The Effect of the Built Environment on the COVID-19 Pandemic at the Initial Stage: A County-Level Study of the USA
Abstract
:1. Introduction
2. Materials and Methods
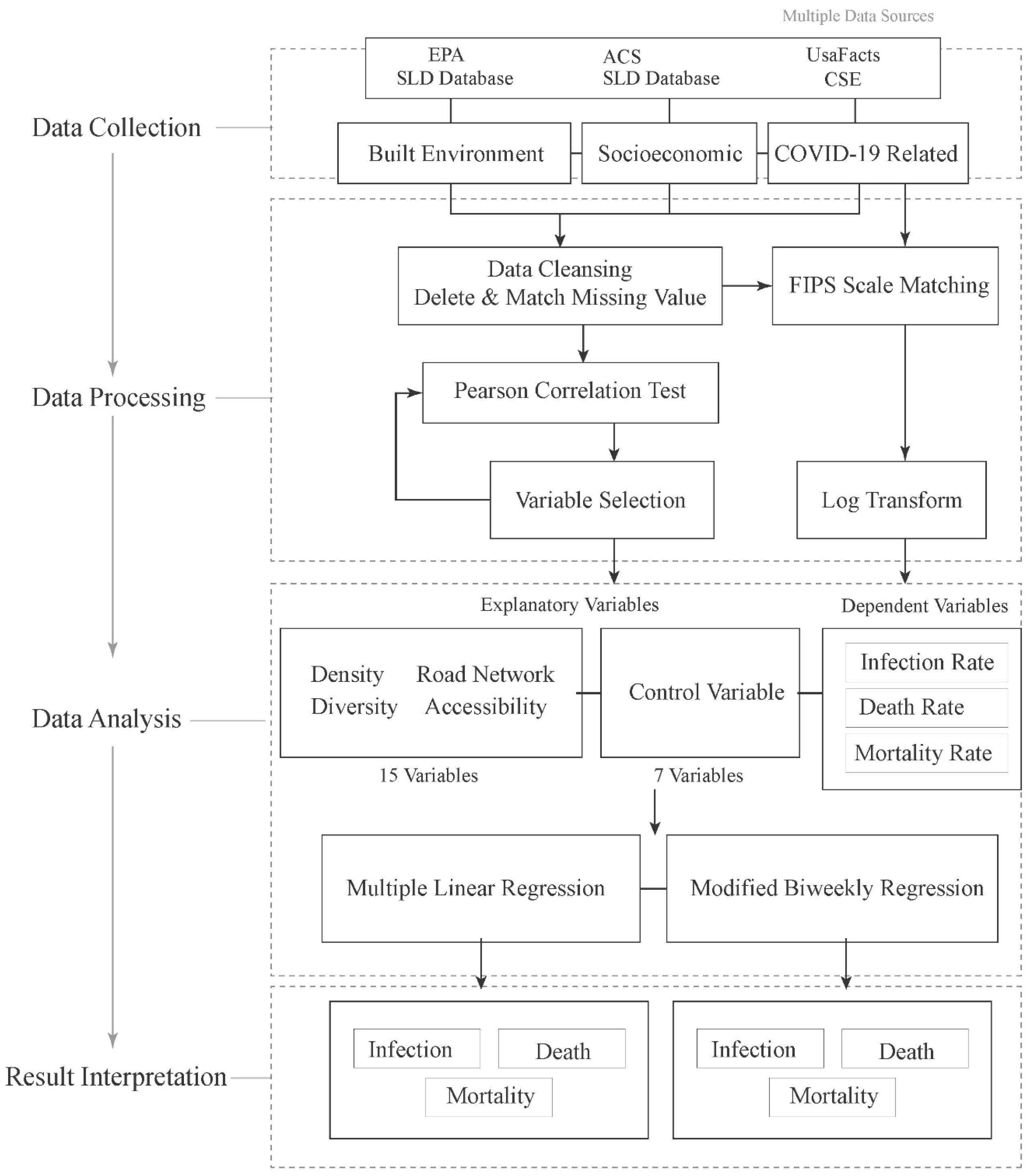
2.1. Research Framework
2.2. Study Area and Data Collection
2.3. Data Processing and Regression Models
2.3.1. Outcome Variables
2.3.2. Variable Processing
Regional Diversity
Job Equilibrium Index (JEI)
Job Accessibility
2.3.3. Ordinary Least Square Analysis
3. Results
3.1. Descriptive Summary of COVID-19 and the Built Environment Variables
3.2. OLS Regressions on Infection Rate, Death Rate, and Mortality Rate
3.3. Biweekly Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sun, F.; Matthews, S.A.; Yang, T.-C.; Hu, M.-H. A spatial analysis of the COVID-19 period prevalence in U.S. counties through June 28, 2020: Where geography matters? Ann. Epidemiol. 2020, 52, 54–59.e1. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, S.; Ewing, R.; Sabouri, S. Longitudinal analyses of the relationship between development density and the COVID-19 morbidity and mortality rates: Early evidence from 1165 metropolitan counties in the United States. Health Place 2020, 64, 102378. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.; Arif, A.A.; Adeyemi, O.; Ghosh, S.; Han, D. Progression of COVID-19 From Urban to Rural Areas in the United States: A Spatiotemporal Analysis of Prevalence Rates. J. Rural Health 2020, 36, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Zenic, N.; Taiar, R.; Gilic, B.; Blazevic, M.; Maric, D.; Pojskic, H.; Sekulic, D. Levels and Changes of Physical Activity in Adolescents during the COVID-19 Pandemic: Contextualizing Urban vs. Rural Living Environment. Appl. Sci. 2020, 10, 3997. [Google Scholar] [CrossRef]
- Liu, C.; Liu, Z.; Guan, C. The impacts of the built environment on the incidence rate of COVID-19: A case study of King County, Washington. Sustain. Cities Soc. 2021, 74, 103144. [Google Scholar] [CrossRef]
- Zulu, L.C.; Kalipeni, E.; Johannes, E. Analyzing spatial clustering and the spatiotemporal nature and trends of HIV/AIDS prevalence using GIS: The case of Malawi, 1994–2010. BMC Infect. Dis. 2014, 14, 285. [Google Scholar] [CrossRef] [Green Version]
- Brizuela, N.G.; García-Chan, N.; Pulido, H.G.; Chowell, G. Understanding the role of urban design in disease spreading. Proc. R. Soc. A 2021, 477, 20200524. [Google Scholar] [CrossRef]
- Xiao, H.; Lin, X.; Chowell, G.; Huang, C.; Gao, L.; Chen, B.; Wang, Z.; Zhou, L.; He, X.; Liu, H.; et al. Urban structure and the risk of influenza A (H1N1) outbreaks in municipal districts. Chin. Sci. Bull. 2014, 59, 554–562. [Google Scholar] [CrossRef]
- Apolloni, A.; Poletto, C.; Colizza, V. Age-specific contacts and travel patterns in the spatial spread of 2009 H1N1 influenza pandemic. BMC Infect. Dis. 2013, 13, 176. [Google Scholar] [CrossRef] [Green Version]
