Information Technology Ambidexterity-Driven Patient Agility, Patient Service- and Market Performance: A Variance and fsQCA Approach
Abstract
:1. Introduction
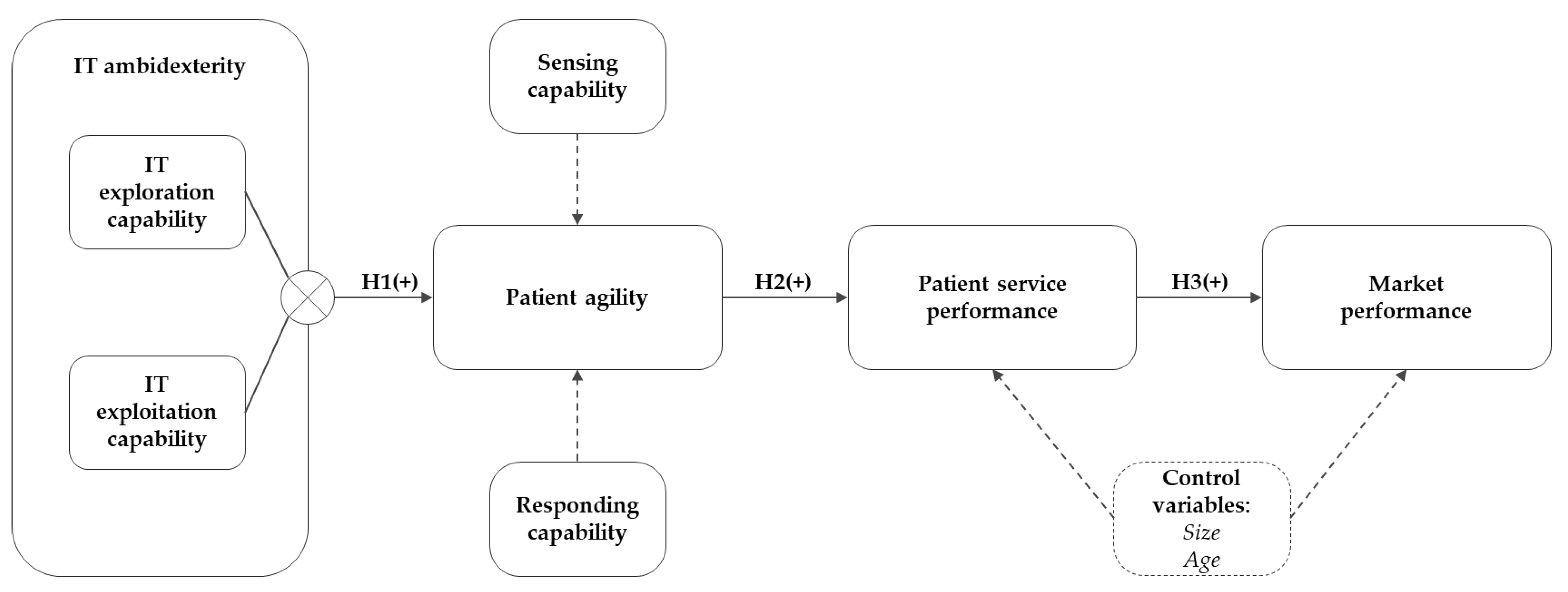
Current Literature Limitations and Research Question
- To what extent does IT ambidexterity affect the hospital departments’ patient agility and, thus, its ability to timely and adequately sense and respond to the patient’s needs and demands? Furthermore;
- What is the role of patient agility in converting the contributions of IT ambidexterity to the department’s patient service and market performance?
2. Theoretical Context
2.1. The Concept of IT Ambidexterity
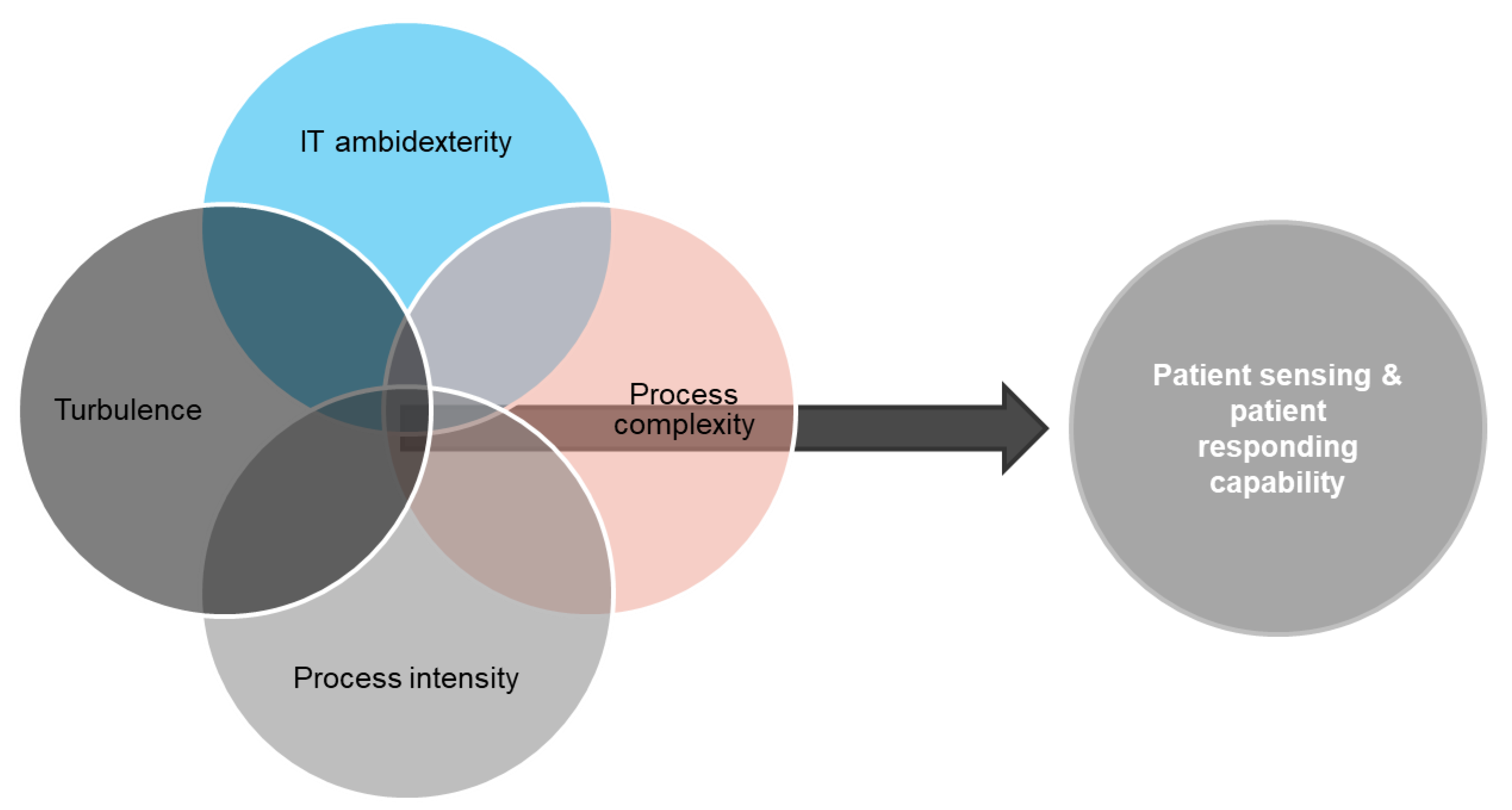
2.2. Dynamic Capabilities View and Patient Agility
2.3. Hypothesis Development
3. Methods
3.1. Data Collection Procedure
3.2. A Composite-Based Approach Using Partial Least Squares SEM
3.3. Measures, Items, and Composite Operationalization
4. Results
4.1. Measurement Model Analyses Using PLS
4.2. Hypotheses Testing
4.3. Configuration Analyses Using fsQCA
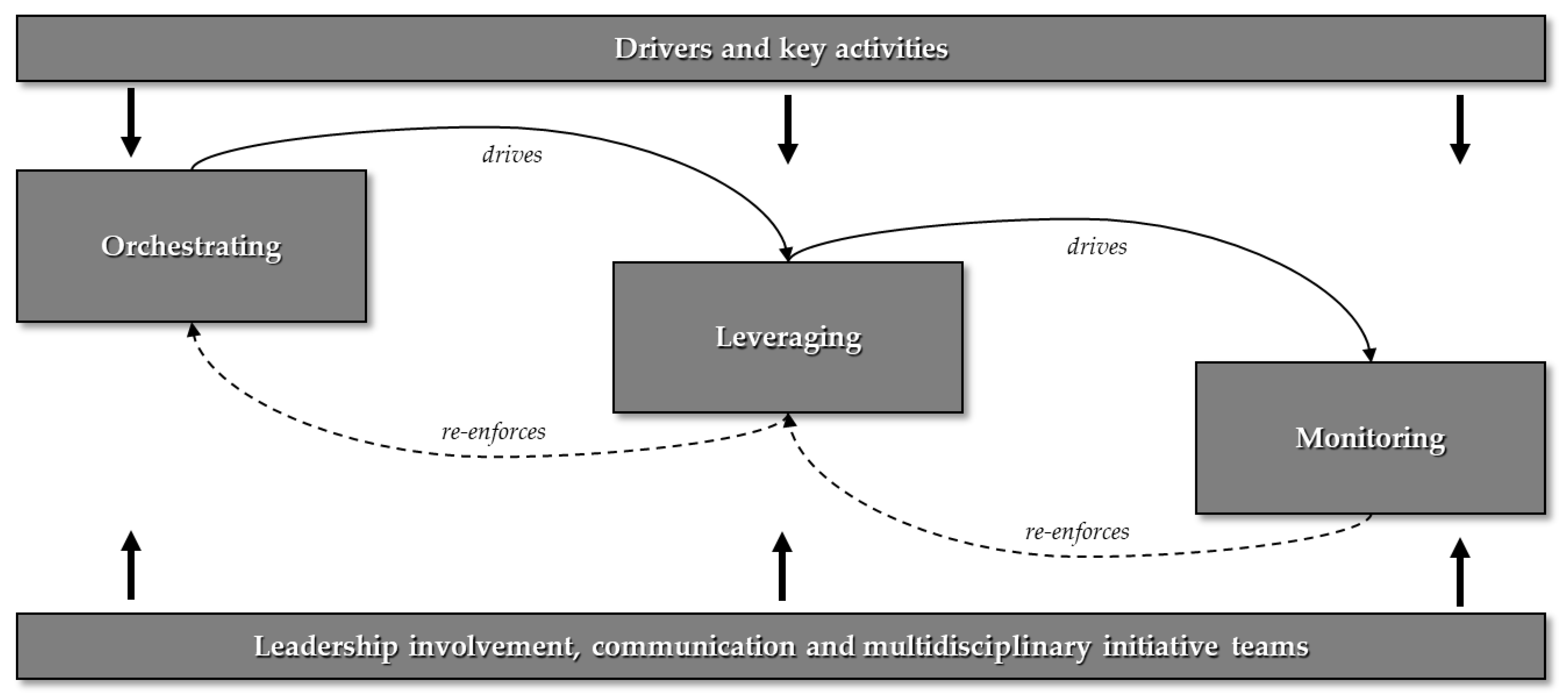
5. A Framework for IT-Driven Patient Agility and Digital Transformation
5.1. Orchestrating IT Capabilities
5.2. Leveraging Patient Agility
5.3. Monitoring Service and Market Value
6. Discussion and Concluding Remarks
6.1. Theoretical Contributions
6.2. Practical Implications
6.3. Limitations and Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lopes, C.M.; Scavarda, A.J.; Vaccaro, G.L.R.; Pohlmann, C.R.; Korzenowski, A.L. Perspective of business models and innovation for sustainability transition in hospitals. Sustainability 2018, 11, 5. [Google Scholar] [CrossRef] [Green Version]
- Walraven, P.; Van de Wetering, R.; Versendaal, J.; Caniëls, M. Using a co-evolutionary is-alignment approach to understand EMR implementations. In Proceedings of the 27th European Conference on Information Systems (ECIS), Stockholm & Uppsala, Sweden, 8–14 June 2019; ISBN 978-1-7336325-0-8. [Google Scholar]
- Kaplan, B. Revisiting health information technology ethical, legal, and social issues and evaluation: Telehealth/telemedicine and COVID-19. Int. J. Med. Inform. 2020, 143, 104239. [Google Scholar] [CrossRef] [PubMed]
- Kohli, R.; Tan, S.S.-L. Electronic health records: How can IS researchers contribute to transforming healthcare? MIS Q. 2016, 40, 553–573. [Google Scholar] [CrossRef]
- Van de Wetering, R. Enhancing clinical decision support through information processing capabilities and strategic IT alignment. In Business Information Systems Workshops; Abramowicz, W., Paschke, A., Eds.; BIS 2018; Lecture Notes in Business Information Processing; Springer: Cham, Switzerland, 2018; Volume 339. [Google Scholar] [CrossRef]
- Wang, Y.; Kung, L.; Gupta, S.; Ozdemir, S. Leveraging big data analytics to improve quality of care in healthcare organizations: A configurational perspective. Br. J. Manag. 2019, 30, 362–388. [Google Scholar] [CrossRef]
