Abstract
We examined the associations of plasma vitamin D concentration and adverse pregnancy outcomes among HIV-negative women in Dar-es-Salaam, Tanzania. We used an unmatched case-control study design, with 25-hydroxyvitamin D [25(OH)D] concentration assessed in the first trimester. Cases were individuals with adverse pregnancy outcomes, including stillbirth, premature birth, or small for gestational age births (SGA). Unconditional logistic regression and weighted logistic regression models were used to describe the associations of 25(OH)D concentration with the composite of adverse pregnancy outcome and individual adverse pregnancy outcomes, respectively. We included 310 cases and 321 controls. In controls, 5(2%) were vitamin D deficient (25(OH)D < 20 ng/mL), and 17(5%) had insufficient 25(OH)D concentration (20.0–29.9 ng/mL). Women with 25(OH)D < 20 ng/mL had 1.82 times the odds of occurrence of the composite adverse pregnancy outcome (OR = 1.82, 95% CI: 0.56–5.93; p = 0.32), however we noted a non-linear association between 25(OH)D concentration and adverse pregnancy outcome (p = 0.02). We found a 3-fold increased odds of stillbirth in women with low 25(OH)D concentration (OR = 3.11, 95% CI: 1.18–8.23, p = 0.02). Vitamin D concentration in early pregnancy may be an important factor in determining the course of pregnancy. Further research is needed to investigate whether the association of maternal 25(OH)D concentration in early pregnancy and stillbirth is causal.
1. Introduction
Adverse pregnancy outcomes are still a major global public health problem. It is estimated that 2.6 million babies were stillborn in 2015 worldwide [1], and that 98% of stillbirths occur in low- and middle-income countries [2]. Prematurity remains a major condition associated with higher infant and child mortality and lifelong disabilities [3,4]. Children who were small for gestational age (SGA) at birth have increased risk of chronic diseases, such as cardiovascular diseases, complications including insulin resistance, and metabolic syndrome [5].
During pregnancy there is an increased demand for micronutrients, including vitamin D, to support fetal growth [6]. Vitamin D has an important role in placental functioning, calcium homeostasis, bone mineralization, muscle contraction, development of the nervous system and cellular function. All these processes are necessary for healthy fetal growth and development [7,8]. Despite its importance, vitamin D deficiency during pregnancy is common, and remains a significant public health problem. High prevalence of vitamin D deficiency in pregnant women has been found in high latitude countries due to limited sunlight and the long winter season [7,8,9,10]. However, in tropical countries where sufficient ultraviolet light is assumed, vitamin D deficiency during pregnancy is also prevalent [11,12,13], possibly related to high skin melanin, aging, skin coverage by clothing, and spending much time in indoors [8,11].
Adverse pregnancy outcomes have been associated with low vitamin D concentrations during pregnancy [7,9,14]. These relationships have been assessed in countries such as the United States of America (USA), China, Bangladesh and the Netherlands [7,10,13,15,16]. In several African settings vitamin D has been examined among Human Immunodeficiency Virus (HIV) infected women [12], with limited assessment among the larger population of HIV-negative women.
Vitamin D concentration may have protective effects during the early period of embryogenesis [7,10,17], with adverse consequences of its deficiency noted later in pregnancy. Few studies have assessed the association of first trimester vitamin D concentration and pregnancy outcomes. This study sought to describe the relationship of first trimester vitamin D concentration with adverse pregnancy outcomes, including stillbirth, premature birth, and SGA birth among HIV-negative women in urban Dar-es-Salaam, Tanzania.
2. Materials and Methods
2.1. Study Design and Participants
We used an unmatched case-control study design. Cases and controls were selected from pregnant women enrolled between 2010 and 2013 in a randomized double-blind, the trial that assessed oral administration of zinc and vitamin A supplementation starting from early pregnancy (<13 weeks of gestation) on the risk of placental malaria infection and adverse pregnancy outcomes [18]. Briefly, HIV-negative pregnant women in their first or second pregnancy were recruited at their first antenatal care visit or through a demographic surveillance system (DSS) in Temeke district, Dar-es-Salaam. First trimester pregnant women identified though the DSS were referred to the nearest recruitment clinic. In addition to trial supplements, participants received iron and folic acid supplements according to Tanzanian standard of prenatal care. At recruitment, participants provided socio-demographic information, underwent a full clinical examination and provided blood sample for complete blood count test.
Among women from the original trial with samples obtained during the first trimester of pregnancy and having gestational age at delivery 30–42 weeks, known pregnancy outcome, and birth weight (for live birth), we included all cases of stillbirth, prematurity (30–33 completed weeks), and SGA. A random sample of women without these outcomes (controls) was selected from women with live births who delivered at 34–42 weeks of gestation and having infants with birth weight appropriate for gestational age.
