Acute Effects of Nutritive and Non-Nutritive Sweeteners on Postprandial Blood Pressure
Abstract
1. Introduction
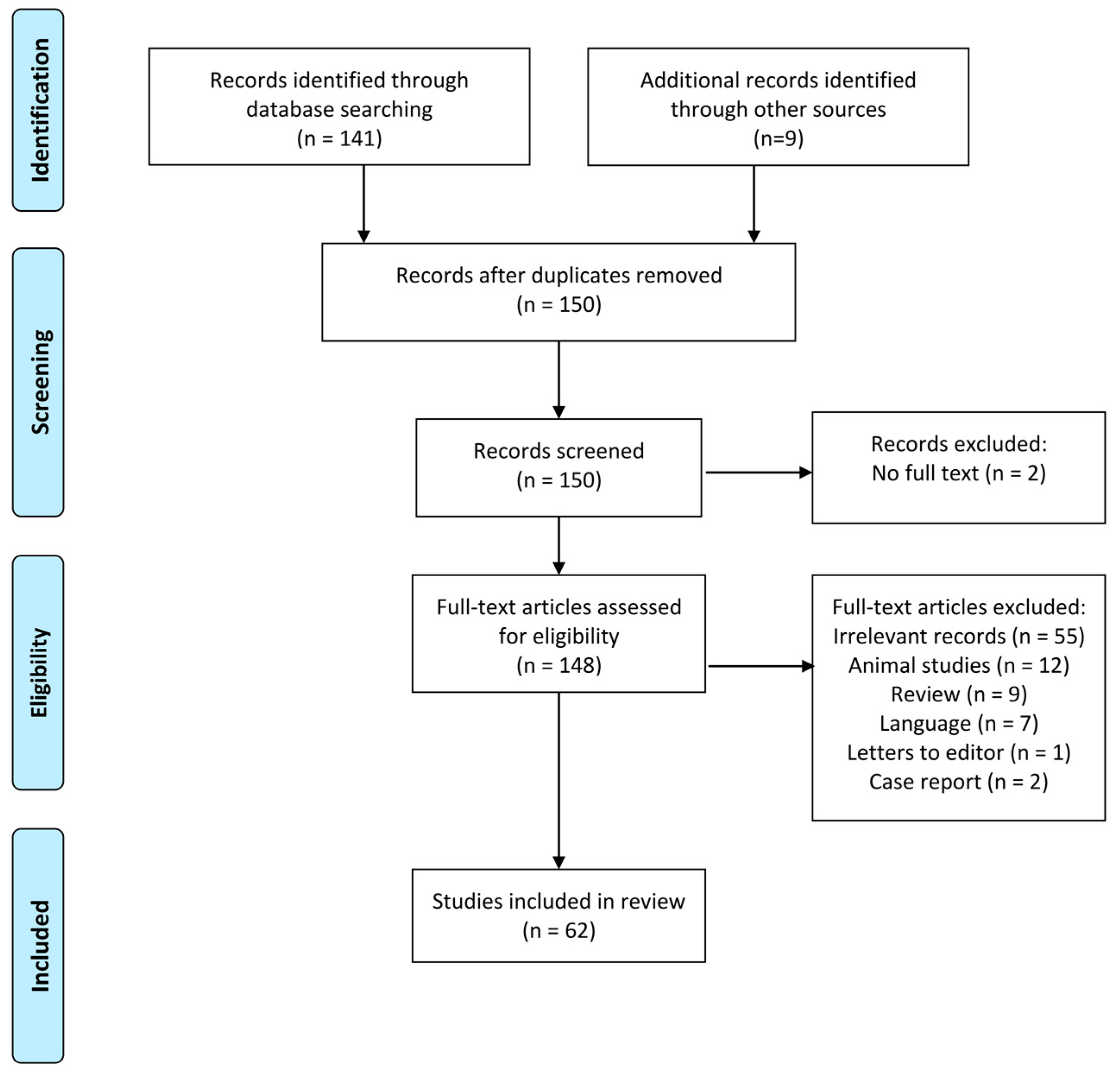
2. Approach
3. Results
4. Nutritive Sweeteners
4.1. Glucose
4.1.1. Intraduodenal Glucose Infusion
4.1.2. Management of PPH
4.2. Fructose
4.3. Sucrose
4.4. d-Xylose and Xylitol
4.5. Erythritol
4.6. Maltose and Maltodextrin
4.7. Tagatose
5. Non-Nutritive Sweeteners
5.1. Sucralose
5.2. Acesulfame-K
5.3. Aspartame
5.4. Saccharin
5.5. Steviol Glycoside
5.6. Neotame and Advantame
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Malik, V.S.; Willett, W.C.; Hu, F.B. Global obesity: Trends, risk factors and policy implications. Nat. Rev. Endocrinol. 2013, 9, 13. [Google Scholar] [CrossRef] [PubMed]
- Fitch, C.; Keim, K.S. Position of the academy of nutrition and dietetics: Use of nutritive and nonnutritive sweeteners. J. Acad. Nutr. Diet. 2012, 112, 739–758. [Google Scholar] [CrossRef] [PubMed]
- American Dietetic Association. Position of the american dietetic association: Use of nutritive and nonnutritive sweeteners. J. Am. Diet. Assoc. 2004, 104, 255–275. [Google Scholar] [CrossRef]
- Trahair, L.G.; Horowitz, M.; Jones, K.L. Postprandial hypotension: A systematic review. J. Am. Med. Dir. Assoc. 2014, 15, 394–409. [Google Scholar] [CrossRef] [PubMed]
- Jansen, R.W.; Lipsitz, L.A. Postprandial hypotension: Epidemiology, pathophysiology, and clinical management. Ann. Intern. Med. 1995, 122, 286–295. [Google Scholar] [CrossRef]
- Puisieux, F.; Bulckaen, H.; Fauchais, A.L.; Drumez, S.; Salomez-Granier, F.; Dewailly, P. Ambulatory blood pressure monitoring and postprandial hypotension in elderly persons with falls or syncopes. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, M535–M540. [Google Scholar] [CrossRef] [PubMed]
- Fisher, A.A.; Davis, M.W.; Srikusalanukul, W.; Budge, M.M. Postprandial hypotension predicts all-cause mortality in older, low-level care residents. J. Am. Geriatr. Soc. 2005, 53, 1313–1320. [Google Scholar] [CrossRef]
- Zanasi, A.; Tincani, E.; Evandri, V.; Giovanardi, P.; Bertolotti, M.; Rioli, G. Meal-induced blood pressure variation and cardiovascular mortality in ambulatory hypertensive elderly patients. J. Hypertens. 2012, 30, 2125–2132. [Google Scholar] [CrossRef]
- Aronow, W.S.; Ahn, C. Association of postprandial hypotension with incidence of falls, syncope, coronary events, stroke, and total mortality at 29-month follow-up in 499 older nursing home residents. J. Am. Geriatr. Soc. 1997, 45, 1051–1053. [Google Scholar] [CrossRef]
- Jansen, R.W.; Peeters, T.L.; Van Lier, H.J.; Hoefnagels, W.H. The effect of oral glucose, protein, fat and water loading on blood pressure and the gastrointestinal peptides VIP and somatostatin in hypertensive elderly subjects. Eur. J. Clin. Invest. 1990, 20, 192–198. [Google Scholar] [CrossRef]
- Jones, K.L.; Tonkin, A.; Horowitz, M.; Wishart, J.M.; Carney, B.I.; Guha, S.; Green, L. Rate of gastric emptying is a determinant of postprandial hypotension in non-insulin-dependent diabetes mellitus. Clin. Sci. 1998, 94, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Pham, H.; Phillips, L.; Trahair, L.; Hatzinikolas, S.; Horowitz, M.; Jones, K.L. Longitudinal changes in the blood pressure responses to, and gastric emptying of, an oral glucose load in healthy older subjects. J. Gerontol. A Biol. Sci. Med. Sci. 2019. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Stevens, J.E.; Wilson, T.; Wells, F.; Tonkin, A.; Horowitz, M.; Jones, K.L. Guar attenuates fall in postprandial blood pressure and slows gastric emptying of oral glucose in type 2 diabetes. Dig. Dis. Sci. 2003, 48, 1221–1229. [Google Scholar] [CrossRef] [PubMed]