- Yin, Y.; Zeng, Y.; Chen, X.; Fan, Y. The internet of things in healthcare: An overview. J. Ind. Inf. Integr. 2016, 1, 3–13. [Google Scholar] [CrossRef]
- The Council for Health & Society. Zorg op afstand dichterbij? Digitale zorg na de coronacrisis. The Council for Health & Society: The Hague, Netherlands, 2020. Available online: https://www.raadrvs.nl/documenten/publicaties/2020/08/27/zorg-op-afstand-dichterbij (accessed on 15 February 2022).
- Foglia, E.; Ferrario, L.; Lettieri, E.; Porazzi, E.; Gastaldi, L. What drives hospital wards’ ambidexterity: Insights on the determinants of exploration and exploitation. Health Policy 2019, 123, 1298–1307. [Google Scholar] [CrossRef] [Green Version]
- Van de Wetering, R.; Versendaal, J.; Walraven, P. Examining the Relationship between a Hospital’s IT Infrastructure Capability and Digital Capabilities: A Resource-Based Perspective. In Proceedings of the Twenty-Fourth Americas Conference on Information Systems (AMCIS), New Orleans, LA, USA, 16–18 August 2018. [Google Scholar]
- Devaraj, S.; Ow, T.T.; Kohli, R. Examining the impact of information technology and patient flow on healthcare performance: A Theory of Swift and Even Flow (TSEF) perspective. J. Oper. Manag. 2013, 31, 181–192. [Google Scholar] [CrossRef]
- Aral, S.; Weill, P. IT assets, organizational capabilities, and firm performance: How resource allocations and organizational differences explain performance variation. Organ. Sci. 2007, 18, 763–780. [Google Scholar] [CrossRef]
- Joshi, K.D.; Chi, L.; Datta, A.; Han, S. Changing the Competitive Landscape: Continuous Innovation Through IT-Enabled Knowledge Capabilities. Inf. Syst. Res. 2010, 21, 472–495. [Google Scholar] [CrossRef]
- van de Wetering, R. IT-Enabled Clinical Decision Support: An Empirical Study on Antecedents and Mechanisms. J. Healthc. Eng. 2018, 2018, 10. [Google Scholar] [CrossRef] [Green Version]
- Asagbra, O.E.; Burke, D.; Liang, H. Why hospitals adopt patient engagement functionalities at different speeds? A moderated trend analysis. Int. J. Med. Informatics 2018, 111, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Van de Wetering, R. IT ambidexterity and patient agility: The mediating role of digital dynamic capability. In Proceedings of the 29th European Conference on Information Systems, Marrakech, Morocco, 14–16 June 2021. [Google Scholar]
- Van de Wetering, R. Achieving digital-driven patient agility in the era of big data. In Proceedings of the I3E: Conference on e-Business, e-Services and e-Society—Responsible AI and Analytics for an Ethical and Inclusive Digitized Society, Galway, Ireland, 1–3 September 2021. [Google Scholar] [CrossRef]
- Agarwal, R.; Selen, W. Dynamic Capability Building in Service Value Networks for Achieving Service Innovation. Decis. Sci. 2009, 40, 431–475. [Google Scholar] [CrossRef]
