and use of ICT, and Health conditions) was also tested to predict professional development. Over 80% of the residents expressed having problems with their professional performance, activities, and attention span during the residency. The adjusted logistic regression model explained 42% of the effect of factors that make the emergence of challenges for medical residents more probable in the performance of professional activities. Likewise, the structural regression model indicated a good fit, where all three factors significantly explained medical residents’ professional performance; however, the Mentorship and use of ICTs factor was the best predictor of professional performance during the residency program.
1. Introduction
The advent of the COVID-19 pandemic brought many changes to programs that were, essentially, in-person. Adding virtual education to programs that were essentially in-person could have been based on a democratic perspective looking to diversify opportunities and access to education for students and college students [1]. However, virtuality has differentially impacted the college student population, configuring different situations and contexts [2,3], some of which have been negative for many students.
Based on their socioeconomic status, college students from different academic levels experience and perceive online classes, vocational training, and postgraduate studies during the pandemic in different ways. For example, a study of college students from different engineering fields reported that the students emphasized the advantages of online education for their personal and professional development during the pandemic, but the notion that the pandemic brought adverse consequences for student’s health and quality of life was also highlighted [4]. Other studies have reported differences in perception amongst the college community regarding the implementation, process, and effects of eLearning and education during the pandemic which are dependent on geographical and socio-economical location: the northern, southern, eastern, or western hemispheres [1]. Unequal access to quality online education during the pandemic has also been reported by students of various disciplines [5].
Various studies have reported on the effects of student connectivity and accessibility to the internet and to other technological gadgets, of teacher’s skills for technological resources and online classes, as well as of student self-teaching/learning skills, on the assessment of advantages and the effectiveness of postgraduate online courses during the pandemic [6,7,8,9,10]. Thus, during the pandemic, students have valued remote learning, comfortability, user-friendliness, accessibility, and student-centered education as important advantages of online classes. Nonetheless, students have also reported that online classes are inefficient and ineffective for teaching practical skills (for example, in Anatomy); they do not promote student participation or comments, they require many technological resources, attention is limited, and there is a risk of plagiarism by the student [11].
In other findings, during online classes due to the pandemic, students mentioned having connectivity issues, financial problems, and dedicating around 16 h a week to their homework; they considered that online classes were not enough to learn, so they had to dedicate extra time and resources for autonomous learning [12].
In a systematic review paper about Latin American college students’ participation and compromise to online learning due to the COVID-19 pandemic [13], the authors concluded with five requirements that must be considered for online learning in Latin America: (a) transformation of higher-level education, (b) providence of adequate professional training, (c) improvement of internet connectivity, (d) guaranteed quality online learning in higher-level education, and (e) emotional support. Similarly, a study about ergonomic and health changes perceived by Peruvian (in the city of Lima) college students during online classes due to the COVID-19 pandemic, found that 44% presented weight variations and 84% presented muscular pain, with a prevalence of back, neck, waist, shoulder, and neck pain [14]. Additionally, 79% presented eye discomfort (burning, itching, dryness, eye strain, and tearing during class); only 46.3% practiced physical exercise and more than 40% varied their intake of liquids and fruit consumption [14].
Research regarding medical training and education during the pandemic has also been conducted. Sierra et al. [15] noted that 59% of physicians in training, in Mexico, received classes via Zoom; 67% of the survey respondents rated the learning experience in prerecorded lessons or video conferences as the same or worse than in-person classes; 80% pointed out that the main limitations of live video conferences are the scarce interactions with their professors and classmates, as well not enough capacity to concentrate. A study with Hungarian students in their third and fourth year of medical school, during the pandemic, reported that via long-distance education and by making use of materials that were available at home, they were taught basic surgical knot and suture techniques as well as basic laparoscopy; therefore, students achieved the learning goals and they gave ratings of satisfactory and equivalent to the performance achieved in in-person modality before the pandemic [16].
Rajab et al. [17] reported a study with medical students in Saudi Arabia where 42% manifested having little or no online learning experience before the pandemic; 63% preferred combining online and in-person learning; 59% reported having trouble with communication during class; and 57% stated proficiency in using technological tools. An important aspect of the study was that 48% expressed having felt anxiety or stress regarding the pandemic. Despite these limitations, 71% of the college population that was surveyed believes that the COVID-19 pandemic has strengthened their trust in the efficacy of online medical services, and 76% noted that they wished to integrate their online training experience during the pandemic to their professional practice.
Various studies have reported on the diversity of situations that affect students in medical training. Literature on this topic is significant, has been reported from different parts of the world [6,18,19,20,21,22,23,24,25,26], and continues to grow. However, for specialization teaching or postgraduate contexts (like medical residency programs), the effect of virtual classes may be more harmful than good for student health because of the demands of their professional activity and the long hours that they have to spend in a hospital. Having this in mind, there are other factors that are associated with medical residency programs and can affect physical and emotional health, such as stress, anxiety, fatigue, muscular pain, sleep disorders, and weight, amongst others.
