Towards Sustainable Healthcare: Exploring Factors Influencing Use of Mobile Applications for Medical Escort Services
Abstract
:1. Introduction
2. Literature Review
2.1. Importance and Implementation of MA-MES
2.2. Application of UTAUT 2 in mHealth
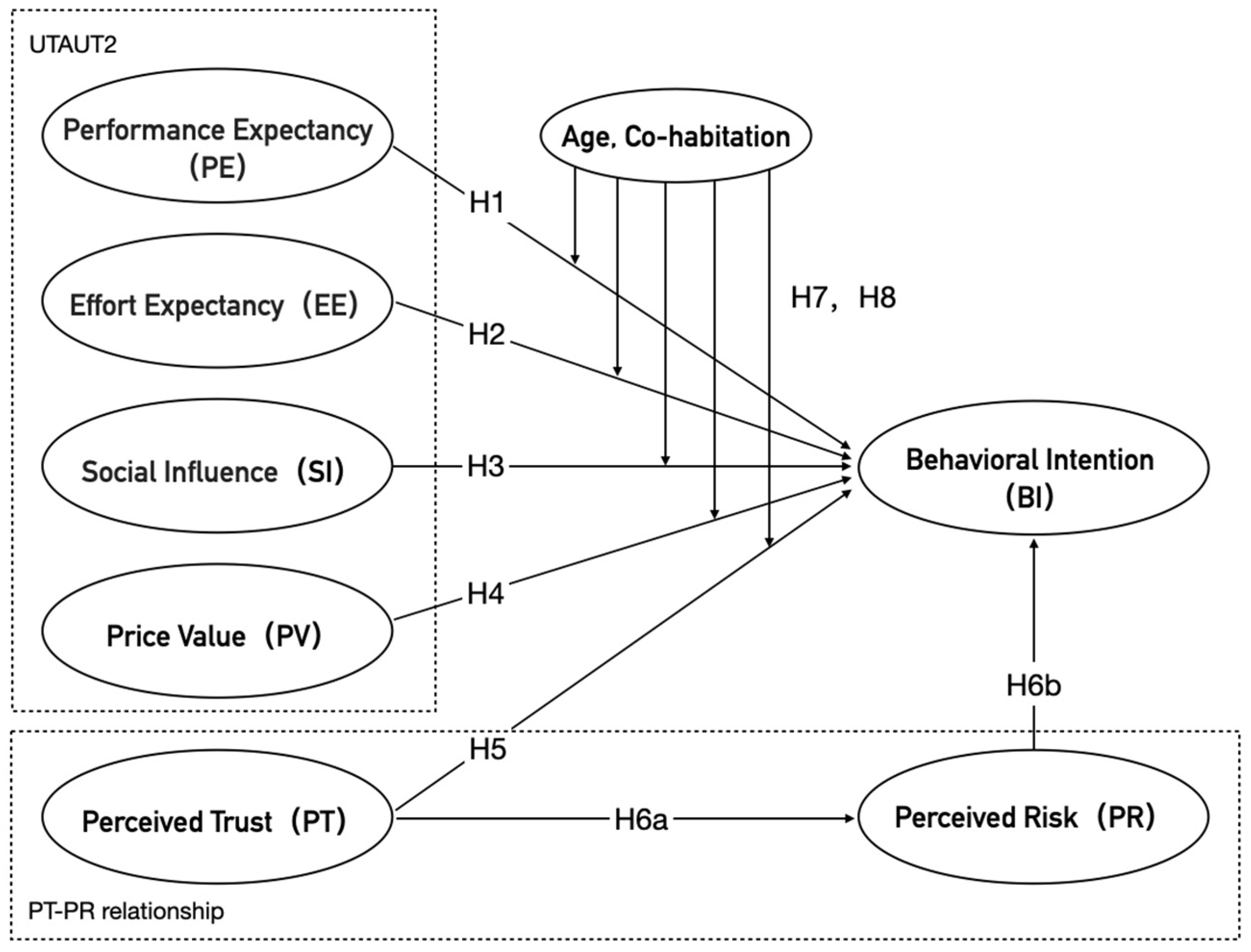
3. Theoretical Framework and Hypothesis Development
3.1. Behavioral Intention (BI)
3.2. Performance Expectancy (PE)
3.3. Effort Expectancy (EE)
3.4. Social Influence (SI)
3.5. Price Value (PV)
3.6. Perceived Trust–Perceived Risk Relationship (PT–PR Relationship)
3.7. Moderating Role of Age
3.8. Moderating Role of Cohabitating with Elderly Parents
3.9. Hypothetical Model
4. Methodologies
4.1. Measurement
4.2. Sample and Data Collection
4.3. Analysis Method
5. Date Analysis and Results
5.1. Descriptive Statistics
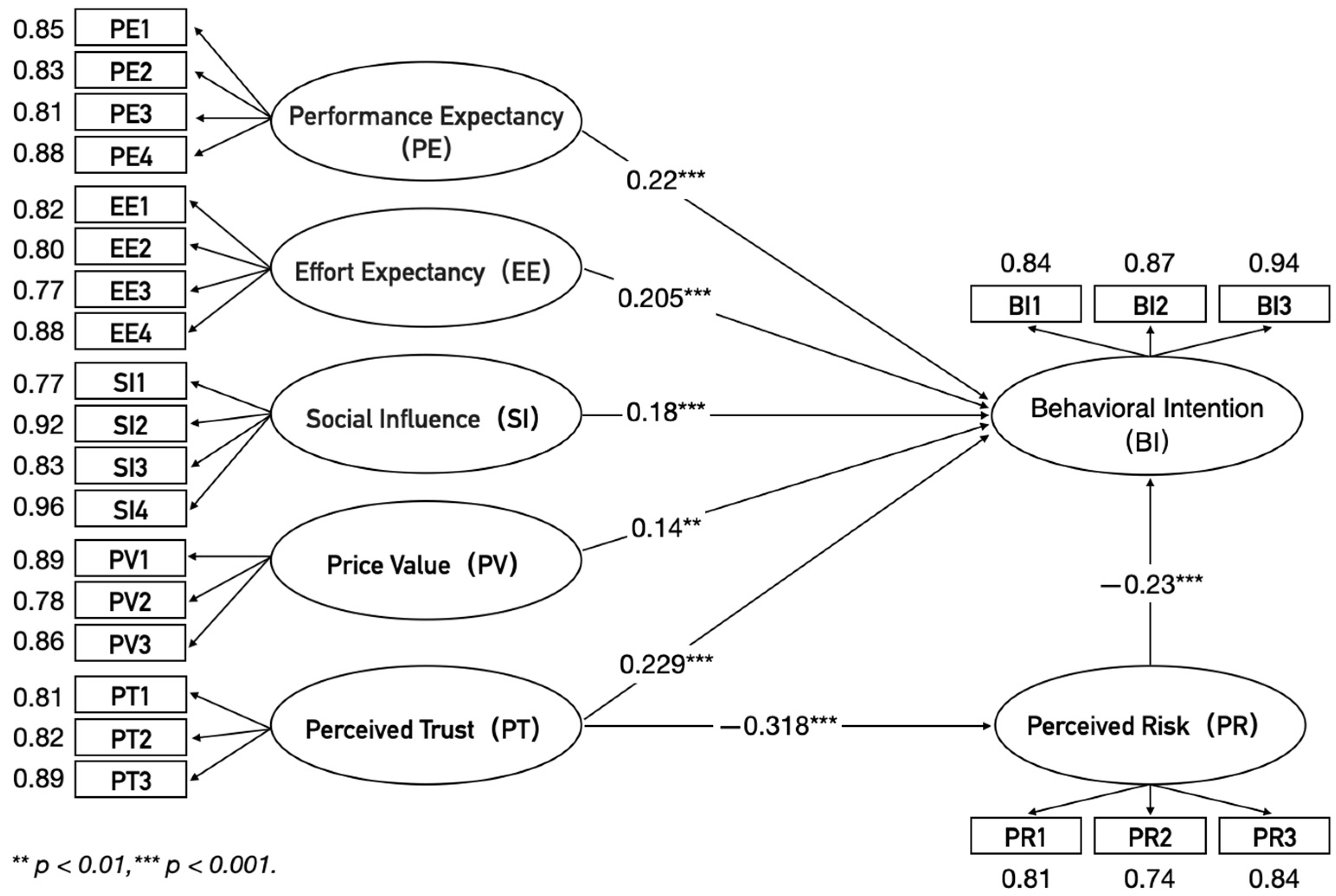
5.2. Reliability and Validity
5.3. Model Fit Adequacy
5.4. Testing Hypotheses
5.4.1. Testing the Impact of Core Factors on BI
5.4.2. Testing the Influence of PT on PR
5.4.3. Mediating Role of PR
5.4.4. Modulation Effect of Age
5.4.5. Modulation Effect of Cohabitation Status
6. Discussion
6.1. Main Findings
6.2. Theoretical Contributions
6.3. Practical Implications
6.4. Limitations and Future Research Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
References
- Fang, E.F.; Xie, C.L.; Schenkel, J.A.; Wu, C.; Long, Q.; Cui, H.; Aman, Y.; Frank, J.; Liao, J.; Zou, H.; et al. A research agenda for ageing in China in the 21st century: Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res. Rev. 2020, 64, 101174. [Google Scholar] [CrossRef]