- Gentilcore, D.; Hausken, T.; Meyer, J.H.; Chapman, I.M.; Horowitz, M.; Jones, K.L. Effects of intraduodenal glucose, fat, and protein on blood pressure, heart rate, and splanchnic blood flow in healthy older subjects. Am. J. Clin. Nutr. 2008, 87, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Nauck, M.A. Incretin-based therapies for type 2 diabetes mellitus: Properties, functions, and clinical implications. Am. J. Med. 2011, 124, S3–S18. [Google Scholar] [CrossRef] [PubMed]
- Trahair, L.G.; Horowitz, M.; Stevens, J.E.; Feinle-Bisset, C.; Standfield, S.; Piscitelli, D.; Rayner, C.K.; Deane, A.M.; Jones, K.L. Effects of exogenous glucagon-like peptide-1 on blood pressure, heart rate, gastric emptying, mesenteric blood flow and glycaemic responses to oral glucose in older individuals with normal glucose tolerance or type 2 diabetes. Diabetologia 2015, 58, 1769–1778. [Google Scholar] [CrossRef]
- Meier, J.J.; Gallwitz, B.; Salmen, S.; Goetze, O.; Holst, J.J.; Schmidt, W.E.; Nauck, M.A. Normalization of glucose concentrations and deceleration of gastric emptying after solid meals during intravenous glucagon-like peptide 1 in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 2003, 88, 2719–2725. [Google Scholar] [CrossRef]
- Trahair, L.G.; Horowitz, M.; Hausken, T.; Feinle-Bisset, C.; Rayner, C.K.; Jones, K.L. Effects of exogenous glucagon-like Peptide-1 on the blood pressure, heart rate, mesenteric blood flow, and glycemic responses to intraduodenal glucose in healthy older subjects. J. Clin. Endocrinol. Metab. 2014, 99, E2628–E2634. [Google Scholar] [CrossRef]
- Edholm, T.; Degerblad, M.; Grybäck, P.; Hilsted, L.; Holst, J.J.; Jacobsson, H.; Efendic, S.; Schmidt, P.; Hellström, P.M. Differential incretin effects of GIP and GLP-1 on gastric emptying, appetite, and insulin-glucose homeostasis. Neurogastroenterol. Motil. 2010, 22. [Google Scholar] [CrossRef]
- Meier, J.J.; Goetze, O.; Anstipp, J.; Hagemann, D.; Holst, J.J.; Schmidt, W.E.; Gallwitz, B.; Nauck, M.A. Gastric inhibitory polypeptide does not inhibit gastric emptying in humans. Am. J. Physiol. Endocrinol. Metab. 2004, 286, E621–E625. [Google Scholar] [CrossRef]
- Jansen, R.W.; Hoefnagels, W.H. Hormonal mechanisms of postprandial hypotension. J. Am. Geriatr. Soc. 1991, 39, 1201–1207. [Google Scholar] [CrossRef]
- Maule, S.; Tredici, M.; Dematteis, A.; Matteoda, C.; Chiandussi, L. Postprandial hypotension treated with acarbose in a patient with type 1 diabetes mellitus. Clin. Auton. Res. 2004, 14, 405–407. [Google Scholar] [CrossRef]
- Dhingra, R.; Sullivan, L.; Jacques, P.; Wang, T.; Fox, C.; Meigs, J.D.; Agostino, R.B.; Gaziano, J.M.; Vasan, R.S. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 2007, 116, 480–488. [Google Scholar] [CrossRef]
- Popkin, B.M.; Hawkes, C. Sweetening of the global diet, particularly beverages: Patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 2016, 4, 174–186. [Google Scholar] [CrossRef]
- Malik, V.S.; Li, Y.; Pan, A.; De Koning, L.; Schernhammer, E.; Willett, W.C.; Hu, F.B. Long-term Consumption of sugar-sweetened and artificially sweetened beverages and Risk of mortality in US adults. Circulation 2019, 18, 2113–2125. [Google Scholar] [CrossRef]
- Piernas, C.; Ng, S.W.; Popkin, B. Trends in purchases and intake of foods and beverages containing caloric and low-calorie sweeteners over the last decade in the United States. Pediatr. Obes. 2013, 8, 294–306. [Google Scholar] [CrossRef]
- Johnson, R.K.; Lichtenstein, A.H.; Anderson, C.A.; Carson, J.A.; Després, J.P.; Hu, F.B.; Kris-Etherton, P.M.; Otten, J.J.; Towfighi, A.; Wylie-Rosett, J. Low-calorie sweetened beverages and cardiometabolic health: A science advisory from the american heart association. Circulation 2018, 138, e126–e140. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Raychaudhuri, U.; Chakraborty, R. Artificial sweeteners–A review. J. Food Sci. Technol. 2014, 51, 611–621. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Additional Information about High-Intensity Sweeteners Permitted for Use in Food in the United States; US Food and Drug Administration: Silver Spring, MD, USA, 2018.
