Abstract
As of the end of February 2021, more than 420,000,000 confirmed cases of COVID-19 have been reported worldwide, with 5,856,224 deaths. Transmission of the different genetically engineered variants of SARS-CoV-2, which have been isolated since the beginning of the pandemic, occurs from one infected person to another by the same means: the airborne route, indirect contact, and occasionally the fecal–oral route. Infection is asymptomatic or may present with flulike symptoms such as fever, cough, and mild to moderate and severe respiratory distress, requiring hospitalization and assisted ventilation support. To control the spread of COVID-19, the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) have indicated that the appropriate use of personal protective equipment (PPE), as well as the adoption of effective hygiene systems, is one of the primary prevention measures for the entire population. Companies and institutions around the world are therefore trying to find the best ways to reorganize their operations, minimizing the risk of infection among their employees, in order to protect their health and prevent internal outbreaks of SARS-CoV-2, including through the development of new technologies that could also be an innovative and driving factor for the relaunch of companies in a more sustainable, ethically correct, and safe for the health of employees perspective. On the basis of the above premises, in view of the coexistence with SARS-CoV-2 that will most likely accompany us in the coming years, and in view of the vaccination campaign adopted worldwide, the purpose of our narrative review is to update the previous operational protocols with the latest scientific knowledge to be adopted in the workplace even when the emergency crisis is over.
1. Introduction
The coronavirus disease 2019 (COVID-19) outbreak is still attracting global attention. As of December 2021, more than 400,000,000 confirmed cases were recorded worldwide with more than 5,000,000 deaths, one of the most affected geographical areas being the Mediterranean basin, also related to possible climatic factors [1,2].
SARS-CoV-2 was shown to be transmitted mainly through close human-to-human contact, especially via droplets. Of these, the smallest particles containing the virus (known as aerosols with a diameter of fewer than 1 μm) can be left suspended in the air, even travelling long distances [3]. In this context, the Centers for Disease Control and Prevention (CDC) [4] and the World Health Organization (WHO) [5] have called for increasing attention and effective mitigation strategies, especially in indoor public spaces such as restaurants, offices, cinemas, schools, etc. SARS-CoV-2 is also transmitted by contact with infected persons or by drips containing the virus, hugging or inanimate surfaces [6]; the droplets, contaminating the hands, can subsequently enter the body through the mouth, nose, and the mucous membranes of the eyes [7].
The infection usually does not present any visible symptoms, or could have mild flu symptoms and respiratory distress ranging from mild–moderate to severe, requiring hospitalization and support by assisted ventilation [8]. It is believed that the latter symptomatology occurs in those who, although young, have a poorly active immune system because they are undergoing acute or chronic immunosuppressive therapy, are genetically predisposed [9], or have an excessive psychophysical environmental workload. For example, the development of organic diseases or the generation of addictions [10] has been observed in subjects who perform heavy work [11] or work that impairs the normal circadian rhythm by working at night, such as nurses or night watchmen, which may be the basis for a lowering, albeit transitory, of immune defenses [12].
In order to control the spread of COVID-19, authorities in the last two years have provided several prevention and protection guidelines, both for the general population and for those who, such as healthcare workers, are more likely to come into contact with the virus. The WHO and CDC have indicated that the appropriate use of personal protective equipment (PPE) [13,14] is one of the primary prevention measures for the whole population. Wearing a face mask or face shield in enclosed public spaces or transport has also been introduced as a mandatory recommendation or rule in more than 70 countries worldwide [15].
PPE used in the prevention of COVID-19 mainly includes filtering masks, face shield/visors, goggles, gloves, and gowns [16]. Apart from gloves and gowns, other PPE is mainly used to protect the facial area and its mucous membranes (nose, eyes, and mouth) from splashes and splashes of body fluids during medical procedures or from aerosols during breathing, coughing, and speaking.
Since December 2020, the advent of vaccines and their spread to almost the entire population of industrialized countries has gradually changed the pandemic scenario for the better, allowing a gradual return to normality [17].
Based on these premises, in view of the coexistence with SARS-CoV 2 that will most likely accompany us in the coming years, and for the revival of companies, which have suffered the devastating economic effects of the pandemic, the purpose of our technical review is to update and simplify our previous operational protocol, also in a more sustainable, ethically correct and safe way for the health of employees, with the latest scientific knowledge to be adopted in the workplace, even when the emergency crisis is over [18].