For the Present Study
One of the research questions that guided this study was: What are the variables that most frequently influence the activities, professional performance, and attention of medical residents who are enrolled in a private university in northern Peru for their second specialization? A second question was: How is the latent variable of professional performance during the medical residency (academic development and professional training) influenced by other latent variables that are configured from indicators of Academic and professional training received during the residency; Quality of mentorship and/or classes in the university and/or hospital; Accessibility and management of virtual environments to take classes and receive training; Problems related to eating, sleeping, and body weight; Physical and ocular discomfort; Loss of close family and friends due to COVID-19; and Other associated problems?
The aim of this study was to determine the effect of variables like Academic and professional training; Challenges and conditions related to virtual classes during the residency; Physical health factors (Academic Training); Quality of mentorship and/or classes in the university and/or hospital; Accessibility and management of virtual environments to take classes and receive training; Problems related to eating, sleeping, and body weight; Physical and ocular discomfort; Loss of friends and family due to COVID-19; and Other associated problems, on the professional performance of medical residents during the residency program. A second aim was to identify the variables that most frequently influence the activities, professional performance, and attention of residents in their second medical specialty program.
2. Materials and Methods
2.1. Participants
The study consisted of 184 medical students enrolled in the first year of their residency program, for their second medical specialization, at a private university in the city of Trujillo, Peru. According to Soper’s formula for Structural Equation Models (SEM), the minimum sample size required to be able to detect the effect in the frame of the Structural Equations Model (SEM) for a medium a priori effect size (0.3), the desired level of statistical power (0.80), the number of latent variables (3), the number of manifested variables (7), and the level of desired probability (0.05), corresponds to 119 cases [27]. Furthermore, for an Analysis of Multiple Regression, the minimum sample size that is required, according to Soper’s calculator [27], is 103 cases for a medium a priori effect size of 0.15, the statistical power of 0.80, considering a number of 7 predictors, and a level of probability of 0.05. Therefore, the sample size of this investigation is acceptable considering the aim of this research paper.
The final sample consisted of 142 first-year medical residents (66 women and 77 men) who had previously read and signed informed consent to participate in the study. The age of the participants varied between 25 and 48 years, with a median of 32.
The medical residents that participated in this study were from different clinical and surgical specialty backgrounds which are provided by third-level hospitals in Peru; these hospitals have the capacity to satisfy health needs via specialized outpatient care. Third-level Hospitals have these medical specialties: Gynecology and Obstetrics, Rehabilitation Medicine, Intensive Care, Internal Medicine, Oncology, Nephrology, Pneumology, Neurosurgery, Neurology, Ophthalmology, Orthopedics, Traumatology, Otolaryngology (ENT), Pediatrics, Psychiatry, Rheumatology, Urology, and others.
Selection process. During a virtual meeting, the 184 residents were introduced to the investigation that was being conducted and all their questions were answered. Most questions were oriented towards knowing if they would receive benefits if they responded to the survey; they were informed that they would not receive direct benefits, but that their intervention would facilitate knowledge regarding the factors and relations between factors that could contribute to their learning. Students were guaranteed no reprisal or harm if they decided not to participate in the study. The significance of scientific research related to the educational model adopted because of the health situation due to the pandemic was emphasized. Every resident was provided with informed consent which they sent back through the online teaching platform they used.
Characteristics of the medical residency program in Peru. The medical residency is a program that a physician enrolls in to get their second specialization in Medicine. The model implies activities of assistance, conferences related to topics of the medical specialty, and general courses that must be imparted in every specialty (health management, epidemiology, scientific research). The program is three to four years long, carried out in a facility that allows assistance, where residents are tutored by a professor from the university that works in that facility and is specialized in the medical specialty the residents are training in. Generally, doctors finish the residency in three years. These residents are joined through a competition held by the National Council of Medical Residents where they have to pass a national-level exam. The population of this research paper was configured by residents that did their residency program in hospitals located in Northern Peru, but it is important to highlight that the contest is held nationwide.
2.2. Instruments
A questionnaire was developed, and it consisted of eight open-ended questions that asked for an assessment of training and the conditions in the medical residency (Residency Program) during the academic cycle of August–September 2021. The questionnaire is attached in Appendix A, and it includes eight aspects: Academic and professional training received during the residency; Activities, professional performance, and attention during the residency; Quality of mentorship and/or classes in the university and/or hospital; Accessibility and management of virtual environments to take classes and receive training; Problems related to eating, sleeping, and body weight; Physical and ocular discomforts during the residency; The most important loss due to COVD-19, of family members, friends, colleagues, or coworkers; and other problems that affect academic development and professional formation in the residency. These eight general categories were determined by the panel of researchers for this study and were based on the literature that was consulted.
Answers to all eight questions of the survey were assessed in terms of a dichotomy: no difficulty (0) and difficulty (1). Satisfactory evidence of validity of the internal structure was obtained based on a CFA with a robust WLSMV estimator: X2 (19) = 18.856, p = 0.403; CFI = 0.996, TLI = 0.993, RMSEA = 0.018 [CI 90% 0.000, 0.077]; McDonald’s omega coefficient of 0.794 is evidence that the questionnaire offers adequate reliability; an ordinal coefficient theta for internal consistency of 0.809 also supports reliability.
