Abstract
As technology advances, virtual reality (VR) is increasingly being integrated into healthcare education to enhance learning outcomes. This systematic literature review and meta-analysis examined the effectiveness of virtual reality-based healthcare education. Randomized controlled trials (RCTs) published over the past 10 years were retrieved from 10 databases using VR, healthcare, and education as the primary keywords. Following the inclusion and exclusion criteria, 45 studies were included in the final analysis. A meta-analysis was performed to analyze the effects of VR in terms of knowledge, skill, and attitude. The results revealed that the use of VR significantly improved the knowledge (SMD: 0.28, 95% CI: 0.18–0.39, p < 0.001) and skill scores (SMD: 0.23, 95% CI: 0.11–0.34, p < 0.001), shortened the skill performance time (SMD: −0.59, 95% CI: −0.82 to −0.35, p < 0.001), and improved the satisfaction (SMD: 0.65, 95% CI: 0.48–0.81, p < 0.001) and confidence levels (SMD: 0.60, 95% CI: 0.41–0.80, p < 0.001). The in-depth analysis highlighted the significant potential of VR and provided practical implications in educational settings. In conclusion, effectively integrating VR with traditional educational methods is necessary to enhance both the quality of learning and the overall competence of healthcare professionals.
1. Introduction
The use of virtual reality (VR) in healthcare education and clinical practice has increased in recent years [1,2]. VR-based clinical practice education aims to improve the clinical skills of healthcare professionals [3] by providing them with opportunities to apply theoretical knowledge in real-world healthcare settings [4]. Consequently, it has emerged as an alternative to traditional clinical practice education. Traditional clinical practice education involves the use of hospital-based clinical practice or mannequin-based simulations. This system of education is limited by temporal and spatial constraints, as well as a limited variety of clinical cases [5]. Traditional methods are limited by the availability of time and space for practice. Furthermore, the diversity and comprehensiveness of clinical cases that learners can experience are also limited. Educational approaches using technologies such as VR, AR, and XR have been developed as alternatives and complements to address these limitations. Digital transformation (Hololens released in 2015, and Oculus (currently MetaQuest) released in 2016) and the coronavirus disease 2019 (COVID-19) pandemic have accelerated the growth of VR-based education [6,7,8]. VR-based clinical practice education provides healthcare professionals with access to repetitive practice anytime and anywhere, thereby enabling them to experience a wider range of real clinical scenarios [8,9,10].
VR-based education uses computer technology to create interactive 3D worlds that provide realistic experiences for learners [11]. VR can be categorized into VR, augmented reality (AR), and MR (mixed reality) in terms of technology [12]. VR immerses the user in a completely virtual environment; in contrast, AR overlays digital information onto the real environment. MR enables the user to perceive the real world and place virtual objects within it, thereby facilitating interaction between the two worlds. VR can be classified into non-immersive, immersive, and semi-immersive VR in terms of form [13,14,15]. VR-based education includes the provision of various clinical cases and opportunities for repetitive practice [16,17]. Furthermore, it provides opportunities for healthcare professionals to gain advanced skills and distance learning, thereby contributing to the improvement of clinical skills [18,19]. In detail, it can enhance a student’s cognitive ability and expertise [10,20,21,22,23], practical and social skills [10,24], and reduce errors [25]. Also, it can increase a student’s self-confidence [26,27,28,29], self-efficacy [28,30], and satisfaction [28,29,30] with clinical knowledge and skills. Furthermore, it has fewer financial, ethical, and supervisory constraints and poses no risk to patients [9]. VR technology is more economical than those using existing standardized patients or high-fidelity mannequins. It prevents the violation of patient rights, such as privacy violations, which is a concern associated with the use of actual patients as training participants [31,32,33]. However, VR-based education has some disadvantages, such as a high cost of development, the requirement for specialized equipment, and potential visual fatigue for users [34]. Furthermore, previous studies have reported conflicting results regarding the educational effectiveness of VR, with some studies reporting positive results, some reporting no statistically significant differences [35,36], and others reporting that VR is less effective than traditional methods in terms of knowledge and performance scores [10,37,38].
Recently, many studies have been conducted to evaluate the impact of VR-based medical education to clarify the educational and overall effectiveness of VR. However, these studies have several limitations. First, the majority of these studies focused on nursing education [4,14], indicating the requirement for studies on the effects of VR across a broader healthcare context, including medicine, dentistry, and complementary and alternative medicine. Second, although new technologies such as extended reality (XR) have emerged in recent years, research has predominantly focused on VR technology [10,14,39,40,41]. Thus, further studies must be conducted to evaluate AR, MR, and XR in addition to VR. Third, the majority of previous studies have focused on immersive [39] or non-immersive [40] forms of VR. Further studies must be conducted to comprehensively evaluate its effects from immersive to semi-immersive to non-immersive forms. Lastly, scoping reviews [11] and systematic reviews [9] made up the majority of studies. Therefore, additional meta-analyses must be conducted to evaluate the educational effectiveness of VR in an objective and reliable manner.
Based on the limitations of the prior studies and the need for further research, this systematic review and meta-analysis aimed to elucidate the overall educational effectiveness of VR in healthcare education. Studies conducted in the field of healthcare (such as medicine, dentistry, and nursing education) that incorporated technologies (such as VR, AR, MR, and XR) and its various forms (such as immersive, semi-immersive, and non-immersive) were included in the present study to verify the overall educational effectiveness of VR. Only randomized controlled trials (RCTs) were included in the present study to test the educational effectiveness of VR rigorously. The specific research questions of this study are as follows:
Q1. What are the study characteristics and study quality of the selected literature?
Q2. What are the effects of VR on learners’ knowledge in healthcare education?
Q3. What are the effects of VR on learners’ skills in healthcare education?
Q4. What are the effects of VR on learners’ attitudes in healthcare education?
2. Methods
This study was conducted according to the Cochrane Collaboration Handbook for Systematic Reviews [42] and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [43]. The study protocol was pre-registered with the PROSPERO International Prospective Register of Systematic Reviews (CRD42024576792) (https://www.crd.york.ac.uk/PROSPERO/#recordDetails, accessed on 21 September 2024).
2.1. Data Source and Search Strategy
The databases of MEDLINE (Ovid), Embase (Elsevier), Cochrane Library (Wiley), CINAHL (EBSCO), PsycINFO (EBSCO), ProQuest Central, Web of Science (Clarivate Analytics), Scopus (Elsevier), EBSCO (Academic Search Complete), and the Education Resources Information Centre (EBSCO) were searched to retrieve peer-reviewed articles from the field of medicine and education. Articles published between 1 January 2014 and 11 July 2024 were retrieved using the following terms and protocols: (“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”) AND (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”) AND (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”). Appendix A presents the details of the search strategy used for each database.
2.2. Inclusion Criteria and Exclusion Criteria
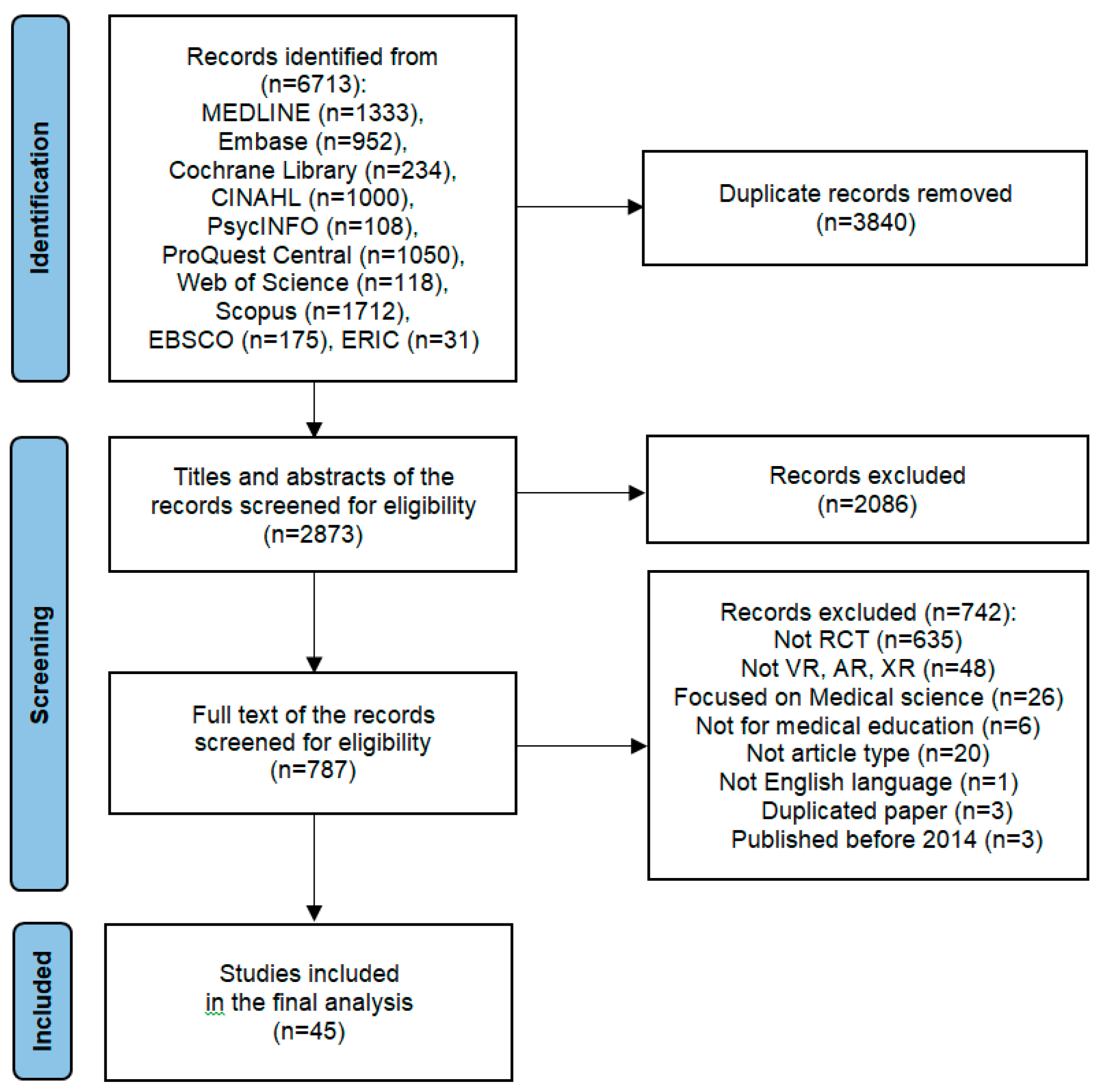
The population, intervention, comparison, outcome, and study design (PICO) framework was used [43,44]. The inclusion criteria were as follows: (a) the study population comprised healthcare personnel; (b) VR/AR/MR/XR teaching methods were implemented as the interventions in the experimental group; (c) traditional teaching methods or non-VR/AR/MR/XR teaching methods were implemented as the interventions in the comparison group; (d) the outcomes were focused on knowledge, skills, attitude (satisfaction and confidence), and behavior (performance time); and (e) the study type was an RCT. The exclusion criteria were as follows: (a) the study population comprised non-healthcare personnel; (b) non-VR/AR/MR/XR interventions were implemented as the interventions in the experimental group; (c) a study design other than an RCT; (d) studies that were published in languages other than English; (e) non-journal article types (conference papers, commentaries, editorials, book chapters, letters, and corrections). Figure 1 presents the PRISMA flowchart depicting the search and screening processes. The titles and abstracts of the articles were screened initially. The full text of the article was reviewed if the titles and abstracts lacked clarity or relevance. Any disagreements between the two authors who reviewed the studies were resolved by reaching a consensus through discussion.
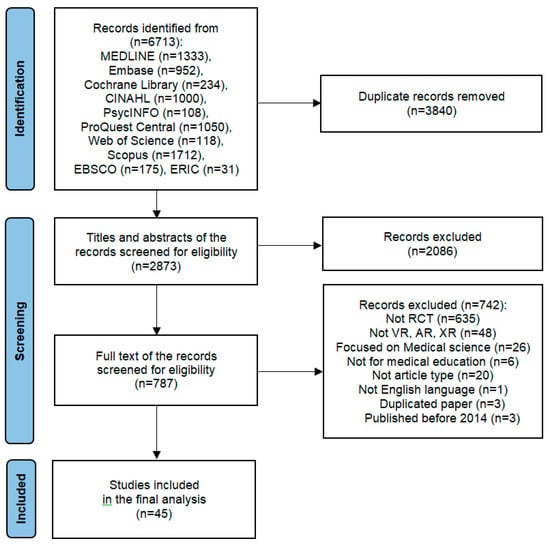
Figure 1.
The PRISMA flowchart.
2.3. Data Extraction and Study Quality Assessment
Four researchers each extracted data and assessed study quality. Data regarding the following elements were extracted from each study: first author, publication year, country, participants, study method, technology (with devices), teaching topics, interventions, assessments, and results. The potential risk of bias in the RCTs was appraised using the Cochrane Risk of Bias2 (ROB 2) tool (http://handbook.cochrane.org, accessed on 21 September 2024), which included five items, namely the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. The bias risk of each domain was categorized as “high”, “some concerns”, or “low” for all studies. The results of the five domains were combined to determine the overall bias in the study. In the process of data extraction and study quality assessment, discrepancies between the researchers (H.S., M.K., J.P., Y.H.) were resolved through discussion. If a consensus could be reached, another researcher (N.S.) was consulted to make the final decision.
2.4. Data Synthesis and Analysis
The meta-analysis was performed using Review Manager software version 5.4.1. Similar outcomes were compared using the standardized mean difference (SMD) with a 95% confidence interval (CI). The heterogeneity between the studies was analyzed using the Cochran Q test (p < 0.10 considered statistically significant) and the I2 value. Subgroup analyses were used to compare the differences between the fields of medical, nursing, and dental education. The meta-analysis results were conducted and described in terms of knowledge, skill (performance score and performance time), and attitude (satisfaction and confidence) based on Bloom’s taxonomy of educational objectives of knowledge [45]. Specifically, knowledge refers to participants’ cognitive understanding of learning content, skills denote the ability of participants to demonstrate a procedure or technique, performance time represents the time taken to complete the test task, satisfaction reflects participants’ perception of the VR intervention, and confidence pertains to their self-confidence in learning the content and process [10].
3. Results
Among the 6713 studies retrieved from 10 databases, 3840 duplicates and papers that did not meet the inclusion criteria were excluded. A review of the title and abstract of 2873 papers led to the exclusion of 2086 papers. A review of the full text of 787 papers led to the exclusion of 742 papers. Thus, 45 studies involving 3329 participants were included in the analysis. Figure 1 presents the flowchart of the study selection process.
3.1. Study Characteristics
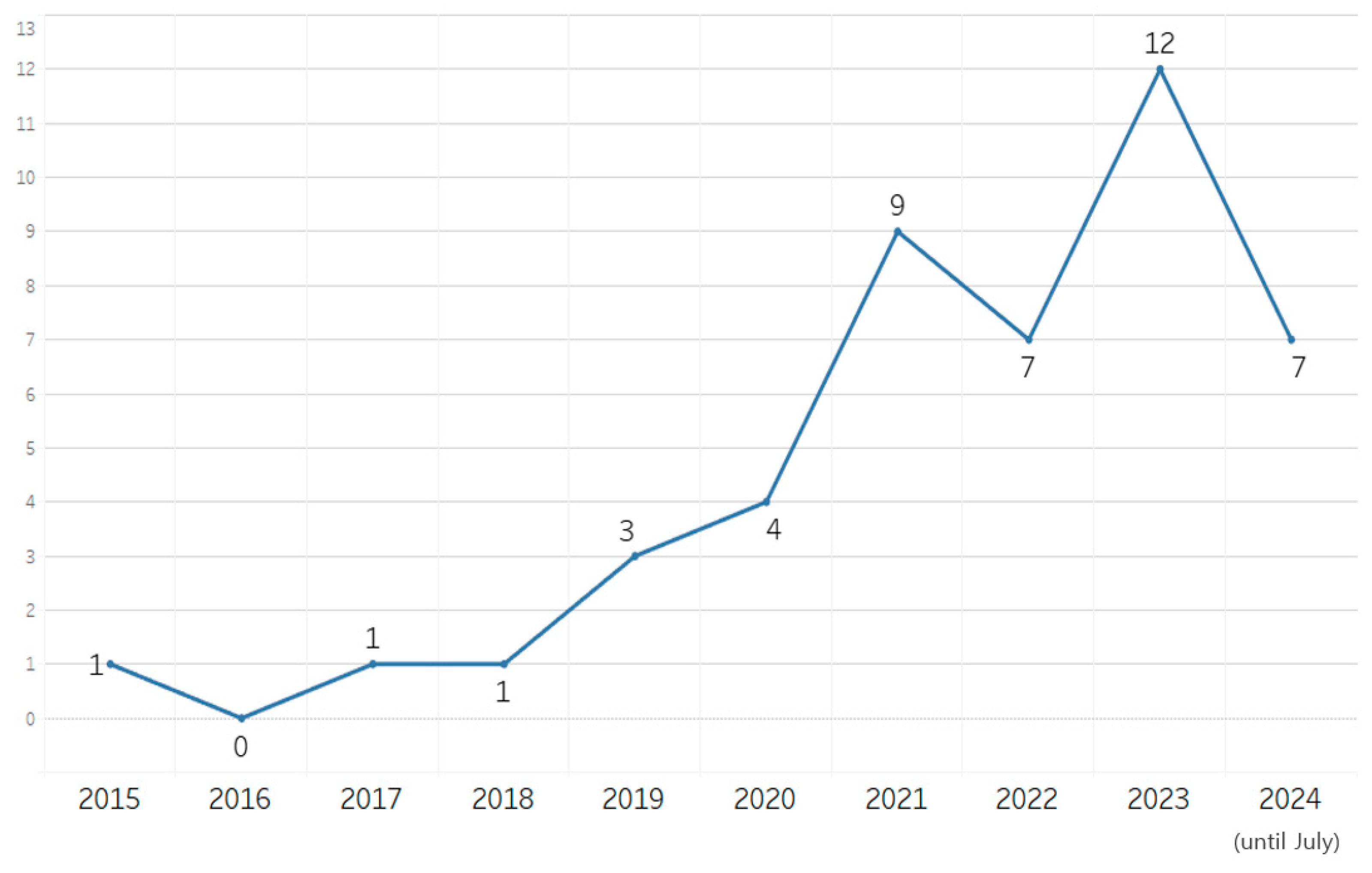
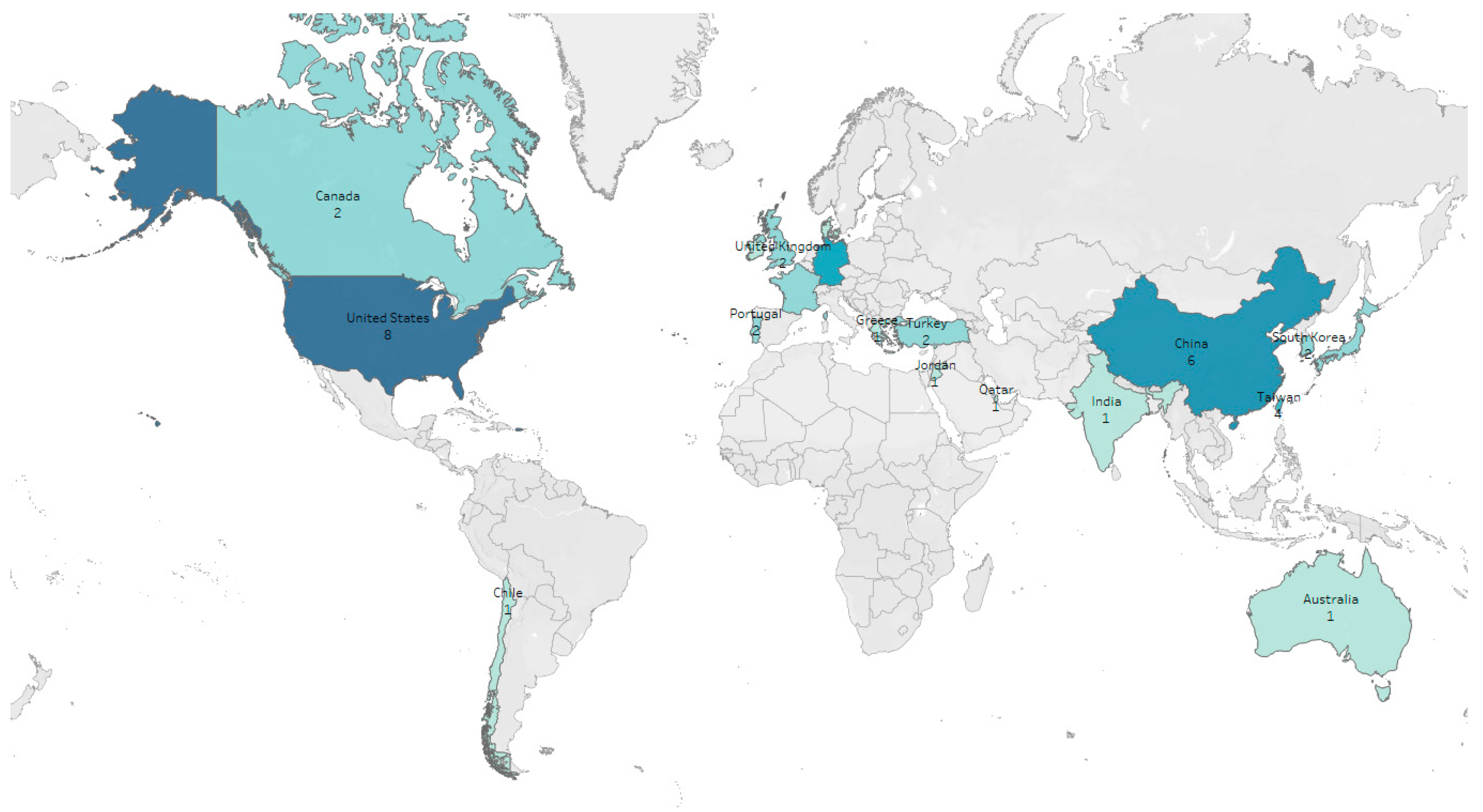
Table 1 presents the characteristics of the 45 studies included in this review. Several studies related to this field were published after 2019, with most studies being published in 2023 (Figure 2). The search was conducted until July 2024; thus, only seven studies published in the first half of 2024 were included in this review. This finding indicates that the number of studies related to this field has increased in recent years. The studies included in this review were conducted in various countries, with the largest number of studies being conducted in Asia (n = 17), followed by Europe (n = 14) and North America (n = 10). A notably higher concentration of studies was observed in Asia, Europe, and North America (Figure 3). A total of 3329 participants were included in the 45 studies, with the number of participants ranging from 13 to 164 in each study. Classifying the studies according to specialized education fields revealed that 26 [20,21,22,27,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67], 14 [26,28,29,68,69,70,71,72,73,74,75,76,77,78], and five [30,79,80,81,82] papers were published in the domain of medical, nursing, and dental education, respectively. Classifying the studies according to the usage of VR was overwhelmingly high, with VR being used in 38 (84.4%) of the 45 studies. AR, including AR and MR utilizing AR, was used in five (11.1%) studies.

