Symptoms of Anxiety and Depression in Polish Population in the Context of the War in Ukraine: Analysis of Risk Factors and Practical Implications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Procedure
2.2. Participants
2.3. Research Tools
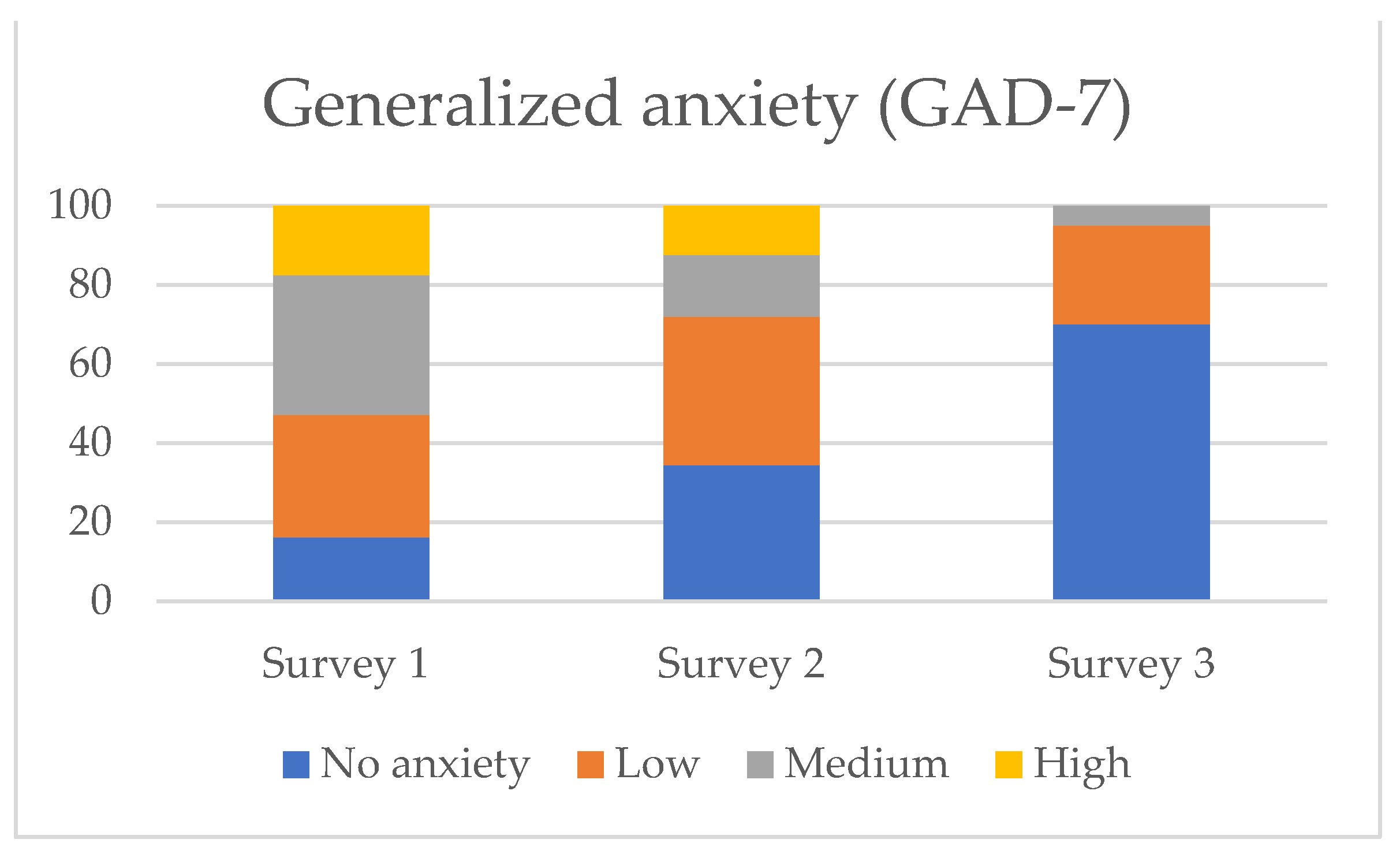
- Generalized Anxiety Disorder Questionnaire (GAD-7) [21]. This is a self-report scale used to assess the severity of anxiety and the risk of generalized anxiety disorder (GAD). The scale contains 7 items, the scoring range is 0–21 points. Scores of 5, 10, 15 are defined as cut-off values for the presence of mild, moderate and severe severity of anxiety, respectively [21].