- Paré, G.; Trudel, M.-C. Knowledge barriers to PACS adoption and implementation in hospitals. Int. J. Med. Inform. 2007, 76, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; Heaton, P.S.; Rudin, R.S.; Schneider, E. Unraveling the IT Productivity Paradox—Lessons for Health Care. New Engl. J. Med. 2012, 366, 2243–2245. [Google Scholar] [CrossRef] [PubMed]
- Lee, O.-K.; Sambamurthy, V.; Lim, K.H.; Wei, K.K. How Does IT Ambidexterity Impact Organizational Agility? Inf. Syst. Res. 2015, 26, 398–417. [Google Scholar] [CrossRef]
- Menachemi, N.; Matthews, M.; Ford, E.W.; Hikmet, N.; Brooks, R.G. The relationship between local hospital IT capabilities and physician EMR adoption. J. Med. Syst. 2008, 33, 329–335. [Google Scholar] [CrossRef]
- Teece, D.; Peteraf, M.; Leih, S. Dynamic Capabilities and Organizational Agility: Risk, Uncertainty, and Strategy in the Innovation Economy. Calif. Manag. Rev. 2016, 58, 13–35. [Google Scholar] [CrossRef] [Green Version]
- Roberts, N.; Grover, V. Investigating firm’s customer agility and firm performance: The importance of aligning sense and respond capabilities. J. Bus. Res. 2012, 65, 579–585. [Google Scholar] [CrossRef]
- Pang, M.-S.; Lee, G.; DeLone, W.H. IT resources, organizational capabilities, and value creation in public-sector organizations: A public-value management perspective. J. Inf. Technol. 2014, 29, 187–205. [Google Scholar] [CrossRef]
- Gerybadze, A. Technological Competence Assessment within the Firm: Applications of Competence Theory to Managerial Practice; Forschungsstelle International Management und Innovation: Stuttgart, Germany, 1998. [Google Scholar]
- Van de Wetering, R.; Versendaal, J. Information technology ambidexterity, digital dynamic capability, and knowledge processes as enablers of patient agility: Empirical study. JMIRx Med. 2021, 2, e32336. [Google Scholar] [CrossRef]
- Overby, E.; Bharadwaj, A.; Sambamurthy, V. Enterprise agility and the enabling role of information technology. Eur. J. Inf. Syst. 2006, 15, 120–131. [Google Scholar] [CrossRef]
- Ministry of Public Health, Welfare and Sport. Healthcare in the Netherlands; Ministry of Public Health: The Hague, Netherlands, 2016. [Google Scholar]
- Di Stefano, G.; Peteraf, M.; Verona, G. The Organizational Drivetrain: A Road To Integration of Dynamic Capabilities Research. Acad. Manag. Perspect. 2014, 28, 307–327. [Google Scholar] [CrossRef] [Green Version]
- Van de Wetering, R. Understanding the Impact of Enterprise Architecture Driven Dynamic Capabilities on Agility: A Variance and fsQCA Study. Pac. Asia J. Assoc. Inf. Syst. 2021, 13, 2. [Google Scholar]
- Van de Wetering, R.; Hendrickx, T.; Brinkkemper, S.; Kurnia, S. The Impact of EA-Driven Dynamic Capabilities, Innovativeness, and Structure on Organizational Benefits: A Variance and fsQCA Perspective. Sustainability 2021, 13, 5414. [Google Scholar] [CrossRef]
- Gibson, C.B.; Birkinshaw, J. The Antecedents, Consequences and Mediating Role of Organizational Ambidexterity. Acad. Manag. J. 2004, 47, 209–226. [Google Scholar]