2.2. Assessment of Vitamin D Status
Plasma 25-hydroxyvitamin D [25(OH)D] concentrations were assessed during early pregnancy (4–13 weeks of gestation). Venous blood (1–2 mL) was collected into an EDTA vacutainer tube and transferred to the laboratory within two hours in a 4 °C container. Specimens were centrifuged for 10 min at 2500 rpm to obtain plasma, which was aliquoted into sterile cryovials and stored at −80 °C freezer in a Clinical Research Laboratory at Muhimbili University of Health and Allied Science (MUHAS), Dar-es-Salaam. The frozen plasma samples were transferred to the University of Toronto, Ontario, Canada for analysis.
Plasma 25(OH)D concentrations were measured by Enzyme Immunoassay (EIA) (Immunodiagnostic Systems Ltd.,Tyne and Wear, United Kingdom) according to the manufacturer’s instructions with 10% of the samples on each plate performed in duplicate. Laboratory technicians were blinded to the study outcomes. The final EIA plates were read by ELISA reader at 405 nm. Concentrations were extrapolated from a 4-parameter non-linear regression curve using Prism7 for Mac OS X software (version 7.0e). The range of detection for 25(OH)D was 6.5 ng/mL to 96.8 ng/mL. One sample (0.2% of all samples) fell below the lower limit of detection and was included at it was read by ELISA reader. There were no samples above the upper limit of detection.
The 25(OH)D concentrations were classified in three ways: (1) Sufficient vitamin D concentration (25(OH)D ≥ 30.0 ng/mL) and low vitamin D concentration (25(OH)D < 30.0 ng/mL), because plasma 25(OH)D concentrations above 30.0 ng/mL are association with beneficial effects on calcium, bone, and muscle metabolism [19]; (2) the Institute of Medicine (IOM) define vitamin D deficiency being the 25(OH)D < 20.0 ng/mL [20]. Therefore we defined sufficient vitamin D concentration as 25(OH)D ≥ 30.0 ng/mL, insufficient vitamin D concentration being 25(OH)D between 20.0–29.9 ng/mL and vitamin D deficient being 25(OH)D ˂ 20.0 ng/mL [19]; and (3) low vitamin D concentration was defined as 25(OH)D < 40.0 ng/mL because the circulating 25(OH)D of at least 40.0 ng/mL is required to support achievement of maximum production of the active hormone 1,25(OH)2D in pregnant women [21]. The 25(OH)D concentration < 40.0 ng/mL corresponded to lowest tertile of vitamin D concentration of study participants. We also examined the association of continuous 25(OH)D concentration with the outcomes of interest.
2.3. Definition of Cases and Controls
Since vitamin D deficiency may affect stillbirth, early prematurity, and SGA by a common pathway, we used the composite outcome of any of these 3 as our primary outcome. Controls for the primary outcome were women with live birth who delivered at 34–42 weeks of gestation and having infants with birth weight appropriate for gestational age. Stillbirth was defined as fetal demise before birth (after 28 weeks). Early premature birth was defined among live births as occurring at 30–33 weeks of gestational age. The cut-off point of birth <34 weeks was selected to minimize the likelihood of misclassification of prematurity as gestational age was estimated using the date of last menstrual period, which may overestimate premature births [22]. SGA was defined as a live born infant with birth weight below the 10th percentile for gender based on the INTERGROWTH-21st standards [23], which were applicable to gestational ages from 33–42 weeks. We extrapolated values for 30–32 weeks using the equations provided. We examined the association of vitamin D concentration and individual components of the composite adverse pregnancy outcome. The controls for stillbirth were live births regardless of prematurity status or SGA status. The controls for premature outcome were non-premature (34–42 weeks of gestation) regardless of SGA status. The controls for SGA were appropriate weight-for-gestational age regardless of prematurity status.
2.4. Statistical Analysis
In the primary analysis, unconditional logistic regression models were used to describe the association of 25(OH)D concentrations and the composite outcome [24,25,26]. The possibility of a non-linear relationship of 25(OH)D concentrations with the composite adverse pregnancy outcome was examined non-parametrically with restricted cubic splines [27]. A test for non-linearity was done using the likelihood ratio test which compared the model with only the linear term to the model with the linear and the cubic spline terms. Covariates for all multivariable analyses (including non-linear models) were selected based on prior knowledge of possible associations with individual adverse pregnancy outcomes. These included maternal age; number of previous pregnancies; body mass index (BMI) (weight (kg)/height (m)2) categorized as underweight (BMI < 18.5kg/m2), normal weight (BMI within 18.5–24.9 kg/m2) and overweight/obese (BMI ≥ 25.0 kg/m2); anaemia (defined as haemoglobin < 11.0 g/dL); and experimental regimen received (zinc and vitamin A supplements). Other socio-economic variables with p-value < 0.25 in univariable models were included.
