Wearables and Their Potential to Transform Health Management: A Step towards Sustainable Development Goal 3
Abstract
1. Introduction
2. Literature Review
2.1. Wearables for Health and Well-Being Management
2.2. Health and Well-Being as SDG: Significance and Progress
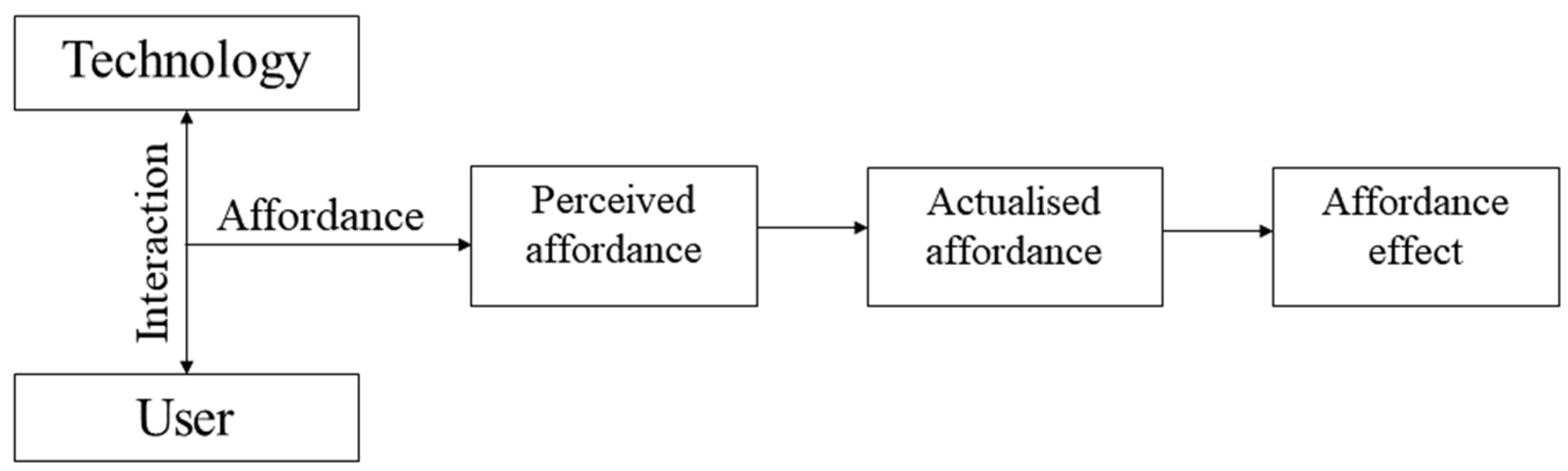
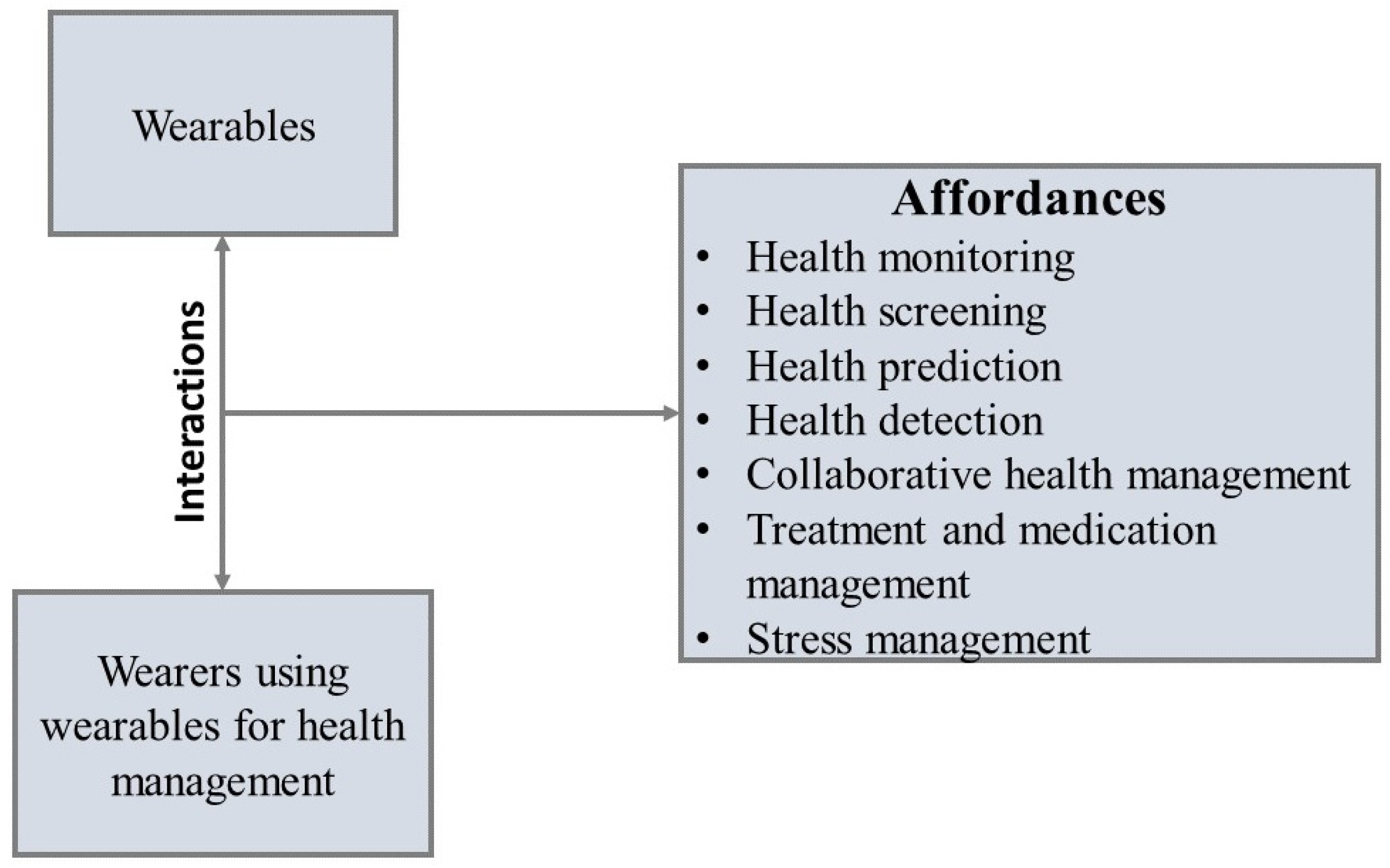
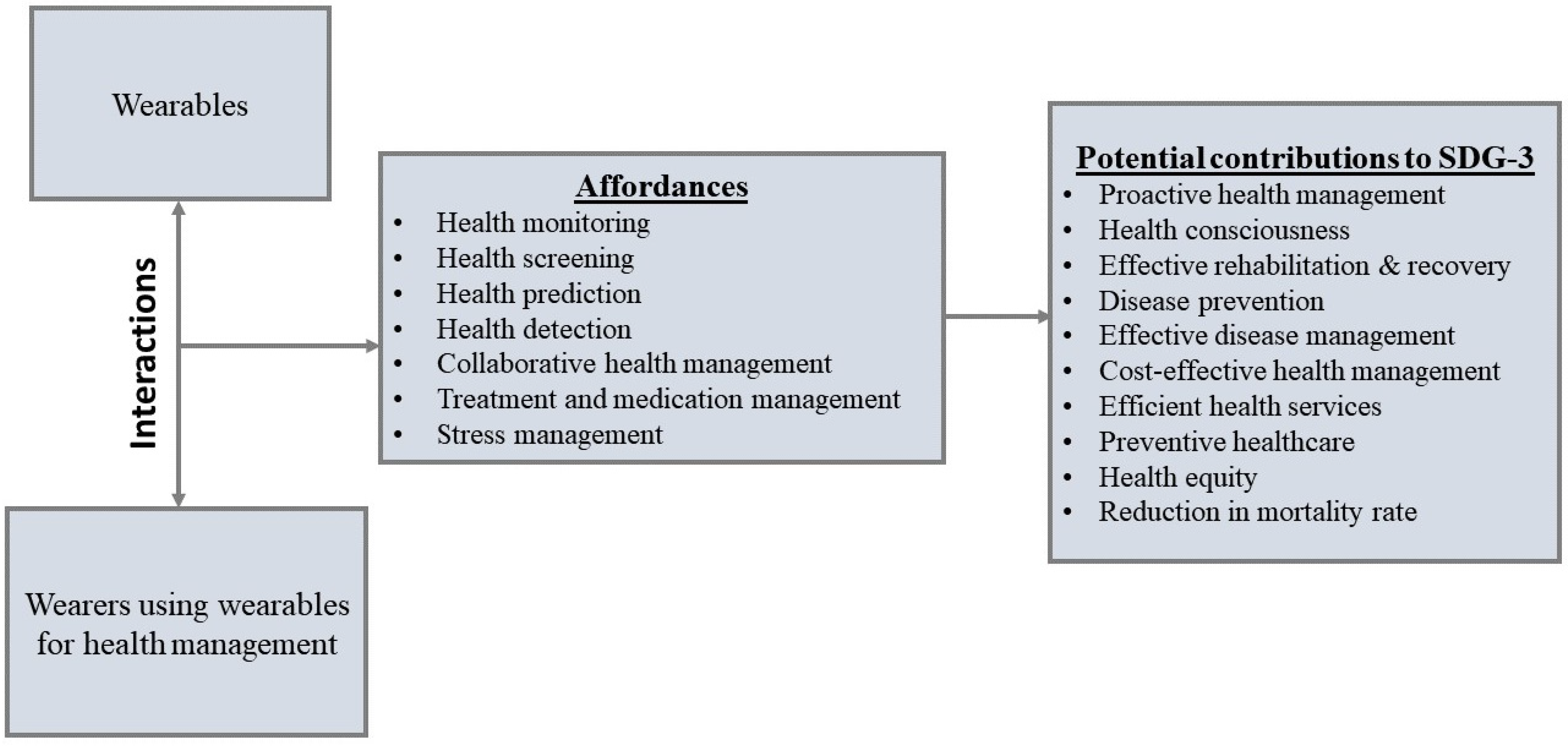
3. Theoretical Background: Affordance Theory (AT)
4. Methodology
5. Findings
6. Discussion
6.1. Health Monitoring Affordance (HMA)
6.2. Health Screening Affordance (HSA)
6.3. Health Detection Affordance (HDA)
6.4. Health Prediction Affordance (HPA)
6.5. Collaborative Health Management Affordance (CHMA)
6.6. Health Treatment and Medication Management Affordance (HTMMA)
6.7. Stress Management Affordance (SMA)
7. Implications for SDG-3 Achievement
8. Limitations and Future Research
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Types | Placement | Brand Name | Data Collected and Measured |
|---|---|---|---|
| Smartwatch | Wrist | PKG Watch | Parkinson’s motor symptoms like immobility, tremors, involuntary (Dyskinesia) or slow movements (Bradykinesia), and fluctuations in motor skills [23,38,39,40,41]. |
| Apple Watch | Blood oxygen level, ECG, and sleep patterns [29,30,36]. | ||
| Fitbit Sense | ECG data, Blood oxygen saturation, skin temperature, sleep pattern, and electrodermal activity [17,28]. | ||
| Mi Band 6 | Heart rate [17]. | ||
| Sony Smartwatch 4 | Heart rate [17]. | ||
| Garmin VivoSmart | Heart rate and calories [17]. | ||
| HELO LX | Heart rate, sugar level, blood pressure, ECG, blood temperature, oxygen saturation, breathing rate, calories, mood, and sleep cycle [24,37]. | ||
| E4 Wristband | Blood pulse volume, skin temperature, movement, and stress level [37]. | ||
| Reign Active recovery band | Heart rate, calories, and sleep patterns [37]. | ||
| Amiigo | Blood pressure, heart rate, pulse volume, arterial blood gas, oxygen saturation, respiratory rate, skin temperature, calories burned, and sleep time and quality [37]. | ||
| Smart handband | Wrist | Mio SLICETM | Heart rate [37]. |
| Samsung Galaxy Fit | Heart rate [23]. | ||
| Xiaomi Mi Smart Band 4 | Heart rate [23]. | ||
| Huawei Band 3 Pro | Calories burned [23]. | ||
| Smart headband | Head | MuseTM | Measures EEG-related data [37]. |
| B2v2 Headband | EEG-related data [37]. | ||
| Smart headset | Starstim fNIRS | Measuring EEG-related data and blood flow (hemodynamics) [37]. | |
| Smart patches/e-patches | Chest | ZephyrTM | Heart rate, breathing rate, heart rate variability, blood pressure, arterial blood oxygen saturation, and calories burned [24,36,37]. |
| Lief | ECG-related data such as breathing rate and heart rate variability [23,37]. | ||
| Mesana | Data relating to circulatory diagnostics and cardiovascular prevention [23]. | ||
