Abstract
Background: The COVID-19 pandemic put considerable strain on individual mental health. The current study aimed to determine the prevalence and severity of insomnia symptoms among students and employees during this period. Methods: This paper is a cross-sectional analysis using convenience sampling. A web-based anonymous survey was developed and included questions about socio-demographic characteristics, contact with COVID-19, and the Athens Insomnia Scale. Results: 620 participants, 331 students, and 289 employees were included in the final sample. According to the current findings, 21.29% (n = 132) of participants met the criteria for insomnia, and 39.03% (n = 242) met the criteria for mild sleep disturbances. Conclusions: Although respondents reported an increased prevalence of sleep disorders, these changes were not directly related to the presence or severity of the infection but rather to a variety of socio-demographic and lifestyle-related variables. Students associated more frequently with the next-day consequences of insomnia (overall functioning and sleepiness during the day), while for employees, the most prevalent were awakenings during the night and early morning awakenings. Furthermore, sleep difficulties were more prevalent in women, single people, sedentary people, and those with psychiatric disorders.
1. Introduction
The novel coronavirus disease, or COVID-19, is an acute respiratory illness caused by a newly discovered Severe Acute Respiratory Syndrome Corona-2 virus (SARS-CoV-2) that emerged in December 2019 [1,2]. During the last two years, the COVID-19 pandemic has drastically altered everyday life for much of the world’s population, thus putting individuals under heavy stress and causing considerable disruption [3]. Following social distancing and economic insecurity, significant increases in mental health concerns arose, including loneliness, anxiety, or depression, contributing to poor sleep quality [4,5,6,7,8].
Sleep is a crucial physiological process for maintaining physical and mental health with a wide impact on Quality of Life (QOL) [9,10]. Disruptions to regular sleep cycles can cause sleep deprivation and extended awareness, thereby increasing the chance of insomnia, daytime instability, nightmares, and weariness. Studies indicate that sleep disturbances affect up to one-quarter of individuals [11] and are associated with a variety of negative health effects, such as an increased risk of hypertension, obesity, diabetes, metabolic syndrome, cerebrovascular disorders, musculoskeletal illnesses, cancer, and septicemia [9,10,12]. Potential risk factors for sleep difficulties include severe stress, sadness, anxiety, trauma, poor socioeconomic position, urban life, increasing use of technology, and social media [9,10,11,13].
The prevalence of sleep difficulties in the general population is very high [14], and its socioeconomic consequences may be most obvious in the active population, namely students and employees (i.e., whose disruption carries the most weight in terms of lost productivity). Especially among the former, schedules have shifted in the last two years due to the COVID-19 pandemic. The lockdown prompted educational institutions to adapt, allowing students to reschedule their study hours since they were no longer obligated to attend early classes. All these changes to teaching and schedules contributed to sleep disturbances and diminished academic performance [15,16,17].
The incidence of poor sleep quality is believed to be approximately 60% or even higher among university students [18]. Previous research has shown that disturbed sleep patterns may result in poor performance, behavioral changes, and dietary changes [19,20,21,22]. Although the effects of the current pandemic on sleep are not fully understood, we do know that the population spent more time in bed, used digital devices at bedtime, went to bed later, and experienced a decline in sleep quality [23]. Even so, the changes to sleep behaviors brought on by pandemic stressors are subject to much individual variation [12].
Such changes are of particular interest when taking into account sleep’s implications in both mental and physical health [20,24]. Sleep disorders can impair decision-making and psychological functioning; expose the immune system; lead to mood changes; increase the risk of accidents; increase medical expenditures; and negatively affect cognitive abilities, rendering individuals more susceptible to contracting the virus [25].
To make matters worse, even before the pandemic, Romania’s health system was already limited by budgetary restraints that made it hard to provide medical services equitably. Shortly after the start of the pandemic, the country’s health system had to quickly adapt and allocate resources in a manner that was both financially viable and fair for people with different illnesses while also focusing on preventive medicine principles and ensuring equitable, global access to COVID-19 diagnostics, vaccination, and therapy [26,27]. Mental health was particularly affected by COVID-19: inpatient admission for psychotic and affective disorders dropped sharply during the pandemic, increasing after the restrictions were raised but still remaining below pre-pandemic levels, reflecting lower accessibility despite the increase in their prevalence [8,28]. An epidemiological snapshot into sleep disorders in Romanian’s active population can prove informative for both clinicians and policymakers and lead to more precise, cost-effective, and sustainable interventions for this vulnerable segment of the population.
Therefore, the main objective of this study was to explore the prevalence and severity of insomnia in students and employees during the COVID-19 pandemic and to determine the risk and protective factors associated with the quality of sleep. While the study mainly looks at both employees and students as a single group, it also briefly looks into the characteristic sleep disturbance differences in each sub-group.
2. Materials and Methods
2.1. Participants and Procedures
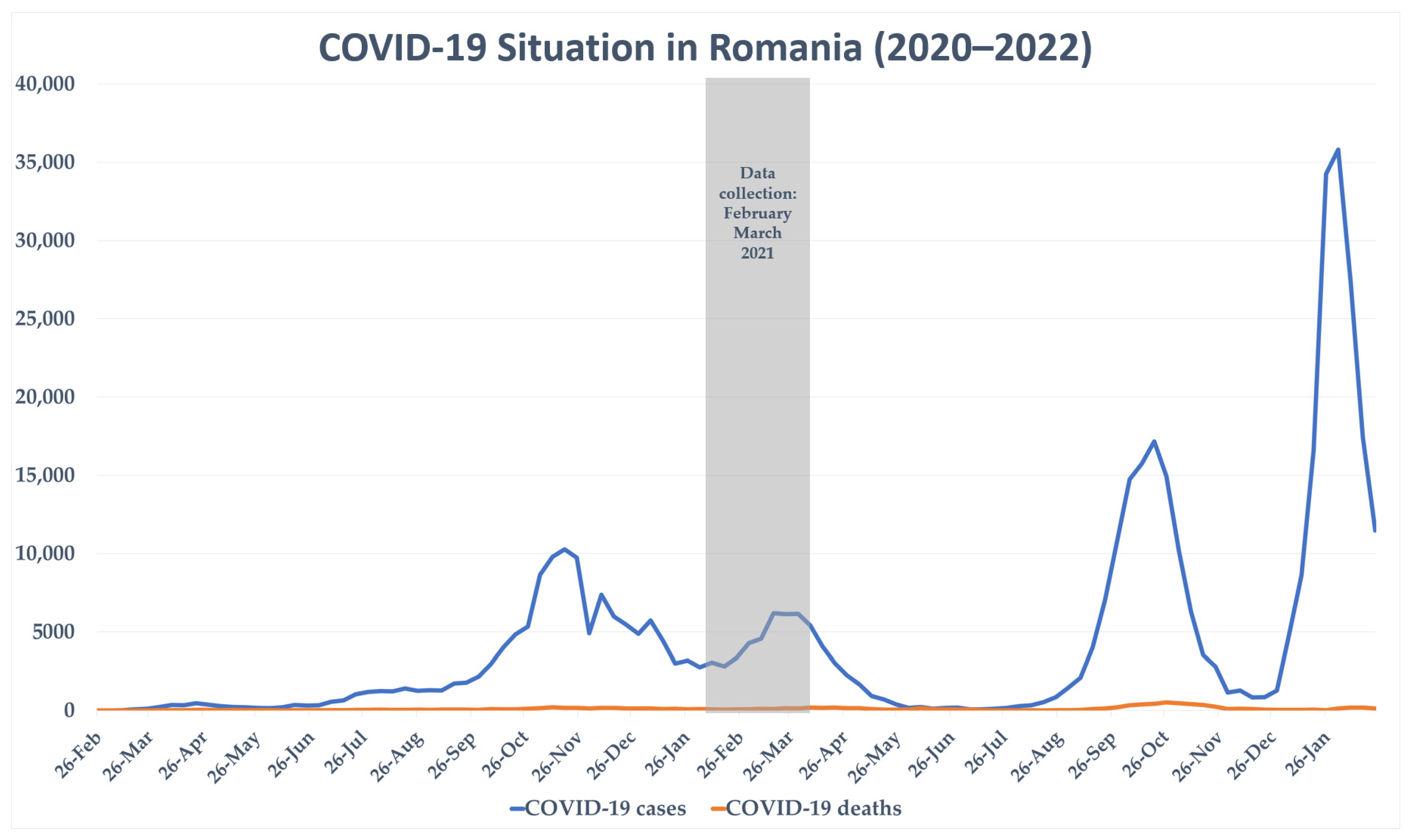
The current study is a cross-sectional investigation, with data collected between February and March of 2021, during the alpha wave of COVID-19 Pandemic (Figure 1). Social media and other communication platforms (Twitter®, Facebook®, Instagram®, and WhatsApp®) were used to advertise the online questionnaire. The questionnaire was distributed with the support of a non-governmental group that has access to about 150,000 individuals via Romania’s major social media platforms and was pushed to this audience. The organization’s principal source of income is the promotion of various products or services to this sample. This sample includes persons of various ages, jobs, and socioeconomic classes; they have no direct relationship to the organization’s principal theme. This was conducted to ensure that the questionnaire received objectively high publicity among Romanians and internet users while avoiding the possibility of collection errors caused by directing the questionnaire primarily to specific social or professional groups.
