The Utilization of Selected Threatened or Protected Plant Species; A Case of Limpopo Province, South Africa
Abstract
:1. Introduction
2. Materials and Methods
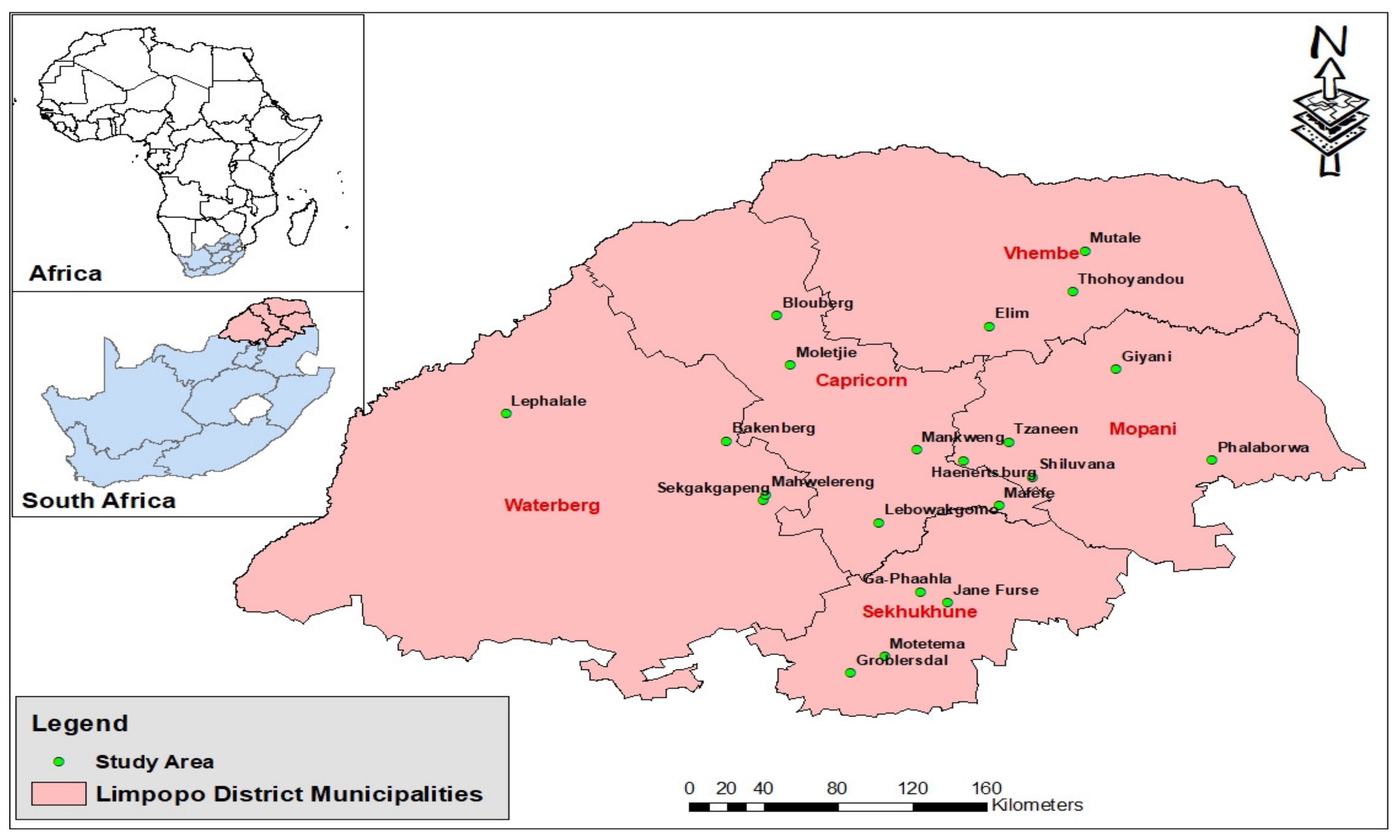
2.1. Study Area
2.2. Data Collection
2.3. Species Utilization
2.4. Medicinal Application of Plants
2.5. Plant Collection
2.6. Ethical Considerations
2.7. Data Analysis
3. Results
3.1. Species Utilization
3.2. Medicinal Applications of Plants
3.2.1. Circulatory Problems
3.2.2. Digestive Problems
3.2.3. Respiratory Problems
3.2.4. Parapsychological Problems
3.3. Herbal Remedies
3.3.1. Parts Used
3.3.2. Method of Preparation
3.3.3. Mode of Administration
3.4. Plant Collection
3.4.1. Source
3.4.2. Perception on Local Availability
4. Discussion
4.1. Species Utilization
4.2. Medicinal Applications of Plants
4.2.1. Circulatory Problems
4.2.2. Digestive Problems
4.2.3. Respiratory Problems
4.2.4. Parapsychological Problems
4.3. Herbal Remedies
4.3.1. Parts Used
4.3.2. Methods of Herbal Preparations
4.3.3. Mode of Administration
4.4. Plant Collection
4.4.1. Source
4.4.2. Perception on Local Availability
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van der Merwe, D.; Swan, G.E.; Botha, C.J. Use of ethnoveterinary medicinal plants in cattle by Setswana-speaking people in the Madikwe area of the North West Province of South Africa. J. S. Afr. Vet. Assoc. 2001, 72, 189–196. [Google Scholar] [CrossRef] [Green Version]
- Sobiecki, J.F. The intersection of culture and science in South African traditional medicine. Indo-Pac. J. Phenom 2014, 14, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Ross, E. Inaugural lecture: African spirituality, ethics and traditional healing–implications for indigenous South African social work education and practice. S. Afr. J. Bioeth. Law 2010, 3, 44–51. [Google Scholar]
- Makunga, N.P. African medicinal flora in the limelight. S. Afr. J. Sci. 2011, 107, 12. [Google Scholar] [CrossRef] [Green Version]
- Mongalo, N.I. Antibacterial Activities of Selected Medicinal Plants Used to Treat Sexually Transmitted Infections in Blouberg Area, Limpopo Province. Master’s Thesis, University of Zululand, KwaZulu-Natal, South Africa, 2013. [Google Scholar]
