Lean, Six Sigma, and Simulation: Evidence from Healthcare Interventions
Abstract
1. Introduction
- RQ1. What are the effects of dual interventions of LSS and simulation on healthcare services?
- RQ2. How is such a dual intervention of simulation and LSS implemented in healthcare?
- RQ3. What simulation paradigms have been used to support dual interventions in healthcare?
- RQ4. What tools of LSS have been used to support dual interventions in healthcare?
- RQ5. What are the complementary roles of simulation and LSS in healthcare?
- RQ6. What is the effect on patient and staff satisfaction after a dual intervention?
2. Theoretical Framework
2.1. Simulation
2.2. Lean Interventions
2.3. Six Sigma
2.4. Main Outcomes in Simulation and Improvement Approaches Interventions
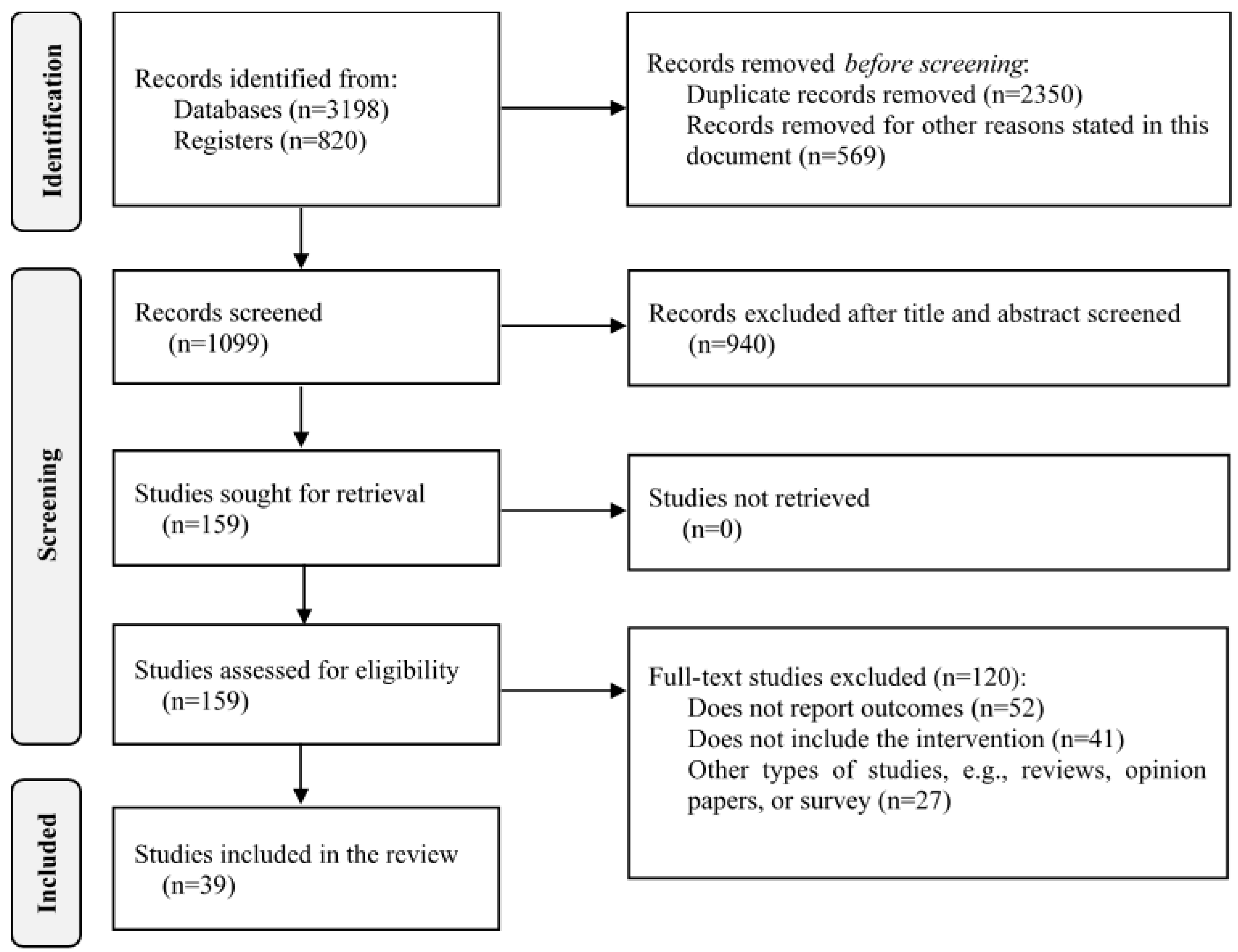
3. Materials and Methods
3.1. Search Strategy
3.2. Selection of Studies
| Process | Criteria | Description |
|---|---|---|
| Search strategy | Data sources |
|
| Studies |
| |
| Selection of studies | Participants |
|
| Intervention |
| |
| Comparator |
| |
| Outcomes |
| |
| Study design |
| |
| Exclusion criteria |
| |
| Data extraction and synthesis | Review processExtracted data |
|
| Risk of bias | Tool |
|
3.3. Data Analysis, Synthesis, and Risk of Bias
4. Results
5. Discussion
5.1. Effects of LSS and Simulation on Healthcare Services
5.2. Dual Interventions of LSS and Simulation in Healthcare Services
5.3. Simulation Paradigms Utilized in the Interventions
5.4. LSS Tools Utilized in the Interventions
5.5. Complementary Role of Simulation and LSS in the Interventions
5.6. Effects on Patient and Staff Satisfaction
5.7. Barriers and Challenges
5.8. Study Limitations
6. Conclusions
7. Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hathaliya, J.J.; Tanwar, S.; Tyagi, S.; Kumar, N. Securing electronics healthcare records in Healthcare 4.0: A biometric-based approach. Comput. Electr. Eng. 2019, 76, 398–410. [Google Scholar] [CrossRef]
- Tanwar, S.; Parekh, K.; Evans, R. Blockchain-based electronic healthcare record system for healthcare 4.0 applications. J. Inf. Secur. Appl. 2020, 50, 102407. [Google Scholar] [CrossRef]
- Tortorella, G.L.; Fogliatto, F.S.; Mac Cawley Vergara, A.; Vassolo, R.; Sawhney, R. Healthcare 4.0: Trends, challenges and research directions. Prod. Plan. Control 2020, 31, 1245–1260. [Google Scholar] [CrossRef]
- Marshall, D.; Burgos-Liz, L.; Ijzerman, M.; Crown, W.; Padula, W.; Wong, P.; Pasupathy, K.; Higashi, M.; Osgood, N. Selecting a dynamic simulation modeling method for health care delivery research—Part 2: Report of the ISPOR dynamic simulation modeling emerging good practices task force. Value Health 2015, 18, 147–160. [Google Scholar] [CrossRef]
- De Mast, J.; Kemper, B.; Does, R.J.M.M.; Mandjes, M.; Van Der Bijl, Y. Process improvement in healthcare: Overall resource efficiency. Qual. Reliab. Eng. Int. 2011, 27, 1095–1106. [Google Scholar] [CrossRef]
- Holtz, B.E. Patients Perceptions of Telemedicine Visits before and after the Coronavirus Disease 2019 Pandemic. Telemed. e-Health 2021, 27, 107–112. [Google Scholar] [CrossRef]
- Lee, E.; Atallah, H.; Wright, M.; Post, E.; Thomas, C.; Wu, D.; Haley, L. Transforming hospital emergency department workflow and patient care. Interfaces 2015, 45, 58–82. [Google Scholar] [CrossRef]
- Arcidiacono, G.; Pieroni, A. The revolution Lean Six Sigma 4.0. Int. J. Adv. Sci. Eng. Inf. Technol. 2018, 8, 141–149. [Google Scholar] [CrossRef]
- Baril, C.; Gascon, V.; Miller, J.; Côté, N. Use of a discrete-event simulation in a Kaizen event: A case study in healthcare. Eur. J. Oper. Res. 2016, 249, 327–339. [Google Scholar] [CrossRef]
- Davies, R.; Davies, H. Modelling Patient Flows and Resource Provision in Health Systems. Omega 1994, 22, 123–131. [Google Scholar] [CrossRef]
- Forsberg, H.H.; Aronsson, H.; Keller, C.; Lindblad, S. Managing health care decisions and improvement through simulation modeling. Qual. Manag. Health Care 2011, 20, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Tlapa, D.; Tortorella, G.; Fogliatto, F.; Kumar, M.; Mac Cawley, A.; Vassolo, R.; Enberg, L.; Baez-Lopez, Y. Effects of Lean Interventions Supported by Digital Technologies on Healthcare Services: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9018. [Google Scholar] [CrossRef] [PubMed]
- DelliFraine, J.L.; Wang, Z.; McCaughey, D.; Langabeer, J.R.; Erwin, C.O. The use of six sigma in health care management: Are we using it to its full potential? Qual. Manag. Health Care 2014, 23, 240–253. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chiarini, A.; Baccarani, C. TQM and lean strategy deployment in Italian hospitals: Benefits related to patient satisfaction and encountered pitfalls. Leadersh. Health Serv. 2016, 29, 377–391. [Google Scholar] [CrossRef]
- Sirvent, J.M.; Gil, M.; Alvarez, T.; Martin, S.; Vila, N.; Colomer, M.; March, E.; Loma-Osorio, P.; Metje, T. Lean techniques to improve flow of critically ill patients in a health region with its epicenter in the intensive care unit of a reference hospital. Med. Intensiv. (Engl. Ed.) 2016, 40, 266–272. [Google Scholar] [CrossRef]
- Hseng-Long, Y.; Chin-Sen, L.; Chao-Ton, S.; Pa-Chun, W. Applying lean six sigma to improve healthcare: An empirical study. Afr. J. Bus. Manag. 2011, 5, 12356–12370. [Google Scholar] [CrossRef]
- Gayed, B.; Black, S.; Daggy, J.; Munshi, I.A. Redesigning a Joint Replacement Program using Lean Six Sigma in a Veterans Affairs Hospital. JAMA Surg. 2013, 148, 1050–1056. [Google Scholar] [CrossRef]
- Cromwell, S.; Chiasson, D.A.; Cassidy, D.; Somers, G.R. Improving Autopsy Report Turnaround Times by Implementing Lean Management Principles. Pediatr. Dev. Pathol. 2018, 21, 41–47. [Google Scholar] [CrossRef]
- Van Vliet, E.J.; Sermeus, W.; Van Gaalen, C.M.; Sol, J.C.A.; Vissers, J.M.H. Efficacy and efficiency of a lean cataract pathway: A comparative study. Qual. Saf. Health Care 2010, 19, 83–93. [Google Scholar] [CrossRef]
- Hydes, T.; Hansi, N.; Trebble, T.M. Lean thinking transformation of the unsedated upper gastrointestinal endoscopy pathway improves efficiency and is associated with high levels of patient satisfaction. BMJ Qual. Saf. 2012, 21, 63–69. [Google Scholar] [CrossRef]
- Blackmore, C.; Kaplan, G. Lean and the perfect patient experience. BMJ Qual. Saf. 2017, 26, 85–86. [Google Scholar] [CrossRef] [PubMed]
- McDermott, A.; Kidd, P.; Gately, M.; Casey, R.; Burke, H.; O’Donnell, P.; Kirrane, F.; Dinneen, S.F.; O’Brien, T. Restructuring of the Diabetes Day Centre: A pilot lean project in a tertiary referral centre in the West of Ireland. BMJ Qual. Saf. 2013, 22, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Halim, U.A.; Khan, M.A.; Ali, A.M. Strategies to Improve Start Time in the Operating Theatre: A Systematic Review. J. Med. Syst. 2018, 42, 160. [Google Scholar] [CrossRef] [PubMed]