- Kojima, G.; Liljas, A.E.M.; Iliffe, S. Frailty Syndrome: Implications and Challenges for Health Care Policy. Risk Manag. Healthc. Policy 2019, 12, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Peng, X. Coping with population ageing in mainland China. Asian Popul. Stud. 2021, 17, 1–6. [Google Scholar] [CrossRef]
- Zanobini, P.; Del Riccio, M.; Lorini, C.; Bonaccorsi, G. Empowering Sustainable Healthcare: The Role of Health Literacy. Sustainability 2024, 16, 3964. [Google Scholar] [CrossRef]
- Fineberg, H.V. A Successful and Sustainable Health System—How to Get There from Here. N. Engl. J. Med 2012, 366, 1020–1027. [Google Scholar] [CrossRef]
- Enjoy Accompany. Available online: http://www.huachengenjoy.com/home (accessed on 16 June 2024).
- Du, G.; Li, W. Multi-Objective Home Healthcare Routing and Scheduling Problem Based on Sustainability and “Physician-Patient” Satisfaction. Ann. Oper. Res. 2024, 1–43. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Wang, S.; Chen, S.; Nah, K. Exploring the Mechanisms Influencing Users’ Willingness to Pay for Green Real Estate Projects in Asia Based on Technology Acceptance Modeling Theory. Buildings 2024, 14, 349. [Google Scholar] [CrossRef]
- Gao, Y.; Li, H.; Luo, Y. An Empirical Study of Wearable Technology Acceptance in Healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar] [CrossRef]
- Ng, S.; David, M.E.; Dagger, T.S. Generating positive word-of-mouth in the service experience. Manag. Serv. Qual. Int. J. 2011, 21, 133–151. [Google Scholar] [CrossRef]
- Chen, L.N.; Ge, M.H.; Zheng, G.P. Operation Effect Analysis of District-Town Integrated Close Medical Consortium. China Mod. Dr. 2016, 54, 125–128. [Google Scholar]
- Li, T.; Fan, W.; Song, J. The household structure transition in China: 1982–2015. Demography 2020, 57, 1369–1391. [Google Scholar] [CrossRef] [PubMed]