2. Materials and Methods
For the update of our previous protocol, we analyzed the most recent guidelines based on the study of the effects that the epidemic has caused in the world until now. We also reviewed clinical evaluations of various respiratory tract personal protective equipment (EPP) and epidemiological data on SARS-CoV-2. The main WHO reports were taken into account, as well as those of the Food and Drug Administration and AIFA. Finally, from the main databases used by the scientific community, PubMed and Google Scholar, approximately 210 articles relevant to our research were selected (last accessed in January 2022). The papers analyzed were from late 2020 to January 2022, with topics always related to prevention, PPE, and SARS-CoV-2 transmission routes.
3. Prevention and Protection
Companies and institutions around the world are trying to find the best ways to reorganize their operations, minimizing the risk of contagion among their employees, in order to protect their health and prevent internal outbreaks of SARS-CoV-2, including through the development of new technologies that facilitate social distancing, even in the workplace [19].
3.1. Organizational Measures
Organizational prevention and protection measures aim to reduce the probability of being exposed to SARS-CoV-2. These measures, which mainly consist of detecting body temperature upon entering the company or the presence of flulike symptoms, thus allowing an early diagnosis of the worker who is positive for SARS-CoV-2 [20], have been implemented by the adoption of additional computerized control systems, such as those related to the execution of the swab in the 48 h preceding, or in the verification of the validity of the planned vaccination cycle; measures, among others, made mandatory by specific ministerial decrees [21,22].
The measures to be taken are:
- Control of green pass or green pass reinforced by vaccination or cure until revoked;
- Selective measurement in order to control the possible pyrexia to all the collaborators, including external ones;
- Cutting the staff in order to avoide closeness between people;
- Composition, if possible, of different closed and independent working groups;
- Adoption, where possible, and following ministerial guidelines of smart working;
- Preparation and adherence to protocols for dressing and stripping PPE;
- Creation of specific access and exit routes from workplaces to avoid possible contamination.
3.2. Environmental Measures
Environmental measures include the use of specific chemicals that were shown to be effective in cleaning and sanitizing enclosed spaces where it is suspected that organic traces containing SARS-CoV-2 may be present. Among these substances, those that have been found to be most effective include the use of chemical solutions made by different substances based on sodium hypochlorite (0.1–0.5%), ethanol (62–71%) or hydrogen peroxide (0.5%). Another measure is to ensure adequate ventilation of enclosed spaces for a sufficient period of time [23].
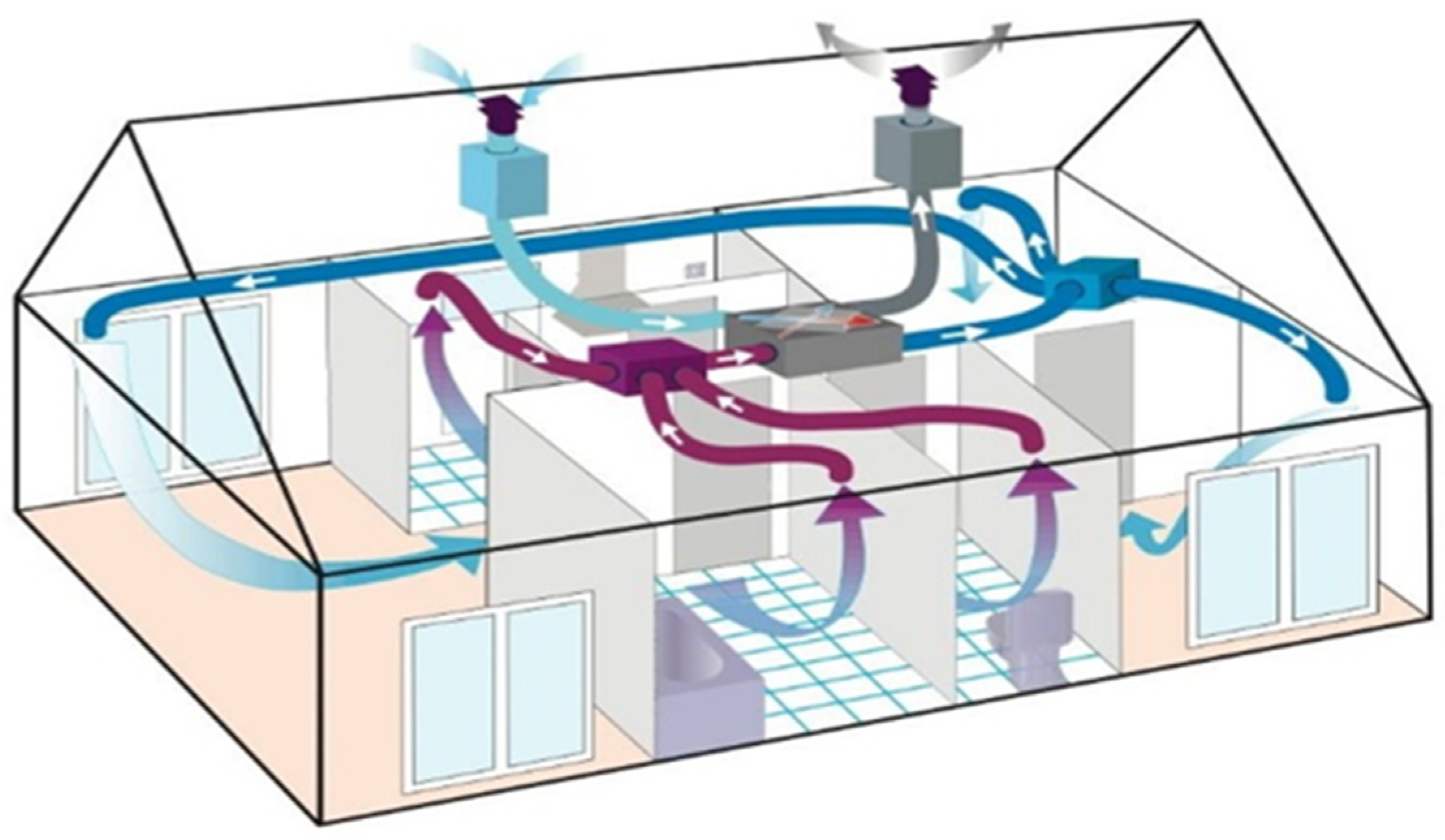