- Perrier, J.D.; Mihalov, J.J.; Carlson, S.J. FDA regulatory approach to steviol glycosides. Food Chem. Toxicol. 2018, 122, 132–142. [Google Scholar] [CrossRef]
- Ruiz-Ojeda, F.J.; Plaza-Díaz, J.; Sáez-Lara, M.J.; Gil, A. Effects of sweeteners on the gut microbiota: A review of experimental studies and clinical trials. Adv. Nutr. 2019, 10, S31–S48. [Google Scholar] [CrossRef]
- Godswill, A.C. Sugar alcohols: Chemistry, production, health concerns and nutritional importance of mannitol, sorbitol, xylitol, and erythritol. Int. J. Adv. Acad. Res. 2017, 3, 32–66. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Galant, A.L.; Kaufman, R.C.; Wilson, J.D. Glucose: Detection and analysis. Food Chem. 2015, 188, 149–160. [Google Scholar] [CrossRef]
- Deibert, P.; Konig, D.; Kloock, B.; Groenefeld, M.; Berg, A. Glycaemic and insulinaemic properties of some German honey varieties. Eur. J. Clin. Nutr. 2010, 64, 762–764. [Google Scholar] [CrossRef]
- Chareoansiri, R.; Kongkachuichai, R. Sugar profiles and soluble and insoluble dietary fiber contents of fruits in Thailand markets. Int. J. Food Sci. Nutr. 2009, 60 (Suppl. 4), 126–139. [Google Scholar] [CrossRef]
- Blanco, A.; Blanco, G. Chapter 14—Carbohydrate metabolism. In Medical Biochemistry; Blanco, A., Blanco, G., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 283–323. [Google Scholar]
- Borg, M.J.; Jones, K.L.; Sun, Z.; Horowitz, M.; Rayner, C.K.; Wu, T. Metformin attenuates the postprandial fall in blood pressure in type 2 diabetes. Diabetes Obes. Metab. 2019, 21, 1251–1254. [Google Scholar] [CrossRef]
- Brown, C.M.; Dulloo, A.G.; Yepuri, G.; Montani, J.P. Fructose ingestion acutely elevates blood pressure in healthy young humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 294, R730–R737. [Google Scholar] [CrossRef]
- Grasser, E.K.; Dulloo, A.; Montani, J.P. Cardiovascular responses to the ingestion of sugary drinks using a randomised cross-over study design: Does glucose attenuate the blood pressure-elevating effect of fructose? Br. J. Nutr. 2014, 112, 183–192. [Google Scholar] [CrossRef]
- Jansen, R.W.M.M.; Penterman, B.J.M.; Van Lier, H.J.J.; Hoefnagels, W.H.L. Blood pressure reduction after oral glucose loading and its relation to age, blood pressure and insulin. Am. J. Cardiol. 1987, 60, 1087–1091. [Google Scholar] [CrossRef]
- Jones, K.L.; O’Donovan, D.; Russo, A.; Meyer, J.H.; Stevens, J.E.; Lei, Y.; Keogh, J.; Tonkin, A.; Horowitz, M. Effects of drink volume and glucose load on gastric emptying and postprandial blood pressure in healthy older subjects. Am. J. Physiol. Gastrointest. Liver Physiol. 2005, 289, G240–G248. [Google Scholar] [CrossRef]
- Mathias, C.J.; da Costa, D.F.; McIntosh, C.M.; Fosbraey, P.; Bannister, R.; Wood, S.M.; Bloom, S.R.; Christensen, N.J. Differential blood pressure and hormonal effects after glucose and xylose ingestion in chronic autonomic failure. Clin. Sci. 1989, 77, 85–92. [Google Scholar] [CrossRef]
- Nguyen, T.A.N.; Ali Abdelhamid, Y.; Weinel, L.M.; Hatzinikolas, S.; Kar, P.; Summers, M.J.; Phillips, L.K.; Horowitz, M.; Jones, K.L.; Deane, A.M. Postprandial hypotension in older survivors of critical illness. J. Crit. Care 2018, 45, 20–26. [Google Scholar] [CrossRef]
- Robinson, B.J.; Stowell, L.I.; Purdie, G.L.; Palmer, K.T.; Johnson, R.H. Autonomic responses to carbohydrate ingestion and head-up tilt in elderly subjects with orthostatic hypotension. Clin. Auton. Res. 1992, 2, 309–316. [Google Scholar] [CrossRef]
- Trahair, L.G.; Horowitz, M.; Jones, K.L. Postprandial hypotension is associated with more rapid gastric emptying in healthy older individuals. J. Am. Med. Dir. Assoc. 2015, 16, 521–523. [Google Scholar] [CrossRef]