- March, J.G. Exploration and Exploitation in Organizational Learning. Organ. Sci. 1991, 2, 71–87. [Google Scholar] [CrossRef]
- Tarenskeen, D.; van de Wetering, R.; Bakker, R.; Brinkkemper, S. The Contribution of Conceptual Independence to IT Infrastructure Flexibility: The Case of openEHR. Health Policy Technol. 2020, 9, 235–246. [Google Scholar] [CrossRef]
- Syed, T.A.; Blome, C.; Papadopoulos, T. Impact of IT ambidexterity on new product development speed: Theory and empirical evidence. Decis. Sci. 2020, 51, 655–690. [Google Scholar] [CrossRef]
- Bardhan, I.R. and M.F. Thouin, Health information technology and its impact on the quality and cost of healthcare delivery. Decis. Support Syst. 2013, 55, 438–449. [Google Scholar] [CrossRef]
- He, Z.-L.; Wong, P.K. Exploration vs. Exploitation: An Empirical Test of the Ambidexterity Hypothesis. Organ. Sci. 2004, 15, 481–494. [Google Scholar] [CrossRef]
- Eisenhardt, K.M.; Martin, J.A. Dynamic capabilities: What are they? Strateg. Manag. J. 2000, 21, 1105–1121. [Google Scholar] [CrossRef]
- Drnevich, P.L.; Kriauciunas, A.P. Clarifying the conditions and limits of the contributions of ordinary and dynamic capabilities to relative firm performance. Strat. Manag. J. 2011, 32, 254–279. [Google Scholar] [CrossRef]
- Pavlou, P.A.; El Sawy, O.A. The “third hand”: IT-enabled competitive advantage in turbulence through improvisational capabilities. Inf. Syst. Res. 2010, 21, 443–471. [Google Scholar] [CrossRef]
- Van de Wetering, R. Enterprise architecture resources, dynamic capabilities, and their pathways to operational value. In Proceedings of the ICIS 2019, Munich, Germany, 15–18 December 2019; p. 17. [Google Scholar]
- Sambamurthy, V.; Bharadwaj, A.; Grover, V. Shaping agility through digital options: Reconceptualizing the role of information technology in contemporary firms. MIS Q. 2003, 27, 237–263. [Google Scholar] [CrossRef] [Green Version]
- Chakravarty, A.; Grewal, R.; Sambamurthy, V. Information technology competencies, organizational agility, and firm performance: Enabling and facilitating roles. Inf. Syst. Res. 2013, 24, 976–997. [Google Scholar] [CrossRef]
- Tallon, P.P.; Queiroz, M.; Coltman, T.; Sharma, R. Information technology and the search for organizational agility: A systematic review with future research possibilities. J. Strat. Inf. Syst. 2019, 28, 218–237. [Google Scholar] [CrossRef]
- Setia, P.; University of Arkansas; Venkatesh, V.; Joglekar, S. Leveraging Digital Technologies: How Information Quality Leads to Localized Capabilities and Customer Service Performance. MIS Q. 2013, 37, 565–590. [Google Scholar] [CrossRef] [Green Version]
- Van de Wetering, R.; Versendaal, J. Flexible collaboration infrastructures and healthcare information exchange in hospitals: An empirical resource-based perspective. Int. J. Netw. Virtual Organ. 2020, 23, 171–188. [Google Scholar] [CrossRef]
- Gregory, R.W.; Keil, M.; Muntermann, J.; Mähring, M. Paradoxes and the Nature of Ambidexterity in IT Transformation Programs. Inf. Syst. Res. 2015, 26, 57–80. [Google Scholar] [CrossRef]