- Mao, L.; Bian, L. Spatial–temporal transmission of influenza and its health risks in an urbanized area. Comput. Environ. Urban Syst. 2010, 34, 204–215. [Google Scholar] [CrossRef]
- Cai, J.; Xu, B.; Chan, K.K.Y.; Zhang, X.; Zhang, B.; Chen, Z.; Xu, B. Roles of Different Transport Modes in the Spatial Spread of the 2009 Influenza A(H1N1) Pandemic in Mainland China. Int. J. Environ. Res. Public Health 2019, 16, 222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maliszewski, P.J.; Wei, R. Ecological factors associated with pandemic influenza A (H1N1) hospitalization rates in California, USA: A geospatial analysis. Geospat. Health 2011, 6, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalziel, B.D.; Kissler, S.; Gog, J.R.; Viboud, C.; Bjørnstad, O.N.; Metcalf, C.J.E.; Grenfell, B.T. Urbanization and humidity shape the intensity of influenza epidemics in U.S. cities. Science 2018, 362, 75–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dowd, J.B.; Andriano, L.; Brazel, D.M.; Rotondi, V.; Block, P.; Ding, X.; Liu, Y.; Mills, M.C. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 9696–9698. [Google Scholar] [CrossRef] [Green Version]
- Lee, B.; Raszka, W.V. COVID-19 Transmission and Children: The Child Is Not to Blame. Pediatrics 2020, 146, e2020004879. [Google Scholar] [CrossRef]
- Millett, G.A.; Jones, A.T.; Benkeser, D.; Baral, S.; Mercer, L.; Beyrer, C.; Honermann, B.; Lankiewicz, E.; Mena, L.; Crowley, J.S.; et al. Assessing differential impacts of COVID-19 on black communities. Ann. Epidemiol. 2020, 47, 37–44. [Google Scholar] [CrossRef]
- Yancy, C.W. COVID-19 and African Americans. JAMA J. Am. Med Assoc. 2020, 323, 1891. [Google Scholar] [CrossRef] [Green Version]
- Cordes, J.; Castro, M.C. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spat. Spatio-Temporal Epidemiol. 2020, 34, 100355. [Google Scholar] [CrossRef]
- Sannigrahi, S.; Pilla, F.; Basu, B.; Basu, A.S. The overall mortality caused by COVID-19 in the European region is highly associated with demographic composition: A spatial regression-based approach. arXiv 2020, arXiv:2005.04029. [Google Scholar]
- Desai, N.; Neyaz, A.; Szabolcs, A.; Shih, A.R.; Chen, J.H.; Thapar, V.; Nieman, L.T.; Solovyov, A.; Mehta, A.; Lieb, D.J.; et al. Temporal and spatial heterogeneity of host response to SARS-CoV-2 pulmonary infection. Nat. Commun. 2020, 11, 1–15. [Google Scholar] [CrossRef]
- Hamidi, S.; Sabouri, S.; Ewing, R. Does Density Aggravate the COVID-19 Pandemic? Early Findings and Lessons for Planners. J. Am. Plan. Assoc. 2020, 86, 495–509. [Google Scholar] [CrossRef]
- Zhang, C.H.; Schwartz, G.G. Spatial Disparities in Coronavirus Incidence and Mortality in the United States: An Ecological Analysis as of May 2020. J. Rural Health 2020, 36, 433–445. [Google Scholar] [CrossRef] [PubMed]