Secondary analysis of individual components of the composite outcome used weighted logistic regression models [28,29]. We sought to produce a control sample for each component that would resemble a control sample chosen for that component in an independent analysis. Since we had a complete sample of the other components of the composite outcome, those who had experienced one or more of three secondary outcomes were oversampled relative to the original controls. We therefore down weighted them so that the sum of the weights would equal the number expected to be chosen if the sampling proportions had been the same as for the original controls. For each individual outcome, cases received unit weight and controls received outcome specific weight (non-premature SGA, non-premature non-SGA, premature non-SGA, and premature-SGA) equal to the ratio of the selection probabilities in the main analysis and the current study sample. The Firth penalized maximum likelihood estimation method for logistic regression model was adopted in the presence of complete separation of data points for all analysis of individual component outcomes [30,31,32]. Due to low prevalence of vitamin D deficiency, statistical analysis for individual adverse pregnancy outcomes did not use the three level vitamin D classification as defined by the IOM except for descriptive analysis. To investigate possible bias induced by missing vitamin D concentration for premature birth <30 weeks of gestation, sensitivity analysis was done using multiple imputation techniques with 10 imputed dataset [33]. The imputation of missing 25(OH)D was done using full conditional specification [FCS] method [34], and actual weeks of gestation was used in this model. Results were considered statistically significant if the 2-sided p-value was <0.05. Data management and data analysis were done in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethical approvals were obtained from the Harvard T.H. Chan School of Public Health Institutional Review Board, the Muhimbili University of Health and Allied Sciences (MUHAS) Senate of Research and Publications Committee, Tanzania’s National Institute for Medical Research, and the University Health Network (Toronto, ON, Canada). The IRB approval code for Harvard is 18,573, the MUHAS is Ref.No.2015-06-26/AEC/Vol.IX/119 and the University Health Network is 14-7313.
3. Results
3.1. Participants
Among 2500 pregnant women in the parent trial, 487 were excluded because of miscarriages, fetal losses of unknown date, unknown pregnancy outcome, unknown delivery gestational age, implausible gestational age, implausible birth weight for gestational age, missing birth weight, gestational age < 30 weeks or > 42 weeks (Figure 1). Of the remaining 2013 women, 534 women did not have a baseline plasma sample available for 25(OH)D concentration analysis and 32 women had twin pregnancy. Of the remaining participants, 310 women had one or more adverse pregnancy outcome and were considered cases: 36 had stillbirths, 72 had premature live births, and 203 had SGA live births (including one participant who had both premature and SGA birth). Among the 203 SGA, 194 (96%) were term (birth > 37 weeks) births. We randomly selected 321 women from women with live, non-premature births with birth weight appropriate for gestational age as controls.
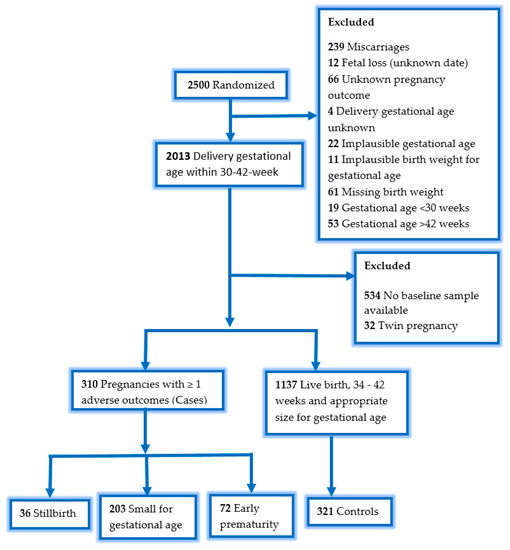
Figure 1.
Sample flowchart, one pregnancy had premature birth and small for gestational age birth.
The average gestational age at baseline was 10 (standard deviation (SD): 2.4) weeks and was similar between cases and controls (Table 1). The majority of participants were ≤24 years, unemployed, married or cohabiting, with 0–7 years of education, and classified as normal BMI. This was similar for individual adverse pregnancy outcomes (Table S1).

Table 1.
Baseline maternal characteristics among cases of adverse pregnancy outcomes and controls in Dar-es-Salaam, Tanzania.
3.2. The Association of Vitamin D Concentration and the Composite Adverse Pregnancy Outcomes
In controls, 5(2%) were vitamin D deficient (<20.0 ng/mL), 17(5%) had insufficient vitamin D concentration (20.0–29.9 ng/mL) and 299(93%) had sufficient vitamin D concentration (25(OH) ≥ 30.0 ng/mL). The average 25(OH)D concentrations were 42.3 (SD: 8.0) ng/mL in the cases and 42.7 (SD: 8.6) ng/mL in the controls. Pregnant women with 25(OH)D concentrations classified in second tertile (40.10–46.71 ng/mL) had slightly high proportions of the composite outcome (37%) compared to controls (31%) (Table S2). There was no association between 25(OH)D concentrations and having the composite adverse pregnancy outcome. Compared to women with sufficient 25(OH)D concentrations, women with 25(OH)D < 20.0 ng/mL had 1.82 times the odds of having the outcome (OR = 1.82, 95% CI: 0.56–5.93; p = 0.32) (Table 2).

