Learning from the Past: Pandemics and the Governance Treadmill
Abstract
:1. Introduction
2. The Governance Treadmill
3. Responding to a Specific Crisis
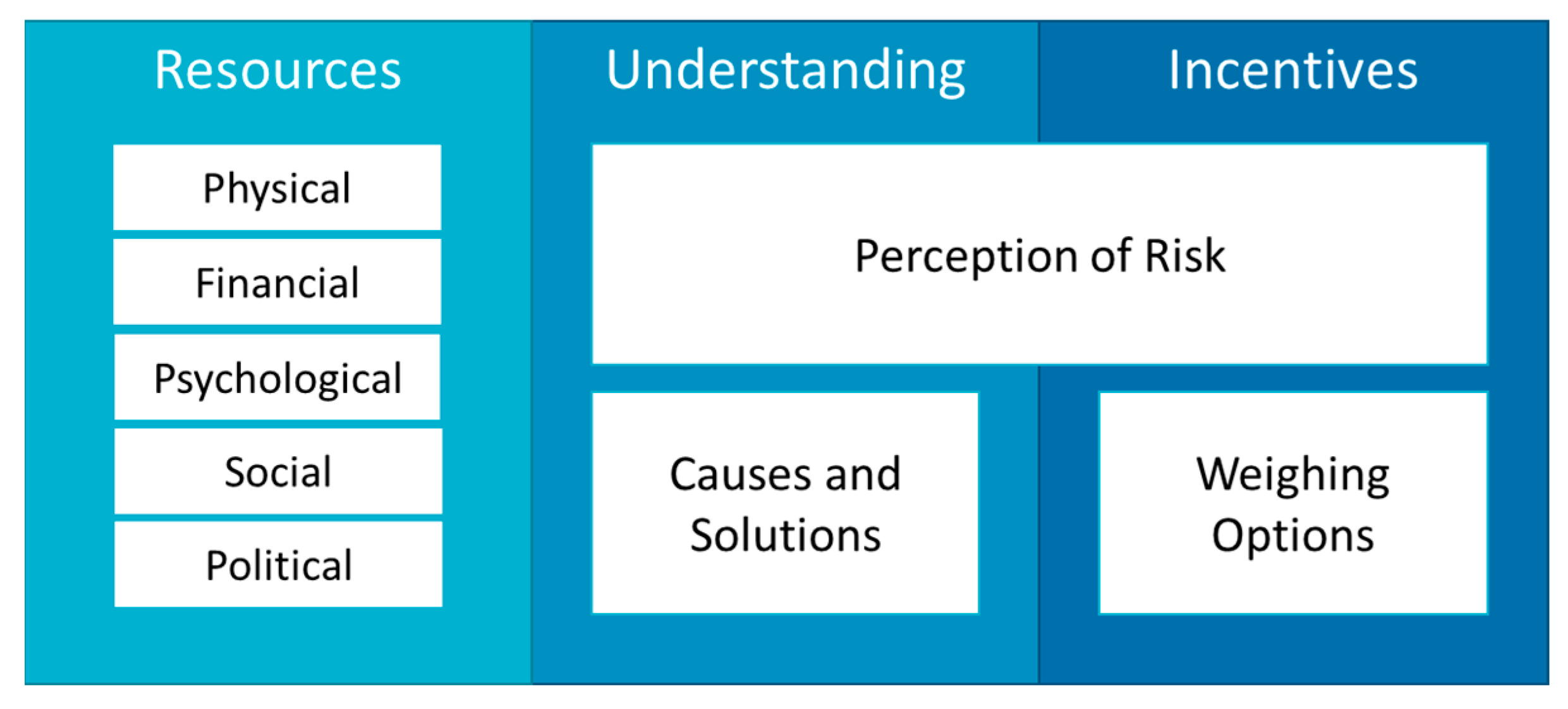
3.1. Aligning Capacities for Effective Governance
3.2. Illustrating Alignment Successes and Failures
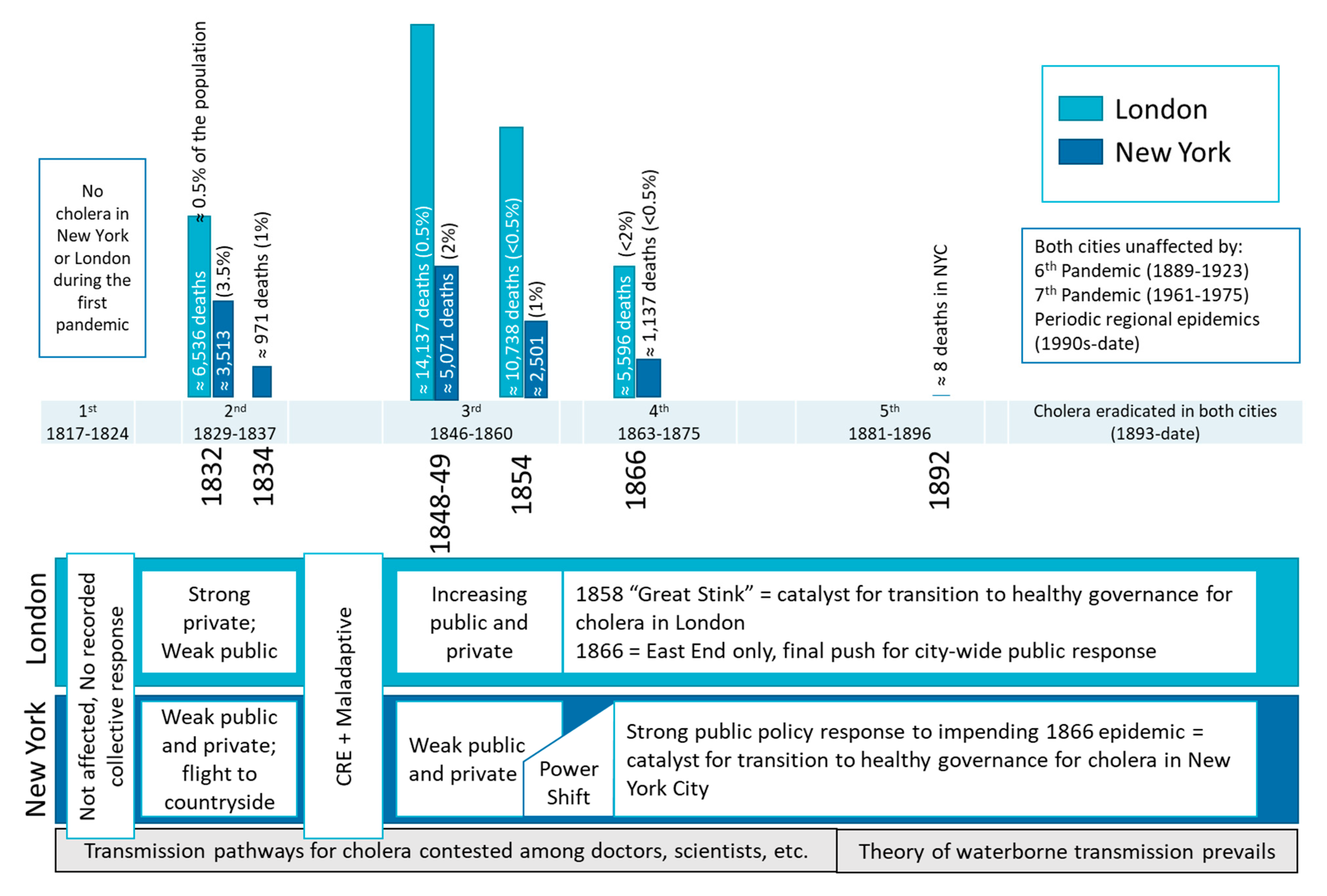
4. Transition to Healthy Governance–Learning Lessons for Subsequent Crises
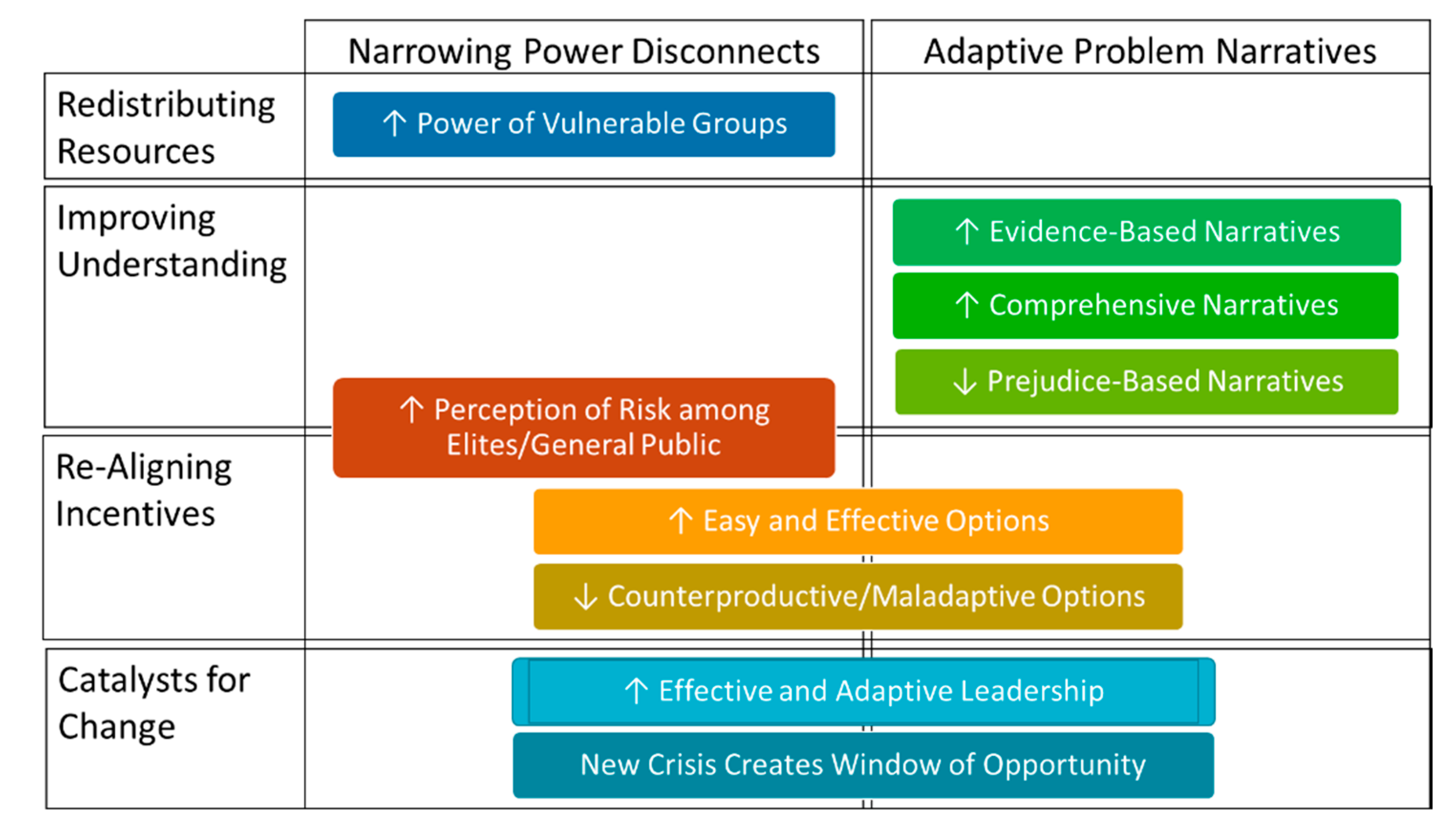
4.1. Components of Healthy Governance
4.2. Barriers to Healthy Governance
4.3. Precursours of Healthy Governance
4.4. Scope and Scale
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Egede, L.E.; Walker, R.J. Structural racism, social risk factors, and COVID-19—A Dangerous convergence for Black Americans. N. Engl. J. Med. 2020, 383, e77. [Google Scholar] [CrossRef] [PubMed]
- Walensky, R.P.; del Rio, C. From mitigation to containment of the COVID-19 pandemic: Putting the SARS-CoV-2 genie back in the bottle. JAMA 2020, 323, 1889. [Google Scholar] [CrossRef] [PubMed]
- Bucciardini, R.; Contoli, B.; De Castro, P.; Donfrancesco, C.; Falzano, L.; Ferrelli, R.; Giammarioli, A.M.; Mattioli, B.; Medda, E.; Minardi, V.; et al. The Health Equity in All Policies (HEiAP) Approach before and beyond the COVID-19 pandemic in the Italian context. Int. J. Equity Health 2020, 19, 92. [Google Scholar] [CrossRef] [PubMed]
- Brownson, R.C.; Burke, T.A.; Colditz, G.A.; Samet, J.M. Reimagining public health in the aftermath of a pandemic. Am. J. Public Health 2020, 110, 1605–1610. [Google Scholar] [CrossRef]
- Meier, B.M.; Gostin, L.O. A Timely history: Examining the history of the World Health Organization to frame the future of global health governance. Am. J. Public Health 2020, 110, 1592–1594. [Google Scholar] [CrossRef]
- Haldon, J.; Eisenberg, M.; Mordechai, L.; Izdebski, A.; White, S. Lessons from the past, policies for the future: Resilience and sustainability in past crises. Environ. Syst. Decis. 2020, 40, 287–297. [Google Scholar] [CrossRef]