- Fragapane, G.; Roy, D.; Sgarbossa, F.; Strandhagen, J.O. Planning Autonomous Material Transportation in Hospitals. In Advances in Production Management Systems. Artificial Intelligence for Sustainable and Resilient Production Systems; Springer: Cham, Switzerland, 2021; pp. 24–32. [Google Scholar]
- El Hage, J.; Gravitt, P.; Ravel, J.; Lahrichi, N.; Gralla, E. Supporting scale-up of COVID-19 RT-PCR testing processes with discrete event simulation. PLoS ONE 2021, 16, e0255214. [Google Scholar] [CrossRef] [PubMed]
- Kern, C.; König, A.; Fu, D.J.; Schworm, B.; Wolf, A.; Priglinger, S.; Kortuem, K.U. Big data simulations for capacity improvement in a general ophthalmology clinic. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 1289–1296. [Google Scholar] [CrossRef] [PubMed]
- Noto, G.; Cosenz, F. Introducing a strategic perspective in lean thinking applications through system dynamics modelling: The dynamic Value Stream Map. Bus. Process Manag. J. 2020, 27, 306–327. [Google Scholar] [CrossRef]
- Possik, J.; Gorecki, S.; Asgary, A.; Solis, A.O.; Zacharewicz, G.; Tofighi, M.; Shafiee, M.A.; Merchant, A.A.; Aarabi, M.; Guimaraes, A.; et al. A Distributed Simulation Approach to Integrate AnyLogic and Unity for Virtual Reality Applications: Case of COVID-19 Modelling and Training in a Dialysis Unit. In Proceedings of the 2021 IEEE/ACM 25th International Symposium on Distributed Simulation and Real Time Applications, DS-RT, Valencia, Spain, 27–29 September 2021. [Google Scholar]
- Kongpakwattana, K.; Chaiyakunapruk, N. Application of Discrete-Event Simulation in Health Technology Assessment: A Cost-Effectiveness Analysis of Alzheimer’s Disease Treatment Using Real-World Evidence in Thailand. Value Health 2020, 23, 710–718. [Google Scholar] [CrossRef] [PubMed]
- O’mahony, L.; McCarthy, K.; O’donoghue, J.; Teeling, S.P.; Ward, M.; McNamara, M. Using lean six sigma to redesign the supply chain to the operating room department of a private hospital to reduce associated costs and release nursing time to care. Int. J. Environ. Res. Public Health 2021, 18, 11011. [Google Scholar] [CrossRef]
- Peimbert-García, R.E.; Gutiérrez-Mendoza, L.M.; García-Reyes, H. Applying lean healthcare to improve the discharge process in a mexican academic medical center. Sustainability 2021, 13, 10911. [Google Scholar] [CrossRef]
- Daly, A.; Wolfe, N.; Teeling, S.P.; Ward, M.; McNamara, M. Redesigning the process for scheduling elective orthopaedic surgery: A combined lean six sigma and person-centred approach. Int. J. Environ. Res. Public Health 2021, 18, 11946. [Google Scholar] [CrossRef]
- Alowad, A.; Samaranayake, P.; Ahsan, K.; Alidrisi, H.; Karim, A. Enhancing patient flow in emergency department (ED) using lean strategies–an integrated voice of customer and voice of process perspective. Bus. Process Manag. J. 2020, 27, 75–105. [Google Scholar] [CrossRef]
- Creed, M.; McGuirk, M.; Buckley, R.; De Brún, A.; Kilduff, M. Using Lean Six Sigma to Improve Controlled Drug Processes and Release Nursing Time. J. Nurs. Care Qual. 2019, 34, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Romano, E.; Falegnami, A.; Cagliano, A.C.; Rafele, C. Lean ICU Layout Re-Design: A Simulation-Based Approach. Informatics 2022, 9, 35. [Google Scholar] [CrossRef]
- Bhosekar, A.; Ekşioğlu, S.; Işık, T.; Allen, R. A discrete event simulation model for coordinating inventory management and material handling in hospitals. Ann. Oper. Res. 2021. [Google Scholar] [CrossRef]
- Gabriel, G.T.; Campos, A.T.; de Lima Magacho, A.; Segismondi, L.C.; Vilela, F.F.; de Queiroz, J.A.; Montevechi, J.A.B. Lean thinking by integrating with discrete event simulation and design of experiments: An emergency department expansion. PeerJ Comput. Sci. 2020, 6, e284. [Google Scholar] [CrossRef] [PubMed]
- Rahul, G.; Samanta, A.K.; Varaprasad, G. A Lean Six Sigma approach to reduce overcrowding of patients and improving the discharge process in a super-specialty hospital. In Proceedings of the 2020 International Conference on System, Computation, Automation and Networking, ICSCAN, Pondicherry, India, 3–4 July 2020. [Google Scholar]
- Ortiz-Barrios, M.; Alfaro-Saiz, J.J. An integrated approach for designing in-time and economically sustainable emergency care networks: A case study in the public sector. PLoS ONE 2020, 15, e0234984. [Google Scholar] [CrossRef]
- Al-Zain, Y.; Al-Fandi, L.; Arafeh, M.; Salim, S.; Al-Quraini, S.; Al-Yaseen, A.; Abu Taleb, D. Implementing Lean Six Sigma in a Kuwaiti private hospital. Int. J. Health Care Qual. Assur. 2019, 32, 431–446. [Google Scholar] [CrossRef]
- Lo, M.; Rutman, L.; Migita, R.; Woodward, G. Rapid electronic provider documentation design and implementation in an academic pediatric emergency department. Pediatr. Emerg. Care 2015, 31, 798–804. [Google Scholar] [CrossRef]
- Hussey, P.; De Vries, H.; Romley, J.; Wang, M.; Chen, S.; Shekelle, P.; McGlynn, E. A systematic review of health care efficiency measures: Health care efficiency. Health Serv. Res. 2009, 44, 784–805. [Google Scholar] [CrossRef]
- Mazzocato, P.; Savage, C.; Brommels, M.; Aronsson, H.; Thor, J. Lean thinking in healthcare: A realist review of the literature. Qual. Saf. Health Care 2010, 19, 376–382. [Google Scholar] [CrossRef]
- Crema, M.; Verbano, C. Lean Management to support Choosing Wisely in healthcare: The first evidence from a systematic literature review. Int. J. Qual. Health Care 2017, 29, 889–895. [Google Scholar] [CrossRef]
- Tasdemir, C.; Gazo, R. A systematic literature review for better understanding of lean driven sustainability. Sustainability 2018, 10, 2544. [Google Scholar] [CrossRef]
- Terra, J.D.R.; Berssaneti, F.T. Application of lean healthcare in hospital services: A review of the literature (2007 to 2017). Production 2018, 28, 1–14. [Google Scholar] [CrossRef][Green Version]
- Dellifraine, J.; Langabeer, J.; Nembhard, I. Assessing the evidence of six sigma and lean in the health care industry. Qual. Manag. Health Care 2010, 19, 211–225. [Google Scholar] [CrossRef] [PubMed]
- Holden, R.J. Lean thinking in emergency departments: A critical review. Ann. Emerg. Med. 2011, 57, 265–278. [Google Scholar] [CrossRef]
- Nicolay, C.; Purkayastha, S.; Greenhalgh, A.; Benn, J.; Chaturvedi, S.; Phillips, N.; Darzi, A. Systematic review of the application of quality improvement methodologies from the manufacturing industry to surgical healthcare. Br. J. Surg. 2012, 99, 324–335. [Google Scholar] [CrossRef]