2.3. Ethical Aspects
Residents were presented with all the information available so that they could have knowledge of the intended research. Actions of autonomy, justice, and non-maleficence were emphasized (the conversation about beneficence was aforementioned). Residents were asked to evidence their willingness to participate with sincere and unhindered answers. Regarding the questions and their answers, participants were assured that not sending in the answers would not affect anybody because recollected data would be anonymous. Students that wished to participate in the study had to send their informed consent via email.
2.4. Procedure
Once the medical residents expressed their desire to participate in the study by sending in their informed consent, an email was sent to them, on the first week of December 2021, containing the questionnaire in Microsoft Word and indicating that they had a maximum of one week to send it back via email. Two days before the deadline, every student that expressed consent to participate in the study was sent a reminder. All surveys that were sent in before Tuesday, 14 December 2021, were included in the study.
2.5. Data Analysis
Completed questionnaires were revised online by the research team and exported to Microsoft Excel. Subsequently, content analysis was conducted, and general categories were created for each one of the eight questions. Apart from the seventh question, which included eight categories, every other question contained between five and six categories depending on the various difficulties and challenges the participants expressed in their answers. The answers were organized by conceptual similarities according to the common difficulties or characteristics that were expressed. The resulting categories for each question are mutually exclusive. Appendix B lists the categories that were derived from each one of the eight questions.
Once the categories were formed, the database was restructured by making sure that each one of the participant’s answers was allocated to one of the possible categories per question. This data was imported into JASP, which is a free software for statistical analysis provided by the University of Amsterdam. Descriptive frequency analyses and cumulative percentages were calculated for each question and its categories using JASP 0.16.2; logistic regression analyses were also computed.
The structural regression model analysis was calculated with R (version 4.2.1) [28] using the Weighted Least Squares Mean and Variance (WLSMV) estimator considering that latent variables are configured from manifest variables with categorical values. The adjustment to the structural model is based on what the literature recommends, in other words, the model is considered valid when the Chi-square goodness-of-fit test presents a p-value that is greater than 0.05; CFI and TLI resulting in ≥0.90 indicate a good fit and ≥0.90 indicate a great fit [29,30]; indices resulting in ≤0.08 for SRMEA and SRMR indicate an adequate fit and ≤0.06 indicate a great fit [29,30].
3. Results
The descriptive analysis of the various challenges and difficulties medical residents face during their professional training and practice, in the context of the COVID-19 pandemic, is presented below.
3.1. Academic and Professional Training Received during the Residency
The challenges that first-year medical residents are faced with regarding academic and professional training received during the residency are presented in Table 1. According to the data, 93% of the residents stated that they experienced difficulties in their academic and professional training. The main problem, referred by the participants, was related to management and organizational aspects of the residency program directed by the university which is also related to the orientation and mentorship of the residents (28% of the sample). A second problem, highlighted by 21% of the sample, was related to the activities schedule and the short amount of time that they had because of hospital activities. A third aspect that was pointed out as a problem was the scarce academic activity and teacher performance (17%). To a smaller extent, 15% of the residents expressed that their relationship with tutors, the senior residents, and the assistants during the residency was challenging.

Table 1.
Prevalence of challenges presented during academic and professional training.
3.2. Activities, Professional Performance, and Attention during the Residency Program
Challenges in the performance of professional activities are presented in Table 2. Around 80% of the residents stated that various difficulties were presented when offering their professional services and activities during the medical residency. Most of the residents (32%) mentioned that the main problem was the distribution of activities and the workload. A second aspect that affected professional performance had to do with problems related to the services that were provided by the hospital where the residency program was taking place, the lack of medical specialties, and challenges related to patient demand (14%). The categories that remain were perceived by the residents as presenting similar levels of difficulty and in smaller proportions (between 11% and 12%).

Table 2.
Prevalence of challenges presented during professional activities and performance.
3.3. Mentorship and/or Class Quality in the University and/or Hospital
The quality of mentorship and/or classes in the university is presented in Table 3; 78% of the residents reported difficulties. The fourth part of the sample referred to problems of accessibility, and 2 out of every 10 residents mentioned that the quality of the tutoring sessions and/or classes had been negatively affected because of poor planning and organization. Likewise, for a lower percentage of residents, challenges were related to teacher or hospital mentor support (17%) and schedules (16%).

Table 3.
Prevalence of challenges due to mentorship and/or classes in the university and/or hospital.
3.4. Accessibility and Management of Virtual Environments for Classes and Training
Around three-fourths of the sample of medical residents mentioned challenges related to accessibility and management of virtual environments for classes and training (Table 4). Connectivity represented the biggest problem (30%). Likewise, every 2 out of every 10 residents mentioned that they experienced problems with access to equipment or workspaces and with the overall management of the institution.

Table 4.
Prevalence of challenges related to accessibility and management of virtual environments for classes and training.
3.5. Problems Related to Eating, Sleeping, and Body Weight
During the pandemic, around 80% of the residents mentioned problems related to eating, sleeping, and body weight (Table 5); the most prevalent, affecting at least half of the residents, were skipping or postponing meals and sleep disorders. The data shows that 28% of the residents mentioned having difficulties due to a poor diet and variations in weight.

Table 5.