Table 1.
Study characteristics.
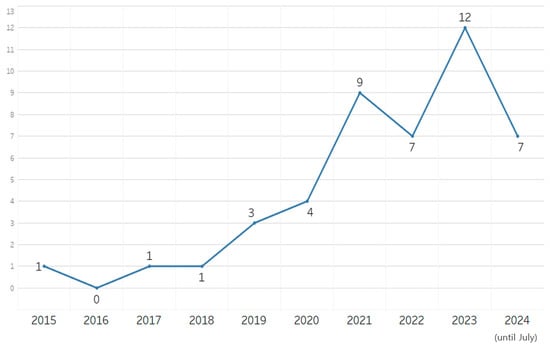
Figure 2.
Yearly publication trend in the included studies.
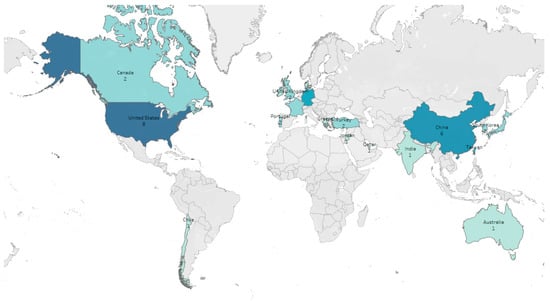
Figure 3.
Geographical distribution of the included studies.
The educational programs being evaluated varied across studies. The educational programs evaluated in the 45 studies included in this review were as follows: internal medicine in 10 studies [22,28,46,47,52,56,65,71,72,76], emergency medicine in seven studies [53,55,57,58,59,64,75], surgery in five studies [49,51,54,71,73], dentistry in five studies [30,79,80,81,82], simple surgical techniques in four studies [63,68,69,78], anatomy in four studies [48,51,60,66], otolaryngology in three studies [20,50,74], pediatrics in three studies [29,67,77], the nervous system in two studies [46,47], history taking and patient relationships in two studies [21,70], obstetrics and gynecology in two studies [26,27], dermatology in one study [62], and ultrasound practice in one study [61]. The evaluation criteria also varied across the studies; however, knowledge, skills, and techniques were assessed using multiple-choice tests, questionnaires, and expert evaluations. Twenty-five studies (55.6%) assessed knowledge [20,26,27,28,46,47,48,51,52,55,56,60,62,63,66,68,69,72,73,74,75,76,77,80,82], 26 studies (57.8%) assessed clinical skills [20,21,22,27,29,49,50,53,54,55,57,58,59,61,63,64,67,68,69,70,71,73,74,75,78,82], and 32 studies (71.1%) assessed learners’ attitudes [20,22,26,27,28,29,30,46,47,48,49,50,51,53,56,59,60,61,62,65,68,69,70,71,72,73,74,75,77,78,79,81]. Appendix B presents the detailed evaluation criteria and results for each study. Knowledge was assessed using multiple-choice tests or questionnaires in the majority of studies. Various scales were used to assess clinical ability; however, the OSCE scores, checklists, or expert evaluations were used most commonly. Other evaluation indices included skill performance time and penalty errors. Attitudes were assessed mostly through self-administered questionnaires that included items to assess satisfaction, self-confidence, self-efficacy, emotions, preferences, discomfort, stress, program acceptability, usability, and other evaluations of the program. Appendix B presents the study characteristics.
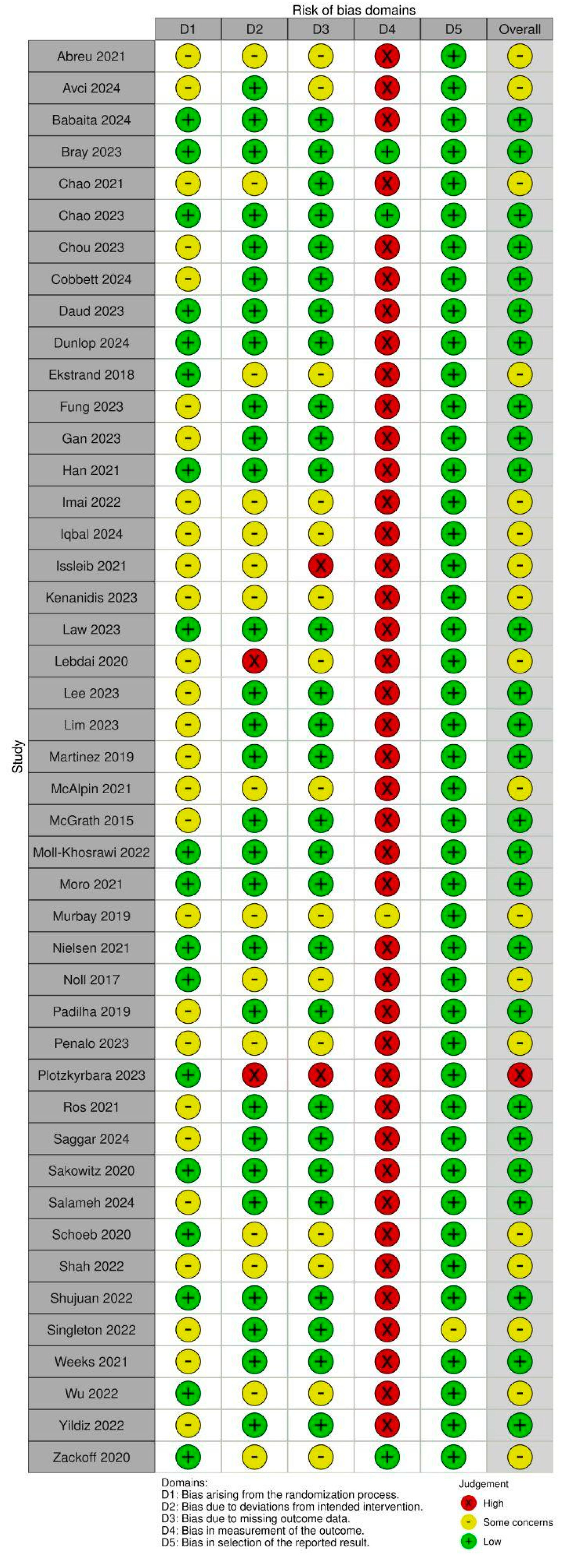
3.2. Study Quality
Figure 4 presents the results of the assessment according to the Cochrane risk-of-bias (ROB) 2.0 criteria. In terms of the domain of randomization (domain 1), ROB 2.0 criteria revealed allocation concealment in 17 studies [21,22,27,47,48,50,55,59,60,61,62,69,74,75,77,79,82]. Among these 17 studies, six [27,59,61,62,67,82] were double-blind. Eighteen studies, including one study that did not overlap with the allocation concealment group above [67], were categorized as “low-risk”. The remaining studies were all RCTs categorized as “some concerns”. In terms of the bias assessment of the interventions (domain 2), ROB 2.0 criteria revealed that two studies (4.4%) had a high risk of bias. One study involved participants who received duplicate interventions [74]. Another study [56], wherein the difference in the number of dropouts between the intervention and control groups was seven, was categorized as “high-risk”; however, no detailed explanation was provided for this. Fifteen studies (33.3%) [20,22,46,48,51,52,53,54,62,65,67,73,77,80,81] were categorized as “some concern”, as the exact number of participants excluded from receiving the intervention was unclear. Twenty-eight studies (62.2%) [21,26,27,28,29,30,47,49,50,55,57,58,59,60,61,63,64,66,68,69,70,71,72,75,76,78,79,82] were categorized as “low-risk”.

Figure 4.
Risk of bias analysis of the included study.
Regarding the bias assessment of the outcome data (domain 3), two studies (4.4%) [53,74] were categorized as “high-risk”, as some participants dropped out between the intervention and the time of outcome reporting; however, detailed descriptions were provided. Fifteen studies (33.3%) [22,46,48,51,52,54,56,62,65,67,68,73,77,80,81] were categorized as “some concerns”, as it was unclear whether the participants dropped out after the intervention. Twenty-eight studies (62.2%) [20,21,26,27,28,29,30,47,49,50,55,57,58,59,60,61,63,64,66,69,70,71,72,75,76,78,79,82] were categorized as “low-risk”. In terms of the assessment of bias in (domain 4), the assessors were blinded in four studies [21,47,67,81]. A satisfaction questionnaire was used as an indicator in one study [81], which may have affected the subjectivity of the assessors. This study was categorized as “some concern”. The other three studies were categorized as “low-risk”, as objective assessments were observed in these studies [21,47,67]. Forty-three studies were categorized as “high-risk”, as assessor blinding was not implemented in these studies and educational methods wherein the participants were likely to be aware of their interventions were used in these methods. The bias associated with the reported outcomes (domain 5) was low in all 45 studies, as data on all participants who completed the studies were included in these studies. This may be attributed to the training methods for VR being specific such that the participants could not be unaware of their interventions. Moreover, the risk of bias was very high, as the assessments were conducted using self-administered questionnaires rather than tests or blinded assessors. The overall risk of bias in the studies was low, with only one of the 45 studies being categorized as “high-risk”, 18 studies (40%) being categorized as “some concern”, and 26 studies (57.8%) being categorized as “low-risk”. An assessment performed using the criteria of ROB 2 revealed that the ROB of the studies as a whole was categorized as “slight concern”; however, the overall bias of the studies is thought to be lower, assuming that there was no dropout in most studies with unclear data reporting.
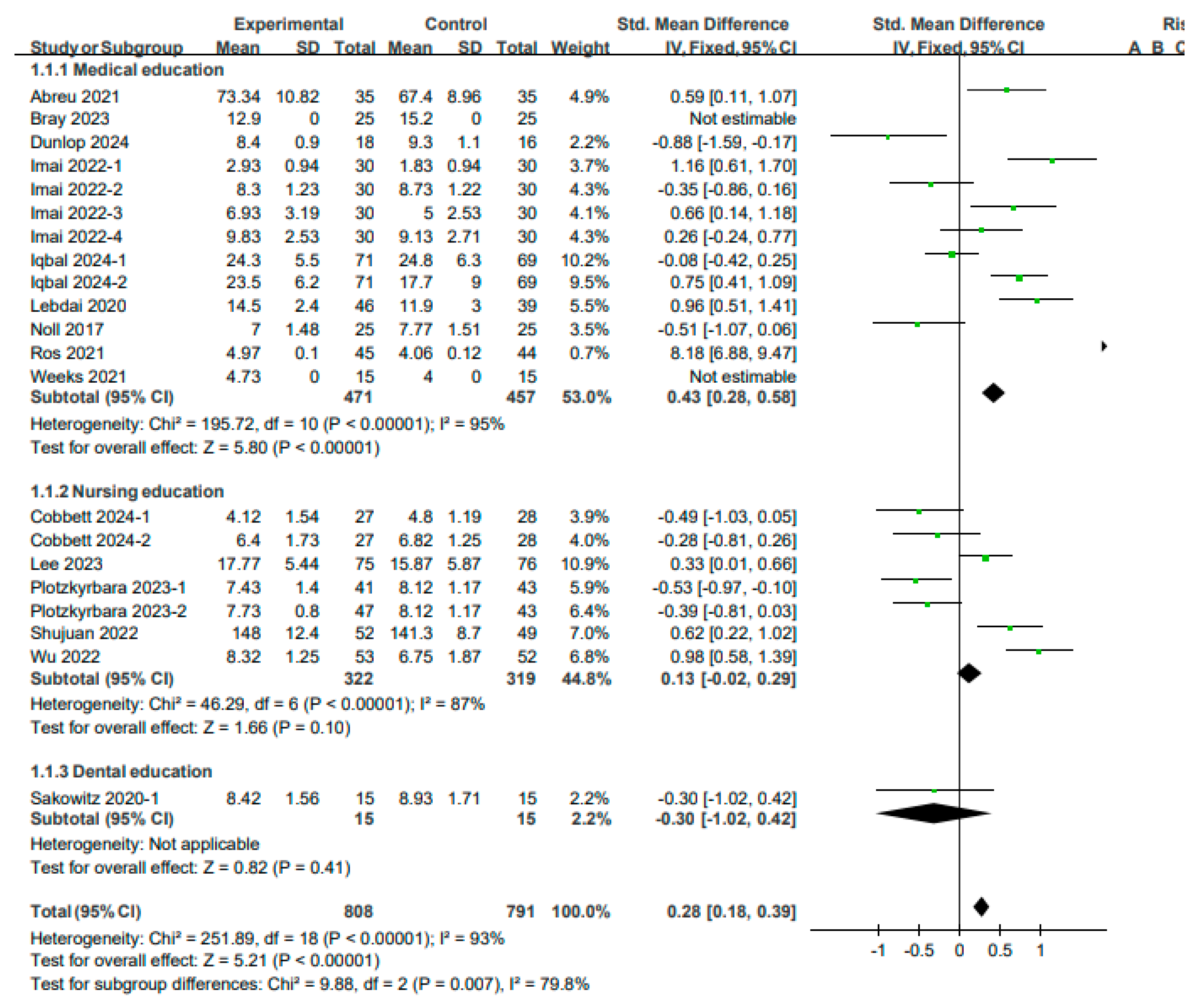
3.3. Effects of VR on Knowledge
A meta-analysis was performed using a fixed model, as the studies included in the analysis of the knowledge levels exhibited high heterogeneity (I2 = 93%, p < 0.0001). An analysis of nine studies (13 results) on medical education revealed that the improvement in knowledge was significantly higher in the experimental group than in the control group (SMD: 0.43, 95% CI: 0.28–0.58, p < 0.0001). An analysis of five studies (seven results) on nursing education revealed that the difference between the experimental and control groups was not significant (SMD: 0.13, 95% CI: −0.02–0.29, p < 0.00001). An analysis of one study on dental education revealed that the difference between the groups was not significant (SMD: −0.30, 95% CI: −1.02–0.42, p > 0.05). In summary, the results of the meta-analysis of 21 results from 15 studies involving 1599 participants indicated that VR education yielded a significant improvement in knowledge (SMD: 0.28, 95% CI: 0.18–0.39, p < 0.00001) (see Figure 5).
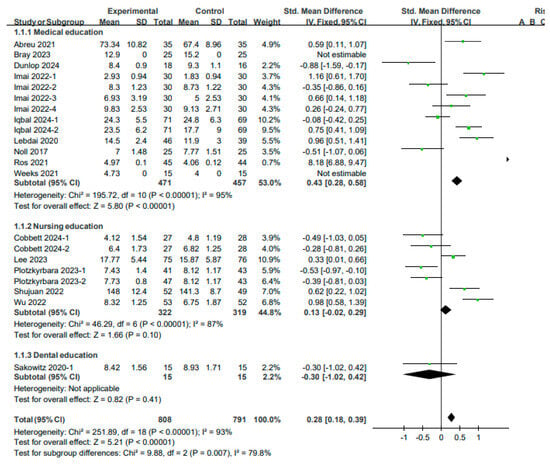
Figure 5.
Forest plot for the effects of VR on knowledge.
