Post-Traumatic Stress in Children and Adolescents during the COVID-19 Pandemic: A Meta-Analysis and Intervention Approaches to Ensure Mental Health and Well-Being
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.1.1. Selection Criteria
2.1.2. Data Extraction
3. Methodological Quality Assessment
Statistical Analysis
4. Results
4.1. Search and Selection
4.2. Characteristics and Methodological Quality of the Included Studies
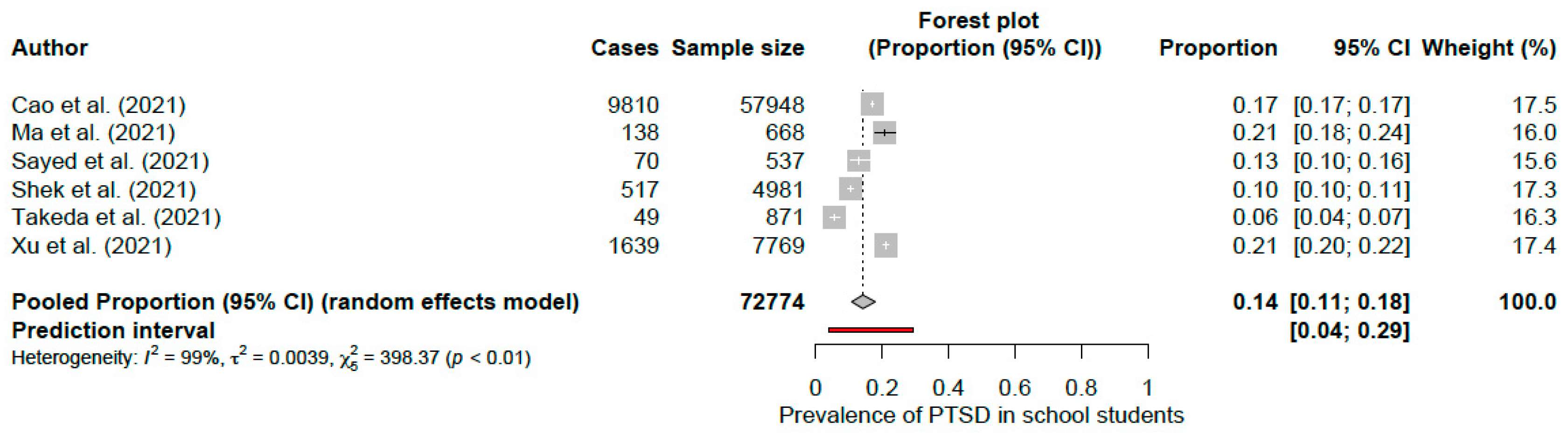
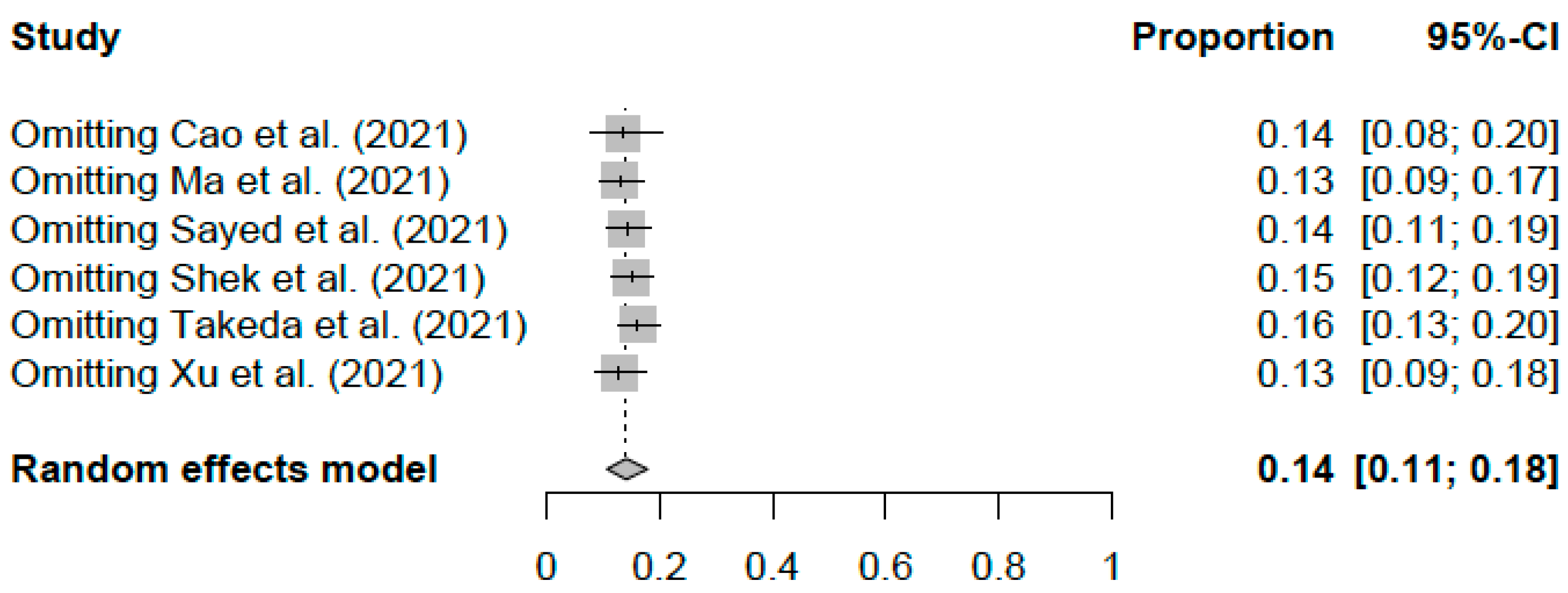
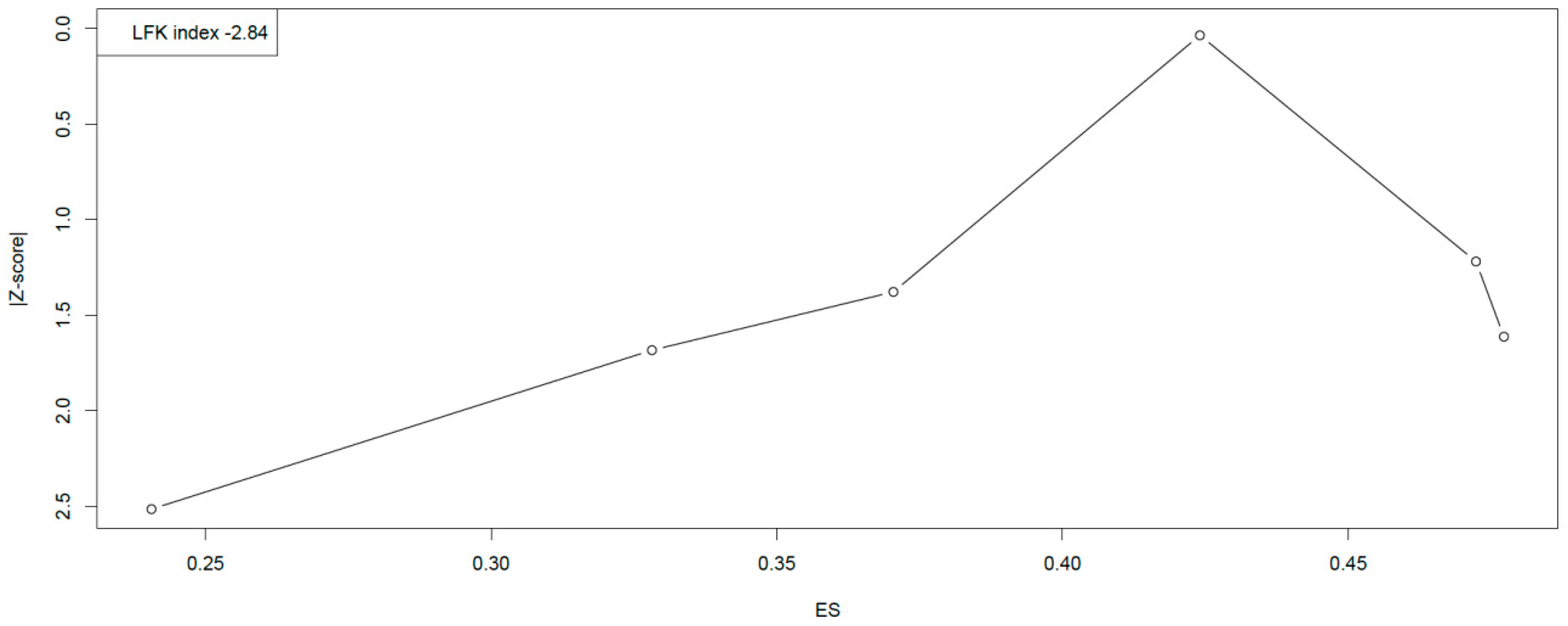
4.3. PTSD Prevalence
5. Recommendations for Intervention
6. Discussion
6.1. The Importance of Intervening in Order to Respond to the Impact of the Pandemic on Children’s Mental Health and Well-Being
- -
- Work on emotional self-knowledge. In this way, children would learn more about emotions and their causes.