Table 2.
Relationship of composite adverse pregnancy outcomes and vitamin D concentration during early pregnancy, Dar-es-Salaam, Tanzania 1.
However, the results showed a non-linear association between first trimester 25(OH)D concentrations and the composite adverse pregnancy outcome (p = 0.02, Figure 2). A higher risk of the composite adverse pregnancy outcome was observed at low levels of 25(OH)D concentrations (25(OH)D < 20.0 ng/mL), but the confidence intervals were wide due to few data points. High levels of 25(OH)D concentrations (25(OH)D > 48 ng/mL) were associated with reduced odds of the composite adverse pregnancy outcome.
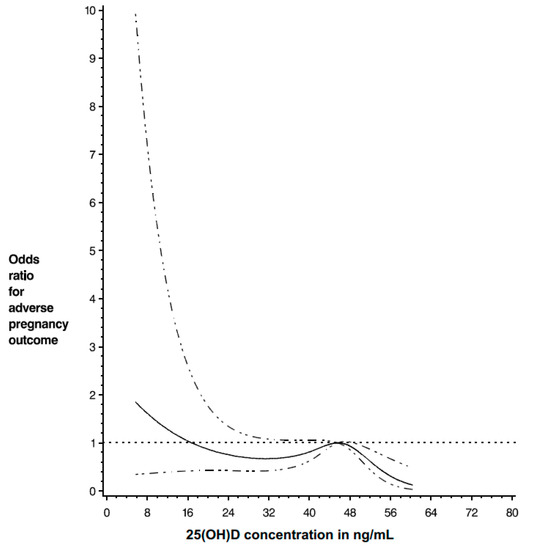
Figure 2.
The adjusted relationship of 25(OH)D concentration and the composite adverse pregnancy outcome. The model included maternal age, employment status, wealth quartile, number of previous pregnancies, zinc supplement, vitamin A supplement, body mass index and anaemia status.
3.3. The Association of Vitamin D Concentration and Individual Adverse Pregnancy Outcomes
Among women who experienced stillbirth, 14% had 25(OH)D concentrations < 30.0 ng/mL and 6% had 25(OH)D concentrations < 20.0 ng/mL; the corresponding proportions for controls were 6% and 2% (Table 3).

Table 3.
Distribution of vitamin D concentration among cases and control for individual pregnancy outcome, Dar-es-Salaam, Tanzania.
There was a 3-fold increased odds of stillbirth in women with 25(OH)D concentrations < 30.0 ng/mL during early pregnancy (OR = 3.11, 95% CI: 1.18–8.23, p = 0.02) (Table 4). Similarly, women in the first tertile of 25(OH)D concentrations (5.71–40.03 ng/mL) had an increased odds of stillbirth compared to women in third tertile (46.73–60.35 ng/mL) (OR = 2.46, 95% CI: 1.12–5.43, p = 0.03) (Table S3). We did not note significant associations of 25(OH)D concentrations during early pregnancy and premature or SGA births.

Table 4.
Relationships of individual adverse pregnancy outcomes and vitamin D concentration during early pregnancy, Dar-es-Salaam, Tanzania 1.
4. Discussion
Vitamin D deficiency was not common in these mostly young, low parity women in urban Tanzania. We noted there was a non-linear association of first trimester 25(OH)D concentration and the composite adverse pregnancy outcome of stillbirth, premature, or SGA births, in which a protective association was observed from 25(OH)D concentration above 48 ng/mL. The 25(OH)D concentration was also associated with stillbirth as an individual outcome.
The association of stillbirth and low 25(OH)D concentration contrasts with findings in Bangladesh [13] and China [35], where no such association was observed. However, these studies differ from our study in terms of gestational age at which 25(OH)D concentration was assessed. The Bangladesh and China studies assessed 25(OH)D concentration at 17–24 weeks of gestation and 16–20 weeks of gestation, respectively, compared to 4–13 weeks in the current study. Our results also conflict with a study which assessed 25(OH)D concentration in the first trimester (10–14 week of gestation) among Australian women in a sun-rich latitude where vitamin D supplementation was uncommon; the findings did not support the association of maternal vitamin D status and stillbirth [17]. We speculate that geographical location and socioeconomic factors may explain the discrepancies observed between the study and ours despite similarities in prevalence of vitamin D deficiency. Hollis and Wagner [36], suggested that during early pregnancy, vitamin D prevents fetal rejection by the mother through its immunomodulatory effects, providing a possible mechanism that could explain the association of increased risk of stillbirths among women with low 25(OH)D concentrations.