An analysis of the studies on medical education focusing on internal medicine diseases revealed that the score of the VR evaluation was significantly higher than that of the general evaluation (p < 0.01). This finding may be attributed to VR facilitating a simulation environment that improves the reasoning and clinical skills of the students, leading to an increase in scores [46]. An analysis of the studies on medical education focusing on urological diseases revealed that knowledge was significantly higher in the VR group when VR was compared with general practice (p < 0.001) [56]. An analysis of the studies on medical education focusing on head and neck anatomy revealed that the score for AR was significantly higher when 3D AR was compared with 2D AR (p < 0.05) [66]. A comparison between VR and 3D simulation using four knowledge scales in studies on medical education for anatomy and surgery of the esophagus and mediastinum revealed that the level of CT and surgical images were significantly higher in VR (p < 0.05); however, no significant differences were observed between the groups in terms of the level of mediastinal structure and general knowledge (p > 0.05) [51]. Comparison between VR and general lectures in studies on medical education for ECG interpretation revealed no significant differences between the two groups in terms of knowledge regarding a normal ECG (p > 0.05); however, knowledge regarding an abnormal ECG was significantly higher in the VR group (p < 0.001). Moreover, 8 weeks later, the knowledge survey score was significantly higher in the VR group (p < 0.001) [52]. An analysis of the studies on nursing education focusing on blood transfusion revealed that the test scores in the VR group were significantly higher than those in the group that received general lectures on VR (p < 0.01) [28]. In nursing education focusing on pediatric epilepsy, knowledge significantly increased in VR compared to general lectures (p < 0.01) [77]. An analysis of the studies on medical education focusing on internal and surgical diseases revealed no significant difference between 3D VR and 2D VR (p > 0.05); however, a significant increase in knowledge after education was observed in both groups (p < 0.05) [47]. This finding suggests that the two groups achieved similar levels of learning as the scenario formats were almost identical and the emotional engagement levels were similar. In addition, these results also suggest that higher immersion does not necessarily yield higher educational effects and that multiple cognitive processes may affect the educational effects. An analysis of the studies on medical education focusing on postpartum hemorrhage revealed that the difference between the VR and general lecture groups was not significant (p > 0.05); however, a significant increase in knowledge after education was observed in both groups (p < 0.001) [27]. An analysis of the studies on medical education focusing on skin diseases revealed that a comparison between AR and non-AR mobile education revealed no significant differences (p > 0.05); however, a significant increase in knowledge after education was observed in both groups (p > 0.05) [62]. The MCQ scores for dental diagnosis and treatment education did not differ significantly between the groups (p > 0.05) [82]. An analysis of the studies on nursing education focusing on perinatal diseases revealed that the difference between the groups was not significant for either scenario (p > 0.05) [26]. Thus, the abovementioned studies confirmed that although the difference between the experimental and control groups was not significant, VR can yield effects similar to those of conventional education methods. Moreover, both education methods exhibited a tendency toward an improvement in scores after the intervention; consequently, they can be considered effective education methods. A comparison between VR and general medical education focusing on lumbar puncture revealed that the oral examination scores were significantly lower in the VR group (p < 0.001) [63]. This finding may be attributed to the demonstration or model education exhibiting a better educational effect than VR on techniques such as LP. An analysis of the studies on nursing education focusing on tracheal suctioning revealed that the knowledge scores of the three groups (2D video, low-level VR, and high-level VR) were comparable, with no significant differences being observed among the three groups (p > 0.05); however, the scores increased significantly after the education. A comparison between 2D videos and VR-low revealed that the VR-low score was significantly lower (p < 0.05). A comparison between 2D videos and VR-high revealed no significant difference between the groups (p > 0.05) [74], indicating that VR and 2D education had similar effects or that 2D education may be more efficient.
3.4. Effects of VR on Skills
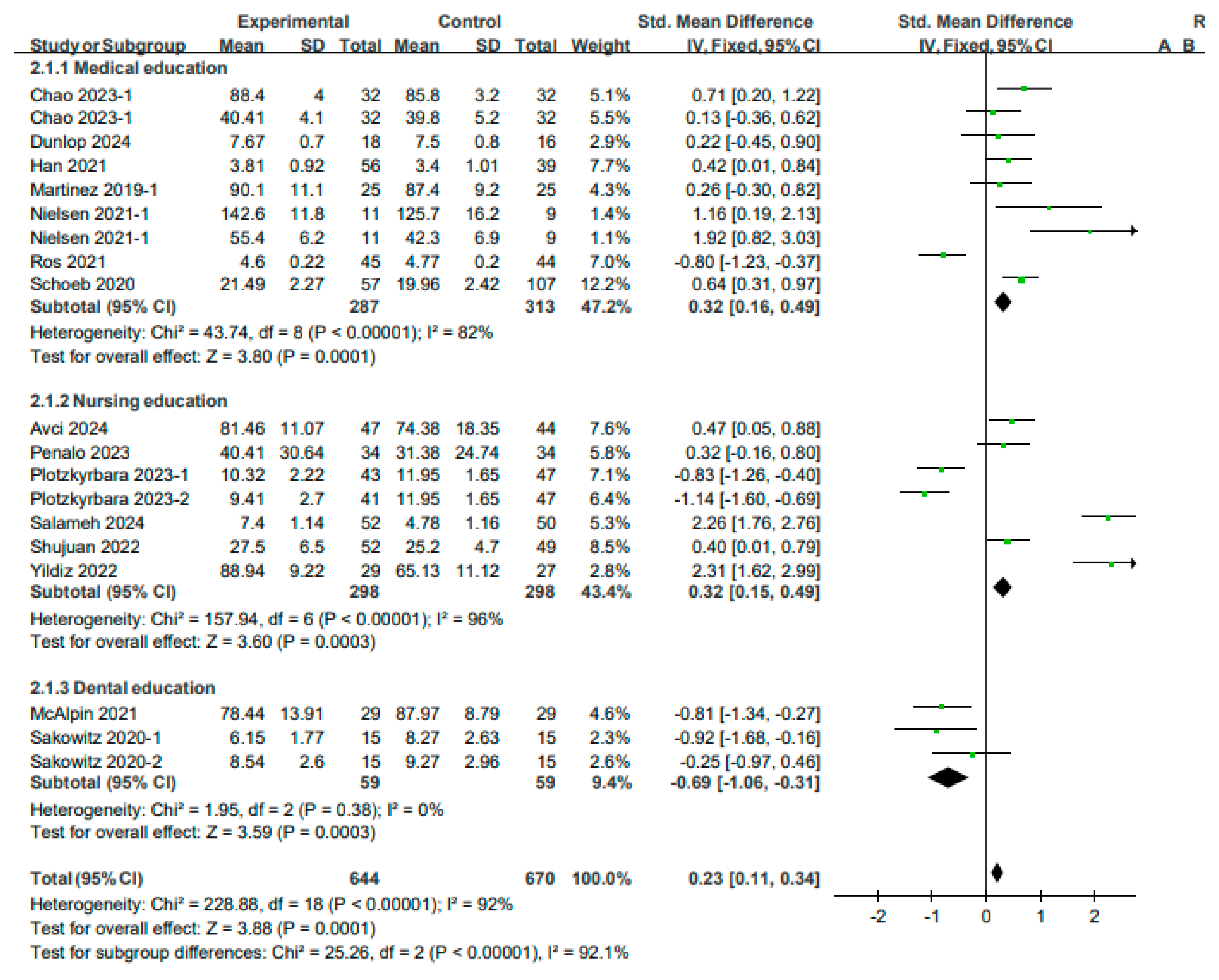
3.4.1. Performance Score
A fixed-effects model was used to perform the analysis, as the studies included in the score analysis for skills exhibited high heterogeneity (I2 = 92%, p < 0.00001). An analysis of seven studies (nine results) in the field of medical education revealed that the skill scores in the experimental group exhibited a more significant improvement than those in the control group (SMD: 0.32, 95% CI: 0.16–0.49, p < 0.00001). An analysis of six studies (seven results) in the field of nursing education revealed a more significant improvement in the skill scores in the experimental group than that in the control group (SMD: 0.32, 95% CI: 0.15–0.49, p < 0.0001). An analysis of two studies (three results) in the field of dental education revealed a more significant effect in the control group than in the experimental group (SMD: −0.69, 95% CI: −1.06 to −0.31, p < 0.001). In summary, the results of a meta-analysis of 19 results from 15 studies involving a total of 1314 participants revealed that VR education yielded a significant improvement in clinical skills (SMD: 0.23, 95% CI: 0.11–0.34, p < 0.00001) (see Figure 6).
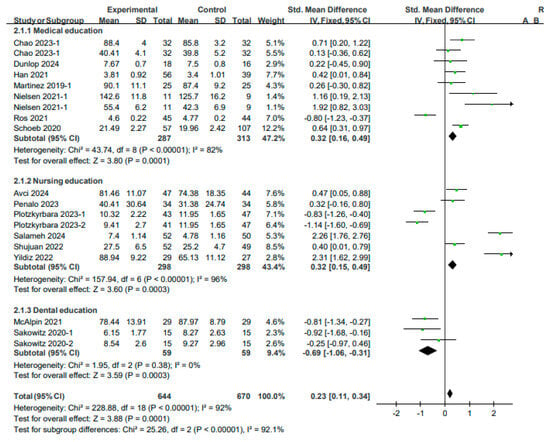
Figure 6.
Forest plot for effects of VR on the skill performance score.
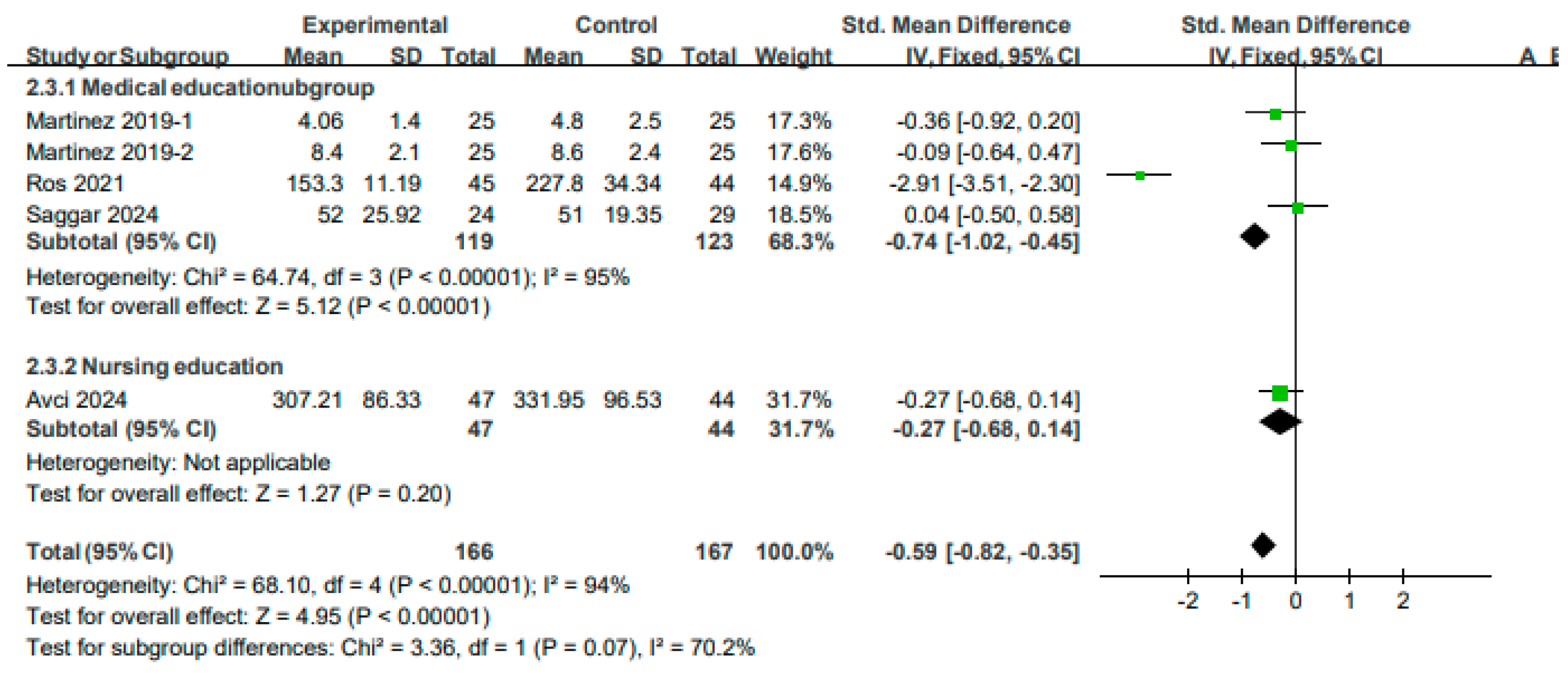
3.4.2. Performance Time
A fixed-effects model was used to perform the analysis, as the studies included in the analysis of technique performance time exhibited high heterogeneity (I2 = 94%, p < 0.00001). An analysis of three studies (four outcomes) on medical education revealed that the skill performance in the experimental group was significantly shorter than that in the control group (SMD: −0.74, 95% CI: −1.02 to −0.45, p < 0.00001). An analysis of one study on nursing education revealed no significant differences between the experimental and control groups (SMD: −0.27, 95% CI: −0.68 to 0.14, p > 0.05). In summary, the results of a meta-analysis of four studies (five results) involving a total of 333 participants revealed that VR education had a positive effect on reducing the time required for performing the procedure (SMD: −0.59, 95% CI: −0.82 to −0.35, p < 0.0001) (see Figure 7).
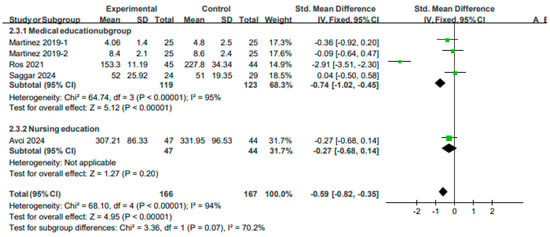
Figure 7.
Forest plot for effects of VR on skill performance time.
A comparison between the effects of the AR app and the standard simulator on medical education focusing on medical history taking revealed that the DOPS score was significantly higher in AR (p < 0.05). Moreover, no significant differences were observed between the groups in terms of the Mini-CEX score (p > 0.05) [21]. A comparison between the effects of VR and e-learning on medical education focusing on ultrasound revealed that the OSAUS score was significantly higher in the VR group (p < 0.01). The hand-eye score was higher in the VR group; however, the difference was not significant (p > 0.05) [61]. A comparison between VR-standardized patients with standardized patients in a study on medical education focusing on dizziness revealed that the scores for the neurological examination were significantly higher in the VR group (p < 0.05) [50]. Furthermore, an analysis of a study on VR with a case discussion in medical education focusing on myocardial infarction revealed no significant differences between the groups in terms of the OSCE score and the performance time for an EKG and thrombolysis (p > 0.05) [57]. An analysis of a study on the effects of VR with general lectures on medical education focusing on perinatal diseases revealed no significant difference between the groups (p > 0.05); however, the performance time for the procedure was significantly shorter (p < 0.05) [27]. This finding indicates that VR is effective in shortening the performance time for the procedure. A comparison between the effects of VR and general lectures on medical education focusing on lumbar puncture patients revealed that the skill evaluation did not differ significantly between the groups (p > 0.05); however, the skill performance time was significantly shorter in the VR group (p < 0.01) [63]. A comparison between the effects of MR and face-to-face instruction on medical education focusing on bladder catheters revealed that the OSCE score was significantly higher in the MR group (p < 0.01) [22]. A comparison between the effects of the AR app and simulator education on nursing education focusing on IV catheters revealed that the IVC–PPSF score was significantly higher in the AR group (p < 0.05); however, the skill time did not differ significantly between the groups (p > 0.05) [68]. A comparison between the effects of VR with and without structured briefing on nursing education focusing on surgery revealed that the performance scores did not differ significantly between the groups (p < 0.05) [73]. A comparison between the OSCE scores of 2D, VR-low, and VR-high nursing education focusing on tracheal suctioning revealed that the scores for 2D education were more effective in each domain [74]. An analysis of a study on the effects of VR and general education on nursing education focusing on pediatric examination revealed the scores were significantly higher in the VR group (p > 0.001) [73]. A comparison between the effects of VR and a practice model on nursing education focusing on IV catheters revealed that the skill scores were significantly higher in the VR group (p < 0.01) [78]. A comparison between cases of correct responses in the practice process of VR and 2D education in dental diagnosis and treatment revealed that the control group had a significantly higher score in the first scenario (p < 0.05); however, no significant difference was observed between the groups in the second scenario (p > 0.05) [82]. Thus, education using VR technologies has a significant positive effect or a similar effect on improving clinical skills compared with existing education.
3.5. Effects of VR on Attitudes
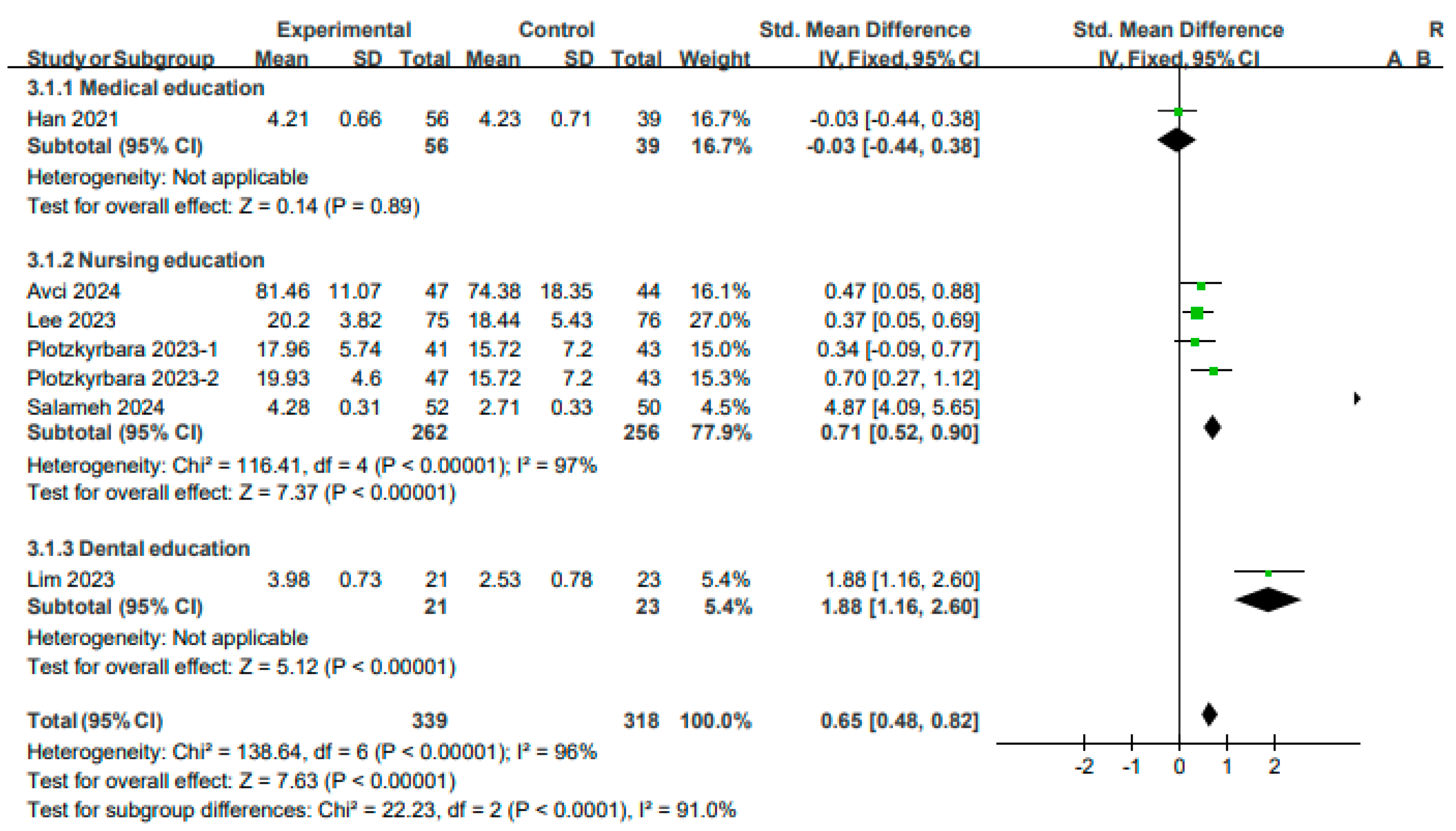
3.5.1. Satisfaction
Analyses of educational satisfaction were performed using a fixed model, as the studies included exhibited high heterogeneity (I2 = 96%, p < 0.00001). An analysis of one study on medical education revealed no significant differences between the experimental and control groups (SMD: −0.03, 95% CI: −0.44–0.38, p > 0.05). An analysis of four studies on nursing education (five outcomes) revealed that the satisfaction scores in the experimental group were significantly higher than those in the control group (SMD: 0.71, 95% CI: 0.52–0.89, p < 0.00001). An analysis of one study on dental education revealed that the satisfaction scores in the experimental group were significantly higher than those in the control group (SMD: 1.88, 95% CI: 1.16–2.60, p < 0.00001). In summary, the results of a meta-analysis of six studies (seven results) involving a total of 657 participants revealed that VR education yielded higher satisfaction levels (SMD: 0.65, 95% CI: 0.48–0.81, p < 0.00001) (see Figure 8).