| Wearable Ultrasound Patch | ECG-related data such as internal blood pressure like blood pressure inside deep arteries, lungs, or heart [19,23]. | ||
| Smart glasses/eyewear | Eye | Lowdown Focus | EEG-related data like brain activity and cognitive training activities [37]. |
| E-textiles/clothing | Body | Hexoskin | Heart rate, heart rate variability, breathing rate, tidal volume, cadence, and calories burned [24,37] |
References
- Papa, A.; Mital, M.; Pisano, P.; Del Giudice, M. E-health and well-being monitoring using smart healthcare devices: An empirical investigation. Technol. Forecast. Soc. Chang. 2020, 153, 119226. [Google Scholar] [CrossRef]
- Trencher, G.; Karvonen, A. Stretching “smart”: Advancing health and well-being through the smart city agenda. In Smart and Sustainable Cities? Barr, S., Krueger, R., Nakajima, M., Thompson-Fawcett, M., Eds.; Routledge: London, UK, 2019; Volume 24, pp. 610–627. [Google Scholar]
- World Commission on Environment and Development (WCED). Our Common Future: Report of the World Commission on Environment and Development (The Brundtland Report); Oxford University Press: Oxford, UK, 1987. [Google Scholar]
- United Nations (UN). Transforming our world: The 2030 Agenda for Sustainable Development. In Proceedings of the United Nations General Assembly 4th Plenary Meeting, New York, NY, USA, 25 September 2015. [Google Scholar]
- Srividya, S.; Velayudhan, A. Sustainability and Health. Int. J. Indian Psych. 2016, 3, 55–62. [Google Scholar] [CrossRef]
- Howden-Chapman, P.; Siri, J.; Chisholm, E.; Chapman, R.; Doll, C.N.; Capon, A. SDG 3: Ensure healthy lives and promote well-being for all at all ages. In A Guide to SDG Interactions: From Science to Implementation; International Council for Science: Paris, France, 2017; pp. 81–126. [Google Scholar]
- Tremblay, D.; Fortier, F.; Boucher, J.F.; Riffon, O.; Villeneuve, C. Sustainable development goal interactions: An analysis based on the five pillars of the 2030 agenda. Sustain. Dev. 2020, 28, 1584–1596. [Google Scholar] [CrossRef]
- Boyacioğlu, E.Z. The importance of health expenditures on sustainable development. Int. J. Soc. Sci. Humanit. Stud. 2012, 4, 147–158. [Google Scholar]
- United Nations (UN). The Sustainable Development Goals Report 2023: Special Edition; UN Publications: New York, NY, USA, 2023; pp. 1–100. [Google Scholar]
- Meskó, B. Digital health technologies and well-being in the future. IT Prof. 2022, 22, 20–23. [Google Scholar] [CrossRef]
- Baig, M.M.; Hosseini, H.G.; Afifi, S.; Mirza, F. Current challenges and barriers to the wider adoption of wearable sensor applications and Internet-of-Things in health and well-being. In Proceedings of the International Conference on Information Resources Management, Auckland, New Zealand, 27–29 May 2019. [Google Scholar]
- Wortley, D.; An, J.Y.; Nigg, C.R. Wearable technologies, health and well-being: A case review. Digit. Med. 2017, 3, 11–17. [Google Scholar] [CrossRef]