Additional effective environmental measures have proved to be those involving periodic air exchange, including mechanical aids such as specific ventilation systems, which are most effective in increasing air exchange and significantly decreasing the risk of contamination (Figure 1). For this reason, an Italian study suggests that efficient ventilation systems, compared with natural air exchange, can reduce the transmission of COVID-19 in schools by more than 80%, as well as improve air quality in terms of environmental contaminants and carbon dioxide concentration [24].
Figure 1.
Diagram of correct circuit for air exchange.
Lastly, the use of suitable instruments for sanitizing environments using chemical–physical agents is becoming increasingly popular, including ozone gas, which has proved effective in removing pathogens including SARS-CoV-2 [25], the use of UV-C irradiation or dry heat treatment for the inactivation of both SARS-CoV-2 (Table 1) and other pathogens that could contaminate surfaces and PPE [26].

Table 1.
List of chemical and physical disinfectants active on viruses and their relative areas of application.
3.3. Personal Measures
3.3.1. Hand Washing
To avoid the indirect transmission of SARS-CoV-2, it is important to wash your hands properly, as they represent an indirect means of infection. It is recommended to wash them with soap and water for about one minute or, alternatively, to sanitize them with 62–71% alcohol-based solutions [27].
Hands should be washed:
- At the beginning of the shift, especially if it is a contact with the public;
- After contact with other staff or customers;
- After contact with any biological fluid;
- After contact with potentially contaminated objects (gloves, clothing, masks, used fabrics, and waste);
- Immediately after removing gloves and other protective equipment.
Moreover, remember not to touch the mucous membranes with your hands unless they have been washed and disinfected. Although SARS-CoV-2 is transmitted mainly by respiratory route, it can also enter the body through mucous membranes coming into contact with contaminated surfaces [28].
3.3.2. Personal Protective Equipment (PPE)
Gloves
Only use products that comply with the requirements of the technical standard EN 374, which categorizes such PPE as third class for protection against specific pathogens (CE marking must be present to identify them as PPE) [29].
Disposable protective gloves made of nitrile are made with a composition based on butadine and acrylonitrile; they cause few allergic reactions and due to their properties can be used in different professional activities.
Indications for the use of gloves:
- Must be worn properly and removed immediately after use;
- They must be intact and have no cuts on the surface;
- Decontamination of gloves before removal with hypochlorite, after any contact with other inanimate surfaces, and during undressing procedures [30].
Disposable Masks/Respirators
As the pandemic situation continues, several studies have been carried out on the suitability of filtering masks [31], which have assessed two main factors regarding their effectiveness: the degree of filtration of the material and the fit.
With regard to the degree of filtration, there are several standards adopted worldwide, the one of the U.S. National Institute for Occupational Safety and Health (NIOSH) being one of the most considered and reliable; this system evaluates the degree of filtration as a percentage of inhalable particles moving in and out [32].