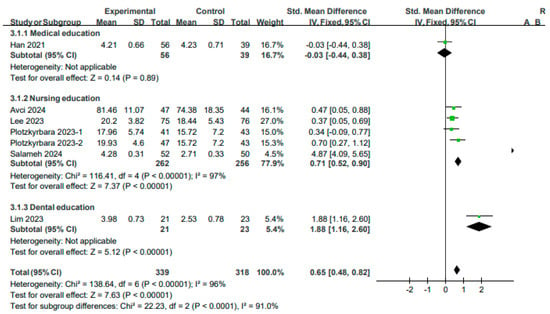
Figure 8.
Forest plot for the effects of VR on satisfaction.
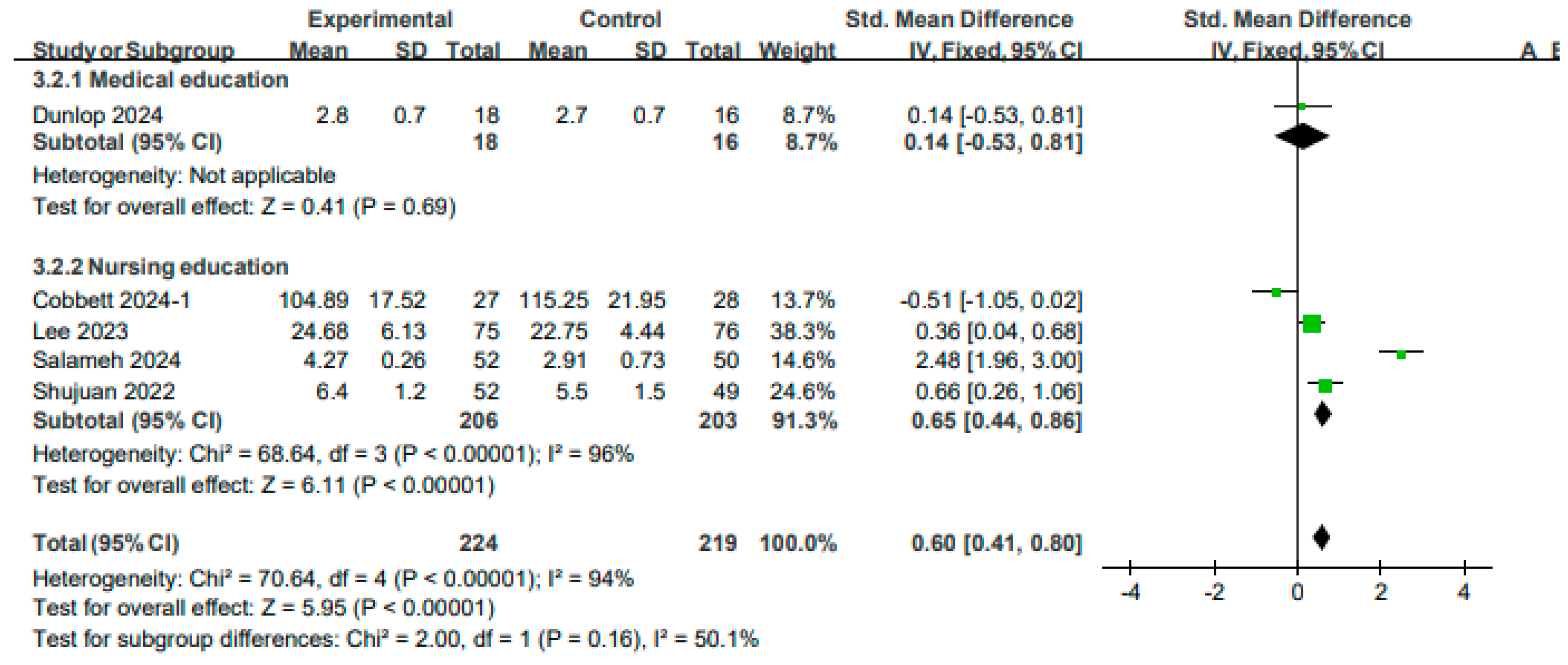
3.5.2. Confidence
A fixed model was used to perform analyses of confidence after education as the studies included exhibited high heterogeneity (I2 = 94%, p < 0.00001). An analysis of one study on medical education revealed that the difference between the experimental and control groups was not significant (SMD: 0.14, 95% CI: −0.53–0.81, p > 0.05). An analysis of four studies on nursing education revealed that the level of confidence in the experimental group was significantly higher than that in the control group (SMD: 0.65, 95% CI: 0.44~0.86, p < 0.00001). Overall, confidence was significantly higher after VR education (SMD: 0.60, 95% CI: 0.41–0.80, p < 0.00001) (see Figure 9). An analysis of a study comparing VR-standardized patients with standardized patients in a study on medical education focusing on patients with dizziness revealed no significant differences between the groups in terms of satisfaction and sense of presence (p > 0.05) [50]. An analysis of a study comparing the effects of AR app and simulator education focusing on nursing education focusing on IV catheters revealed no significant differences between the groups in terms of satisfaction and confidence (p > 0.05) [68]. An analysis of a study comparing the effects of VR and general lectures on medical education for postpartum hemorrhage revealed no significant differences between the groups in terms of satisfaction and confidence (p > 0.05) [27]. An analysis of a study comparing the effects of VR and Zoom lectures on nursing education for blood transfusion revealed that the satisfaction and confidence levels in the VR group were significantly higher (p < 0.05). The self-efficacy levels were higher in the test group; however, the difference was not significant (p > 0.05) [28]. An analysis of a study comparing the effects of VR and general lectures on nursing education for pediatric examinations revealed that the satisfaction and confidence levels in the VR group were significantly higher (p < 0.001) [29]. Similarly, an analysis of a study comparing the effects of VR and 2D lectures on dental imaging-related education learning revealed that the satisfaction and self-efficacy levels were significantly higher in the test group (p < 0.01) [30]. An analysis of a study on perinatal nursing education revealed that the confidence level was higher in the VR group; however, this difference was not significant (p > 0.05). Moreover, the anxiety levels were significantly higher in the VR group (p < 0.01) [26]. An evaluation of the acceptability of the program and the overall program experience of VR and 2D education in the medical education for internal medicine and surgical diseases revealed that most of the responses to the evaluation of the experience were positive and that four of the 11 items were significantly higher in the VR group (p < 0.05). A comparison between 3D and 2D VR revealed that the participants in the 2D group were more aware of the changes in the external environment; however, the participants in the 3D VR group exhibited a higher level of presence [47].
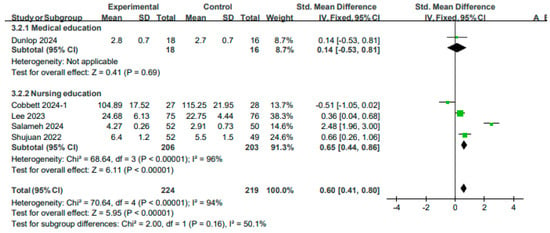
Figure 9.
Forest plot for the effects of VR on confidence.
4. Discussion
4.1. Study Characteristics
This systematic review and meta-analysis aimed to analyze the educational effects and influence of VR in the field of health education. An analysis of the year of publication revealed that many studies have been published consistently from 2021 to the present, owing to the significant changes in the field of education caused by the increased interest in non-face-to-face education and the rapid development of technology since the outbreak of the COVID-19 pandemic. Although studies have been conducted in 19 countries, the majority (n = 17) were conducted in Asia, followed by Europe (n = 14) and North America (n = 10). Notably, few studies have been conducted in low-income countries; this may be attributed to various technical and cost constraints [65,75]. Programs specifically designed for low-income countries must be conducted, considering the impact of VR technology on improving medical education, which may be attributed to its economic feasibility and high efficiency, excluding the initial cost. Twenty-six, fourteen, and five studies have been conducted in the fields of medical, nursing, and dental education. Studies on oriental medicine, alternative medicine education, and VR-based education focusing on image analysis workers were retrieved initially; however, these studies were excluded from the final analysis as they were not RCTs. Ten (22.2%), seven (n = 15.6%), five (11.1%), five (11.1%), and four (8.9%) studies focused on the topic of internal medicine, emergency medicine, surgery, dentistry, and simple skill practice, respectively. Only two BLS courses on cardiopulmonary resuscitation were included [53,59]. Most scenarios in other fields were also related to emergency situations for patients. This finding indicates that VR facilitates the simulation of emergency situations that are difficult to reproduce in real life or surgeries and techniques that are difficult to practice on patients. A classification of the studies according to the technology used in education revealed that VR was used in 38 of the 45 studies (84.4%), AR was used in four studies (8.9%), and MR was used in one study (2.2%). No studies were conducted using XR. Thus, it can be concluded most studies utilized VR, as it is more suitable for implementation in educational settings in terms of the cost accessibility of HMD and the diversity of programs.
4.2. Effects of VR on Knowledge
A meta-analysis of the evaluation of knowledge revealed that the knowledge score in the VR education group was significantly higher than that in the control group (SMD 0.28 [0.18, 0.39]). Positive effects were observed for medical education (SMD 0.43, [0.28, 0.58]), nursing education (SMD 0.13 [−0.02, 0.29]), and dental education (SMD −0.30 [−1.02, 0.42]) (p > 0.05). A study on the effects of AR on medical education for head and neck anatomy revealed that the knowledge scores in the AR group were higher than those in the 2D group (p < 0.05) [66]. A study on the effects of VR on medical education for urological diseases revealed that knowledge scores in the VR group were significantly higher than those in the general practice group (p < 0.001) [56]. A study on the effects of VR on medical education focusing on the anatomy and surgery of the esophagus and mediastinum revealed that the understanding of CT and surgical images in the VR group was higher than that in the 3D group (p < 0.05); however, knowledge regarding the mediastinal structure and general structure was similar in both groups (p > 0.05) [51]. A study on the effects of VR on medical education focusing on ECGs revealed that the knowledge regarding normal ECGs was similar in the general lecture and VR groups (p > 0.05); however, knowledge regarding abnormal ECGs (p < 0.001) was higher in the VR group, especially after eight weeks (p < 0.01) [52]. This finding played a significant role in improving and maintaining knowledge. A study on the effects of VR on nursing education focusing on blood transfusion revealed that the knowledge scores in the VR group were higher than those in the Zoom lecture group (p < 0.01) [28]. A study on the effects of VR on nursing education focusing on pediatric epilepsy revealed that the knowledge scores in the VR group were higher than those in the general lecture group (p < 0.01) [77]. This finding indicates that the effects of VR can be significantly more positive than those of existing educational methods. A study on the effects of VR on medical education focusing on internal medicine and surgery revealed that similar knowledge scores were observed in the VR and 2D groups (p > 0.05); however, the knowledge scores increased significantly after education (p < 0.05) [47]. This finding suggests that the two groups achieved similar levels of learning as the scenario formats and emotional engagement levels were almost identical. In addition, these results also suggest that higher immersion does not necessarily lead to higher educational effects and that multiple cognitive processes may affect educational effects. A study on the effects of VR on medical education focusing on postpartum hemorrhage revealed that the knowledge scores in the VR and general lecture groups were similar (p > 0.05); however, the knowledge scores increased significantly after education (p < 0.001) [27]. A study on the effects of AR on medical education focusing on skin diseases revealed that the effects of AR were similar to those of mobile devices without AR (p > 0.05); however, the knowledge scores increased significantly after education (p > 0.05) [62]. A study on the effects of VR on dental diagnosis and treatment education revealed that no significant differences were observed in the VR group in terms of the 2D and knowledge assessment (MCQ) scores (p > 0.05) [82]. A study on the effects of VR on medical education focusing on internal diseases revealed that evaluation scores in the VR group were higher than those of the general evaluation group (p < 0.01). This finding indicates that the use of VR improves reasoning and clinical skills by providing realistic simulations [46]. The findings of the abovementioned studies indicate that the use of VR had an effect similar to that of existing educational methods, regardless of whether the effects observed in the experimental group were positive effects or not significant. A significant improvement after education was observed in the experimental and control groups. This finding indicates that both types of education were effective; therefore, it is desirable to combine the two educational methods according to the purpose. Furthermore, no significant differences were observed between VR and high-fidelity mannequin simulation education in terms of knowledge scores in a study evaluating the effect of VR on nursing education focusing on perinatal disease (p > 0.05) [26]. High-fidelity simulation is expensive, as it requires intensive manpower and equipment [83,84]. In contrast, VR is relatively inexpensive and safe, can facilitate repetitive learning without restrictions, and has similar educational effects; therefore, its implementation in the field of education is feasible. A study on the effects of VR on medical education focusing on lumbar puncture revealed that the oral exam scores in the VR group were lower than those in the general education group (p < 0.001) [63]. A study on the effects of VR on nursing education focusing on tracheal suction revealed that the knowledge scores were similar in the 2D, low-level VR, and high-level VR groups (p > 0.05); however, the scores increased after the education. The scores in the 2D group were higher than those in the VR-low group (p < 0.05), whereas the scores in the 2D and VR-high groups were similar (p > 0.05) [74]. This finding suggests that VR and 2D education have similar effects or that 2D education may be more efficient, which may be attributed to discomfort, unfamiliarity, and concentration loss when operating VR-based education. Previous studies have shown that VR is effective in improving clinical competency [85,86,87,88]. Moreover, it can help gain knowledge by enabling self-directed learning and promoting active participation [89]. Previous studies have also reported that compared with non-immersive techniques, immersive VR learning can provide more knowledge [90]. VR provides visual, auditory, and various other forms of stimuli [91,92]; provides immediate feedback to learners via real-time interaction [93]; and improves the knowledge retention ability by enhancing three-dimensional imagination, active manipulation, and the exploration of learning skills. It also creates an enjoyable and attractive learning environment that fosters interest and curiosity [94,95,96]. Furthermore, the amount of learning increases as the learning satisfaction of the students increases; similarly, their dissatisfaction with learning decreases as their academic performance improves [83]. AR creates an immersive environment via a three-dimensional approach, wherein anatomy and virtual environments coexist and interact in the same space and time to enhance knowledge and understanding [84]. Thus, VR can aid in improving knowledge among medical professionals in various ways.
4.3. Effects of VR on Skills
The results of the meta-analysis of the skill scores conducted using the OSCE, checklist, and self-reported assessment revealed that VR was more effective in improving skill (SMD 0.23 [0.11, 0.34]). VR exhibited positive effects on medical (SMD 0.32 [0.16, 0.49]) and nursing (SMD 0.32, [0.15, 0.49]) education; however, it exhibited negative effects on dental education (SMD −0.69 [−1.06, −0.31]). The results of the meta-analysis of skill time revealed that this duration was shorter in the experimental group. The VR intervention was effective in reducing time in the experimental group (SMD −0.59 [−0.82, −0.35]). A decrease in the duration was also observed for medical education (SMD −0.74 [−1.02, −0.45]) and nursing education (SMD −0.27 [−0.68, 0.14]). A study on the effect of VR on medical education focusing on ultrasound revealed that the OSAUS score in the VR group was higher than that in the e-learning group (p < 0.01). Although the hand-eye score was also higher, it was not statistically significant (p > 0.05) [61]. A study on the effect of VR on medical education focusing on dizziness revealed that VR-standardized patients had higher skill scores than general standardized patients (p < 0.05) [50]. A study on the effect of VR on medical education focusing on myocardial infarction revealed that the OSCE scores and EKG/thrombolysis performance times in the VR group were similar to those in the discussion classes group (p > 0.05) [57]. This may be attributed to the advantages associated with discussion classes (control group) such as interest, maintenance and improvement of knowledge and skills, teamwork ability, and self-directed learning [97,98,99]. Moreover, the education was conducted once or for a short period of time. Thus, further expansion and long-term education are warranted in the future. A study on the effect of VR on medical education focusing on perinatal diseases revealed that the skill scores in the VR and general lecture groups were similar (p > 0.05); however, the skill performance time was shorter (p < 0.05) [27]. This finding indicates that VR is effective in reducing the performance time. A study on the effect of VR on medical education focusing on lumbar puncture revealed that the skill scores in the VR and general lecture groups were similar (p > 0.05); however, the skill performance time was shorter (p < 0.01) [63]. A study on medical education focusing on bladder catheters revealed that the OSCE scores of the MR education group were higher than those of the face-to-face instruction group (p < 0.01) [22]. A study on the effect of AR on nursing education focusing on IV catheters revealed that the skill scores (IVC–PPSF) in the AR group were higher than those of the simulator education group (p < 0.05); however, the skill times were similar (p > 0.05) [68]. A study on the effect of AR on medical education focusing on history taking revealed that the skill scores (DOPS) in the AR group were higher than those in the standard simulator group (p < 0.05); however, the skill scores (Mini-CEX) for other skills were similar (p > 0.05) [21]. This may be attributed to the high cognitive load interfering with learning performance as the intrinsic cognitive load increases in the VR group [100]. Furthermore, VR novices may face difficulty while operating the Mini-CEX, and the measurement scores may be similar because of the characteristics of Mini-CEX. Thus, a design that can control the intrinsic cognitive load while achieving effective educational effects must be used when designing a program. A comparison between the effects of structured and non-structured briefings on VR-based surgical nursing education revealed that the skill scores were similar (p < 0.05) [73]. A comparison among the OSCE scores of the 2D, VR-low, and VR-high groups in a study on the effects of VR on nursing education focusing on tracheal suction revealed that the scores of the 2D group were higher than those of the VR-low and VR-high groups [74]. This finding may be attributed to 70% of students being unfamiliar with VR interventions, which led to them focusing on procedural learning. Unlike 2D video-based approaches, which show real catheters or gloves, VR-based approaches show abstract objects, which leads to low accuracy. The multifunctionality of VR-high in terms of simulation focus or interaction fidelity may lead to cognitive overload. Similarly, the haptic function may be awkward to use as it is unintuitive, which may frustrate users. Thus, adding skills using real mannequins to future VR-based education will produce better results. A study on the effect of VR on nursing education focusing on pediatric examination revealed that the skill scores in the VR group were higher than those in the general education group (p > 0.001) [73]. Similarly, a study on the effect of VR on nursing education focusing on IV catheters revealed that the skill scores in the VR group were higher than those in the practice model group (p < 0.01) [78]. A study on the effects of VR on dental diagnosis and treatment revealed that the skill scores in the VR group were higher than those of the control group for the first scenario in practice performance (p < 0.05); no significant differences were observed for the other scenarios (p > 0.05) [82]. A similar or more positive ability to improve the clinical skills was observed in the experimental group compared with that in the control group. Thus, VR improves psychomotor skills by facilitating learning through various senses and allowing repeated performance without space and time constraints [74]. VR surgical simulators are effective in improving surgical skills, as they are associated with a short setup time and are repeatable [101,102]. Immersive VR-based education enables learners to perform clinical techniques, such as anesthesia, more accurately and confidently [91]. This approach has the advantage of enabling learners to directly repeat procedural steps until they build confidence and avoid harming the patient during the process [92,103]. Although not included in the meta-analysis, the skill score (CSA) in the VR group was higher than that in the general education group in six of the eleven cases (p < 0.05) in a BLS medical education study; moreover, the no flow time was longer (p < 0.001) [53]. Notably, the VR group had a shorter no flow time (p < 0.01), lower performance penalty (p < 0.001), and higher skill scores (CSAs) in five of the 11 cases (p < 0.001) in another BLS education study [59]. A comparison between the effects of a 2-week and a 4-week VR-based education program on emergency medicine education revealed that the OSCE scores were similar (p > 0.05) but higher in the 4-week education group (p < 0.05) [55]. In addition, a study on the effect of VR on nursing education focusing on disaster situations revealed that compared with mannequin education, the use of VR improved knowledge, skills, and confidence (p < 0.01) [75]. This educational method utilizes the greatest advantage of VR technology, thereby enabling learning in a safe and controlled manner while practicing skills by implementing situations that cannot be reproduced, such as emergencies and disaster situations [104].
