Meta-Analysis of Implementation Intentions Interventions in Promoting Physical Activity among University Students
Abstract
:1. Introduction
2. Methods
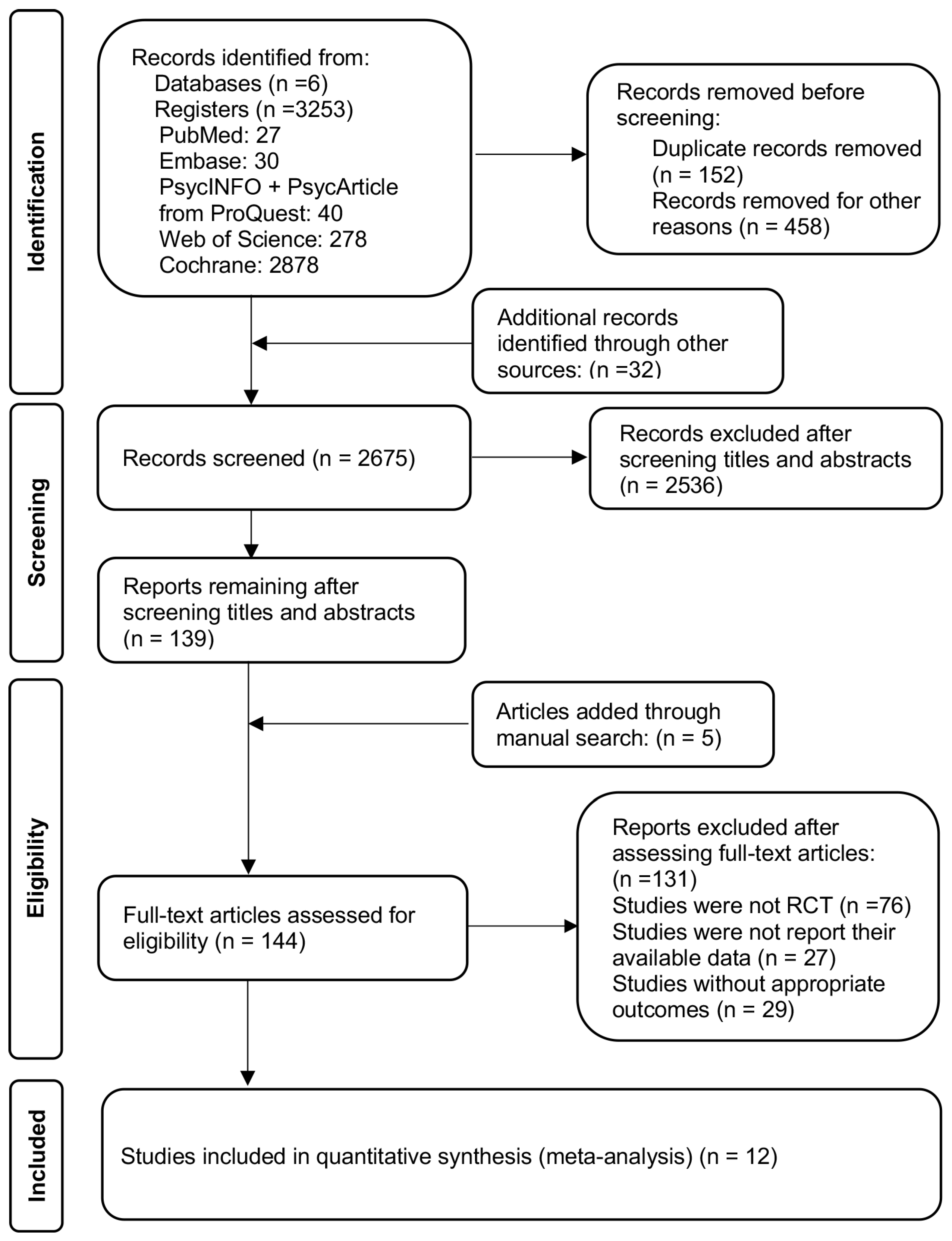
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
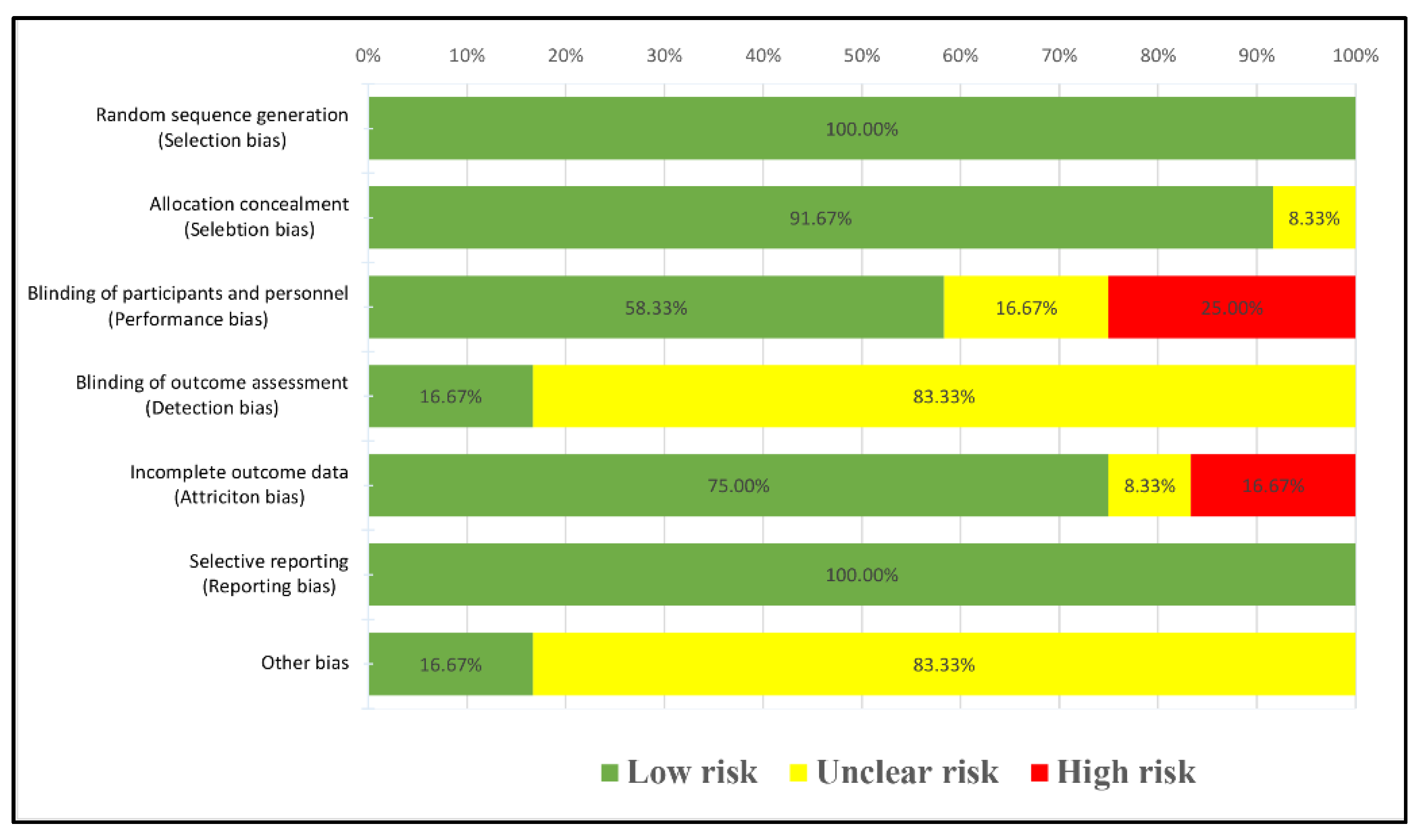
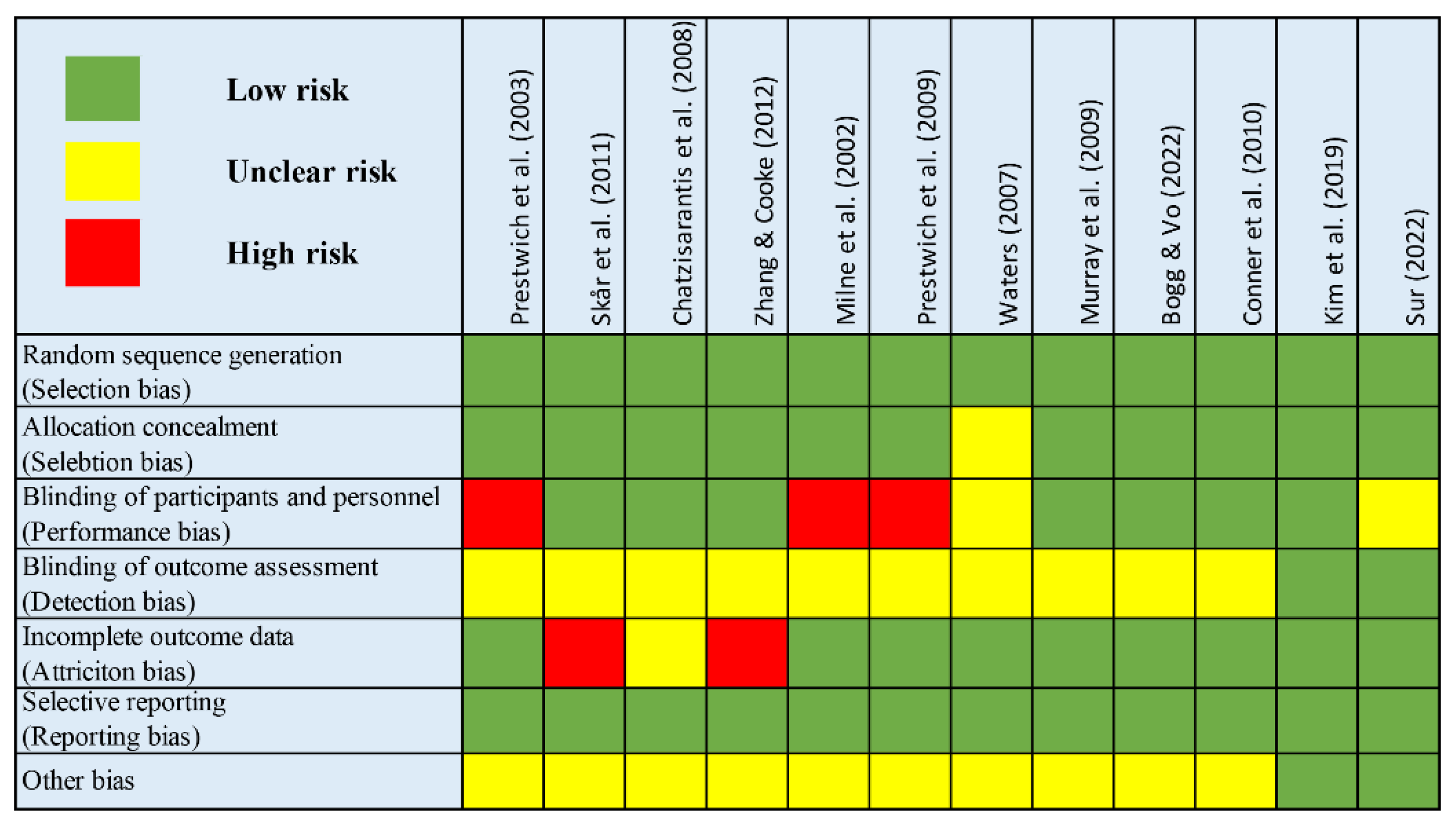
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Studies’ Characteristics
3.2. Quality of Included Studies
3.3. Primary Outcomes
3.4. Subgroup Analysis
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Physical Activity. 2022. Available online: https://www.who.int/health-topics/physical-activity#tab=tab_1 (accessed on 18 April 2023).
- World Health Organization. Global Status Report on Physical Activity. 2022. Available online: https://www.who.int/teams/health-promotion/physical-activity/global-status-report-on-physical-activity-2022 (accessed on 18 April 2023).
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Corder, K.; Winpenny, E.; Love, R.; Brown, H.E.; White, M.; Sluijs, E.V. Change in physical activity from adolescence to early adulthood: A systematic review and meta-analysis of longitudinal cohort studies. Br. J. Sports Med. 2019, 53, 496–503. [Google Scholar] [CrossRef]
- Lu, C.C.; Stolk, R.P.; Sauer, P.J.J.; Sijtsma, A.; Wiersma, R.; Huang, G.W.; Corpeleijn, E. Factors of physical activity among Chinese children and adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 36. [Google Scholar] [CrossRef]
- Plotnikoff, R.C.; Costigan, S.A.; Williams, R.L.; Hutchesson, M.J.; Kennedy, S.G.; Robards, S.L.; Allen, J.; Collins, C.E.; Callister, R.; Germov, J. Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 45. [Google Scholar] [CrossRef]
- Favieri, F.; French, M.N.; Casagrande, M.; Chen, E.Y. Physical activity interventions have a moderate effect in increasing physical activity in university students-a meta-analysis. J. Am. Coll. Health 2022, 1–12. [Google Scholar] [CrossRef]
- Schroe, H.; Van Dyck, D.; De Paepe, A.; Poppe, L.; Loh, W.W.; Verloigne, M.; Loeys, T.; De Bourdeaudhuij, I.; Crombez, G. Which behaviour change techniques are effective to promote physical activity and reduce sedentary behaviour in adults: A factorial randomized trial of an e- and m-health intervention. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 127. [Google Scholar] [CrossRef]
- Duff, O.M.; Walsh, D.M.; Furlong, B.A.; O’Connor, N.E.; Moran, K.A.; Woods, C.B. Behavior Change Techniques in Physical Activity eHealth Interventions for People With Cardiovascular Disease: Systematic Review. J. Med. Internet Res. 2017, 19, e281. [Google Scholar] [CrossRef]