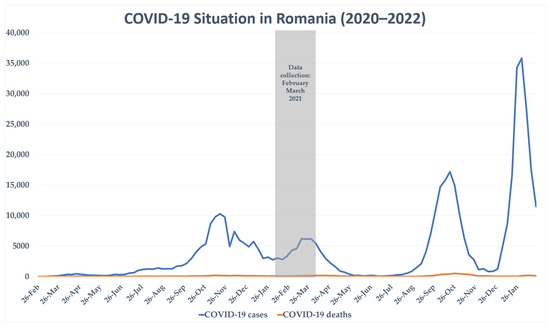
Figure 1.
COVID-19 situation in Romania during recruitment. Data from Johns Hopkins University.
2.2. Quality Control
The same IP address could only provide one response, and all entries were marked as mandatory. The questionnaire was only emailed after all items had been completed. Otherwise, the system marked the result as incomplete. Participants completed the questionnaire after agreeing to an electronic informed consent request for each participant. The survey took approximately 10 min to complete. Inclusion in the study group was based on student or employee status.
The study sample size was estimated using the Raosoft sample size calculator. A minimum of 385 participants were required at a margin error of 5%, with a 95% confidence interval (CI), for a population size of 6 million people (the total number of students and employers in Romania) at a 50% response distribution. The final sample consisted of 620 participants, 331 students, and 289 workers.
The study was developed in accordance with the World Health Organization (WHO), the Declaration of Helsinki, European Union legislation, and the ethical principles of clinical research of the Guidelines for Good Clinical Practice (ICH-GCP).
The protocol and the informed consent were approved by the Ethical Committee of the College of Physicians of Bacau (approval number 46/18 January 2021).
2.3. Measures
Demographic variables: The questionnaire included a short segment which inquired about the following: occupational status (“student”, “employed”); gender (“male” and “female”); age (“18–24 yrs”, “25–34 yrs”, “35–44 yrs”, “45–54 yrs”, “55–64 yrs”, and “65 or more yrs” (for the regression analysis, the two highest categories were combined to represent “55+ yrs”)); marital status (“married”, “cohabitating couple”, “single”, “divorced”, “widowed”); household composition (“living alone”, or living with “partner”, “children”, “parents”, “grandparents”, “siblings”, “friends/flat-mates”, “others”); current caretaking of an elderly person; pet ownership; residency (“urban”, “rural”); level of education (“high school graduation”, “Bachelor’s degree”, “Master’s degree”, “Doctoral degree”, “postdoctoral studies”); monthly income (“0–€99/person”, “€100–€199/person”, “€200–€399/person”, “€400–€799/person”, “€800–€1599/person”, “€1600 or more/person”) and working time (“under 10 h/week”, “10 to 20 h/week”, “20 to 40 h/week”, “40 to 60 h/week”, “over 60 h/week”).
Medical and psychiatric comorbidities: Participants were questioned about any medical and/or mental problems they may have. Those who responded to the preceding questions by stating that they had medical and/or psychiatric comorbidities were asked to define the diagnosis. For the regression analysis, the responses were classified as follows: cardiovascular, pulmonary, endocrinologic, diabetic, and metabolic, other comorbidities (for physical conditions), and major depressive disorder, anxiety disorder, and other disorders (for psychiatric disorders).
Lifestyle-related characteristics: The questionnaire also included questions that assessed lifestyle and behavioral characteristics. Physical activity during the last month was evaluated according to intensity. Smoking history was assessed by accounting for both frequency and history of past use, while alcohol was only evaluated for frequency in standard units (Table A1). For the regression analysis, the response variables of smoking and alcohol consumption were combined as smokers and non-smokers, and no alcohol consumption, occasional alcohol consumption, and daily alcohol consumption, respectively.
COVID-19: Participants were asked whether they had gone through the infection and, in case of a positive answer, were further required to state the severity/intensity of their symptoms. They were also asked if they had loved ones who had been diagnosed with COVID-19 and a separate question about close ones who passed away because of complications from the infection.
Athens Insomnia Scale: This scale is an eight-item instrument designed for quantifying sleep difficulty based on the ICD-10 criteria [29]. The first five items pertain to sleep induction, awakenings during the night, final awakening, total sleep duration, and sleep quality, while the last three refer to well-being, functional capacity, and sleepiness during the day. Each item is scored on a scale ranging from 0 to 3 (with 0 corresponding to “no concern” and 3 to a “very serious concern”). The respondents were required to provide a positive rating if they experienced the sleep difficulty described by each item at least three times a week during the last month.
The AIS has shown reasonable validity and reliability indicators in the Romanian population [30]. In the present study, high internal consistency (Cronbach’s alpha of 0.83 and McDonald’s Omega ML of 0.84) was observed for the AIS.