- Giffinger, R.; Fertner, C.; Kramar, H.; Meijers, E. City-ranking of European medium-sized cities. Cent. Reg. Sci. Vienna UT 2007, 9, 1–12. [Google Scholar]
- Van Der Hoogen, A.; Scholtz, B.; Calitz, A. Using Theories to Design a Value Alignment Model for Smart City Initiatives. In Responsible Design, Implementation and Use of Information and Communication Technology; Hattingh, M., Matthee, M., Smuts, M., Pappas, I., Dwivedi, Y.K., Mäntymäki, M., Eds.; Springer: New York, NY, USA, 2020; Volume 12066, pp. 55–66. [Google Scholar]
- Park, E.; Del Pobil, A.P.; Kwon, S.J. The role of Internet of Things (IoT) in smart cities: Technology roadmap-oriented approaches. Sustainability 2018, 10, 1388. [Google Scholar] [CrossRef]
- Ometov, A.; Shubina, V.; Klus, L.; Skibińska, J.; Saafi, S.; Pascacio, P.; Flueratoru, L.; Gaibor, D.Q.; Chukhno, N.; Chukhno, O.; et al. A survey on wearable technology: History, state-of-the-art and current challenges. Comput. Netw. 2021, 193, 108074. [Google Scholar] [CrossRef]
- Vijayan, V.; Connolly, J.P.; Condell, J.; McKelvey, N.; Gardiner, P. Review of wearable devices and data collection considerations for connected health. Sensors 2021, 21, 5589. [Google Scholar] [CrossRef]
- Benbunan-Fich, R. An affordance lens for wearable information systems. Eur. J. Inf. Syst. 2019, 28, 256–271. [Google Scholar] [CrossRef]
- Guk, K.; Han, G.; Lim, J.; Jeong, K.; Kang, T.; Lim, E.-K.; Jung, J. Evolution of Wearable Devices with Real-Time Disease Monitoring for Personalized Healthcare. Nanomaterials 2019, 9, 813. [Google Scholar] [CrossRef]
- Alhejaili, R.; Alomainy, A. The Use of Wearable Technology in Providing Assistive Solutions for Mental Well-Being. Sensors 2023, 23, 7378. [Google Scholar] [CrossRef]
- Zovko, K.; Šerić, L.; Perković, T.; Belani, H.; Šolić, P. IoT and health monitoring wearable devices as enabling technologies for sustainable enhancement of life quality in smart environments. J. Clean. Product. 2023, 413, 137506. [Google Scholar] [CrossRef]
- Parisi, S. Applying the DATEMATS Method and Tools to Wearable ICS Materials: A Dialogue Between E-textiles and Active Lighting Technologies for Caring and Well-Being. In Materialising the Future: A Learning Path to Understand, Develop and Apply Emerging Materials and Technologies; Springer International Publishing: Cham, Switzerland, 2023; pp. 103–132. [Google Scholar]
- Nahavandi, D.; Alizadehsani, R.; Khosravi, A.; Acharya, U.R. Application of artificial intelligence in wearable devices: Opportunities and challenges. Comput. Methods Programs Biomed. 2022, 213, 106541. [Google Scholar] [CrossRef] [PubMed]
- Aliverti, A. Wearable technology: Role in respiratory health and disease. Breathe 2017, 13, e27–e36. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Yu, B.; Wang, F. Artificial intelligence/machine learning solutions for mobile and wearable devices. In Digital Health: Mobile and Wearable Devices for Participatory Health Applications; Elsevier: Amsterdam, The Netherlands, 2020; pp. 55–77. [Google Scholar]