- Skórka, P.; Grzywacz, B.; Moroń, D.; Lenda, M. The macroecology of the COVID-19 pandemic in the Anthropocene. PLoS ONE 2020, 15, e0236856. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, A.; Wang, J. Exploring the roles of high-speed train, air and coach services in the spread of COVID-19 in China. Transp. Policy 2020, 94, 24–42. [Google Scholar] [CrossRef] [PubMed]
- Peters, D.J. Community Susceptibility and Resiliency to COVID-19 Across the Rural-Urban Continuum in the United States. J. Rural Health 2020, 36, 446–456. [Google Scholar] [CrossRef]
- Block, P.; Hoffman, M.; Raabe, I.J.; Dowd, J.B.; Rahal, C.; Kashyap, R.; Mills, M.C. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nat. Hum. Behav. 2020, 4, 588–596. [Google Scholar] [CrossRef]
- Kraemer, M.U.G.; Yang, C.-H.; Gutierrez, B.; Wu, C.-H.; Klein, B.; Pigott, D.M.; Open COVID-19 Data Working Group; du Plessis, L.; Faria, N.R.; Li, R.; et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020, 368, 493–497. [Google Scholar] [CrossRef] [Green Version]
- Lau, M.S.Y.; Grenfell, B.; Thomas, M.; Bryan, M.; Nelson, K.; Lopman, B. Characterizing superspreading events and age-specific infectiousness of SARS-CoV-2 transmission in Georgia, USA. Proc. Natl. Acad. Sci. USA 2020, 117, 22430–22435. [Google Scholar] [CrossRef]
- Li, B.; Peng, Y.; He, H.; Wang, M.; Feng, T. Built environment and early infection of COVID-19 in urban districts: A case study of Huangzhou. Sustain. Cities Soc. 2021, 66, 102685. [Google Scholar] [CrossRef]
- Li, S.; Ma, S.; Zhang, J. Association of built environment attributes with the spread of COVID-19 at its initial stage in China. Sustain. Cities Soc. 2021, 67, 102752. [Google Scholar] [CrossRef]
- Megahed, N.A.; Ghoneim, E.M. Antivirus-built environment: Lessons learned from Covid-19 pandemic. Sustain. Cities Soc. 2020, 61, 102350. [Google Scholar] [CrossRef] [PubMed]
- Palm, M.; Allen, J.; Liu, B.; Zhang, Y.; Widener, M.; Farber, S. Riders Who Avoided Public Transit During COVID-19. J. Am. Plan. Assoc. 2021, 87, 455–469. [Google Scholar] [CrossRef]



| Variable | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|
| Socioeconomic | ||||
| Population | 104.59 | 333.65 | 0.27 | 10,039.11 |
| Senior population | 0.20 | 0.05 | 0.05 | 0.58 |
| Unemployment | 4.00 | 1.46 | 1.40 | 18.30 |
| Population change | −0.04 | 0.38 | −0.89 | 2.80 |
| Working age population | 0.77 | 0.04 | 0.58 | 0.98 |
| Car ownership | 0.04 | 0.04 | 0.00 | 0.49 |
| Change of employment | −0.10 | 1.50 | −39.49 | 1.00 |
| Density | ||||
| Residential density | 4.25 | 8.07 | 0.00 | 112.63 |
| Population density | 9.76 | 18.35 | 0.00 | 291.53 |
| Employment density | 3.05 | 7.77 | 0.00 | 177.55 |
| Diversity (Job and Household) | ||||
| Jobs per household | 1.13 | 1.20 | 0.00 | 28.32 |
| Job diversity | 0.17 | 0.09 | 0.00 | 0.99 |