- Mason, S.; Nicolay, C.; Darzi, A. The use of Lean and Six Sigma methodologies in surgery: A systematic review. Surgeon 2015, 13, 91–100. [Google Scholar] [CrossRef]
- Andersen, H.; Røvik, K.A.; Ingebrigtsen, T. Lean thinking in hospitals: Is there a cure for the absence of evidence? A systematic review of reviews. BMJ Open 2014, 4, 3505. [Google Scholar] [CrossRef]
- D’Andreamatteo, A.; Ianni, L.; Lega, F.; Sargiacomo, M. Lean in healthcare: A comprehensive review. Health Policy 2015, 119, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Costa, L.; Godinho Filho, M. Lean healthcare: Review, classification and analysis of literature. Prod. Plan. Control 2016, 27, 823–836. [Google Scholar] [CrossRef]
- Amaratunga, T.; Dobranowski, J. Systematic Review of the Application of Lean and Six Sigma Quality Improvement Methodologies in Radiology. J. Am. Coll. Radiol. 2016, 13, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Serrano, J.I.; Peimbert-García, R.E.; Cárdenas-Barrón, L.E. Discrete-event simulation modeling in healthcare: A comprehensive review. Int. J. Environ. Res. Public Health 2021, 18, 12262. [Google Scholar] [CrossRef] [PubMed]
- Fone, D.; Hollinghurst, S.; Temple, M.; Round, A.; Lester, N.; Weightman, A.; Roberts, K.; Coyle, E.; Bevan, G.; Palmer, S. Systematic review of the use and value of computer simulation modelling in population health and health care delivery. J. Public Health Med. 2003, 25, 325–335. [Google Scholar] [CrossRef]
- Brailsford, S.C.; Harper, P.R.; Pitt, M. An analysis of the academic literature on simulation and modelling in health care. J. Simul. 2009, 3, 130–140. [Google Scholar] [CrossRef]
- Jun, G.T.; Morris, Z.; Eldabi, T.; Harper, P.; Naseer, A.; Patel, B.; Clarkson, J.P. Development of modelling method selection tool for health services management: From problem structuring methods to modelling and simulation methods. BMC Health Serv. Res. 2011, 11, 108. [Google Scholar] [CrossRef]
- Salleh, S.; Thokala, P.; Brennan, A.; Hughes, R.; Booth, A. Simulation Modelling in Healthcare: An Umbrella Review of Systematic Literature Reviews. Pharmacoeconomics 2017, 35, 937–949. [Google Scholar] [CrossRef] [PubMed]
- Krishna Priya, S.; Jayakumar, V.; Suresh Kumar, S. Defect analysis and lean six sigma implementation experience in an automotive assembly line. Mater. Today Proc. 2020, 22, 948–958. [Google Scholar] [CrossRef]
- Tlapa, D.; Limon, J.; García-Alcaraz, J.L.; Baez, Y.; Sánchez, C. Six Sigma enablers in Mexican manufacturing companies: A proposed model. Ind. Manag. Data Syst. 2016, 116, 926–959. [Google Scholar] [CrossRef]
- Guleria, P.; Pathania, A.; Sharma, S.; Sá, J.C. Lean six-sigma implementation in an automobile axle manufacturing industry: A case study. Mater. Today Proc. 2021, 50, 1739–1746. [Google Scholar] [CrossRef]
- Crema, M.; Verbano, C. Simulation modelling and lean management in healthcare: First evidences and research agenda. Total Qual. Manag. Bus. Excell. 2019, 1–19. [Google Scholar] [CrossRef]
- Al-Kaf, A.; Jayaraman, R.; Demirli, K.; Simsekler, M.C.E.; Ghalib, H.; Quraini, D.; Tuzcu, M. A critical review of implementing lean and simulation to improve resource utilization and patient experience in outpatient clinics. TQM J. 2022. [Google Scholar] [CrossRef]
- Flanary, J.T.; Rocco, N.R.; Dougherty, T.; Christman, M.S. Use of Lean Six Sigma to Improve Access to Care in a Surgical Subspecialty Clinic. Mil. Med. 2020, 185, E887–E893. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.D.; Jin, X.; Chia, S.Y. Simulation based lean six sigma approach to reduce patients waiting time in an outpatient eye clinic. In Proceedings of the IEEE International Conference on Industrial Engineering and Engineering Management, Selangor, Malaysia, 9–12 December 2014; pp. 394–398. [Google Scholar]
- Garza-Reyes, J.; Villarreal, B.; Kumar, V.; Diaz-Ramirez, J. A lean-TOC approach for improving Emergency Medical Services (EMS) transport and logistics operations. Int. J. Logist. Res. Appl. 2019, 22, 253–272. [Google Scholar] [CrossRef]
- Doğan, N.Ö.; Unutulmaz, O. Lean production in healthcare: A simulation-based value stream mapping in the physical therapy and rehabilitation department of a public hospital. Total Qual. Manag. Bus. Excell. 2016, 27, 64–80. [Google Scholar] [CrossRef]
- Converso, G.; Improta, G.; Mignano, M.; Santillo, L.C. A Simulation approach for Implementing of Agile Production Logic for a Hospital Emergency Unit. Intell. Softw. Method. Tools Tech. 2015, 532, 623–634. [Google Scholar] [CrossRef]
- Haddad, M.; Zouein, P.; Salem, J.; Otayek, R. Case Study of Lean in Hospital Admissions to Inspire Culture Change. EMJ—Eng. Manag. J. 2016, 28, 209–223. [Google Scholar] [CrossRef]
- Hilton, R.; Balla, M.; Sohal, A.S. Factors critical to the success of a Six-Sigma quality program in an Australian hospital. Total Qual. Manag. Bus. Excell. 2008, 19, 887–902. [Google Scholar] [CrossRef]
- Beck, M.; Gosik, K. Redesigning an inpatient pediatric service using Lean to improve throughput efficiency. J. Hosp. Med. 2015, 10, 220–227. [Google Scholar] [CrossRef]
- Burkitt, K.; Mor, M.K.; Jain, R.; Kruszewski, M.; Mccray, E.; Moreland, M.; Muder, R.; Obrosky, D.S.; Mary, S.; Wilson, M.; et al. Toyota production system quality improvement initiative improves perioperative antibiotic therapy. Am. J. Manag. Care 2009, 15, 633–642. [Google Scholar]
- Wongkrajang, P.; Reesukumal, K.; Pratumvinit, B. Increased effectiveness of urinalysis testing via the integration of automated instrumentation, the lean management approach, and autoverification. J. Clin. Lab. Anal. 2020, 34, e23029. [Google Scholar] [CrossRef]
- Recht, M.; Block, K.T.; Chandarana, H.; Friedland, J.; Mullholland, T.; Teahan, D.; Wiggins, R. Optimization of MRI turnaround times through the use of dockable tables and innovative architectural design strategies. Am. J. Roentgenol. 2019, 212, 855–858. [Google Scholar] [CrossRef] [PubMed]
- Rutman, L.; Stone, K.; Reid, J.; Woodward, G.A.T.; Migita, R. Improving patient flow using lean methodology: An emergency medicine experience. Curr. Treat. Options Pediatr. 2015, 1, 359–371. [Google Scholar] [CrossRef]
- Ankrum, A.L.; Neogi, S.; Morckel, M.A.; Wilhite, A.W.; Li, Z.; Schaffzin, J.K. Reduced isolation room turnover time using Lean methodology. Infect. Control Hosp. Epidemiol. 2019, 40, 1151–1156. [Google Scholar] [CrossRef] [PubMed]
- Eller, A. Rapid assessment and disposition: Applying LEAN in the emergency department. J. Healthc. Qual. 2009, 31, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Vijay, S.A. Reducing and optimizing the cycle time of patients discharge process in a hospital using six sigma dmaic approach. Int. J. Qual. Res. 2014, 8, 169–182. [Google Scholar]