4.4. Effects of VR on Attitudes
The results of the meta-analysis on satisfaction and confidence performed by analyzing the satisfaction, confidence, self-efficacy, usability, technology acceptance, presence, emotion, subjective experience, and preference levels to evaluate attitude revealed positive effects on satisfaction (SMD 0.65 [0.48, 0.82]) and confidence (SMD 0.60 [0.41, 0.80]). In satisfaction, VR exhibited negative effects on medical (SMD −0.03 [−0.44, 0.38]) and positive effects on nursing (SMD 0.71, [0.52, 0.90]) and dental (SMD 1.88, [1.16, 2.60]) education. And in confidence, VR exhibited positive effects on medical (SMD 0.14 [−0.53, 0.81]) and nursing (SMD 0.65, [0.44, 0.86]) education.
This finding indicates that VR exerts a positive effect on learning attitude. A study on the effect of VR on medical education focusing on dizzy patients revealed that VR-standardized patients had similar satisfaction and sense of presence as standardized patients (p > 0.05) [50]. A study on the effect of AR on nursing education focusing on IV catheters revealed that AR and simulator education yielded similar satisfaction and confidence levels (p > 0.05) [68]. A study on the effect of VR on medical education focusing on postpartum hemorrhage revealed that VR and general lectures yielded similar satisfaction and confidence levels (p > 0.05) [27]. A study on the effect of VR on nursing education focusing on transfusion revealed that the satisfaction and confidence levels in the VR group were higher than those in the Zoom lecture group (p < 0.05), and self-efficacy was higher but not significant (p > 0.05) [28]. Confidence is the belief that a specific expectation can be achieved, whereas self-efficacy is the judgment of the ability to perform necessary actions. The experimental group gained more knowledge and confidence; however, no significant differences were observed in terms of their ability to perform in a real environment. Therefore, VR must be designed such that higher practicality and educational effects can be achieved in future studies [28]. A study on the effect of VR on nursing education focusing on tracheal suction revealed that the satisfaction levels were in order of VR-low> VR-high> 2D video (p < 0.001) [74]. The VR experience was realistic, interactive, and immersive. Furthermore, it enabled healthcare personnel to practice skills in a safe environment, learn from mistakes, and increase knowledge and confidence. The simpler VR-low had higher satisfaction levels; therefore, complex functions that cause an excessive cognitive load must be avoided when developing a VR program. A study on the effect of VR on nursing education focusing on pediatric examination revealed that the satisfaction and confidence levels in the VR group were higher than those in the general lecture group (p < 0.001) [29]. A study on the effect of VR on dental imaging revealed that the learning satisfaction and self-efficacy levels in the VR group were higher than those in the 2D video group (p < 0.01) [30]. In addition, a study on the effect of VR on nursing education focusing on perinatal nursing revealed that the anxiety and confidence levels of the participants in the VR group were higher than those of the participants in the mannequin simulation group (p < 0.01); however, this was not significant (p > 0.05) [26]. This finding indicates that the confidence levels were increased in both groups; however, a significant increase in anxiety may have been observed due to the VR technology itself. Previous studies have suggested support and kindness from faculty, mentoring from seniors, and orientation on the environment and simulation can reduce anxiety [105]. Thus, VR simulation can greatly influence the attitude of the learners by creating a realistic and safe environment for students to practice; helping them gain knowledge; help them improve clinical performance, critical thinking, and decision-making; and increase the confidence and communication levels [26,106]. Although not included in the research synthesis, previous studies have shown that VR-based education is highly acceptable in terms of program acceptability and overall evaluation [107]; however, there were cases wherein face-to-face simulation was preferred [26]. This may be attributed to technical reasons. Thus, configuring it in an easy and convenient method is necessary so that students can concentrate without becoming lost. In addition, a study on the effect of VR on medical education focusing on internal and surgical diseases revealed that the scores in the VR group were higher than those in the 2D group in four of the eleven experiential evaluations (p < 0.05). External changes were more recognizable in the 2D group; however, a higher presence was observed in the VR group [47]. High participation and positive responses were observed in the VR group. Thus, it may be suitable to develop a 3D that is more suitable for group-based simulation and 2D as a self-directed learning tool using familiar equipment at home.
5. Limitations
The articles with RCTs published in English were included in the present study, but its scope may be limited. Various VR technologies were evaluated in this study; however, significant differences have been observed even within the same VR and AR technologies depending on the type of HMDs and the level of program sophistication used. The high heterogeneity between the studies made it difficult to perform the meta-analysis. The study design of the included studies varied, and the educational content, educational time, and educational period of the intervention group were diverse. Heterogeneity was also observed between the control groups of different studies, such as general face-to-face lectures, Zoom lectures, e-learning, high-fidelity and low-fidelity simulations, and 2D images. The study population comprised both students and residents. Heterogeneity may be observed among the students in terms of knowledge and skills in each grade.
6. Conclusions
This systematic literature review and meta-analysis of RCTs aimed to examine the significance of VR in healthcare education. An analysis of the 45 selected studies revealed that the implementation of VR facilitated a significant improvement in the knowledge (SMD: 0.28, 95% CI: 0.18–0.39, p < 0.001) and skill scores (SMD: 0.23, 95% CI: 0.11–0.34, p < 0.001), shortened the skill performance time (SMD: −0.59, 95% CI: −0.82 to −0.35, p < 0.001), and improved the satisfaction (SMD: 0.65, 95% CI: 0.48–0.81, p < 0.001) and confidence levels (SMD: 0.60, 95% CI: 0.41–0.80, p < 0.001). The findings of this study indicate that VR can substantially enhance learning outcomes while reducing the logistical challenges such as manpower, time, space, and cost often associated with traditional training methods. Based on the analysis of prior studies, the following suggestions are proposed for future research: First, studies based on educational theory and frameworks using objective evaluation tools must be conducted in the future. Second, studies that include long-term education focusing on a large number of participants are needed. Third, VR simulations that exploit collaboration with other participants in the virtual world must be developed. In the coming years, VR technologies will be utilized more actively in healthcare education with more realistic and user-friendly simulations. VR-based education will promote self-directed learning by providing immersive, interactive, and immediate feedback on their experiences. This approach could be especially effective when integrating VR with traditional educational methods, as it enhances both the quality of learning and the overall competence of healthcare professionals.
Author Contributions
Conceptualization, N.S. and Y.H.; methodology, Y.H. and J.P.; software, M.K. and J.P.; validation, H.S., Y.H., and J.P.; formal analysis, H.S. and Y.H.; investigation, H.S. and Y.H.; resources, H.S. and Y.H.; data curation, H.S. and Y.H.; writing—original draft preparation, H.S. and Y.H.; writing—review and editing, N.S. and M.K.; visualization, Y.H.; supervision, N.S. and Y.H.; project administration, N.S. and Y.H.; funding acquisition, H.S. and J.P. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A. Search Strings
| MEDLINE (EBSCO) | ||
| 1 | (“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”).m_titl. | 71,845 |
| 2 | (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”).m_titl. | 462,755 |
| 3 | (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”).m_titl. | 500,667 |
| 4 | 1 and 2 and 3 | 1333 |
| Embase (Elsevier) | ||
| 1 | (‘vr’:ti OR ‘virtual’:ti OR ‘virtual reality’:ti OR ‘vrs’:ti OR ‘vre’:ti OR ‘ar’:ti OR ‘augmented’:ti OR ‘augmented reality’:ti OR ‘mr’:ti OR ‘mixed reality’:ti OR ‘xr’:ti OR ‘extended reality’:ti) AND [2014–2024]/py | 69,969 |
| 2 | (‘medical’:ti OR ‘medicine’:ti OR ‘doctor’:ti OR ‘dental’:ti OR ‘dentistry’:ti OR ‘complementary medicine’:ti OR ‘traditional chinese medicine’:ti OR ‘korean medicine’:ti OR ‘nurse’:ti OR ‘nursing’:ti) AND [2014–2024]/py | 388,917 |
| 3 | (‘education’:ti OR ‘teach’:ti OR ‘teaching’:ti OR ‘learn’:ti OR ‘learning’:ti OR ‘lesson’:ti OR ‘instruction’:ti OR ‘practice’:ti OR ‘clerkship’:ti OR ‘clinical practice’:ti OR ‘clinical clerkship’:ti OR ‘experimental education’:ti OR ‘experimental teaching’:ti OR ‘internship’:ti OR ‘residency’:ti OR ‘bedside teaching’:ti OR ‘student’:ti OR ‘undergraduate’:ti OR ‘intern’:ti OR ‘resident’:ti OR ‘fellow’:ti) AND [2014–2024]/py | 422,394 |
| 4 | 1 and 2 and 3 | 952 |
| Cochrane Library (Wiley) | ||
| 1 | (“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”):ti | 132,39 |
| 2 | (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”):ti | 47,419 |
| 3 | (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”):ti | 56,280 |
| 4 | 1 and 2 and 3 | 234 |
| CINAHL (EBSCO) | ||
| 1 | (VR or virtual or virtual reality or VRS or VRE or AR or augmented or augmented reality or MR or mixed reality or XR or extended reality).m_titl. | 11,839 |
| 2 | (medical or medicine or doctor or dental or dentistry or complementary medicine or traditional chinese medicine or korean medicine or nurse or nursing).m_titl. | 76,674 |
| 3 | (education or teach or teaching or learn or learning or lesson or instruction or practice or clerkship or clinical practice or clinical clerkship or experimental education or experimental teaching or internship or residency or bedside teaching or student or undergraduate or intern or resident or fellow).m_titl. | 67,806 |
| 4 | 1 and 2 and 3 | 1000 |
| PsycINFO (EBSCO) | ||
| 1 | TI (“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”) | 11,307 |
| 2 | TI (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”) | 34,189 |
| 3 | TI (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”) | 160,495 |
| 4 | 1 and 2 and 3 | 108 |
| ProQuest Central | ||
| 1 | title(“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”)Limits applied | 1,016,668 |
| 2 | title(“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”)Limits applied | 2,922,279 |
| 3 | title(“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”)Limits applied | 3,910,942 |
| 4 | 1 and 2 and 3 | 1050 |
| Web of Science (Clarivate Analytics) | ||
| 1 | TI = (“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”) | 151,266 |
| 2 | TI = (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”) | 365,469 |
| 3 | TI = (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”) | 1,026,916 |
| 4 | 1 and 2 and 3 | 1118 |
| Scopus (Elsevier) | ||
| 1 | TITLE (“vr” OR “virtual” OR “virtual reality” OR “vrs” OR “vre” OR “ar” OR “augmented” OR “augmented reality” OR “mr” OR “mixed reality” OR “xr” OR “extended reality”) AND PUBYEAR > 2013 | 193,784 |
| 2 | TITLE (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”) AND PUBYEAR > 2013 | 516,771 |
| 3 | TITLE (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”) AND PUBYEAR > 2013 | 1,705,878 |
| 4 | 1 and 2 and 3 | 1712 |
| EBSCO (Academic Search Complete) | ||
| 1 | TI (“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”) | 23,072 |
| 2 | TI (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”) | 89,381 |
| 3 | TI (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”) | 207,452 |
| 4 | 1 and 2 and 3 | 175 |
| Education Resources Information Centre (EBSCO) | ||
| 1 | TI (“VR” OR “virtual” OR “virtual reality” OR “VRS” OR “VRE” OR “AR” OR “augmented” OR “augmented reality” OR “MR” OR “mixed reality” OR “XR” OR “extended reality”) | 2441 |
| 2 | TI (“medical” OR “medicine” OR “doctor” OR “dental” OR “dentistry” OR “complementary medicine” OR “traditional chinese medicine” OR “korean medicine” OR “nurse” OR “nursing”) | 1748 |
| 3 | TI (“education” OR “teach” OR “teaching” OR “learn” OR “learning” OR “lesson” OR “instruction” OR “practice” OR “clerkship” OR “clinical practice” OR “clinical clerkship” OR “experimental education” OR “experimental teaching” OR “internship” OR “residency” OR “bedside teaching” OR “student” OR “undergraduate” OR “intern” OR “resident” OR “fellow”) | 104,234 |
| 4 | 1 and 2 and 3 | 31 |
Appendix B. Key Information of the Included Studies
| First Author (Year), Country | Participants (n) | Study Method | Tech, Devices | Topics | Interventions | Assessments | Results |
| Abreu (2021) [46] Portugal | Medical students (n = 35) Ⓔ n = 35 Ⓒ n = 35 | RCT (cross -over) | VR, BodyInteract | Four scenarios of internal medicine1) | Ⓔ VR (test by virtual interactive patients (VIPs), 20 min Ⓒ test by MCQ2), 20 min | Test Scores | Ⓔ > Ⓒ p < 0.01, Ⓔ 73.34 ± 10.82 Ⓒ 67.40 ± 8.96 |
| Satisfaction | adequate, satisfactory in both Ⓔ, Ⓒ Ⓔ > Ⓒ in knowledge, approximation to reality p < 0.05 | ||||||
| Avci (2024) [68] Turkey | Nursing students (n = 91) Ⓔ n = 47 Ⓒ n = 44 | RCT | AR, mobile app | IV catheter placement skill training | Ⓔ AR mobile app (10 min) Ⓒ Standard simulator | IVC–PPSF3) | Ⓔ > Ⓒ p > 0.05, Ⓔ 81.46 ± 11.07 Ⓒ 74.38 ± 18.35 |
| Average of time(s) | Ⓔ < Ⓒ p > 0.05, Ⓔ 307.21 ± 86.33 Ⓒ 331.95 ± 96.53 | ||||||
| SCLS4) (1) Satisfaction (2) Self-confidence | n/s5) in Ⓔ, Ⓒ p > 0.05, Ⓔ 54.31 ± 5.25 Ⓒ 51.52 ± 5.32 1) Ⓔ 81.46 ± 11.07 Ⓒ 74.38 ± 18.35 p > 0.05 2) Ⓔ 54.31 ± 5.25 Ⓒ 51.52 ± 5.32 p < 0.05 | ||||||
| Babaita (2024) [69] Japan | Nursing students (n = 57) Ⓔ n = 27 Ⓒ n = 30 | RCT | 360° VR, HMD6) (Meta Quest2) | Closed tracheal suction training | Ⓔ 360° VR simulation + hands-on practice with mannequin Ⓒ Instructor’s demonstration + hands-on practice with mannequin | Psychomotor skills | n/s in Ⓔ, Ⓒ p = 0.700 |
| Knowledge | n/s in Ⓔ, Ⓒ p = 0.952 | ||||||
| Satisfaction | Ⓔ > Ⓒ p < 0.01 | ||||||
| Confidence | n/s in Ⓔ, Ⓒ p = 0.273 | ||||||
| Bray (2023) [47] UK | Medical students (n = 25) | RCT (cross -over) | VR, HMD (OculusRift) | 4 scenarios (3D meningitis, 3D neutropenia, 2D divericulitis, 2D pulmonary embolism) | Ⓔ 3D VR (OculusRift headset + hand controller) Ⓒ 2D (laptop + mouse) | MCQ2) | n/s in Ⓔ, Ⓒ p = 0.56 Ⓔ 11.6 (pre)→12.9 (post)→15.3 (1 mon) Ⓒ 14.2 (pre)→15.2 (post)→13.3 (1 mon) |
| Evaluation of experiences | 4 of 11 items Ⓔ > Ⓒ p < 0.05 | ||||||
| Chao (2021) [20] Taiwan | Medical students (n = 32) Ⓔ n = 16 Ⓒ n = 16 | RCT (pilot, mixed) | 360° VR, HMD (HTC Vive) | Clinical scenario of otolaryngology | Ⓔ 360° VR (immersive) with HMD 10 min Ⓒ 120° 2D (non-immersive) with HMD, 10 min | Paas-CLS6) | n/s in Ⓔ, Ⓒ p = 0.78 |
| NASA-TLX7) | Only ‘physical demand’ was Ⓔ > Ⓒ p = 0.047 | ||||||
| Task reaction time | Ⓔ (11 s) > Ⓒ (1.3 s) p < 0.001 * | ||||||
| HRV8) | n/s in Ⓔ, Ⓒ p > 0.05 | ||||||
| Milestone level | n/s in Ⓔ, Ⓒ p = 0.02 | ||||||
| AttrakDiff2 | n/s in Ⓔ, Ⓒ p > 0.05 | ||||||
| Chao (2023) [21] Taiwan | Medical students (n = 64) Ⓔ n = 32 Ⓒ n=32 | RCT | VR, HMD (HTC Vive) | Training of history taking and physical examination | Ⓔ 360° VR 10 min Ⓒ 2D video 10 min | DOPS9) | Ⓔ > Ⓒ p = 0.01, Ⓔ 88.4 ± 4.0 Ⓒ 85.8 ± 3.2 |
| Mini-CEX10) | Ⓔ > Ⓒ p = 0.75, Ⓔ 40.41 ± 4.1 Ⓒ 39.8 ± 5.2 | ||||||