Prevalence of challenges related to eating, sleeping, and body weight.
3.6. Physical and Visual Discomfort
According to Table 6, a total of 8 out of 10 residents have experienced physical and ocular discomfort. One-third of the residents expressed musculoskeletal disorders. Likewise, an important part of the sample (30%), mentioned feeling fatigue, headaches, and migraines. Only 10% referred to vision-related discomfort.

Table 6.
Prevalence of challenges related to physical and visual discomfort.
3.7. Loss of Family Members or Close Friends Due to COVID-19
Data presented in Table 7 shows that 40% of the residents lost a family member or a close friend to COVID-19. Around 28% reported the loss of family members, both close relatives and next of kin. Additionally, 12.7% of the residents mentioned the passing of friends and coworkers due to COVID-19.

Table 7.
Prevalence of challenges related to the loss of family members or close friends due to COVID-19.
3.8. Other Challenges That Affect Academic Growth and Professional Training
According to the data presented in Table 8, at least 64% of the residents identify additional challenges that affect their academic growth and professional training. A group of residents (18.3%) identified the inefficiency of the residency program, and the lack of academic materials, internet service, and arrangements as a problem. Other difficulties that were referred by 19.7% of the residents were work overload, lack of rotation, mistreatment, and problematic work relationships and environment. The third group of problems, mentioned by 26% of the residents, was related to health issues, fear of COVID-19, and being away from their families.

Table 8.
Prevalence of other challenges that affect academic growth and professional training.
3.9. Factors That Are Associated with Difficulties Regarding Professional Activities or Services Provided during the Medical Residency
After multivariate logistic regression analysis, crude and adjusted by sex and age of the participants, the possibility of confounding factors related to sex and age was discarded. The results of two binomial logistic regression models to evaluate the effects of academic and personal factors associated with challenges related to professional activities or services provided during the residency are shown in Table 9. The adjusted regression model shows almost similar relations between the predictor variables and the dependent variable (professional performance), in relation to the crude model.

Table 9.
Binomial logistic regression models for professional growth during the medical residency.
The global goodness-of-fit test of the adjusted model was satisfactory because the log-likelihood value of −2 reduced significantly with respect to the base model (Δ −2LL = 42.67); McFadden’s R2 indicated very good model fit (R2McF = 0.31); the Hosmer and Lemeshow test also indicated good model fit (X2 (8) = 4.494, p = 0.81); the area under the curve AUC-ROC allows for the correct classification of 86% (over the critical value of ≥ 70%), evidencing that the result that was found corresponds with a good logistic model; also, according to Nagelkerke’s R2, the model allows for the explanation of the DV based on the risk factors at 41.7%. Consequently, all these measurements support the adjusted logistic model as valid for the explanation of challenges that first-year medical residents find when performing professional activities or providing a service during the residency program.
On the other hand, according to the Odds Ratio (OR) values, four factors that were considered in the model, affect the medical resident’s performance negatively (OR > 1). Specifically, medical residents with difficulties related to the quality of the mentorship and classes provided by the university (F2); accessibility and management of virtual environments to take classes (F3); diet, sleep, and body weight (F4); as well as other challenges that affect academic and professional training (F7), have 3 to 4 times more probability of encountering difficulties when performing professional activities and providing services during the residency program, than the residents that did not experience or identify those challenges.
3.10. Explanatory Structural Model of the Difficulties Related to the Professional Performance of Medical Residents
With the purpose of offering a robust and parsimonious model which allows for the explanation of the professional performance of medical residents in relation to latent variables (constructs) based on indicators that were directly measured, a structural model was tested using a structural regression modeling technique (Figure 1). The manifest variables of perceived challenges related to “academic and professional development” and “other factors that affect academic development” make the “Academic Training” construct; the manifest variables “mentorship and online class quality” along with “access and use of technology for virtual education” constitute a latent variable because they refer to the teaching-learning construct which is an inherent part of medical resident’s training; a third construct is represented by two manifest variables that are linked to the concept “Health Condition”.
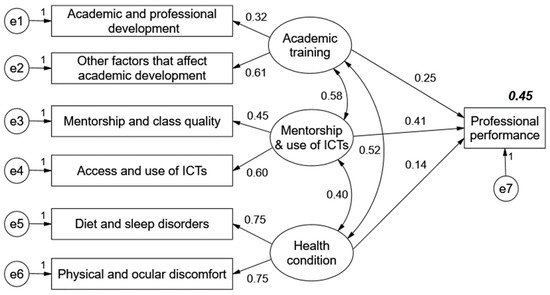
Figure 1.
Explanatory structural model of the difficulties related to the professional performance of medical residents.
The structural model (Figure 1) is valid because it presents very satisfactory goodness-of-fit indices: χ2 (9) = 13.578, p = 0.138; CFI = 0.97; TLI = 0.92; RMSEA = 0.06 [0.00, 0.12]; SRMR = 0.04; in other words, the results indicate that the structural model presents adequate fit (χ2), acceptable parsimony (χ2/gl = 1.51), very good—good fit for incremental adjustment indices (CFI and TLI), and good fit for absolute fit indices (RMSEA and SRMR).