- Lalongo, C.; Bernardini, S. Timeliness “at a glance”: Assessing the turnaround time through the six sigma metrics. Biochem. Medica 2016, 26, 98–102. [Google Scholar] [CrossRef]
- Ortiz Barrios, M.A.; Felizzola Jiménez, H. Use of Six Sigma Methodology to Reduce Appointment Lead-Time in Obstetrics Outpatient Department. J. Med. Syst. 2016, 40, 220. [Google Scholar] [CrossRef]
- Prajapati, D.; Suman, G. Six sigma approach for neonatal jaundice patients in an Indian rural hospital—A case study. Int. J. Health Care Qual. Assur. 2019, 33, 36–51. [Google Scholar] [CrossRef]
- Boronat, F.; Budia, A.; Broseta, E.; Ruiz-Cerdá, J.L.; Vivas-Consuelo, D. Application of Lean Healthcare methodology in a urology department of a tertiary hospital as a tool for improving efficiency. Actas Urol. Esp. 2018, 42, 42–48. [Google Scholar] [CrossRef]
- Hicks, C.; Mcgovern, T.; Prior, G.; Smith, I. Applying lean principles to the design of healthcare facilities. Intern. J. Prod. Econ. 2015, 170, 677–686. [Google Scholar] [CrossRef]
- Cançado, T.O.D.B.; Cançado, F.B.; Torres, M.L.A. Lean Six Sigma and anesthesia. Braz. J. Anesthesiol. (Engl. Ed.) 2019, 69, 502–509. [Google Scholar] [CrossRef]
- Aboueljinane, L.; Frichi, Y. A simulation optimization approach to investigate resource planning and coordination mechanisms in emergency systems. Simul. Model. Pract. Theory 2022, 119, 102586. [Google Scholar] [CrossRef]
- Nikakhtar, A.; Hsiang, S.M. Incorporating the dynamics of epidemics in simulation models of healthcare systems. Simul. Model. Pract. Theory 2014, 43, 67–78. [Google Scholar] [CrossRef]
- Harrison, J.R.; Lin, Z.; Carroll, G.R.; Carley, K.M. Simulation modeling in organizational and management research. Acad. Manag. Rev. 2007, 32, 1229–1245. [Google Scholar] [CrossRef]
- Jahangirian, M.; Eldabi, T.; Naseer, A.; Stergioulas, L.K.; Young, T. Simulation in manufacturing and business: A review. Eur. J. Oper. Res. 2010, 203, 1–13. [Google Scholar] [CrossRef]
- de Paula Ferreira, W.; Armellini, F.; De Santa-Eulalia, L.A. Simulation in industry 4.0: A state-of-the-art review. Comput. Ind. Eng. 2020, 149, 106868. [Google Scholar] [CrossRef]
- Brailsford, S.C. Tutorial: Advances and challenges in healthcare simulation modeling. In Proceedings of the 2007 Winter Simulation Conference, Washington, DC, USA, 9–12 December 2007; pp. 1436–1448. [Google Scholar]
- Ben-Tovim, D.; Filar, J.; Hakendorf, P.; Qin, S.; Thompson, C.; Ward, D. Hospital Event Simulation Model: Arrivals to Discharge–Design, development and application. Simul. Model. Pract. Theory 2016, 68, 80–94. [Google Scholar] [CrossRef]
- Rojas, E.; Munoz-Gama, J.; Sepúlveda, M.; Capurro, D. Process mining in healthcare: A literature review. J. Biomed. Inform. 2016, 61, 224–236. [Google Scholar] [CrossRef]
- Improta, G.; Guizzi, G.; Ricciardi, C.; Giordano, V.; Ponsiglione, A.M.; Converso, G.; Triassi, M. Agile six sigma in healthcare: Case study at santobono pediatric hospital. Int. J. Environ. Res. Public Health 2020, 17, 1052. [Google Scholar] [CrossRef]
- Montesarchio, V.; Grimaldi, A.M.; Fox, B.A.; Rea, A.; Marincola, F.M.; Ascierto, P.A. Lean oncology: A new model for oncologists. J. Transl. Med. 2012, 10, 74. [Google Scholar] [CrossRef]
- Institute of Medicine; Yong, P.L.; Saunders, R.S.; Olsen, L.; Institute of Medicine (U.S.). Roundtable on Value & Science-Driven Health Care. In The Healthcare Imperative: Lowering Costs and Improving Outcomes; Yong, P., Saunders, R., Olsen, L., Eds.; National Academies Press: Washington, DC, USA, 2010; ISBN 9780309144339. [Google Scholar]
- Damle, A.; Andrew, N.; Kaur, S.; Orquiola, A.; Alavi, K.; Steele, S.R.; Maykel, J. Elimination of waste: Creation of a successful Lean colonoscopy program at an academic medical center. Surg. Endosc. 2016, 30, 3071–3076. [Google Scholar] [CrossRef]
- White, B.A.; Yun, B.J.; Lev, M.H.; Raja, A.S. Applying Systems Engineering Reduces Radiology Transport Cycle Times in the Emergency Department. West. J. Emerg. Med. 2017, 18, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Weaver, A.; Greeno, C.G.; Goughler, D.H.; Kathleen Yarzebinski, M.; Tina Zimmerman, B.; Carol Anderson, L. The impact of system level factors on treatment timeliness: Utilizing the toyota production system to implement direct intake scheduling in a semi-rural community mental health clinic. J. Behav. Health Serv. Res. 2013, 40, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Umut, B.; Alipour, P.; Sarvari, P.A. Applying lean tools in the clinical laboratory to reduce turnaround time for blood test results. Int. J. Adv. Sci. Eng. Technol. 2016, 4, 1–6. [Google Scholar]
- Chan, H.; Lo, S.; Lee, L.; Lo, W.; Yu, W.; Wu, Y.; Ho, S.; Yeung, R.; Chan, J. Lean techniques for the improvement of patients’ flow in emergency department. World J. Emerg. Med. 2014, 5, 24–28. [Google Scholar] [CrossRef][Green Version]
- Westwood, N.; James-Moore, M.; Cooke, M.; Wiseman, N.; Westwood, N.; James-Moore, M.; Cooke, M. Going Lean in the NHS. Available online: https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Going-Lean-in-the-NHS.pdf (accessed on 20 January 2020).
- Bercaw, R. Taking Improvement from the Assembly Line to Healthcare: The Application of Lean within the Healthcare Industry, 1st ed.; CRC Press: Boca Raton, FL, USA, 2011. [Google Scholar]
- Cohen, R.I. Lean Methodology in Health Care. Chest 2018, 154, 1448–1454. [Google Scholar] [CrossRef] [PubMed]
- Celano, G.; Costa, A.; Fichera, S.; Tringali, G. Linking Six Sigma to simulation: A new roadmap to improve the quality of patient care. Int. J. Health Care Qual. Assur. 2012, 25, 254–273. [Google Scholar] [CrossRef]
- Frankel, H.L.; Crede, W.B.; Topal, J.E.; Roumanis, S.A.; Devlin, M.W.; Foley, A.B. Use of corporate six sigma performance-improvement strategies to reduce incidence of catheter-related bloodstream infections in a surgical ICU. J. Am. Coll. Surg. 2005, 201, 349–358. [Google Scholar] [CrossRef]
- Ren, X.-L.L.; Chai, Z.-Y.Y.; Qi, F.; Zheng, L.-Z.Z.; Zeng, B.-J.J.; Hu, H.-M.M.; Ren, X.-L.L.; Zeng, B.-J.J.; Zheng, L.-Z.Z.; Qi, F. Applying Lean Six Sigma methodology to reduce cesarean section rate. J. Eval. Clin. Pract. 2016, 23, 562–566. [Google Scholar] [CrossRef]
- Adams, R.; Warner, P.; Hubbard, B.; Goulding, T. Decreasing Turnaround Time between General Surgery Cases: A Six Sigma Initiative. J. Nurs. Adm. 2004, 34, 140–148. [Google Scholar] [CrossRef]
- Cochrane Effective Practice and Organisation of Care (EPOC). What Outcomes Should Be Reported in Cochrane Effective Practice and Organisation of Care (EPOC) Reviews? Available online: http://epoc.cochrane.org/resources/epoc-resources-review-authors (accessed on 15 November 2018).