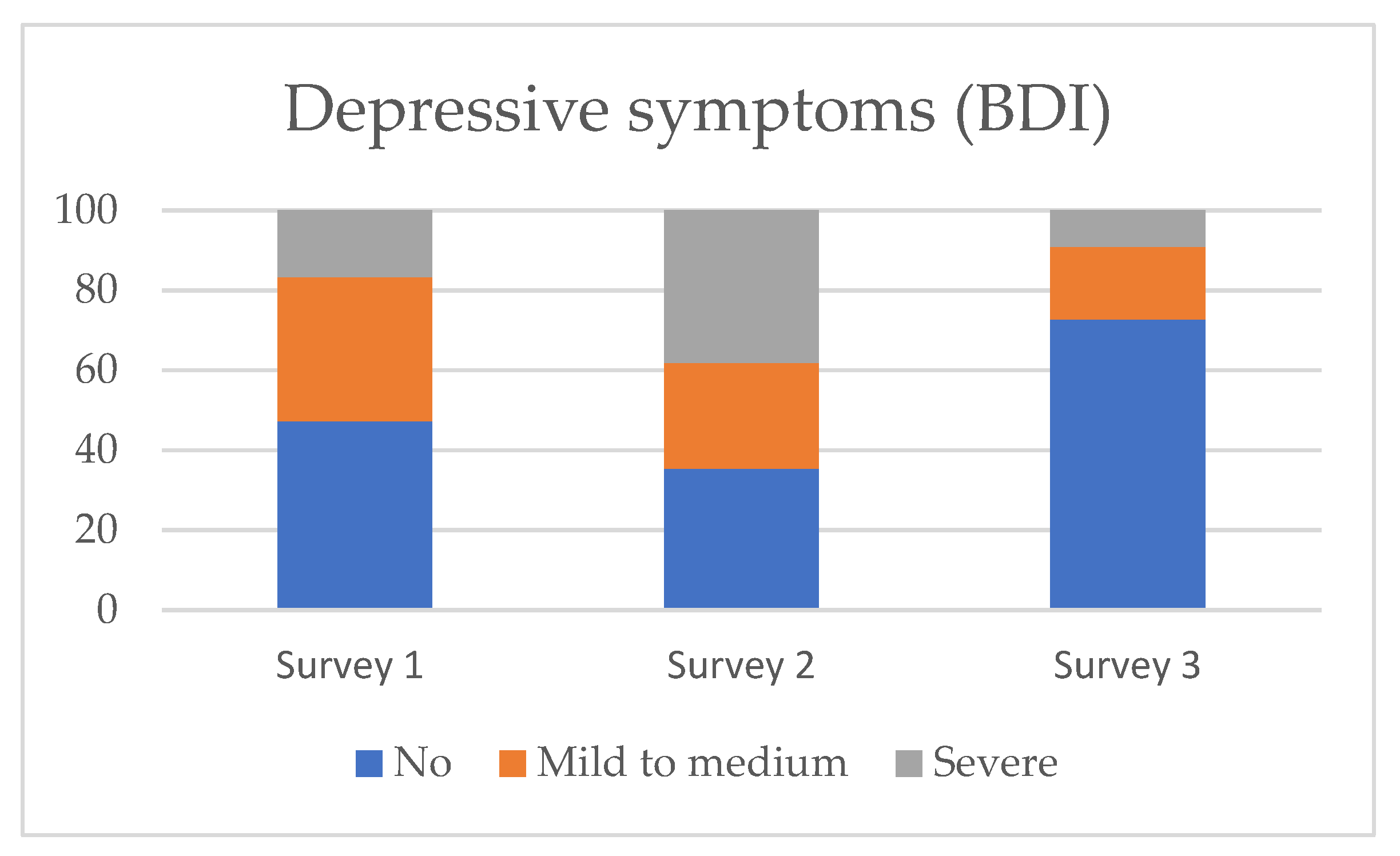
- Beck Depression Inventory (BDI). This is a screening tool used to assess the presence and severity of depressive symptoms. It consists of 21 statements scored from 0 to 3 points. The following cut-off points are used: 0–9 no depression, 10–18 mild to moderate symptom severity, 19–29 moderate to severe and 30–63 severe depression [22,23].
- The abovementioned questionnaires are validated and have good psychometric properties.
- A questionnaire including demographic data, questions on relationships with close people, diet, physical activity, sleep, history of psychiatric treatment, alcohol consumption, time spent by respondents watching the news and conducting conversations about Russia’s war with Ukraine, fear of an armed attack on Poland, impact of war on the sense of security and concerns about the deterioration of their financial situation due to war. The survey was designed by our team on the basis of literature data regarding mental health symptoms in previous disasters. Questions concerning putative factors associated with mental health were either Likert-like (items A–G) or dichotomous (items H-J). For the purpose of statistical analysis, the Likert-like items were dichotomized (1–2 vs. 3–4). The questionnaire is presented in Supplementary Materials.