- Trahair, L.G.; Kimber, T.E.; Flabouris, K.; Horowitz, M.; Jones, K.L. Gastric emptying, postprandial blood pressure, glycaemia and splanchnic flow in Parkinson’s disease. World J. Gastroenterol. 2016, 22, 4860–4867. [Google Scholar] [CrossRef]
- Trahair, L.G.; Rajendran, S.; Visvanathan, R.; Chapman, M.; Stadler, D.; Horowitz, M.; Jones, K.L. Comparative effects of glucose and water drinks on blood pressure and cardiac function in older subjects with and without postprandial hypotension. Physiol. Rep. 2017, 5, e13341. [Google Scholar] [CrossRef]
- Vanis, L.; Hausken, T.; Gentilcore, D.; Rigda, R.S.; Rayner, C.K.; Feinle-Bisset, C.; Horowitz, M.; Jones, K.L. Comparative effects of glucose and xylose on blood pressure, gastric emptying and incretin hormones in healthy older subjects. Br. J. Nutr. 2011, 105, 1644–1651. [Google Scholar] [CrossRef]
- Visvanathan, R.; Chen, R.; Garcia, M.; Horowitz, M.; Chapman, I. The effects of drinks made from simple sugars on blood pressure in healthy older people. Br. J. Nutr. 2005, 93, 575–579. [Google Scholar] [CrossRef]
- Edwards, B.J.; Perry, H.M., 3rd; Kaiser, F.E.; Morley, J.E.; Kraenzle, D.; Stevenson, R.; Kreutter, D. Relationship of age and calcitonin gene-related peptide to postprandial hypotension. Mech. Ageing Dev. 1996, 87, 61–73. [Google Scholar] [CrossRef]
- Fagius, J.; Berne, C. Increase in muscle nerve sympathetic activity in humans after food intake. Clin. Sci. 1994, 86, 159–167. [Google Scholar] [CrossRef]
- Fagius, J.; Ellerfelt, K.; Lithell, H.; Berne, C. Increase in muscle nerve sympathetic activity after glucose intake is blunted in the elderly. Clin. Auton. Res. 1996, 6, 195–203. [Google Scholar] [CrossRef]
- Gentilcore, D.; Nair, N.S.; Vanis, L.; Rayner, C.K.; Meyer, J.H.; Hausken, T.; Horowitz, M.; Jones, K.L. Comparative effects of oral and intraduodenal glucose on blood pressure, heart rate, and splanchnic blood flow in healthy older subjects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 297, R716–R722. [Google Scholar] [CrossRef]
- Heseltine, D.; Dakkak, M.; Woodhouse, K.; Macdonald, I.A.; Potter, J.F. The effect of caffeine on postprandial hypotension in the elderly. J. Am. Geriatr. Soc. 1991, 39, 160–164. [Google Scholar] [CrossRef]
- Hirayama, M.; Watanabe, H.; Koike, Y.; Hasegawa, Y.; Kanaoke, Y.; Sakurai, N.; Hakusui, S.; Takahashi, A. Postprandial hypotension: Hemodynamic differences between multiple system atrophy and peripheral autonomic neuropathy. J. Auton. Nerv. Syst. 1993, 43. [Google Scholar] [CrossRef]
- Hirayama, M.; Watanabe, H.; Koike, Y.; Kaneoke, Y.; Sakurai, N.; Hakusui, S.; Takahashi, A. Treatment of postprandial hypotension with selective alpha 1 and beta 1 adrenergic agonists. J. Auton. Nerv. Syst. 1993, 45, 149–154. [Google Scholar] [CrossRef]
- Hoeldtke, R.D.; Dworkin, G.E.; Gaspar, S.R.; Israel, B.C.; Boden, G. Effect of the somatostatin analogue SMS-201–995 on the adrenergic response to glucose ingestion in patients with postprandial hypotension. Am. J. Med. 1989, 86, 673–677. [Google Scholar] [CrossRef]
- Jansen, R.W.; van Lier, H.J.; Hoefnagels, W.H. Effects of nitrendipine and hydrochlorothiazide on postprandial blood pressure reduction and carbohydrate metabolism in hypertensive patients over 70 years of age. J. Cardiovasc. Pharmacol. 1988, 12 (Suppl. 4), S59–S63. [Google Scholar] [CrossRef]
- Jansen, R.W.; Peeters, T.L.; Lenders, J.W.; van Lier, H.J.; V’T Laar, A.; Hoefnagels, W.H. Somatostatin analog octreotide (SMS 201–995) prevents the decrease in blood pressure after oral glucose loading in the elderly. J. Clin. Endocrinol. Metab. 1989, 68, 752–756. [Google Scholar] [CrossRef]
- Jansen, R.W.; de Meijer, P.H.; van Lier, H.J.; Hoefnagels, W.H. Influence of octreotide (SMS 201–995) and insulin administration on the course of blood pressure after an oral glucose load in hypertensive elderly subjects. J. Am. Geriatr. Soc. 1989, 37, 1135–1139. [Google Scholar] [CrossRef]