- Toledo, A.; Carroll, T.; Arnold, E.; Tulu, Z.; Caffey, T.; Kearns, L.; Gerber, D. Reducing liver transplant length of stay: A lean six sigma approach. Prog. Transplant. 2013, 23, 350–364. [Google Scholar] [CrossRef] [PubMed]
- Trzeciak, S.; Mercincavage, M.; Angelini, C.; Cogliano, W.; Damuth, E.; Roberts, B.W.; Zanotti, S.; Mazzarelli, A.J. Lean Six Sigma to Reduce Intensive Care Unit Length of Stay and Costs in Prolonged Mechanical Ventilation. J. Healthc. Qual. 2018, 40, 36–43. [Google Scholar] [CrossRef]
- Brunsman, A. Using lean methodology to optimize time to antibiotic administration in patients with sepsis. Am. J. Health Pharm. 2018, 75, S13–S23. [Google Scholar] [CrossRef]
- Hitti, E.A.; El-Eid, G.R.; Tamim, H.; Saleh, R.; Saliba, M.; Naffaa, L. Improving Emergency Department radiology transportation time: A successful implementation of lean methodology. BMC Health Serv. Res. 2017, 17, 625. [Google Scholar] [CrossRef]
- Murrell, K.L.; Offerman, S.R.; Kauffman, M.B. Applying Lean: Implementation of a Rapid Triage and Treatment System. West. J. Emerg. Med. 2011, 12, 184–191. [Google Scholar] [PubMed]
- Artenstein, A.W.; Rathlev, N.K.; Neal, D.; Townsend, V.; Vemula, M.; Goldlust, S.; Schmidt, J.; Visintainer, P.; Albert, M.; Alli, G.; et al. Decreasing Emergency Department Walkout Rate and Boarding Hours by Improving Inpatient Length of Stay. West. J. Emerg. Med. 2017, 18, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Molla, M.; Warren, D.S.; Stewart, S.L.; Stocking, J.; Johl, H.; Sinigayan, V. A Lean Six Sigma Quality Improvement Project Improves Timeliness of Discharge from the Hospital. Jt. Comm. J. Qual. Patient Saf. 2018, 44, 401–412. [Google Scholar] [CrossRef]
- King, D.L.; Ben-Tovim, D.I.; Bassham, J. Redesigning emergency department patient flows: Application of Lean Thinking to health care. Emerg. Med. Australas. 2006, 18, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Beck, M.; Okerblom, D.; Kumar, A.; Bandyopadhyay, S.; Scalzi, L. Lean intervention improves patient discharge times, improves emergency department throughput and reduces congestion. Hosp. Pract. 2016, 44, 252–259. [Google Scholar] [CrossRef]
- Castaldi, M.; Sugano, D.; Kreps, K.; Cassidy, A.; Kaban, J. Lean philosophy and the public hospital. Perioper. Care Oper. Room Manag. 2016, 3, 25–28. [Google Scholar] [CrossRef]
- Hassanain, M.; Zamakhshary, M.; Farhat, G.; Al-Badr, A. Use of Lean methodology to improve operating room efficiency in hospitals across the Kingdom of Saudi Arabia. Int. J. Health Plann. Manag. 2017, 32, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Bender, J.; Nicolescu, T.; Hollingsworth, S.B.; Murer, K.; Wallace, K.R.; Ertl, W.J. Improving operating room efficiency via an interprofessional approach. Am. J. Surg. 2015, 209, 447–450. [Google Scholar] [CrossRef] [PubMed]
- Nicosia, F.M.; Park, L.G.; Gray, C.P.; Yakir, M.J.; Hung, D.Y. Nurses’ Perspectives on Lean Redesigns to Patient Flow and Inpatient Discharge Process Efficiency. Glob. Qual. Nurs. Res. 2018, 5, 2333393618810658. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.A.; Clarke, M.; Devereaux, P.J.J.; Kleijnen, J.; Moher, D.; et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 89. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions, 5th ed.; Higgins, J., Green, S., Eds.; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef]
- Tlapa, D.; Zepeda-Lugo, C.A.; Tortorella, G.L.; Baez-Lopez, Y.A.; Limon-Romero, J.; Alvarado-Iniesta, A.; Rodriguez-Borbon, M.I. Effects of Lean Healthcare on Patient Flow: A Systematic Review. Value Health 2020, 23, 260–273. [Google Scholar] [CrossRef]
- Zepeda-Lugo, C.; Tlapa, D.; Baez-Lopez, Y.; Limon-Romero, J.; Ontiveros, S.; Perez-Sanchez, A.; Tortorella, G. Assessing the impact of lean healthcare on inpatient care: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 5609. [Google Scholar] [CrossRef]
- Moraros, J.; Lemstra, M.; Nwankwo, C. Lean interventions in healthcare: Do they actually work? A systematic literature review. Int. J. Qual. Health Care 2016, 28, 150–165. [Google Scholar] [CrossRef]
- Centers for Medicare & Medicaid Services HCAHPS Survey. Available online: http://www.hcahpsonline.org/files/2017_SurveyInstruments_English_Mail.pdf (accessed on 16 September 2019).
- Sterne, J.A.C.; Higgins, J.P.T.; Elbers, R.G.; Reeves, B.C.; Development group for ROBINS-I. Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I): Detailed Guidance, Updated 12 October 2016. Available online: https://sites.google.com/site/riskofbiastool/welcome/home/current-version-of-robins-i/robins-i-detailed-guidance-2016?authuser=0 (accessed on 20 January 2022).
- Sterne, J.; Hernán, M.; Reeves, B.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.; Ansari, M.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Indrawati, S.; Madarja, E.R. Lean Healthcare Improvement Model Using Simulation-Based Lean Six-Sigma and TRIZ. Math. Model. Eng. Probl. 2022, 9, 849–855. [Google Scholar] [CrossRef]
- Lokesh, K.; Samanta, A.K.; Varaprasad, G. Reducing the turnaround time of laboratory samples by using Lean Six Sigma methodology in a tertiary-care hospital in India. In Proceedings of the 2020 International Conference on System, Computation, Automation and Networking, ICSCAN, Pondicherry, India, 3–4 July 2020. [Google Scholar]
- Agnetis, A.; Bianciardi, C.; Iasparra, N. Integrating lean thinking and mathematical optimization: A case study in appointment scheduling of hematological treatments. Oper. Res. Perspect. 2019, 6, 100110. [Google Scholar] [CrossRef]
- Ortíz-Barrios, M.; Escorcia-Caballero, J.; Sánchez-Sánchez, F.; De Felice, F.; Petrillo, A. Efficiency Analysis of Integrated Public Hospital Networks in Outpatient Internal Medicine. J. Med. Syst. 2017, 41, 163. [Google Scholar] [CrossRef]
- Salam, M.A.; Khan, S.A. Value creation through lean management: A case study of healthcare service operations. Int. J. Serv. Oper. Manag. 2016, 25, 275–293. [Google Scholar] [CrossRef]
- Bhat, S.; Gijo, E.V.; Jnanesh, N.A.A. Productivity and performance improvement in the medical records department of a hospital An application of Lean Six Sigma. Int. J. Product. Perform. Manag. 2016, 65, 98–125. [Google Scholar] [CrossRef]
- Hirisatja, T.; Lila, B.; Chantrasa, R. Healthcare Operations Improvement with an Integration of Discrete-Event Simulation and Lean Thinking. In Proceedings of the International conference on Innovative Engineering Technologies (ICIET’2014), Bangkok, Thailand, 28–29 December 2014; pp. 85–91. [Google Scholar]
- Bhat, S.; Jnanesh, N.A. Application of Lean Six Sigma methodology to reduce the cycle time of out-patient department service in a rural hospital. Int. J. Healthc. Technol. Manag. 2014, 14, 222–237. [Google Scholar] [CrossRef]
- Kim, C.S.; Hayman, J.A.; Billi, J.E.; Lash, K.; Lawrence, T.S. The application of lean thinking to the care of patients with bone and brain metastasis with radiation therapy. J. Oncol. Pract. 2007, 3, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Nelson-Peterson, D.L.; Leppa, C.J. Creating an environment for caring using lean principles of the Virginia Mason production system. J. Nurs. Adm. 2007, 37, 287–294. [Google Scholar] [CrossRef]
- Ajdari, A.; Boyle, L.N.; Kannan, N.; Wang, J.; Rivara, F.P.; Vavilala, M.S. Simulation of the Emergency Department Care Process for Pediatric Traumatic Brain Injury. J. Healthc. Qual. 2018, 40, 110–118. [Google Scholar] [CrossRef]
- Joshi, V.; Lim, C.; Teng, S.G. Simulation Study: Improvement for Non-Urgent Patient Processes in the Emergency Department. EMJ—Eng. Manag. J. 2016, 28, 145–157. [Google Scholar] [CrossRef]