- Mothibe, M.E.; Sibanda, M. African Traditional Medicine: South African Perspective. In Traditional and Complementary Medicine; Mordeniz, C., Ed.; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef] [Green Version]
- Makueti, J.T.; Tsobeng, A.; Tchoundjeu, Z.; Tsafack, S.; Numbissi, F. Population structure and traditional management patterns of two threatened medicinal tree species (Garcinia lucida and Pausinystalia johimbe) in the humid southern forest of Cameroon. J. Biodivers. Environ. Sci. 2015, 7, 459–481. [Google Scholar]
- Semenya, S.S.; Maroyi, A. Ethnobotanical survey of plants used by Bapedi traditional healers to treat tuberculosis and its opportunistic infections in the Limpopo Province, South Africa. S. Afr. J. Bot. 2019, 122, 401–421. [Google Scholar] [CrossRef]
- Semenya, S.S.; Potgieter, M.J.; Erasmus, L.J.C. Indigenous plant species used by Bapedi healers to treat sexually transmitted infections: Their distribution, harvesting, conservation and threats. S. Afr. J. Bot. 2013, 87, 66–75. [Google Scholar] [CrossRef] [Green Version]
- Semenya, S.S. Bapedi Phytomedicine and Their Use in the Treatment of Sexually Transmitted Diseases in Limpopo Province, South Africa. Master’s Thesis, University of Limpopo, Mankweng, South Africa, 2012. [Google Scholar]
- Mathibela, K.M. An Investigation into Aspects of Medicinal Plant Use by Traditional Healers from Blouberg Mountain, Limpopo Province, South Africa. Master’s Thesis, University of Limpopo, Mankweng, South Africa, 2013. [Google Scholar]
- Semenya, S.S.; Potgieter, M.J.; Tshisikhawe, M.P. Use, conservation and present availability status of ethnomedicinal plants of Matebele-village in the Limpopo Province, South Africa. Afr. J. Biotechnol. 2013, 12, 2393–2405. [Google Scholar]
- Mucina, L.; Rutherford, M.C. The Vegetation of South Africa, Lesotho and Swaziland; Strelizia 19, South African National Biodiversity Institute Pretoria: Silverton, CO, USA, 2006; 807p. [Google Scholar]
- Neto, E.M.F.; Peroni, N.; Albuquerque, U.P. Traditional knowledge and management of umbu (Spondias tuberosa, Anacardiaceae): An endemic species from semi-arid region of north-eastern Brazil. Econ. Bot. 2010, 64, 11–21. [Google Scholar] [CrossRef]
- Red List of South African Plants Version 2020.1. Available online: http://redlist.sanbi.org/ (accessed on 15 September 2021).