- McIntosh, J.R.D.; Jay, S.; Hadden, N.; Whittaker, P.J. Do E-health interventions improve physical activity in young people: A systematic review. Public Health 2017, 148, 140–148. [Google Scholar] [CrossRef]
- Peng, S.; Yuan, F.; Othman, A.T.; Zhou, X.; Shen, G.; Liang, J. The Effectiveness of E-Health Interventions Promoting Physical Activity and Reducing Sedentary Behavior in College Students: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2022, 20, 318. [Google Scholar] [CrossRef]
- Maselli, M.; Ward, P.B.; Gobbi, E.; Carraro, A. Promoting Physical Activity Among University Students: A Systematic Review of Controlled Trials. Am. J. Health Promot. 2018, 32, 1602–1612. [Google Scholar] [CrossRef]
- Gollwitzer, P.M.; Oettingen, G. Implementation Intentions. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1043–1048. [Google Scholar]
- Gollwitzer, P.M. Implementation intentions—Strong effects of simple plans. Am. Psychol. 1999, 54, 493–503. [Google Scholar] [CrossRef]
- Schwarzer, R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl. Psychol. 2008, 57, 1–29. [Google Scholar] [CrossRef]
- Prestwich, A.; Sheeran, P.; Webb, T.; Gollwitzer, P. Implementation Intentions. In Predicting and Changing Health Behaviour: Research and Practice with Social Cognition Models; McGraw-Hill Education: London, UK, 2015; pp. 321–357. [Google Scholar]
- Pirolli, P.; Mohan, S.; Venkatakrishnan, A.; Nelson, L.; Silva, M.; Springer, A. Implementation Intention and Reminder Effects on Behavior Change in a Mobile Health System: A Predictive Cognitive Model. J. Med. Internet Res. 2017, 19, e397. [Google Scholar] [CrossRef]
- Sheeran, P. Intention—Behavior Relations: A Conceptual and Empirical Review. Eur. Rev. Social. Psychol. 2002, 12, 1–36. [Google Scholar] [CrossRef]
- Bieleke, M.; Martarelli, C.S.; Wolff, W. If-then planning, self-control, and boredom as predictors of adherence to social distancing guidelines: Evidence from a two-wave longitudinal study with a behavioral intervention. Curr. Psychol. 2021, 32, 9095–9108. [Google Scholar] [CrossRef]
- Norman, P.; Conner, M. The theory of planned behavior and exercise: Evidence for the mediating and moderating roles of planning on intention-behavior relationships. J. Sport. Exerc. Psychol. 2005, 27, 488–504. [Google Scholar] [CrossRef]
- Schwarzer, R.; Lippke, S.; Luszczynska, A. Mechanisms of health behavior change in persons with chronic illness or disability: The Health Action Process Approach (HAPA). Rehabil. Psychol. 2011, 56, 161–170. [Google Scholar] [CrossRef]
- Sussman, R.; Gifford, R. Causality in the Theory of Planned Behavior. Pers. Soc. Psychol. Bull. 2019, 45, 920–933. [Google Scholar] [CrossRef]