- Chandra, S.; Christensen, J.; Likhtman, S. Connectivity and seasonality: The 1918 influenza and COVID-19 pandemics in global perspective. J. Glob. Hist. 2020, 15, 408–420. [Google Scholar] [CrossRef]
- WHO. Advancing Public Health for Sustainable Development in the WHO European Region; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2018. [Google Scholar]
- United Nations Sustainable Development Goals. Available online: https://sustainabledevelopment.un.org/topics (accessed on 30 December 2021).
- North, D.C. Institutions, Institutional Change, and Economic Performance; Cambridge University Press: Cambridge, UK, 1990. [Google Scholar]
- Kreienkamp, J.; Pegram, T. Governing complexity: Design principles for the governance of complex global catastrophic risks. Int. Stud. Rev. 2021, 23, 779–806. [Google Scholar] [CrossRef]
- Webster, D.G. Beyond the Tragedy in Global Fisheries; MIT Press: Cambridge, MA, USA, 2015. [Google Scholar]
- Garrett, G.; Lange, P. Internationalization, institutions, and political change. Int. Organ. 1995, 49, 627–655. [Google Scholar] [CrossRef]
- Simmons, B.A. Mobilizing for Human Rights: International Law in Domestic Politics; Cambridge University Press: Cambridge, UK, 2009; ISBN 978-0-521-88510-2. [Google Scholar]
- Risse, T.; Ropp, S.C.; Sikkink, K. (Eds.) The Persistent Power of Human Rights: From Commitment to Compliance; Cambridge Studies in International Relations; Cambridge University Press: Cambridge, UK, 2013; ISBN 978-1-107-02893-7. [Google Scholar]
- WHO. Roadmap to Implement the 2030 Agenda for Sustainable Development, Building on Health 2020, the European Policy for Health and Well-Being; World Health Organization Regional Office for Europe: Budapest, Hungary, 2017. [Google Scholar]
- Hammond, M.L. Epidemics and the Modern World; University of Toronto Press: Toronto, ON, Canada, 2020. [Google Scholar]
