Feralgine™ a New Approach for Iron Deficiency Anemia in Celiac Patients
Abstract
:1. Introduction
2. Patients and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lebwohl, B.; Sanders, D.S.; Green, P.H.R. Coeliac disease. Lancet 2018, 391, 70–81. [Google Scholar] [CrossRef]
- Gisbert, J.; Gomolln, F. A short review of malabsorption and anemia. World J. Gastroenterol. 2009, 15, 4644–4652. [Google Scholar]
- Halfdanarson, T.R.; Litzow, M.R.; Murray, J.A. Hematologic Manifestation of celiac disease. Blood 2007, 109, 412–421. [Google Scholar] [CrossRef]
- Mahadev, S.; Laszkowska, M.; Sundström, J.; Björkholm, M.; Lebwohl, B.; Green, P.H.R.; Ludvigsson, J.F. Prevalence of Celiac Disease in Patients with Iron Deficiency Anemia-A Systematic Review with Meta-analysis. Gastroenterology 2018, 155, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Ertekin, V.; Tosun, M.S.; Küçük, N. The prevalence of celiac disease in children with iron deficiency anemia. Turk. J. Gastroenterol. 2013, 24, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Heethira, T.G.; Dennis, M.; Leffler, D.A. Nutritional consequences of celiac disease and the gluten-free diet. Expert Rev. Gastroenterol. Hepatol. 2014, 8, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Vici, G.; Belli, L.; Biondi, M.; Polzonetti, V. Gluten free diet and nutrient deficiencies: A review. Clin. Nutr. 2016, 35, 1236–1241. [Google Scholar] [CrossRef]
- Freeman, H.J. Iron deficiency anemia in celiac disease. World J. Gastroenterol. 2015, 21, 9233–9238. [Google Scholar] [CrossRef]
- DeLoughery, T.G. Ion Deficiency Anemia. Med. Clin. N. Am. 2017, 101, 319–332. [Google Scholar] [CrossRef]
- Alleyne, M.; Horne, M.K.; Miller, J.L. Individualized treatment for iron deficiency anemia in adults. Am. J. Med. 2008, 121, 943–948. [Google Scholar] [CrossRef] [Green Version]
- Camaschella, C. Iron-deficiency anemia. N. Engl. J. Med. 2015, 372, 1832–1843. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, M.M.; Nogueira, N.N.; Diniz, A.S. Effectiveness of different iron supplementation strategies on hemoglobin and ferritin levels among schoolchildren in Teresina, Piauí State, Brazil. Cad. Saude Publica 2007, 23, 1547–1552. [Google Scholar]
- Hertrampf, E.; Olivares, M. Iron amino acid chelates. Int. J. Vitam. Nutr. Res. 2004, 74, 435–443. [Google Scholar] [CrossRef]
- Duque, X.; Martinez, H.; Vilchis-Gil, J.; Mendoza, E.; Flores-Hernànez, S.; Moràn, S.; Navarro, F.; Roque-Evangelista, V.; Serrano, A.; Mera, R.M. Effect of supplementation with ferrous sulfate or iron bis-glycinate chelate on ferritin concentration in Mexican schoolchildren: A randomized controlled trial. Nutr. J. 2014, 13, 71. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, P.; Nicolini, A.; Manca, M.L.; Rossi, G.; Anselmi, L.; Conte, M.; Carpi, A.; Bonino, F. Treatment of mild non-chemotherapy-induced iron deficiency anemia in cancer patients: Comparison between oral ferrous bisglycinate chelate and ferrous sulfate. Biomed. Pharmacother. 2012, 66, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Pineda, O.; Ashmead, H.D. Effectiveness of treatment of iron-deficiency anemia in infants and young children with ferrous bis-glycinate chelate. Nutrition 2001, 17, 381–384. [Google Scholar] [CrossRef]
- Opinion of the Scientific Panel on Food Additives, Flavorings, Processing Aids and materials in Contact with Food. Ferrous bisglycinate as a source of iron for use in the manufacturing of foods and in food supplements. EFSA J. 2006, 299, 1–17.