- Sheeran, P.; Webb, T.L. The Intention-Behavior Gap. Soc. Personal. Psychol. Compass 2016, 10, 503–518. [Google Scholar] [CrossRef]
- Gollwitzer, P.M.; Sheeran, P. Implementation Intentions and Goal Achievement: A Meta-analysis of Effects and Processes. Adv. Exp. Soc. Psychol. 2006, 38, 69–119. [Google Scholar]
- Rhodes, R.E.; Dickau, L. Experimental evidence for the intention-behavior relationship in the physical activity domain: A meta-analysis. Health Psychol. 2012, 31, 724–727. [Google Scholar] [CrossRef]
- Hagger, M.S.; Luszczynska, A. Implementation intention and action planning interventions in health contexts: State of the research and proposals for the way forward. Appl. Psychol. Health Well Being 2014, 6, 1–47. [Google Scholar] [CrossRef]
- Vila, I.; Carrero, I.; Redondo, R. Reducing fat intake using implementation intentions: A meta-analytic review. Br. J. Health Psychol. 2017, 22, 281–294. [Google Scholar] [CrossRef]
- Adriaanse, M.A.; Vinkers, C.D.; De Ridder, D.T.; Hox, J.J.; De Wit, J.B. Do implementation intentions help to eat a healthy diet? A systematic review and meta-analysis of the empirical evidence. Appetite 2011, 56, 183–193. [Google Scholar] [CrossRef]
- McWilliams, L.; Bellhouse, S.; Yorke, J.; Lloyd, K.; Armitage, C.J. Beyond “planning”: A meta-analysis of implementation intentions to support smoking cessation. Health Psychol. 2019, 38, 1059–1068. [Google Scholar] [CrossRef]
- Belanger-Gravel, A.; Godin, G.; Amireault, S. A meta-analytic review of the effect of implementation intentions on physical activity. Health Psychol. Rev. 2013, 7, 23–54. [Google Scholar] [CrossRef]
- Peng, S.; Othman, A.T.; Yuan, F.; Liang, J. The Effectiveness of Planning Interventions for Improving Physical Activity in the General Population: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public. Health 2022, 19, 7337. [Google Scholar] [CrossRef]
- Carraro, N.; Gaudreau, P. Spontaneous and experimentally induced action planning and coping planning for physical activity: A meta-analysis. Psychol. Sport. Exerc. 2013, 14, 228–248. [Google Scholar] [CrossRef]
- Lin, H.; Yu, P.; Yang, M.; Wu, D.; Wang, Z.; An, J.; Duan, H.; Deng, N. Making Specific Plan Improves Physical Activity and Healthy Eating for Community-Dwelling Patients With Chronic Conditions: A Systematic Review and Meta-Analysis. Front. Public Health 2022, 10, 721223. [Google Scholar] [CrossRef]