The second parameter of the filtering masks evaluated is that of fit, in terms of the possibility to adhere to the shape of the face with a negative pressure that allows the filtration of the air, especially at the entry point. In this regard, several design characteristics of the masks, both surgical and FFP2/N95, were analyzed [33].
Disposable Surgical Masks
Disposable masks (surgical masks) are made up of three layers: the outer layer with filtering action, the middle layer, and the inner layer, which allows the passage of air but prevents the passage of liquids. This last one, in contact with the skin, has at the top end a metal wire that makes the device adaptable to the physiognomy of the face; it is held in place by elastic bands [34]. These devices protect the nose and mouth against contamination by particles with an average diameter of 4.5 µm [35]. Although they stem from the need to protect the patient (surgical operations and aseptic maneuvers), they have also been observed to be useful in preventing operators from contacting infected biological fluids [36].
Overall, surgical masks provide a good fit and filtering capacity for some community contexts but are lacking in particular production cycles where the use of FFP2/N95 or FFP3 masks is more appropriate to reduce the possibility of SARS-CoV-2 transmission.
The use of a surgical mask is recommended:
- In technical and administrative support activities.
Filtering Face Piece (FFP)
The term filtering face piece (FFP) is used for high-performance filtering masks. Filtration is provided by the use of complex polypropylene microfibres, and these masks are used to filter vapors, dust particles, and infectious agents. Compared with other types of filtering masks, they have the advantage of purifying the air and reducing the risk of contamination for the wearer, protecting against the inhalation of particulate material such as dust, droplets, and aerosols [37].
There are three categories of protection among FFP masks: FFP1 filters at least 80% of airborne particles, FFP2 filters at least 94% of airborne particles, and finally FFP3, which provides a more durable precautionary aspect with a filtration degree of at least 98% of airborne particles and an inward leakage of less than 2% [38].
FFP2, according to NIOSH, are identified by the designation N95. The designation “95” means that, when tested, the respirator blocks at least 95 per cent of particles with a little size (0.3 μm) upon entry or exit. This test is carried out at flow rates of 85 L/min, which simulates a high work rate, which is an order of magnitude higher than resting or low-intensity breathing, and these tests are carried out under more severe conditions than can be encountered in a working environment, so that particles that are much smaller than those carrying viruses are used at flow rates much higher than those normally seen in working environments [39].
For these reasons, FFP2 masks, which are already compulsory in Italy in means of transport and in many indoor activities according to the Legislative Decree of 24 December 2021, no. 221, should be compulsorily used in workplaces with several employees and where social distancing or ventilation of the rooms may often be lacking due to particular production cycles [40].
FFP3 protective masks are the only masks that are strongly recommended for use by people working in healthcare settings, especially those working in close contact with COVID-19-positive patients, or performing procedures where either aerosols are generated or close contact with a high risk of infection occurs, such as performing spirometry or performing manoeuvres such as intubation or surgical practices. Such PPE is believed to provide almost 99% protection from inhalation of particles between 100 and 5000 nm [41,42].
Safety Glasses and Spray Visor
Different bacterial and viral pathogens can enter the body through the conjunctiva, so it is necessary to protect the eyes from potential exposure to such viruses by using specific PPE certified by the technical standard EN 166 to prevent contact with infected biological material [43]. These protective devices should be used whenever there is potentially close contact with a suspected case, particularly when the potentially infected person is not wearing a surgical mask that could reduce the spread of viruses into the environment. It is important to decontaminate them after use, as they can act as a SARS-CoV-2 transmission vectors on their own [44]. All PPE described above must be removed and disposed of following the correct procedures by the user.
Isolation Clothing
Disposable insulating garments have the function of preventing the penetration of biological liquids, and are combined with impenetrable materials such as plastic films. They can be produced using a variety of nonwoven technologies (thermal, chemical or mechanical) to provide integrity and strength [45].
4. Discussion
In view of the now ubiquitous spread of the virus which no longer favors particular areas or geographical regions, but which is also common to the Mediterranean basin area due to possible climatic factors, the assessment of the biological risk from SARS-CoV-2 is carried out, almost exclusively, on the basis of the type of work carried out. For companies where biological agents are deliberately used, such as research laboratories, or where there is a possibility of high exposure related to the type of activity carried out, such as health care facilities [46], the employer should carry out a risk assessment also for this factor, updating the DVR with all the necessary prevention and protection measures to ensure the control of exposure to this risk [47], as well as integrating a health protocol, adding to the screening health examinations to be carried out on all workers in the same homogeneous group [48], such as further diagnostic examinations in relation to SARS-COV-2, such as antibody quantification, which has been shown to be predictive in assessing the degree of protection, even over long periods, against SARS-CoV-2 [49,50].