- Jansen, R.W.M.M.; Hoefnagels, W.H.L. The Influence of oral glucose loading on baroreflex function in the elderly. J. Am. Geriatr. Soc. 1989, 37, 1017–1022. [Google Scholar] [CrossRef]
- Jones, K.L.; MacIntosh, C.; Su, Y.C.; Wells, F.; Chapman, I.M.; Tonkin, A.; Horowitz, M. Guar gum reduces postprandial hypotension in older people. J. Am. Geriatr. Soc. 2001, 49, 162–167. [Google Scholar] [CrossRef]
- Jones, K.L.; Rigda, R.S.; Buttfield, M.D.M.; Hatzinikolas, S.; Pham, H.T.; Marathe, C.S.; Wu, T.; Lange, K.; Trahair, L.G.; Rayner, C.K.; et al. Effects of lixisenatide on postprandial blood pressure, gastric emptying and glycaemia in healthy people and people with type 2 diabetes. Diabetes Obes. Metab. 2019. [Google Scholar] [CrossRef]
- Maruta, T.; Komai, K.; Takamori, M.; Yamada, M. Voglibose inhibits postprandial hypotension in neurologic disorders and elderly people. Neurology 2006, 66, 1432–1434. [Google Scholar] [CrossRef]
- Masuo, K.; Mikami, H.; Ogihara, T.; Tuck, M.L. Mechanisms mediating postprandial blood pressure reduction in young and elderly subjects. Am. J. Hypertens. 1996, 9, 536–544. [Google Scholar] [CrossRef][Green Version]
- Nair, S.; Visvanathan, R.; Gentilcore, D. Intermittent walking: A potential treatment for older people with postprandial hypotension. J. Am. Med. Dir. Assoc. 2015, 16, 160–164. [Google Scholar] [CrossRef]
- Nair, S.; Visvanathan, R.; Piscitelli, D. Effects of postprandial blood pressure on gait parameters in older people. Nutrients 2016, 8, 219. [Google Scholar] [CrossRef]
- Sasaki, E.; Kitaoka, H.; Ohsawa, N. Postprandial hypotension in patients with non-insulin-dependent diabetes mellitus. Diabetes Res. Clin. Pract. 1992, 18, 113–121. [Google Scholar] [CrossRef]
- Takamori, M.; Hirayama, M.; Kobayashi, R.; Ito, H.; Mabuchi, N.; Nakamura, T.; Hori, N.; Koike, Y.; Sobue, G. Altered venous capacitance as a cause of postprandial hypotension in multiple system atrophy. Clin. Auton. Res. 2007, 17, 20–25. [Google Scholar] [CrossRef]
- Umehara, T.; Toyoda, C.; Oka, H. Postprandial hypotension in de novo Parkinson’s disease: A comparison with orthostatic hypotension. Parkinsonism Relat. Disord. 2014, 20, 573–577. [Google Scholar] [CrossRef]
- Umehara, T.; Nakahara, A.; Matsuno, H.; Toyoda, C.; Oka, H. Predictors of postprandial hypotension in elderly patients with de novo Parkinson’s disease. J. Neural. Transm. 2016, 123, 1331–1339. [Google Scholar] [CrossRef]
- Visvanathan, R.; Horowitz, M.; Chapman, I. The hypotensive response to oral fat is comparable but slower compared with carbohydrate in healthy elderly subjects. Br. J. Nutr. 2006, 95, 340–345. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gentilcore, D.; Doran, S.; Meyer, J.H.; Horowitz, M.; Jones, K.L. Effects of intraduodenal glucose concentration on blood pressure and heart rate in healthy older subjects. Dig. Dis. Sci. 2006, 51, 652–656. [Google Scholar] [CrossRef] [PubMed]
- Gentilcore, D.; Meyer, J.H.; Rayner, C.K.; Horowitz, M.; Jones, K.L. Gastric distension attenuates the hypotensive effect of intraduodenal glucose in healthy older subjects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 295, R472–R477. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marathe, C.S.; Horowitz, M.; Trahair, L.G.; Bound, M.; Checklin, H.; Lange, K.; Rayner, C.K.; Jones, K.L. Effect of duodenal glucose load on blood pressure in type 2 diabetes. Diabetes Res. Clin. Pract. 2016, 113, 38–40. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, D.; Feinle, C.; Tonkin, A.; Horowitz, M.; Jones, K.L. Postprandial hypotension in response to duodenal glucose delivery in healthy older subjects. J. Physiol. 2002, 540, 673–679. [Google Scholar] [CrossRef]