- Tejedor-Panchón, F.; Montero-Pérez, F.J.; Tejedor-Fernández, M.; Jiménez-Murillo, L.; Calderón De La Barca-Gázquez, J.M.; Quero-Espinosa, F.B. Improvement in hospital emergency department processes with application of lean methods. Emergencias 2014, 26, 84–93. [Google Scholar]
- Rosmulder, R.W. Improving Healthcare Delivery with Lean Thinking: Action Research in an Emergency Department; University of Twente: Enschede, The Netherlands, 2011. [Google Scholar]
- Mandahawi, N.; Al-Shihabi, S.; Abdallah, A.A.; Alfarah, Y.M. Reducing waiting time at an emergency department using design for Six Sigma and discrete event simulation. Int. J. Six Sigma Compet. Advant. 2010, 6, 91–104. [Google Scholar] [CrossRef]
- Bhat, S.; Gijo, E.V.; Jnanesh, N.A. Application of Lean Six Sigma methodology in the registration process of a hospital. Int. J. Product. Perform. Manag. 2014, 63, 613–643. [Google Scholar] [CrossRef]
- Yu, Q.; Yang, K. Hospital registration waiting time reduction through process redesign. Int. J. Six Sigma Compet. Advant. 2008, 4, 240. [Google Scholar] [CrossRef]
- Khurma, N.; Bacioiu, G.M.; Pasek, Z.J. Simulation-based verification of lean improvement for emergency room process. In Proceedings of the 2008 Winter Simulation Conference, Miami, FL, USA, 7–10 December 2008; pp. 1490–1499. [Google Scholar] [CrossRef]
- Amati, M.; Valnegri, A.; Bressan, A.; La Regina, D.; Tassone, C.; Lo Piccolo, A.; Mongelli, F.; Saporito, A. Reducing Changeover Time Between Surgeries Through Lean Thinking: An Action Research Project. Front. Med. 2022, 9, 822964. [Google Scholar] [CrossRef]
- Demir, E.; Southern, D.; Rashid, S.; Lebcir, R. A discrete event simulation model to evaluate the treatment pathways of patients with cataract in the United Kingdom. BMC Health Serv. Res. 2018, 18, 933. [Google Scholar] [CrossRef]
- Barnabè, F.; Giorgino, M.C.; Guercini, J.; Bianciardi, C.; Mezzatesta, V. Management simulations for Lean healthcare: Exploiting the potentials of role-playing. J. Health Organ. Manag. 2018, 32, 298–320. [Google Scholar] [CrossRef]
- Po, J.; Rundall, T.G.; Shortell, S.M.; Blodgett, J.C. Lean Management and U.S. Public Hospital Performance: Results from a National Survey. J. Healthc. Manag. 2019, 64, 363–379. [Google Scholar] [CrossRef]
- Shortell, S.; Blodgett, J.; Rundall, T.; Kralovec, P. Use of Lean and Related Transformational Performance Improvement Systems in Hospitals in the United States: Results From a National Survey. Jt. Comm. J. Qual. Patient Saf. 2018, 44, 574–582. [Google Scholar] [CrossRef]
- Kaasalainen, K.; Kalmari, J.; Ruohonen, T. Developing and testing a discrete event simulation model to evaluate budget impacts of diabetes prevention programs. J. Biomed. Inform. 2020, 111, 103577. [Google Scholar] [CrossRef] [PubMed]
- Mansur dos Reis, M.E.D.; de Abreu, M.F.; Neto, O.D.O.B.; Viera, L.E.V.; Torres, L.F.; Calado, R.D. DMAIC in improving patient care processes: Challenges and facilitators in context of healthcare. IFAC-PapersOnLine 2022, 55, 215–220. [Google Scholar] [CrossRef]
- Bashar, A.; Hasin, A.A.; Adnan, Z.H. Impact of lean manufacturing: Evidence from apparel industry in Bangladesh. Int. J. Lean Six Sigma 2021, 12, 923–943. [Google Scholar] [CrossRef]
- Becich, M.J.; Gilbertson, J.R.; Gupta, D.; Patel, A.; Grzybicki, D.M.; Raab, S.S. Pathology and patient safety: The critical role of pathology informatics in error reduction and quality initiatives. Clin. Lab. Med. 2004, 24, 913–943. [Google Scholar] [CrossRef] [PubMed]
- Aleem, S. Translating 10 lessons from lean six sigma project in paper-based training site to electronic health record-based primary care practice: Challenges and opportunities. Qual. Manag. Health Care 2013, 22, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Eitel, D.R.; Rudkin, S.E.; Malvehy, M.A.; Killeen, J.P.; Pines, J.M. Improving Service Quality by Understanding Emergency Department Flow: A White Paper and Position Statement Prepared For the American Academy of Emergency Medicine. J. Emerg. Med. 2010, 38, 70–79. [Google Scholar] [CrossRef]
- Baysan, S.; Kabadurmus, O.; Cevikcan, E.; Satoglu, S.I.; Durmusoglu, M.B. A simulation-based methodology for the analysis of the effect of lean tools on energy efficiency: An application in power distribution industry. J. Clean. Prod. 2019, 211, 895–908. [Google Scholar] [CrossRef]
- Liu, Q.; Yang, H. An improved value stream mapping to prioritize lean optimization scenarios using simulation and multiple-attribute decision-making method. IEEE Access 2020, 8, 204914–204930. [Google Scholar] [CrossRef]
- Gunal, M.M. A guide for building hospital simulation models. Health Syst. 2012, 1, 17–25. [Google Scholar] [CrossRef]
- Keshtkar, L.; Rashwan, W.; Abo-Hamad, W.; Arisha, A. A hybrid system dynamics, discrete event simulation and data envelopment analysis to investigate boarding patients in acute hospitals. Oper. Res. Health Care 2020, 26, 100266. [Google Scholar] [CrossRef]
- Allen, T. Decision Support and Voting Systems Case Study. In Introduction to Discrete EVENT Simulation and Agent-Based Modeling: Voting Systems, Health Care, Military, and Manufacturing; Springer: London, UK, 2011; pp. 87–110. [Google Scholar] [CrossRef]
- Silverman, B.G.; Hanrahan, N.; Bharathy, G.; Gordon, K.; Johnson, D. A systems approach to healthcare: Agent-based modeling, community mental health, and population well-being. Artif. Intell. Med. 2015, 63, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Metcalf, S.S.; Palmer, H.D.; Northridge, M.E. Developing an agent-based model of oral healthcare utilization by Chinese Americans in New York City. Health Place 2022, 73, 102740. [Google Scholar] [CrossRef] [PubMed]
- Aissaoui, N.O.; Khlif, H.H.; Zeghal, F.M. Integrated proactive surgery scheduling in private healthcare facilities. Comput. Ind. Eng. 2020, 148, 106686. [Google Scholar] [CrossRef]
- Fum, W.K.S.; Wong, J.H.D.; Tan, L.K. Monte Carlo-based patient internal dosimetry in fluoroscopy-guided interventional procedures: A review. Phys. Medica 2021, 84, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Nonthaleerak, P.; Hendry, L.C. Six sigma: Literature review and key future research areas. Int. J. Six Sigma Compet. Advant. 2005, 2, 105–161. [Google Scholar] [CrossRef]
- Silvester, K.; Lendon, R.; Bevan, H.; Steyn, R.; Walley, P.; Lee, M. Reducing waiting times in the NHS: Is lack of capacity the problem? Clin. Manag. 2004, 12, 105–111. [Google Scholar]
- Li, J.; Carayon, P. Health Care 4.0: A vision for smart and connected health care. IISE Trans. Healthc. Syst. Eng. 2021, 11, 171–180. [Google Scholar] [CrossRef]
- Aggarwal, A.; Aeran, H.; Rathee, M. Quality management in healthcare: The pivotal desideratum. J. Oral Biol. Craniofacial Res. 2019, 9, 180–182. [Google Scholar] [CrossRef]
- Poksinska, B.B.; Fialkowska-Filipek, M.; Engström, J. Does Lean healthcare improve patient satisfaction? A mixed-method investigation into primary care. BMJ Qual. Saf. 2017, 26, 95–103. [Google Scholar] [CrossRef]
- Yang, T.; Wang, T.K.; Li, V.C.; Su, C.-L. The Optimization of Total Laboratory Automation by Simulation of a Pull-Strategy. J. Med. Syst. 2015, 39, 162. [Google Scholar] [CrossRef]