Figure 1 shows that challenges related to academic training, mentorship, access to ICT, and health problems, have a direct impact on 45% of the overall difficulties related to professional performance during the residency. According to the coefficient paths or estimated parameters, the factor with the most impact is the one related to problems with mentorship and the use of ICT for online education. The second factor that directly aggravated professional performance was the one related to problems with academic training. Finally, health problems also negatively affect the quality and efficiency of the professional performance of medical residents.
4. Discussion
In light of the results of the present study, the first aspect to highlight is that 80% of the physicians who were surveyed and went through postgraduate specialization training (the medical residency in Perú) expressed having difficulties in their professional performance during the residency program. What are the reasons for the challenges that medical residents experience in their residency programs which affect their professional development? The results suggest that one of the main contributing factors has to do with the academic and professional training challenges that resulted from the shift to online classes due to the pandemic, considering that the program is planned to be (and essentially was) an in-person program. This finding aligns with the results that were reported in previous studies about student perceptions of pertinence and quality of online classes due to the pandemic [7,8,9,10,13,15]. Students that participated in such studies expressed their contention with the training quality of professional competencies via online classes due to the pandemic. Nonetheless, the results of the present study paint a considerably wider picture, where 93% of the students expressed having difficulties in their academic training and not just disagreement with the quality of the training. This should be considered an important factor because medical residencies are advanced levels of education (in Peru they are equivalent to a postgraduate specialization). Therefore, for a big part of the sample of residents that were surveyed, specialized training has not been satisfactory, and they consider that this factor (online training) is a problem that affects their professional growth in the residency program. These difficulties, which were revealed during the training of medical residents, can have an impact on the fulfillment of their professional competencies [31].
A second aspect that resulted as relevant was the one concerning the health conditions of medical residents during the pandemic and their residency program; specifically, conditions related to diet, sleep, and body weight disorders, as well as physical discomfort and problems with their vision. Apparently, these are common symptoms related to online medical training during the pandemic [4,14]. However, the data from this study must be considered with caution when trying to explain the relationship between physical health issues and the professional performance of medical residents. Residents expressed having physical health problems and this might be due to the nature of their professional medical activity at such a specialized level (postgraduate) in a hospital, or to the additional activities that the resident had to perform during the pandemic such as online classes, tutoring sessions, and homework.
The findings of this study coincide with the results that were obtained by other researchers when studying health problems in medical students taking classes during the COVID-19 pandemic. Similar to what was found in this study, other papers have reported that medical students have various physical health problems [23,26]. Likewise, most of the symptoms reported by medical students are associated with emotional and mental health issues [19,21], such as depression [18], anxiety [24], and stress [22,25]. Another aspect to consider is the risk of burnout among medical residency students [32].
A third aspect related to the challenges medical residents face during their professional training includes two fundamental factors of the specialization training process: the quality of mentorship and accessibility to, as well as management of, virtual environments. Both aspects have been identified as factors that hinder the performance of medical residents. The first aspect is related to the supervision and support teachers give students, aspects which have previously been reported as fundamental for growth within the discipline and professional development [7,33,34]. Clearly, the difficulty for medical residents to receive tutoring sessions, support, and feedback on their learning is an essential part of why they express having problems in their training as medical residents.
In this sense, medical residents face two main problems in their professional and academic development during the pandemic: (1) Their services and performance are affected by the circumstances and the risk of transmission that exists in their places of work (hospitals that host their residency program) and during their commute to the hospital which may involve public transportation; (2). Their performance is also affected by the tutoring and support they receive during training. The present study found that the quality and pertinence of mentorship and support during the training of medical residents is perceived as an aspect that affects professional and academic performance.
Another factor that presents difficulties for the professional performance of medical residents is the problem with access to online resources and connectivity issues. The medical residents that were surveyed for this study expressed that the places that host their residency programs do not have the resources or conditions for online work, this being taking online classes, having mentorship meetings, searching for information that is up to date, or any other professional activity that requires virtual resources. Given that in-person gatherings are limited, students would hope that the hospitals that host their residency programs could provide better conditions for access to technological resources and overall connectivity. Accessibility issues in postgraduate medical training programs have also been reported by Pomares-Bory et al. [8]. In addition, after a systematic revision of Learning in Latin American Higher Education during the COVID-19 Pandemic, Salas-Pilco et al. [13] suggested two aspects related to college training during the pandemic that needed urgent attention: (a) improving internet connectivity, and (b) a guarantee of quality online learning for higher education.
Inequality of opportunity to access virtual environments and unequal availability of technological resources in the hospitals that host residency programs can be determining factors for the differences in academic growth and professional performance of medical residents. Thus, residency program hosts or venues can hinder equality of opportunity to access training and experience professional growth through virtual environments [1,2,3,5,6], contributing to inequality in higher-level specialized medical education.
When considering the effect of second-order latent variables (such as Academic training, Mentorship and use of ICT, and Health conditions) over the professional performance of medical residents, the factor with the most predictive power is Mentorship and use of ICT, followed by Academic training. This finding means that, for medical residents during the pandemic, health conditions are important, but factors associated with mentorship and academic training are better at predicting their professional performance.