- -
- Learn the difference between action and emotion.
- -
- Learn to manage the following emotions: frustration, anger management, stress management or feelings of inferiority.
- -
- Work empathy: to learn how to understand others, their feelings and how to listen. In this way, they would be more able to understand and analyze others, help deal with conflicts, improve communication and create more cooperation.
6.2. Strengths and Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reuge, N.; Jenkins, R.; Brossard, M.; Soobrayan, B.; Mizunoya, S.; Ackers, J.; Jones, L.; Taulo, W.G. Education response to COVID 19 pandemic, a special issue proposed by UNICEF: Editorial review. Int. J. Educ. Dev. 2021, 87, 102485. [Google Scholar] [CrossRef] [PubMed]
- Francis, N.N.; Pegg, S. Socially distanced school-based nutrition program under COVID-19 in the rural Niger Delta. Extr. Ind. Soc. 2020, 7, 576–579. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 and Children. 2022. Available online: https://www.euro.who.int/en/health-topics/Life-stages/child-and-adolescent-health/covid-19-and-children (accessed on 1 December 2022).
- Berasategi Sancho, N.; Idoiaga Mondragon, N.; Dosil Santamaria, M.; Eiguren Munitis, A. The Well-being of children in lock-down: Physical, emotional, social and academic impact. Child. Youth Serv. Rev. 2021, 127, 106085. [Google Scholar] [CrossRef]
- Grechyna, D. Health Threats Associated with Children Lockdown in Spain during COVID-19. 2020. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3567670 (accessed on 14 November 2021).
- Luijten, M.A.J.; van Muilekom, M.M.; Teela, L.; Polderman, T.J.C.; Terwee, C.B.; Zijlmans, J.; Klaufus, L.; Popma, A.; Oostrom, K.J.; van Oers, H.A.; et al. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. Qual. Life Res. 2021, 30, 2795–2804. [Google Scholar] [CrossRef]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef]
- Thakur, K.; Kumar, N.; Sharma, N. Effect of the Pandemic and Lockdown on Mental Health of Children. Indian J. Pediatr. 2020, 87, 552. [Google Scholar] [CrossRef]
- Transforming Our World: The 2030 Agenda for Sustainable Development. 2015. Available online: https://sdgs.un.org/2030agenda (accessed on 27 April 2022).
- ESCAP UN; World Health Organization. SDG 3 Goodhealth and Well-Being: Ensure Healthy Lives and Promote Well-Being for All at All Ages; ESCAP Publications: Bangkok, Thailand, 2021. [Google Scholar]
- Khetrapal, S.; Bhatia, R. Impact of COVID-19 pandemic on health system & Sustainable Development Goal 3. Indian J. Med. Res. 2020, 151, 395–399. [Google Scholar]
- Idoiaga, N.; Berasategi, N.; Eiguren, A.; Picaza, M. Exploring Children’s Social and Emotional Representations of the COVID-19 Pandemic. Front. Psychol. 2020, 11, 1952. [Google Scholar] [CrossRef]
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020, 221, 264–266.e1. [Google Scholar] [CrossRef] [PubMed]
- Okruszek, L.; Aniszewska-Stańczuk, A.; Piejka, A.; Wiśniewska, M.; Żurek, K. Safe but lonely? Loneliness, mental health symptoms and COVID-19. Front. Psychol. 2020, 11, 579181. [Google Scholar] [CrossRef]
- Singh, J.; Singh, J. COVID-19 and its impact on society. Electron. Res. J. Soc. Sci. Humanit. 2020, 2. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3567837 (accessed on 29 January 2023).