- Kotar, S.L.; Gessler, J.E. Cholera: A Worldwide History; McFarland & Company, Inc.: Jefferson, NC, USA, 2014. [Google Scholar]
- Snow, J. On the Mode of Communication of Cholera, 1st ed.; Wilson and Ogilvy: London, UK, 1849. [Google Scholar]
- Snow, J. On the Mode and Communication of Cholera, 2nd ed.; John Churchill: London, UK, 1855. [Google Scholar]
- Snowden, F.M. Epidemics and Society: From the Black Death to the Present; Yale University Press: New Haven, CT, USA, 2019. [Google Scholar]
- Sawchuk, L.A.; Tripp, L.; Samakaroon, M. Assessing a Syndemic: Gibraltar in the Time of Cholera. Soc. Sci. Med. 2020, 295, 112956. [Google Scholar] [CrossRef]
- Courtin, E.; Vineis, P. COVID-19 as a Syndemic. Front. Public Health 2021, 9, 1401. [Google Scholar] [CrossRef] [PubMed]
- Caron, R.M.; Adegboye, A.R.A. COVID-19: A Syndemic Requiring an Integrated Approach for Marginalized Populations. Front. Public Health 2021, 9, 515. [Google Scholar] [CrossRef] [PubMed]
- Cohen, G. Climate change calls for a new Hippocratic Oath. Health Affairs, 14 July 2021. [Google Scholar] [CrossRef]
- Wilson, J.; Yan, L.; Wilson, C. The precursors of governance in the maine lobster fishery. Proc. Natl. Acad. Sci. USA 2007, 104, 15212–15217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CGG. Our Global Neighborhood: The Report of the Commission on Global Governance; Oxford University Press: Oxford, NY, USA, 1995. [Google Scholar]
- Mohai, P.; Pellow, D.; Roberts, J.T. Environmental Justice. Annu. Rev. Environ. Resour. 2009, 34, 405–430. [Google Scholar] [CrossRef]
- Jones, C.P. Levels of racism: A theoretic framework and a gardener’s tale. Am. J. Public Health 2000, 90, 1212–1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, O.R. Governing Complex Systems: Social Capital for the Anthropocene; MIT Press: Cambridge, MA, USA, 2017. [Google Scholar]
- CDC Prevention. Available online: https://www.cdc.gov/pictureofamerica/pdfs/Picture_of_America_Prevention.pdf (accessed on 13 October 2020).