- Kane, M.; Chui, K.; Rimicci, J.; Callagy, P.; Hereford, J.; Shen, S.; Norris, R.; Pickham, D. Lean manufacturing improves emergency department throughput and patient satisfaction. J. Nurs. Adm. 2015, 45, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Singer, S.J. Value of a value culture survey for improving healthcare quality. BMJ Qual. Saf. 2022, 31, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Zegers, M.; Veenstra, G.L.; Gerritsen, G.; Verhage, R.; van der Hoeven, H.J.G.; Welker, G.A. Perceived Burden Due to Registrations for Quality Monitoring and Improvement in Hospitals: A Mixed Methods Study. Int. J. Health Policy Manag. 2022, 11, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Rees, G.H.; Gauld, R. Can lean contribute to work intensification in healthcare? J. Health Organ. Manag. 2017, 31, 369–384. [Google Scholar] [CrossRef]
- Morgan, M.W.; Salzman, J.G.; Le Fevere, R.C.; Thomas, A.J.; Isenberger, K.M.; LeFevere, R.; Thomas, A.J.; Isenberger, K.M. Demographic, operational, and healthcare utilization factors associated with emergency department patient satisfaction. West. J. Emerg. Med. 2015, 16, 516–526. [Google Scholar] [CrossRef]
- Joosten, T.; Bongers, I.; Janssen, R. Application of lean thinking to health care: Issues and observations. Int. J. Qual. Health Care 2009, 21, 341–347. [Google Scholar] [CrossRef]
- Elamir, H. Improving patient flow through applying lean concepts to emergency department. Leadersh. Health Serv. 2018, 31, 293–309. [Google Scholar] [CrossRef]
- Johnson, A.E.; Winner, L.; Simmons, T.; Eid, S.M.; Hody, R.; Sampedro, A.; Augustine, S.; Sylvester, C.; Parakh, K. Using Innovative Methodologies From Technology and Manufacturing Companies to Reduce Heart Failure Readmissions. Am. J. Med. Qual. 2016, 31, 272–278. [Google Scholar] [CrossRef]
- Montella, E.; Di Cicco, M.V.; Ferraro, A.; Centobelli, P.; Raiola, E.; Triassi, M.; Improta, G. The application of Lean Six Sigma methodology to reduce the risk of healthcare–associated infections in surgery departments. J. Eval. Clin. Pract. 2017, 23, 530–539. [Google Scholar] [CrossRef]
- Chen, X.; Li, X.; Liu, Y.; Yao, G.; Yang, J.; Li, J.; Qiu, F. Preventing dispensing errors through the utilization of lean six sigma and failure model and effect analysis: A prospective exploratory study in China. J. Eval. Clin. Pract. 2021, 27, 1134–1142. [Google Scholar] [CrossRef]
- Sanders, J.; Karr, T. Improving ED specimen TAT using Lean Six Sigma. Int. J. Health Care Qual. Assur. 2015, 28, 428–440. [Google Scholar] [CrossRef] [PubMed]
- Raja, R.; Mukherjee, I.; Sarkar, B.K.; Ali, S. A Systematic Review of Healthcare Big Data. Sci. Program. 2020, 2020, 5471849. [Google Scholar] [CrossRef]
- Gupta, S.; Modgil, S.; Gunasekaran, A. Big data in lean six sigma: A review and further research directions. Int. J. Prod. Res. 2020, 58, 947–969. [Google Scholar] [CrossRef]
- Bhat, S.; Gijo, E.V.; Antony, J.; Cross, J. Strategies for successful deployment and sustainment of Lean Six Sigma in healthcare sector in India: A multi-level perspective. TQM J. 2022. ahead of print. [Google Scholar] [CrossRef]
- Santos, C.H.D.; de Queiroz, J.A.; Leal, F.; Montevechi, J.A.B. Use of simulation in the industry 4.0 context: Creation of a Digital Twin to optimise decision making on non-automated process. J. Simul. 2020, 16, 284–297. [Google Scholar] [CrossRef]
- Rosen, R.; Von Wichert, G.; Lo, G.; Bettenhausen, K.D. About the importance of autonomy and digital twins for the future of manufacturing. IFAC-PapersOnLine 2015, 28, 567–572. [Google Scholar] [CrossRef]
- Rodič, B. Industry 4.0 and the New Simulation Modelling Paradigm. Organizacija 2017, 50, 193–207. [Google Scholar] [CrossRef]
- Reijula, J.; Tommelein, I.D. Lean hospitals: A new challenge for facility designers. Intell. Build. Int. 2012, 4, 126–143. [Google Scholar] [CrossRef]
- Young, T. An agenda for healthcare and information simulation. Health Care Manag. Sci. 2005, 8, 189–196. [Google Scholar] [CrossRef]
- Ali, S.M.; Hossen, M.A.; Mahtab, Z.; Kabir, G.; Paul, S.K.; Adnan, Z.H. Barriers to lean six sigma implementation in the supply chain: An ISM model. Comput. Ind. Eng. 2020, 149, 106843. [Google Scholar] [CrossRef]
- Ilangakoon, T.S.; Weerabahu, S.K.; Samaranayake, P.; Wickramarachchi, R. Adoption of Industry 4.0 and lean concepts in hospitals for healthcare operational performance improvement. Int. J. Product. Perform. Manag. 2022, 71, 2188–2213. [Google Scholar] [CrossRef]
- Fournier, P.L.; Jobin, M.H.; Lapointe, L.; Bahl, L. Lean implementation in healthcare: Offsetting Physicians’ resistance to change. Prod. Plan. Control 2021, 1–13. [Google Scholar] [CrossRef]
- Leite, H.; Williams, S.; Radnor, Z.; Bateman, N. Emergent barriers to the lean healthcare journey: Baronies, tribalism and scepticism. Prod. Plan. Control 2022, 1–18. [Google Scholar] [CrossRef]
- Akmal, A.; Foote, J.; Podgorodnichenko, N.; Greatbanks, R.; Gauld, R. Understanding resistance in lean implementation in healthcare environments: An institutional logics perspective. Prod. Plan. Control 2022, 33, 356–370. [Google Scholar] [CrossRef]
- Macias-Aguayo, J.; Garcia-Castro, L.; Barcia, K.F.; McFarlane, D.; Abad-Moran, J. Industry 4.0 and Lean Six Sigma Integration: A Systematic Review of Barriers and Enablers. Appl. Sci. 2022, 12, 11321. [Google Scholar] [CrossRef]


| First Author, Year; Country | Setting; Study Design; n; Time Frame | Main Intervention | Outcomes | Summary of Findings | Software; Simulation or Implementation |
|---|---|---|---|---|---|
| Indrawati, 2022; Indonesia [134] | Clinic; case study; n = 96 | Lean and DES | Mean Lead time | Reduced from 6398 s to 3084 s | FlexSim; Simulation |
| Lokesh, 2020; India [135] | Pediatric emergency; case study; n = 44; 1 mo | LSS and DES | Mean TAT of tests | Reduced from 69 min to 36 min | Arena; Simulation |
| Noto, 2020; Italy [27] | Ambulatory care; case study; pre-post; n = 5 | Lean and SD | Mean time of the process | Reduced from 92 min to 65 min | Not Specified; Simulation |
| Agnetis, 2019; Italy [136] | Hematological center; case study; n = 49 | Lean and DES | Mean patient lead time | Reduced from 1165.8 min to 747.4 min | Arena; Simulation |
| Garza-Reyes, 2019; UK [67] | Ambulance service; case study; n = 850 ambulances; 1 mo | Lean, simulation (not specified), internet-based technologies, and GPS tracking devices. | Mean ambulance cycle time | Reduced from 124.9 min to 75.8 min | ProModel; Simulation |
| Ortiz, 2017; Colombia [137] | Internal medicine; case study; pre-post | Lean and DES | Mean lead time | Reduced from 9.9 days to 7.6 days | Arena; Simulation |
| Salam, 2016; Thailand [138] | Medical center; case study; pre-post | Lean and DES | Mean cycle time | Reduced from 5.8 h to 3.8 h | I-Grafx; Simulation |
| Haddad, 2016; Lebanon [70] | Radiology department; case study; n = 6 | Lean and DES | Mean total patient time in the system | Reduced from 98.1 min to 15.9 min | Arena; Simulation |
| Bhat, 2016; India [139] | Medical record department; case study; pre-post; n = 100; 2 mo | LSS and simulation (not specified) | Mean TAT | Reduced from 19 min to 8 min | Arena; Simulation |
| Hirisatja, 2014; Thailand [140] | Out-patient surgery department; case study | Lean and DES | Mean TAT with appointment | Reduced from 144.2 min to 114.5 min | Arena; Simulation |
| Mean TAT without appointment | Reduced from 178.2 min to 152.5 min | ||||
| Bhat, 2014a; India [141] | Out-patient department, case study; n = 56; 2 mo | LSS and DES | Mean cycle time and Standard Deviation | Reduced from 4.27 min to 1.5 min | Arena; Implementation |
| Kim, 2007; USA [142] | Radiation oncology department; case study; n = 6 mo | Lean and Simulation (not specified) | Mean Process time | Reduced from 290 min to 225 min | Not Specified; Simulation |