- Lippi, G.; Henry, B.M.; Bovo, C.; Sanchis-Gomar, F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis 2020, 7, 85–90. [Google Scholar] [CrossRef]
- Wang, G.; Zhang, Y.; Zhao, J.; Zhang, J.; Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 395, 945–947. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.V.; Chuang, R.; Rushing, M.; Naylor, B.; Ranjit, N.; Pomeroy, M.; Markham, C. Peer reviewed: Social determinants of health–related needs during COVID-19 among low-income households with children. Prev. Chronic Dis. 2020, 17, E119. [Google Scholar] [CrossRef]
- Ramkissoon, H. COVID-19 Place Confinement, Pro-Social, Pro-environmental Behaviors, and Residents’ Wellbeing: A New Conceptual Framework. Front. Psychol. 2020, 11, 2248. [Google Scholar] [CrossRef]
- Jiloha, R.C. COVID-19 and mental health. Epidemiol. Int. 2020, 5, 7–9. [Google Scholar] [CrossRef]
- de Figueiredo, C.S.; Sandre, P.C.; Portugal, L.C.L.; Mázala-de-Oliveira, T.; da Silva Chagas, L.; Raony, Í.; Ferreira, E.S.; Giestal-de-Araujo, E.; dos Santos, A.A.; Bomfim, P.O.-S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110171. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef]
- Kleinberg, B.; van der Vegt, I.; Mozes, M. Measuring emotions in the COVID-19 real world worry dataset. arXiv 2020, arXiv:2004.04225. [Google Scholar]
- Malboeuf-Hurtubise, C.; Léger-Goodes, T.; Mageau, G.A.; Joussemet, M.; Herba, C.; Chadi, N.; Lefrançois, D.; Camden, C.; Bussières, È.-L.; Taylor, G.; et al. Philosophy for children and mindfulness during COVID-19: Results from a randomized cluster trial and impact on mental health in elementary school students. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110260. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Idoiaga Mondragon, N.; Orcasitas-Vicandi, M.; Roman Etxebarrieta, G. Impact of emergency eLearning in a multilingual context with a minority language: How has the absence of school affected the use of Basque, English, and Spanish in the Basque context? Int. J. Biling. Educ. Biling. 2022, 25, 3533–3550. [Google Scholar] [CrossRef]
- UNESCO. Survey on National Education Responses to COVID-19 School Closures, Round 2; UNESCO: Paris, France, 2020. [Google Scholar]
- Berasategi Sancho, N.; Idoiaga Mondragon, N.; Dosil Santamaria, M.; Picaza Gorrotxategi, M. The well-being of children with special needs during the COVID-19 lockdown: Academic, emotional, social and physical aspects. Eur. J. Spec. Needs Educ. 2021, 37, 776–789. [Google Scholar] [CrossRef]
- Fomenko, L.; De Schrijver, L.; Vandeviver, C.; Keygnaert, I. Locked up at home: A cross-sectional study into the effects of COVID-19 lockdowns on domestic violence in households with children in Belgium. BMC Public Health 2022, 22, 1719. [Google Scholar] [CrossRef]
- Griffith, A.K. Parental Burnout and Child Maltreatment During the COVID-19 Pandemic. J. Fam. Violence 2020, 37, 725–731. [Google Scholar] [CrossRef]
- Pereda, N.; Díaz-Faes, D.A. Family violence against children in the wake of COVID-19 pandemic: A review of current perspectives and risk factors. Child Adolesc. Psychiatry Ment. Health. 2020, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Education in Emergencies in EU-Funded Humanitarian Aid Operations DG ECHO Thematic Policy Document No 10. 2019. Available online: https://ec.europa.eu/echo/files/news/eie_in_humanitarian_assistance.pdf (accessed on 29 January 2023).