- Wen, L.; Sadeghi, N. Addressing racial health disparities in the COVID-19 pandemic: Immediate and long-term policy solutions. Health Affairs, 20 July 2020. [Google Scholar] [CrossRef]
- Green, K.; Zook, M. When talking about social determinants, precision matters. Health Affairs, 29 October 2019. [Google Scholar] [CrossRef]
- Nussbaum, M.; Sen, A. The Quality of Life; Clarendon Press: Oxford, UK, 1993. [Google Scholar]
- Holland, B. Justice and the environment in Nussbaum’s “Capabilities Approach”: Why Sustainable ecological capacity is a meta-capability. Political Res. Q. 2008, 61, 319–332. [Google Scholar] [CrossRef]
- Schiavo, R. Advocacy, community engagement and cross-sectoral collaborations as key strategies during COVID-19 response and beyond: New directions for a new decade. J. Commun. Healthc. 2020, 13, 1–5. [Google Scholar] [CrossRef]
- Witte, K. Putting the fear back into fear appeals: The extended parallel process model. Commun. Monogr. 1992, 59, 329–349. [Google Scholar] [CrossRef]
- Kahneman, D.; Klein, G. Conditions for intuitive expertise: A failure to disagree. Am. Psychol. 2009, 64, 515–526. [Google Scholar] [CrossRef] [Green Version]
- Tversky, A.; Kahneman, D. Judgment under uncertainty: Heuristics and biases. Science 1974, 185, 1124–1131. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Wipfli, H.L.; Samet, J. Framing progress in global tobacco control to inform action on noncommunicable diseases. Health Affairs 2015, 34, 1480–1488. [Google Scholar] [CrossRef] [PubMed]
- Vasterman, P. From Media Hype to Twitter storm: New Explosions and Their Impact on Issues, Crises and Public Opinion; Amsterdam University Press: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Soroka, S.N. Media, public opinion, and foreign policy. Int. J. Press Politics 2003, 8, 27–48. [Google Scholar] [CrossRef]
- Fenichel, E.P. Economic considerations for social distancing and behavioral based policies during an epidemic. J. Health Econ. 2013, 32, 440–451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neuwirth, K.; Dunwoody, S.; Griffin, R.J. Protection motivation and risk communication. Risk Anal. 2000, 20, 721–734. [Google Scholar] [CrossRef] [PubMed]
- Gersovitz, M.; Hammer, J.S. The economical control of infectious diseases. Econ. J. 2004, 114, 1–27. [Google Scholar] [CrossRef]
- Sanghi, A.; Lokshin, M. Can public policy incentivize staying at home during COVID-19? Brookings, 23 April 2020. [Google Scholar]
- Vlaev, I.; King, D.; Darzi, A.; Dolan, P. Changing health behaviors using financial incentives: A review from behavioral economics. BMC Public Health 2019, 19, 1059. [Google Scholar] [CrossRef] [Green Version]
- Young, O.R. The Institutional Dimensions of Environmental Change: Fit, Interplay, and Scale; MIT Press: Cambridge, MA, USA, 2002; ISBN 978-0-262-74024-1. [Google Scholar]
- Axelrod, M.; Flowers, A.; Groff, K.; Novak Colwell, J.M. Governance for conservation risks and crime. In Conservation Criminology; Gore, M.L., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2017. [Google Scholar]
- Albin, C. Negotiating international cooperation: Global public goods and fairness. Rev. Int. Stud. 2003, 29, 365–385. [Google Scholar] [CrossRef]
- Gottfried, M.S.; Trager, R.F. A preference for war: How fairness and rhetoric influence leadership incentives in crises. Int. Stud. Q. 2016, 60, 243–257. [Google Scholar] [CrossRef] [Green Version]
- Bevir, M. How narratives explain. In Interpretation and Method: Empirical Research Methods and the Interpretive Turn; Yanow, D., Schwartz-Shea, P., Eds.; M.E. Sharpe, Inc.: Armonk, NY, USA, 2005; pp. 281–290. [Google Scholar]
- Bayes, R.H.; Grief, A.; Levi, M.; Rsenthal, J.-L.; Weingast, B.R. Analytic Narratives; Princeton University Press: Princeton, NJ, USA, 1998. [Google Scholar]
- Burnstein, E.; Berbaum, M.L. Stages in group decision making: The decomposition of historical narratives. Political Psychol. 1983, 4, 531–561. [Google Scholar] [CrossRef]
- Kunda, Z. The case for motivated reasoning. Psychol. Bull. 1990, 108, 480–498. [Google Scholar] [CrossRef] [PubMed]
- Hallegatte, S. Strategies to adapt to an uncertain climate change. Glob. Environ. Chang. 2009, 19, 240–247. [Google Scholar] [CrossRef]
- Bodansky, D.J. Scientific uncertainty and the precautionary principle. Environment 1991, 33, 43. [Google Scholar]
- Berkes, F. Sacred Ecology: Traditional Ecological Knowledge and Resource Management, 1st ed.; Taylor and Francis: New York, NY, USA, 1999. [Google Scholar]
- Arvai, J.; Gregory, R.; Ohlson, D.; Blackwell, B.; Gray, R. Letdowns, Wake-up calls, and constructed preferences: People’s responses to fuel and wildfire risks. J. For. 2006, 104, 173–181. [Google Scholar]