- Gervasi, G.B.; Baldacci, M.; Bertini, M. Feralgine® a new co-processed substance to improve oral iron bioavailability, taste and tolerability in iron deficiency patients. Arch. Med. 2016, 8, 13. [Google Scholar]
- Hacibekiroglu, T.; Akinci, S.; Basturk, A.R.; Bakanay, S.M.; Ulas, T.; Guney, T.; Dilek, I. A forgotten screening test for iron deficiency anemia: Oral iron absorbtion test. Clin. Ter. 2013, 164, 495–497. [Google Scholar]
- Santarpia, L.; Pagano, M.C.; Cuomo, R.; Alfonso, L.; Contaldo, F.; Pasanisi, F. Iron absorption following a single oral dose of ferrous sulfate or ferric gluconate in patients with gastrectomy. Ann. Nutr. Metab. 2013, 63, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Kobune, M.; Miyanishi, K.; Takada, K.; Kawano, Y.; Nagashima, H.; Kikuchi, S.; Murase, K.; Iyama, S.; Sato, T.; Sato, Y.; et al. Establishment of a simple test for iron absorption from the gastrointestinal tract. Int. J. Hematol. 2011, 93, 715–719. [Google Scholar] [CrossRef]
- Fleming, M.D. Disorders of Iron and Copper Metabolism, the Sideroblastic Anemias, and Lead Toxicity. In Nathan and Oski’s Hematology and Oncology of Infancy and Childhood; Orkin, S.H., Fisher, D.E., Ginsburg, D., Look, A.T., Lux, S.E., Nathan, D.G., Eds.; Elsevier Inc.: Philadelphia, PA, USA, 2015; pp. 344–381. [Google Scholar]
- Jensen, N.M.; Brandsborg, M.; Boesen, A.M.; Yde, H.; Dahlerup, J.F. Low-dose oral iron absorption test: Establishment of a reference interval. Scand. J. Clin. Lab. Investig. 1998, 58, 511–519. [Google Scholar] [CrossRef]