- Hutchings, A. A survey and-analysis of traditional medicinal plants as used by the Zulu, Xhosa and Sotho. Bothalia 1989, 19, 111–123. [Google Scholar] [CrossRef]
- Quinlan, M.B. Considerations for collecting freelists in the field: Examples from ethnobotany. Field Methods 2005, 17, 1–16. [Google Scholar] [CrossRef]
- Pérez-Vicente, S.; Ruiz, M.E. Descriptive statistics. Allergol. Immunopathol. 2009, 37, 314–320. [Google Scholar] [CrossRef]
- Moeng, T.E. An Investigation into the Trade of Medicinal Plants by Muthi Shops and Street Vendors in the Limpopo Province, South Africa. Master’s Thesis, University of Limpopo, Mankweng, South Africa, 2010. [Google Scholar]
- Tshisikhawe, M.P.; Van Rooyen, M.W.; Bhat, R.B. An evaluation of the extent and threat of bark harvesting of medicinal plant species in the Venda region, Limpopo Province, South Africa. Int. J. Exp. Bot. 2012, 81, 89–100. [Google Scholar]
- Magwede, K.; Van Wyk, B.-E.; Van Wyk, A.E. An inventory of Vhavenḓa useful plants. S. Afr. J. Bot. 2019, 122, 57–89. [Google Scholar] [CrossRef]
- Hulela, K.; Thobega, M. Botswana faith leaders’ attitudes towards the use of indigenous medicinal herbs. J. Med. Plants Res. 2013, 7, 1550–1556. [Google Scholar]
- Maroyi, A. Warburgia salutaris (Bertol. f.) Chiov.: A multi-use ethnomedicinal plant species. J. Med. Plants Res. 2013, 7, 53–60. [Google Scholar]
- Rasethe, M.T.; Semenya, S.S.; Maroyi, A. Medicinal Plants Traded in Informal Herbal Medicine Markets of the Limpopo Province, South Africa. Evid. Based Complement. Alternat. Med. 2019, 2019, 2609532. [Google Scholar] [CrossRef] [Green Version]
- Komoreng, L.; Thekisoe, O.; Lehasa, S.; Tiwani, T.; Mzizi, N.; Mokoena, N.; Khambule, N.; Ndebele, S.; Mdletshe, N. An ethnobotanical survey of traditional medicinal plants used against lymphatic filariasis in South Africa. S. Afr. J. Bot. 2017, 111, 12–16. [Google Scholar] [CrossRef]
- Philander, L.A. An ethnobotany of Western Cape Rasta bush medicine. J. Ethnopharmacol. 2011, 138, 578–594. [Google Scholar] [CrossRef] [PubMed]
- Kelmanson, J.E.; Jager, A.K.; Van Staden, J. Zulu medicinal plants with antibacterial activity. J. Ethnopharmacol. 2000, 69, 241–246. [Google Scholar] [CrossRef]
- Cogne, A.-L.; Marston, A.; Mavi, S.; Hostettmann, K. Study of two plants used in traditional medicine in Zimbabwe for skin problems and rheumatism: Dioscorea sylvatica and Urginea altissima. J. Ethnopharmacol. 2001, 75, 51–53. [Google Scholar] [CrossRef]
- Motlhanka, D.M.T.; Nthoiwa, G.P. Ethnobotanical survey of medicinal plants of Tswapong North, in Eastern Botswana: A case of plants from Mosweu and Seolwane villages. Eur. J. Med. Plants 2013, 3, 10–24. [Google Scholar] [CrossRef]
- Rankoana, S.A. Sustainable Use and Management of Indigenous Plant Resources: A Case of Mantheding Community in Limpopo Province, South Africa. Sustainability 2016, 8, 221. [Google Scholar] [CrossRef] [Green Version]