- Bennet, P.; Calman, K.; Calman, B.P. Risk Communication and Public Health, 2nd ed.; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Cameron, T.A. Updating subjective risks in the presence of conflicting information: An application to climate change. J. Risk Uncertain. 2005, 30, 63–97. [Google Scholar] [CrossRef] [Green Version]
- Douglas, M.; Wildavsky, A. Risk and Culture; University of California Press: Berkeley, CA, USA, 1983. [Google Scholar]
- Sunstein, C.R. Risk and Reason: Safety, Law, and the Environment; Cambridge University Press: Cambridge, UK, 2002. [Google Scholar]
- Groenendyk, E.W. Competing Motives in the Partisan Mind: How Loyalty and Responsiveness Shape Party Identification and Demoracy; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Janis, I.L. Groupthink; Wadsworth Publishing Company: Boston, MA, USA, 1982. [Google Scholar]
- Oreskes, N.; Conway, E.M. Merchants of Doubt: How a Handful of Scientists Obscured the Truth on Issues from Tobacco Smoke to Global Warming, 1st ed.; Bloomsbury Press: New York, NY, USA, 2010; ISBN 9781596916104. [Google Scholar]
- Kuruppu, N.; Liverman, D. Mental preparation for climate adaptation: The role of cognition and culture in enhancing adaptive capacity of water management in Kiribati. Glob. Environ. Chang. 2011, 21, 657–669. [Google Scholar] [CrossRef]
- Armitage, D.; Berkes, F.; Dale, A.; Kocho-Schellenberg, E.; Patton, E. Co-management and the co-production of knowledge: Learning to adapt in Canada’s Arctic. Glob. Environ. Chang. 2011, 21, 995–1004. [Google Scholar] [CrossRef]
- Gómez-Baggethun, E.; Corbera, E.; Reyes-García, V. Traditional Ecological knowledge and global environmental change: Research findings and policy implications. Ecol. Soc. 2013, 18, 72. [Google Scholar] [CrossRef] [Green Version]
- Young, O.R.; Webster, D.G.; Cox, M.E.; Raakjær, J.; Blaxekjær, L.Ø.; Einarsson, N.; Virginia, R.A.; Acheson, J.; Bromley, D.; Cardwell, E.; et al. Moving beyond Panaceas in Fisheries Governance. Proc. Natl. Acad. Sci. USA 2018, 115, 9065–9073. [Google Scholar] [CrossRef] [Green Version]
- Bullard, R.D. The Quest for Environmental Justice; University of California Press: San Francisco, CA, USA, 2005. [Google Scholar]
- Webster, D.G. Scapegoats, silver bullets, and other pitfalls in the path to sustainability. Elem. Sustain. Transit. 2017, 5, 15. [Google Scholar] [CrossRef] [Green Version]
- Krasner, S.D. State power and the structure of international trade. World Politics 1976, 28, 317–347. [Google Scholar] [CrossRef]
- Keohane, R.O.; Nye, J.S. Power and Interdependence, 3rd ed.; Keohane, R.O., Nye, J.S., Eds.; Longman: New York, NY, USA, 2001. [Google Scholar]
- Gorman, S.E.; Gorman, J.M. Denying to the Grave: Why We Ignore the Facts That Will Save Us; Oxford University Press: Oxford, UK, 2017. [Google Scholar]
- Hughes, M. The Victorian London sanitation projects and the sanitation of projects. JPMA 2013, 31, 682–691. [Google Scholar] [CrossRef]
- Jackson, L. Dirty Old London: The Victorian Fight Against Filth; Yale University Press: New Haven, CT, USA; London, UK, 2014. [Google Scholar]
- Luckin, B. Pollution and Control: A Social History of the Thames in the Nineteenth Century; Adam Hilger: Boston, MA, USA, 1986. [Google Scholar]
- Haliday, S. The Great Stink of London; The History Press: Stroud, UK, 2013. [Google Scholar]
- Otter, C. Cleansing and clarifying: Technology and perception in Nineteenth-Century London. J. Br. Stud. 2019, 1930, 40–64. [Google Scholar] [CrossRef]
- Goldman, J.A. Building New York’s Sewers: Developing Mechanisms of Urban Management; Purdue University Press: West Lafayette, IN, USA, 1997. [Google Scholar]
- Caplan, J.M.; Kennedy, L.W.; Neudecker, C.H. Cholera deaths in Soho, London, 1854: Risk terrain modeling for epidemiological investigations. PLoS ONE 2020, 15, e0230725. [Google Scholar] [CrossRef] [Green Version]
- Osborne, J.B. Preparing for the pandemic: City boards of health and the arrival of cholera in Montreal, New York, and Philadelphia in 1832. UHR 2013, 36, 29–42. [Google Scholar] [CrossRef] [Green Version]
- Burrows, E.G.; Wallace, M. Gotham: A History of New York City to 1898; The History of NYC; Oxford University Press: New York, NY, USA, 1999. [Google Scholar]
- Demographia City of New York & Boroughs: Population & Population Density from 1790. Available online: http://www.demographia.com/dm-nyc.htm (accessed on 14 July 2020).
- Demographia Greater London, Inner London Population & Density History. Available online: http://www.demographia.com/dm-lon31.htm (accessed on 14 July 2020).