| Job equilibrium | 0.29 | 0.11 | 0.00 | 0.99 |
| Road network | ||||
| Total road density | 14.19 | 6.76 | 0.39 | 45.42 |
| Auto-oriented road density | 1.99 | 1.50 | 0.00 | 17.01 |
| Pedestrian-oriented road density | 63.63 | 38.10 | 0.10 | 382.02 |
| People-oriented street intersection | 1.15 | 1.37 | 0.00 | 24.78 |
| Auto-oriented street intersection | 10.95 | 9.08 | 0.00 | 140.44 |
| Accessibility | ||||
| Transit proximity | 143.50 | 167.26 | 0.00 | 1098.57 |
| Transit-oriented job access | 0.03 | 0.09 | 0.00 | 1.00 |
| Transit frequency | 422.61 | 2468.38 | 0.00 | 118,204.78 |
| Auto-oriented job access | 112.16 | 138.70 | 0.00 | 1134.71 |
| Workforce access | 177.53 | 225.92 | 0.32 | 1345.42 |
| (1) | (2) | (3) | |
|---|---|---|---|
| Infection | Death | Mortality | |
| Socioeconomic | |||
| Population | −0.0000 ** | −0.0000 ** | −0.0000 *** |
| Senior population | −1.1600 *** | 0.0928 | 0.3985 |
| Unemployment | −0.0164 ** | 0.0062 | 0.0223 *** |
| Population change | −0.0475 * | 0.0604 * | 0.0247 |
| Working age population | −2.3170 *** | −3.1452 *** | −0.0098 |
| Car ownership | 0.9962 *** | 1.8808 *** | 0.5162 ** |
| Change of employment | 0.0115 | 0.0202 *** | 0.0064 |
| Density | |||
| Residential density | 0.0676 * | 0.0515 | 0.0631 ** |
| Population density | −0.0472 *** | −0.0578 *** | −0.0514 *** |
| Employment density | −0.0102 | 0.0175 | 0.0146 |
| Diversity (Job and Household) | |||
| Jobs per household | 0.0879 ** | 0.0197 | −0.0586 ** |
| Job diversity | 0.2972 ** | −0.2673 * | 0.3513 *** |
| Job equilibrium | −0.1647 | −0.6630 *** | −0.2035 *** |
| Road network | |||
| Total road density | 0.1714 *** | 0.0704 ** | 0.1302 *** |
| Auto-oriented road density | −0.1860 *** | 0.0992 | 0.0033 |
| Pedestrian-oriented road density | −0.1329 *** | 0.0197 | −0.0804 *** |
| People-oriented street intersection | −0.0086 *** | −0.0088 *** | −0.0071 *** |
| Auto-oriented street intersection | −0.0167 | −0.0783 | −0.0781 ** |
| Accessibility | |||
| Transit proximity | 0.0000 | −0.0008 *** | 0.0001 |
| Transit-oriented job access | 0.7617 | 0.6724 | 0.0087 |
| Transit frequency | 0.0000 | 0.0000 | 0.0000 |
| Auto-oriented job access | −0.0000 | −0.0000 ** | −0.0000 *** |
| Population access | 0.0000 *** | 0.0000 *** | 0.0000 *** |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
|---|---|---|---|---|---|---|---|
| Variables | Weeks 1–2 | Weeks 3–4 | Weeks 5–6 | Weeks 7–8 | Weeks 9–10 | Weeks 11–12 | Weeks 13–14 |
| Socioeconomic | |||||||
| Population | −0.0000 *** | 0.0000 ** | 0.0000 | 0.0000 | −0.0000 | −0.0000 | 0.0000 |
| Senior population | −0.2977 | −1.1371 *** | −2.1156 *** | −2.3441 *** | −2.2181 *** | −1.8857 *** | −1.4291 *** |
| Unemployment | 0.0410 *** | −0.0153 * | 0.0217 ** | 0.0095 | −0.0066 | −0.0024 | 0.0019 |
| Population change | 0.0107 | 0.0623 * | 0.1015 *** | 0.0460 | −0.0288 | −0.0110 | 0.0782 ** |