It is postulated that vitamin D during early pregnancy has a role in implantation, placentation and maintenance of health pregnancy [37]. In normal early pregnancy, vitamin D receptors increases significantly. It has been suggested that a decrease in placental vitamin D receptors contributes to an increase in apoptosis which is associated with fetal growth retardation pathogenesis [37]. This mechanism is biologically plausible, but unlike others [7,10,16,38] we did not find an evidence for the association of 25(OH)D concentrations and SGA births.
A cohort study conducted in China which assessed SGA births in term infants found increased risk of SGA births in women with vitamin D deficiency during the first prenatal visit [10]. However, most other studies were conducted in high latitude countries where the prevalence of vitamin D deficiency during pregnancy is high due to limited sun light and long winter seasons, compared to tropical countries. This geographical heterogeneity may contribute to conflicting results in these studies. It has also been argued that null findings in these studies stem from methodological problems, small sample size, or assessment of 25(OH)D concentration late in pregnancy [10]. Our study is notable because unlike most previous studies, we assessed 25(OH)D concentrations in the first trimester.
We found no an association of 25(OH)D concentration during early pregnancy and prematurity. This finding was inconsistent with a large study conducted in the USA [39] which reported a 2-fold increased risk of premature births (births < 34 weeks of gestation) in women with 25(OH)D < 20.0 ng/mL. In addition, McDonnell et al. [40], found maternal 25(OH)D concentration ≥ 40.0 ng/mL (versus < 40.0 ng/mL) was associated with 60% reduced risk of premature births (birth < 37 weeks of gestations). We also examined the association of premature (birth < 34 weeks of gestation) and concentration < 40.0 ng/mL and we did not observe an association. Since 25(OH)D concentration during early pregnancy has a role of immunomodulatory effects [36,41], infection and inflammation during pregnancy contributes to prematurity [41], it is thought that sufficient 25(OH)D concentration during pregnancy will contribute to protect premature births through its anti-inflammatory activities [41]. However, our results do not support this hypothesized mechanism.
As we noted above, various cut-off points of 25(OH)D concentration exist in the literature. Low 25(OH)D concentration has been assessed using cut-off points ranging from <12.0 ng/mL up to <40.0 ng/mL. To some extent this could explain the contradicting findings observed in previous studies. We also noted that the prevalence of low 25(OH)D concentration was dependent on cut-off points implemented (7% for 25(OH)D < 30.0 ng/mL and 33% for 25(OH)D < 40.0 ng/mL). These variations highlight the need for a universally adopted 25(OH)D concentration classification for pregnant women. Nevertheless, we noted that the association between 25(OH)D concentration during pregnancy and adverse pregnancy outcomes did not substantially differ with different cut-offs.
Using 25(OH)D concentrations of <20.0 ng/mL and <30.0 ng/mL to define insufficiency, we found the prevalence of low 25(OH)D concentration was uncommon, in contrast to estimates obtained from a comparable HIV-negative population in Kenya [42]. HIV status may also play role in determining prenatal 25(OH)D concentrations. A study done among HIV positive pregnant women in Dar-es-Salaam, Tanzania found high prevalence (39%) of low vitamin D concentrations (25(OH)D < 32.0 ng/mL) at 12–27 weeks of gestation [12].
Strengths of the study include being among the first large and appropriately analyzed study in Africa to investigate the association of first trimester 25(OH)D concentrations and the composite adverse pregnancy outcomes as well as individual adverse pregnancy outcomes. We were able to show a non-linear association of the first trimester 25(OH)D concentrations and the composite adverse pregnancy outcomes. We also assessed the association of individual pregnancy outcomes given that the burden of these adverse outcomes is still high.
The study has several limitations worth noting. Gestational age was estimated based on date of last menstrual period, the approach may overestimate [22] or underestimate [43] the occurrence of premature births. However, a large study conducted in the USA comparing gestational age based on last menstrual period and clinically estimated gestational age (ultrasound) showed similar results by both methods [15]. In Tanzania ultrasound is not routinely available. While misclassification of premature births may have occurred, this is likely to be non-differential with respect to 25(OH)D concentrations. To reduce the effect of misclassification in the definition of prematurity, we defined prematurity as births occurring before 34 weeks of gestation. We could not investigate the effect of vitamin D concentration on other conditions related to prematurity such as preeclampsia as data on these outcomes were not available. Further, the study was restricted to women who delivered between 30–42 weeks of gestation, which could have attenuated our results if those who delivered before 30 weeks were more likely to be vitamin D deficient. Only 11 women among those who delivered before 30 weeks had a baseline sample, however sensitivity analysis done using multiple imputation techniques showed consistent findings with the primary findings.