- Blackmar, E. Accountability for Public Health: Regulating the Housing Market in Nineteenth-Century New York City. In Hives of Sickness; Rosner, D., Ed.; Rutgers University Press: New Brunswick, NJ, USA, 1995; pp. 42–64. [Google Scholar]
- Carwardine, R. The Second great awakening in the urban centers: An examination of methodism and the ‘New Measures’. J. Am. Hist. 1972, 59, 327–340. [Google Scholar] [CrossRef]
- Brown, C.; Harrison, D.; Burns, H.; Ziglio, E. Governance for Health Equity: In the WHO European Region; Updated Reprint 2014; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2014; ISBN 978-92-890-0055-0. [Google Scholar]
- WHO Commission on Social Determinants of Health; World Health Organization (Eds.) Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Commission on Social Determinants of Health Final Report; World Health Organization, Commission on Social Determinants of Health: Geneva, Switzerland, 2008; ISBN 978-92-4-156370-3. [Google Scholar]
- Halpern, S.D.; Truog, R.D.; Miller, F.G. Cognitive bias and public health policy during the COVID-19 pandemic. JAMA 2020, 324, 337. [Google Scholar] [CrossRef]
- Hulme, D. Governing Global quality? Global ambivalence and the millennium development goals. In Global Governance, Poverty and Inequality; Clapp, J., Wilkinson, R., Eds.; Routledge: New York, NY, USA, 2010; pp. 135–161. [Google Scholar]
- Siddiqui, N.; Andrulis, D.; Chapman, D. The COVID-19 crisis: An opportunity to build a fairer, healthier nation. Health Affairs, 24 June 2020. [Google Scholar] [CrossRef]
- Anderies, J.M. Robustness, institutions, and large-scale change in social-ecological systems: The Hohokam of the Phoenix Basin. J. Inst. Econ. 2006, 2, 133–155. [Google Scholar] [CrossRef] [Green Version]
- Allen, C.R.; Holling, C.S. Novelty, adaptive capacity, and resilience. Ecol. Soc. 2010, 15, 24. [Google Scholar] [CrossRef]
- Anderies, J.M.; Janssen, M.A. The fragility of robust social-ecological systems. Glob. Environ. Change 2011, 21, 1153–1156. [Google Scholar] [CrossRef]
- Sen, A. Development as Freedom; Oxford University Press: Oxford, UK, 1999. [Google Scholar]
- Van den Berg, H. Economic Growth and Development, 3rd ed.; World Scientific Publishing Co.: London, UK, 2017. [Google Scholar]
- Easterlin, R.A. Happiness, Growth, and the Life Cycle; Hinte, H., Zimmermann, K.F., Eds.; Oxford University Press: New York, NY, USA, 2010. [Google Scholar]
- Ansell, C.; Gash, A. Collaborative governance in theory and practice. J. Public Adm. Res. Theory 2007, 18, 543–571. [Google Scholar] [CrossRef] [Green Version]
- Bellinson, R.; Chu, E. Learning pathways and the governance of innovations in urban climate change resilience and adaptation. J. Environ. Policy Plan. 2019, 21, 76–89. [Google Scholar] [CrossRef]
- Termeer, C.; Dewulf, A.; van Rijswick, H.; van Buuren, A.; Huitema, D.; Rayner, T.; Wiering, M. The Regional governance of climate adaptation: A framework for developing legitimate, effective, and resilient governance arrangements. Clim. Law 2011, 2, 159–179. [Google Scholar] [CrossRef]
- Dai, X. International Institutions and National Policies; Cambridge University Press: Cambridge, UK, 2007; ISBN 978-0-521-87404-5. [Google Scholar]
- Carlisle, K.; Gruby, R.L. Polycentric systems of governance: A theoretical model for the commons. Policy Stud. J. 2019, 47, 927–952. [Google Scholar] [CrossRef] [Green Version]
- Keohane, R.O.; Ostrom, E. (Eds.) Local Commons and Global Interdependence: Heterogeneity and Cooperation in Two Domains; Sage Publications: London, UK, 1995. [Google Scholar]
- Pearson, A.; Mack, E.; Ross, A.; Marcantonio, R.; Zimmer, A.; Bunting, E.; Smith, A.; Miller, J.; Evans, T. The HWISE Research Coordination Network interpersonal conflict over water is associated with household demographics, domains of water insecurity, and regional conflict: Evidence from nine sites across eight Sub-Saharan African countries. Water 2021, 13, 1150. [Google Scholar] [CrossRef]
- Nickerson, R.S. Confirmation bias: A ubiquitous phenomenon in many guises. Rev. Gen. Psychol. 1998, 2, 175–220. [Google Scholar] [CrossRef]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.M.; Cunha, R.; Mosley, L. Categories, creditworthiness, and contagion: How investors’ shortcuts affect sovereign debt markets. Int. Stud. Q. 2015, 59, 587–601. [Google Scholar] [CrossRef]
- Finucane, M.L.; Alhakami, A.; Slovic, P.; Johnson, S.M. The Affect heuristic in judgments of risks and benefits. J. Behav. Decis. Mak. 2000, 13, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Einhorn, H.J.; Hogarth, R.M. Judging probable cause. Psychol. Bull. 1986, 99, 3–19. [Google Scholar] [CrossRef]
- Kim, H.; Stolte, M.; Humphreys, G.W. The relations between temporal and social perceptual biases: Evidence from perceptual matching. Atten. Percept. Psychophys. 2019, 81, 599–606. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, R. Assessing Risk, Automating racism. Science 2019, 366, 421. [Google Scholar] [CrossRef]
- Strickland, A.A.; Taber, C.S.; Lodge, M. Motivated reasoning and public opinion. J. Health Polit. Policy Law 2011, 36, 935–944. [Google Scholar] [CrossRef] [PubMed]