- Ferreira Silva, R.M.; Mendonca, C.R.; Azevedo, V.D.; Raoof Memon, A.; Noll, P.; Noll, M. Barriers to high school and university students’ physical activity: A systematic review. PLoS ONE 2022, 17, e0265913. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rucker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomized controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Milne, S.; Orbell, S.; Sheeran, P. Combining motivational and volitional interventions to promote exercise participation: Protection motivation theory and implementation intentions. Br. J. Health Psychol. 2002, 7, 163–184. [Google Scholar] [CrossRef]
- Prestwich, A.; Lawton, R.; Conner, M. The use of implementation intentions and the decision balance sheet in promoting exercise behaviour. Psychol. Health 2003, 18, 707–721. [Google Scholar] [CrossRef]
- Waters, E.A. Increasing Physical Activity in Female College Students: A Possible Selves Intervention; ProQuest: Ann Arbor, MI, USA, 2007. [Google Scholar]
- Chatzisarantis, N.L.; Hagger, M.S.; Thøgersen-Ntoumani, C. The Effects of Self-Discordance, Self-Concordance, and Implementation Intentions on Health Behavior. J. Appl. Biobehav. Res. 2008, 13, 198–214. [Google Scholar] [CrossRef]
- Murray, T.C.; Rodgers, W.M.; Fraser, S.N. Examining implementation intentions in an exercise intervention: The effects on adherence and self-efficacy in a naturalistic setting. J. Appl. Social. Psychol. 2009, 39, 2303–2320. [Google Scholar] [CrossRef]
- Prestwich, A.; Perugini, M.; Hurling, R. Can the effects of implementation intentions on exercise be enhanced using text messages? Psychol. Health 2009, 24, 677–687. [Google Scholar] [CrossRef]
- Conner, M.; Sandberg, T.; Norman, P. Using action planning to promote exercise behavior. Ann. Behav. Med. 2010, 40, 65–76. [Google Scholar] [CrossRef]
- Skar, S.; Sniehotta, F.F.; Molloy, G.J.; Prestwich, A.; Araujo-Soares, V. Do brief online planning interventions increase physical activity amongst university students? A randomized controlled trial. Psychol. Health 2011, 26, 399–417. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Cooke, R. Using a combined motivational and volitional intervention to promote exercise and healthy dietary behaviour among undergraduates. Diabetes Res. Clin. Pract. 2012, 95, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, M.J.; Kim, S.H.; Kim, S.Y.; Park, C.Y.; Bang, J.Y. Effectiveness of Health Promotion Program Using Action Planning Strategy for Young Adults. J. Korean Acad. Nurs. 2019, 49, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Bogg, T.; Vo, P.T. Realistic effort action plans (REAP) for exercise among underactive and inactive university students: A randomized trial. J. Am. Coll. Health 2022, 1–10. [Google Scholar] [CrossRef]