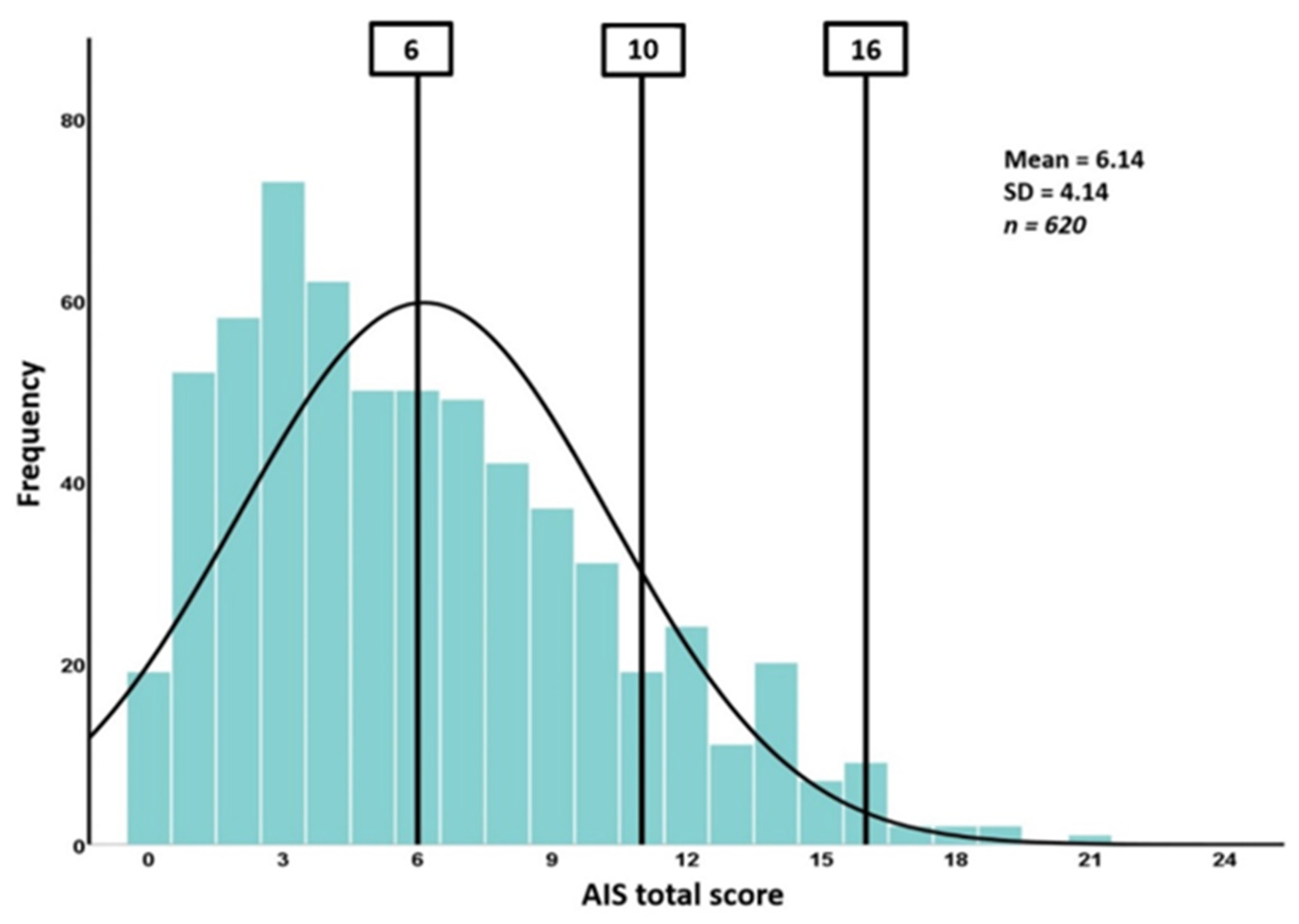
A score from 0 to 5 indicates normal sleep; from 6 to 10, mild problems with sleep; and a score of 11 and above corresponds to insomnia. A new range of cut-offs for AIS was proposed, and the severity criteria were capable of categorizing insomnia severity as follows: absence of insomnia (0–5), mild insomnia (6–9), moderate insomnia (10–15), and severe insomnia (16–24) [31]. When diagnosing individuals with a score of 6 or higher as insomniacs, the scale presents with 93% sensitivity and 85% specificity (90% overall correct case identification). For this cut-off score in the general population, the scale has a positive predictive value of 41% and a negative predictive value of 99% [29]. Based on the cut-offs proposed by Soldatos, the new cut-offs proposed in 2020 have the advantage of staging the severity of symptoms. In practice, this staging adds two new cut-offs that divide patients with insomnia criteria (over 10 points) into two groups: moderate (10–15) and severe (over 15 points).
2.4. Statistical Analysis
IBM® SPSS® Statistics version 26 was used to analyze the data (IBM®, Armonk, NY, USA) and perform descriptive statistics and significance tests. The Chi-Square test, the corrections when the criteria were not met (Likelihood ratio, Fisher test), and the Phi and Cramer V parameters were used to check the interval combinations. The t-independent test with the reporting of the degrees of release, the difference in means, the Levene′s test for the homogeneity test, the Kolmogorov–Smirnov and Shapiro–Wilk normality tests for the subgroups with less than 30 respondents, and the confidence interval was also used to check the interval combinations. Where the conditions of the normality tests were not met, the non-parametric Mann–Whitney U test was used. The ANOVA test, the Levene’s and Welch tests were also used.
3. Results
The final sample consisted of 620 participants (331 students and 289 workers). Most of the respondents were female (74.8%, n = 464), and four out of five were young adults aged between 18 and 34 years (82.3%, n = 511). Most participants (65.8%, n = 408) were in a relationship, while the rest of them were either single, divorced, or widowed (Table A1).
The vast majority (91.8%, n = 569) of the respondents were living in urban areas. More than half (57.1%, n = 354) of the respondents have an academic degree (either Bachelor’s, Master’s, or Ph.D.) (Table A2).
About 10.3% of respondents (n = 64) suffered from a pre-existing physical illness, mainly pulmonary diseases (3.6%, n = 22), cardiovascular diseases (3.1%, n = 19), as well as diabetes and metabolic disorders (1.8%, n = 11). Regarding mental disorders, 6.7% (n = 42) were reported to have a pre-existing diagnostic, with the most common being major depressive and anxiety disorders (Table A3).
In terms of lifestyle characteristics, two-thirds (67.3%, n = 417) reported engaging in physical activity ranging from mild to intense (Table A4). 65.0% (n = 403) of participants did not smoke at the time of the survey, while the solid majority (61.5%, n = 381) described themselves as occasional drinkers.
Regarding COVID-19 disease, 16% (n = 100) tested positive for SARS-CoV-2, of which 65% had a mild form. A great number of individuals had close relatives/friends that tested positive for COVID-19, and 7.1% had close relatives/friends who died of COVID-19 (Table A5).
For our study, Cronbach’s Alpha for the total group was 0.832. Using the predefined cut-offs of the AIS scoring system to screen for insomnia, we found that every second participant in the survey (n = 374, 60.32%) presented insomnia symptoms (Figure 2). With scores between 6 and 10, more than one-third of the respondents (n = 242, 39.03%) screened positive for mild sleep problems, while 132 (21.29%) of them screened positive for insomnia (score ≥ 11).
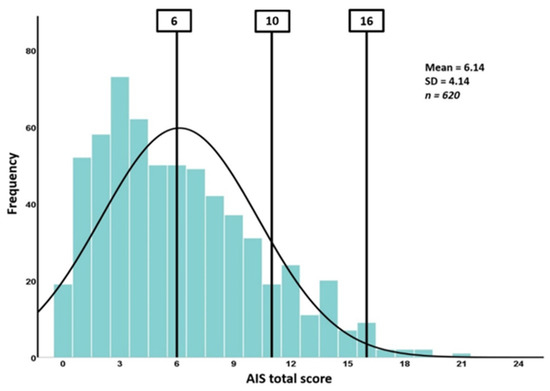
Figure 2.
The severity of sleep-related problems according to AIS. AIS (Athens Insomnia Scale); the severity criteria of the AIS were categorizing insomnia severity as follows: absence of insomnia (0–5), mild insomnia (6–9), moderate insomnia (10–15), and severe insomnia (16–24).