In jobs where the risk of exposure to SARS-CoV-2 is not directly related to the activity carried out but is correlated to all the other specific conditions of the epidemiological context, this risk is to be considered generic or aggravated generic, for example in all industrial activities where the omnipresent use of machinery exposes workers to a greater risk of accidents requiring rescue and close contact [51]. In these production activities, it is therefore sufficient for the preventive measures indicated by the health authorities to be taken in order to contain the spread of the virus, keeping track of it through a special annex to the DVR [52]. Having said this, it is necessary to integrate the information according to the type of activity carried out, with the frequency of possible contacts with external personnel (customers, collaborators or suppliers) and the ability to maintain the correct social distance. Companies can be divided into:
- Companies with low risk:
- ○
- Performing mainly in an office with reduced contact with the public.
- Companies with medium risk:
- ○
- Carrying out mainly commercial activities;
- ○
- Where employees have contact with customers;
- ○
- Performing front-office activities;
- ○
- Places of education such as schools and universities;
- ○
- With frequent travelling personnel.
- High-risk companies:
They are those operating in the health sector, where SARS-CoV-2 is assessed as a specific risk, also in relation to the high degree of stress and tension characteristic of these activities during the pandemic [53]. In these companies, the exposed workers are: healthcare workers (doctors, nurses, dentists, paramedics, emergency medical technicians, etc.), especially if they perform specific procedures in which droplets or aerosols may be generated (such as intubation, cough induction procedures, performing spirometry examinations, etc.), healthcare or laboratory staff collecting or handling biological samples, or morgue workers performing autopsies [54].
On the basis of the above, we have proposed, in Table 2, a summary of the proposed prevention and protection measures according to the risk level of the company:

Table 2.
Summary of the prevention and protection measures proposed according to the risk level.
5. Conclusions
The experience accumulated over the two years of the pandemic has made it possible to address with greater scientific certainty which prevention systems can be adopted in the workplace. Moreover, the advantages brought about by the large-scale use of a vaccine that is effective both in reducing contagions and in drastically reducing the hospitalization of those infected with SARS-CoV-2 have favorably changed the initial scenario of the pandemic.
The widespread use of PPE, including FFP2 masks, even outside workplaces, has ensured greater control of the spread of the virus among the population.
The constant cleaning of workplaces with the indicated detergents has become a practice that has certainly drastically decreased the possible presence of the virus in workplaces, as has the use of additional sanitation and hygiene systems, which in these two years of the pandemic has become increasingly frequent in those activities where the risk from SARS-CoV-2 is specific, such as in hospitals and laboratories. Systems to improve the natural exchange of air have also proved to be very effective, especially in those environments that are particularly crowded such as front offices, classrooms, meeting rooms, and gyms.
Among the organizational measures indicated, it should be noted that checking the regularity of vaccination, or taking a swab within the last 48 h, are effective tools for significantly reducing the risk of infection. Constant measurement of body temperature or the presence of symptoms such as colds or coughs, considering that the period in which there is maximum infectious power coincides with the symptomatic period, is a rule that, although no longer compulsory and of certain effectiveness, can continue to be used as a further measure to exclude those who, despite meeting the requirements for certification, may be positive for the virus and showing mild symptoms.
An organizational measure that proved to be highly effective was the composition of different closed and independent work groups to enable the company in the event of the presence of an employee who tested positive for SARS-CoV-2 to isolate only one work group, placing it in a possible state of self-monitoring or home quarantine in accordance with the regulations in force in the event of an infection.
Author Contributions
Conceptualization and management, E.C. and L.C.; methodology, F.P. and D.M.; investigation, E.V., C.L. and G.L.; writing, D.V., A.A. and S.Z.; resources, L.C., F.P., V.R. and C.L.; writing—original draft, D.M. and F.P.; supervision and revision, E.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 14 January 2022).