2.4. Statistical Analysis
3. Results
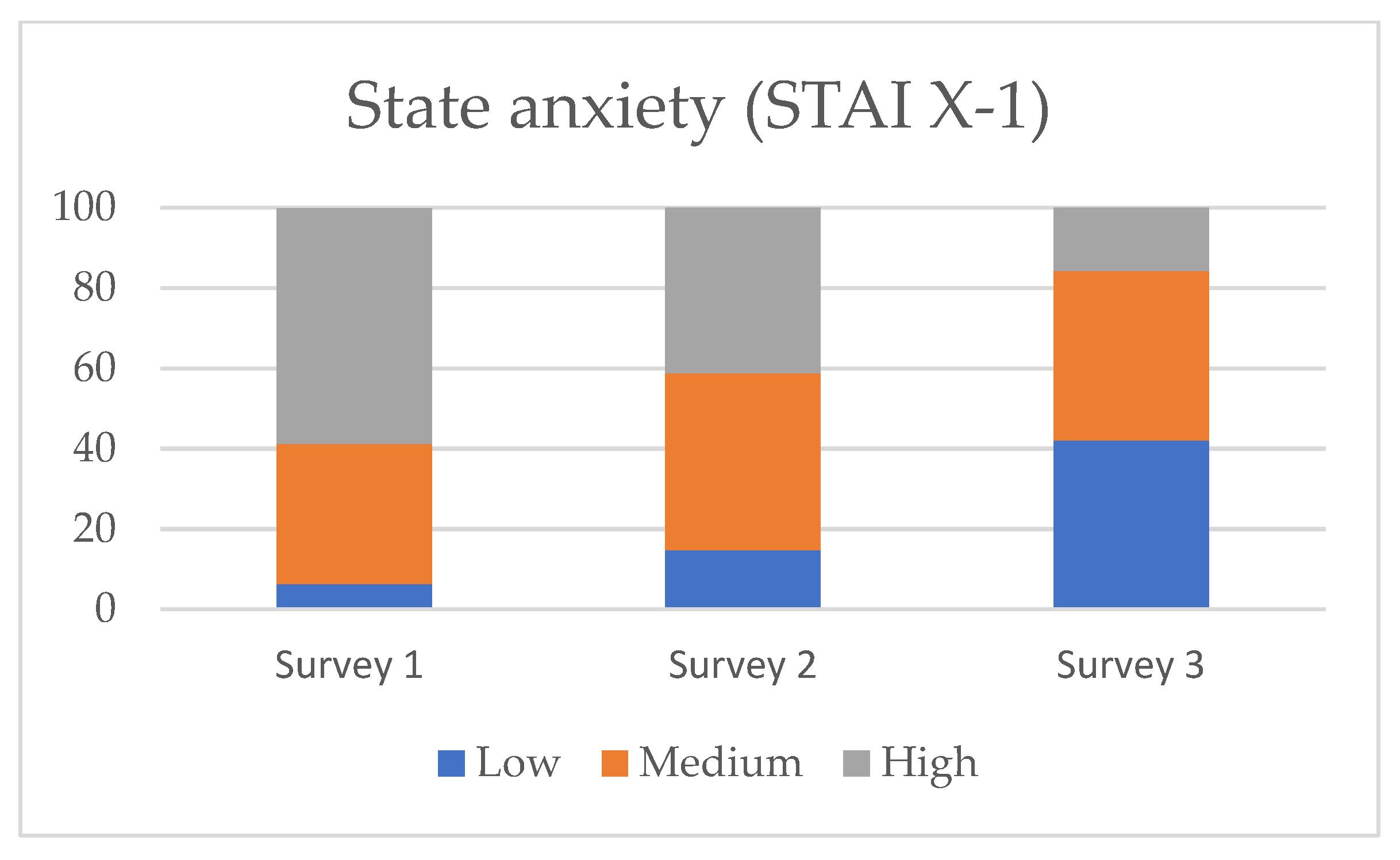
3.1. Severity of Symptoms of Anxiety and Depression—Changes over Time
3.2. Determinants of Depression and Anxiety Severity
- women;
- persons with lower income per family member;
- persons declaring poor quality of sleep;
- persons who were more likely to read information about the war and to discuss it with others;
- persons who feared the immediate consequences of the war for Poland and themselves;
- persons whose sense of security was impacted by war.
- unemployed persons;
- people who declared a lack of good relations with close people;
- people concerned about the worsening of their financial situation due to war.
4. Discussion
4.1. Severity of Symptoms of Anxiety and Depression in People Indirectly Affected by War
4.2. Short- and Long-Term Effects for Those Indirectly Affected by the Consequences of War
4.3. Identification of Individuals at Risk of Anxiety and Depressive Symptoms
4.4. Practical Implications
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guenette, J.D.; Kenworthy, P.G.; Wheeler, C.M. Implications of the War in Ukraine for the Global Economy; World Bank: Washington, DC, USA, 2022. [Google Scholar]
- Jankowski, M.; Lazarus, J.V.; Kuchyn, I.; Zemskov, S.; Gałązkowski, R.; Gujski, M. One Year On: Poland’s Public Health Initiatives and National Response to Millions of Refugees from Ukraine. Med. Sci. Monit. 2023, 29, e940223. [Google Scholar] [CrossRef] [PubMed]
- UNHCR. United Nations High Commissioner for Refugees. The UN Refugee Agency. Poland Welcomes More Than Two Million Refugees from Ukraine. Available online: https://www.unhcr.org/news/news-releases/poland-welcomes-more-two-million-refugees-ukraine (accessed on 4 February 2023).