- John, W.K. A Survey of Traditional Health Remedies Used by the Maasai of Southern Kaijiado District, Kenya. Ethnobot. Res. Appl. 2006, 4, 061–073. [Google Scholar]
- Senkoro, A.M.; Talhinhas, P.; Simões, F.; Batista-Santos, P.; Shackleton, C.M.; Voeks, R.A.; Marques, I.; Ribeiro-Barros, A.I. The genetic legacy of fragmentation and overexploitation in the threatened medicinal African pepper-bark tree, Warburgia salutaris. Sci. Rep. 2020, 10, 19725. [Google Scholar] [CrossRef] [PubMed]
- Marx, J.; Pretorius, E.; Espang, W.J.; Bester, M.J. Urginea sanguinea: Medicinal wonder or death in disguise? Environ. Toxicol. Pharmacol. 2005, 20, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Phanuel, A.S.; Nyunja, R.O.; Onyango, J.C. Plant species in the folk medicine of Kit Mikayi Region, Western Kenya. Ethnobot. Leaflets 2010, 14, 836–840. [Google Scholar]
- Omoruyi, B.E.; Bradley, G.; Afolayan, A.J. Ethnomedicinal survey of medicinal plants used for the management of HIV/AIDS infection among local communities of Nkonkobe Municipality, Eastern Cape, South Africa. J. Med. Plants Res. 2012, 6, 3603–3608. [Google Scholar] [CrossRef]
- Semenya, S.S.; Maroyi, A. Source, harvesting, conservation status, threats and management of indigenous plant used for respiratory infections and related symptoms in the Limpopo Province, South Africa. Biodiversitas 2019, 20, 790–811. [Google Scholar] [CrossRef] [Green Version]
- Maroyi, A. Ethnobotanical study of two threatened medicinal plants in Zimbabwe. Int. J. Biodivers. Sci. Manag. 2008, 4, 148–153. [Google Scholar] [CrossRef]
- Wintola, O.A.; Afolayan, A.J. Ethnobotanical survey of plants used for the treatment of constipation within Nkonkobe Municipality of South Africa. Afr. J. Biotechnol. 2010, 9, 7767–7770. [Google Scholar] [CrossRef] [Green Version]
- Semenya, S.S.; Mokgoebo, M.J. The Utilization and Conservation of Indigenous Wild Plant Resources in the Limpopo Province, South Africa. In Natural Resources Management and Biological Sciences; Rhodes, E.R., Naser, H., Eds.; IntechOpen: London, UK, 2020. [Google Scholar] [CrossRef]
- Stoffersen, A.; Winstrup, M.; Nieminen, R.; Allerton, T. Medicinal Plants and Traditional Healing in Contemporary Rural South Africa: The sustainability of Medicinal Plant Use in the Local Culture in Ongeluksnek, Eastern Cape, South Africa; Report from Faculty of Life Sciences; University of Copenhagen: Copenhagen, Denmark, 2011. [Google Scholar]
- Ribeiro, A.; Romeiras, M.M.; Tavares, J.; Faria, M.T. Ethnobotanical survey in Canhane village, district of Massingir, Mozambique: Medicinal plants and traditional knowledge. J. Ethnobiol. Ethnomed. 2010, 6, 33–40. [Google Scholar] [CrossRef] [Green Version]
- Setsogo, M.P.; Mbereki, C.M. Floristic diversity and uses of medicinal plants sold by street Vendors in Gaborone, Botswana. Afr. J. Plant Sci. Biotechnol. 2011, 5, 69–74. [Google Scholar]
- Jeruto, P.; Mutai, C.; George, O.; Lukhoba, C.; Nyamaka, R.; Manani, S.D. Ethnobotanical survey and propagation of some endangered medicinal plants from south Nandi district of Kenya. J. Anim. Plant Sci. 2010, 8, 1016–1043. [Google Scholar]