- Pham, H.T.; Stevens, J.E.; Rigda, R.S.; Phillips, L.K.; Wu, T.; Hausken, T.; Soenen, S.; Visvanathan, R.; Rayner, C.K.; Horowitz, M.; et al. Effects of intraduodenal administration of the artificial sweetener sucralose on blood pressure and superior mesenteric artery blood flow in healthy older subjects. Am. J. Clin. Nutr. 2018, 108, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Trahair, L.G.; Vanis, L.; Gentilcore, D.; Lange, K.; Rayner, C.K.; Horowitz, M.; Jones, K.L. Effects of variations in duodenal glucose load on blood pressure, heart rate, superior mesenteric artery blood flow and plasma noradrenaline in healthy young and older subjects. Clin. Sci. 2012, 122, 271–279. [Google Scholar] [CrossRef]
- Trahair, L.G.; Wu, T.; Feinle-Bisset, C.; Marathe, C.S.; Rayner, C.K.; Horowitz, M.; Jones, K.L. Comparative effects of small intestinal glucose on blood pressure, heart rate, and noradrenaline responses in obese and healthy subjects. Physiol. Rep. 2018, 6. [Google Scholar] [CrossRef]
- Van Orshoven, N.P.; van Schelven, L.J.; Akkermans, L.M.; Jansen, P.A.; Horowitz, M.; Feinle-Bisset, C.; van Huffelen, A.C.; Oey, P.L. The effect of intraduodenal glucose on muscle sympathetic nerve activity in healthy young and older subjects. Clin. Auton. Res. 2008, 18, 28–35. [Google Scholar] [CrossRef]
- Vanis, L.; Gentilcore, D.; Rayner, C.K.; Wishart, J.M.; Horowitz, M.; Feinle-Bisset, C.; Jones, K.L. Effects of small intestinal glucose load on blood pressure, splanchnic blood flow, glycemia, and GLP-1 release in healthy older subjects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011, 300, R1524–R1531. [Google Scholar] [CrossRef]
- Gentilcore, D.; Little, T.J.; Feinle-Bisset, C.; Samsom, M.; Smout, A.J.; Horowitz, M.; Jones, K.L. Role of 5-hydroxytryptamine mechanisms in mediating the effects of small intestinal glucose on blood pressure and antropyloroduodenal motility in older subjects. Am. J. Physiol. Gastrointest. Liver Physiol. 2007, 293, G692–G698. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, D.; Feinle-Bisset, C.; Chong, C.; Cameron, A.; Tonkin, A.; Wishart, J.; Horowitz, M.; Jones, K.L. Intraduodenal guar attenuates the fall in blood pressure induced by glucose in healthy older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Thazhath, S.S.; Marathe, C.S.; Wu, T.; Chang, J.; Khoo, J.; Kuo, P.; Checklin, H.L.; Bound, M.J.; Rigda, R.S.; Horowitz, M.; et al. Acute effects of the glucagon-like peptide-1 receptor agonist, exenatide, on blood pressure and heart rate responses to intraduodenal glucose infusion in type 2 diabetes. Diabetes Vasc. Dis. Res. 2017, 14, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Vanis, L.; Gentilcore, D.; Hausken, T.; Pilichiewicz, A.N.; Lange, K.; Rayner, C.K.; Feinle-Bisset, C.; Meyer, J.H.; Horowitz, M.; Jones, K.L. Effects of gastric distension on blood pressure and superior mesenteric artery blood flow responses to intraduodenal glucose in healthy older subjects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 299, R960–R967. [Google Scholar] [CrossRef] [PubMed]
- Vanis, L.; Gentilcore, D.; Lange, K.; Gilja, O.H.; Rigda, R.S.; Trahair, L.G.; Feinle-Bisset, C.; Rayner, C.K.; Horowitz, M.; Jones, K.L. Effects of variations in intragastric volume on blood pressure and splanchnic blood flow during intraduodenal glucose infusion in healthy older subjects. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2012, 302, R391–R399. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Trahair, L.G.; Little, T.J.; Bound, M.J.; Zhang, X.; Wu, H.; Sun, Z.; Horowitz, M.; Rayner, C.K.; Jones, K.L. Effects of vildagliptin and metformin on blood pressure and heart rate responses to small intestinal glucose in type 2 diabetes. Diabetes Care 2017, 40, 702–705. [Google Scholar] [CrossRef] [PubMed]