- Zhen, J.; Xie, Z.; Dong, K. Impact of IT governance mechanisms on organizational agility and the role of top management support and IT ambidexterity. Int. J. Account. Inf. Syst. 2021, 40, 100501. [Google Scholar] [CrossRef]
- Smith, J.B.; Colgate, M. Customer Value Creation: A Practical Framework. J. Mark. Theory Pr. 2007, 15, 7–23. [Google Scholar] [CrossRef]
- Wu, L.; Hu, Y.-P. Examining knowledge management enabled performance for hospital professionals: A dynamic capability view and the mediating role of process capability. J. Assoc. Inf. Syst. 2012, 13, 976. [Google Scholar] [CrossRef]
- Anderson, J.C.; Narus, J.A.; Van Rossum, W. Customer value propositions in business markets. Harv. Bus. Rev. 2006, 84, 90–99. [Google Scholar] [PubMed]
- Nasution, H.N.; Mavondo, F.T. Organisational capabilities: Antecedents and implications for customer value. Eur. J. Mark. 2008, 42, 477–501. [Google Scholar] [CrossRef]
- Narver, J.C.; Slater, S.F. The effect of a market orientation on business profitability. J. Mark. 1990, 54, 20–35. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, Y.; Nevo, S.; Jin, J.; Wang, L.; Chow, W.S. IT capability and organizational performance: The roles of business process agility and environmental factors. Eur. J. Inf. Syst. 2014, 23, 326–342. [Google Scholar] [CrossRef]
- Salge, T.O.; Vera, A. Hospital innovativeness and organizational performance: Evidence from English public acute care. Health Care Manag. Rev. 2009, 34, 54–67. [Google Scholar] [CrossRef]
- Li, W.; Liu, K.; Yang, H.; Yu, C. Integrated clinical pathway management for medical quality improvement–based on a semiotically inspired systems architecture. Eur. J. Inf. Syst. 2014, 23, 400–417. [Google Scholar] [CrossRef] [Green Version]
- Chakraborty, S.; Bhatt, V.; Chakravorty, T. Impact of IoT adoption on agility and flexibility of healthcare organization. Int. J. Innov. Technol. Explor. Eng. 2019, 8, 2673–2681. [Google Scholar]
- Gordon, S.R.; Tarafdar, M. How do a company’s information technology competences influence its ability to innovate? J. Enterp. Inf. Manag. 2007, 20, 271–290. [Google Scholar] [CrossRef]
- Tang, C.; Lorenzi, N.; Harle, C.A.; Zhou, X.; Chen, Y. Interactive systems for patient-centered care to enhance patient engagement. J. Am. Med. Inform. Assoc. 2016, 23, 2–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGlynn, E.A.; Asch, S.M.; Adams, J.; Keesey, J.; Hicks, J.; DeCristofaro, A.; Kerr, E.A. The Quality of Health Care Delivered to Adults in the United States. N. Engl. J. Med. 2003, 348, 2635–2645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.-Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879. [Google Scholar] [CrossRef]
- Ringle, C.M.; Wende, S.; Becker, J.-M. SmartPLS 3; SmartPLS GmbH: Boenningstedt, Germany, 2015; Available online: http://www.smartpls.com (accessed on 15 February 2022).