- Qian, H.; Lu, W.; Zhang, D. Empirical Investigation on the Characteristics and Perceived Value of Patients in Medical Treatment Seeking: In-Depth Research in Zhejiang Province of China. Biomed Res. Int. 2021, 2021, 5245041. [Google Scholar] [CrossRef] [PubMed]
- Schwanen, T.; Dijst, M.; Dieleman, F.M. Leisure Trips of Senior Citizens: Determinants of Modal Choice. Tijdschr. Econ. Soc. Geogr. 2001, 92, 347–360. [Google Scholar] [CrossRef]
- Schilling, L.M.; Scatena, L.; Steiner, J.F.; Albertson, G.A.; Lin, C.T.; Cyran, L.; Ware, L.; Anderson, R.J. The Third Person in the Room: Frequency, Role, and Influence of Companions during Primary Care Medical Encounters. J. Fam. Pract. 2002, 51, 685–690. [Google Scholar]
- Clayman, M.L.; Roter, D.; Wissow, L.S.; Bandeen-Roche, K. Autonomy-Related Behaviors of Patient Companions and Their Effect on Decision-Making Activity in Geriatric Primary Care Visits. Soc. Sci. Med. 2005, 60, 1583–1591. [Google Scholar] [CrossRef]
- Wolff, J.L. Hidden in plain sight: Medical visit companions as a resource for vulnerable older adults. Arch. Intern. Med. 2008, 168, 1409–1415. [Google Scholar] [CrossRef]
- DiMatteo, M.R. Social Support and Patient Adherence to Medical Treatment: A Meta-Analysis. Health Psychol. 2004, 23, 207–218. [Google Scholar] [CrossRef]
- Seeman, T.E. Health Promoting Effects of Friends and Family on Health Outcomes in Older Adults. Am. J. Health Promot. 2000, 14, 362–370. [Google Scholar] [CrossRef]
- Christakis, N.A.; Allison, P.D. Mortality after the Hospitalization of a Spouse. N. Engl. J. Med. 2006, 354, 719–730. [Google Scholar] [CrossRef]
- Briefing on Key Data from the China Urban and Rural Elderly Population Tracking Survey. 2010. Available online: http://www.crca.cn/index.php/19-life/26-2010.html (accessed on 1 November 2023).