| CLC11) | Ⓔ > Ⓒ p = 0.04, Ⓔ 20.1 ± 2.0 Ⓒ 18.9 ± 2.5 | ||||||
| Chou (2024) [70] Taiwan | Nursing students (n = 84) Ⓔ n = 42 Ⓒ n = 42 | RCT (pragmatic) | VR, HMD (HTC Vive Focus 3) | Nurse–patient relationship establishment | Ⓔ VR communication simulation (VRCS) Ⓒ 2D nurse–patient communication teaching video | Communication ability | Ⓔ > Ⓒ p < 0.001 |
| Communication confidence | Ⓔ > Ⓒ p < 0.001 | ||||||
| Clinical practice stress | Ⓔ < Ⓒ p < 0.05 | ||||||
| Learning satisfaction | Ⓔ > Ⓒ p < 0.001 | ||||||
| Cobbett (2024) [26] Canada | Nursing students (n = 56) Ⓔ n = 27 Ⓒ n = 28 | RCT | VR, with v-Sim®12) | Maternal newborn nursing (preeclampsia, group-B strep | Ⓔ VR simulation, 45 min Ⓒ Face-to-face high-fidelity mannequin clinical simulation, 45 min | NASC-CDM13) (1) Anxiety (2) Confidence | 1) Ⓔ > Ⓒ p = 0.002, Ⓔ 73.26 ± 19.95 Ⓒ 57.75 ± 15.25 2) Ⓔ > Ⓒ p = 0.059, Ⓔ 104.89 ± 17.52 Ⓒ 115.25 ± 21.95 |
| Knowledge test | n/s in Ⓔ, Ⓒ p > 0.05 1) Ⓔ 4.12 ± 1.54 Ⓒ 4.80 ± 1.19 p = 0.09 2) Ⓔ 6.40 ± 1.73 Ⓒ 6.82 ± 1.25 p = 0.31 | ||||||
| Daud (2023) [79] Qatar | Dental students (n = 23) Ⓔ n = 12 Ⓒ n = 11 | RCT, cross -over | VR, SIM to CARE DenteⓇ14) | Case of clinical restorative dentistry | ① VRHS15) → CSE16) ② CSE → VRHS | Perceptions | Three of 14 items significant difference |
| Dunlop (2024) [27] Ireland | Medical students (n = 34) Ⓔ n = 18 Ⓒ n = 16 | RCT, double-blind | VR, HMD (Oculus lens-2) | Two clinical scenarios of postpartum17) | Ⓔ VR immersive tutorial Ⓒ Traditional lecture with PPT18), 15 min | MCQ | n/s in Ⓔ, Ⓒ p = 0.770 Ⓔ 7.7 ± 0.8→9.4 ± 0.9 p < 0.001 Ⓒ 6.7 ± 2.0→9.3 ± 1.1 p < 0.001 |
| Skill assessment | n/s in Ⓔ, Ⓒ p = 0.743, Ⓔ 7.6 ± 0.7 Ⓒ 7.5 ± 0.8 | ||||||
| Time to complete task(s) | Ⓔ < Ⓒ p = 0.039, Ⓔ 1.01~2.0 Ⓒ 2.01~3.0 | ||||||
| Confidence levels | n/s in Ⓔ, Ⓒ p = 0.639 Ⓔ 1.3 ± 0.6→2.8 ± 0.7 p < 0.001 Ⓒ 1.1 ± 0.5→2.7 ± 0.7 p < 0.001 | ||||||
| Satisfaction | n/s in Ⓔ, Ⓒ p > 0.05 | ||||||
| Ekstrand (2018) [48] Canada | Medical students (n = 64) Ⓔ n = 31 Ⓒ n = 33 | RCT | VR, HMD (HTC Vive) | Neuroanatomy | Ⓔ VR-based study Ⓒ Paper-based study | Score of test | n/s in Ⓔ, Ⓒ p > 0.05 |
| Satisfaction | Neurophobia decreased | ||||||
| Fung (2023) [71] China | Nursing students (n = 61) Ⓔ n = 30 Ⓒ n = 31 | RCT, cross- over | VR, with DxR Nursing SELECT platform | Two clinical scenarios19) | Ⓔ VR simulation, 3 h Ⓒ PBL20) with Zoom, 3 h (with pre-briefing 15 min, after debriefing) | CCQ21) | n/s in Ⓔ, Ⓒ p > 0.05 |
| IAPCC-SV22) | n/s in Ⓔ, Ⓒ p > 0.05 | ||||||
| Gan (2023) [49] China | Medical students (n = 108) Ⓔ n = 53 Ⓒ n = 55 | RCT | VR, with SteamVR (PC, HMD) | Tendon suture operation skill | (8 h lecture, 6 h practice for 2 weeks) Ⓔ VR simulator Ⓒ Lecture with PPT | Questionnaire about carrier choice and study habits | Two items Ⓔ > Ⓒ p < 0.05, n/s in other p > 0.05 |
| Total score of clinical practice in internship | Ⓔ > Ⓒ p < 0.05 | ||||||
| OSCE score | n/s in Ⓔ, Ⓒ p = 0.103 3 items Ⓔ > Ⓒ p < 0.05 (PE23), suturing, knotting) | ||||||
| Han (2021) [50] Korea | Medical students (n = 95) Ⓔ n = 56 Ⓒ n = 39 | RCT, single blinded | VR, VRNET, HMD (Oculus Rift) | One scenario (patient with dizziness) | Ⓔ VR-SP24) with VRNET 10 min Ⓒ SP 10 min | Realness | n/s in Ⓔ, Ⓒ p = 0.92, Ⓔ 4.28 ± 0.56 Ⓒ 4.27 ± 0.75 |
| Satisfaction | n/s in Ⓔ-Ⓒ p = 0.849, Ⓔ 4.21 ± 0.66 Ⓒ 4.23 ± 0.71 | ||||||
| NPE25) | Ⓔ > Ⓒ p = 0.043, Ⓔ 3.81 ± 0.92 Ⓒ 3.40 ± 1.01 | ||||||
| Imai (2022) [51] Japan | Medical students (n = 60) Ⓔ n = 30 Ⓒ n = 30 | RCT | VR, HMD (Oculus Quest) | Case of esophageal and mediastinal anatomy and surgery | Ⓔ Lecture with VR images Ⓒ Lecture with 3D images | Understanding CT26) images | Ⓔ > Ⓒ p = 0.0001, Ⓔ 2.93 ± 0.94 Ⓒ 1.83 ± 0.94 |
| Understanding of the mediastinal structure | n/s in Ⓔ, Ⓒ p > 0.05, Ⓔ 8.30 ± 1.23 Ⓒ 8.73 ± 1.22 | ||||||
| Interpretation of surgical images | Ⓔ > Ⓒ p = 0.0163, Ⓔ 6.93 ± 3.19 Ⓒ 5.00 ± 2.53 | ||||||
| The establishment of general knowledge | n/s in Ⓔ, Ⓒ p > 0.05, Ⓔ 9.83 ± 2.53 Ⓒ 9.13 ± 2.71 | ||||||
| Questionnaire | Ⓔ > Ⓒ in 2 items p < 0.05 | ||||||
| Iqbal (2024) [52] India | Medical students (n = 140) Ⓔ n = 71 Ⓒ n = 69 | RCT | VR, HMD | Interpreting ECG | Ⓔ VR simulation Ⓒ Didactic lecture ① Normal ECG ② Abnormal ECG | Test score (pre, post) | ① n/s in Ⓔ, Ⓒ p = 0.757, Ⓔ > Ⓒ (8 W) p < 0.001 Ⓔ 9.8 ± 8.4→24.3 ± 5.5→25.3 ± 5.6 (8 W) Ⓒ 8.3 ± 7.5→24.8 ± 6.3→20.7 ± 6.9 (8 W) ② Ⓔ > Ⓒ p < 0.001, Ⓔ > Ⓒ (8 W) p = 0.001 Ⓔ 7.0 ± 6.0→23.5 ± 6.2→19.2 ± 6.9 (8 W) Ⓒ 8.3 ± 6.6→17.7 ± 9.0→13.3 ± 10.2 (8 W) |
| No flow time (s) | Ⓔ > Ⓒ p = 0.000, Ⓔ 92.963 Ⓒ 82.031 | ||||||
| Issleib (2021) [53] Germany | Medical students (n = 160) Ⓔ n = 56 Ⓒ n = 104 | RCT | VR, VIREED | BLS27) course | Ⓔ VR-BLS 35 min + Laerdal QCPR mannequin (<1 h) Ⓒ Regular-BLS course lecture 45 min+ practice 1 h | CSA28) | Ⓔ > Ⓒ in 6 of 11 items p < 0.05 |
| SUS29) | 96% would like to use VR more frequently and felt very confident | ||||||
| Kenanidis (2023) [54] Greece | Medical students (n = 101) Ⓔ n = 47 Ⓒ n = 54 | RCT | VR, ORama VR30) | Case of THA31) (three sessions) | ① Ⓔ VR-Cup Ⓒ Stem w/o VR ② Ⓔ VR-Stem Ⓒ Cup w/o VR | Accuracy of skill32) | Ⓔ < Ⓒ p = 0.004 (closer to target) Ⓔ 54.5 ± 106.6° Ⓒ 89.9 ± 133.9° |
| Time to task complete | n/s in Ⓔ, Ⓒ p > 0.05 ① Ⓔ < Ⓒ p = 0.661 ② Ⓔ > Ⓒ p = 0.061 | ||||||
| Mistake number | Control-Stem > VR-Stem p = 0.016 | ||||||
| Law (2023) [55] China | Medical students (n = 130) Ⓔ n = 69 Ⓒ n = 69 | RCT | VR, Bodyinteract | 30 cases of emergency syndromes | Ⓔ VR during 4 W Ⓒ VR during 2 W | Test score | Ⓔ > Ⓒ p < 0.01 Ⓔ 8.9 ± 11.2→60.6 ± 26.0 p < 0.01 Ⓒ 9.1 ± 9.0→42.8 ± 21.3 p < 0.01 |
| OSCE score (/25) | Ⓔ > Ⓒ p = 0.23 Ⓔ 16.3 ± 3.2→21.7 ± 2.3 p < 0.01 Ⓒ 16.5 ± 2.6→19.1 ± 5.2 p = 0.15 | ||||||
| Satisfaction | 91.1% were responding favorably, 97.2% wants to continue VR in Ⓔ | ||||||
| Lebdai (2020) [56] France | Medical students (n = 85) Ⓔ n = 46 Ⓒ n = 39 | RCT | VR, MedicActiv platform | Case of urological disorders | Ⓔ VR(IVPS33)) 45 min (3 cases) + Ⓒ training +debriefing 45 min Ⓒ Regular faculty courses 12 h | Test score | Ⓔ > Ⓒ p < 0.001 Ⓔ 14.5 ± 2.4 Ⓒ 11.9 ± 3.0 |
| Satisfaction | Ⓔ > Ⓒ p < 0.05 4 items of 15 items | ||||||
| Lee (2023) [28] China | Nursing students (n = 151) Ⓔ n = 75 Ⓒ n = 76 | RCT, Single-blinded | VR, Google cardboard viewer | Blood transfusion education | Ⓔ 360° VR simulation Ⓒ General education with Zoom | RBTKQ-O34) | Ⓔ > Ⓒ p = 0.035 Ⓔ 12.87 ± 4.48→17.77 ± 5.44 Ⓒ 12.64 ± 4.79→15.87 ± 5.87 |
| SSCS35) 1) Self-confidence 2) Satisfaction | 1) Ⓔ > Ⓒ p = 0.013 Ⓔ 20.68 ± 4.91→24.69 ± 6.13 Ⓒ 20.74 ± 4.46→22.75 ± 4.44 2) Ⓔ > Ⓒ p = 0.024 Ⓔ 17.89 ± 3.57→20.20 ± 3.82 Ⓒ 17.89 ± 2.77→18.44 ± 5.43 | ||||||
| GSES36) | n/s in Ⓔ, Ⓒ p > 0.05 (0.825) Ⓔ 28.41 ± 4.72→29.83 ± 4.20 Ⓒ 27.14 ± 4.94→29.32 ± 4.42 | ||||||
| Lim (2023) [30] Korea | Dental students (n = 44) Ⓔ n = 21 Ⓒ n = 23 | RCT | VR, Google cardboard | Dental radiography | Ⓔ VR 360° video Ⓒ 2D video | Learning satisfaction | Ⓔ > Ⓒ p = 0.000, Ⓔ 3.98 ± 0.73 Ⓒ 2.53 ± 0.78 |
| Self-efficacy | Ⓔ > Ⓒ p = 0.000, Ⓔ 3.77 ± 0.47 Ⓒ 2.75 ± 0.78 | ||||||
| Martinez (2019) [57] Chile | Medical students (n = 50) Ⓔ n = 25 Ⓒ n = 25 | RCT, double -blinded | VR with Bodyinteract | Case with myocardial infarction | Ⓔ VR (clinical virtual simulator) 20 min + feedback 30 min Ⓒ Case discussion 60 min | OSCE score | n/s in Ⓔ, Ⓒ p = 0.14, Ⓔ 90.1 ± 11.1 Ⓒ 87.4 ± 9.2 |
| Time to EKG (min) | n/s in Ⓔ, Ⓒ p = 0.19, Ⓔ 4.06 ± 1.4 Ⓒ 4.8 ± 2.5 | ||||||
| Time to thrombolysis (min) | n/s in Ⓔ, Ⓒ p = 0.97, Ⓔ 8.4 ± 2.1 Ⓒ 8.6 ± 2.4 | ||||||
| McAlpin (2021) [80] USA | Dental students (n = 58) Ⓔ n = 29 Ⓒ n = 29 | RCT | VR, with HMD (Oculus Quest) | Case of local anesthesia | Ⓔ VR simulation (VR Sim) Ⓒ Plastic mannequin simulation (PM Sim) | Score of knowledge and skills | Ⓔ < Ⓒ p = 0.003, Ⓔ 78.44 ± 13.91 Ⓒ 87.97 ± 8.79 |
| McGrath (2015) [58] USA | EM37) residents (n = 35) Ⓔ n = 18 Ⓒ n = 17 | RCT | VR, Second Life, Headset | Case with acute myocardial infarction | Ⓔ Test by VR examination format Ⓒ Face-to-face oral examination | Critical action scores | n/s in Ⓔ, Ⓒ p > 0.05 |
| Score of competency | n/s in Ⓔ, Ⓒ p > 0.05 | ||||||
| Evaluation after test | More preference, less intimidating in Ⓔ | ||||||
| Moll-Khosrawi (2022) [59] Germany | Medical students (n = 88) Ⓔ n = 46 Ⓒ n = 42 | RCT, double -blind | VR, VIREED | BLS-course (resuscitation training) | Ⓔ VR-BLS + Ⓒ intro 20 min→VR 35 min→SCE38) with Laerdal QCPR mannequin 3 min Ⓒ Web-based BLS lecture 60 min→practice 120 min | No flow time (s) | Ⓔ < Ⓒ p = 0.009, Ⓔ 6.46 ± 3.49 Ⓒ 11.05 ± 14.89 |
| BLS performance penalty score | Ⓔ < Ⓒ p < 0.001, Ⓔ 13.75 ± 9.66 Ⓒ 29.19 ± 16.31 | ||||||
| CSA subjective learning gain | Ⓔ > Ⓒ p < 0.001 in 5 of 11 items | ||||||
| Moro (2021) [60] Austrailia | Medical students (n = 38) Ⓔ n = 19 Ⓒ n = 19 | RCT | AR, HMD (Hololens39) or Galaxy tabS3) | Physiology and anatomy of the brain | Ⓔ AR with HoloLens Ⓒ AR with tablet intro 5 min→ lecture 6 min→AR max 10 min | Knowledge acquisition | n/s in Ⓔ, Ⓒ p > 0.05 Ⓔ 4.6 ± 1.21→11.89 ± 2.16 Ⓒ 3.84 ± 1.54→11.05 ± 3.75 |
| Adverse health effects | ‘Dizziness’ is significantly Ⓔ > Ⓒ p = 0.04, Ⓔ (n = 25) > Ⓒ (n = 0) | ||||||
| Perception of learning | 1 item is significantly Ⓔ > Ⓒ p = 0.02 n/s in other 7 items p > 0.05 | ||||||
| Murbay (2019) [81] HK-China | Dental students (n = 32) Ⓔ n = 16 Ⓒ n = 16 | RCT | VR, Simodont dental trainer | Direct restorations module of operative dentistry course | Ⓔ Training with VR Ⓒ Training w/o VR | Satisfaction by manual evaluation | Ⓔ > Ⓒ p < 0.05, Ⓔ 83.9% (94/112) Ⓒ 59.8% (67/112) |
| Satisfaction by digital evaluation | Ⓔ > Ⓒ p < 0.05, Ⓔ 85.7% (96/112) Ⓒ 55.4% (62/112) | ||||||
| Nielsen (2021) [61] Denmark | Medical students (n = 20) Ⓔ n = 11 Ⓒ n = 9 | RCT | VR, with HMD (VitaSim) | Introductory courses of ultrasound | Ⓔ VR training 15 min 4 sessions with intro 60 min Ⓒ E-learning | US Skills by OSAUS score | Ⓔ > Ⓒ p = 0.01, Ⓔ 142.6 ± 11.8 Ⓒ 125.7 ± 16.2 |
| US Skills hand-eye score | Ⓔ > Ⓒ p = 0.32, Ⓔ 55.4 ± 6.2 Ⓒ 52.3 ± 6.9 | ||||||
| Preference | 91% (n = 11) wanted more VR learning | ||||||
| Noll (2017) [62] Germany | Medical students (n = 44) Ⓔ n = 25 Ⓒ n = 25 | RCT double -blinded | AR with moblie app | Dermatology education | Ⓔ Mobile education with AR 45 min Ⓒ Mobile education w/o AR 45 min | Single choice test | n/s in Ⓔ, Ⓒ p = 0.10 Ⓔ 3.41 ± 1.33→7.00 ± 1.48→6.67 ± 1.62 (2 W) Ⓒ 3.91 ± 1.90→7.77 ± 1.51→6.63 ± 1.30 (2 W) |
| POMS40) (Emotional involvement) | n/s in Ⓔ, Ⓒ p > 0.05 | ||||||
| AttrakDiff-241) | n/s in Ⓔ, Ⓒ p > 0.05 | ||||||
| Padilha (2019) [72] Portugal | Nursing students (n = 42) Ⓔ n = 21 Ⓒ n = 21 | RCT | VR, BodyInteract | Case of ineffective airway clearance and hypoxia | Ⓔ Training with VR simulator Ⓒ Training with low fidelity simulator (lecture 45 min→briefing 5 min →simulation 20 min →debriefing 20 min) | Score of knowledge | After intervention: significant difference p = 0.001 After 2 mon: significant difference p = 0.02 |
| Learning satisfaction | significant difference p < 0.001 | ||||||
| Self-efficacy perceptions | n/s in Ⓔ, Ⓒ p = 0.09 | ||||||
| Penalo (2023) [73] USA | Nursing students (n = 76) Ⓔ n = 34 Ⓒ n = 34 | RCT, Quasi | VR, V-sim | 10 surgical nursing cases | Ⓔ VR with PEARLS debriefing framework42) Ⓒ VR with unstructured briefing43) | COPE-MI-SET44) | n/s in Ⓔ, Ⓒ p > 0.05 |
| VSS45) | Ⓔ > Ⓒ p < 0.05 | ||||||
| Performance score | Ⓔ > Ⓒ p = 0.186 Ⓔ 40.41 ± 30.64 p < 0.001 Ⓒ 31.38 ± 24.74 p < 0.001 | ||||||
| Plotzky (2023) [74] Germany | Nursing students (n = 131) ①n = 43 ②n = 41 ③n = 47 | RCT, mixed | VR, HMD (Oculus Quest 2) | Endotracheal suctioning (ETS) | ① 2D video ② VR-low46) ③ VR-high47) (prebrief 10 min→theory 15 min→ program 20 min→questionnaire 20 min→OSCE 15 min→postbrief and FGI48) 40 min) | Knowledge test | n/s in ①,②,③ p > 0.05 |
| OSCE score | ① > ② p < 0.001 ① > ③ p < 0.001 | ||||||
| ABC-SAT49) | ② > ③>① p = 0006, ② > ① p = 0.004 | ||||||
| VR-HAM50) | ② > ③ in 2 of 5 items p < 0.05 | ||||||
| Ros (2021) [63] France | Medical students (n = 89) Ⓔ n = 45 Ⓒ n = 44 | RCT | VR, IVRA-FPV51) | Lumbar puncture | Ⓔ VR training Ⓒ Direct lecture | Oral assessment score | Ⓔ < Ⓒ p < 0.001, Ⓔ 4.06 ± 0.12 Ⓒ 4.97 ± 0.10 |
| Practical assessment score | n/s in Ⓔ, Ⓒ p = 0.55, Ⓔ 4.60 ± 0.22 Ⓒ 4.77 ± 0.20 | ||||||
| Time to task complete | Ⓔ < Ⓒ p < 0.01, Ⓔ 153.26 ± 11.19 Ⓒ 227.80 ± 34.34 | ||||||
| Saggar (2024) [64] USA | EM52) residents (n = 53) Ⓔ n = 24 Ⓒ n = 29 | RCT | VR, Train XR | Tourniquet application skills for hemorrhage control | Ⓔ VR training 25 min Ⓒ IP (In-Person) training 30 min | Successful placement (%) | n/s in Ⓔ, Ⓒ p = 0.58, Ⓔ 92% Ⓒ 97% |
| Time to placement (s) | n/s in Ⓔ, Ⓒ p = 0.91 Ⓔ 52 ± 25.92 Ⓒ 51 ± 19.35 | ||||||
| Called 9-1-1 | n/s in Ⓔ, Ⓒ p = 0.27, Ⓔ 92% Ⓒ 79% | ||||||
| Scene safety | n/s in Ⓔ, Ⓒ p = 0.2 Ⓔ 96% Ⓒ 83% | ||||||
| Sakowitz (2020) [82] USA | Dental students (n = 30) Ⓔ n = 15 Ⓒ n = 15 | RCT | VR, HMD (Oculus Rift DK2) | Two diagnosis and treatment of orthognathic cases | Ⓔ VR patient simulation 30 min Ⓒ 2D tracing with verbal instruction and demonstration 30 min | MCQ | n/s in Ⓔ, Ⓒ p > 0.05 Ⓔ 7.33 ± 1.37→8.42 ± 1.56→8.17 ± 1.12 (2 W) Ⓒ 7.93 ± 2.12→8.93 ± 1.71→8.13 ± 2.23 (2 W) |
| Written case analysis (1) Recognition response (2) Correct response | 1) n/s in Ⓔ, Ⓒ p > 0.05 2) ① Ⓔ < Ⓒ p = 0.021 ② n.s. in Ⓔ, Ⓒ p > 0.05 | ||||||
| Salameh (2024) [29] Jordan | Nursing students (n = 102) Ⓔ n = 52 Ⓒ n = 50 | RCT | VR, HMD (HTC Vive) | Pediatric physiological measures (arterial pressure, pulse rate) | Ⓔ VR Ⓒ Lecture (3~4 h) | Satisfaction | Ⓔ > Ⓒ p < 0.001 Ⓔ 3.06 ± 0.46→4.28 ± 0.31 p = 0.000 Ⓒ 2.60 ± 0.31→2.71 ± 0.33 p = 0.121 |
| Self-confidence | Ⓔ > Ⓒ p < 0.001 Ⓔ 2.94 ± 0.39→4.27 ± 0.26 p = 0.000 Ⓒ 2.72 ± 0.27→2.91 ± 0.73 p = 0.092 | ||||||
| Performance | Ⓔ > Ⓒ p < 0.001 Ⓔ 5.94 ± 1.46→7.40 ± 1.14 p = 0.000 Ⓒ 4.30 ± 1.43→4.78 ± 1.16 p = 0.068 | ||||||
| Schoeb (2020) [22] Germany | Medical students (n = 164) Ⓔ n = 57 Ⓒ n = 107 | RCT, single -blinded | MR HMD (Hololens) | Bladder catheterization training(male) | Ⓔ MR guidance system Ⓒ Instructions by instructor | Teaching evaluation | Ⓔ > Ⓒ in 4 of 8 items p < 0.01 , n/s in other p > 0.05 |
| Self-evaluation | n/s in Ⓔ, Ⓒ p > 0.05 (1 of 11 items was Ⓔ > Ⓒ p = 0.01) | ||||||
| OSCE score | Ⓔ > Ⓒ p = 0.00, Ⓔ 21.49 ± 2.27 Ⓒ 19.96 ± 2.42 | ||||||
| SUS | 56.6 (Low) | ||||||
| NASA-TLX | Total 24.2 ± 7.3 mental demand 3.58 ± 1.8, physical demand 2.48 ± 1.9, time 4.09 ± 1.8, perceived success 4.30 ± 2.26, overall effort 4.37 ± 2.0, emotional stress 5.39 ± 2.8 | ||||||
| Shah (2022) [65] USA | Medical residents (n = 13) ① n = 6 ② n = 7 | RCT | VR, HMD (Oculus Go and Google cardboard viewer) | Case of treatment for cervical cancer (intracavitary brachytherapy) | ① VR with integrated headset (IHVR) ② VR with cardboard viewer (CVVR) | Overall satisfaction | pre < post in ①,② p < 0.05 |
| Perceived assembling skill | pre < post in ①,② p < 0.05 | ||||||
| Perceived insertion skill | pre < post in ① p > 0.05 n/s in ② p < 0.05 | ||||||
| Comfort with independently performing | n/s in ① p > 0.05 pre < post in ② p < 0.05 | ||||||
| Evaluation of VR technology | n/s in Ⓔ, Ⓒ p > 0.05 (enjoyable, engaging, recommendable) | ||||||
| Shujuan (2022) [75] China | Nursing students (n = 101) Ⓔ n = 52 Ⓒ n = 49 | RCT | VR, HMD (HTC Vive) | Disaster preparedness | Ⓔ VR simulation (12 scenarios) Ⓒ Lecture (24 times) + mannequin simulation (4 times) | DPQ53) | Ⓔ > Ⓒ p = 0.001 Ⓔ 93.6 ± 7.8→148.0 ± 12.4 Ⓒ 93.8 ± 9.4→141.3 ± 8.7 |
| Confidence | Ⓔ > Ⓒ p = 0.008 Ⓔ 4.0 ± 1.3→6.4 ± 1.2 Ⓒ 3.9 ± 1.4→5.5 ± 1.5 | ||||||
| Performance | Ⓔ > Ⓒ p = 0.045 Ⓔ 14.8 ± 4.5→27.5 ± 6.5 Ⓒ 14.9 ± 3.6→25.2 ± 4.7 | ||||||
| Singleton (2022) [76] UK | Nursing students (n = 171) Ⓔ n = 88 Ⓒ n = 83 | RCT | VR | Case of type-2 diabetes patient nursing | Ⓔ VR with pre-briefing and debriefing Ⓒ Traditional lecture | Score of knowledge | Ⓔ > Ⓒ p < 0.001 |