- Laricchia, F. Wearables-Statistics & Facts. Statista. 2022. Available online: https://www.statista.com/topics/1556/wearable-technology/#topicHeader__wrapper (accessed on 22 July 2022).
- Hänsel, K.; Wilde, N.; Haddadi, H.; Alomainy, A. Challenges with current wearable technology in monitoring health data and providing positive behavioural support. In Proceedings of the 5th EAI International Conference on Wireless Mobile Communication and Healthcare, London, UK, 14–16 December 2015. [Google Scholar]
- Arkenberg, C. Why Consumers- and Doctors-Are Wary about Wearable Data: Consumer Wearable Companies Are Smart to Watch for Compliance and Privacy Concerns. Deloitte Insights. Available online: https://www2.deloitte.com/za/en/insights/industry/technology/wearable-technology-healthcare-data.html (accessed on 10 August 2022).
- Apple Newsroom. Apple Reveals Apple Watch Series 8 and the New Apple Watch SE. Available online: https://www.apple.com/newsroom/2022/09/apple-reveals-apple-watch-series-8-and-the-new-apple-watch-se/ (accessed on 28 September 2023).
- Williams, J. Empowering people to live a healthier day: Innovation using Apple technology to support personal health, research, and care. In Apple Health Report; Apple Incorporated: Cupertino, CA, USA, 2022; pp. 1–58. [Google Scholar]
- Prasitlumkum, N.; Cheungpasitporn, W.; Chokesuwattanaskul, A.; Thangjui, S.; Thongprayoon, C.; Bathini, T.; Vallabhajosyula, S.; Kanitsoraphan, C.; Leesutipornchai, T.; Chokesuwattanaskul, R. Diagnostic accuracy of smart gadgets/wearable devices in detecting atrial fibrillation: A systematic review and meta-analysis. Arch. Cardiovasc. Dis. 2021, 114, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Luo, J. Wearable technology applications in healthcare: A literature review. Online J. Nurs. Inform. 2019, 23. Available online: https://www.proquest.com/openview/6c96964dfb83ca06895f330233831a50/1?pq-origsite=gscholar&cbl=2034896 (accessed on 28 July 2022).
- Harvard Medical School. Heart Health: Heart Rhythm Monitoring with a Smartwatch. Available online: https://www.health.harvard.edu/heart-health/heart-rhythm-monitoring-with-a-smartwatch (accessed on 20 July 2022).
- Loucks, J.; Bucailles, A.; Stewart, D.; Crossan, G. Wearable Technology in Health Care: Getting Better All the Time. Deloitte Insight. Available online: https://www2.deloitte.com/za/en/insights/industry/technology/technology-media-and-telecom-predictions/2022/wearable-technology-healthcare.html (accessed on 12 May 2022).
- Statista. Number of Users of Smartwatches Worldwide 2019–2028. Available online: https://www.statista.com/forecasts/1314339/worldwide-users-of-smartwatches (accessed on 26 November 2023).