- Fatyga, E.; Dzięgielewska-Gęsiak, S.; Muc-Wierzgoń, M. Organization of Medical Assistance in Poland for Ukrainian Citizens During the Russia-Ukraine War. Front. Public Health 2022, 10, 904588. [Google Scholar] [CrossRef] [PubMed]
- Domaradzki, J.; Walkowiak, D.; Bazan, D.; Baum, E. Volunteering in the front line of the Ukrainian refugee crisis: A brief report from Poland. Front. Public Health 2022, 10, 979751. [Google Scholar] [CrossRef] [PubMed]
- RRRP. Final Report 2022 Regional Refugee Response Plan for the Ukraine Situation March–December 2022. Available online: https://data2.unhcr.org/en/situations/ukraine (accessed on 4 February 2023).
- Republic of Poland. Office for Foreigners: Amendment to the Law on Assistance to Ukrainian Citizens in Connection with the Armed Conflict on the Territory of the Country. 28 March 2022. Available online: https://www.gov.pl/web/udsc-en/the-law-on-assistance-to-ukrainian-citizens-in-connection-with-the-armed-conflict-on-the-territory-of-the-country-has-entered-into-force (accessed on 4 January 2023).
- UNHCR. United Nations High Commissioner for Refugees Operational Data Portal. Ukraine Refugee Situation. Available online: https://data.unhcr.org/en/situations/ukraine (accessed on 5 April 2023).
- Sheather, J. As Russian troops cross into Ukraine, we need to remind ourselves of the impact of war on health. BMJ 2022, 376, o499. [Google Scholar] [CrossRef] [PubMed]
- Shoib, S.; Javed, S.; Alamrawy, R.G.; Nigar, A.; Das, S.; Saeed, F.; Handuleh, J.I.M.; Shellah, D.; Dazhamyar, A.R.; Chandradasa, M. Challenges in mental health and psychosocial care in conflict-affected low- and middle-income countries. Asian J. Psychiatry 2022, 67, 102894. [Google Scholar] [CrossRef]
- Bryant, R.A.; Schnurr, P.P.; Pedlar, D. Addressing the mental health needs of civilian combatants in Ukraine. Lancet Psychiatry 2022, 9, 346–347. [Google Scholar] [CrossRef]
- Charlson, F.; van Ommeren, M.; Flaxman, A.; Cornett, J.; Whiteford, H.; Saxena, S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet 2019, 394, 240–248. [Google Scholar] [CrossRef]
- Pavlova, I.; Graf-Vlachy, L.; Petrytsa, P.; Wang, S.; Zhang, S.X. Early evidence on the mental health of Ukrainian civilian and professional combatants during the Russian invasion. Eur. Psychiatry 2022, 65, e79. [Google Scholar] [CrossRef]
- Xu, W.; Pavlova, I.; Chen, X.; Petrytsa, P.; Graf-Vlachy, L.; Zhang, S.X. Mental health symptoms and coping strategies among Ukrainians during the Russia-Ukraine war in March 2022. Int. J. Soc. Psychiatry 2023, 69, 957–966. [Google Scholar] [CrossRef]
- Rizzi, D.; Ciuffo, G.; Sandoli, G.; Mangiagalli, M.; de Angelis, P.; Scavuzzo, G.; Nych, M.; Landoni, M.; Ionio, C. Running Away from the War in Ukraine: The Impact on Mental Health of Internally Displaced Persons (IDPs) and Refugees in Transit in Poland. Int. J. Environ. Res. Public Health 2022, 19, 16439. [Google Scholar] [CrossRef]
- Elvevåg, B.; DeLisi, L.E. The mental health consequences on children of the war in Ukraine: A commentary. Psychiatry Res. 2022, 317, 114798. [Google Scholar] [CrossRef] [PubMed]
- Greenglass, E.; Begic, P.; Buchwald, P.; Karkkola, P.; Hintsa, T. Watching the War in Ukraine and Psychological Factors: Comparisons between Europe und North America. In Proceedings of the Conference of Stress, Trauma, Anxiety and Resilience Society, Faro, Portugal, 19–21 July 2023. [Google Scholar]
- Moshagen, M.; Hilbig, B. Citizens’ Psychological Reactions following the Russian invasion of the Ukraine: A cross-national study. Ed. PsyArXiv. 2022. [Google Scholar] [CrossRef]
- Riad, A.; Drobov, A.; Krobot, M.; Antalová, N.; Alkasaby, M.A.; Peřina, A.; Koščík, M. Mental Health Burden of the Russian-Ukrainian War 2022 (RUW-22): Anxiety and Depression Levels among Young Adults in Central Europe. Int. J. Environ. Res. Public Health 2022, 19, 8418. [Google Scholar] [CrossRef] [PubMed]
- Shevlin, M.; Hyland, P.; Karatzias, T. The psychological consequences of the Ukraine war: What we know, and what we have to learn. Acta Psychiatr. Scand. 2022, 146, 105–106. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Parnowski, T.; Jernajczyk, W. Inwentarz depresji Beck’a w ocenie nastroju osób zdrowych i chorych na choroby afektywne. [Beck Depression Inventory in assessing the mood of healthy people and patients with affective disorders.]. Psychiatr. Pol. 1977, 9, 417–421. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Carbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.; Lushene, R. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Wrześniewski, K.; Sosnowski, T.; Jaworowska, A.; Fecenec, D. Inwentarz Stanu i Cechy Lęku. Polska Adaptacja STAI. [State and Trait Anxiety Inventory. Polish Adaptation of STAI]; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2011. [Google Scholar]