- Rondinelli, M.B.; Di Bartolomei, A.; De Rosa, A.; Pirelli, L. Oral Iron Absorption Test (OIAT): A forgotten screening test for iron absorption from the gastrointestinal tract. A casa series of Iron Deficiency Anemia (IDA) patients treated with FERALGINEE®. J. Blood Disord. Med. 2017, 2, 1. [Google Scholar]
- Andersen, S.L.; Gyrup, C.; Handberg, A.; Nielsen, G.L. Oral iron absorption test should not be performed with iron drops containing ferric iron. Dan. Med. J. 2015, 62, A5116. [Google Scholar] [PubMed]
- Crosby, W.H.; O’Neil-Cutting, M.A. A small-dose iron tolerance test as an indicator of mild iron deficiency. JAMA 1984, 251, 1986–1987. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Dayley, D.; Thanigaikumar, M. The Cost-effective Usefulness of Oral Iron Absorption Test—Prospective Evaluation in Premenopausal Women with Newly Diagnosed Iron Deficiency Anemia. Ann. Hematol. Oncol. 2018, 5, 4. [Google Scholar]
- Mazza, G.A.; Pedrelli, L.; Battaglia, E.; Giancotti, L.; Miniero, R. Oral iron absorption test with ferrous bisglycinate chelate in children with celiac disease: Preliminary results. Minerva Pediatr. 2019, 10, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Barisani, D.; Parafioriti, A.; Bardella, M.T.; Zoller, H.; Conte, D.; Armiraglio, E.; Trovato, C.; Koch, R.O.; Weiss, G. Adaptive changes of duodenal iron transport proteins in celiac disease. Physiol Genom. 