- Idoiaga Mondragon, N.; Eiguren Munitis, A.; Berasategi Sancho, N.; Ozamiz Etxebarria, N. Drawing the COVID-19 pandemic: How do children incorporate the health crisis and its consequences into their everyday thinking? Psychol. Health 2022, 1–20. [Google Scholar] [CrossRef]
- Paterson, D.C.; Ramage, K.; Moore, S.A.; Riazi, N.; Tremblay, M.S.; Faulkner, G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: A scoping review of evidence after the first year. J. Sport Health Sci. 2021, 10, 675–689. [Google Scholar] [CrossRef]
- Rozhnova, G.; van Dorp, C.H.; Bruijning-Verhagen, P.; Bootsma, M.C.J.; van de Wijgert, J.H.H.M.; Bonten, M.J.M.; Kretzschmar, M.E. Model-based evaluation of school- and non-school-related measures to control the COVID-19 pandemic. Nat. Commun. 2021, 12, 1614–1616. [Google Scholar] [CrossRef] [PubMed]
- Willem, L.; Abrams, S.; Libin, P.J.K.; Coletti, P.; Kuylen, E.; Petrof, O.; Møgelmose, S.; Wambua, J.; Herzog, S.A.; Faes, C.; et al. The impact of contact tracing and household bubbles on deconfinement strategies for COVID-19. Nat. Commun. 2021, 12, 1524–1527. [Google Scholar] [CrossRef]
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental health impacts of the COVID-19 pandemic on children and youth—A systematic review. Child Adolesc. Ment. Health. 2022, 27, 173–189. [Google Scholar] [CrossRef]
- Bhushan, B.; Basu, S.; Ganai, U.J. Post-traumatic Stress and Growth Among the Children and Adolescents in the Aftermath of COVID-19. Front. Psychol. 2021, 12, 791263. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Powell, T.; Wegmann, K.M.; Backode, E. Coping and Post-Traumatic Stress in Children and Adolescents after an Acute Onset Disaster: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4865. [Google Scholar] [CrossRef]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef]
- Idoiaga Mondragon, N.; Fernandez, I.L.; Ozamiz-Etxebarria, N.; Villagrasa, B.; Santabarbara, J. PTSD (Posttraumatic Stress Disorder) in Teachers: A Mini Meta-Analysis during COVID-19. Int. J. Environ. Res. Public Health 2023, 20, 1802. [Google Scholar] [CrossRef] [PubMed]
- Lasheras, I.; Gracia-García, P.; Lipnicki, D.M.; Bueno-Notivol, J.; López-Antón, R.; De La Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of anxiety in medical students during the COVID-19 pandemic: A rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 6603. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Methods Group of the Campbell Collaboration. Methodological Expectations of Campbell Collaboration Intervention Reviews: Conduct Standards; Campbell Policies and Guidelines Series; Campbell Collaboration: Oslo, Norway, 2016; Volume 3. [Google Scholar]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis with R: A Hands-on Guide; Chapman and Hall/CRC: Boca Raton, FL, USA, 2021. [Google Scholar]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetc, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Systematic reviews of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual, 5th ed.; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Lin, L.; Xu, C. Arcsine-based transformations for meta-analysis of proportions: Pros, cons, and alternatives. Health Sci. Rep. 2020, 3, e178. [Google Scholar] [CrossRef] [PubMed]
- Knapp, G.; Hartung, J. Improved tests for a random effects meta-regression with a single covariate. Stat. Med. 2003, 22, 2693–2710. [Google Scholar] [CrossRef]
- Langan, D.; Higgins, J.P.; Jackson, D.; Bowden, J.; Veroniki, A.A.; Kontopantelis, E.; Viechtbauer, W.; Simmonds, M. A comparison of heterogeneity variance estimators in simulated random-effects meta-analyses. Res. Synth. Methods 2019, 10, 83–98. [Google Scholar] [CrossRef]
- von Hippel, P.T. The heterogeneity statistic I 2 can be biased in small meta-analyses. BMC Med. Res. Methodol. 2015, 15, 35. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Thompson, S.G.; Higgins, J.P. How should meta-regression analyses be undertaken and interpreted? Stat. Med. 2002, 21, 1559–1573. [Google Scholar] [CrossRef]