- Sadler, R.C.; Highsmith, A.R. Rethinking Tiebout: The contribution of political fragmentation and racial/economic segregation to the flint water crisis. Environ. Justice 2016, 9, 143–151. [Google Scholar] [CrossRef] [Green Version]
- Fredrickson, G.M. The Arrogance of Race: Historical Perspectives on Slavery, Racism, and Social Inequality; Wesleyan University Press: Middletown, CT, USA, 1989; ISBN 978-0-8195-6217-3. [Google Scholar]
- Embrick, D.G. Two nations, revisited: The lynching of black and brown bodies, police brutality, and racial control in ‘post-racial’ Amerikkka. Crit. Sociol. 2015, 41, 835–843. [Google Scholar] [CrossRef]
- Moe, T.M. Power and political institutions. Perspect. Politics 2005, 3, 215–233. [Google Scholar] [CrossRef] [Green Version]
- Juarez, P.D.; Matthews-Juarez, P.; Hood, D.B.; Im, W.; Levine, R.S.; Kilbourne, B.J.; Langston, M.A.; Al-Hamdan, M.Z.; Crosson, W.L.; Estes, M.G.; et al. The public health exposome: A Population-based, exposure science approach to health disparities research. Int. J. Environ. Res. Public Health 2014, 11, 12866–12895. [Google Scholar] [CrossRef] [PubMed]
- Nwanaji-Enwerem Jamaji, C.; Jackson, C.L.; Ottinger, M.A.; Cardenas, A.; James, K.A.; Malecki, K.M.C.; Chen, J.-C.; Geller, A.M.; Mitchell, U.A. Adopting a “Compound” Exposome Approach in Environmental Aging Biomarker Research: A Call to Action for Advancing Racial Health Equity. Environ. Health Perspect. 2021, 129, 045001. [Google Scholar] [CrossRef] [PubMed]
- Axelrod, M. Saving Institutional Benefits: Path Dependence in International Law. Ph.D. Thesis, Duke University, Durham, NC, USA, 2008. [Google Scholar]
- Krasner, S.D. Structural Conflict: The Third World against Global Liberalism; University of California Press: Berkeley, CA, USA, 1985. [Google Scholar]
- Baumgartner, F.R.; Jones, B.D. Agenda Dynamics and Policy Subsystems. J. Politics 1991, 53, 1044–1074. [Google Scholar] [CrossRef] [Green Version]
- Jones, B.D.; Baumgartner, F.R. The Politics of Attention: How Government Prioritizes Problems; University of Chicago Press: Chicago, IL, USA, 2005. [Google Scholar]
- Sabatier, P.A. Knowledge, policy-oriented learning, and policy change: An advocacy coalition framework. Knowledge 1987, 8, 649–692. [Google Scholar] [CrossRef]
- Kingdon, J.W. Agendas, Alternatives, and Public Policies, 3rd ed.; Longman: Boston, MA, USA, 2011. [Google Scholar]
- Collier, R.B.; Collier, D. Shaping the Political Arena: Critical Junctures, the Labor Movement, and Regime Dynamics in Latin America; University of Notre Dame Press: Notre Dame, IN, USA, 2002; ISBN 0268017727. [Google Scholar]
- Ikenberry, G.J. After Victory: Institutions, Strategic Restraint, and the Rebuilding of Order after Major Wars; Princeton University Press: Princeton, NJ, USA, 2001; ISBN 978-0-691-05090-4. [Google Scholar]
- Tamarack Institute Collective Impact Self-Assessment Planning Tool. Available online: https://cdn2.hubspot.net/hubfs/316071/Tamarack_New_Website/CI_FIVE_Phases_-_Self_Assessment_Tool.pdf?t=1461695421806&__hstc=&__hssc=&hsCtaTracking=f8530cef-15e0-4fdc-88de-ab7048b28075%7C965d7122-1291-445d-8ef7-797c05d8ba53 (accessed on 30 December 2021).
- Wright, T.R. The Religion of Humanity: The Impact of Comtean Positivism on Victorian Britain; Cambridge University Press: Cambrdge, UK, 1986. [Google Scholar]
- Condran, G.A. Changing Patterns of Epidemic Disease in New York City. In Hives of Sickness; Rutgers University Press: New Brunswick, NJ, USA, 1995; pp. 27–41. [Google Scholar]
- Pellow, D.N. Toward a critical environmental justice studies: Black Lives Matter as an environmental justice challenge. Du Bois Rev. 2016, 13, 221–236. [Google Scholar] [CrossRef] [Green Version]
- WHO Cholera. Available online: https://www.who.int/news-room/fact-sheets/detail/cholera (accessed on 20 July 2020).
- Orata, F.D.; Keim, P.S.; Boucher, Y. The 2010 cholera outbreak in Haiti: How science solved a controversy. PLoS Pathog. 2014, 10, e1003967. [Google Scholar] [CrossRef] [PubMed]
- Federspiel, F.; Ali, M. The cholera outbreak in Yemen: Lessons learned and way forward. BMC Public Health 2018, 18, 1338. [Google Scholar] [CrossRef] [PubMed]
- Dryzek, J.; Pickering, J. Politics of the Anthropocene; Oxford University Press: Oxford, UK, 2019. [Google Scholar]
- Kashwan, P.; Biermann, F.; Gupta, A.; Okereke, C. Planetary justice: Prioritizing the poor in earth system governance. Earth Syst. Gov. 2020, 6, 100075. [Google Scholar] [CrossRef]
- Tatar, M.; Shoorekchali, J.M.; Faraji, M.R.; Wilson, F.A. International COVID-19 vaccine inequality amid the pandemic: Perpetuating a global crisis? J. Glob. Health 2021, 11, 03086. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Nagendra, H.; Shi, P.; Liu, H. Cities: Build networks and share plans to emerge stronger from COVID-19. Nature 2020, 584, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Amicizia, D.; Micale, R.T.; Pennati, B.M.; Zangrillo, F.; Iovine, M.; Lecini, E.; Marchini, F.; Lai, P.L.; Panatto, D. Burden of the typhoid fever and cholera: Similarities and differences. prevention strategies for international travelers to endemic/epidemic areas. J. Prev. Med. Hyg. 2019, 60, E271–E285. [Google Scholar] [CrossRef]