In the student group, sleep induction was more affected compared to the employees’ group (p = 0.013, df = 3, Phi = 0.132, moderate association) (Table 1). Perception of physical and mental functioning during the day (p < 0.001, df = 3, Phi = 0.206, strong association) and sleepiness during the daytime (p < 0.001, df = 3, Phi = 0.189, strong association) are more prevalent among students. In contrast, awakenings during the night are more prevalent among employees (p < 0.001, df = 3, Phi = 0.185, strong association), and the final awakening is also found to be earlier than desired (p = 0.002, df = 3, Phi = 0.155, strong association).

Table 1.
Bivariate analysis for the association between individual-level variables and insomnia score on AIS (n = 620).
Single people (divorced, widowed, single) experienced more awakenings during the night compared to those who are married or in a relationship (p < 0.001, df = 12, Phi = 0.369, strong association). On the other hand, married people tend to (p = 0.040, df = 12, Phi = 0.184, strong association).
Regarding household size and structure, participants who lived with their partners reported falling asleep easier (p = 0.008, df = 3, Phi = 0.150, strong association) and less daytime sleepiness (p = 0.019, df = 3, Phi = 0.139, moderate association). Partnered individuals also experienced higher levels of perceived functionality (p = 0.022, df = 3, Phi = 0.136, moderate association). Participants who lived with their partner had normal scores on AIS, lower than 5 (p = 0.024, df = 1, Phi = 0.099, weak association).
Studied participants that were living with their children experienced more frequent awakenings during the night (p = 0.018, df = 2, Phi = 0.116, moderate association) but less daytime sleepiness (p = 0.001, df = 1, Phi = 0.146, moderate association) and better functioning during the day (p = 0.001, df = 3, Phi = 0.176, strong association), in contrast with participants living with their parents. Living with grandparents was associated with a longer time to fall asleep (p < 0.001, df = 3, Phi = 0.211, strong association) and worse quality of sleep (p = 0.020, df = 3, Phi = 0.138, moderate association). A worse quality of sleep was also observed in the participants who lived with a roommate (p = 0.027, df = 3, Phi = 0.133, moderate association), who also declared a worse state of well-being during the day (p = 0.023, df = 3, Phi = 0.135, moderate association).
Taking care of an older person was associated with a delay in falling asleep (p = 0.037, df = 3, Phi = 0.117, moderate association) and waking before the desired time (p = 0.003, df = 3, Phi = 0.173, strong association). Participants who care for older people often had more clinically significant scores on the AIS (p = 0.024, df = 3, Phi = 0.091, weak association).
Pet owners have a shorter duration of falling asleep (p = 0.036, df = 3, Phi = 0.117, moderate association). However, they experience more sleepiness during the day (p = 0.028, df = 3, Phi = 0.121, moderate association). However, in terms of the AIS total score, there are no differences between pet owners and those who do not own pets.
Respondents from urban areas reported a lower quality of sleep, according to AIS scores (p = 0.035) (Table 2). Lower educational levels were associated with higher levels of dysfunctionality during the day (p < 0.001, df = 2, Phi = 0.199, strong association). Nonetheless, the AIS total score was not statistically significant and not influenced by educational level.

Table 2.
Bivariate analysis for the association between socio-demographic characteristics and insomnia score on AIS (n = 620).
Low- and middle-income participants took longer to fall asleep (p = 0.046, df = 15, Phi = 0.217, strong association), while higher-income participants reported feeling more sluggish during the day (p = 0.014, df = 15, Phi = 0.224, strong association). Despite these particularities, no difference in AIS total score was associated with monthly income (p = 0.233). In relation to weekly working hours, people who work more often feel that sleep duration is not enough (p = 0.050, df = 12, Phi = 0.181, strong association).
Sedentary participants scored higher on the AIS scale (p = 0.001, df = 4, Phi = 0.175, moderate association) (Table 3). Less active participants had overall less sleep (p = 0.039, df = 12, Phi = 0.179, strong association), worse quality of sleep (p = 0.004, df = 12, Phi = 0.217, strong association), lower day functioning (p = 0.001, df = 1, Phi = 0.228, strong association), and experienced more somnolence during waking hours (p = 0.001, df = 12, Phi = 0.207, strong association).

Table 3.
Bivariate analysis for the association between lifestyle-related characteristics and insomnia score on AIS (n = 620).
Smokers reported greater difficulty falling asleep (p = 0.004, df = 3, Phi = 0.147, moderate association), more frequent awakenings during the night (p = 0.014, df = 3, Phi = 0.131, moderate association), unsatisfactory total sleep time (p 0.001, df = 3, Phi = 0.231, strong association), and unsatisfactory sleep quality (p = 0.001, df = 3, Phi = 0.167, moderate association). Furthermore, smokers scored significantly higher AIS scores compared to non-smokers (p 0.001, df = 1, Phi = 0.144, moderate association). There were no differences in AIS scores related to alcohol consumption (no alcohol, occasionally, daily) (p = 0.741).
As expected, participants with psychiatric comorbidities exhibited clinically significant scores (over 6) on the AIS more frequently than participants without psychiatric comorbidities. In the studied group, psychiatric ailments were associated with more awakening during the night (p = 0.001, df = 3, Phi = 0.206, strong association), awakening before the desired time (p = 0.029, df = 3, Phi = 0.146, moderate association) and unsatisfactory total duration and quality of sleep (p = 0.035, df = 3, Phi = 0.118, moderate association; p = 0.003, df = 3, Phi = 0.150, strong association). Furthermore, participants with mental disorders experienced the following consequences of insomnia: decreased well-being (p = 0.001), worse functioning (p = 0.001), and somnolence (p = 0.010). Participants with mental disorders, after all, had higher AIS scores (p 0.001, df = 1, Phi = 0.165, strong association). In terms of physical comorbidities, respondents who reported having at least one such comorbidity reported having higher difficulty initiating sleep (p = 0.020) as well as daytime sleepiness (p = 0.004).
Surprisingly, regarding COVID-19, there were no significant differences between participants in the study who were infected with SARS-CoV-2 and those unaffected. There was no difference on the insomnia scale in relation to the time interval elapsed since infection with SARS-CoV-2 or the severity of associated symptoms of the infection. Moreover, infection or death due to COVID-19 of loved ones is not a risk factor for sleep disturbances in the studied group.
4. Discussion
This web-based study revealed a few interesting aspects related to insomnia. Numerous studies have reported a significant increase in the prevalence of insomnia in the general population during the current pandemic, with this increase being attributed to a range of factors in varying proportions, including fear of infection of oneself or loved ones or fear of financial insecurity [32,33,34,35]. Distress levels rise during an infection outbreak due to worry about health, changes in social life and daily routine, and finally, financial concerns [36,37,38].
In this study, more than 21.29% (n = 132) of the participants scored above the cut-off score for insomnia. This percentage is at the upper limit of the worldwide insomnia prevalence, estimated before the pandemic between 3.9% and 22% [39]. More than a third, 39.03% (n = 242), screened positive for minor problems with sleep. All these results indicate an exacerbation of sleep disturbances. According to a meta-analysis, the prevalence of sleep problems during the COVID-19 pandemic is high and affects approximately 40% of the general population [40].
According to the current study, although there is a high prevalence of sleep disorders among respondents, these changes were not directly associated with the presence of the infection or its severity but rather with various demographic and socioeconomic variables and, finally, with the presence of a pre-existing psychiatric disorder.