- Egger, M.; Schneider, M.; Davey Smith, G. Spurious precision? Meta-analysis of observational studies. BMJ 1998, 316, 140–144. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Hunter, J.P.; Saratzis, A.; Sutton, A.J.; Boucher, R.H.; Sayers, R.D.; Bown, M.J. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014, 67, 897–903. [Google Scholar] [CrossRef]
- Furuya-Kanamori, L.; Xu, C.; Lin, L.; Doan, T.; Chu, H.; Thalib, L.; Doi, S.A.R. P value-driven methods were underpowered to detect publication bias: Analysis of Cochrane review meta-analyses. J. Clin. Epidemiol. 2020, 118, 86–92. [Google Scholar] [CrossRef]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef]
- Rosenberg, M.S. The file-drawer problem revisited: A general weighted method for calculating fail-safe numbers in meta-analysis. Evolution 2005, 59, 464–468. [Google Scholar]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- R Core Team; R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Cao, C.; Wang, L.; Fang, R.; Liu, P.; Bi, Y.; Luo, S.; Grace, E.; Olff, M. Anxiety, depression, and PTSD symptoms among high school students in china in response to the COVID-19 pandemic and lockdown. J. Affect. Disord. 2022, 296, 126–129. [Google Scholar] [CrossRef]
- Ma, Z.; Idris, S.; Zhang, Y.; Zewen, L.; Wali, A.; Ji, Y.; Pan, Q.; Baloch, Z. The impact of COVID-19 pandemic outbreak on education and mental health of Chinese children aged 7–15 years: An online survey. BMC Pediatr. 2021, 21, 95. [Google Scholar] [CrossRef]
- Sayed, M.H.; Hegazi, M.A.; El-Baz, M.S.; Alahmadi, T.S.; Zubairi, N.A.; Altuwiriqi, M.A.; Saeedi, F.A.; Atwah, A.F.; Abdulhaq, N.M.; Almurashi, S.H. COVID-19 related posttraumatic stress disorder in children and adolescents in Saudi Arabia. PLoS ONE 2021, 16, e0255440. [Google Scholar] [CrossRef]
- Shek, D.T.L.; Zhao, L.; Dou, D.; Zhu, X.; Xiao, C. The Impact of Positive Youth Development Attributes on Posttraumatic Stress Disorder Symptoms Among Chinese Adolescents Under COVID-19. J. Adolesc. Health 2021, 68, 676–682. [Google Scholar] [CrossRef]
- Takeda, T.; Kai, S.; Yoshimi, K. Association between Premenstrual Symptoms and Posttraumatic Stress Symptoms by COVID-19: A Cross-Sectional Study with Japanese High School Students. Tohoku J. Exp. Med. 2021, 255, 71–77. [Google Scholar] [CrossRef]
- Xu, H.; Zhang, H.; Huang, L.; Wang, X.; Tang, X.; Wang, Y.; Xiao, Q.; Xiong, P.; Jiang, R.; Zhan, J.; et al. Increased symptoms of post-traumatic stress in school students soon after the start of the COVID-19 outbreak in China. BMC Psychiatry 2021, 21, 330–333. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental Health Status Among Children in Home Confinement During the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898–900. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.; Mukunzi, J.N.; McIntee, S.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef]
- Zhang, L.; Pan, R.; Cai, Y.; Pan, J. The prevalence of post-traumatic stress disorder in the general population during the COVID-19 pandemic: A systematic review and single-arm meta-analysis. Psychiatry Investig. 2021, 18, 426–433. [Google Scholar] [CrossRef]
- Salehi, M.; Amanat, M.; Mohammadi, M.; Salmanian, M.; Rezaei, N.; Saghazadeh, A.; Garakani, A. The prevalence of post-traumatic stress disorder related symptoms in Coronavirus outbreaks: A systematic-review and meta-analysis. J. Affect. Disord. 2021, 282, 527–538. [Google Scholar] [CrossRef]
- Qiu, D.; Li, Y.; Li, L.; He, J.; Ouyang, F.; Xiao, S. Prevalence of post-traumatic stress symptoms among people influenced by coronavirus disease 2019 outbreak: A meta-analysis. Eur. Psychiatry 2021, 64, e30. [Google Scholar] [CrossRef] [PubMed]
- Idoiaga, N.; Ozamiz-Etxebarria, N.; Villagrasa, B.; Santabárbara, J. Meta-analysis of the prevalence of PTSD (post-traumatic stress disorders) in teachers during COVID-19. Arch. Psychiatr. Nurs. 2022, in press.