- Wilson, S.; Laing, R. Wearable technologies: Present and future. In Integrating Design with Sustainable Technology, Proceeding of the 91st World Conference of the Textile Institute, Leeds, UK, 23–26 July 2018; Textile Institute: Manchester, UK, 2018; Volume 1, pp. 1–15. [Google Scholar]
- Peake, J.M.; Kerr, G.; Sullivan, J.P. A critical review of consumer wearables, mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front. Physiol. 2018, 9, 743. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, K.R.; Hand, A.; Obam, F.; Belsey, J. Cost-effectiveness analysis of the Parkinson’s KinetiGraph and clinical assessment in the management of Parkinson’s Disease. J. Med. Econ. 2022, 25, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Dominey, T.; Kehagia, A.A.; Gorst, T.; Pearson, E.; Murphy, F.; King, E.; Carroll, C. Introducing the Parkinson’s KinetiGraph into routine Parkinson’s disease care: A 3-year single centre experience. J. Park. Dis. 2020, 10, 1827–1832. [Google Scholar] [CrossRef]
- Monje, M.H.; Foffani, G.; Obeso, J.; Sánchez-Ferro, Á. New sensor and wearable technologies to aid in the diagnosis and treatment monitoring of Parkinson’s disease. Annu. Rev. Biomed. Eng. 2019, 21, 111–143. [Google Scholar] [CrossRef]
- Pahwa, R.; Isaacson, S.H.; Torres-Russotto, D.; Nahab, F.B.; Lynch, P.M.; Kotschet, K.E. Role of the Personal KinetiGraph in the routine clinical assessment of Parkinson’s disease: Recommendations from an expert panel. Expert Rev. Neurotherapeut. 2018, 18, 669–680. [Google Scholar] [CrossRef]
- Choi, J.; Kim, S. Is the Smartwatch an IT product or a fashion product? A study on factors affecting the intention to use smartwatches. Comput. Hum. Behav. 2016, 63, 777–786. [Google Scholar] [CrossRef]
- Chong, K.P.; Woo, B.K. Emerging wearable technology applications in gastroenterology: A review of the literature. World J. Gastroenterol. 2021, 27, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, D.; Ryoo, H.Y.; Shin, B.S. Sustainable wearables: Wearable technology for enhancing the quality of human life. Sustainability 2016, 8, 466. [Google Scholar] [CrossRef]
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 2018, 4, 195–202. [Google Scholar] [PubMed]
- Quévat, A.; Heinze, A. The digital transformation of preventive telemedicine in France based on the use of connected wearable device. Glob. Bus. Organ. Excell. 2020, 39, 17–27. [Google Scholar] [CrossRef]
- Jin, D.; Adams, H.; Cocco, A.M.; Martin, W.G.; Palmer, S. Smartphones and wearable technology: Benefits and concerns in cardiology. Med. J. Aust. 2020, 212, 54–56. [Google Scholar] [CrossRef] [PubMed]
- Abd-Alrazaq, A.; AlSaad, R.; Harfouche, M.; Aziz, S.; Ahmed, A.; Damseh, R.; Sheikh, J. Wearable Artificial Intelligence for Detecting Anxiety: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2023, 25, e48754. [Google Scholar] [CrossRef]
- American Psychiatric Association (APA) Webpage. What Are Anxiety Disorders? Available online: https://www.psychiatry.org/patients-families/anxiety-disorders/what-are-anxiety-disorders#:~:text=Anxiety%20disorders%20are%20the%20most,a%20number%20of%20psychotherapeutic%20treatments (accessed on 16 November 2023).
- Global Burden of Disease (GBD) Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results; Institute for Health Metrics and Evaluation (IHME): Seattle, WA, USA, 2019. [Google Scholar]
- Abd-Alrazaq, A.; AlSaad, R.; Aziz, S.; Ahmed, A.; Denecke, K.; Househ, M.; Farooq, F.; Sheikh, J. Wearable artificial intelligence for anxiety and depression: Scoping review. J. Med. Internet Res. 2023, 25, e42672. [Google Scholar] [CrossRef]
- Gilmore, J.N. Everywear: The quantified self and wearable fitness technologies. New Media Soc. 2016, 18, 2524–2539. [Google Scholar] [CrossRef]
- Jiang, D.; Shi, G. Research on data security and privacy protection of wearable equipment in healthcare. J. Healthc. Eng. 2021, 2021, 6656204. [Google Scholar] [CrossRef]
- Nunes, A.R.; Lee, K.; O’Riordan, T. The importance of an integrating framework for achieving the Sustainable Development Goals: The example of health and well-being. BMJ Glob. Health 2016, 1, e000068. [Google Scholar] [CrossRef]
- Helldén, D.; Weitz, N.; Nilsson, M.; Alfvén, T. Situating health within the 2030 Agenda—A practical application of the Sustainable Development Goals Synergies Approach. Public Health Rev. 2022, 43, 1604350. [Google Scholar] [CrossRef]
- United Nations (UN). Agenda 21. In Proceedings of the Report of the United Nations Conference on Environment and Development, Rio de Janeiro, Brazil, 3–14 June 1992; United Nations: New York, NY, USA, 1992. (A/CONF.151/26). [Google Scholar]
- United Nations Development Programme (UNDP). Goal 3: Good Health and Well-Being. Available online: https://www.undp.org/sustainable-development-goals/good-health?gad_source=1&gclid=Cj0KCQiAgK2qBhCHARIsAGACuzmHDdoqX8_2Ayv6R6FYmLzzMkCDsqnzOEkuk5QNikuIxJ3iQJ3Zdi4aArcrEALw_wcB (accessed on 28 October 2023).