- Martin, L.A. Program Evaluation of a Community-Based Door-Through-Door Medical Escort Service; Gerontology Institute Publications: Atlanta, GA, USA, 2010. [Google Scholar]
- Sheehan, O.C.; Blinka, M.D.; Roth, D.L. Can Volunteer Medical Visit Companions Support Older Adults in the United States? BMC Geriatr. 2021, 21, 253. [Google Scholar] [CrossRef]
- Tu, J.-C.; Luo, S.C.; Lee, Y.-L.; Shih, M.-F.; Chiu, S.-P. Exploring Usability and Patient Attitude towards a Smart Hospital Service with the Technology Acceptance Model. Int. J. Environ. Res. Public Health 2022, 19, 6059. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Ma, G.X.; Wang, Y.F.; Shi, J.; Ran, D.; Zhang, J.Y. Analysis of Children’s Willingness and Demand for Accompanying Medical Services for the Elderly in Changzhou. Chin. J. Prev. Med. 2022, 23, 286–292. [Google Scholar]
- Kay, M.; Santos, J.; Takane, M. mHealth: New Horizons for Health through Mobile Technologies; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Octavius, G.S.; Antonio, F. Antecedents of intention to adopt mobile health (mHealth) application and its impact on intention to recommend: An evidence from Indonesian customers. Int. J. Telemed. Appl. 2021, 9, 6698627. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Schwartzberg, S. The Theory of Reasoned Action: Its Application to AIDS-Preventive Behaviour. Soc. Sci. Med. 1995, 40, 1587–1588. [Google Scholar] [CrossRef]
- Wu, I.-L.; Li, J.-Y.; Fu, C.-Y. The Adoption of Mobile Healthcare by Hospital’s Professionals: An Integrative Perspective. Decis. Support Syst. 2011, 51, 587–596. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, J.; Luximon, Y.; Qin, M.; Geng, P.; Tao, D. The Determinants of User Acceptance of Mobile Medical Platforms: An Investigation Integrating the TPB, TAM, and Patient-Centered Factors. Int. J. Environ. Res. Public Health 2022, 19, 10758. [Google Scholar] [CrossRef]
- Samsuri, A.S.; Hussin, S.M.; Badaruddin, M.N.A.; Arifin, T.R.T.; Zainol, S.S.; Mohamad, Z.Z. Antecedents of User Satisfaction and Continuance Usage of Mobile Health Applications: A Study on MySejahtera Apps in Malaysia. Asian J. Behav. Sci. 2022, 4, 91–105. [Google Scholar]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.; Xu, X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Q. 2012, 36, 157. [Google Scholar] [CrossRef]
- Pan, S.; Jordan-Marsh, M. Internet Use Intention and Adoption among Chinese Older Adults: From the Expanded Technology Acceptance Model Perspective. Comput. Human Behav. 2010, 26, 1111–1119. [Google Scholar] [CrossRef]
- Verdegem, P.; De Marez, L. Rethinking Determinants of ICT Acceptance: Towards an Integrated and Comprehensive Overview. Technovation 2011, 31, 411–423. [Google Scholar] [CrossRef]
- Ravangard, R.; Kazemi, Z.; Abbasali, S.Z.; Sharifian, R.; Monem, H. Development of the UTAUT2 Model to Measure the Acceptance of Medical Laboratory Portals by Patients in Shiraz. Electron. Physician 2017, 9, 3862–3869. [Google Scholar] [CrossRef]
- Schomakers, E.-M.; Lidynia, C.; Vervier, L.S.; Calero Valdez, A.; Ziefle, M. Applying an Extended UTAUT2 Model to Explain User Acceptance of Lifestyle and Therapy Mobile Health Apps: Survey Study. JMIR mHealth uHealth 2022, 10, e27095. [Google Scholar] [CrossRef]