| Working age population | 2.3823 *** | −0.7323 | 1.2620 ** | −0.3882 | −2.1036 *** | −3.2293 *** | −4.3355 *** |
| Car ownership | −0.7978 *** | 0.5767 * | 1.3240 *** | 1.4903 *** | 1.0235 ** | 1.8022 *** | 1.5565 *** |
| Change of employment | 0.0000 | −0.0000 ** | −0.0000 | −0.0000 | −0.0000 | −0.0000 | −0.0000 |
| Density | |||||||
| Residential density | −0.1784 *** | 0.2420 *** | 0.0883 * | 0.0503 | 0.0405 | 0.0468 | 0.0580 |
| Population density | 0.0563 *** | −0.1284 *** | −0.0860 *** | −0.0714 *** | −0.0567 ** | −0.0590 ** | −0.0585 ** |
| Employment density | 0.0735 *** | −0.0303 | 0.0346 | 0.0423 * | 0.0246 | 0.0213 | 0.0138 |
| Diversity (Job and Household) | |||||||
| Jobs per household | 0.1516 *** | −0.0002 | −0.0157 | −0.0142 | 0.0210 | 0.0939 | 0.1427 ** |
| Job diversity | −0.2168 ** | 0.8060 *** | 1.0501 *** | 0.8125 *** | 0.5634 *** | 0.5193 *** | 0.3842 ** |
| Job equilibrium | −0.1053 | −0.2133 * | −0.7651 *** | −0.8249 *** | −0.6743 *** | −0.8359 *** | −0.8070 *** |
| Road network | |||||||
| Total road density | 0.0852 *** | 0.1452 *** | 0.3036 *** | 0.3519 *** | 0.3395 *** | 0.3321 *** | 0.2840 *** |
| Auto-oriented road density | −0.0342 | −0.2465 *** | −0.1996 *** | −0.2119 *** | −0.0974 | −0.0535 | −0.1418 * |
| Pedestrian-oriented road density | −0.0951 *** | −0.0430 | −0.1945 *** | −0.2384 *** | −0.2500 *** | −0.2355 *** | −0.1498 *** |
| People-oriented street intersection | 0.0010 | −0.0168 *** | −0.0177 *** | −0.0187 *** | −0.0154 *** | −0.0169 *** | −0.0216 *** |
| Auto-oriented street intersection | −0.0841 ** | 0.0555 | −0.1447 ** | −0.1534 ** | −0.1991 *** | −0.2212 *** | −0.1003 |
| Accessibility | |||||||
| Transit proximity | 0.0003 ** | 0.0003 | 0.0002 | 0.0000 | 0.0000 | −0.0001 | −0.0002 |
| Transit-oriented job access | 1.8384 *** | 0.9669 | 0.7883 | 0.9536 | 0.8895 | 0.6939 | 0.4814 |
| Transit frequency | −0.0001 ** | 0.0001 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Auto-oriented job access | −0.0000 | −0.0000 *** | −0.0000 *** | −0.0000 *** | −0.0000 | −0.0000 | −0.0000 * |
| Population access | 0.0000 | 0.0000 *** | 0.0000 *** | 0.0000 *** | 0.0000 *** | 0.0000 ** | 0.0000 ** |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
|---|---|---|---|---|---|---|---|
| Variables | Weeks 1–2 | Weeks 3–4 | Weeks 5–6 | Weeks 7–8 | Weeks 9–10 | Weeks 11–12 | Weeks 13–14 |
| Socioeconomic | |||||||
| Population | 0.0000 ** | −0.0000 *** | −0.0000 | −0.0000 | −0.0000 | −0.0000 | −0.0000 |
| Senior population | 0.0178 | −0.1554 | −0.0660 | −0.1180 | −0.2427 | 0.0988 | 0.0239 |
| Unemployment | 0.0063 *** | 0.0042 | 0.0126 ** | 0.0124 ** | 0.0147 ** | 0.0258 *** | 0.0266 *** |
| Population change | 0.0027 | −0.0216 ** | −0.0400 ** | −0.0606 *** | −0.0549 ** | −0.0717 *** | −0.0634 *** |