| Nelson-Peterson, 2007; USA [143] | Telemetry unit on hospital; time-series, pre-post; n = 8; 5 mo | Lean and Simulation (not specified) | Mean Registered nurse lead time | Reduced from 240 min to 126 min | Not Specified; Simulation |
| First Author, Year; Country | Setting; Study Design; n; Time Frame | Main Intervention | Outcomes | Summary of Findings | Software; Simulation or Implementation |
|---|---|---|---|---|---|
| Romano, 2022; Italy [35] | ICU; case study; n = 112 | Lean and DES | Mean LOS | Reduced from 8.5 days/patient to 7.5 days/patient | PowerSim; simulation |
| Gabriel 2020; Brazil [37] | ED; case study; 12 mo | LSS and DES | Mean LOS | Reduced from 2213.7 min to 461.2 min | FlexSim; simulation |
| Ajdari 2017; USA [144] | ED; case study; pre-post; n = 56 | Lean and DES | Mean LOS | Reduced from 69.75 min to 57.43 min | Simio; simulation |
| Dogan, 2016; Turkey [68] | Rehabilitation at public hospital; case study; n = 625,168 | Lean and SD | Mean LOS | Reduced from 13,790 min to 11,558 min | Arena; simulation |
| Joshi, 2016; USA [145] | ED; case study; n = 200 | Lean and DES | Mean LOS: patients stay for test results and prescription | Reduced from 128 min to 119 min | Arena; simulation |
| Mean LOS: patients need only prescription | Reduced from 59 min to 42 min | ||||
| Lee, 2015; USA [7] | Emergency care center; case study; n = 18,726; 9 mo | Lean, ABS, machine learning, simulation, optimization | Mean overall LOS | Reduced from 10.5 h to 7.1 h | Real Opt; simulation |
| Lo, 2015; USA [41] | Pediatric ED; pre-post; 7 mo | Lean, DES, real-time voice recognition system, simulation, and electronic charting | Mean discharged patients LOS | Increased from 161 min to 168 min | Dragon; implementation |
| Mean LOS | No change (270 min) | ||||
| Converso, 2015; Italy [69] | ED; case study | Lean and SD | Mean residence time | Reduced from 6 days to 5 days | PowerSim; simulation |
| Rutman, 2015; [76] USA | ED; pre-post; n = 98; 7 mo | Lean, and in situ simulation and EMR | Mean LOS in ED | Reduced by 30 min | Not apply (in situ); simulation |
| Tejedor-Panchon, 2014; Spain [146] | ED; case study; pre-post; n = 256,628; 36 mo | Lean, DES, and digital technology in X-ray | Mean LOS in ED (time spent in the examination area) | Reduced from 80.4 min to 61.6 min (p < 0.001) | I-Grafx, implementation |
| Mean LOS in TC | Reduced from 137.8 min to 123.8 min (p < 0.05) | ||||
| Mean LOS in MSC | Reduced from 219.7 min to 209.3 min (p = 0.108) | ||||
| Rosmulder, 2011; The Netherlands [147] | ED; case study; n = 704, 24 mo | Lean and DES | Mean LOS | Reduced from 97 min to 83 min (p = 0.05) | Tecnomatix; simulation |
| Mandahawi, 2010; Jordan [148] | ED; case study; n = 163 | SS and DES | Mean LOS | Reduced from 84.49 min to 55.50 min | ProModel; simulation |
| First Author, Year; Country | Setting; Study Design; n; Time Frame | Main Intervention | Outcomes | Summary of Findings | Software; Simulation or Implementation |
|---|---|---|---|---|---|
| Noto, 2020; Italy [27] | Ambulatory care; case study; pre-post; n = 5 | Lean and SD | Mean waiting time for patients to be registered | Reduced from 8 min to 1 min | Not specified; simulation |
| Rahul 2020; India [38] | ED; case study; n = 190; 1 mo | LSS and DES | Mean waiting time | Reduced 76 min to 22 min | Arena; simulation |
| Ortiz-Barrios, 2020; Colombia [39] | ED; case study; n = 16,741; 15 mo | Lean, DES and virtual modelling | Mean waiting time | Reduced from 201.6 min to 103.1 min | Minitab; simulation |
| Bhosekar, 2021; USA [36] | OR, case study, 24 mo | Lean (just-in-time) and DES | Mean delay in surgery | Reduced from 31.2 min to 1.4 min | Arena; simulation |
| Al-Zain, 2018; Kuwait [40] | Obstetrics and gynecology; case study; n = 168 | LSS and DES | Mean waiting time for appointment patients | Reduced from 59.8 min to 19.8 min | Arena; simulation |
| Baril, 2016; [9] Canada | Hematology–oncology clinic; case study; 10 mo, 2 mo of follow up | Lean, DES, and business game-virtual environment | Mean patient waiting time before treatment | Reduced from 61 min to 16 min | Arena; simulation |
| Joshi, 2016; USA [145] | ED; case study; n = 200 | Lean and DES | Mean waiting Time | Reduced from 31 min to 8.3 min | Arena; simulation |
| Converso, 2015; Italy [69] | ED; case study | Lean and SD | Mean waiting for the surgery (max) | Reduced from 450 min to 354 min | PowerSim; simulation |
| Rutman, 2015; [76] USA | ED; case study; pre-post; n = 98; 7 mo | Lean, in situ simulation, and electronic medical records | Median time to see a provider | Reduced from 43 min to 7 min | Not apply (in situ); simulation |
| Percentage of patients seen within 30 min | Increased from 33% to 93% | ||||
| Lin, 2014; Singapore [66] | Eye clinic; case study | LSS and DES | Mean patient waiting time | Reduced from 135.6 min to 103.5 min | FlexSim; simulation |
| Tejedor-Panchon, 2014 Spain [146] | ED; case study; pre-post study; n = 256,628; 36 mo | Lean, DES, and digital technology in X-ray | Mean wait time to see a physician | Reduced from 58 min to 49.1 min (p < 0.001) | I-Grafx; implementation |
| Hirisatja, 2014; Thailand [140] | Out-patient surgery department; case study | Lean and DES | Mean waiting time with appointment | Reduced from 89.2 min to 74.7 min | Arena; simulation |
| Mean waiting time without appointment | Reduced from 120.5 min to 106.1 min | ||||
| Bhat, 2014b; India [149] | Health information department; case study; n = 224 | LSS and DES | Mean waiting time in the system | Reduced from 21.1 min to 1.1 min | Arena; simulation |
| Bhat 2014a; India [141] | Out-patient department; case study; n = 56; 2 mo | LSS and DES | Mean waiting time in the system | Reduced from 32 min to 1 min | Arena, implementation |
| Mandahawi, 2010; Jordan [148] | ED; case study; n = 163 | SS and DES | Mean patient waiting time | Reduced from 33.2 min to 12.9 min | ProModel; simulation |
| Khurma, 2008; Canada [151] | ED; case study; 1 mo | Lean and DES | Mean waiting time in 1st shift | Reduced from 226.9 min to 4.9 min | ProModel; simulation |
| Mean waiting time in 2nd shift | Reduced from 124 min to 9.1 min | ||||
| Yu, 2008; USA [150] | Registration department; case study; n = 362; 3 mo | Lean six sigma and DES | Mean waiting time | Reduced from 42.3 min to 6.5 min | Arena; simulation |
| Kim, 2007; USA [142] | Radiation oncology department; case study; n = 6 mo | Lean and simulation (not specified) | Mean waiting time of treatments initiated | Reduced from 7 days to 1 day | Not specified; simulation |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tlapa, D.; Franco-Alucano, I.; Limon-Romero, J.; Baez-Lopez, Y.; Tortorella, G. Lean, Six Sigma, and Simulation: Evidence from Healthcare Interventions. Sustainability 2022, 14, 16849. https://doi.org/10.3390/su142416849
Tlapa D, Franco-Alucano I, Limon-Romero J, Baez-Lopez Y, Tortorella G. Lean, Six Sigma, and Simulation: Evidence from Healthcare Interventions. Sustainability. 2022; 14(24):16849. https://doi.org/10.3390/su142416849
Chicago/Turabian StyleTlapa, Diego, Ignacio Franco-Alucano, Jorge Limon-Romero, Yolanda Baez-Lopez, and Guilherme Tortorella. 2022. "Lean, Six Sigma, and Simulation: Evidence from Healthcare Interventions" Sustainability 14, no. 24: 16849. https://doi.org/10.3390/su142416849
APA StyleTlapa, D., Franco-Alucano, I., Limon-Romero, J., Baez-Lopez, Y., & Tortorella, G. (2022). Lean, Six Sigma, and Simulation: Evidence from Healthcare Interventions. Sustainability, 14(24), 16849. https://doi.org/10.3390/su142416849