- Atlas, R.M.; Maloy, S. (Eds.) Cholera: Environmental Reservoirs and Impact on Disease Transmission. In One Health: People, Animals, and the Environment; American Society of Microbiology: Washington, DC, USA, 2014; pp. 149–165. ISBN 978-1-55581-842-5. [Google Scholar]
- Dimitrov, R.S.; Sprinz, D.F.; Digiusto, G.M.; Kelle, A. International nonregimes: A research agenda. Int. Stud. Rev. 2007, 9, 230–258. [Google Scholar] [CrossRef] [Green Version]
- Howard-Jones, N. The Scientific Background of the International Sanitary Conferences 1851–1938; World Health Organization: Geneva, Switzerland, 1975; p. 108. [Google Scholar]
- Hanrieder, T. The path-dependent design of international organizations: Federalism in the World Health Organization. Eur. J. Int. Relat. 2014, 21, 215–239. [Google Scholar] [CrossRef] [Green Version]
- Cueto, M.; Brown, T.M.; Fee, E. The World Health Organization: A History; Global Health Histories; Cambridge University Press: Cambridge, UK, 2019; ISBN 978-1-108-48357-5. [Google Scholar]
- WHO. Adelaide Statement on Health in All Policies: Moving towards a Shared Governance for Health and Well-Being; World Health Organization, Government of South Australia: Adelaide, Australia, 2010. [Google Scholar]
- DeSalvo, K.B. Public Health 3.0: A call to action for public health to meet the challenges of the 21st century. Prev. Chronic Dis. 2017, 14, E78. [Google Scholar] [CrossRef] [Green Version]
- Wardle, C.; Derakhshan, H. Information Disorder: Toward an Interdisciplinary Framework for Research and Policymaking; Council of Europe: Strasbourg, France, 2017; p. 109. [Google Scholar]
- Krieger, N. Enough: COVID-19, structural racism, police brutality, plutocracy, climate change—And time for health justice, democratic governance, and an equitable, sustainable future. Am. J. Public Health 2020, 110, 1620–1623. [Google Scholar] [CrossRef] [PubMed]
- MacNairn, E. Health volunteers overseas: A model for ethical and effective short-term global health training in low-resource countries. Glob. Health Sci. Pract. 2019, 7, 344–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stokes, L.C. Short Circuiting Policy: Interest Groups and the Battle over Clean Energy and Climate Policy in the American States; Oxford University Press: Oxford, UK, 2020; ISBN 978-0-19-007429-6. [Google Scholar]
- Jasny, L.S.; Fisher, D.; Dow, D. Why Are We Here? Patterns of Intersectional Motivations across the Resistance. Mobilization Int. Q. 2018, 23, 451–468. [Google Scholar] [CrossRef]
- Mascarenhas, M. (Ed.) Lessons in Environmental Justice; SAGE Publications: Thousand Oaks, CA, USA, 2020. [Google Scholar]
- Ahn, M.J. Combating COVID-19: Lessons from South Korea. Brookings, 13 April 2020. [Google Scholar]
- How NZ’s “team of Five Million” Took on COVID-19. BBC News, 20 April 2020.
- Stone, R. Yemen Was Facing the World’s Worst Humanitarian Crisis. Then the Coronavirus Hit. Available online: https://www.sciencemag.org/news/2020/05/yemen-was-facing-worlds-worst-humanitarian-crisis-then-coronavirus-hit (accessed on 8 June 2020).
- Doucleff, M. How Rich Countries Are “Hoarding” The World’s Vaccines, In Charts. National Public Radio, 3 December 2020. [Google Scholar]
- Von Bogdandy, A.; Villarreal, P. The Role of International Law in Vaccinating against COVID-19: Appraising the COVAX Initiative; Social Science Research Network: Rochester, NY, USA, 2020. [Google Scholar]
- Towhey, M.; Collins, K.; Thomas, K. With First Dibs on Vaccines, Rich Countries Have ‘Cleared the Shelves’. The New York Times, 15 December 2020. [Google Scholar]
- Maxmen, A.; Tollefson, J. Two decades of pandemic war games failed to account for Donald Trump. Nature 2020, 584, 26–29. [Google Scholar] [CrossRef] [PubMed]
- Çakmaklı, C.; Demiralp, S.; Kalemli-Özcan, Ṣ.; Yeşiltaş, S.; Yıldırım, M.A. The Economic Case for Global Vaccinations: An Epidemiological Model with International Production Networks; National Bureau of Economic Research: Cambridge, MA, USA, 2021. [Google Scholar]
- Young, O.R. The behavioral effects of environmental regimes: Collective-action vs social-practice models. Int. Environ. Agreem. 2001, 1, 9–29. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Webster, D.G.; Aytur, S.A.; Axelrod, M.; Wilson, R.S.; Hamm, J.A.; Sayed, L.; Pearson, A.L.; Torres, P.H.C.; Akporiaye, A.; Young, O. Learning from the Past: Pandemics and the Governance Treadmill. Sustainability 2022, 14, 3683. https://doi.org/10.3390/su14063683
Webster DG, Aytur SA, Axelrod M, Wilson RS, Hamm JA, Sayed L, Pearson AL, Torres PHC, Akporiaye A, Young O. Learning from the Past: Pandemics and the Governance Treadmill. Sustainability. 2022; 14(6):3683. https://doi.org/10.3390/su14063683
Chicago/Turabian StyleWebster, D. G., Semra A. Aytur, Mark Axelrod, Robyn S. Wilson, Joseph A. Hamm, Linda Sayed, Amber L. Pearson, Pedro Henrique C. Torres, Alero Akporiaye, and Oran Young. 2022. "Learning from the Past: Pandemics and the Governance Treadmill" Sustainability 14, no. 6: 3683. https://doi.org/10.3390/su14063683
APA StyleWebster, D. G., Aytur, S. A., Axelrod, M., Wilson, R. S., Hamm, J. A., Sayed, L., Pearson, A. L., Torres, P. H. C., Akporiaye, A., & Young, O. (2022). Learning from the Past: Pandemics and the Governance Treadmill. Sustainability, 14(6), 3683. https://doi.org/10.3390/su14063683