- Brągiel, A.; Gambin, M. Depressive symptoms and psychological pain experienced by Polish adults in the context of both the war in Ukraine and the COVID-19 pandemic. J. Affect. Disord. 2023, 12, 100487. [Google Scholar] [CrossRef]
- Chudzicka-Czupała, A.; Hapon, N.; Man, R.H.C.; Li, D.J.; Żywiołek-Szeja, M.; Karamushka, L.; Grabowski, D.; Paliga, M.; McIntyre, R.S.; Chiang, S.K.; et al. Associations between coping strategies and psychological distress among people living in Ukraine, Poland, and Taiwan during the initial stage of the 2022 War in Ukraine. Eur. J. Psychotraumatol. 2023, 14, 2163129. [Google Scholar] [CrossRef]
- Kossowska, M.; Szwed, P.; Szumowska, E.; Perek-Białas, J.; Czernatowicz-Kukuczka, A. The role of fear, closeness, and norms in shaping help towards war refugees. Sci. Rep. 2023, 13, 1465. [Google Scholar] [CrossRef]
- Maftei, A.; Dănilă, O.; Măirean, C. The war next-door—A pilot study on Romanian adolescents’ psychological reactions to potentially traumatic experiences generated by the Russian invasion of Ukraine. Front. Psychol. 2022, 13, 1051152. [Google Scholar] [CrossRef]
- Gottschick, C.; Diexer, S.; Massag, J.; Klee, B.; Broda, A.; Purschke, O.; Binder, M.; Sedding, D.; Frese, T.; Girndt, M. Mental health in Germany in the first weeks of the Russo-Ukrainian war. BJPsych Open 2023, 9, e66. [Google Scholar] [CrossRef]
- Jawaid, A.; Gomolka, M.; Timmer, A. Neuroscience of trauma and the Russian invasion of Ukraine. Nat. Hum. Behav. 2022, 6, 748–749. [Google Scholar] [CrossRef] [PubMed]
- Skwirczyńska, E.; Kozłowski, M.; Nowak, K.; Wróblewski, O.; Sompolska-Rzechuła, A.; Kwiatkowski, S.; Cymbaluk-Płoska, A. Anxiety Assessment in Polish Students during the Russian-Ukrainian War. Int. J. Environ. Res. Public Health 2022, 19, 13284. [Google Scholar] [CrossRef] [PubMed]
- Chudzicka-Czupała, A.; Hapon, N.; Chiang, S.K.; Żywiołek-Szeja, M.; Karamushka, L.; Lee, C.T.; Grabowski, D.; Paliga, M.; Rosenblat, J.D.; Ho, R.; et al. Depression, anxiety and post-traumatic stress during the 2022 Russo-Ukrainian war, a comparison between populations in Poland, Ukraine, and Taiwan. Sci. Rep. 2023, 13, 3602. [Google Scholar] [CrossRef]
- Pandi-Perumal, S.R.; Monti, J.M.; Burman, D.; Karthikeyan, R.; BaHammam, A.S.; Spence, D.W.; Brown, G.M.; Narashimhan, M. Clarifying the role of sleep in depression: A narrative review. Psychiatry Res. 2020, 291, 113239. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Zhao, J.; Zhai, S.; Ye, H.; Bu, L.; Fan, F. Does sleep disturbance predicts posttraumatic stress disorder and depression among college students during COVID-19 lockdown? A longitudinal survey. Front. Public Health 2022, 10, 986934. [Google Scholar] [CrossRef] [PubMed]
- Fan, F.; Zhou, Y.; Liu, X. Sleep Disturbance Predicts Posttraumatic Stress Disorder and Depressive Symptoms: A Cohort Study of Chinese Adolescents. J. Clin. Psychiatry 2017, 78, 882–888. [Google Scholar] [CrossRef]
- Surzykiewicz, J.; Skalski, S.B.; Niesiobędzka, M.; Gladysh, O.; Konaszewski, K. Brief screening measures of mental health for war-related dysfunctional anxiety and negative persistent thinking. Pers. Individ. Differ. 2022, 195, 111697. [Google Scholar] [CrossRef]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; Newman, E.; Nelson, S.D.; Nitiéma, P.; Pfefferbaum, R.L.; Rahman, A. Disaster media coverage and psychological outcomes: Descriptive findings in the extant research. Curr. Psychiatry Rep. 2014, 16, 464. [Google Scholar] [CrossRef] [PubMed]
- Nowicka, M.; Jarczewska-Gerc, E.; Marszal-Wisniewska, M. Response of Polish Psychiatric Patients to the Russian Invasion of Ukraine in February 2022-Predictive Role of Risk Perception and Temperamental Traits. Int. J. Environ. Res. Public Health 2022, 20, 325. [Google Scholar] [CrossRef] [PubMed]
- Sternik, I.; Solomon, Z.; Ginzburg, K.; Enoch, D. Psychiatric patients in war: A study of anxiety, distress and world assumptions. Anxiety Stress Coping 1999, 12, 235–246. [Google Scholar] [CrossRef]
- Wickham, S.R.; Amarasekara, N.A.; Bartonicek, A.; Conner, T.S. The Big Three Health Behaviors and Mental Health and Well-Being Among Young Adults: A Cross-Sectional Investigation of Sleep, Exercise, and Diet. Front. Psychol. 2020, 11, 579205. [Google Scholar] [CrossRef] [PubMed]
- Bloxham, L. What Is a Humanitarian Crisis? Available online: https://www.concern.org.uk/news/what-is-a-humanitarian-crisis (accessed on 5 June 2023).