As a final note regarding the use of medical simulation education, during the COVID- 2019 pandemic, postgraduate medical programs in Peru did not use simulation teaching because both training and professional attention were offered in person.
5. Conclusions
Professionals that pursue medical residency programs during the pandemic face two situations they must simultaneously consider while receiving specialized training in public hospitals that belong to The Ministry of Health of Perú. On the one hand, residents must take academic courses and have tutoring sessions; on the other, they must also perform professional activities related to a medical specialty.
In the case of this group of Peruvian medical residents that are enrolled in a private university and perform professional activities in different hospitals, the factors that primarily affect their professional development and growth during the residency program are the challenges related to academic training and tutoring during their first year of the program. Furthermore, an important percentage of these first-year medical residents expressed having experienced diet, sleep, and body weight disorders, as well as physical discomfort and problems with their vision. Although these health problems influence the occurrence of certain difficulties while residents are providing professional medical services, once the effects of academic training and tutoring during the residency are controlled, they can also be predictors of the professional performance of these physicians in training.
The present study allowed the knowledge of variables that explain, through self-reports, the challenges first-year medical residents face in relation to their professional performance, development, and growth. Future research should be oriented towards the comparison of these types of relationships in contexts with and without a pandemic. This will allow for a better understanding of how the current pandemic situation affects the training process and health conditions of medical residents.
Author Contributions
Conceptualization, A.B.-R.; methodology, A.B.-R., M.T.-A., W.C.-L., M.C.-R. and J.Q.-P.; validation, W.C.-L. and A.B.-R.; formal analysis, M.C.-R.; investigation, A.B.-R. and M.T.-A.; resources, A.B.-R., M.T.-A., W.C.-L., M.C.-R. and J.Q.-P.; data curation, A.B.-R. and W.C.-L.; writing—original draft preparation, A.B.-R. and W.C.-L.; writing—review and editing, M.C.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received funding from the 2021 Research Support Fund, Universidad Cesar Vallejo University. Project code, MD-16.
Institutional Review Board Statement
The study was conducted according to the Principles of the Declaration of Helsinki. The administration of questionnaires and research on medical residents was authorized by the high board of the Universidad Privada Antenor Orrego of the City of Trujillo for strictly scientific purposes. In addition, because the study was exploratory, of short duration, and had no funding, no ethical revision and approval were solicited.
Informed Consent Statement
Informed consent was obtained from every participant involved in the study.
Data Availability Statement
The authors manifest that the data (answers to the questions and the database), sans personal information of the participants, will be available and can be solicited by contacting the first author of this paper. Shared data will comply with the consent provided by the participants regarding the use of confidential data.
Conflicts of Interest
The authors declare no conflict of interest that could have an inappropriate influence on the representation or interpretation of the results of the investigation. This investigation was free of institutional encroachment or interest. No funding was provided by any institution or person that could distort our findings or weigh in on the decision of publishing results.
Appendix A
Formative Assessment and Conditions Questionnaire
GENERAL INFORMATION
Sex _____ Age ___________ Date _________ Current Training Cycle ______________
Residency Location _________________________ Year of enrollment _____________
Dear student, this questionnaire aims to identify the difficulties you may have faced in your formation during the current academic cycle.
Please, respond honestly.
Instructions:
Write, at least, two difficulties you have faced during this cycle (August–December 2021) in each one of the different aspects listed below:
- Academic and professional training received during the residency
_____________________________
_____________________________
- 2.
- Your activities, professional performance, and attention during the residency
_____________________________
_____________________________
- 3.
- The quality of your mentorship and/or classes in the university and/or hospital
_____________________________
_____________________________
- 4.
- Accessibility and management of virtual environments to take your classes and receive training
_____________________________
_____________________________
- 5.
- Problems related to eating, sleeping, and body weight
_____________________________
_____________________________
- 6.
- Mention some of the physical and vision-related discomforts you have had
_____________________________
_____________________________
- 7.
- Mention the most important loss you have had, due to COVD-19, of family members, friends, colleagues, or coworkers
_____________________________
_____________________________
- 8.
- Mention any other problem that currently affects your academic development and professional formation in the residency
_____________________________
_____________________________
Appendix B

Table A1.
Categories that resulted from the answers to each one of the eight questions.
Table A1.
Categories that resulted from the answers to each one of the eight questions.