5. Conclusions
Maternal nutritional factors associated with increased risk of stillbirths and other adverse pregnancy outcomes such as premature births and SGA births are crucial to examine, given the burden and long term effects of these outcomes. In this study, we noted the non-linear association of 25(OH)D concentration during early pregnancy and the composite of adverse pregnancy outcomes of stillbirth, SGA birth and premature birth. We also noted a significantly increased risk of stillbirths in women with low 25(OH)D concentration during early pregnancy. Vitamin D concentration in early pregnancy may be an important factor in determining the course of pregnancy, and further research is warranted to examine whether this association is causal.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/11/12/2906/s1, Table S1: Distribution of baseline characteristics for each individual pregnancy outcome, Dar-es-Salaam, Tanzania. Table S2: The distribution of vitamin D concentration tertiles among cases of adverse pregnancy outcomes and controls in Dar-es-Salaam, Tanzania Table S3: Relationships of the composite and individual adverse pregnancy outcomes and vitamin D concentration tertiles during early pregnancy, Dar-es-Salaam, Tanzania.
Author Contributions
Conceptualization, K.C.K. and W.W.F.; software, A.V.K., A.M.D. and E.H.; validation, A.M.D.; formal analysis, A.V.K.; investigation, A.M.D., F.M., J.W., A.I.A., S.A., C.M., C.R.S. and W.W.F.; resources, K.C.K. and W.W.F.; data curation, A.M.D. and E.H.; writing—original draft preparation, A.V.K.; writing—review and editing, A.M.D., E.H., C.R.S., K.C.K., and W.W.F.; visualization, A.V.K.; supervision, K.C.K. and W.W.F.; project administration, A.M.D.; funding acquisition, K.C.K. and W.W.F.
Funding
The current study was possible through Global Infectious Diseases (GID) training program sponsored by the U.S. National Institute of Health (NIH) Fogarty International Center, grant number D43 TW 007886. The parent trial was supported by grant from the National Institute of Child Health and Human Development (NICHD RO1 HD057941-01). Partly supported (laboratory analysis of 25-hydroxyvitamin D concentration) by a Canadian Institutes of Health Research (CIHR) Foundation grant, grant number FDN-148439 [Kevin C. Kain] and the Canada Research Chairs Program [Kevin C. Kain]. All funding sources had no role in the study design and data collection, analysis, and interpretation of data and in writing manuscript.
Acknowledgments
Research reported in this publication was supported by Fogarty International Center, of the National Institutes of Health under the Award Number D43 TW 007886. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Blencowe, H.; Cousens, S.; Jassir, F.B.; Say, L.; Chou, D.; Mathers, C.; Hogan, D.; Shiekh, S.; Qureshi, Z.U.; You, D.; et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: A systematic analysis. Lancet Glob. Health 2016, 4, e98–e108. [Google Scholar] [CrossRef]
- Lawn, J.E.; Blencowe, H.; Pattinson, R.; Cousens, S.; Kumar, R.; Ibiebele, I.; Gardosi, J.; Day, L.T.; Stanton, C. Lancet’s Stillbirths Series steering committee Stillbirths: Where? When? Why? How to make the data count? Lancet 2011, 377, 1448–1463. [Google Scholar] [CrossRef]
- Bickle Graz, M.; Tolsa, J.-F.; Fischer Fumeaux, C.J. Being Small for Gestational Age: Does it Matter for the Neurodevelopment of Premature Infants? A Cohort Study. PLoS ONE 2015, 10, e0125769. [Google Scholar] [CrossRef] [PubMed]
- Bianchi-Jassir, F.; Seale, A.C.; Kohli-Lynch, M.; Lawn, J.E.; Baker, C.J.; Bartlett, L.; Cutland, C.; Gravett, M.G.; Heath, P.T.; Ip, M.; et al. Preterm Birth Associated with Group B Streptococcus Maternal Colonization Worldwide: Systematic Review and Meta-analyses. Clin. Infect. Dis. 2017, 65, S133–S142. [Google Scholar] [CrossRef] [PubMed]
- Meas, T.; Deghmoun, S.; Armoogum, P.; Alberti, C.; Levy-Marchal, C. Consequences of Being Born Small for Gestational Age on Body Composition: An 8-Year Follow-Up Study. J. Clin. Endocrinol. Metab. 2008, 93, 3804–3809. [Google Scholar] [CrossRef] [PubMed]