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); Sage Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Hair, J.F., Jr.; Sarstedt, M.; Ringle, C.M.; Gudergan, S.P. Advanced Issues in Partial Least squares Structural Equation Modeling; Sage Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Rigdon, E.E.; Sarstedt, M.; Ringle, C.M. On comparing results from CB-SEM and PLS-SEM: Five perspectives and five recommendations. Mark. Zfp 2017, 39, 4–16. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henseler, J. Composite-Based Structural Equation Modeling: Analyzing Latent and Emergent Variables; Guilford Press: New York, NY, USA, 2020. [Google Scholar]
- Becker, J.-M.; Klein, K.; Wetzels, M. Hierarchical Latent Variable Models in PLS-SEM: Guidelines for Using Reflective-Formative Type Models. Long Range Plan. 2012, 45, 359–394. [Google Scholar] [CrossRef]
- Hsu, P.-F. Integrating ERP and e-business: Resource complementarity in business value creation. Decis. Support Syst. 2013, 56, 334–347. [Google Scholar] [CrossRef]
- Schryen, G. Revisiting IS business value research: What we already know, what we still need to know, and how we can get there. Eur. J. Inf. Syst. 2013, 22, 139–169. [Google Scholar] [CrossRef]
- Rodrigues, J.; Ruivo, P.; Oliveira, T. Mediation role of business value and strategy in firm performance of organizations using software-as-a-service enterprise applications. Inf. Manag. 2021, 58, 103289. [Google Scholar] [CrossRef]
- Chen, J.-S.; Tsou, H.-T. Performance effects of IT capability, service process innovation, and the mediating role of customer service. J. Eng. Technol. Manag. 2012, 29, 71–94. [Google Scholar] [CrossRef]
- Rai, A.; Tang, X. Leveraging IT capabilities and competitive process capabilities for the management of interorganizational relationship portfolios. Inf. Syst. Res. 2010, 21, 516–542. [Google Scholar] [CrossRef]
- Kumar, N.; Stern, L.W.; Anderson, J.C. Conducting interorganizational research using key informants. Acad. Manag. J. 1993, 36, 1633–1651. [Google Scholar]
- Fornell, C.; Bookstein, F. Two structural equation models: LISREL and PLS applied to consumer exit-voice theory. J. Mark. Res. 1982, 19, 440–452. [Google Scholar] [CrossRef] [Green Version]
- Fornell, C.; Larcker, D. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Farrell, A.M. Insufficient discriminant validity: A comment on Bove, Pervan, Beatty, and Shiu (2009). J. Bus. Res. 2010, 63, 324–327. [Google Scholar] [CrossRef] [Green Version]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef] [Green Version]
- Kock, N.; Lynn, G. Lateral Collinearity and Misleading Results in Variance-Based SEM: An Illustration and Recommendations. J. Assoc. Inf. Syst. 2012, 13, 546–580. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Fiss, P.C. A set-theoretic approach to organizational configurations. Acad. Manag. Rev. 2007, 32, 1180–1198. [Google Scholar] [CrossRef] [Green Version]
- Rihoux, B.; Ragin, C.C. Configurational Comparative Methods: Qualitative Comparative Analysis (QCA) and Related Techniques; Sage: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Karimi, J.; Somers, T.M.; Bhattacherjee, A. The Role of Information Systems Resources in ERP Capability Building and Business Process Outcomes. J. Manag. Inf. Syst. 2007, 24, 221–260. [Google Scholar] [CrossRef]
- El Sawy, O.A.; Malhotra, A.; Park, Y.; Pavlou, P.A. Research Commentary—Seeking the Configurations of Digital Ecodynamics: It Takes Three to Tango. Inf. Syst. Res. 2010, 21, 835–848. [Google Scholar] [CrossRef]
- Fiss, P.C. Building Better Causal Theories: A Fuzzy Set Approach to Typologies in Organization Research. Acad. Manag. J. 2011, 54, 393–420. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Mezei, J.; Kostakos, V.; Li, H. Applying configurational analysis to IS behavioural research: A methodological alternative for modelling combinatorial complexities. Inf. Syst. J. 2017, 27, 59–89. [Google Scholar] [CrossRef] [Green Version]
- Woodside, A.G. Moving Beyond Multiple Regression Analysis to Algorithms: Calling for Adoption of a Paradigm Shift from Symmetric to Asymmetric Thinking in Data Analysis and Crafting Theory; Elsevier: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Van de Wetering, R.; Mikalef, P.; Helms, R. Driving organizational sustainability-oriented innovation capabilities: A complex adaptive systems perspective. Curr. Opin. Environ. Sustain. 2017, 28, 71–79. [Google Scholar] [CrossRef]
- Ragin, C.C. Qualitative comparative analysis using fuzzy sets (fsQCA). Config. Comp. Methods Qual. Comp. Anal. (QCA) Relat. Tech. 2009, 51, 87–121. [Google Scholar]
- Misangyi, V.F.; Acharya, A.G. Substitutes or Complements? A Configurational Examination of Corporate Governance Mechanisms. Acad. Manag. J. 2014, 57, 1681–1705. [Google Scholar] [CrossRef] [Green Version]
- Ordanini, A.; Parasuraman, A.; Rubera, G. When the recipe is more important than the ingredients: A qualitative comparative analysis (QCA) of service innovation configurations. J. Serv. Res. 2014, 17, 134–149. [Google Scholar] [CrossRef]