| Factors | Categories/Descriptors |
|---|---|
| 1. Academic and professional training received during the residency | Inadequate equipment and didactic resources Incompatible schedules and times Teachers and scarce academic activity Assistants, senior residents, and tutors University, mentorship, orientation, and organization I do not have problems, it is okay |
| 2. Activities, professional performance, and attention during the residency | Distribution and workload (overload) Program venue, facilities, equipment, and services Professional activity The support and supervision of senior residents, tutors, and/or teachers Professional services, specializations, and patient demand No difficulties |
| 3. The quality of your mentorship and/or classes in the university and/or hospital | Schedules Teacher or hospital mentor backup Planning and organization of the university/residency program Accessibility issues (coverage and connectivity) No problem |
| 4. Accessibility and management of virtual environments to take your classes and receive training | Equipment, cellphone Connectivity issues Access to equipment, workspaces, or rooms Programming or planning by the institution No problem |
| 5. Problems related to eating, sleeping, and body weight | Weight loss or gain Poor diet (heavy on carbohydrates) Sleep problems Skipping or postponing meals No problem |
| 6. Physical and ocular discomforts | Musculoskeletal disorders and back pain Generalized fatigue, exhaustion Headache, migraines Stomach, skin, and lower limb disorders Problems with vision No discomfort |
| 7. Important loss due to COVD-19, of family members, friends, colleagues, or coworkers | Direct family (father/mother, partner, son/daughter, brother/sister) Close relatives (uncles/aunts, grandparents, cousins, father/mother-in-law) Colleagues and coworkers (in the Health field) Close friends and acquaintances None |
| 8. Other problem that currently affecting academic growth and professional training in the residency | Being away from my family/family load Distance between the residency and work Lack of academic material, internet service, and arrangements Work relationships, work environment, mistreatment Health and personal problems Pandemic, and fear of COVID Time, work overload, no rotation None |
References
- O’Dea, X.C.; Stern, J. Virtually the same? Online higher education in the post COVID-19 era. Br. J. Educ. Technol. 2022, 53, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Tapia, J.; Merino-Tejedor, E.; Huertas, J.A. Academic engagement: Assessment, conditions, and effects a study in higher education from the perspective of the person-situation interaction. Eur. J. Psychol. Educ. 2022, 37, 1–25. [Google Scholar]
- Greenhow, C.; Lewin, C. Online and blended learning: Contexts and conditions for education in an emergency. Br. J. Educ. Technol. 2021, 52, 1301–1305. [Google Scholar] [CrossRef]
- Spunei, E.; Frumusanu, N.-M.; Muntean, R.; Mărginean, G. Impact of COVID-19 pandemic on the educational-instructional process of the students from technical faculties. Sustainability 2022, 14, 8586. [Google Scholar] [CrossRef]
- Meletiou-Mavrotheris, M.; Eteokleous, N.; Stylianou-Georgiou, A. Emergency remote learning in higher education in Cyprus during COVID-19 lockdown: A zoom-out view of challenges and opportunities for quality online learning. Educ. Sci. 2022, 12, 477. [Google Scholar] [CrossRef]
- Bazán-Ramírez, A.; Quispe-Morales, R.A.; Huauya-Quispe, P.; Ango-Aguilar, H. Accesibilidad, dificultades y ventajas del estudio online por COVID-19 en un posgrado presencial en educación. [Accessibility, difficulties, and advantages of the online study for COVID-19 in a presential postgraduate on education]. Propósitos Y Represent. 2020, 8, e659. [Google Scholar] [CrossRef]
- Liu, J.; Cohen, J. Measuring teaching practices at scale: A novel application of text-as-data methods. Educ. Eval. Pol. Anal. 2021, 43, 587–614. [Google Scholar] [CrossRef]
- Pomares-Bory, E.; Arencibia-Flores, L.; Miralles-Aguilera, E.; Iglesias-Ramírez, B. Maestría en educación médica versión online de un curso presencial durante la pandemia COVID-19. [Online version of a master’s degree in medical education as part of face-to face course during the COVID-19 pandemic]. Rev. Cuba. Educ. Medica Super 2021, 35, e3018. [Google Scholar]
- Torres Martín, C.; Acal, C.; El Homrani, M.; Mingorance Estrada, Á.C. Impact on the virtual learning environment due to COVID-19. Sustainability 2021, 13, 582. [Google Scholar] [CrossRef]
- Wang, R.; Han, J.; Liu, C.; Xu, H. How do university students’ perceptions of the instructor’s role influence their learning outcomes and satisfaction in cloud-based virtual classrooms during the COVID-19 pandemic. Front. Psychol. 2021, 13, 627443. [Google Scholar] [CrossRef]
- Mukhtar, K.; Javed, K.; Arooj, M.; Sethi, A. Advantages, limitations and recommendations for online learning during COVID-19 pandemic era. Pak. J. Med. Sci. 2020, 36, 27–31. [Google Scholar] [CrossRef]
- Bravo, F.; Quezada, T. Educación virtual en la universidad en tiempos de COVID-19. [Virtual education at the university in times of COVID-19]. Espíritu Emprend. TES 2021, 5, 154–166. [Google Scholar] [CrossRef]