- Brenčič, M.; Trkman, M.M. Analyzing Older Users’ Home Telehealth Services Acceptance Behavior-Applying an Extended UTAUT Model. Int. J. Med. Inform. 2016, 90, 22–31. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, N.; Guo, X.; Peng, Z. Understanding the Acceptance of Mobile Health Services: A Comparison and Integration of Alternative Models. J. Electron. Commer. Res. 2013, 14, 183–200. [Google Scholar]
- Hoque, R.; Sorwar, G. Understanding Factors Influencing the Adoption of mHealth by the Elderly: An Extension of the UTAUT Model. Int. J. Med. Inform. 2017, 101, 75–84. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Shareef, M.A.; Simintiras, A.C.; Lal, B.; Weerakkody, V. A Generalised Adoption Model for Services: A Cross-Country Comparison of Mobile Health (m-Health). Gov. Inf. Q. 2016, 33, 174–187. [Google Scholar] [CrossRef]
- Jang, S.H.; Kim, R.H.; Lee, C.W. Effect of U-Healthcare Service Quality on Usage Intention in a Healthcare Service. Technol. Forecast. Soc. Change 2016, 113, 396–403. [Google Scholar] [CrossRef]
- Prabhakar, K.K. Initial Trust and the Adoption of B2C E-Commerce: The Case of Internet Banking. ACM Sigmis Database 2004, 35, 50–64. [Google Scholar]
- Guo, X.; Zhang, X.; Sun, Y. The Privacy–Personalization Paradox in mHealth Services Acceptance of Different Age Groups. Electron. Commer. Res. Appl. 2016, 16, 55–65. [Google Scholar] [CrossRef]
- AlHogail, A.; AlShahrani, M. Building Consumer Trust to Improve Internet of Things (IoT) Technology Adoption. In Advances in Neuroergonomics and Cognitive Engineering; Springer: Cham, Switzerland, 2019; pp. 325–334. [Google Scholar]
- Bugshan, H.; Attar, R.W. Social Commerce Information Sharing and Their Impact on Consumers. Technol. Forecast. Soc. Change 2020, 153, 119875. [Google Scholar] [CrossRef]
- Arfi, W.B.; Nasr, I.B.; Kondrateva, G.; Hikkerova, L. The Role of Trust in Intention to Use the IoT in eHealth: Application of the Modified UTAUT in a Consumer Context. Technol. Forecast. Soc. Change 2021, 167, 120688. [Google Scholar] [CrossRef]
- Morris, M.G.; Venkatesh, V. Age Differences in Technology Adoption Decisions: Implications for a Changing Work Force. Pers. Psychol. 2000, 53, 375–403. [Google Scholar] [CrossRef]
- Taylor, S.; Todd, P. Decomposition and Crossover Effects in the Theory of Planned Behavior: A Study of Consumer Adoption Intentions. Int. J. Res. Mark. 1995, 12, 137–155. [Google Scholar] [CrossRef]
- Thompson, R.L.; Higgins, C.A.; Howell, J.M. Personal Computing: Toward a Conceptual Model of Utilization. MIS Q. 1991, 15, 125. [Google Scholar] [CrossRef]
- Chopdar, P.K.; Korfiatis, N.; Sivakumar, V.J.; Lytras, M.D. Mobile Shopping Apps Adoption and Perceived Risks: A Cross-Country Perspective Utilizing the Unified Theory of Acceptance and Use of Technology. Comput. Human Behav. 2018, 86, 109–128. [Google Scholar] [CrossRef]
- Venkatesh, V.; Davis, F.D. A Theoretical Extension of the Technology Acceptance Model: Four Longitudinal Field Studies. Manag. Sci. 2000, 46, 186–204. [Google Scholar] [CrossRef]