- Trickey, D.; Siddaway, A.P.; Meiser-Stedman, R.; Serpell, L.; Field, A.P. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin. Psychol. Rev. 2012, 32, 122–138. [Google Scholar] [CrossRef] [PubMed]
- Salmon, K.; Bryant, R.A. Posttraumatic stress disorder in children. The influence of developmental factors. Clin. Psychol. Rev. 2002, 22, 163–188. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Fattah, H. Emotional intelligence and emotional stability in crises. J. Psychiatry Psychiatr. Disord. 2020, 4, 56–62. [Google Scholar]
- Chandra, Y. Online education during COVID-19: Perception of academic stress and emotional intelligence coping strategies among college students. Asian Educ. Dev. Stud. 2020, 10, 229–238. [Google Scholar] [CrossRef]
- Drigas, A.; Papoutsi, C. The Need for Emotional Intelligence Training Education in Critical and Stressful Situations: The Case of COVID-19. Int. J. Recent Contrib. Eng. Sci. IT 2020, 8, 20–36. [Google Scholar] [CrossRef]
- Martín-Requejo, K.; Santiago-Ramajo, S. Reduced Emotional Intelligence in Children Aged 9–10 caused by the COVID-19 Pandemic Lockdown. Mind Brain Educ. 2021, 15, 269–272. [Google Scholar] [CrossRef]
- Goleman, D. Emotional Intelligence; Bantam Books: New York, NY, USA, 1995. [Google Scholar]
- Fessell, D.; Cherniss, C. Coronavirus disease 2019 (COVID-19) and beyond: Micropractices for burnout prevention and emotional wellness. J. Am. Coll. Radiol. 2020, 17, 746–748. [Google Scholar] [CrossRef]
- Reivich, K.; Shatte, A. The Resilience Factor: 7 Essential Skills for Overcoming Life’s Inevitable Obstacles; Broadway Books: New York, NY, USA, 2002. [Google Scholar]
- Boix, C. Educar para ser feliz. In Una Propuesta de Educación Emocional; CEPE: Madrid, Spain, 2007. [Google Scholar]
- Salovey, P.; Mayer, J.D. Emotional intelligence. Imagin. Cogn. Personal. 1990, 9, 185–211. [Google Scholar] [CrossRef]
- Cummings, S.R.; Browner, W.S.; Hulley, S.B. Conceiving the research question and developing the study plan. Des. Clin. Res. 2013, 4, 14–22. [Google Scholar]
- Goh, J.X.; Hall, J.A.; Rosenthal, R. Mini meta-analysis of your own studies: Some arguments on why and a primer on how. Soc. Personal. Psychol. Compass 2016, 10, 535–549. [Google Scholar] [CrossRef]
- Valls-Llobet, C. La salud bio-psico-social re-generada. Quad. Psicol. 2010, 12, 175–181. [Google Scholar] [CrossRef]
- Rosa, E.M.; Tudge, J. Urie Bronfenbrenner’s theory of human development: Its evolution from ecology to bioecology. J. Fam. Theory Rev. 2013, 5, 243–258. [Google Scholar] [CrossRef]
- Cavaleri, M.A.; Olin, S.S.; Kim, A.; Hoagwood, K.E.; Burns, B.J. Family support in prevention programs for children at risk for emotional/behavioral problems. Clin. Child Fam. Psychol. Rev. 2011, 14, 399–412. [Google Scholar] [CrossRef]
- Roa García, A. La educación emocional, el autoconcepto, la autoestima y su importancia en la infancia. Edetania 2013, 44, 241–257. [Google Scholar]
- Romagnoli, C.; Gallargo, G. Alianza Efectiva Familia Escuela: Para Promover el Desarrollo Intelectual, Emocional, Social y Ético de los Estudiantes; Valoras UC: Santiago de Chile, Chile, 2018. [Google Scholar]
- Ramírez, F.B.; Misol, R.C.; Alonso, M.d.C.F.; Tizón, J.L. Pandemia de la COVID-19 y salud mental: Reflexiones iniciales desde la atención primaria de salud española. Atención Primaria 2021, 53, 89–101. [Google Scholar] [CrossRef]

| Study | Country | Sample Size | Age Mean (SD) | Proportion Females | Response Rate | Sampling Method (Sampling Technique Category) | JBI Critical Appraisal |
|---|---|---|---|---|---|---|---|
| Cao et al. (2021) [63] | China | 57,948 | 14.8 (1.6) | 51.6% | NR | NR | 4 |
| Ma et al. (2021) [64] | China | 668 | NR | 49.7% | 98.2% | Purposive (Non-probability sampling) | 5 |
| Sayed et al. (2021) [65] | Kingdom of Saudi Arabia | 537 | 12.2 (3.7) | 51.2% | NR | Convenience (Non-probability sampling) | 4 |