On the report of these results, the risk of insomnia symptoms was higher among women and those who live in urban areas. This trend may have been amplified in the current research by the fact that those are more likely to utilize social media and are, therefore, overrepresented in our sample. Nevertheless, a previous study from Greece, where the authors used a similar methodology as we did in studying insomnia (an online survey included questions regarding socio-demographic variables and contact with COVID-19, as well as the AIS), indicated that 37.6% (n = 233) of the participants scored over the insomnia cut-off level [41]. As expected, older age was associated with an increase in awakenings during the night. The results of this study could indicate that insomnia relates to psychological responses to the COVID-19 epidemic and poor sleep hygiene, with women and residents of urban areas being more susceptible to sleep disturbance.
Partnered (married or cohabiting) participants at the time of the sleep study had better sleep quality, while sleep impairment was substantially correlated with loneliness. These results correspond to the findings of previous studies, which have demonstrated that co-sleeping with a partner is related to an improvement in sleep quality as well as a reduction in the daily manifestations of insomnia [42,43,44].
Participants who took care of older people had more frequent sleep disturbances, with elderly care being associated with a delay in falling asleep and waking up before the desired time. Most respondents indicated that they cared for at least one elderly person, which is most likely related to Romania’s distinct culture [45,46]. Additionally, Romania, like other southern and eastern European countries, is characterized by cultural norms associated with strong family ties, attitudes toward family care, and mutual intergenerational support [47,48]. The distinctions could be partly explained by Romania’s economic and housing crises. In general, it seems likely that the value placed on family ties grew in Romania following the collapse of the socialist regime. In terms of sleep disturbance, this can be explained in part by the high rates of stress indicated by people who self-identify as informal caregivers of the elderly and by the fact that this age bracket is the most vulnerable to the SARS-CoV-2 infection [49,50].
Sedentary people had worse quality of sleep and presented higher AIS scores. In contrast, engaging in mild, moderate, or vigorous physical exercise was associated with improved sleep quality. Physical activity is widely regarded as a non-pharmacologic intervention that improves sleep and, hence, one of the most important interventions in managing and treating insomnia, including COVID-19-related sleep disturbances [51,52,53]. Sedentary people had worse sleep quality and self-reported higher AIS scores. In contrast, engaging in mild, moderate, or vigorous physical exercise is associated with improved sleep quality. Physical activity is widely regarded as a non-pharmacologic habit that improves sleep; hence, it is advised as a treatment for those with sleep difficulties [51,52]. Furthermore, regular exercise is a valuable preventive intervention and treatment factor in the management of COVID-19-related sleep disturbances and other mental disorders [53].
Consistent with previous studies, our results showed a significant association between smoking and low quality of sleep. Those who smoked cigarettes were more likely to suffer from insomnia [54,55].
The presence of psychiatric or physical comorbidities impaired sleep quality in the study population. Sleep disturbances are a diagnostic criterion for psychiatric diseases such as major depressive disorder and bipolar disorder and are, therefore, more likely to be established during the evaluation [56]. On the other hand, when it comes to physical comorbidities, there is a frequent risk of not evaluating sleep disorders clinically, even though multiple studies demonstrate a statistical association between sleep and morbidity [57]. Numerous studies report that, in addition to enhancing the overall quality of life, improved sleep quality relates to an increase in treatment compliance and efficacy [58,59,60].
Comparing the two main sub-groups in the study showed that students presented more frequent consequences of insomnia (overall functioning and sleepiness during the day), while workers reported a higher number of awakenings during the night and early mornings. Concerning the high prevalence of insomnia among students, there is a substantial body of study on the subject, even before the pandemic [61,62,63]. Moreover, the pandemic’s emergence resulted in several significant changes to students’ lifestyles and daily experiences (e.g., light exposure, social relationships, work schedules, physical activities, family management, and the use of electronic devices), all of which are associated with changes in mood, stress levels, and sleep [18,64,65,66]. A recent study conducted between March and June 2021 found that a sample of students attending a large Italian university had significant rates of poor sleep quality and insomnia, with up to 65% reporting poor sleep quality and 33% reporting a habitual sleep duration of fewer than 7 h. This study also found a strong connection between the main components of sleep quality and physical and mental health-related quality of life after considering health-related characteristics and perceived stress [67]. Another study looked at one of the factors usually associated with lower quality of sleep, namely the use of social media, and painted a more nuanced picture, showing its many benefits during the pandemic despite its potential impact on sleep [68].
Despite our findings, such a study design presents important limitations that need to be considered when interpreting the data. On the one hand, the use of a self-reported questionnaire is prone to response (extreme response, social desirability) and recall (inaccurate memory) biases. On the other hand, online surveys suffer from two main methodological limitations: restricted access to certain portals and respondents with biases may select themselves into the sample; thus, more robust research on insomnia during a pandemic crisis is necessary. The study takes into account the subject’s self-reporting of any formal medical diagnoses or psychological assessments and provides no means of verifying their validity. For all these reasons, the generalizability of the reported findings may be restricted, and caution should be exercised when comparing them to earlier findings. Furthermore, our study was cross-sectional, and no causal implications can be derived from the data; longitudinal studies should be conducted to untangle and better understand the distinctive bidirectional interplay between sleep and the risk and protective factors. Finally, it should be noted that since the study was conducted during the early stages of the COVID-19 vaccination, its beneficial effects on stress associated with SARS-CoV-2 infection and possible indirect effects on sleep quality cannot be determined [69,70].
5. Conclusions
Insomnia is a major health issue associated with great psychological burdens. This study uncovered high levels of self-reported insomnia among professionally active (non-retired) adults during the COVID-19 pandemic. Women, single individuals, sedentary individuals, and those with psychiatric conditions were more vulnerable to sleep disturbances. It is important to recognize and treat insomnia in stressful situations such as the COVID-19 pandemic. Doctors should be trained to evaluate and treat sleep disturbances, as this all-around approach could reduce psychological stress and stop the development of other mental health disorders. Furthermore, access to medical treatments for psychological first aid during significant disasters should be bolstered.
Author Contributions
Conceptualization, T.C.I., B.I.F., S.Z., E.-M.M. and C.T.; methodology, T.C.I., S.Z. and C.T.; software, T.C.I., S.Z. and E.-M.M.; validation, B.I.F., S.Z. and C.T.; formal analysis, T.C.I., S.Z., E.-M.M. and C.T.; investigation, T.C.I. and S.Z.; resources, T.C.I., B.I.F., S.Z., E.-M.M. and C.T.; data curation, T.C.I., B.I.F., S.Z., E.-M.M. and C.T.; writing—original draft preparation, T.C.I., B.I.F. and C.T.; writing—review and editing, B.I.F., S.Z. and C.T.; visualization, T.C.I., B.I.F., S.Z., E.-M.M. and C.T.; supervision, C.T.; project administration, T.C.I. and B.I.F.; funding acquisition, T.C.I., B.I.F., S.Z., E.-M.M. and C.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of the Ethical Committee of the College of Physicians of Bacau (approval number 46/18 January 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Individual-level variables.
Table A1.