2004, 17, 316–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yanatori, I.; Kishi, F. DMT1 and iron transport. Free Radic. Biol. Med. 2019, 133, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Begum, J.; Eksteen, B.; Elagib, A.; Brookes, M.; Cooper, B.T.; Tselepis, C.; Iqbal, T.H. Differential ferritin expression is associated with iron deficiency in coeliac disease. Eur. J. Gastroenterol. Hepatol. 2009, 21, 794–804. [Google Scholar] [CrossRef] [PubMed]
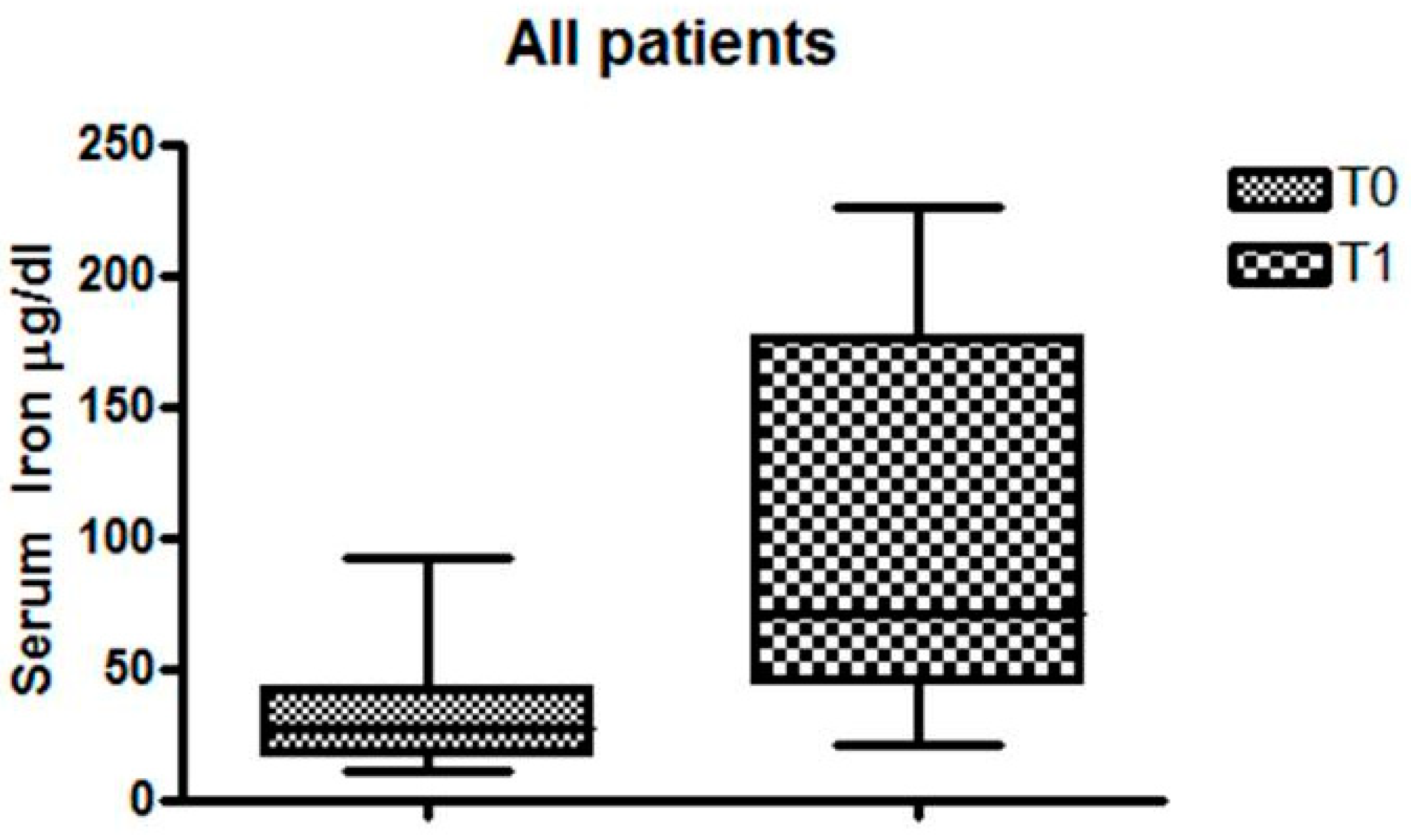
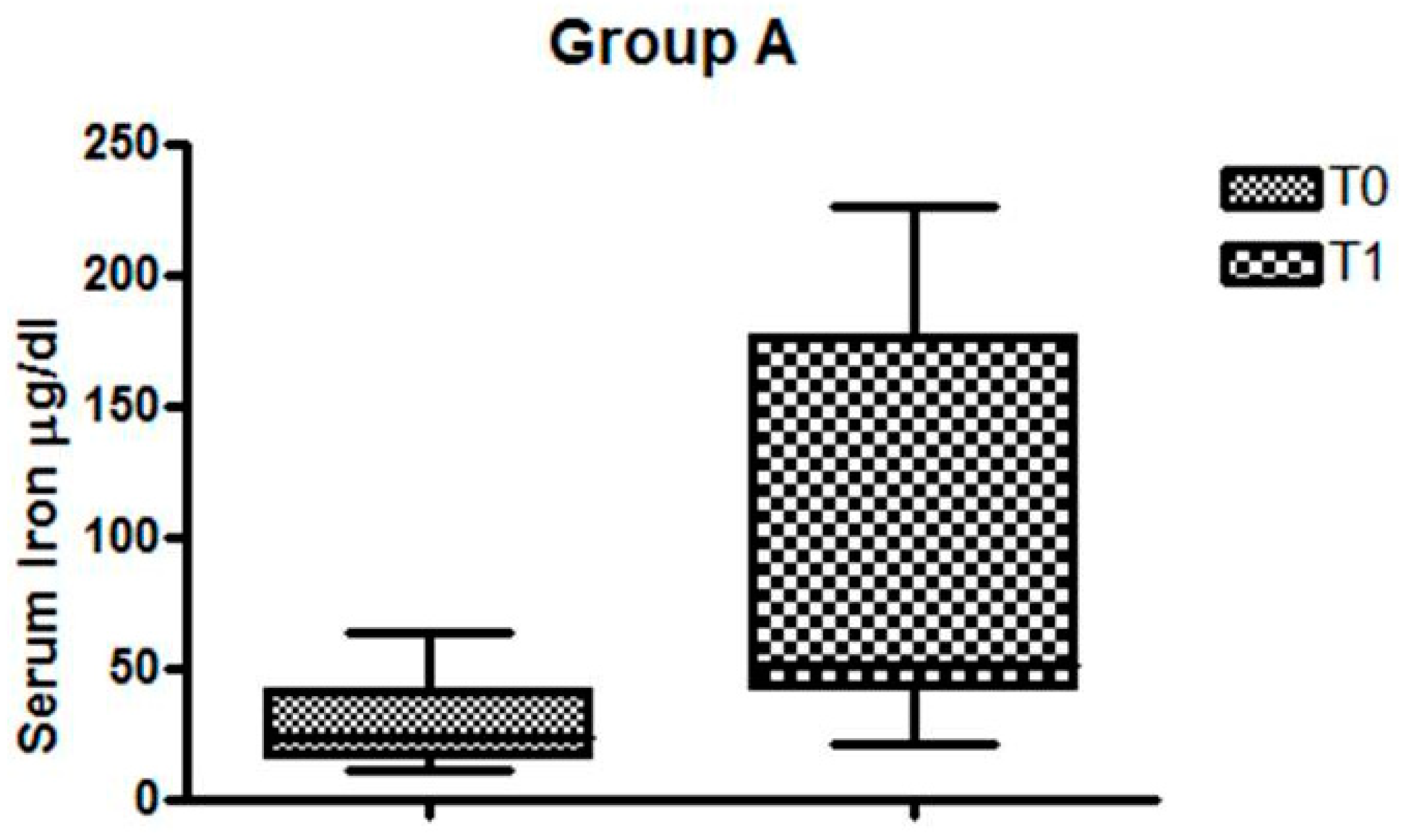

| MALE | FEMALE | HAEMOGLOBIN ± SD (g/dL) | FERRITIN ± SD (ng/dL) | SERUM IRON ± SD (µg/dL) | |
|---|---|---|---|---|---|
| CELIAC-IDA | 2 | 12 | 11.07 ± 1.04 | 10.44 ± 15.9 | 28.21 ± 14.9 |
| NON CELIAC-IDA | 0 | 12 | 10.80 ± 0.9 | 12.30 ± 13.8 | 34.91 ± 23.2 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giancotti, L.; Talarico, V.; Mazza, G.A.; Marrazzo, S.; Gangemi, P.; Miniero, R.; Bertini, M. Feralgine™ a New Approach for Iron Deficiency Anemia in Celiac Patients. Nutrients 2019, 11, 887. https://doi.org/10.3390/nu11040887
Giancotti L, Talarico V, Mazza GA, Marrazzo S, Gangemi P, Miniero R, Bertini M. Feralgine™ a New Approach for Iron Deficiency Anemia in Celiac Patients. Nutrients. 2019; 11(4):887. https://doi.org/10.3390/nu11040887
Chicago/Turabian StyleGiancotti, Laura, Valentina Talarico, Giuseppe Antonio Mazza, Santina Marrazzo, Pietro Gangemi, Roberto Miniero, and Marco Bertini. 2019. "Feralgine™ a New Approach for Iron Deficiency Anemia in Celiac Patients" Nutrients 11, no. 4: 887. https://doi.org/10.3390/nu11040887