| Working age population | 0.2378 *** | 0.1236 | −0.1212 | −0.0415 | −0.5071 | −0.8897 ** | −0.7289 ** |
| Car ownership | −0.0911 ** | 0.1170 | 0.6333 *** | 1.4228 *** | 0.9599 *** | 0.8446 *** | 0.8679 *** |
| Change of employment | −0.0000 *** | 0.0000 *** | −0.0000 | −0.0000 | −0.0000 | −0.0000 | 0.0000 |
| Density | |||||||
| Residential density | −0.0161 ** | 0.0137 | 0.0551 ** | 0.0240 | 0.0524 | 0.0572 * | 0.0550 * |
| Population density | 0.0106 *** | −0.0053 | −0.0498 *** | −0.0505 *** | −0.0543 *** | −0.0449 *** | −0.0397 *** |
| Employment density | 0.0019 | 0.0059 | 0.0132 | 0.0285 ** | 0.0119 | −0.0050 | −0.0059 |
| Diversity (Job and Household) | |||||||
| Jobs per household | 0.0204 *** | 0.0152 | 0.0022 | −0.0172 | 0.0361 | 0.0566 * | 0.0287 |
| Job diversity | −0.0249 | 0.0519 | 0.2367 *** | 0.2673 *** | 0.2065 ** | 0.3063 *** | 0.2911 *** |
| Job equilibrium | −0.0280 * | −0.0064 | −0.0279 | −0.0961 | −0.1165 | −0.1839 ** | −0.1669 ** |
| Road network | |||||||
| Total road density | 0.0253 *** | −0.0107 | 0.0841 *** | 0.1378 *** | 0.1726 *** | 0.1411 *** | 0.1077 *** |
| Auto-oriented road density | −0.0088 | −0.0210 | −0.1475 *** | −0.1686 *** | −0.2446 *** | −0.1508 *** | −0.1128 ** |
| Pedestrian-oriented road density | −0.0226 *** | −0.0012 | −0.0560 *** | −0.0865 *** | −0.1381 *** | −0.1175 *** | −0.0884 *** |
| People-oriented street intersection | −0.0005 | 0.0008 | −0.0045 *** | −0.0079 *** | −0.0063 *** | −0.0047 *** | −0.0037 ** |
| Auto-oriented street intersection | −0.0212 *** | 0.0162 | 0.0096 | −0.0110 | −0.0073 | −0.0324 | −0.0450 |
| Accessibility | |||||||
| Transit proximity | 0.0000 | −0.0004 *** | 0.0001 | 0.0002 | 0.0004 *** | 0.0003 ** | 0.0001 |
| Transit-oriented job access | −0.4898 *** | 0.7034 *** | 1.1896 *** | 1.0467 ** | 1.1786 *** | 0.6838 | 0.2316 |
| Transit frequency | 0.0000 | −0.0000 ** | −0.0000 | −0.0000 | −0.0000 | −0.0000 | 0.0000 |
| Auto-oriented job access | 0.0000 *** | −0.0000 *** | −0.0000 *** | −0.0000 *** | −0.0000 * | −0.0000 | −0.0000 |
| Population access | −0.0000 *** | 0.0000 *** | 0.0000 *** | 0.0000 *** | 0.0000 *** | 0.0000 ** | 0.0000 ** |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
|---|---|---|---|---|---|---|---|
| Variables | Weeks 1–2 | Weeks 3–4 | Weeks 5–6 | Weeks 7–8 | Weeks 9–10 | Weeks 11–12 | Weeks 13–14 |
| Socioeconomic | |||||||
| Population | 0.0000 | −0.0000 | −0.0000 | 0.0000 | 0.0000 | −0.0000 | −0.0000 |
| Senior population | 0.0310 | −0.1608 | 0.1861 | −0.1007 | 0.0204 | 0.2735 | −0.0408 |
| Unemployment | 0.0001 | 0.0081 ** | 0.0109 ** | 0.0051 | 0.0104 * | 0.0142 ** | 0.0128 ** |
| Population change | 0.0059 | 0.0384 *** | 0.0273 | 0.0230 | 0.0394 * | 0.0064 | −0.0282 |
| Working age population | −0.0394 | 0.2268 | −0.4536 | 0.1763 | −0.1947 | −0.2548 | 0.0734 |