Individual-level variables.
| Lot Characteristics | Answers | n (%) | |
|---|---|---|---|
| Occupational status | Student | 331 (53.4%) | |
| Employees | 289 (46.6%) | ||
| Gender | Male | 156 (25.2%) | |
| Female | 464 (74.8%) | ||
| Age groups | 18 to 24 years | 374 (60.3%) | |
| 25 to 34 years | 137 (22.1%) | ||
| 35 to 44 years | 44 (7.1%) | ||
| 45 to 54 years | 35 (5.6%) | ||
| 55 years and over | 30 (4.9%) | ||
| Marital status | No relationship 212 (34.2%) | Divorced | 11 (1.8%) |
| Widowed | 3 (0.5%) | ||
| Single | 198 (31.9%) | ||
| In a relationship 408 (65.8%) | Cohabitating couple | 293 (47.3%) | |
| Married | 115 (18.5%) | ||
| Household size and composition | Living alone | 99 (15.8%) | |
| Living with somebody else 521 (84.2%) | Partner | 249 (40.2%) | |
| Children | 82 (13.2%) | ||
| Parents | 236 (38.1%) | ||
| Grandparents | 36 (5.8%) | ||
| Siblings | 92 (14.8%) | ||
| Friends/Flat-mates | 41 (6.6%) | ||
| Others | 7 (1.1%) | ||
| Taking care of an older person | Yes | 574 (92.6%) | |
| No | 46 (7.4%) | ||
| Pet owner | Yes | 250 (40.3%) | |
| No | 370 (59.7%) | ||
Values are depicted as percentages and numerical data.

Table A2.
Socio-demographic characteristics.
Table A2.
Socio-demographic characteristics.
| Lot Characteristics | Answers | n (%) |
|---|---|---|
| Residency | Urban | 569 (91.8%) |
| Rural | 51 (8.2%) | |
| Education level | High School Graduation | 266 (42.9%) |
| Bachelor’s Degree Certificate | 229 (36.9%) | |
| Master’s Degree Certificate | 117 (18.9%) | |
| Doctoral Degree Certificate and Postdoctoral studies | 8 (1.3%) | |
| Family/personal income * | 0–€99/person | 20 (3.4%) |
| n = 586 | €100–€199/person | 54 (9.2%) |
| €200–€399/person | 104 (17.7%) | |
| €400–€799/person | 216 (36.9%) | |
| €800–€1599/person | 136 (23.2%) | |
| €1600 or more/person | 56 (9.6%) | |
| Number of hours of weekly work ** | Under 10 h/week | 119 (19.2%) |
| 10 to 20 h/week | 66 (10.6%) | |
| 20 to 40 h/week | 204 (32.9%) | |
| 40 to 60 h/week | 195 (31.5%) | |
| Over 60 h/week | 36 (5.8%) |
Values are depicted as percentages and numerical data. * A total of 36 respondents chose not to respond; ** Does not include time spent by students studying online/on campus.

Table A3.
Physical and psychiatric comorbidities.
Table A3.
Physical and psychiatric comorbidities.
| Lot Characteristics | Answers | n (%) |
|---|---|---|
| Do you have any psychical comorbidities? | Yes | 64 (10.3%) |
| No | 556 (89.7%) | |
| Physical condition(s) * | Cardiovascular | 19 (3.1%) |
| Pulmonary | 22 (3.6%) | |
| Endocrine | 9 (1.5%) | |
| Diabetic and Metabolic | 11 (1.8%) | |
| Others | 10 (1.6%) | |
| Have you ever been diagnosed with any psychiatric disorders? | Yes | 42 (6.7%) |
| No | 578 (93.3%) | |
| Psychiatric diagnosis | Major depressive disorder | 18 (2.9%) |
| (n = 42) | General anxiety disorder | 16 (2.6%) |
| Others | 8 (1.4%) |
Values are depicted as percentages and numerical data. * Comorbidities are not mutually exclusive. A total of 7 participants had two or more physical comorbidities.

Table A4.
Physical activity and smoking and drinking habits.
Table A4.
Physical activity and smoking and drinking habits.
| Lot Characteristics | Answers | n (%) |
|---|---|---|
| Physical activity | Sedentary | 203 (32.7%) |
| Mild | 249 (40.2%) | |
| Moderate | 119 (19.2%) | |
| Intense | 49 (7.9%) | |
| Smoking status | No, I have never smoked | 277 (44.7%) |
| No, but I was a smoker | 126 (20.3%) | |
| Yes, I smoke under 1 pack/week | 85 (13.7%) | |
| Yes, I smoke at most 1 pack/day | 119 (19.2%) | |
| Yes, I smoke more than 1 pack/day | 13 (2.1%) | |
| Alcohol consumption | No alcohol consumption | 196 (31.6%) |
| Occasional consumption (less than 6 units/week) | 381 (61.5%) | |
| 1–2 units/day | 30 (4.8%) | |
| 2–5 units/day | 11 (1.8%) | |
| 6–10 units/day | 1 (0.2%) | |
| Over 10 units/day | 1 (0.2%) |
Values are depicted as percentages and numerical data.

Table A5.
Descriptive data regarding level of COVID-19 contact (infection and/or consequences of the infection in the close social circle).
Table A5.
Descriptive data regarding level of COVID-19 contact (infection and/or consequences of the infection in the close social circle).
| Lot Characteristics | Answers | n (%) |
|---|---|---|
| SARS-CoV-2 infection | Yes, I am positive now | 28 (4.5%) |
| Yes, I was infected last month | 39 (6.3%) | |
| Yes, I was infected in the last 6 months | 27 (4.4%) | |
| Yes, I was infected more than 6 months ago | 5 (0.8%) | |
| No | 520 (84%) | |
| Severity of symptoms (n = 100) | Asymptomatic | 10 (10%) |
| Few symptoms | 65 (65%) | |
| Moderate symptoms | 25 (25%) | |
| Severe symptoms | 0 (0%) | |
| Someone close been infected with SARS-CoV-2 | Yes | 439 (70.8%) |
| No | 181 (29.2%) | |
| Someone close died of COVID-19 infection | Yes | 44 (7.1%) |
| No | 576 (92.9%) |
Values are depicted as percentages and numerical data.