- Van Wyk, A.S.; Prinsloo, G. Medicinal plant harvesting, sustainability and cultivation in South Africa. Biol. Conserv. 2018, 227, 335–342. [Google Scholar] [CrossRef]
- Semenya, S.S.; Potgieter, M.J. Medicinal plants cultivate in Bapedi traditional healers homegardens, Limpopo Province, South Africa. Afr. J. Tradit. Complement. Altern. Med. 2014, 11, 126–132. [Google Scholar] [CrossRef] [PubMed]







| Groups | Districts | Total | ||||
|---|---|---|---|---|---|---|
| Capricorn | Sekhukhune | Mopani | Waterberg | Vhembe | ||
| THPs | 40 | 40 | 40 | 40 | 20 | 180 |
| CMs | 25 | 25 | 25 | 25 | 10 | 110 |
| Total | 65 | 65 | 65 | 65 | 30 | 290 |
| Species | Participants | Districts | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C | S | M | W | V | |||||||||
| No | % | No | % | No | % | No | % | No | % | No | % | ||
| Alepidea amatymbica | CMs | 0 | 0 | 5 | 20 | 7 | 28 | 3 | 12 | 0 | 0 | 15 | 14 |
| THPs | 23 | 57.5 | 33 | 82.5 | 33 | 82.5 | 28 | 70 | 4 | 20 | 121 | 67 | |
| Brackenridgea zanguebarica | CMs | 0 | 0 | 3 | 12 | 2 | 8 | 1 | 4 | 0 | 0 | 6 | 6 |
| THPs | 19 | 47.5 | 13 | 32.5 | 27 | 67.5 | 13 | 32.5 | 16 | 80 | 88 | 49 | |
| Dioscorea sylvatica | CMs | 3 | 12 | 7 | 28 | 3 | 12 | 0 | 0 | 0 | 0 | 13 | 12 |
| THPs | 1 | 2.5 | 28 | 45 | 24 | 60 | 4 | 10 | 8 | 40 | 65 | 36 | |
| Drimia sanguinea | CMs | 17 | 68 | 15 | 60 | 21 | 84 | 25 | 100 | 6 | 60 | 84 | 76 |
| THPs | 37 | 92.5 | 32 | 80 | 35 | 87.5 | 39 | 97.5 | 18 | 90 | 161 | 89 | |
| Siphonochilus aethiopicus | CMs | 21 | 84 | 22 | 88 | 24 | 96 | 25 | 100 | 8 | 80 | 100 | 91 |
| THPs | 40 | 100 | 35 | 87.5 | 35 | 87.5 | 40 | 100 | 18 | 90 | 168 | 93 | |
| Warburgia salutaris | CMs | 23 | 92 | 19 | 76 | 15 | 60 | 21 | 84 | 5 | 50 | 83 | 75 |
| THPs | 40 | 100 | 37 | 92.5 | 32 | 80 | 39 | 97.5 | 18 | 90 | 166 | 92 | |
| Species | Participants | Disease Categories (Numbers) | Total (Numbers) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C | De | Di | E | G | I | N | O | P | Rp | Rs | S | Sm | ||||
| Alepidea amatymbica | CMs | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 11 | 0 | 2 | 0 | 0 | 18 | 187 |
| THPs | 2 | 2 | 11 | 0 | 0 | 4 | 4 | 0 | 114 | 5 | 26 | 0 | 1 | 169 | ||
| Brackenridgea zanguebarica | CMs | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 22 | 0 | 0 | 0 | 0 | 24 | 158 |
| THPs | 4 | 12 | 5 | 0 | 0 | 1 | 3 | 0 | 108 | 1 | 0 | 0 | 0 | 134 | ||
| Dioscorea sylvatica | CMs | 6 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 12 | 86 |
| THPs | 20 | 3 | 3 | 0 | 0 | 6 | 0 | 0 | 42 | 0 | 0 | 0 | 0 | 74 | ||
| Drimia sanguinea | CMs | 73 | 17 | 4 | 4 | 0 | 13 | 0 | 0 | 10 | 3 | 2 | 11 | 0 | 137 | 392 |
| THPs | 131 | 19 | 15 | 3 | 2 | 16 | 3 | 0 | 33 | 10 | 6 | 16 | 1 | 255 | ||
| Siphonochilus aethiopicus | CMs | 1 | 6 | 77 | 1 | 1 | 1 | 1 | 0 | 35 | 1 | 55 | 2 | 0 | 181 | 466 |
| THPs | 2 | 14 | 69 | 3 | 0 | 3 | 8 | 0 | 68 | 1 | 115 | 2 | 0 | 285 | ||