- Mithal, A.; Kalra, S. Vitamin D supplementation in pregnancy. Indian J. Endocrinol. Metab. 2014, 18, 4. [Google Scholar]
- Miliku, K.; Vinkhuyzen, A.; Blanken, L.M.; McGrath, J.J.; Eyles, D.W.; Burne, T.H.; Hofman, A.; Tiemeier, H.; Steegers, E.A.; Gaillard, R.; et al. Maternal vitamin D concentrations during pregnancy, fetal growth patterns, and risks of adverse birth outcomes. Am. J. Clin. Nutr. 2016, 103, 1514–1522. [Google Scholar] [CrossRef] [PubMed]
- Thorne-Lyman, A.; Fawzi, W.W. Vitamin D during pregnancy and maternal, neonatal and infant health outcomes: A systematic review and meta-analysis. Paediatr. Perinat. Epidemiol. 2012, 26, 75–90. [Google Scholar] [CrossRef] [PubMed]
- Hart, P.H.; Lucas, R.M.; Walsh, J.P.; Zosky, G.R.; Whitehouse, A.J.O.; Zhu, K.; Allen, K.L.; Kusel, M.M.; Anderson, D.; Mountain, J.A. Vitamin D in Fetal Development: Findings from a Birth Cohort Study. Pediatrics 2015, 135, e167–e173. [Google Scholar] [CrossRef]
- Wang, H.; Xiao, Y.; Zhang, L.; Gao, Q. Maternal early pregnancy vitamin D status in relation to low birth weight and small-for-gestational-age offspring. J. Steroid Biochem. Mol. Biol. 2018, 175, 146–150. [Google Scholar] [CrossRef]
- Palacios, C.; Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid Biochem. Mol. Biol. 2014, 144PA, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.L.; Mehta, S.; Duggan, C.; Manji, K.P.; Mugusi, F.M.; Aboud, S.; Spiegelman, D.; Msamanga, G.I.; Fawzi, W.W. Maternal Vitamin D Status and Child Morbidity, Anemia, and Growth in Human Immunodeficiency Virus-Exposed Children in Tanzania. Pediatr. Infect. Dis. J. 2012, 31, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Morris, S.K.; Zlotkin, S.; Gernand, A.D.; Ahmed, T.; Shanta, S.S.; Papp, E.; Korsiak, J.; Shi, J.; Islam, M.M.; et al. Vitamin D Supplementation in Pregnancy and Lactation and Infant Growth. N. Engl. J. Med. 2018, 379, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Amegah, A.K.; Klevor, M.K.; Wagner, C.L. Maternal vitamin D insufficiency and risk of adverse pregnancy and birth outcomes: A systematic review and meta-analysis of longitudinal studies. PLoS ONE 2017, 12, e0173605. [Google Scholar] [CrossRef] [PubMed]
- Ananth, C.V.; Vintzileos, A.M. Distinguishing pathological from constitutional small for gestational age births in population-based studies. Early Hum. Dev. 2009, 85, 653–658. [Google Scholar] [CrossRef]
- Chen, Y.; Zhu, B.; Wu, X.; Li, S.; Tao, F. Association between maternal vitamin D deficiency and small for gestational age: Evidence from a meta-analysis of prospective cohort studies. BMJ Open 2017, 7, e016404. [Google Scholar] [CrossRef]
- Schneuer, F.J.; Roberts, C.L.; Guilbert, C.; Simpson, J.M.; Algert, C.S.; Khambalia, A.Z.; Tasevski, V.; Ashton, A.W.; Morris, J.M.; Nassar, N. Effects of maternal serum 25-hydroxyvitamin D concentrations in the first trimester on subsequent pregnancy outcomes in an Australian population. Am. J. Clin. Nutr. 2014, 99, 287–295. [Google Scholar] [CrossRef]
- Darling, A.M.; Mugusi, F.M.; Etheredge, A.J.; Gunaratna, N.S.; Abioye, A.I.; Aboud, S.; Duggan, C.; Mongi, R.; Spiegelman, D.; Roberts, D.; et al. Vitamin A and Zinc Supplementation Among Pregnant Women to Prevent Placental Malaria: A Randomized, Double-Blind, Placebo-Controlled Trial in Tanzania. Am. J. Trop. Med. Hyg. 2017, 96, 826–834. [Google Scholar] [CrossRef]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Endocrine Society Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Dietary Reference Intakes for Calcium and Vitamin D. In The National Academies Collection: Reports Funded by National Institutes of Health; Ross, A.C., Taylor, C.L., Yaktine, A.L., Del Valle, H.B., Eds.; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Hollis, B.W.; Johnson, D.; Hulsey, T.C.; Ebeling, M.; Wagner, C.L. Vitamin D supplementation during pregnancy: Double-blind, randomized clinical trial of safety and effectiveness. J. Bone Miner. Res. 2011, 26, 2341–2357. [Google Scholar] [CrossRef]