- Charriere, N.; Loonam, C.; Montani, J.P.; Dulloo, A.G.; Grasser, E.K. Cardiovascular responses to sugary drinks in humans: Galactose presents milder cardiac effects than glucose or fructose. Eur. J. Nutr. 2017, 56, 2105–2113. [Google Scholar] [CrossRef][Green Version]
- Brener, W.; Hendrix, T.R.; McHugh, P.R. Regulation of the gastric emptying of glucose. Gastroenterology 1983, 85, 76–82. [Google Scholar]
- Trahair, L.G.; Horowitz, M.; Rayner, C.K.; Gentilcore, D.; Lange, K.; Wishart, J.M.; Jones, K.L. Comparative effects of variations in duodenal glucose load on glycemic, insulinemic, and incretin responses in healthy young and older subjects. J. Clin. Endocrinol. Metab. 2012, 97, 844–851. [Google Scholar] [CrossRef]
- Hanover, L.M.; White, J.S. Manufacturing, composition, and applications of fructose. Am. J. Clin. Nutr. 1993, 58, 724S–732S. [Google Scholar] [CrossRef]
- Guss, J.L.; Kissileff, H.R.; Pi-Sunyer, F.X. Effects of glucose and fructose solutions on food intake and gastric emptying in nonobese women. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1994, 267, R1537–R1544. [Google Scholar] [CrossRef] [PubMed]
- Teff, K.L.; Elliott, S.S.; Tschop, M.; Kieffer, T.J.; Rader, D.; Heiman, M.; Townsend, R.R.; Keim, N.L.; D’Alessio, D.; Havel, P.J. Dietary fructose reduces circulating insulin and leptin, attenuates postprandial suppression of ghrelin, and increases triglycerides in women. J. Clin. Endocrinol. Metab. 2004, 89, 2963–2972. [Google Scholar] [CrossRef] [PubMed]
- Yandell, R.; Baker, B.; Wittert, G.; Wishart, J.; Morris, H.; Horowitz, M.; Chapman, I. Glycemic, hormone, and appetite responses to monosaccharide ingestion in patients with type 2 diabetes. Metabolism 2002, 51, 949–957. [Google Scholar]
- Gerrits, P.M.; Tsalikian, E. Diabetes and fructose metabolism. Am. J. Clin. Nutr. 1993, 58, 796S–799S. [Google Scholar] [CrossRef] [PubMed]
- Hallfrisch, J.; Ellwood, K.C.; Michaelis, O.E.T.; Reiser, S.; O’Dorisio, T.M.; Prather, E.S. Effects of dietary fructose on plasma glucose and hormone responses in normal and hyperinsulinemic men. J. Nutr. 1983, 113, 1819–1826. [Google Scholar] [CrossRef]
- Feinman, R.D.; Fine, E.J. Fructose in perspective. Nutr. Metab. 2013, 10, 45. [Google Scholar] [CrossRef] [PubMed]
- Ter Horst, K.W.; Serlie, M.J. Fructose consumption, lipogenesis, and non-alcoholic fatty liver disease. Nutrients 2017, 9, 981. [Google Scholar] [CrossRef]
- Wolfsdorf, J.I.; Garvey, K.C. Chapter 49—Management of diabetes in children. In Endocrinology: Adult and Pediatric, 7th ed.; Jameson, J.L., De Groot, L.J., de Kretser, D.M., Giudice, L.C., Grossman, A.B., Melmed, S., Potts, J.T., Weir, G.C., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2016; pp. 854–882. [Google Scholar]
- Sun, S.Z.; Empie, M.W. Fructose metabolism in humans—What isotopic tracer studies tell us. Nutr. Metab. 2012, 9, 89. [Google Scholar] [CrossRef]
- Hallfrisch, J. Metabolic effects of dietary fructose. FASEB J. 1990, 4, 2652–2660. [Google Scholar] [CrossRef]
- Mooradian, A.D.; Smith, M.; Tokuda, M. The role of artificial and natural sweeteners in reducing the consumption of table sugar: A narrative review. Clin. Nutr. ESPEN 2017, 18. [Google Scholar] [CrossRef]
- Gallagher, C.; Keogh, J.B.; Pedersen, E.; Clifton, P.M. Fructose acute effects on glucose, insulin, and triglyceride after a solid meal compared with sucralose and sucrose in a randomized crossover study. Am. J. Clin. Nutr. 2016, 103, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Gentilcore, D.; Bryant, B.; Wishart, J.M.; Morris, H.A.; Horowitz, M.; Jones, K.L. Acarbose attenuates the hypotensive response to sucrose and slows gastric emptying in the elderly. Am. J. Med. 2005, 118, 1289.e5–1289.e11. [Google Scholar] [CrossRef] [PubMed]