- Sur, B. The Road to Health is Paved with Good Intentions: Mental Contrasting and Implementation Intentions as Potential Mechanisms for the Adoption of Physical Activity in College Students. Ph.D. Thesis, The University of Arizona, Tucson, AZ, USA, 2022. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, I.; Strobach, T. Predicting Physical Activity Behavior by Automatic and Reflective Self-Regulatory Processes. Front. Psychol. 2021, 12, 714608. [Google Scholar] [CrossRef]
- Ungar, N.; Rupprecht, F.S.; Steindorf, K.; Wiskemann, J.; Sieverding, M. Worse or even better than expected? Outcome expectancies and behavioral experiences in the context of physical activity among cancer patients. J. Health Psychol. 2021, 26, 659–671. [Google Scholar] [CrossRef]
- Williams, D.M.; Anderson, E.S.; Winett, R.A. A review of the outcome expectancy construct in physical activity research. Ann. Behav. Med. 2005, 29, 70–79. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Grant, S.; de Bruijn, G.-J. Planning and Implementation Intention Interventions. In The Handbook of Behavior Change; Hamilton, K., Cameron, L.D., Hagger, M.S., Hankonen, N., Lintunen, T., Eds.; Cambridge Handbooks in Psychology; Cambridge University Press: Cambridge, UK, 2020; pp. 572–585. [Google Scholar]
- Silva, M.; Sao-Joao, T.M.; Brizon, V.C.; Franco, D.H.; Mialhe, F.L. Impact of implementation intentions on physical activity practice in adults: A systematic review and meta-analysis of randomized clinical trials. PLoS ONE 2018, 13, e0206294. [Google Scholar] [CrossRef]
- Murphy, J.J.; MacDonncha, C.; Murphy, M.H.; Murphy, N.; Nevill, A.M.; Woods, C.B. What Psychosocial Factors Determine the Physical Activity Patterns of University Students? J. Phys. Act. Health 2019, 16, 325–332. [Google Scholar] [CrossRef]
- Carballo-Fazanes, A.; Rico-Diaz, J.; Barcala-Furelos, R.; Rey, E.; Rodriguez-Fernandez, J.E.; Varela-Casal, C.; Abelairas-Gomez, C. Physical Activity Habits and Determinants, Sedentary Behaviour and Lifestyle in University Students. Int. J. Environ. Res. Public Health 2020, 17, 3272. [Google Scholar] [CrossRef]
- Keating, X.D.; Guan, J.; Pinero, J.C.; Bridges, D.M. A meta-analysis of college students’ physical activity behaviors. J. Am. Coll. Health 2005, 54, 116–125. [Google Scholar] [CrossRef]
- McDaniel, M.A.; Scullin, M.K. Implementation intention encoding does not automatize prospective memory responding. Mem. Cogn. 2010, 38, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Kompf, J. Implementation Intentions for Exercise and Physical Activity: Who Do They Work For? A Systematic Review. J. Phys. Act. Health 2020, 17, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Meslot, C.; Gauchet, A.; Allenet, B.; Francois, O.; Hagger, M.S. Theory-Based Interventions Combining Mental Simulation and Planning Techniques to Improve Physical Activity: Null Results from Two Randomized Controlled Trials. Front. Psychol. 2016, 7, 1789. [Google Scholar] [CrossRef] [PubMed]