- Costantino, C.; Cannizzaro, E.; Alba, D.; Conforto, A.; Cimino, L.; Mazzucco, W. SARS-CoV-2 pandemic in the mediterranean area: Epidemiology and perspectives. EuroMediterranean Biomed. J. 2020, 15, 102–106. [Google Scholar]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.; Lau, E.H.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Phelan, A.L.; Katz, R.; Gostin, L.O. The Novel Coronavirus Originating in Wuhan, China. JAMA 2020, 323, 709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- Tellier, R.; Li, Y.; Cowling, B.J.; Tang, J.W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019, 19, 101. [Google Scholar] [CrossRef]
- Cannizzaro, E.; Lo Coco, D.; Lo Coco, G. Post-traumatic stress disorder: A frequent work-related illness. Euromediterranean Biomed. J. 2012, 7, 101–108. [Google Scholar]
- Cannizzaro, E.; Ramaci, T.; Cirrincione, L.; Plescia, F. Work-Related Stress, Physio-Pathological Mechanisms, and the Influence of Environmental Genetic Factors. Int. J. Environ. Res. Public Health 2019, 16, 4031. [Google Scholar] [CrossRef] [Green Version]
- Plescia, F.; Cirrincione, L.; Martorana, D.; Ledda, C.; Rapisarda, V.; Castelli, V.; Martines, F.; Vinnikov, D.; Cannizzaro, E. Alcohol Abuse and Insomnia Disorder: Focus on a Group of Night and Day Workers. Int. J. Environ. Res. Public Health 2021, 18, 13196. [Google Scholar] [CrossRef]
- Cannizzaro, E.; Plescia, F.; Cirrincione, L.; Lo Pinto, E.; Plescia, F. Sport for job. differences in cortisol levels in a water polo team at different times of workout. Euromediterranean Biomed. J. 2018, 13, 181–184. [Google Scholar]
- Cannizzaro, E.; Cirrincione, L.; Mazzucco, W.; Scorciapino, A.; Catalano, C.; Ramaci, T.; Ledda, C.; Plescia, F. Night-Time Shift Work and Related Stress Responses: A Study on Security Guards. Int. J. Environ. Res. Public Health 2020, 17, 562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations during Severe Shortages. Available online: https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages (accessed on 12 January 2022).
- CDC: Guidance for the selection and Use of Personal Protective Equipment (PPE) in Health care Settings. Available online: https://www.cdc.gov/hai/prevent/ppe.html (accessed on 16 January 2022).
- Zhang, M.Q.; Wang, X.H.; Chen, Y.L.; Zhao, K.L.; Cai, Y.Q.; An, C.L.; Lin, M.G.; Mu, X.D. Clinical features of 2019 novel coronavirus pneumonia in the early stage from a fever clinic in Beijing. Chin. J. Tuberc. Respir. Dis. 2020, 43, 13. [Google Scholar]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- COVID-19 and Vaccines: The Numbers in Italy and in the World. Available online: https://www.sanitainformazione.it/uncategorized/la-diffusione-del-coronavirus-in-tempo-reale/ (accessed on 9 January 2022).
- Cirrincione, L.; Plescia, F.; Ledda, C.; Rapisarda, V.; Martorana, D.; Moldovan, R.E.; Theodoridou, K.; Cannizzaro, E. COVID-19 pandemic: Prevention and protection measures to be adopted at the workplace. Sustainability 2020, 12, 3603. [Google Scholar] [CrossRef]
- Cannizzaro, E.; Cirrincione, L.; Plescia, F.; Moldovan, R.E.; Rapisarda, V. Development and validation in a group of industry workers, of an application for audiometric screening: A solution for social distance during COVID-19 emergency. Euromediterranean Biomed. J. 2020, 15, 175–181. [Google Scholar]
- Vitale, E.; Vella, F.; Filetti, V.; Cirrincione, L.; Indelicato, G.; Cannizzaro, E.; Rapisarda, V. How to Prevent SARS-CoV-2 Transmission in the Agri-Food Industry during the First Pandemic Wave: Effects on Seroprevalence. Appl. Sci. 2021, 11, 10051. [Google Scholar] [CrossRef]
- DECREE-LAW No. 1 of 7 January 2022 (Collection 2022) Urgent Measures to Deal with the COVID-19 Emergency, Particularly in Workplaces, Schools and Higher Education Institutions. (22G00002) (OJ General Series n.4 of 07-01-2022). Available online: https://www.gazzettaufficiale.it/eli/id/2022/01/07/22G00002/sg (accessed on 5 January 2022).
- Decree of The President of the Council of Ministers of 21 January 2022 Identification of the Essential and Primary Needs for the Satisfaction of which the Possession of one of the COVID-19 Green Certifications is not Required. (22A00555) (OJ General Series n.18 of 24-01-2022). Available online: https://www.gazzettaufficiale.it/eli/id/2022/01/24/22A00555/sg (accessed on 30 January 2022).
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef] [Green Version]
- Italian Study Shows Ventilation Can Cut School COVID Cases by 82%. Available online: https://www.reuters.com/world/europe/italian-study-shows-ventilation-can-cut-school-covid-cases-by-82-2022-03-22/ (accessed on 10 March 2022).