- Chin, W.W.; Newsted, P.R. Structural Equation Modeling Analysis with Small Samples Using Partial Least Squares. In Statistical Strategies for Small Sample Research; Hoyle, R.H., Ed.; Sage Publications: Thousand Oaks, CA, USA, 1999; pp. 307–341. [Google Scholar]
- Mandeville, G.K.; Roscoe, J.T. Fundamental Research Statistics for the Behavioral Sciences. J. Am. Stat. Assoc. 1971, 66, 224. [Google Scholar] [CrossRef]
- Anderson, J.C.; Gerbing, D.W. Structural Equation Modeling in Practice: A Review and Recommended Two-Step Approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Lee, C.W.; Kwon, I.W.; Severance, D. Relationship between Supply Chain Performance and Degree of Linkage among Supplier, Internal Integration, and Customer Supp. Chain. Manag. Inter. J 2007, 12, 444–452. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39. [Google Scholar] [CrossRef]
- Ren, Z.; Zhou, G. Analysis of Driving Factors in the Intention to Use the Virtual Nursing Home for the Elderly: A Modified UTAUT Model in the Chinese Context. Healthcare 2023, 11, 2329. [Google Scholar] [CrossRef]
- Chen, F.; Ngniatedema, T.; Li, S. A Cross-Country Comparison of Green Initiatives, Green Performance and Financial Performance. Manag. Decis. 2018, 56, 1008–1032. [Google Scholar] [CrossRef]
- Reyes-Mercado, P. Adoption of Fitness Wearables: Insights from Partial Least Squares and Qualitative Comparative Analysis. J. Syst. Inf. Technol. 2018, 20, 103–127. [Google Scholar] [CrossRef]
- Hsieh, P.-J. An Empirical Investigation of Patients’ Acceptance and Resistance toward the Health Cloud: The Dual Factor Perspective. Comput. Human Behav. 2016, 63, 959–969. [Google Scholar] [CrossRef]
- Moon, Y.J.; Hwang, Y.H. A Study of Effects of UTAUT-Based Factors on Acceptance of Smart Health Care Services. In Advanced Multimedia and Ubiquitous Engineering; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Koenig-Lewis, N.; Palmer, A.; Moll, A. Predicting Young Consumers’ Take up of Mobile Banking Services. Int. J. Bank Mark. 2010, 28, 410–432. [Google Scholar] [CrossRef]

| Construct | Item | Measurement | Source |
|---|---|---|---|
| Performance Expectancy (PE) | PE1 | I believe that using MA-MES can bring convenience to the medical visits of elderly parents. | [9] |
| PE2 | I believe that using MA-MES can enhance the efficiency of medical visits for elderly parents. | ||
| PE3 | I believe that using MA-MES can provide real-time services for the medical visits of elderly parents. | ||
| PE4 | I believe that by using MA-MES, I do not have to accompany elderly parents to medical visits personally; I can attend to my affairs. | ||
| Effort Expectancy (EE) | EE1 | It is easy to learn how to use MA-MES. | [9] |
| EE2 | The interaction of MA-MES is clear and easy to understand. | ||
| EE3 | I can use MA-MES smoothly. | ||
| EE4 | I can proficiently use MA-MES. | ||
| Social Influence (SI) | SI1 | I would use MA-MES influenced by family or friends. | [9] |
| SI2 | I would use MA-MES, influenced by colleagues or classmates. | ||
| SI3 | I would use MA-MES influenced by media or internet. | ||
| SI4 | I would use MA-MES influenced by authority or experts. | ||
| Price Value (PV) | PV1 | In terms of price, the service charges of MA-MES are reasonable. | [15] |