| Car ownership | 0.0163 | −0.0435 | 0.2063 | 0.9745 *** | 0.5998 *** | 0.6388 *** | 0.5889 *** |
| Change of employment | −0.0000 | 0.0000 | 0.0000 | −0.0000 | −0.0000 | −0.0000 | 0.0000 |
| Density | |||||||
| Residential density | 0.0058 | 0.0021 | 0.0584 * | 0.0462 | 0.1240 *** | 0.0839 ** | 0.0911 *** |
| Population density | −0.0070 ** | 0.0000 | −0.0354 *** | −0.0469 *** | −0.0795 *** | −0.0620 *** | −0.0602 *** |
| Employment density | 0.0024 | 0.0028 | 0.0024 | 0.0229 | 0.0055 | 0.0115 | 0.0054 |
| Diversity (Job and Household) | |||||||
| Jobs per household | −0.0086 | 0.0080 | −0.0270 | −0.0679 ** | −0.0181 | −0.0297 | −0.0533 * |
| Job diversity | 0.0312 | 0.0632 | 0.4663 *** | 0.4220 *** | 0.2311 ** | 0.4148 *** | 0.4114 *** |
| Job equilibrium | 0.0185 | −0.0416 | −0.1295 * | −0.1690 ** | −0.1008 | −0.1882 ** | −0.2035 *** |
| Road network | −0.0086 | 0.0080 | −0.0270 | −0.0679 ** | −0.0181 | −0.0297 | −0.0533 * |
| Total road density | −0.0054 | 0.0562 *** | 0.1003 *** | 0.1413 *** | 0.1880 *** | 0.1568 *** | 0.1543 *** |
| Auto-oriented road density | 0.0120 | −0.0114 | −0.0481 | −0.0097 | −0.1305 *** | −0.0677 | −0.1238 *** |
| Pedestrian-oriented road density | 0.0084 | −0.0415 *** | −0.0488 ** | −0.0633 ** | −0.1214 *** | −0.1173 *** | −0.1252 *** |
| People-oriented street intersection | −0.0001 | −0.0025 ** | −0.0075 *** | −0.0109 *** | −0.0103 *** | −0.0060 *** | −0.0046 *** |
| Auto-oriented street intersection | 0.0055 | −0.0306 | −0.0051 | −0.0627 | −0.0531 | −0.0817 ** | −0.0796 ** |
| Accessibility | |||||||
| Transit proximity | 0.0001 *** | −0.0000 | 0.0000 | 0.0001 | 0.0002 | 0.0002 * | 0.0002 * |
| Transit-oriented job access | 0.3504 *** | −0.5247 * | −0.4465 | −0.3110 | −0.2484 | −0.0307 | −0.2504 |
| Transit frequency | −0.0000 | −0.0000 | 0.0000 | −0.0000 | 0.0000 | −0.0000 | 0.0000 |
| Auto-oriented job access | −0.0000 | −0.0000 * | −0.0000 *** | −0.0000 *** | −0.0000 *** | −0.0000 *** | −0.0000 *** |
| Population access | 0.0000 | 0.0000 * | 0.0000 *** | 0.0000 *** | 0.0000 *** | 0.0000 *** | 0.0000 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guan, C.; Tan, J.; Hall, B.; Liu, C.; Li, Y.; Cai, Z. The Effect of the Built Environment on the COVID-19 Pandemic at the Initial Stage: A County-Level Study of the USA. Sustainability 2022, 14, 3417. https://doi.org/10.3390/su14063417
Guan C, Tan J, Hall B, Liu C, Li Y, Cai Z. The Effect of the Built Environment on the COVID-19 Pandemic at the Initial Stage: A County-Level Study of the USA. Sustainability. 2022; 14(6):3417. https://doi.org/10.3390/su14063417
Chicago/Turabian StyleGuan, Chenghe, Junjie Tan, Brian Hall, Chao Liu, Ying Li, and Zhichang Cai. 2022. "The Effect of the Built Environment on the COVID-19 Pandemic at the Initial Stage: A County-Level Study of the USA" Sustainability 14, no. 6: 3417. https://doi.org/10.3390/su14063417