- Irie, M.S.; Dietrich, L.; Souza, G.L.; Soares, P.B.F.; Moura, C.C.G.; Silva, G.R.D.; Paranhos, L.R. Ozone disinfection for viruses with applications in healthcare environments: A scoping review. Braz. Oral. Res. 2022, 36, e006. [Google Scholar] [CrossRef]
- Harfoot, R.; Yung, D.B.Y.; Anderson, W.A.; Wild, C.E.K.; Coetzee, N.; Hernández, L.C.; Lawley, B.; Pletzer, D.; Derraik, J.G.B.; Anderson, Y.C.; et al. Ultraviolet-C Irradiation, Heat, and Storage as Potential Methods of Inactivating SARS-CoV-2 and Bacterial Pathogens on Filtering Facepiece Respirators. Pathogens 2022, 11, 83. [Google Scholar] [CrossRef]
- Prevent Infections with Proper Hand Washing. Available online: https://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?menu=notizie&id=4061 (accessed on 15 January 2022).
- General Directorate of Health Prevention. FAQ-Covid-19, Questions and Answers. March 2020. Article Published on ‘Governo.it’. Available online: http://www.salute.gov.it/portale/malattieInfettive/detailFaqMalattieInfettive.jsp?lingua=italiano&id=228 (accessed on 15 March 2020).
- Norm EN 374. 2016. Available online: https://www.uni3servizi.it/2019/07/23/en-iso-374-1-2016/ (accessed on 3 March 2020).
- Casanova, L.M.; Teal, L.J.; Sickbert-Bennett, E.E.; Anderson, D.J.; Sexton, D.J.; Rutala, W.A.; Weber, D.J.; Program, T.C.P.E. Assessment of Self-Contamination during Removal of Personal Protective Equipment for Ebola Patient Care. Infect. Control Hosp. Epidemiol. 2016, 37, 1156–1161. [Google Scholar] [CrossRef]
- Seidi, F.; Deng, C.; Zhong, Y.; Liu, Y.; Huang, Y.; Li, C.; Xiao, H. Functionalized Masks: Powerful Materials against COVID-19 and Future Pandemics. Small 2021, 17, e2102453. [Google Scholar] [CrossRef] [PubMed]
- Corbin, J.C.; Smallwood, G.J.; Leroux, I.D.; Norooz Oliaee, J.; Liu, F.; Sipkens, T.A.; Green, R.G.; Murnaghan, N.F.; Koukoulas, T.; Lobo, P. Systematic experimental comparison of particle filtration efficiency test methods for commercial respirators and face masks. Sci. Rep. 2021, 11, 21979. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef] [PubMed]
- Norm EN 14683. 2019. Available online: https://www.certifico.com/normazione/234-documenti-riservati-normazione/10435-uni-en-14683-requisiti-maschere-facciali-uso-medico-marcate-ce (accessed on 18 December 2021).
- Booth, C.M.; Clayton, M.; Crook, B.; Gawn, J. Effectiveness of surgical masks against influenza bioaerosols. J. Hosp. Infect. 2013, 84, 22–26. [Google Scholar] [CrossRef]
- Van der Sande, M.; Teunis, P.; Sabel, R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS ONE 2008, 3, e2618. [Google Scholar] [CrossRef] [Green Version]
- Das, S.; Sarkar, S.; Das, A.; Das, S.; Chakraborty, P.; Sarkar, J. A comprehensive review of various categories of COVID-19 resistant masks. Clin. Epidemiol. Global Health 2021, 12, 100835. [Google Scholar] [CrossRef]
- Tcharkhtchi, A.; Abbasnezhad, N.; Zarbini Seydani, M.; Zirak, N.; Farzaneh, S.; Shirinbayan, M. An overview of filtration efficiency through masks: Mechanisms of aerosol penetration. Bioact. Mater. 2021, 6, 106–122. [Google Scholar] [CrossRef]
- Brosseau, L.; Ann, R.B. N95 Respirators and Surgical Masks. NIOSH Science Blog. Available online: https://blogs.cdc.gov/niosh-science-blog/2009/10/14/n95/ (accessed on 3 April 2020).
- DECREE-LAW No 221 of 24 December 2021. Extension of the State of National Emergency and Further Measures to Contain the Spread of the VOCID-19 Epidemic. (21G00244) (OJ General Series n.305 of 24-12-2021). Available online: https://www.gazzettaufficiale.it/eli/id/2021/12/24/21G00244/sg (accessed on 5 January 2022).