- Weinstein, J.R.; Thompson, L.M.; Artiga, A.D.; Bryan, J.P.; Arriaga, W.E.; Omer, S.B.; McCracken, J.P. Determining gestational age and preterm birth in rural Guatemala: A comparison of methods. PLoS ONE 2018, 13, e0193666. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Cheikh Ismail, L.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Knol, M.J. A Tutorial on Interaction. Epidemiol. Methods 2014, 3, 33–72. [Google Scholar] [CrossRef]
- McNutt, L.-A.; Wu, C.; Xue, X.; Hafner, J.P. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am. J. Epidemiol. 2003, 157, 940–943. [Google Scholar] [CrossRef] [PubMed]
- Pearce, N. Analysis of matched case-control studies. BMJ 2016, 352, i969. [Google Scholar] [CrossRef] [PubMed]
- Durrleman, S.; Simon, R. Flexible regression models with cubic splines. Stat. Med. 1989, 8, 551–561. [Google Scholar] [CrossRef]
- Saarela, O.; Kulathinal, S.; Arjas, E.; Läärä, E. Nested case-control data utilized for multiple outcomes: A likelihood approach and alternatives. Stat. Med. 2008, 27, 5991–6008. [Google Scholar] [CrossRef]
- Richardson, D.B.; Rzehak, P.; Klenk, J.; Weiland, S.K. Analyses of case-control data for additional outcomes. Epidemiology 2007, 18, 441–445. [Google Scholar] [CrossRef]
- Firth, D. Bias Reduction of Maximum Likelihood Estimates. Biometrika 1993, 80, 27–38. [Google Scholar] [CrossRef]
- Eyduran, E. Usage of Penalized Maximum Likelihood Estimation Method in Medical Research: An Alternative to Maximum Likelihood Estimation Method. J. Res. Med. Sci. 2008, 13, 325–330. [Google Scholar]
- Heinze, G.; Schemper, M. A solution to the problem of separation in logistic regression. Stat. Med. 2002, 21, 2409–2419. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: Hoboken, NJ, USA, 2009; ISBN 978-0-470-31736-5. [Google Scholar]
- van Buuren, S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat. Methods Med. Res. 2007, 16, 219–242. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Su, L.; Liu, M.; Liu, Y.; Cao, X.; Wang, Z.; Xiao, H. Associations between 25-hydroxyvitamin D levels and pregnancy outcomes: A prospective observational study in southern China. Eur. J. Clin. Nutr. 2014, 68, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Hollis, B.W.; Wagner, C.L. New insights into the vitamin D requirements during pregnancy. Bone Res. 2017, 5, 17030. [Google Scholar] [CrossRef] [PubMed]
- Murthi, P.; Yong, H.E.J.; Ngyuen, T.P.H.; Ellery, S.; Singh, H.; Rahman, R.; Dickinson, H.; Walker, D.W.; Davies-Tuck, M.; Wallace, E.M.; et al. Role of the Placental Vitamin D Receptor in Modulating Feto-Placental Growth in Fetal Growth Restriction and Preeclampsia-Affected Pregnancies. Front. Physiol. 2016, 7, 43. [Google Scholar] [CrossRef]
- Wei, S.-Q.; Qi, H.-P.; Luo, Z.-C.; Fraser, W.D. Maternal vitamin D status and adverse pregnancy outcomes: A systematic review and meta-analysis. J. Matern. Fetal. Neonatal. Med. 2013, 26, 889–899. [Google Scholar] [CrossRef]
- Bodnar, L.M.; Platt, R.W.; Simhan, H.N. Early-Pregnancy Vitamin D Deficiency and Risk of Preterm Birth Subtypes. Obstet. Gynecol. 2015, 125, 439–447. [Google Scholar] [CrossRef]
- McDonnell, S.L.; Baggerly, K.A.; Baggerly, C.A.; Aliano, J.L.; French, C.B.; Baggerly, L.L.; Ebeling, M.D.; Rittenberg, C.S.; Goodier, C.G.; Mateus Niño, J.F.; et al. Maternal 25 (OH) D concentrations ≥40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PLoS ONE 2017, 12, e0180483. [Google Scholar] [CrossRef]
- Zhou, S.-S.; Tao, Y.-H.; Huang, K.; Zhu, B.-B.; Tao, F.-B. Vitamin D and risk of preterm birth: Up-to-date meta-analysis of randomized controlled trials and observational studies. J. Obstet. Gynaecol. Res. 2017, 43, 247–256. [Google Scholar] [CrossRef]
- Toko, E.N.; Sumba, O.P.; Daud, I.I.; Ogolla, S.; Majiwa, M.; Krisher, J.T.; Ouma, C.; Dent, A.E.; Rochford, R.; Mehta, S. Maternal Vitamin D Status and Adverse Birth Outcomes in Children from Rural Western Kenya. Nutrients 2016, 8, 794. [Google Scholar] [CrossRef]
- Katz, J.; Wu, L.A.; Mullany, L.C.; Coles, C.L.; Lee, A.C.C.; Kozuki, N.; Tielsch, J.M. Prevalence of Small-for-Gestational-Age and Its Mortality Risk Varies by Choice of Birth-Weight-for-Gestation Reference Population. PLoS ONE 2014, 9, e92074. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).