- Egbende, L.; Helldén, D.; Mbunga, B.; Schedwin, M.; Kazenza, B.; Viberg, N.; Wanyeza, R.; Ali, M.M.; Alfvén, T. Interactions between Health and the Sustainable Development Goals: The Case of the Democratic Republic of Congo. Sustainability 2023, 15, 1259. [Google Scholar] [CrossRef]
- De Neve, J.E.; Sachs, J.D. Sustainable development and human well-being. In World Happiness Report 2020; Helliwell, J.F., Layard, R., Sachs, J.D., De Neve, J.E., Eds.; Sustainable Development Solutions Network: New York, NY, USA, 2020; pp. 112–127. [Google Scholar]
- Pakkan, S.; Sudhakar, C.; Tripathi, S.; Rao, M. A correlation study of sustainable development goal (SDG) interactions. Qual. Quant. 2023, 57, 1937–1956. [Google Scholar] [CrossRef] [PubMed]
- Wanyenze, R.K.; Alfvén, T.; Ndejjo, R.; Viberg, N.; Båge, K.; Batte, C.; Helldén, D.; Lindgren, H.; Mayega, R.W.; Ndeezi, G.; et al. Sustainable health—A call to action. BMC Glob. Public Health 2023, 1, 3. [Google Scholar] [CrossRef]
- Acharya, S.; Lin, V.; Dhingra, N. The role of health in achieving the sustainable development goals. Bull. World Health Organ. 2018, 96, 591–591A. [Google Scholar] [CrossRef]
- Gibson, J.J. The Theory of Affordances. In The Ecological Approach to Visual Perception; Houghton Mifflin: Buston, MA, USA, 1979; pp. 127–137. [Google Scholar]
- Volkoff, O.; Strong, D.M. Critical Realism and Affordances: Theorizing It-Associated Organizational Change Processes. MIS Quart. 2013, 37, 819–834. [Google Scholar] [CrossRef]
- Abouzahra, M.; Ghasemaghaei, M. Effective use of information technologies by seniors: The case of wearable device use. Eur. J. Inf. Syst. 2022, 31, 241–255. [Google Scholar] [CrossRef]
- Vaast, E.; Kaganer, E. Social media affordances and governance in the workplace: An examination of organisational policies. J. Comput-Mediat. Comm. 2013, 19, 78–101. [Google Scholar] [CrossRef]
- Bobsin, D.; Petrini, M.; Pozzebon, M. The value of technology affordances to improve the management of nonprofit organisations. RAUSP Manag. J. 2019, 54, 14–37. [Google Scholar] [CrossRef]
- Valbø, B. The IS-notion of affordances: A mapping of the application of affordance theory in information systems research. In Proceedings of the Information Systems Research Seminar in Scandinavia (IRIS), Norwegian University of Science and Technology, Trondheim, Norway, 9–11 August 2021. [Google Scholar]
- Thapa, D.; Sein, M.K. Trajectory of Affordances: Insights from a case of telemedicine in Nepal. Inf. Syst. J. 2018, 28, 796–817. [Google Scholar] [CrossRef]
- Wang, H.; Wang, J.; Tang, Q. A review of application of affordance theory in information systems. J. Serv. Sci. Manag. 2018, 11, 56. [Google Scholar] [CrossRef]
- Effah, J.; Amankwah-Sarfo, F.; Boateng, R. Affordances and constraints processes of smart service systems: Insights from the case of seaport security in Ghana. Int. J. Inf. Manag. 2021, 58, 102204. [Google Scholar] [CrossRef]
- Evans, S.K.; Pearce, K.E.; Vitak, J.; Treem, J.W. Explicating affordances: A conceptual framework for understanding affordances in communication research. J. Comput-Mediat. Commu. 2017, 22, 35–52. [Google Scholar] [CrossRef]
- Majchrzak, A.; Markus, M.L. Technology Affordances and Constraints in Management Information Systems (MIS). In Encyclopedia of Management Theory; Kessler, E.H., Ed.; Sage: Thousand Oaks, CA, USA, 2012; Volume 1, pp. 832–836. [Google Scholar]
- Lupton, D. The commodification of patient opinion: The digital patient experience economy in the age of big data. Sociol. Health Illn. 2014, 36, 856–869. [Google Scholar] [CrossRef] [PubMed]
- Brooker, P.; Barnett, J.; Vines, J.; Lawson, S.; Feltwell, T.; Long, K. Doing stigma: Online commenting around weight-related news media. New Media Soc. 2018, 20, 3201–3222. [Google Scholar] [CrossRef]
- McAuley, J.; Yang, A. Addressing complex and subjective product-related queries with customer reviews. In Proceedings of the 25th International Conference on World Wide Web, Montreal, QC, Canada, 11–15 April 2016. [Google Scholar]
- Braun, V.; Clarke, V. Thematic analysis. In APA Handbook of Research Methods in Psychology; Cooper, H., Camic, P.M., Long, D.L., Panter, A.T., Rindskopf, D., Sher, K.J., Eds.; American Psychological Association: Washington, DC, USA, 2012; Volume 2, pp. 57–71. [Google Scholar]
- Canali, S.; Schiaffonati, V.; Aliverti, A. Challenges and recommendations for wearable devices in digital health: Data quality, interoperability, health equity, fairness. PLOS Digit. Health 2022, 1, e0000104. [Google Scholar] [CrossRef]
- Bumgarner, J.M.; Lambert, C.T.; Hussein, A.A.; Cantillon, D.J.; Baranowski, B.; Wolski, K.; Lindsay, B.D.; Wazni, O.M.; Tarakji, K.G. Smartwatch Algorithm for Automated Detection of Atrial Fibrillation. J. Am. Coll. Cardiol. 2018, 71, 2381–2388. [Google Scholar] [CrossRef]