- Abrash Walton, A.; Marr, J.; Cahillane, M.J.; Bush, K. Building Community Resilience to Disasters: A Review of Interventions to Improve and Measure Public Health Outcomes in the Northeastern United States. Sustainability 2021, 13, 11699. [Google Scholar] [CrossRef]
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef]
- Hobfoll, S.E.; Watson, P.; Bell, C.C.; Bryant, R.A.; Brymer, M.J.; Friedman, M.J.; Friedman, M.; Gersons, B.P.; de Jong, J.T.; Layne, C.M.; et al. Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry 2007, 70, 283–315. [Google Scholar] [CrossRef]
- Baran, M. Najpierw Pandemia, a Teraz Wojna—Czy Staniemy Się silniejsi? [First a Pandemic, Now a War—Will We Become Stronger?]. Available online: https://swps.pl/centrum-prasowe/informacje-prasowe/24295-najpierw-pandemia-a-teraz-wojna-czy-staniemy-sie-silniejsi (accessed on 2 April 2023).
- Raccanello, D.; Vicentini, G.; Rocca, E.; Barnaba, V.; Hall, R.; Burro, R. Development and Early Implementation of a Public Communication Campaign to Help Adults to Support Children and Adolescents to Cope with Coronavirus-Related Emotions: A Community Case Study. Front. Psychol. 2020, 11, 2184. [Google Scholar] [CrossRef]
- Vicentini, G.; Burro, R.; Rocca, E.; Lonardi, C.; Hall, R.; Raccanello, D. Development and evaluation of psychoeducational resources for adult carers to emotionally support young people impacted by wars: A community case study. Front. Psychol. 2022, 13, 995232. [Google Scholar] [CrossRef]
- Kurniawan, K.; Yosep, I.; Maulana, S.; Mulyana, A.M.; Amirah, S.; Abdurrahman, M.F.; Sugianti, A.; Putri, E.G.; Khoirunnisa, K.; Komariah, M.; et al. Efficacy of Online-Based Intervention for Anxiety during COVID-19: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sustainability 2022, 14, 12866. [Google Scholar] [CrossRef]
- Suwalska, J.; Suwalska, A.; Szczygieł, M.; Łojko, D. Medical students and stigma of depression. Part 2. Self-stigma. Psychiatr. Pol. 2017, 51, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Samochowiec, J.; Dudek, D.; Kucharska-Mazur, J.; Murawiec, S.; Rymaszewska, J.; Kubała, W.J.; Heitzman, J.; Jankowska-Zduńczyk, A.; Chatizów, J.; Bała, M. Diagnostyka i Leczenie Depresji u Dorosłych—Wytyczne dla Lekarzy Rodzinnych. [Diagnosis and Treatment of Depression in Adults—Guidelines for Family Physicians.]. Available online: https://wytyczne.org/bazawiedzy/wytyczne-postepowania-w-depresji-u-doroslych-dla-lekarzy-rodzinnych (accessed on 13 May 2023).
- Kowalski, J.; Elżanowski, A.; Śliwerski, A. A review of selected psychotherapies for PTSD, their efficacy and treatment guidelines in adults. Psychiatr. Pol. 2023, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fullana, M.A.; Hidalgo-Mazzei, D.; Vieta, E.; Radua, J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020, 275, 80–81. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental Health and the COVID-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Dobson, K.S.; Dozois, D.J. Risk Factors in Depression; Elsevier: Amsterdam, The Netherlands, 2011. [Google Scholar]
- Suwalska, J.; Napierała, M.; Bogdański, P.; Łojko, D.; Wszołek, K.; Suchowiak, S.; Suwalska, A. Perinatal Mental Health during COVID-19 Pandemic: An Integrative Review and Implications for Clinical Practice. J. Clin. Med. 2021, 10, 2406. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; Nitiéma, P.; Newman, E. Is Viewing Mass Trauma Television Coverage Associated with Trauma Reactions in Adults and Youth? A Meta-Analytic Review. J. Trauma Stress 2019, 32, 175–185. [Google Scholar] [CrossRef]
- AASM. Healthy Sleep Habits. Available online: https://sleepeducation.org/healthy-sleep/healthy-sleep-habits/ (accessed on 11 April 2023).