- McAuley, E.; Blissmer, B. Self-efficacy determinants and consequences of physical activity. Exerc. Sport. Sci. Rev. 2000, 28, 85–88. [Google Scholar]
- Pekmezi, D.; Jennings, E.; Marcus, B.H. Evaluating and Enhancing Self-Efficacy for Physical Activity. ACSMs Health Fit. J. 2009, 13, 16–21. [Google Scholar] [CrossRef]
- Bandura, A.; Freeman, W.H.; Lightsey, R. Self-Efficacy: The Exercise of Control; Springer: Berlin/Heidelberg, Germany, 1999. [Google Scholar]
- Michie, S.; West, R.; Sheals, K.; Godinho, C.A. Evaluating the effectiveness of behavior change techniques in health-related behavior: A scoping review of methods used. Transl. Behav. Med. 2018, 8, 212–224. [Google Scholar] [CrossRef]
- Ajzen, I.; Schmidt, P. Changing Behavior Using the Theory of Planned Behavior. In The Handbook of Behavior Change; Hamilton, K., Cameron, L.D., Hagger, M.S., Hankonen, N., Lintunen, T., Eds.; Cambridge Handbooks in Psychology; Cambridge University Press: Cambridge, UK, 2020; pp. 17–31. [Google Scholar]
- Skarin, F.; Wastlund, E.; Gustafsson, H. Maintaining or Losing Intervention-Induced Health-Related Behavior Change. A Mixed Methods Field Study. Front. Psychol. 2021, 12, 688192. [Google Scholar] [CrossRef]
- Hooker, S.; Punjabi, A.; Justesen, K.; Boyle, L.; Sherman, M.D. Encouraging Health Behavior Change: Eight Evidence-Based Strategies. Fam. Pract. Manag. 2018, 25, 31–36. [Google Scholar]
- Malaguti, A.; Ciocanel, O.; Sani, F.; Dillon, J.F.; Eriksen, A.; Power, K. Effectiveness of the use of implementation intentions on reduction of substance use: A meta-analysis. Drug Alcohol. Depend. 2020, 214, 108120. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez Salas Duhne, P.; Horan, A.J.; Ross, C.; Webb, T.L.; Hardy, G.E. Assessing and promoting the use of implementation intentions in clinical practice. Soc. Sci. Med. 2020, 265, 113490. [Google Scholar] [CrossRef] [PubMed]
- Oettingen, G.; Gollwitzer, P.M. Health behavior change by self-regulation of goal pursuit: Mental contrasting with implementation intentions. In Routledge International Handbook of Self-Control in Health and Well-Being; Routledge: Abingdon-on-Thames, UK, 2018. [Google Scholar]
- Kohler, S.; Dippon, L.; Helsper, N.; Rutten, A.; Abu-Omar, K.; Birkholz, L.; Pfeifer, K.; Weber, P.; Semrau, J. Population-based physical activity promotion with a focus on health equity: A review of reviews. Int. J. Equity Health 2023, 22, 18. [Google Scholar] [CrossRef] [PubMed]