| Weeks (2021) [66] USA | Medical students (n = 30) Ⓔ n = 15 Ⓒ n = 15 | RCT | AR, with HMD (Hololens) and Dell laptop | Head and neck anatomy | Ⓔ AR simulation 15–30 min Ⓒ 2D screen 15–30 min intro 15 min, total 60 min | Test score | Ⓔ > Ⓒ p = 0.022 Ⓔ 2.93 ± 0.96→4.73 p < 0.001 Ⓒ 2.86 ± 1.19→4.00 p = 0.021 |
| Perceived understanding | n/s in Ⓔ, Ⓒ p = 0.62 Ⓔ 1.07 ± 0.70→3.07 ± 0.80 p < 0.001 Ⓒ 0.79 ± 0.70→3.21 ± 0.80 p < 0.001 | ||||||
| Wu (2022) [77] Taiwan | Third-year nursing students (n = 105) Ⓔ n = 53 Ⓒ n = 52 | RCT (Quasi) | VR, with HMD (Oculus Rift S) | Pediatric seizure management | Ⓔ VR learning (intro 20 min, tutorial = VR session 130 min, debriefing 30 min) Ⓒ Direct lecture (90 min) | SMKT54) | Ⓔ > Ⓒ p < 0.01 Ⓔ 5.74 ± 1.76→8.32 ± 1.25 Ⓒ 5.13 ± 1.73→6.75 ± 1.87 |
| PSM-VRAQ55) | 1) Perceived usefulness: 3.26 2) Perceived ease of use: 3.09 3) Attitude toward use: 3.26 4) Willingness to use: 3.32 | ||||||
| VRSQ56) | 18.17 (n = 35), 18 students had no sickness None stopped VRS due to physical symptoms | ||||||
| Yildiz (2022) [78] Turkey | Nursing students (n = 56) Ⓔ n = 29 Ⓒ n = 27 | RCT | VR, with Medsim program | Intravenous catheterization | Ⓔ VR learning (15–17 min) Ⓒ Intravenous injection model | Checklist score57) | Ⓔ > Ⓒ p = 0.001 Ⓔ 88.94 ± 9.22 Ⓒ 65.13 ± 11.12 |
| Bondy rating scale | n/s in Ⓔ p > 0.05, significant in Ⓒ p < 0.05 | ||||||
| Performance results | 6 of 7 items Ⓔ > Ⓒ | ||||||
| Zackoff (2020) [67] USA | Medical students (n = 168) Ⓔ n = 78 Ⓒ n = 90 | RCT double-blinded | VR, with HMD (Oculus Rift) | 3 cases of infants58) | Ⓔ Ⓒ + VR instruction 30 min Ⓒ Verbal instruction + high-fidelity mannequin simulation 60 min | Objective assessment of competency | Significant difference in Ⓔ-Ⓒ in 1), 2), and 3). 1) Consideration/interpretation of mental status p < 0.01 2) Assignment of the appropriate respiratory status assessment p < 0.01 3) Recognition of a need for escalation of care p = 0.0004 |
Ⓔ = experimental group, Ⓒ = control group. 1) Cardiology, pulmonology, gastroenterology, neurology, 2) MCQ: multiple-choice questions, 3) IVC-PPSF: intravenous catheter placement procedure steps form, 4) SCLS: Student Satisfaction and Self-Confidence in Learning Scale, e) n/s: no significant difference, 5) HMD: head-mounted display, 6) Paas-CLS: Paas Cognitive Load Scale, 7) NASA-TLX: National Aeronautics and Space Administration Task Load Index, 8) HRV: heart rate variability, 9) DOPS: direct observation of procedural skills, 10) Mini-CEX: mini-clinical evaluation exercise, 11) CLC: cognitive load component, 12) vSim®: simulation for nursing co-developed by Laedral and Wolters Kluwer Health from Lippincott, 13) NASC-CDM: nursing anxiety and self-confidence with clinical decision making, 14) SIM to CARE Dente®: SD001, Vreeland, The Netherlands, 15) VRHS: virtual reality haptic simulation, 16) CSE: conventional simulation environment, 17) postpartum hemorrhage emergency management, insertion of postpartum ballon, 18) PPT: PowerPoint presentation, 19) two patients with pneumonia and a surgical case with open reduction internal fixation surgery, brain surgery, 20) PBL: problem-based learning, 21) CCQ: clinical competence questionnaire, 22) IAPCC-SV: The Inventory For Assessing The Process Of Cultural Competence Among Healthcare Professionals, 23) PE: physical examination, 24) SP: standardized patient, 25) NPE: neurologic physical exam, 26) CT: computed tomography, 27) BLS: basic life support of resuscitation training, 28) CSA: comparative self-assessment, 29) SUS: system usability scale, 30) ORama VR from Swiss, Geneva, 31) THA: total hip arthroplasty, 32) accuracy of skill: mean difference between predefined cup inclination (60°) and stem anteversion (20°) compared to the actual implanted values in sawbones between VR and control groups, 33) IVPS: immersive virtual patient simulation, 34) RBTKQ-O: routine blood transfusion knowledge questionnaire, 35) SSCS: student satisfaction and self-confidence, 36) GSES: general self-efficacy scale, 37) EM: emergency medicine, 38) SCE: structured clinical examination, 39) Microsoft Hololens or a mobile handheld tablet device, Samsung Galaxy Tab S3 (Samsung Electronics, Seoul, South Korea) tablet with an online Qualtrics XM (Qualtrics XM), 40) POMS: profile of mood states, 41) AttrakDiff-2: including PQ Pragmaic Quality), HQ-I (Hedonic Quality-Identification), HQ-S (HQ-I: Hedonic Quality-Simulation), ATT (Attractiveness), 42) VR with PEARLS debriefing framework: a) structured pre-briefing (20 min), b) structured debriefing (30 min), and c) second structured debriefing (20 min), 43) VR with unstructured briefing: a) pre-simulation discussion (5 min), b) post-simulation discussion (10 min), and c) second post-simulation discussion (5 min), 44) COPE-MI-SET: care of patients experiencing a myocardial infarction self-efficacy tool, 45) VSS: virtual simulation survey, 46) VR-low with basic technology, 47) VR-high with more experimental technological features, 48) FGI: focus group interview, 49) ABC-SAT: affective behavioral cognitive satisfaction questionnaire, 50) VR-HAM: virtual reality hardware acceptance model, 51) IVRA-FPV: immersive VR application, 52) EM: emergency medicine, 53) DPQ: disaster preparedness questionnaire, 54) SMKT: seizure management knowledge test, 55) PSM-VRAQ: pediatric seizure management virtual reality acceptance questionnaire, 56) VRSQ: virtual reality sickness questionnaire, 57) intravenous catheter application and fluid delivery skills, 58) infant with no distress, respiratory distress, or impending respiratory failure.
References
- Gao, S.; He, T.; Zhang, Z.; Ao, H.; Jiang, H.; Lee, C. A motion capturing and energy harvesting hybridized lower-limb system for rehabilitation and sports applications. Adv. Sci. 2021, 8, e2101834. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Sanchez, M.A.; Palos-Sanchez, P.R.; Folgado-Fernandez, J.A. Systematic Literature Review and Bibliometric Analysis on Virtual Reality and Education. Educ. Inf. Technol. 2022, 28, 155–192. [Google Scholar] [CrossRef] [PubMed]
- Elston, P.; Canale, G.P.; Ail, G.; Fisher, N.; Mahendran, M. Twelve tips for teaching in virtual reality. Med. Teach. 2024, 46, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Walls, R.; Nageswaran, P.; Cowell, A.; Sehgal, T.; White, T.; McVeigh, J.; Staykov, S.; Basett, P.; Mitelpunkt, D.; Sam, A.H. Virtual reality as an engaging and enjoyable method for delivering emergency clinical simulation training: A prospective, interventional study of medical undergraduates. BMC Med. 2024, 22, 222. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.P.; Allman, S.A. Blending virtual reality with traditional approaches to encourage engagement with core chemistry concepts relevant to an undergraduate pharmacy curriculum. Pharm. Educ. 2020, 20, 365–374. [Google Scholar] [CrossRef]
- Han, E.R.; Yeo, S.; Kim, M.J.; Lee, Y.H.; Park, K.H.; Roh, H. Medical education trends for future physicians in the era of advanced technology and artificial intelligence: An integrative review. BMC Med. Educ. 2019, 19, 460. [Google Scholar] [CrossRef] [PubMed]
- Jensen, L.X.; Buhl, A.; Hussain, S.; Karan, A.; Konradsen, F.; Bearman, M. Digital education for health professionals in India: A scoping review of the research. BMC Med. Educ. 2023, 23, 561. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Vimalesvaran, S.; Wang, J.K.; Lim, K.B.; Mogali, S.R.; Car, L.T. Virtual reality in medical students’ education: Scoping review. JMIR Med. Educ. 2022, 8, e34860. [Google Scholar] [CrossRef] [PubMed]
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, mixed, and virtual reality-based head-mounted devices for medical education: Systematic review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.Q.; Leng, Y.F.; Ge, J.F.; Wang, D.W.; Li, C.; Chen, B.; Sun, Z.L. Effectiveness of virtual reality in nursing education: Meta-analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef]
- Miltykh, I.; Kafarov, E.S.; Covantsev, S.; Dadashev, A.S.; Skarlis, A.A.; Zenin, O.K. A new dimension in medical education: Virtual reality in anatomy during COVID-19 pandemic. Clin. Anat. 2023, 36, 24098. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.K.; Kim, M.Y. Enhancing nursing competency through virtual reality simulation among nursing students: A systematic review and meta-analysis. Front. Med. 2024, 11, 1351300. [Google Scholar] [CrossRef] [PubMed]
- Camargo-Vargas, D.; Callejas-Cuervo, M.; Mazzoleni, S. Brain-computer interfaces systems for upper and lower limb rehabilitation: A systematic review. Sensors 2021, 21, 4312. [Google Scholar] [CrossRef] [PubMed]
- Huai, P.; Li, Y.; Wang, X.; Zhang, L.; Liu, N.; Yang, H. The effectiveness of virtual reality technology in student nurse education: A systematic review and meta-analysis. Nurse Educ. Today 2024, 138, 106189. [Google Scholar] [CrossRef] [PubMed]
- Zagury-Orly, I.; Solinski, M.A.; Nguyen, L.H.; Young, M.; Drozdowski, V.; Bain, P.A.; Gantwerker, E.A. What is the current state of extended reality use in otolaryngology training? A scoping review. Laryngoscope 2023, 133, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Plotzky, C.; Lindwedel, U.; Sorber, M.; Loessl, B.; König, P.; Kunze, C.; Kugler, C.; Meng, M. Virtual reality simulations in nurse education: A systematic mapping review. Nurse Educ. Today 2021, 101, 104868. [Google Scholar] [CrossRef] [PubMed]
- Shorey, S.; Ng, E.D. The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse Educ. Today 2021, 98, 104662. [Google Scholar] [CrossRef] [PubMed]
- Treat, C.; Maniker, R.; Kessler, D. 182 All clear! Virtual reality defibrillator training for medical students is feasible, liked, and improves perceived knowledge, comfort, and skills. Ann. Emerg. Med. 2022, 80, S83. [Google Scholar] [CrossRef]
- Jeong, Y.; Lee, H.; Han, J.W. Development and evaluation of virtual reality simulation education based on coronavirus disease 2019 scenario for nursing students: A pilot study. Nurs. Open 2022, 9, 1066–1076. [Google Scholar] [CrossRef] [PubMed]
- Chao, Y.P.; Chuang, H.H.; Hsin, L.J.; Kang, C.J.; Fang, T.J.; Li, H.Y.; Lee, L.A. Using a 360 virtual reality or 2D video to learn history taking and physical examination skills for undergraduate medical students: Pilot randomized controlled trial. JMIR Serious Games 2021, 9, e13124. [Google Scholar] [CrossRef] [PubMed]
- Chao, Y.P.; Kang, C.J.; Chuang, H.H.; Hsieh, M.J.; Chang, Y.C.; Kuo, T.B.J.; Yang, C.C.H.; Huang, C.G.; Fang, T.J.; Li, H.Y.; et al. Comparison of the effect of 360 versus two-dimensional virtual reality video on history taking and physical examination skills learning among undergraduate medical students: A randomized controlled trial. Virtual Real. 2023, 27, 637–650. [Google Scholar] [CrossRef] [PubMed]
- Schoeb, D.S.; Schwarz, J.; Hein, S.; Schlager, D.; Pohlmann, P.F.; Frankenschmidt, A.; Miernik, A. Mixed reality for teaching catheter placement to medical students: A randomized single-blinded, prospective trial. BMC Med. Educ. 2020, 20, 510. [Google Scholar] [CrossRef] [PubMed]
- Ammanuel, S.; Brown, I.; Uribe, J.; Rehani, B. Creating 3D models from radiologic images for virtual reality medical education modules. J. Med. Syst. 2019, 43, 166. [Google Scholar] [CrossRef] [PubMed]
- Klimova, A.; Bilyatdinova, A.; Karsakov, A. Existing teaching practices in augmented reality. Procedia Comput. Sci. 2018, 136, 5–15. [Google Scholar] [CrossRef]
- Piromchai, P.; Avery, A.; Laopaiboon, M.; Kennedy, G.; O’Leary, S. Virtual reality training for improving the skills needed for performing surgery of the ear, nose or throat. Cochrane Database Syst. Rev. 2015, 9, CD010198. [Google Scholar] [CrossRef] [PubMed]
- Cobbett, S.; Snelgrove-Clarke, E. Virtual versus face-to-face clinical simulation in relation to student knowledge, anxiety, and self-confidence in maternal-newborn nursing: A randomized controlled trial. Nurse Educ. Today 2016, 45, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, K.; Dillon, G.; McEvoy, A.; Kane, D.; Higgins, S.; Mangina, E.; McAuliffe, F.M. The virtual reality classroom: A randomized control trial of medical student knowledge of postpartum hemorrhage emergency management. Front. Med. 2024, 11, 1371075. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Tsang, V.W.Y.; Chan, M.M.K.; O’Connor, S.; Lokmic-Tomkins, Z.; Ye, F.; Kwok, J.Y.Y.; Ho, M.H. Virtual reality simulation-enhanced blood transfusion education focusing on undergraduate nursing students: A randomised controlled trial. Nurse Educ. Today 2023, 129, 105903. [Google Scholar] [CrossRef] [PubMed]
- Salameh, A.K.B.; Malak, M.Z.; El-Qirem, F.A.; Alhussami, M.; El-hneiti, M. Effect of virtual reality simulation as a teaching strategy on nursing students’ satisfaction, self-confidence, performance, and physiological measures in Jordan. Teach. Learn. Nurs. 2024, 19, e235–e241. [Google Scholar] [CrossRef]
- Lim, J.E.; Gu, J.Y.; Bae, J.H.; Lee, J.G. Comparative study of 360° virtual reality and traditional two-dimensional video in nonface-to-face dental radiology classes: Focusing on learning satisfaction and self-efficacy. BMC Med. Educ. 2023, 23, 855. [Google Scholar] [CrossRef]
- Rosen, K.R. The history of medical simulation. J. Crit. Care 2008, 23, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Watterson, L.; Flanagan, B.; Donovan, B.; Robinson, B. Anaesthetic simulators: Training for the broader health-care profession. Aust. N. Z. J. Surg. 2000, 70, 735–737. [Google Scholar] [CrossRef] [PubMed]
- Ellis, C.; Hughes, G. Use of human patient simulation to teach emergency medicine trainees advanced airway skills. J. Accid. Emerg. Med. 1999, 16, 395–399. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jensen, L.; Konradsen, F. A review of the use of virtual reality head-mounted displays in education and training. Educ. Inf. Technol. 2018, 23, 1515–1529. [Google Scholar] [CrossRef]
- Hwang, G.J.; Chang, C.Y.; Ogata, H. The effectiveness of the virtual patient-based social learning approach in undergraduate nursing education: A quasi-experimental study. Nurse Educ. Today 2022, 108, 105164. [Google Scholar] [CrossRef]
- Sarvan, S.; Efe, E. The effect of neonatal resuscitation training based on a serious game simulation method on nursing students’ knowledge, skills, satisfaction and self-confidence levels: A randomized controlled trial. Nurse Educ. Today 2022, 111, 105298. [Google Scholar] [CrossRef]
- Bryant, R.; Miller, C.L.; Henderson, D. Virtual clinical simulations in an online advanced health appraisal course. Clin. Simul. Nurs. 2015, 11, 437–444. [Google Scholar] [CrossRef]
- Farra, S.L.; Smith, S.; Gillespie, G.L.; Nicely, S.; Ulrich, D.L.; Hodgson, E.; French, D. Decontamination training: With and without virtual reality simulation. Adv. Emerg. Nurs. J. 2015, 37, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Ng, G.W.; Ye, S.S. Design and evaluation for immersive virtual reality learning environment: A systematic literature review. Sustainability 2023, 15, 1964. [Google Scholar] [CrossRef]
- Qiao, J.; Huang, C.R.; Liu, Q.; Li, S.Y.; Xu, J.; Li, L.; Redding, S.R.; Ouyang, Y.Q. Effectiveness of non-immersive virtual reality simulation in learning knowledge and skills for nursing students: Meta-analysis. Clin. Simul. Nurs. 2023, 76, 26–38. [Google Scholar] [CrossRef]
- Kim, H.-Y.; Kim, E.-Y. Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 3895. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLOS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Amir-Behghadami, M.; Janati, A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg. Med. J. 2020, 37, 387. [Google Scholar] [CrossRef] [PubMed]
- Bloom, B.S. Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook I: Cognitive Domain; David McKay Company: New York, NY, USA, 1956. [Google Scholar]
- Abreu, J.M.; Guimarães, B.; Castelo-Branco, M. The role of virtual interactive simulators in medical education: Exploring their integration as an assessment methodology in clinical years. Educ. Med. 2021, 22, 325–329. [Google Scholar] [CrossRef]