| PV2 | In terms of price, the service of MA-MES provides high cost-effectiveness. | ||
| PV3 | In terms of price, the service value of MA-MES exceeds the cost. | ||
| Perceived Risk (PR) | PR1 | I believe that using MA-MES would cause financial losses for elderly parents. | [26] |
| PR2 | I believe that using MA-MES would provide information about elderly parents to other companies. | ||
| PR3 | I believe that using MA-MES poses risks to the health of elderly parents. | ||
| Perceived Trust (PT) | PT1 | I believe that MA-MES is professional. | [25] |
| PT2 | I believe that MA-MES is trustworthy. | ||
| PT3 | I believe that MA-MES is reliable. | ||
| Behavioral Intention to Use (BI) | BI1 | I would try to use MA-MES for my elderly parents. | [27] |
| BI2 | I would learn to use MA-MES for my elderly parents. | ||
| BI3 | I would recommend using MA-MES for elderly parents to others. |
| Characteristics | n | Percentage | |
|---|---|---|---|
| Gender | Male | 209 | 59.7% |
| Female | 141 | 40.3% | |
| Age | 20–29 | 34 | 9.6% |
| 30–39 | 129 | 36.8% | |
| 40–49 | 166 | 47.4% | |
| 50–59 | 21 | 5.9% | |
| Education level | Junior high school or lower | 22 | 6.3% |
| High school | 77 | 22% | |
| College | 142 | 40.5% | |
| Bachelor’s degree | 75 | 21.4% | |
| Master’s degree or above | 34 | 9.7% | |
| Occupancy | Student | 180 | 51.4% |
| Employee | 80 | 22.8% | |
| Self-employed | 42 | 12% | |
| Unemployed | 19 | 5.4% | |
| Housewife/husband | 29 | 8.2% | |
| Cohabitation with elderly parents | yes | 151 | 43.1% |
| not | 199 | 56.8% | |
| Construct | Item | Mean (SD) | Standardized Factor Loading | Cronbach’ α | CR | AVE |
|---|---|---|---|---|---|---|
| PE | PE1 | 3.043 (1.008) | 0.852 | 0.908 | 0.909 | 0.714 |
| PE2 | 2.937 (0.967) | 0.823 | ||||
| PE3 | 2.891 (0.954) | 0.817 | ||||
| PE4 | 2.943 (0.968) | 0.883 | ||||
| EE | EE1 | 2.929 (1.003) | 0.823 | 0.889 | 0.89 | 0.668 |
| EE2 | 2.937 (1.028) | 0.797 | ||||
| EE3 | 2.857 (1.025) | 0.778 | ||||
| EE4 | 2.929 (0.974) | 0.874 | ||||
| SI | SI1 | 3.151 (0.91) | 0.768 | 0.923 | 0.931 | 0.779 |
| SI2 | 2.986 (0.922) | 0.916 | ||||
| SI3 | 2.914 (0.939) | 0.827 | ||||
| SI4 | 3.089 (1.188) | 0.955 | ||||
| PV | PV1 | 2.951 (0.867) | 0.866 | 0.874 | 0.876 | 0.702 |
| PV2 | 2.969 (0.894) | 0.782 | ||||
| PV3 | 3.026 (0.919) | 0.863 | ||||
| PR | PR1 | 2.997 (0.994) | 0.816 | 0.839 | 0.841 | 0.64 |
| PR2 | 2.846 (0.93) | 0.752 | ||||
| PR3 | 2.937 (0.958) | 0.825 | ||||
| PT | PT1 | 2.929 (1.012) | 0.81 | 0.876 | 0.878 | 0.706 |
| PT2 | 2.911 (1.068) | 0.812 | ||||
| PT3 | 2.929 (1.048) | 0.895 | ||||
| BI | BI1 | 2.991 (0.988) | 0.87 | 0.927 | 0.929 | 0.814 |
| BI2 | 3.057 (0.974) | 0.888 | ||||
| BI3 | 3.146 (0.957) | 0.949 |
| PE | EE | SI | PV | PR | PT | BI | |
|---|---|---|---|---|---|---|---|
| PE | 0.845 | ||||||
| EE | 0.458 | 0.817 | |||||
| SI | 0.11 | 0.228 | 0.883 | ||||
| PV | 0.405 | 0.393 | 0.077 | 0.838 | |||
| PR | −0.424 | −0.41 | −0.216 | −0.428 | 0.8 | ||
| PT | 0.227 | 0.198 | 0.134 | 0.167 | −0.282 | 0.84 | |
| BI | 0.455 | 0.456 | 0.279 | 0.402 | 0.47 | 0.362 | 0.902 |
| Index | Acceptance Level | Index Value | Comments |
|---|---|---|---|
| CMIN | - | 694.830 | Fulfilled |
| DF | - | 245 | Fulfilled |