- Park, Y.; El Sawy, O.A.; Fiss, P.C. The Role of Business Intelligence and Communication Technologies in Organizational Agility: A Configurational Approach. J. Assoc. Inf. Syst. 2017, 18, 648–686. [Google Scholar] [CrossRef]
- Pappas, I.; Giannakos, M.N.; Sampson, D.G. Fuzzy set analysis as a means to understand users of 21st-century learning systems: The case of mobile learning and reflections on learning analytics research. Comput. Hum. Behav. 2019, 92, 646–659. [Google Scholar] [CrossRef]
- Wu, P.-L.; Yeh, S.-S.; Woodside, A.G. Applying complexity theory to deepen service dominant logic: Configural analysis of customer experience-and-outcome assessments of professional services for personal transformations. J. Bus. Res. 2014, 67, 1647–1670. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.; Ramamurthy, K. Understanding the link between information technology capability and organizational agility: An empirical examination. MIS Q. 2011, 35, 931–954. [Google Scholar] [CrossRef] [Green Version]
- Kim, G.; Shin, B.; Kim, K.; Lee, H.G. IT capabilities, process-oriented dynamic capabilities, and firm financial performance. J. Assoc. Inf. Syst. 2011, 12, 487. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Byrd, T.A. Business analytics-enabled decision-making effectiveness through knowledge absorptive capacity in health care. J. Knowl. Manag. 2017, 21, 517–539. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Ke, W.; Wie, K.K.; Hua, Z. The impact of IT capabilities on firm performance: The mediating roles of absorptive capacity and supply chain agility. Decis. Support Syst. 2013, 54, 1452–1462. [Google Scholar] [CrossRef]
- Sabherwal, R.; Jeyaraj, A. Information Technology Impacts on Firm Performance: An Extension of Kohli and Devaraj (2003). MIS Q. 2015, 39, 809–836. [Google Scholar] [CrossRef]
- Gray, C.S. Seeking Meaningful Innovation: Lessons Learned Developing, Evaluating, and Implementing the Electronic Patient-Reported Outcome Tool. J. Med. Internet Res. 2020, 22, e17987. [Google Scholar] [CrossRef]
- Van Velthoven, M.H.; Cordon, C. Sustainable adoption of digital health innovations: Perspectives from a stakeholder workshop. J. Med. Internet Res. 2019, 21, e11922. [Google Scholar] [CrossRef]
- Papoutsi, C.; Wherton, J.; Shaw, S.; Morrison, C.; Greenhalgh, T. Putting the social back into sociotechnical: Case studies of co-design in digital health. J. Am. Med. Inform. Assoc. 2021, 28, 284–293. [Google Scholar]
| Element | Category | Frequency | Percentage |
|---|---|---|---|
| Hospital type | University medical center | 26 | 28.9% |
| Top clinical training hospital | 37 | 41.1% | |
| General Hospital | 27 | 30% | |
| Department age | 0–5 years | 23 | 21.5% |
| 6–10 years | 17 | 15.9% | |
| 11–20 years | 20 | 18.7% | |
| 21–25 years | 6 | 5.6% | |
| Over 25 years | 24 | 22.4% | |
| Number of patients | <4000 | 25 | 23.4% |
| 4000–6500 | 21 | 19.6% | |
| 6500–9000 | 12 | 11.2% | |
| 9000–11500 | 12 | 11.2% | |
| 11,500–14,000 | 11 | 10.3% | |
| >14,000 | 26 | 24.3% |
| Department | # Responses | % of Total |
|---|---|---|
| General Internal Medicine | 2 | 2% |
| Anesthesiology | 3 | 3% |
| Pharmacy | 1 | 1% |
| Cardiology | 7 | 8% |
| Cardiothoracic surgery | 1 | 1% |
| Surgery | 6 | 7% |
| Dermatology | 3 | 3% |
| Geriatrics | 1 | 1% |
| Infectious diseases | 1 | 1% |
| Intensive Care Adults | 5 | 6% |
| Pediatrics | 8 | 9% |
| Neonatology | 1 | 1% |
| Clinical immunology and rheumatology | 2 | 2% |
| Clinical Oncology | 2 | 2% |
| Lung diseases | 2 | 2% |
| Gastrointestinal and liver diseases | 2 | 2% |
| Neurosurgery | 2 | 2% |
| Neurology | 3 | 3% |
| Kidney diseases | 3 | 3% |
| Ophthalmology | 2 | 2% |
| Orthopedics | 5 | 6% |
| Psychiatry | 2 | 2% |
| Revalidation | 1 | 1% |
| First aid | 4 | 4% |
| Urology | 1 | 1% |
| Vascular medicine | 2 | 2% |
| Obstetrics/Gynecology | 8 | 9% |
| Medical imaging | 5 | 6% |
| Day treatment | 3 | 3% |
| Radiotherapy | 1 | 1% |
| Paramedic | 1 | 1% |
| Total | 90 | 100% |
| Construct | Measurement Item | λ | μ | Std. | Reliability Statistics | ||
|---|---|---|---|---|---|---|---|
| ITEXPLORE | Please indicate the ability of your department to: (1. Strongly disagree–7. Strongly agree) | ||||||
| EXLR1 | Acquire new IT resources (e.g., potential IT applications, critical IT skills) | 0.86 | 4.01 | 1.67 | CA: 0.79 CR:0.86 AVE:0.60 | ||
| EXLR2 | Experiment with new IT resources | 0.92 | 3.81 | 1.62 | |||
| EXLR3 | Experiment with new IT management practices | 0.89 | 3.43 | 1.62 | |||
| ITEXPLOIT | EXPT1 | Reuse existing IT components, such as hardware and network resources | 0.91 | 5.29 | 1.28 | CA:0.85 CR:0.90 AVE:0.68 | |
| EXPT2 | Reuse existing IT applications and services | 0.94 | 5.18 | 1.32 | |||
| EXPT3 | Reuse existing IT skills | 0.95 | 5.13 | 1.25 | |||
| Sensing | Indicate the degree to which you agree or disagree with the following statements about whether the department can: (1–strongly disagree 7–strongly agree) | ||||||