- Till, M.; Abu-Omar, K.; Ferschl, S.; Abel, T.; Pfeifer, K.; Gelius, P.; Capital4Health, c. Implementing the capability approach in health promotion projects: Recommendations for implementation based on empirical evidence. Eval. Program Plann. 2022, 95, 102149. [Google Scholar] [CrossRef]
- Deloitte. Smart Campus: The Next-Generation Connected Campus. Available online: https://www2.deloitte.com/content/dam/Deloitte/us/Documents/strategy/the-next-generation-connected-campus-deloitte.pdf (accessed on 18 April 2023).
- Walsh, J.C.; Groarke, J.M. Integrating Behavioral Science With Mobile (mHealth) Technology to Optimise Health Behavior Change Interventions. Eur. Psychol. 2019, 24, 38–48. [Google Scholar] [CrossRef]

| Publication | Sample Size | Country | Sample Characteristics | Intervention Characteristics | Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Female (%) | Participant | Intervention Content | Delivery Mode | Duration | Reinforcement | Instruments | Indicators | |||||
| IG | CG | IG | CG | ||||||||||
| Milne et al., 2002 [40] | 79 | 93 | UK | 20.04 ± 2.23 | 73 | General | AP | Session | 2 W | No | Items (not validated) | No. times MVPA > 20 min/week | |
| Prestwich et al., 2009 [45] | 29 | 34 | UK | 23.76 ± 4.64 | 58.06 | Inactive | AP | Session | 4 W | Reminder by Mobile phone (not mentioned times) | Item (not validated) | No. times of MVPA > 30 min/week | |
| Zhang and Cooke, 2012 [48] | 22 | 21 | UK | 20.56 ± 1.62 | 48.81 | General | AP + CP | Session | 4 W | No | Items (not validated) | No. times MVPA > 20 min/week | |
| Murray et al., 2009 [44] | 29 | 23 | Canada | 30.5 ± 9.8 | 100 | General | AP | Session | 11 W | Three times repetition | Checklist at the gym (not validated) | No.sessions/week | |
| Prestwich et al., 2003 [41] | 18 | 18 | UK | 21.31 ± 4.39 | 51.2 | General | AP | Session | 4 W | No | Items not validated | No. sessions/week | |
| Skår et al., 2011 [47] | 335 | 315 | UK | 22.8 ± 6.7 | 63.4 | General | AP + CP | Online | 6 W | No | Items (validated) | Scores expressing frequency | |
| Chatzisarantis et al., 2008 [43] | 92 | 35 | Singapore | 20.71 ± 6.95 | 72.44 | Inactive | AP | Session | 5 W | No | LTEQ | Scores expressing frequency | |
| Kim et al., 2019 [49] | 51 | 52 | Korea | 22.59 ± 1.77 | 56.3 | General | AP | Session | 5 W | Repetition every week | Items (not validated) | Scores expressing frequency | |
| Conner et al., 2010 [46] | 180 | 176 | UK | 20.7 ± 2.99 | 69 | General | AP | Session | 2 W | No | Items (validated) | Frequency of exercise | |
| Waters, 2007 [42] | 54 | 60 | USA | 18.2 ± 2.0 | 100 | General | AP | Session | 6 W | No | Items (not validated) | Mins of exercise/week | |