- Gupta, R.; Das, S.; Gujar, K.; Mishra, K.K.; Gaur, N.; Majid, A. Clinical Practice Guidelines for Sleep Disorders. Indian J. Psychiatry 2017, 59, S116–S138. [Google Scholar] [CrossRef]
- Hepsomali, P.; Groeger, J.A. Diet, Sleep, and Mental Health: Insights from the UK Biobank Study. Nutrients 2021, 13, 2573. [Google Scholar] [CrossRef]
- Suwalska, J.; Kolasińska, K.; Łojko, D.; Bogdański, P. Eating Behaviors, Depressive Symptoms and Lifestyle in University Students in Poland. Nutrients 2022, 14, 1106. [Google Scholar] [CrossRef]
- Papandreou, C.; Arija, V.; Aretouli, E.; Tsilidis, K.K.; Bulló, M. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID-19 outbreak: Cross-sectional analysis of two different confinement strategies. Eur. Eat. Disord. Rev. 2020, 28, 836–846. [Google Scholar] [CrossRef]
- Fredrickson, B.L.; Tugade, M.M.; Waugh, C.E.; Larkin, G.R. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J. Pers. Soc. Psychol. 2003, 84, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Santabárbara, J.; Lasheras, I.; Lipnicki, D.M.; Bueno-Notivol, J.; Pérez-Moreno, M.; López-Antón, R.; De la Cámara, C.; Lobo, A.; Gracia-García, P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 109, 110207. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.-J.; Zhao, K.; Fils-Aime, F. Response rates of online surveys in published research: A meta-analysis. Comput. Hum. Behav. 2022, 7, 100206. [Google Scholar] [CrossRef]
- Gustavson, K.; von Soest, T.; Karevold, E.; Røysamb, E. Attrition and generalizability in longitudinal studies: Findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Public Health 2012, 12, 918. [Google Scholar] [CrossRef]
| Characteristic | Survey 1 n = 72 | Survey 2 n = 34 | Survey 3 n = 22 | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Sex | ||||||
| Women | 60 | 83.3 | 26 | 76.5 | 11 | 50.0 |
| Men | 12 | 16.7 | 8 | 23.5 | 11 | 50.0 |
| Age | ||||||
| ≤39 years | 55 | 76.4 | 27 | 79.4 | 13 | 59.1 |
| >39 years | 17 | 23.6 | 7 | 20.6 | 9 | 40.9 |
| Place of residence | ||||||
| ≤50,000 inhabitants | 28 | 38.9 | 16 | 47.1 | 11 | 50.0 |
| >50,000 inhabitants | 44 | 61.1 | 18 | 52.9 | 11 | 50.0 |
| Education | ||||||
| No education, primary, secondary | 21 | 29.2 | 15 | 44.1 | 5 | 22.7 |
| Higher | 51 | 70.8 | 19 | 55.9 | 17 | 77.3 |
| Employment | ||||||
| Yes | 56 | 77.8 | 22 | 64.7 | 22 | 100.0 |
| No | 16 | 22.2 | 12 | 35.3 | 0 | 0.0 |
| Monthly income per person in the family | ||||||
| ≤2000 PLN | 12 | 16.7 | 5 | 14.7 | 0 | 0.0 |
| >2000 PLN | 60 | 83.3 | 29 | 85.3 | 22 | 100.0 |
| Marital status | ||||||
| Single | 35 | 48.6 | 16 | 47.1 | 8 | 36.4 |
| In a relationship | 37 | 51.4 | 18 | 52.9 | 14 | 63.6 |
| Living | ||||||
| Alone | 7 | 9.7 | 2 | 5.9 | 5 | 22.7 |
| With others | 65 | 90.3 | 32 | 94.1 | 17 | 77.3 |
| History of psychiatric treatment | ||||||
| Yes | 13 | 18.1 | 6 | 17.6 | 4 | 18.2 |
| No | 59 | 81.9 | 28 | 82.4 | 18 | 81.8 |
| Scale | Severity of Symptoms | p | ||||
|---|---|---|---|---|---|---|
| Survey 1 (S1) | Survey 2 (S2) | Survey 3 (S3) | S1 vs. S2 | S1 vs. S3 | S2 vs. S3 | |