| S1 | We continuously discover additional needs of our patients of which they are unaware | 0.89 | 4.10 | 1.66 | CA:0.89 CR:0.92 AVE:0.71 | ||
| S2 | We extrapolate key trends for insights on what patients will need in the future | 0.77 | 4.43 | 1.63 | |||
| S3 | We continuously anticipate our patients’ needs even before they are aware of them | 0.89 | 4.03 | 1.68 | |||
| S4 | We attempt to develop new ways of looking at patients and their needs | 0.79 | 4.72 | 1.52 | |||
| S5 | We sense our patient’s needs even before they are aware of them | 0.86 | 3.94 | 1.66 | |||
| Responding | R1 | We respond rapidly if something important happens with regard to our patients | 0.93 | 4.52 | 1.50 | CA:0.91 CR:0.93 AVE:0.89 | |
| R2 | We quickly implement our planned activities with regard to patients | 0.91 | 4.52 | 1.42 | |||
| R3 | We quickly react to fundamental changes with regard to our patients | 0.92 | 4.54 | 1.53 | |||
| R4 | When we identify a new patient need, we are quick to respond to it | 0.87 | 4.11 | 1.62 | |||
| R5 | We are fast to respond to changes in our patient’s health service needs | 0.87 | 4.76 | 1.71 | |||
| We perform much better during the last 2 or 3 years than comparable departments from other hospitals in: (1. Strongly disagree–7. Strongly agree). | |||||||
| PSP | PSV1 | Achieving patient satisfaction | 0.83 | 4.98 | 1.32 | CA:0.75 CR:0.85 AVE:0.66 | |
| PSV2 | Providing high-quality service | 0.85 | 5.28 | 1.25 | |||
| PSV3 | Improving the accessibility of medical services | 0.75 | 4.80 | 1.33 | |||
| Market performance | We perform much better during the last 2 or 3 years than comparable departments from other hospitals in: (1. Strongly disagree–7. Strongly agree). | ||||||
| MP1 | Retaining existing patients | 0.76 | 5.25 | 1.36 | CA:0.80 CR:0.86 AVE:0.66 | ||
| MP2 | Attracting new patients | 0.76 | 4.94 | 1.39 | |||
| MP3 | Building a positive branch image | 0.83 | 5.37 | 1.28 | |||
| MP4 | Attaining desired market share | 0.78 | 4.87 | 1.38 | |||
| Assessment of the Fornell-Larcker Criterion | Assessment of HTMT | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 1 | 2 | 3 | 4 | 5 | 6 | |
| 1. EXPLO | 0.94 | 1. EXPLO | ||||||||||
| 2. EXPLR | 0.48 | 0.89 | 2. EXPLR | 0.54 | ||||||||
| 3. PSC | 0.37 | 0.51 | 0.84 | 3. PSC | 0.37 | 0.56 | ||||||
| 4. PRC | 0.30 | 0.33 | 0.52 | 0.90 | 4. PRC | 0.30 | 0.36 | 0.57 | ||||
| 5. PSP | 0.28 | 0.29 | 0.35 | 0.47 | 0.81 | 5. PSP | 0.34 | 0.36 | 0.42 | 0.56 | ||
| 6. MP | 0.24 | 0.17 | 0.11 | 0.12 | 0.57 | 0.85 | 6. MP | 0.29 | 0.22 | 0.17 | 0.14 | |
| Model Path | Path Effect | Confidence Interval | p-Value | t-Value | Outcome |
|---|---|---|---|---|---|
| ITA→PA | 0.48 | CI (0.65–0.77) | <0.001 | 6.48 | H1 Supported |
| PA→PSP | 0.47 | CI (0.12–0.44) | <0.001 | 6.11 | H2 Supported |
| PSP→MP | 0.54 | CI (0.38–0.72) | <0.001 | 7.25 | H3 Supported |
| Mediation analyses | |||||
| ITA→PSP | 0.16 | CI (−0.07–0.37) | 0.15 | 1.45 | Insignificant |
| ITA→PSP (via PA) | 0.19 | CI (0.09–0.30) | <0.001 | 3.40 | Full mediation |
| PA→MP | −1.03 | CI (−0.07–0.37) | 0.32 | 0.99 | Insignificant |
| PA→MP (via PSP) | 0.27 | CI (0.15–0.40) | <0.001 | 4.32 | Full mediation |
| Solutions for Patient Sensing Capability | Solutions for Patient Responding Capability | |||||
|---|---|---|---|---|---|---|
| Configurational Items | I | II | III | IV | V | VI |
| IT ambidexterity | ● | ● | ● | ● | ● | ● |
| Process complexity | ⊗ | ● | ● | |||
| Process intensity | ● | ● | ||||
| Turbulence | ⊗ | ● | ⊗ | |||
| Assessment scores | ||||||
| Raw coverage | 0.472 | 0.227 | 0.335 | 0.315 | 0.411 | 0.421 |
| Unique coverage | 0.157 | 0.091 | 0.066 | 0.0836 | 0.068 | 0.068 |
| Consistency | 0.683 | 0.702 | 0.793 | 0.619 | 0.669 | 0.669 |
| Overall solution consistency | 0.689 | 0.662 | ||||
| Overall solution coverage | 0.649 | 0.602 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van de Wetering, R.; Bosua, R.; Boersma, C.; Dohmen, D. Information Technology Ambidexterity-Driven Patient Agility, Patient Service- and Market Performance: A Variance and fsQCA Approach. Sustainability 2022, 14, 4371. https://doi.org/10.3390/su14074371
van de Wetering R, Bosua R, Boersma C, Dohmen D. Information Technology Ambidexterity-Driven Patient Agility, Patient Service- and Market Performance: A Variance and fsQCA Approach. Sustainability. 2022; 14(7):4371. https://doi.org/10.3390/su14074371
Chicago/Turabian Stylevan de Wetering, Rogier, Rachelle Bosua, Cornelis Boersma, and Daan Dohmen. 2022. "Information Technology Ambidexterity-Driven Patient Agility, Patient Service- and Market Performance: A Variance and fsQCA Approach" Sustainability 14, no. 7: 4371. https://doi.org/10.3390/su14074371
APA Stylevan de Wetering, R., Bosua, R., Boersma, C., & Dohmen, D. (2022). Information Technology Ambidexterity-Driven Patient Agility, Patient Service- and Market Performance: A Variance and fsQCA Approach. Sustainability, 14(7), 4371. https://doi.org/10.3390/su14074371