| CMIN/DF | <3 | 2.2836 | Fulfilled |
| RMSEA | <0.08 | 0.073 | Fulfilled |
| IFI | >0.9 | 0.924 | Fulfilled |
| TLI | >0.9 | 0.914 | Fulfilled |
| CFI | >0.9 | 0.923 | Fulfilled |
| PGFI | >0.5 | 0.689 | Fulfilled |
| PNFI | >0.5 | 0.787 | Fulfilled |
| Hypothesis | Relationship | Estimate | S.E. | C.R. | p | Result |
|---|---|---|---|---|---|---|
| H1 | PE→BI | 0.22 | 0.046 | 4.239 | *** | Supported |
| H2 | EE→BI | 0.205 | 0.046 | 3.937 | *** | Supported |
| H3 | SI→BI | 0.18 | 0.034 | 3.586 | *** | Supported |
| H4 | PV→BI | 0.144 | 0.049 | 2.765 | 0.006 | Supported |
| H5 | PT→BI | 0.229 | 0.046 | 4.073 | *** | Supported |
| H6a | PT→PR | −0.318 | 0.053 | −5.199 | *** | Supported |
| H6b | PR→BI | −0.23 | 0.055 | −3.975 | *** | Supported |
| Hypothesis | Relationship | Estimate | Bias-Corrected 95%CI | Result | ||
|---|---|---|---|---|---|---|
| Lower | Upper | p | ||||
| H6 | PT→PR→BI | 0.059 | 0.024 | 0.113 | 0.001 | Supported |
| Hypothesis | Relationship | Youth (20–39) | Middle-Aged (40–59) | C.R. Difference | Result | ||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | C.R. | p | Estimate | C.R. | p | ||||
| H7a | PE→BI | 0.134 | 1.873 | 0.061 | 0.259 | 3.581 | *** | 1.708 | Not Supported |
| H7b | EE→BI | 0.224 | 3.029 | 0.002 | 0.23 | 3.203 | 0.001 | 0.174 | Not Supported |
| H7c | SI→BI | 0.158 | 2.27 | 0.023 | 0.279 | 3.945 | *** | 1.675 | Not Supported |
| H7d | PV→BI | 0.197 | 2.702 | 0.007 | 0.236 | 3.228 | 0.001 | 0.526 | Not Supported |
| H7e | PT→BI | 0.501 | 6.48 | *** | −0.014 | −0.193 | 0.847 | 6.494 | Supported |
| Hypothesis | Relationship | Cohabitation with Elderly Parents | No Cohabitation with Elderly Parents | C.R. Difference | Result | ||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | C.R. | p | Estimate | C.R. | p | ||||
| H8a | PE→BI | 0.14 | 1.843 | 0.065 | 0.252 | 3.585 | *** | 1.742 | Not Supported |
| H8b | EE→BI | 0.246 | 3.117 | 0.002 | 0.215 | 3.1 | 0.002 | 0.017 | Not Supported |
| H8c | SI→BI | 0.144 | 1.94 | 0.052 | 0.286 | 4.172 | *** | 2.232 | Supported |
| H8d | PV→BI | 0.195 | 2.502 | 0.012 | 0.253 | 3.553 | *** | 1.051 | Not Supported |
| H8e | PT→BI | 0.447 | 5.49 | *** | 0.074 | 1.061 | 0.289 | 4.429 | Supported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, F.; Hu, J.; Liu, D.; Zhou, C. Towards Sustainable Healthcare: Exploring Factors Influencing Use of Mobile Applications for Medical Escort Services. Sustainability 2024, 16, 6058. https://doi.org/10.3390/su16146058
Xu F, Hu J, Liu D, Zhou C. Towards Sustainable Healthcare: Exploring Factors Influencing Use of Mobile Applications for Medical Escort Services. Sustainability. 2024; 16(14):6058. https://doi.org/10.3390/su16146058
Chicago/Turabian StyleXu, Fan, Jing Hu, Duanduan Liu, and Chao Zhou. 2024. "Towards Sustainable Healthcare: Exploring Factors Influencing Use of Mobile Applications for Medical Escort Services" Sustainability 16, no. 14: 6058. https://doi.org/10.3390/su16146058
APA StyleXu, F., Hu, J., Liu, D., & Zhou, C. (2024). Towards Sustainable Healthcare: Exploring Factors Influencing Use of Mobile Applications for Medical Escort Services. Sustainability, 16(14), 6058. https://doi.org/10.3390/su16146058