- Nazarian, S.; Lam, K.; Darzi, A.; Ashrafian, H. Diagnostic accuracy of smartwatches for the detection of cardiac arrhythmia: Systematic review and meta-analysis. J. Med. Internet Res. 2021, 23, e28974. [Google Scholar] [CrossRef]
- Chen, X.; Xiao, Y.; Tang, Y.; Fernandez-Mendoza, J.; Cao, G. Apneadetector: Detecting sleep apnea with smartwatches. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 59. [Google Scholar] [CrossRef]
- Sharma, R.; Nguyen-Luu, T.; Singh, P.K.; Sardar, S.; Saraza, M.; Abbas, S.Z.; Mirza, W. Sleep apnea detection using photoplethysmography using wearable electronic devices: A systematic review and meta-analysis. Sleep 2023, 46, A245–A246. [Google Scholar] [CrossRef]
- Arulvallal, S.; Snekhalatha, U.; Rajalakshmi, T. Design and development of wearable device for continuous monitoring of sleep apnea disorder. In Proceedings of the 2019 International Conference on Communication and Signal Processing (ICCSP), Melmaruvathur, Tamil Nadu, India, 4–6 April 2019. [Google Scholar]
- Guo, Y.; Zhang, H.; Chen, Y. Population screening for atrial fibrillation in subjects with sleep apnea. Eur. Heart J. 2021, 42, ehab724-0454. [Google Scholar] [CrossRef]
- Quer, G.; Radin, J.M.; Gadaleta, M.; Beca-Motes, K.; Ariniello, L.; Ramos, E.; Kheterpal, V.; Topol, E.J.; Steinhubl, S.R. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nat. Med. 2021, 27, 73–77. [Google Scholar] [CrossRef]
- Muthu, B.; Sivaparthipan, C.B.; Manogaran, G.; Sundarasekar, R.; Kadry, S.; Shanthini, A.; Dasel, A. IOT based wearable sensor for diseases prediction and symptom analysis in healthcare sector. Peer Peer Netw. Appl. 2020, 13, 2123–2134. [Google Scholar] [CrossRef]
- Burnham, J.P.; Lu, C.; Yaeger, L.H.; Bailey, T.C.; Kollef, M.H. Using wearable technology to predict health outcomes: A literature review. J. Am. Med. Inform. Assoc. 2018, 25, 1221–1227. [Google Scholar] [CrossRef]
- Mishra, T.; Wang, M.; Metwally, A.A.; Bogu, G.K.; Brooks, A.W.; Bahmani, A.; Alavi, A.; Celli, A.; Higgs, E.; Fay, B.; et al. Pre-symptomatic detection of COVID-19 from smartwatch data. Nat. Biomed. Eng. 2020, 4, 1208–1220. [Google Scholar] [CrossRef]
- Pyrkov, T.V.; Slipensky, K.; Barg, M.; Kondrashin, A.; Zhurov, B.; Zenin, A.; Pyatnitskiy, M.; Menshikov, L.; Markov, S.; Fedichev, P.O. Extracting biological age from biomedical data via deep learning: Too much of a good thing? Sci. Rep. 2018, 8, 5210. [Google Scholar] [CrossRef]
- Singh, G.; Tee, A.; Trakoolwilaiwan, T.; Taha, A.; Olivo, M. Method of respiratory rate measurement using a unique wearable platform and an adaptive optical-based approach. Intensive Care Med. Exp. 2020, 8, 15. [Google Scholar] [CrossRef]
- Morley, L.; Cashell, A. Collaboration in Health Care. J. Med. Imaging Radiat. Sci. 2017, 48, 207–216. [Google Scholar] [CrossRef]
- Maille, B.; Wilkin, M.; Million, M.; Rességuier, N.; Franceschi, F.; Koutbi-Franceschi, L.; Hourdain, J.; Martinez, E.; Zabern, M.; Gardella, C.; et al. Smartwatch Electrocardiogram and Artificial Intelligence for Assessing Cardiac-Rhythm Safety of Drug Therapy in the COVID-19 Pandemic: The QT-logs study. Int. J. Cardiol. 2021, 331, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Powers, R.; Etezadi-Amoli, M.; Arnold, E.M.; Kianian, S.; Mance, I.; Gibiansky, M.; Trietsch, D.; Alvarado, A.S.; Kretlow, J.D.; Herrington, T.M.; et al. Smartwatch inertial sensors continuously monitor real-world motor fluctuations in Parkinson’s disease. Sci. Transl. Med. 2021, 13, eabd7865. [Google Scholar] [CrossRef] [PubMed]
- Bali, A.; Jaggi, A.S. Clinical experimental stress studies: Methods and assessment. Rev. Neurosci. 2015, 26, 555–579. [Google Scholar] [CrossRef] [PubMed]
- De Witte, N.A.; Buyck, I.; Van Daele, T. Combining biofeedback with stress management interventions: A systematic review of physiological and psychological effects. Appl. Psychophysiol. Biofeedback 2019, 44, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.N.; Santoro, E.; Moraveji, N.; Susi, M.; Crum, A.J. Integrating wearables in stress management interventions: Promising evidence from a randomised trial. Int. J. Stress Manag. 2020, 27, 172. [Google Scholar] [CrossRef]
- The National Health Services (NHS) England. Involving People in Their Own Health and Care: Statutory Guidance for Clinical Commissioning Groups and NHS England. Available online: https://www.england.nhs.uk/wp-content/uploads/2017/04/ppp-involving-people-health-care-guidance (accessed on 12 October 2023).
- Babaei, S.; Abolhasani, S. Family’s supportive behaviors in the care of the patient admitted to the cardiac care unit: A qualitative study. J. Caring Sci. 2020, 9, 80–86. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation (WHO) Eastern Mediterranean Region. Health Promotion and Disease Prevention through Population-Based Interventions. Available online: https://www.emro.who.int/about-who/public-health-functions/health-promotion-disease-prevention.html (accessed on 16 November 2023).