- Gawn, J.; Clayton, M.; Makison, C.; Crook, B. Evaluating the Protection Afforded by Surgical Masks against Influenza Bioaerosols: Gross Protection of Surgical Masks Compared to Filtering Facepiece Respirators. Health Saf. Exec. 2008. Available online: https://www.hse.gov.uk/research/rrpdf/rr619.pdf (accessed on 28 January 2022).
- Bałazy, A.H.; Toivola, M.; Adhikari, A.; Sivasubramani, S.K.; Reponen, T.; Grinshpun, S.A. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am. J. Infect. Contr. 2006, 34, 51–57. [Google Scholar] [CrossRef]
- Norm EN 166. 2004. Available online: https://www.univet.it/app/media/Marcature.pdf (accessed on 22 December 2020).
- Ibáñez-Cervantes, G.; Lugo-Zamudio, G.E.; Cruz-Cruz, C.; Durán-Manuel, E.M.; Bravata-Alcántara, J.C.; García-Moncada, E.; Mata-Rocha, M.; Delgado-Balbuena, L.; Cureño-Díaz, M.A.; Ramírez-Cortina, C.R.; et al. Ozone as an alternative decontamination process for N95 facemask and biosafety gowns. Mater. Lett. 2022, 311, 131554. [Google Scholar] [CrossRef]
- Kilinc, F.S. A Review of Isolation Gowns in Healthcare: Fabric and Gown Properties. J. Eng. Fibers Fabr. 2015, 10, 180–190. [Google Scholar] [CrossRef] [Green Version]
- Rapisarda, V.; Cannizzaro, E.; Barchitta, M.; Vitale, E.; Cinà, D.; Minciullo, F.; Matera, S.; Bracci, M.; Agodi, A.; Ledda, C. A Combined Multidisciplinary Intervention for Health Promotion in the Workplace: A Pilot Study. J. Clin. Med. 2021, 10, 1512. [Google Scholar] [CrossRef] [PubMed]
- Cirrincione, L.; Rapisarda, V.; Ledda, C.; Vitale, E.; Provenzano, R.; Cannizzaro, E. Considerations on the Update of the Risk Assessment Document During the Pandemic State by COVID-19 in Italy. Front. Public Health 2021, 9, 655927. [Google Scholar] [CrossRef] [PubMed]
- Soleo, L.; Cannizzaro, E.; Lovreglio, P.; Basso, A.; D’Errico, M.N.; Pira, E. Protocolli per la sorveglianza sanitaria dei lavoratori della pesca [Protocols for the health surveillance of fisherman]. G. Ital. Med. Lav. Ergon. 2013, 35, 222–226. (In Italian) [Google Scholar] [PubMed]
- Cucunawangsih, C.; Wijaya, R.S.; Lugito, N.P.H.; Suriapranata, I. Antibody response after a third dose mRNA-1273 vaccine among vaccinated healthcare workers with two doses of inactivated SARS-CoV-2 vaccine. Int. J. Infect. Dis. 2022, 118, 116–118. [Google Scholar] [CrossRef]
- Vo, H.T.M.; Maestri, A.; Auerswald, H.; Sorn, S.; Lay, S.; Seng, H.; Sann, S.; Ya, N.; Pean, P.; Dussart, P.; et al. Robust and Functional Immune Memory Up to 9 Months After SARS-CoV-2 Infection: A Southeast Asian Longitudinal Cohort. Front. Immunol. 2022, 13, 817905. [Google Scholar] [CrossRef]
- Vitale, E.; Ledda, C.; Adani, R.; Lando, M.; Bracci, M.; Cannizzaro, E.; Tarallo, L.; Rapisarda, V. Management of High-Pressure Injection Hand Injuries: A Multicentric, Retrospective, Observational Study. J. Clin. Med. 2019, 8, 2000. [Google Scholar] [CrossRef] [Green Version]
- Cirrincione, L.; Rapisarda, V.; Mazzucco, W.; Provenzano, R.; Cannizzaro, E. SARS-CoV-2 and the Risk Assessment Document in Italian Work; Specific or Generic Risk Even if Aggravated? Int. J. Environ. Res. Public Health 2021, 18, 3729. [Google Scholar] [CrossRef]
- Ramaci, T.; Barattucci, M.; Vella, F.; Senia, P.; Cannizzaro, E.; Scorciapino, A.; Ledda, C.; De Giorgio, A.; Rapisarda, V. Straining at Work and Its Relationship with Personality Profiles and Individual Consequences in Healthcare Workers (HCWs). Int. J. Environ. Res. Public Health 2020, 17, 610. [Google Scholar] [CrossRef] [Green Version]
- OSHA. Guidance on Preparing Workplaces for COVID-19; OSHA: Washington, DC, USA, 2020. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).