| Shek et al. (2021) [66] | China | 4981 | 13.1 (1.3) | 51.5% | NR | Cluster (Probability sampling) | 5 |
| Takeda et al. (2021) [67] | Japan | 871 | 16.7 (0.9) | 100% | 76.3% | Stratified (Probability sampling) | 6 |
| Xu et al. (2021) [68] | China | 7769 | 15 (NR) | 52.5% | NR | Convenience (Non-probability sampling) | 5 |
| Study | PTSD Assessment | ||
|---|---|---|---|
| Scale | Criteria | No. Cases (Prevalence) | |
| Cao et al. (2021) [63] | GPS-T | ≥3 | 9810 (16.9%) |
| Ma et al. (2021) [64] | IES-R | >20 | 138 (20.7%) |
| Sayed et al. (2021) [65] | UCLA-BCSCA | ≥21 | 70 (13%) |
| Shek et al. (2021) [66] | CRIES-13 | >30 | 517 (10.4%) |
| Takeda et al. (2021) [67] | IES-R | ≥24 | 49 (5.6%) |
| Xu et al. (2021) [68] | CRIES-13 | >30 | 1639 (21.1%) |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Cao et al. (2021) [63] | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 4 |
| Ma et al. (2021) [64] | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 5 |
| Sayed et al. (2021) [65] | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 5 |
| Shek et al. (2021) [66] | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 4 |
| Takeda et al. (2021) [67] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 6 |
| Xu et al. (2021) [68] | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 5 |
| ID | Study | General Recommendations for Intervention |
|---|---|---|
| 1 | Cao et al., 2021 [63] | Improving the family context and increasing social support are strategies to improve long-term mental health in adolescence. |
| 2 | Ma et al., 2021 [64] | As the mental health of the population continues to be deteriorated by COVID-19, authorities must take action and implement online interventions to improve mental health. |
| 3 | Sayed et al., 2021 [65] | Parents and professionals should detect the following alarming symptoms in order to prevent PTSD: intrusion, avoidance, negative mood and arousal/reactivity. If parents and teachers are aware of the severity of the symptoms they can help children to cope with these situations. |
| 4 | Shek et al., 2021 [66] | Psycho-educational programmes, early intervention assessments by teachers and professionals and mental health training for teachers would be very useful to help children and adolescents. |
| 5 | Takeda et al., 2021 [67] | --- |
| 6 | Xu et al., 2021 [68] | --- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozamiz-Etxebarria, N.; Legorburu Fernandez, I.; Idoiaga-Mondragon, N.; Olaya, B.; Cornelius-White, J.H.D.; Santabárbara, J. Post-Traumatic Stress in Children and Adolescents during the COVID-19 Pandemic: A Meta-Analysis and Intervention Approaches to Ensure Mental Health and Well-Being. Sustainability 2023, 15, 5272. https://doi.org/10.3390/su15065272
Ozamiz-Etxebarria N, Legorburu Fernandez I, Idoiaga-Mondragon N, Olaya B, Cornelius-White JHD, Santabárbara J. Post-Traumatic Stress in Children and Adolescents during the COVID-19 Pandemic: A Meta-Analysis and Intervention Approaches to Ensure Mental Health and Well-Being. Sustainability. 2023; 15(6):5272. https://doi.org/10.3390/su15065272
Chicago/Turabian StyleOzamiz-Etxebarria, Naiara, Idoia Legorburu Fernandez, Nahia Idoiaga-Mondragon, Beatriz Olaya, Jeffrey H. D. Cornelius-White, and Javier Santabárbara. 2023. "Post-Traumatic Stress in Children and Adolescents during the COVID-19 Pandemic: A Meta-Analysis and Intervention Approaches to Ensure Mental Health and Well-Being" Sustainability 15, no. 6: 5272. https://doi.org/10.3390/su15065272
APA StyleOzamiz-Etxebarria, N., Legorburu Fernandez, I., Idoiaga-Mondragon, N., Olaya, B., Cornelius-White, J. H. D., & Santabárbara, J. (2023). Post-Traumatic Stress in Children and Adolescents during the COVID-19 Pandemic: A Meta-Analysis and Intervention Approaches to Ensure Mental Health and Well-Being. Sustainability, 15(6), 5272. https://doi.org/10.3390/su15065272