- Bray, L.; Spencer, S.; Pearson, E.; Meznikova, K.; Hepburn, D. Assessing the impact of immersion on learning in medical students: A pilot study comparing two-dimensional and three-dimensional virtual simulation. Simul. Gaming 2023, 54, 576–592. [Google Scholar] [CrossRef]
- Ekstrand, C.; Jamal, A.; Nguyen, R.; Kudryk, A.; Mann, J.; Mendez, I. Immersive and interactive virtual reality to improve learning and retention of neuroanatomy in medical students: A randomized controlled study. CMAJ Open 2018, 6, E103–E109. [Google Scholar] [CrossRef] [PubMed]
- Gan, W.; Mok, T.N.; Chen, J.; She, G.; Zha, Z.; Wang, H.; Li, H.; Li, J.; Zheng, X. Researching the application of virtual reality in medical education: One-year follow-up of a randomized trial. BMC Med. Educ. 2023, 23, 3. [Google Scholar] [CrossRef]
- Han, S.G.; Kim, Y.D.; Kong, T.Y.; Cho, J. Virtual reality-based neurological examination teaching tool(VRNET) versus standardized patient in teaching neurological examinations for the medical students: A randomized, single-blind study. BMC Med. Educ. 2021, 21, 493. [Google Scholar] [CrossRef] [PubMed]
- Imai, T.; Tanaka, Y.; Hatanaka, Y.; Suetsugu, T.; Sato, Y.; Matsuhashi, N.; Tsunekawa, K.; Saiki, T.; Yoshida, K. Incorporation of virtual reality in the clinical training of medical students studying esophageal and mediastinal anatomy and surgery. Surg. Today 2022, 52, 1212–1217. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, N.; Kandasamy, R.; O, J.; R, B.; Jyothish, K. Virtual reality simulation for the acquisition and retention of electrocardiogram interpretation skills: A randomized controlled trial among undergraduate medical students. Cureus 2024, 16, e3958. [Google Scholar] [CrossRef] [PubMed]
- Issleib, M.; Kromer, A.; Pinnschmidt, H.O.; Süss-Havemann, C.; Kubitz, J.C. Virtual reality as a teaching method for resuscitation training in undergraduate first year medical students: A randomized controlled trial. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 27. [Google Scholar] [CrossRef] [PubMed]
- Kenanidis, E.; Boutos, P.; Voulgaris, G.; Zgouridou, A.; Gkoura, E.; Gamie, Z.; Papagiannakis, G.; Tsiridis, E. Effectiveness of virtual reality compared to video training on acetabular cup and femoral stem implantation accuracy in total hip arthroplasty among medical students: A randomised controlled trial. Int. Orthop. 2024, 48, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Law, A.K.K.; Hung, K.K.C.; James, K.S.; Kelly, A.M.; Graham, C.A. Virtual patient simulation in undergraduate emergency medicine education during COVID-19: Randomized controlled trial. Hong Kong J. Emerg. Med. 2023, 30, 439–446. [Google Scholar] [CrossRef]
- Lebdai, S.; Mauget, M.; Cousseau, P.; Granry, J.C.; Martin, L. Improving academic performance in medical students using immersive virtual patient simulation: A randomized controlled trial. J. Surg. Educ. 2021, 78, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.T.; Soto, J.P.; Valenzuela, D.; González, N.; Corsi, J.; Sepúlveda, P. Virtual clinical simulation for training amongst undergraduate medical students: A pilot randomised trial (VIRTUE-pilot). Cureus 2023, 15, e47527. [Google Scholar] [CrossRef] [PubMed]
- McGrath, J.; Kman, N.; Danforth, D.; Bahner, D.P.; Khandelwal, S.; Martin, D.R.; Nagel, R.; Verbeck, N.; Way, D.P.; Nelson, R. Virtual alternative to the oral examination for emergency medicine residents. West. J. Emerg. Med. 2015, 16, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Moll-Khosrawi, P.; Falb, A.; Pinnschmidt, H.; Zöllner, C.; Issleib, M. Virtual reality as a teaching method for resuscitation training in undergraduate first year medical students during COVID-19 pandemic: A randomised controlled trial. BMC Med. Educ. 2022, 22, 483. [Google Scholar] [CrossRef]
- Moro, C.; Phelps, C.; Redmond, P.; Stromberga, Z. HoloLens and mobile augmented reality in medical and health science education: A randomised controlled trial. Brit. J. Educ. Tech. 2021, 52, 680–694. [Google Scholar] [CrossRef]
- Nielsen, M.R.; Kristensen, E.Q.; Jensen, R.O.; Mollerup, A.M.; Pfeiffer, T.; Graumann, O. Clinical ultrasound education for medical students: Virtual reality versus e-learning, a randomized controlled pilot trial. Ultrasound Q. 2021, 37, 292–296. [Google Scholar] [CrossRef]
- Noll, C.; von Jan, U.; Raap, U.; Albrecht, U.V. Mobile augmented reality as a feature for self-oriented, blended learning in medicine: Randomized controlled trial. JMIR MHealth UHealth 2017, 5, e139. [Google Scholar] [CrossRef] [PubMed]
- Ros, M.; Neuwirth, L.S.; Ng, S.; Debien, B.; Molinari, N.; Gatto, F.; Lonjon, N. The effects of an immersive virtual reality application in first person point-of-view (IVRA-FPV) on the learning and generalized performance of a lumbar puncture medical procedure. Educ. Technol. Res. Dev. 2021, 69, 1529–1556. [Google Scholar] [CrossRef]
- Saggar, V.; O’Donnell, P.; Moss, H.; Yoon, A.; Lutz, C.; Restivo, A.; Ahmed, O.; Guha, D.; Jafri, F.; Singh, M. Effectiveness of a virtual reality trainer for retention of tourniquet application skills for hemorrhage control among emergency medicine residents. AEM Educ. Train. 2024, 8, e10986. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.K.; Taunk, N.K.; Maxwell, R.; Wang, X.; Hubley, E.; Anamalayil, S.; Li, T. Comparison of virtual reality platforms to enhance medical education focusing on procedures. Front. Virtual Real. 2022, 3, 1000035. [Google Scholar] [CrossRef]
- Weeks, J.K.; Pakpoor, J.; Park, B.J.; Robinson, N.J.; Rubinstein, N.A.; Prouty, S.M.; Nachiappan, A.C. Harnessing augmented reality and CT to teach first-year medical students head and neck anatomy. Acad. Radiol. 2021, 28, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Zackoff, M.W.; Real, F.J.; Sahay, R.D.; Fei, L.; Guiot, A.; Lehmann, C.; Tegtmeyer, K.; Klein, M. Impact of an immersive virtual reality curriculum on medical students’ clinical assessment of infants with respiratory distress. Pediatr. Crit. Care Med. 2020, 21, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Avci, M.; Kilic, S.P. The effect of augmented reality applications on intravenous catheter placement skill in nursing students: A randomized controlled study. Clin. Simul. Nurs. 2024, 90, 101524. [Google Scholar] [CrossRef]
- Babaita, A.O.; Kako, M.; Teramoto, C.; Okamoto, M.; Hayashi, Y.; Ohshimo, S.; Sadamori, T.; Hattori, M.; Moriyama, M. Face-to-face versus 360 VR video: A comparative study of two teaching methods in nursing education. BMC Nurs. 2024, 23, 199. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.H.; Tai, H.C.; Chen, S.L. The effects of introducing virtual reality communication simulation in students’ learning in a fundamentals of nursing practicum: A pragmatic randomized control trials. Nurse Educ. Pract. 2024, 74, 103837. [Google Scholar] [CrossRef] [PubMed]
- Fung, J.T.C.; Chan, S.L.; Takemura, N.; Chiu, H.Y.; Huang, H.C.; Lee, J.E.; Preechawong, S.; Hyun, M.Y.; Sun, M.; Xia, W.; et al. Virtual simulation and problem-based learning enhance perceived clinical and cultural competence of nursing students in Asia: A randomized controlled cross-over study. Nurse Educ. Today 2023, 123, 105721. [Google Scholar] [CrossRef] [PubMed]
- Padilha, J.M.; Machado, P.P.; Ribeiro, A.L.; Ramos, J.L. Clinical virtual simulation in nursing education. Clin. Simul. Nurs. 2018, 15, 13–18. [Google Scholar] [CrossRef]
- Penalo, L.M. Effect of the Virtual simulation prebriefing-debriefing educational strategy on nursing students’ self-efficacy and performance concerning the care of patients experiencing a myocardial infarction: A quasi-experimental study. Clin. Simul. Nurs. 2023, 82, 101431. [Google Scholar] [CrossRef]
- Plotzky, C.; Loessl, B.; Kuhnert, B.; Friedrich, N.; Kugler, C.; König, P.; Kunze, C. My hands are running away—Learning a complex nursing skill via virtual reality simulation: A randomised mixed methods study. BMC Nurs. 2023, 22, 222. [Google Scholar] [CrossRef] [PubMed]
- Shujuan, L.; Mawpin, T.; Meichan, C.; Weijun, X.; Jing, W.; Biru, L. The use of virtual reality to improve disaster preparedness among nursing students: A randomized study. J. Nurs. Educ. 2022, 61, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Singleton, H.; James, J.; Falconer, L.; Holley, D.; Priego-Hernandez, J.; Beavis, J.; Penfold, S. Effect of non-immersive virtual reality simulation on type 2 diabetes education focusing on nursing students: A randomised controlled trial. Clin. Simul. Nurs. 2022, 66, 50–57. [Google Scholar] [CrossRef]
- Wu, M.L.; Chao, L.F.; Xiao, X. A pediatric seizure management virtual reality simulator for nursing students: A quasi-experimental design. Nurse Educ. Today 2022, 119, 105550. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, H.; Demiray, A. Virtual reality in nursing education 3D intravenous catheterization e-learning: A randomized controlled trial. Contemp. Nurse 2022, 58, 125–137. [Google Scholar] [CrossRef]
- Daud, A.; Matoug-Elwerfelli, M.; Daas, H.; Zahra, D.; Ali, K. Enhancing learning experiences in pre-clinical restorative dentistry: The impact of virtual reality haptic simulators. BMC Med. Educ. 2023, 23, 948. [Google Scholar] [CrossRef] [PubMed]
- McAlpin, E.; Levine, M.; Brenner, C.; Opazo, C.; Bathini, S.; Choi, S.J.V.; Louisville, M.; Grandhi, U. Evaluating the effectiveness of a virtual reality simulation for preclinical local anaesthesia dental education. Eur. J. Dent. Educ. 2022, Online ahead of print. [Google Scholar] [CrossRef]
- Murbay, S.; Neelakantan, P.; Chang, J.W.W.; Yeung, S. Evaluation of the introduction of a dental virtual simulator on the performance of undergraduate dental students in the preclinical operative dentistry course. Eur. J. Dent. Educ. 2020, 24, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Sakowitz, S.M.; Inglehart, M.R.; Ramaswamy, V.; Edwards, S.; Shoukri, B.; Sachs, S.; Kim-Berman, H. A comparison of two-dimensional prediction tracing and a virtual reality patient methods for diagnosis and treatment planning of orthognathic cases in dental students: A randomized preliminary study. Virtual Real. 2020, 24, 399–409. [Google Scholar] [CrossRef]
- Violante, M.G.; Vezzetti, E. Virtual interactive e-learning application: An evaluation of the student satisfaction. Comput. Appl. Eng. Educ. 2015, 23, 72–91. [Google Scholar] [CrossRef]
- Azuma, R.T. A survey of augmented reality. Presence-Teleop VIRT 1997, 6, 355–385. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Tudor Car, L.T.; Carlstedt-Duke, J.; Car, J.; Zary, N. Virtual patient simulations in health professions education: Systematic review and meta-analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef] [PubMed]
- Fealy, S.; Jones, D.; Hutton, A.; Graham, K.; McNeill, L.; Sweet, L.; Hazelton, M. The integration of immersive virtual reality in tertiary nursing and midwifery education: A scoping review. Nurse Educ. Today 2019, 79, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Hanson, J.; Andersen, P.; Dunn, P.K. Effectiveness of three-dimensional visualization on undergraduate nursing and midwifery students’ knowledge and achievement in pharmacology: A mixed methods study. Nurse Educ. Today 2019, 81, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Liaw, S.Y.; Tan, K.K.; Wu, L.T.; Tan, S.C.; Choo, H.; Yap, J.; Lim, S.M.; Wong, L.; Ignacio, J. Finding the right blend of technologically enhanced learning environments: Randomized controlled study of the effect of instructional sequences on interprofessional learning. J. Med. Internet Res. 2019, 21, e12537. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.C.M.; Hamdy, H. Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83: AMEE Guide Number 83. Med. Teach. 2013, 35, e1561–e1572. [Google Scholar] [CrossRef]
- Gutiérrez, F.; Pierce, J.; Vergara, V.M.; Coulter, R.; Saland, L.; Caudell, T.P.; Goldsmith, T.E.; Alverson, D.C. The effect of degree of immersion upon learning performance in virtual reality simulations for medical education. Stud. Health Technol. Inform. 2007, 125, 155–160. [Google Scholar] [PubMed]
- Checa, D.; Miguel-Alonso, I.; Bustillo, A. Immersive virtual reality computer-assembly serious game to enhance autonomous learning. Virtual Real. 2021, 27, 3301–3318. [Google Scholar] [CrossRef] [PubMed]
- Zard, S.G.; Juanes, J.A.; García Peñalvo, F.J.; Estella, J.M.G.; Ledesma, M.J.S.; Ruisoto, P. Virtual reality as an educational and training tool for medicine. J. Med. Syst. 2018, 42, 50. [Google Scholar] [CrossRef]
- Strandbygaard, J.; Bjerrum, F.; Maagaard, M.; Winkel, P.; Larsen, C.R.; Ringsted, C.; Gluud, C.; Grantcharov, T.; Ottesen, B.; Sorensen, J.L. Instructor feedback versus no instructor feedback on performance in a laparoscopic virtual reality simulator: A randomized trial. Ann. Surg. 2013, 257, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Taunk, N.K.; Shah, N.K.; Hubley, E.; Anamalayil, S.; Trotter, J.W.; Li, T. Virtual reality-based simulation improves gynecologic brachytherapy proficiency, engagement, and trainee self-confidence. Brachytherapy 2021, 20, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Antonietti, A.; Rasi, C.; Imperio, E.; Sacco, M. The representation of virtual reality in education. Educ. Inf. Technol. 2000, 5, 317–327. [Google Scholar] [CrossRef]
- Ai-Lim Lee, E.A.L.; Wong, K.W.; Fung, C.C. How does desktop virtual reality enhance learning outcomes? A structural equation modeling approach. Comput. Educ. 2010, 55, 1424–1442. [Google Scholar] [CrossRef]
- Norman, G.R.; Schmidt, H.G. The psychological basis of problem-based learning: A review of the evidence. Acad. Med. 1992, 67, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Euliano, T.Y. Small group teaching: Clinical correlation with a human patient simulator. Adv. Physiol. Educ. 2001, 25, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Meo, S.A. Basic steps in establishing effective small group teaching sessions in medical schools. Pak. J. Med. Sci. 2013, 29, 1071–1076. [Google Scholar] [CrossRef] [PubMed]
- Sewell, J.L.; Maggio, L.A.; Ten Cate, O.; van Gog, T.; Young, J.Q.; O’Sullivan, P.S. Cognitive load theory for training health professionals in the workplace: A BEME review of studies among diverse professions: BEME Guide No. 53. Med. Teach. 2019, 41, 256–270. [Google Scholar] [CrossRef]
- Blackburn, S.C.; Griffin, S.J. Role of simulation in training the next generation of endoscopists. World J. Gastrointest. Endosc. 2014, 16, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Van Herzeele, I.; Aggarwal, R.; Neequaye, S.; Darzi, A.; Vermassen, F.; Cheshire, N.J. Cognitive training improves clinically relevant outcomes during simulated endovascular procedures. J. Vasc. Surg. 2008, 48, 1223–1230. [Google Scholar] [CrossRef] [PubMed]
- Graafland, M.; Schraagen, J.M.; Schijven, M.P. Systematic review of serious games for medical education and surgical skills training. Br. J. Surg. 2012, 99, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.; Jones, D.; Walker, R. Consideration of using virtual reality for teaching neonatal resuscitation to midwifery students. Nurse Educ. Pract. 2018, 31, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Nielson, B.; Harder, N. Causes of student anxiety during simulation: What the literature says. Clin. Simul. Nurs. 2013, 2013, e507–e512. [Google Scholar] [CrossRef]
- Sankaranarayanan, G.; Wooley, L.; Hogg, D.; Dorozhkin, D.; Olasky, J.; Chauhan, S.; Fleshman, J.W.; De, S.; Scott, D.; Jones, D.B. Immersive virtual reality-based training improves response in a simulated operating room fire scenario. Surg. Endosc. 2018, 32, 3439–3449. [Google Scholar] [CrossRef] [PubMed]
- Cant, R.P.; Cooper, S.J. Simulation in the internet age: The place of web-based simulation in nursing education. An integrative review. Nurse Educ. Today 2014, 34, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).