| Bogg and Vo, 2022 [50] | 73 | 74 | USA | 20.56 ± 2.04 | 60 | Inactive | AP | Session | 2 M | Three times by email, reminding | Pedometer + Items (not validated) | METs Exercise | |
| Sur, 2022 [51] | 24 | 29 | USA | 19 | N/R | Inactive | AP + CP | Online | 2 W | Repetition every day | IPAQ | Mins of MVPA/week | |
| Moderators | Category | Studies | Heterogeneity Test | SMD and 95%CI | p | |
|---|---|---|---|---|---|---|
| p | I2 (%) | |||||
| Publish Year | ≥2013 | 3 | 0.004 | 82.2 | 0.60 (0.02, 1.17) | 0.042 |
| <2013 | 9 | 0.020 | 55.9 | 0.22 (0.04, 0.39) | 0.015 | |
| Overall | 12 | <0.001 | 70.1 | 0.31 (0.12, 0.50) | 0.001 | |
| Between | 0.216 | |||||
| Participant | General | 8 | <0.001 | 73.7 | 0.27 (0.04, 0.50) | 0.023 |
| Inactive | 4 | 0.053 | 61.0 | 0.40 (0.05, 0.74) | 0.025 | |
| Overall | 12 | <0.001 | 70.1 | 0.31 (0.12, 0.50) | 0.001 | |
| Between | 0.550 | |||||
| Intervention Strategy | AP | 9 | 0.004 | 64.9 | 0.36 (0.14, 0.57) | 0.001 |
| AP + CP | 3 | 0.099 | 56.7 | 0.15 (−0.22, 0.52) | 0.418 | |
| Overall | 12 | <0.001 | 70.1 | 0.31 (0.12, 0.50) | 0.001 | |
| Between | 0.349 | |||||
| Reinforcement | Yes | 5 | 0.008 | 71.1 | 0.45 (0.08, 0.83) | 0.019 |
| No | 7 | 0.008 | 65.5 | 0.22 (0.01, 0.42) | 0.036 | |
| Overall | 12 | <0.001 | 70.1 | 0.31 (0.12, 0.50) | 0.001 | |
| Between | 0.285 | |||||
| Duration | ≥6 weeks | 4 | 0.550 | 0.0 | 0.05 (−0.07, 0.18) | 0.407 |
| <6 weeks | 8 | 0.004 | 66.0 | 0.42 (0.17, 0.67) | 0.001 | |
| Overall | 12 | <0.001 | 70.1 | 0.31 (0.12, 0.50) | 0.001 | |
| Between | 0.010 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, S.; Othman, A.T.; Khairani, A.Z.; Zhou, Z.; Zhou, X.; Yuan, F.; Liang, J. Meta-Analysis of Implementation Intentions Interventions in Promoting Physical Activity among University Students. Sustainability 2023, 15, 12457. https://doi.org/10.3390/su151612457
Peng S, Othman AT, Khairani AZ, Zhou Z, Zhou X, Yuan F, Liang J. Meta-Analysis of Implementation Intentions Interventions in Promoting Physical Activity among University Students. Sustainability. 2023; 15(16):12457. https://doi.org/10.3390/su151612457
Chicago/Turabian StylePeng, Sanying, Ahmad Tajuddin Othman, Ahmad Zamri Khairani, Zhuang Zhou, Xiaogang Zhou, Fang Yuan, and Jinghong Liang. 2023. "Meta-Analysis of Implementation Intentions Interventions in Promoting Physical Activity among University Students" Sustainability 15, no. 16: 12457. https://doi.org/10.3390/su151612457
APA StylePeng, S., Othman, A. T., Khairani, A. Z., Zhou, Z., Zhou, X., Yuan, F., & Liang, J. (2023). Meta-Analysis of Implementation Intentions Interventions in Promoting Physical Activity among University Students. Sustainability, 15(16), 12457. https://doi.org/10.3390/su151612457