References
- Eurosurveillance Editorial Team. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Eurosurveillance 2020, 25, 200131e. [Google Scholar] [CrossRef]
- Zanke, A.A.; Thenge, R.R.; Adhao, V.S. A Pandemic Declare by World Health Organization: COVID-19. IP Int. J. Compr. Adv. Pharmacol. 2021, 5, 449–457. [Google Scholar] [CrossRef]
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Owens, H.; Christian, B.; Polivka, B. Sleep behaviors in traditional-age college students: A state of the science review with implications for practice. J. Am. Assoc. Nurse Pract. 2017, 29, 695–703. [Google Scholar] [CrossRef]
- Petrovič, F.; Murgaš, F.; Králik, R. Happiness in Czechia during the COVID-19 Pandemic. Sustainability 2021, 13, 10826. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Dalamitros, A.; Beltran-Velasco, A.I.; Mielgo-Ayuso, J.; Tornero-Aguilera, J.F. Social and Psychophysiological Consequences of the COVID-19 Pandemic: An Extensive Literature Review. Front. Psychol. 2020, 11, 580225. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Martínez-González, M.B.; Benitez-Agudelo, J.C.; Navarro-Jiménez, E.; Beltran-Velasco, A.I.; Ruisoto, P.; Diaz-Arroyo, E.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. The Impact of the COVID-19 Pandemic on Mental Disorders. A Critical Review. Int. J. Environ. Res. Public Health 2021, 18, 10041. [Google Scholar] [CrossRef]
- Tkáčová, H.; Pavlíková, M.; Tvrdoň, M.; Jenisová, Z. The Use of Media in the Field of Individual Responsibility for Sustainable Development in Schools: A Proposal for an Approach to Learning about Sustainable Development. Sustainability 2021, 13, 4138. [Google Scholar] [CrossRef]
- Colten, H.R.; Altevogt, B.M. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; National Academies Press: Washington, DC, USA, 2006. [Google Scholar] [CrossRef]
- Seng, E.K.; Cervoni, C.; Lawson, J.L.; Oken, T.; Sheldon, S.; McKee, M.D.; Bonuck, K.A. The burden of sleep problems: A pilot observational study in an ethnically diverse urban primary care setting. J. Prim. Care Community Health 2016, 7, 276–280. [Google Scholar] [CrossRef]
- Chattu, V.; Manzar, M.; Kumary, S.; Burman, D.; Spence, D.; Pandi-Perumal, S. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare 2018, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Szczegielniak, A.; Palka, J.; Krysta, K. Problems associated with the use of social networks: A pilot study. Psychiatr. Danub. 2013, 25, 212–215. [Google Scholar]
- Grandner, M.A. Sleep, health, and society. Sleep Med. Clin. 2017, 12, 1–22. [Google Scholar] [CrossRef]
- Onyper, S.V.; Thacher, P.V.; Gilbert, J.W.; Gradess, S.G. Class start times, sleep, and academic performance in college: A path analysis. Chronobiol. Int. 2012, 29, 318–335. [Google Scholar] [CrossRef] [PubMed]
- Beşoluk, Ş.; Önder, İ.; Deveci, İ. Morningness-eveningness preferences and academic achievement of university students. Chronobiol. Int. 2011, 28, 118–125. [Google Scholar] [CrossRef]
- Pavlíková, M.; Sirotkin, A.; Králik, R.; Petrikovicová, L.; Martin, J.G. How to Keep University Active during COVID-19 Pandemic: Experience from Slovakia. Sustainability 2021, 13, 10350. [Google Scholar] [CrossRef]
- Lund, H.G.; Reider, B.D.; Whiting, A.B.; Prichard, J.R. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 2010, 46, 124–132. [Google Scholar] [CrossRef]
- DePierro, J.; Lowe, S.; Katz, C. Lessons learned from 9/11: Mental health perspectives on the COVID-19 pandemic. Psychiatry Res. 2020, 288, 113024. [Google Scholar] [CrossRef]
- Ghebreyesus, T.A. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129. [Google Scholar] [CrossRef]
- Gorgoni, M.; Scarpelli, S.; Mangiaruga, A.; Alfonsi, V.; Bonsignore, M.R.; Fanfulla, F.; Ferini-Strambi, L.; Nobili, L.; Plazzi, G.; De Gennaro, L.; et al. Persistence of the Effects of the COVID-19 Lockdown on Sleep: A Longitudinal Study. Brain Sci. 2021, 11, 1520. [Google Scholar] [CrossRef]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef] [PubMed]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef] [PubMed]
- Sade, R.M. Ethical Guidelines and Psychological Distress in a Pandemic. Ann. Thorac. Surg. 2020, 112, 342–343. [Google Scholar] [CrossRef] [PubMed]
- Smolarczyk-Kosowska, J.; Szczegielniak, A.; Legutko, M.; Zaczek, A.; Kunert, Ł.; Piegza, M.; Pudlo, R. Assessment of the impact of a daily rehabilitation program on anxiety and depression symptoms and the quality of life of people with mental disorders during the CoVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 1434. [Google Scholar] [CrossRef]
- Medic, G.; Wille, M.; Hemels, M.E. Short-and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151. [Google Scholar] [CrossRef]
- Paveliu, S.; Radu, C.-P.; Tudose, F.; Tudose, C.; Arsene, A. Cost-effectiveness analysis and the concept of quality adjusted life year (QALY) in Romania. Farmacia 2011, 59, 304–320. [Google Scholar]
- Dionisie, V.; Ciobanu, A.M.; Moisa, E.; Manea, M.C.; Puiu, M.G. The Impact of the COVID-19 Pandemic on Inpatient Admissions for Psychotic and Affective Disorders: The Experience of a Large Psychiatric Teaching Hospital in Romania. Healthcare 2022, 10, 1570. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]
- Iorga, M.; Iurcov, R.; Pop, L.M. The Relationship between Fear of Infection and Insomnia among Dentists from Oradea Metropolitan Area during the Outbreak of Sars-CoV-2 Pandemic. J. Clin. Med. 2021, 10, 2494. [Google Scholar] [CrossRef]
- Okajima, I.; Miyamoto, T.; Ubara, A.; Omichi, C.; Matsuda, A.; Sumi, Y.; Matsuo, M.; Ito, K.; Kadotani, H. Evaluation of severity levels of the athens insomnia scale based on the criterion of insomnia severity index. Int. J. Environ. Res. Public Health 2020, 17, 8789. [Google Scholar] [CrossRef]
- Bartoszek, A.; Walkowiak, D.; Bartoszek, A.; Kardas, G. Mental Well-Being (Depression, Loneliness, Insomnia, Daily Life Fatigue) during COVID-19 Related Home-Confinement—A Study from Poland. Int. J. Environ. Res. Public Health 2020, 17, 7417. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Zhang, S.X.; Looi, K.H.; Su, R.; Li, J. Perception of Health Conditions and Test Availability as Predictors of Adults’ Mental Health during the COVID-19 Pandemic: A Survey Study of Adults in Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 5498. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Qin, Q.; Sun, Q.; Sanford, L.D.; Vgontzas, A.N.; Tang, X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J. Clin. Sleep Med. 2020, 16, 1417–1418. [Google Scholar] [CrossRef]
- Burkova, V.N.; Butovskaya, M.L.; Randall, A.K.; Fedenok, J.N.; Ahmadi, K.; Alghraibeh, A.M.; Allami, F.B.M.; Alpaslan, F.S.; Al-Zu’bi, M.A.A.; Biçer, D.F.; et al. Predictors of Anxiety in the COVID-19 Pandemic from a Global Perspective: Data from 23 Countries. Sustainability 2021, 13, 4017. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Sekścińska, K.; Trzcińska, A.; Pankowski, D.; Pisula, E.; Wytrychiewicz-Pankowska, K. Financial Factors and Psychological Distress during the COVID-19 Pandemic in Poland. Int. J. Environ. Res. Public Health 2022, 19, 1798. [Google Scholar] [CrossRef]
- Kay-Stacey, M.; Attarian, H. Advances in the management of chronic insomnia. BMJ 2016, 354, i2123. [Google Scholar] [CrossRef]
- Jahrami, H.; BaHammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef]
- Voitsidis, P.; Gliatas, I.; Bairachtari, V.; Papadopoulou, K.; Papageorgiou, G.; Parlapani, E.; Syngelakis, M.; Holeva, V.; Diakogiannis, I. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020, 289, 113076. [Google Scholar] [CrossRef]
- Drews, H.J.; Wallot, S.; Brysch, P.; Berger-Johannsen, H.; Weinhold, S.L.; Mitkidis, P.; Baier, P.C.; Lechinger, J.; Roepstorff, A.; Göder, R. Bed-Sharing in Couples Is Associated with Increased and Stabilized REM Sleep and Sleep-Stage Synchronization. Front. Psychiatry 2020, 11, 583. [Google Scholar] [CrossRef] [PubMed]
- Rogojanski, J.; Carney, C.E.; Monson, C.M. Interpersonal factors in insomnia: A model for integrating bed partners into cognitive behavioral therapy for insomnia. Sleep Med. Rev. 2013, 17, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Yu, X.; Zhang, D.; Zheng, X.; Zhang, Z.; Lee, R.C.-M.; Cheung, P.M.-H.; Wong, S.Y.-S. Does It Matter Who You Live with during COVID-19 Lockdown? Association of Living Arrangements with Psychosocial Health, Life Satisfaction, and Quality of Life: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 1827. [Google Scholar] [CrossRef] [PubMed]
- Fitzek, S. The difficulties of Romanian families with elderly people in care (a diagnosis of the Romanian elderly who are at risk). J. Community Posit. Pract. 2019, 19, 11–27. [Google Scholar] [CrossRef]
- Bajenaru, L.; Marinescu, I.A.; Dobre, C.; Prada, G.I.; Constantinou, C.S. Towards the development of a personalized healthcare solution for elderly: From user needs to system specifications. In Proceedings of the 12th International Conference on Electronics, Computers and Artificial Intelligence, Bucharest, Romania, 25–27 June 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Castiglioni, M.; Hărăguş, M.; Faludi, C.; Hărăguş, P.T. Is the family system in Romania similar to those of southern European countries? Comp. Popul. Stud. 2016, 41, 57–86. [Google Scholar] [CrossRef]
- Schulz-Nieswandt, F.; Jochimsen, M.; Maier-Rigaud, R.; Kurscheid, C. Care Regimes for the Elderly in South Eastern Europe in a European Comparative Perspective. In Fianancing Health Care. A Dialogue between South Eastern Europe and Germany; Hans Jacobs Publishing Company: Lage, Germany, 2006; Volume 18, pp. 257–277. [Google Scholar]
- Etxeberria, I.; Zamora, G.; Bianchi, C.; Marchisio, C.; Rogozea, L.; Camci, Y. Psychological needs perception and stress, depression, insomnia and medical problems in caregivers. Transform. Care 2010, 1–29. Available online: https://hdl.handle.net/2318/87148 (accessed on 5 November 2022).