- Salas-Pilco, S.Z.; Yang, Y.; Zhang, Z. Student engagement in online learning in Latin American higher education during the COVID-19 pandemic: A systematic review. Br. J. Educ. Technol. 2022, 53, 593–619. [Google Scholar] [CrossRef]
- Alamo, Y.; Espinoza, D.; Huillca, H.; Miranda, A.; Palomino, L.; Romero, D.; Urbano, A.; Guzmán, S.; Moscoso, J.; Pérez, A. Cambios en la ergonomía en tiempos de COVID-19 en estudiantes de una universidad peruana. [Changes in ergonomics in times of COVID-19 in students of a Peruvian university]. J. Health Med. Sci. 2021, 7, 67–74. [Google Scholar]
- Sierra, C.R.; López, M.; Azar, F.; Trevethan, S. La educación médica durante la contingencia sanitaria por COVID-19: Lecciones para el futuro. [Medical Education during the health contingency by COVID-19: Lessons for the future]. Arch. Cardiol. Mex. 2020, 90 (Suppl. S1), 50–55. [Google Scholar]
- Schlégl, Á.T.; Pintér, Z.B.; Kovács, A.; Kopjár, E.; Varga, P.; Kardos, D.; Berner-Juhos, K.; Maróti, P.; Füzesi, Z. Distance education for basic surgical skills using homemade tools—diy methods for emergency situations. Sustainability 2022, 14, 8639. [Google Scholar] [CrossRef]
- Rajab, M.H.; Gazal, A.M.; Alkattan, K. Challenges to Online Medical Education during the COVID-19 Pandemic. Cureus 2020, 12, e8966. [Google Scholar] [CrossRef]
- Aamir, S.; Winkel, C. The impact of COVID-19 on Saudi Arabian female students: An application of the CES-D depression scale. J. Educ. Soc. Res. 2021, 11, 23–31. [Google Scholar] [CrossRef]
- Akpınar, E. The effect of online learning on tertiary level students’ mental health during the COVID-19 lockdown. Eur. J. Soc. Behav. Sci. 2021, 30, 52–62. [Google Scholar] [CrossRef]
- Al-Alami, Z.M.; Adwan, S.W.; Alsous, M. Remote learning during COVID-19 lockdown: A study on anatomy and histology education for pharmacy students in Jordan. Anat. Sci. Educ. 2022, 15, 249–260. [Google Scholar] [CrossRef]
- Bolatov, A.K.; Seisembekov, T.Z.; Askarova, A.Z.; Baikanova, R.K.; Smailova, D.S.; Fabbro, E. Online-learning due to COVID-19 improved mental health among medical students. Medical Sci. Educ. 2021, 31, 183–192. [Google Scholar] [CrossRef] [PubMed]
- De la Fuente, J.A. Path analysis model of protection and risk factors for university academic stress: Analysis and psychoeducational implications for the COVID-19 emergency. Front. Psychol. 2021, 12, 562372. [Google Scholar] [CrossRef] [PubMed]
- Sanz, E.J.; Vicente, J.; Prieto, A. Experiencias de docencia virtual en facultades de medicina españolas durante la pandemia COVID-19 (II): Farmacología, inmunología [Virtual Teaching Experiences in Spaniard Schools of Medicine during the COVID-19 pandemic (II): Pharmacology, Immunology]. Rev. Espa. Educ. Méd. 2020, 1, 74–81. [Google Scholar]
- Saravia-Bartra, M.M.; Cazorla-Saravia, P.; Cedillo-Ramírez, L. Anxiety level of first-year medical students in a private university in Peru during COVID-19. Rev. Fac. Med. Hum. URP 2020, 20, 568–573. [Google Scholar]
- Schmits, E.; Dekeyser, S.; Klein, O.; Luminet, O.; Yzerbyt, V.; Glowacz, F. Psychological distress among students in higher education: One year after the beginning of the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 7445. [Google Scholar] [CrossRef]
- Srivastava, S.; Jacob, J.; Charles, A.S.; Daniel, P.; Mathew, J.K.; Shanthi, P.; Devamanic, K.; Mahasampathd, G.; Rabi, S. Emergency remote learning in anatomy during the COVID-19 pandemic: A study evaluating academic factors contributing to anxiety among first year medical students. Med. J. Armed. Forces India 2021, 77, 90–98. [Google Scholar] [CrossRef]
- Soper, D.S. A-priori Sample Size Calculator for Structural Equation Models [Software]. 2021. Available online: https://www.danielsoper.com/statcalc (accessed on 15 August 2022).
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://cran.r-projet.org/ (accessed on 10 June 2022).
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling; Routledge: London, UK, 2016. [Google Scholar]
- Bianchi, S.; Gatto, R.; Fabiani, L. Effects of the SARS-CoV-2 pandemic on medical education in Italy: Considerations and tips. Euro Mediterr. Biomed. J. 2020, 15, 100–101. [Google Scholar] [CrossRef]
- Alsaywid, B.; Housawi, A.; Lytras, M.; Halabi, H.; Abuzenada, M.; Alhaidar, S.A.; Abuznadah, W. Residents’ Training in COVID-19 Pandemic Times: An Integrated Survey of Educational Process, Institutional Support, Anxiety and Depression by the Saudi Commission for Health Specialties (SCFHS). Sustainability 2020, 12, 10530. [Google Scholar] [CrossRef]
- Bazán-Ramírez, A.; Capa-Luque, W.; Bello-Vidal, C.; Quispe-Morales, R. Influence of teaching and the teacher’s feedback perceived on the didactic performance of Peruvian postgraduate students attending virtual classes during the COVID-19 pandemic. Front. Educ. 2022, 7, 818209. [Google Scholar] [CrossRef]
- Krijgsman, C.; Mainhard, T.; Borghouts, L.; van Tartwijk, J.; Haerens, L. Do goal clarification and process feedback positively affect students’ need-based experiences? A quasi-experimental study grounded in self-determination theory. Phys. Edu. Sport Pedagog. 2021, 26, 483–503. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).