| Warburgia salutaris | CMs | 22 | 3 | 3 | 1 | 0 | 14 | 1 | 0 | 5 | 5 | 57 | 3 | 0 | 114 | 380 |
| THPs | 67 | 19 | 15 | 2 | 0 | 35 | 3 | 1 | 20 | 5 | 98 | 1 | 0 | 266 | ||
| Total | 330 | 96 | 205 | 15 | 3 | 93 | 24 | 1 | 473 | 31 | 361 | 35 | 2 | |||
| Plant Species | Parts Used | State of Plant Parts |
|---|---|---|
| Alepidea amatymbica | Roots (100%) | Dry |
| Brackenridgea zanguebarica | Roots (97%) and bark (3%) | Dry |
| Dioscorea sylvatica | Tuber (100%) | Dry |
| Drimia sanguinea | Bulb (100%) | Fresh |
| Siphonochilus aethiopicus | Rhizome (100%) | Fresh |
| Warburgia salutaris | Bark (94%), roots (4%) and leaves (2%) | Dry |
| Plant Species | Participants | Capricorn District | Sekhukhune District | Mopani District | Waterberg District | Vhembe District | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Source of Plant (% of Participants) | ||||||||||||||||
| W | H | B | W | H | B | W | H | B | W | H | B | W | H | B | ||
| Alepidea amatymbica | THPs | 30 | 0 | 70 | 41 | 3 | 59 | 29 | 3 | 68 | 18 | 0 | 82 | 0 | 0 | 100 |
| CMs | 0 | 0 | 0 | 0 | 0 | 100 | 71 | 0 | 29 | 0 | 0 | 100 | 0 | 0 | 0 | |
| Brackenridgea zanguebarica | THPs | 32 | 0 | 68 | 23 | 0 | 77 | 19 | 0 | 81 | 14 | 0 | 86 | 25 | 0 | 75 |
| CMs | 0 | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 0 | |
| Dioscorea sylvatica | THPs | 100 | 0 | 0 | 86 | 0 | 14 | 67 | 0 | 33 | 25 | 0 | 75 | 0 | 0 | 100 |
| CMs | 100 | 0 | 0 | 100 | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Drimia sanguinea | THPs | 73 | 16 | 11 | 81 | 0 | 19 | 77 | 0 | 23 | 41 | 3 | 56 | 44 | 0 | 56 |
| CMs | 59 | 12 | 29 | 80 | 0 | 20 | 62 | 0 | 38 | 40 | 0 | 60 | 0 | 0 | 100 | |
| Siphonochilus aethiopicus | THPs | 8 | 5 | 88 | 20 | 3 | 77 | 49 | 0 | 51 | 20 | 3 | 78 | 11 | 17 | 72 |
| CMs | 13 | 0 | 87 | 0 | 0 | 100 | 29 | 0 | 71 | 0 | 0 | 100 | 0 | 0 | 100 | |
| Warburgia salutaris | THPs | 75 | 0 | 25 | 76 | 0 | 24 | 38 | 0 | 63 | 18 | 0 | 82 | 33 | 0 | 67 |
| CMs | 61 | 0 | 58 | 58 | 0 | 42 | 20 | 0 | 80 | 10 | 0 | 90 | 0 | 0 | 100 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rasethe, M.; Potgieter, M.; Pfab, M. The Utilization of Selected Threatened or Protected Plant Species; A Case of Limpopo Province, South Africa. Sustainability 2022, 14, 1073. https://doi.org/10.3390/su14031073
Rasethe M, Potgieter M, Pfab M. The Utilization of Selected Threatened or Protected Plant Species; A Case of Limpopo Province, South Africa. Sustainability. 2022; 14(3):1073. https://doi.org/10.3390/su14031073
Chicago/Turabian StyleRasethe, Marula, Martin Potgieter, and Michèle Pfab. 2022. "The Utilization of Selected Threatened or Protected Plant Species; A Case of Limpopo Province, South Africa" Sustainability 14, no. 3: 1073. https://doi.org/10.3390/su14031073
APA StyleRasethe, M., Potgieter, M., & Pfab, M. (2022). The Utilization of Selected Threatened or Protected Plant Species; A Case of Limpopo Province, South Africa. Sustainability, 14(3), 1073. https://doi.org/10.3390/su14031073