| GAD-7 | 9.8 ± 5.2 | 7.0 ± 5.6 | 3.5 ± 3.5 | 0.038 * | <0.001 * | 0.054 |
| STAI X1 | 48.2 ± 10.4 | 45.2 ± 13.9 | 36.2 ± 11.1 | 0.802 | 0.001 * | 0.036 * |
| BDI | 10.4 ± 7.5 | 15.4 ± 12.7 | 6.1 ± 7.2 | 0.463 | 0.040 * | 0.003 * |
| Factor | GAD | STAI X-1 | BDI | ||||
|---|---|---|---|---|---|---|---|
| M ± SD | p | M ± SD | p | M ± SD | p | ||
| Gender | Female | 9.2 ± 5.4 | <0.001 * | 47.4 ± 11.6 | 0.004 * | 12.2 ± 9.6 | 0.004 * |
| Male | 4.1 ± 4.3 | 39.4 ± 12.5 | 7.3 ± 8.6 | ||||
| Income >2000 PLN # | No | 10.9 ± 5.4 | 0.020 * | 51.9 ± 9.9 | 0.020 * | 17.6 ± 9.9 | 0.002 * |
| Yes | 7.5 ± 5.5 | 44.2 ± 12.4 | 9.9 ± 9.1 | ||||
| Employment | No | 9.3 ± 6.0 | 0.188 | 51.2 ± 10.9 | 0.004 * | 16.4 ± 11.2 | 0.002 * |
| Yes | 7.6 ± 5.4 | 43.4 ± 12.2 | 9.5 ± 8.5 | ||||
| History of psychiatric treatment | Yes | 10.1 ± 6.9 | 0.103 | 49.7 ± 14.5 | 0.074 | 15.6 ± 13.0 | 0.103 |
| No | 7.5 ± 5.1 | 44.3 ± 11.6 | 9.9 ± 8.3 | ||||
| Good quality of sleep | No | 10.3 ± 5.8 | 0.007 * | 52.2 ± 10.3 | <0.001 * | 18.2 ± 9.8 | <0.001 * |
| Yes | 7.1 ± 5.2 | 42.6 ± 12.0 | 8.1 ± 7.8 | ||||
| Daily tracking of war news | Yes | 9.8 ± 5.5 | <0.001 * | 49.1 ± 11.2 | <0.001 * | 12.8 ± 10.1 | <0.011 * |
| No | 5.5 ± 4.7 | 40.5 ± 12.1 | 8.6 ± 8.3 | ||||
| Daily conversations about war | Yes | 9.9 ± 5.4 | <0.001 * | 49.8 ± 10.1 | 0.001 * | 12.5 ± 9.1 | <0.024 * |
| No | 6.4 ± 5.3 | 42.1 ± 12.8 | 9.8 ± 9.8 | ||||
| Good relations with close people | No | 7.8 ± 4.9 | 0.920 | 48.9 ± 10.9 | 0.015 * | 16.4 ± 9.9 | <0.001 * |
| Yes | 8.0 ± 5.8 | 43.8 ± 12.6 | 8.9 ± 8.6 | ||||
| Fear of an armed attack on Poland | Yes | 10.4 ± 5.4 | <0.001 * | 51.1 ± 9.6 | <0.001 * | 13.8 ± 9.8 | <0.001 * |
| No | 5.8 ± 4.8 | 40.3 ± 12.3 | 8.5 ± 8.7 | ||||
| Impact of war on the sense of security | Yes | 11.0 ± 5.2 | <0.001 * | 50.6 ± 9.5 | <0.001 * | 12.7 ± 8.9 | <0.004 * |
| No | 5.0 ± 4.2 | 41.0 ± 12.7 | 9.4 ± 9.8 | ||||
| Concerns about worsening of financial situation due to war | Yes | 8.2 ± 5.6 | 0.132 | 46.2 ± 12.4 | 0.031 * | 11.6 ± 9.6 | <0.006 * |
| No | 5.8 ± 4.9 | 38.7 ± 9.4 | 5.2 ± 6.9 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kasierska, M.; Suwalska, J.; Łojko, D.; Jakubiak-Głowacka, M.; Tobis, S.; Suwalska, A. Symptoms of Anxiety and Depression in Polish Population in the Context of the War in Ukraine: Analysis of Risk Factors and Practical Implications. Sustainability 2023, 15, 14230. https://doi.org/10.3390/su151914230
Kasierska M, Suwalska J, Łojko D, Jakubiak-Głowacka M, Tobis S, Suwalska A. Symptoms of Anxiety and Depression in Polish Population in the Context of the War in Ukraine: Analysis of Risk Factors and Practical Implications. Sustainability. 2023; 15(19):14230. https://doi.org/10.3390/su151914230
Chicago/Turabian StyleKasierska, Maria, Julia Suwalska, Dorota Łojko, Marta Jakubiak-Głowacka, Sławomir Tobis, and Aleksandra Suwalska. 2023. "Symptoms of Anxiety and Depression in Polish Population in the Context of the War in Ukraine: Analysis of Risk Factors and Practical Implications" Sustainability 15, no. 19: 14230. https://doi.org/10.3390/su151914230