- Jimmy, B.; Jose, J. Patient medication adherence: Measures in daily practice. Oman Med. J. 2011, 26, 155–159. [Google Scholar] [CrossRef]
- Singh, V.; Kumar, A.; Gupta, S. Mental health prevention and promotion: A narrative review. Front. Psychiatry 2022, 13, 898009. [Google Scholar] [CrossRef]
| Affordances | Examples of Related RTs |
|---|---|
| Health Monitoring (f = 126) | RT1: “I’ve been doing research on my health condition about congestive heart failure… I suffered a cardiac arrest last year and comatose for 5 days and recovering, but I needed a device that will monitor my daily routine so I watched video of people who experienced sudden heart attack. This watch is perfect for me…” RT2: “Being that I have sleep apnea I want to track everything and get written reports” RT3: “… it’s about what you would expect with it constantly monitoring your vitals and anything else you set it up to keep track of”. RT4: “Got it for Heart monitoring…Works great. It must pair with your iPhone, confusing which is dominant on various apps. Helpful to have an Apple store nearby or a teenager”. |
| Health Screening (f = 27) | RT1: “…The reason I did this was to try to make sure that I didn’t have any sleep apnea issues as I’ve been accused of snoring and wanted to make sure that that didn’t indicate any potential problems. So far the watch seems to indicate that I’m OK”. RT2: “I upgraded because I felt suspicious about my heartbeat. Sure enough, it was messaging me like crazy! I sent the results to my doctor who ordered more tests and now I’m on medication and feeling so much better”. RT3: “I used my Apple Watch to screen for heart arrhythmias and blood oxygen saturation levels. It works great for this purpose.” RT4: “As someone conscious of COVID hazards, I find having the oximeter App built in has me screening my blood O2 every day vs. a few times a week”. |
| Health Detection (f = 31) | RT1: “I got the Apple Watch because, honestly, I’m getting older and I wanted the fall detection and health features” RT2: “…it helps me with my low blood pressure, it alerts me every time I’m in my anxieties and it tells me how much my heart rate is!!” RT3: “I’m 80 and was paying a monthly fee for a medical device w/fall detection & my Fitbit wasn’t syncing with my iPhone. So happy to find this Watch at such a great price that not only tracks my steps but has fall detection, and it fits on my wrist.” RT4: “First off this watch saved my life!! I have never been diagnosed with Afib. This past Friday night my watch told me I was in Afib and I went to the ER. My heart rate was 147 beats a minute. Had I not had this watch I would have just thought I was having an anxiety attack”. |
| Health Prediction (f = 9) | RT1: “I live in a senior gated community and tell all seniors to buy one because this watch will sense if you are in trouble and you can hit the button for help. My neighbour came over and thanked me for recommending this watch to her it saved her life because it will monitor her heart, she told me the watch sent her a SOS about her heart being in trouble, she went to the hospital and it saved her from a heart attack, because of the early warning with this watch”. RT2: “This gives you an accurate Lead I (RA-LA) ECG waveform. You can print strips on your iPhone and bring them to your Cardiologist if needed, the SpO2 has been accurate as well. I compared all values to an acute care patient monitor for reference”. RT3: “The oxygen is another plus for since I have asthma I can keep a track when I’m sick”. |
| Collaborative Health Management (f = 23) | RT1: “My heart doctor suggested I buy an Apple Watch after having a couple of procedures. Said heart apps were great way to monitor heart activity. He was right. The blood oxygen and ECG apps are easy to use and accurate. Heart Rate app keeps me updated on what my heart is doing and gives me the option to send results to my doctor”. RT2: “Due to health issues, my wife convinced me to get the cellular capability. In an emergency, these will call 911, even when your phone is not around, and even when you don’t subscribe for service. That’s important”. RT3: “ECG, sleep info, hard fall info being sent to emergency services are quality features for all of us and certainly important for octogenarians like my mom” |
| Health Treatment and Medication Management (f = 13) | RT1: “…I had a cardioversion and was put on a beta blocker which worked well for about 6 days. Then my heart would kick back into AFIB for a little while, then the beta blocker would try to convert back to sinus rhythm, in doing so, my heart would do what they call ‘conversion pauses’, only mine would pause to the point of nearly passing out. I happened to catch one of the worst pauses that lasted 8.7 s. I was using my Apple Watch in the ECG mode to check AFIB, at the time. My heart was pausing multiple times. Sent the recordings to my heart Dr. and he took me off the beta blocker for now. I will go back on those after I get my pacemaker the end of the month. If it had not been for the watch and the ability to do the ECGs, I would have not known what was going on and would have thought it to be common under the circumstances. So, I think the watch may have saved my life, by helping to figure out the pauses, which kept getting worse”. RT2: “A few months back, I was diagnosed with a decrease in heart function. The most likely cause, tests revealed, was a sedentary lifestyle. So, in order to help me get moving, track my activity, and monitor my heart, I purchased this Apple Watch. I wear it everywhere except in the shower and when it is charging. It is helping me track longitudinal data about my movement habits…” |
| Stress Management (f = 10) | RT1: …“In addition to indicating when you should take breaks to stop because you have been sitting for more than an hour and also control your breathing to relax and lower stress levels”. RT2: “I’m 37 have had 2 open heart surgery and brain surgery back in 2020 and its perfect for monitoring my stress my heart rate” RT3: “In terms of feature benefits, my main interest are the heart health functions including the Mindfulness/Breath app”. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Izu, L.; Scholtz, B.; Fashoro, I. Wearables and Their Potential to Transform Health Management: A Step towards Sustainable Development Goal 3. Sustainability 2024, 16, 1850. https://doi.org/10.3390/su16051850
Izu L, Scholtz B, Fashoro I. Wearables and Their Potential to Transform Health Management: A Step towards Sustainable Development Goal 3. Sustainability. 2024; 16(5):1850. https://doi.org/10.3390/su16051850
Chicago/Turabian StyleIzu, Lydia, Brenda Scholtz, and Ifeoluwapo Fashoro. 2024. "Wearables and Their Potential to Transform Health Management: A Step towards Sustainable Development Goal 3" Sustainability 16, no. 5: 1850. https://doi.org/10.3390/su16051850
APA StyleIzu, L., Scholtz, B., & Fashoro, I. (2024). Wearables and Their Potential to Transform Health Management: A Step towards Sustainable Development Goal 3. Sustainability, 16(5), 1850. https://doi.org/10.3390/su16051850