- Santini, S.; Socci, M.; Fabbietti, P.; Lamura, G.; Teti, A. Factors Worsening and Mitigating the Consequences of the COVID-19 Outbreak on the Overall Health of Informal Caregivers of Older People with Long-Term Care Needs Living in Germany and in Italy. Int. J. Environ. Res. Public Health 2022, 19, 1694. [Google Scholar] [CrossRef] [PubMed]
- Orr, K.; Ta, Z.; Shoaf, K.; Halliday, T.M.; Tobin, S.; Baron, K.G. Sleep, Diet, Physical Activity, and Stress during the COVID-19 Pandemic: A Qualitative Analysis. Behav. Sci. 2022, 12, 66. [Google Scholar] [CrossRef]
- Atkinson, G.; Davenne, D. Relationships between sleep, physical activity and human health. Physiol. Behav. 2007, 90, 229–235. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Beltrán-Velasco, A.I.; Ramos-Campo, D.J.; Mielgo-Ayuso, J.; Nikolaidis, P.A.; Belando, N.; Tornero-Aguilera, J.F. Physical activity and COVID-19. The basis for an efficient intervention in times of COVID-19 pandemic. Physiol. Behav. 2022, 244, 113667. [Google Scholar] [CrossRef]
- Brook, D.W.; Rubenstone, E.; Zhang, C.; Brook, J.S. Trajectories of cigarette smoking in adulthood predict insomnia among women in late mid-life. Sleep Med. 2012, 13, 1130–1137. [Google Scholar] [CrossRef]
- Wetter, D.W.; Young, T.B. The relation between cigarette smoking and sleep disturbance. Prev. Med. 1994, 23, 328–334. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Altena, E.; Ellis, J.G. How Sleep Affects Daytime Functioning: The Latest Insights from Different Patient and Age Groups. Brain Sci. 2021, 11, 1163. [Google Scholar] [CrossRef] [PubMed]
- Biggio, G.; Biggio, F.; Talani, G.; Mostallino, M.C.; Aguglia, A.; Aguglia, E.; Palagini, L. Melatonin: From Neurobiology to Treatment. Brain Sci. 2021, 11, 1121. [Google Scholar] [CrossRef]
- Scarpelli, S.; Alfonsi, V.; Gorgoni, M.; Camaioni, M.; Giannini, A.M.; De Gennaro, L. Age-Related Effect of Sleepiness on Driving Performance: A Systematic-Review. Brain Sci. 2021, 11, 1090. [Google Scholar] [CrossRef] [PubMed]
- Plotogea, O.-M.; Ilie, M.; Bungau, S.; Chiotoroiu, A.L.; Stanescu, A.M.A.; Diaconu, C.C. Comprehensive Overview of Sleep Disorders in Patients with Chronic Liver Disease. Brain Sci. 2021, 11, 142. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.-L.; Zheng, X.-Y.; Yang, J.; Ye, C.-P.; Chen, Y.-Y.; Zhang, Z.-G.; Xiao, Z.-J. A systematic review of studies on the prevalence of insomnia in university students. Public Health 2015, 129, 1579–1584. [Google Scholar] [CrossRef]
- Taylor, D.J.; Bramoweth, A.D.; Grieser, E.A.; Tatum, J.I.; Roane, B.M. Epidemiology of insomnia in college students: Relationship with mental health, quality of life, and substance use difficulties. Behav. Ther. 2013, 44, 339–348. [Google Scholar] [CrossRef]
- Taylor, D.J.; Gardner, C.E.; Bramoweth, A.D.; Williams, J.M.; Roane, B.M.; Grieser, E.A.; Tatum, J.I. Insomnia and mental health in college students. Behav. Sleep Med. 2011, 9, 107–116. [Google Scholar] [CrossRef]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef]
- Dąbrowska-Galas, M.; Ptaszkowski, K.; Dąbrowska, J. Physical Activity Level, Insomnia and Related Impact in Medical Students in Poland. Int. J. Environ. Res. Public Health 2021, 18, 3081. [Google Scholar] [CrossRef]
- Fila-Witecka, K.; Malecka, M.; Senczyszyn, A.; Wieczorek, T.; Wieckiewicz, M.; Szczesniak, D.; Piotrowski, P.; Rymaszewska, J. Sleepless in Solitude—Insomnia Symptoms Severity and Psychopathological Symptoms among University Students during the COVID-19 Pandemic in Poland. Int. J. Environ. Res. Public Health 2022, 19, 2551. [Google Scholar] [CrossRef] [PubMed]
- Carpi, M.; Cianfarani, C.; Vestri, A. Sleep Quality and Its Associations with Physical and Mental Health-Related Quality of Life among University Students: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2874. [Google Scholar] [CrossRef] [PubMed]
- Tkáčová, H.; Pavlíková, M.; Jenisová, Z.; Maturkanič, P.; Králik, R. Social Media and Students’ Wellbeing: An Empirical Analysis during the Covid-19 Pandemic. Sustainability 2021, 13, 10442. [Google Scholar] [CrossRef]
- Sellner, J.; Jenkins, T.; von Oertzen, T.; Bassetti, C.; Beghi, E.; Bereczki, D.; Bodini, B.; Cavallieri, F.; Di Liberto, G.; Helbok, R. Primary prevention of COVID-19: Advocacy for vaccination from a neurological perspective. J. Neurol. 2021, 28, 3226–3229. [Google Scholar] [CrossRef]
- Perez-Arce, F.; Angrisani, M.; Bennett, D.; Darling, J.; Kapteyn, A.; Thomas, K. COVID-19 vaccines and mental distress. PLoS ONE 2021, 16, e0256406. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).