- Gentilcore, D.; Vanis, L.; Wishart, J.M.; Rayner, C.K.; Horowitz, M.; Jones, K.L. The alpha (α)-glucosidase inhibitor, acarbose, attenuates the blood pressure and splanchnic blood flow responses to intraduodenal sucrose in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Teunissen-Beekman, K.F.; Dopheide, J.; Geleijnse, J.M.; Bakker, S.J.; Brink, E.J.; de Leeuw, P.W.; Serroyen, J.; van Baak, M.A. Differential effects of proteins and carbohydrates on postprandial blood pressure-related responses. Br. J. Nutr. 2014, 112, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Goldfein, K.R.; Slavin, J.L. Why sugar is added to food: Food science 101. Compr. Rev. Food Sci. Food Saf. 2015, 14, 644–656. [Google Scholar] [CrossRef]
- Robayo-Torres, C.C.; Quezada-Calvillo, R.; Nichols, B.L. Disaccharide digestion: Clinical and molecular aspects. Clin. Gastroenterol. Hepatol. 2006, 4, 276–287. [Google Scholar] [CrossRef]
- Monnard, C.R.; Grasser, E.K. Perspective: Cardiovascular responses to sugar-sweetened beverages in humans: A narrative review with potential hemodynamic mechanisms. Adv. Nutr. 2018, 9, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Breuer, H.W. Review of acarbose therapeutic strategies in the long-term treatment and in the prevention of type 2 diabetes. Int. J. Clin. Pharmacol. Ther. 2003, 41, 421–440. [Google Scholar] [CrossRef]
- Qualmann, C.; Nauck, M.A.; Holst, J.J.; Orskov, C.; Creutzfeldt, W. Glucagon-like peptide 1 (7–36 amide) secretion in response to luminal sucrose from the upper and lower gut. A study using alpha-glucosidase inhibition (acarbose). Scand. J. Gastroenterol. 1995, 30, 892–896. [Google Scholar] [CrossRef]
- Enç, F.Y.; Akin, L.; Turoğlu, T.; Dede, F.; Haklar, G.; Beki, N.; Yeğen, B.; Rehfeld, J.F.; Holst, J.J. Inhibition of gastric emptying by acarbose is correlated with GLP-1 response and accompanied by CCK release. Am. J. Physiol. Gastrointest. Liver Physiol. 2001, 281, G752–G763. [Google Scholar] [CrossRef]
- Fordtran, J.S.; Soergel, K.H.; Ingelfinger, F.J. Intestinal absorption of d-xylose in man. N. Engl. J. Med. 1962, 267, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Nair, N.U.; Zhao, H. Selective reduction of xylose to xylitol from a mixture of hemicellulosic sugars. Metab. Eng. 2010, 12, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Yoshitake, J.; Ohiwa, H.; Shimamura, M.; Imai, T. Production of polyalcohol by a corynebacterium sp. Agric. Biol. Chem. 1971, 35, 905–911. [Google Scholar] [CrossRef][Green Version]
- Wolnerhanssen, B.K.; Cajacob, L.; Keller, N.; Doody, A.; Rehfeld, J.F.; Drewe, J.; Peterli, R.; Beglinger, C.; Meyer-Gerspach, A.C. Gut hormone secretion, gastric emptying, and glycemic responses to erythritol and xylitol in lean and obese subjects. Am. J. Physiol. Endocrinol. Metab. 2016, 310, E1053–E1061. [Google Scholar] [CrossRef] [PubMed]
- Salminen, E.K.; Salminen, S.J.; Porkka, L.; Kwasowski, P.; Marks, V.; Koivistoinen, P.E. Xylitol vs glucose: effect on the rate of gastric emptying and motilin, insulin, and gastric inhibitory polypeptide release. Am. J. Clin. Nutr. 1989, 49, 1228–1232. [Google Scholar] [CrossRef] [PubMed]
- Noda, K.; Nakayama, K.; Oku, T. Serum glucose and insulin levels and erythritol balance after oral administration of erythritol in healthy subjects. Eur. J. Clin. Nutr. 1994, 48, 286–292. [Google Scholar]
- De Cock, P. Erythritol. In Sweeteners and Sugar Alternatives in Food Technology; John Wiley & Sons: Hoboken, NJ, USA, 2012; pp. 213–241. [Google Scholar]
- Flint, N.; Hamburg, N.M.; Holbrook, M.; Dorsey, P.G.; LeLeiko, R.M.; Berger, A.; de Cock, P.; Bosscher, D.; Vita, J.A. Effects of erythritol on endothelial function in patients with type 2 diabetes mellitus: A pilot study. Acta Diabetol. 2014, 51, 513–516. [Google Scholar] [CrossRef][Green Version]
- Engelking, L.R. Chapter 18—Carbohydrate structure. In Textbook of Veterinary Physiological Chemistry, 3rd ed.; Engelking, L.R., Ed.; Academic Press: Boston, MA, USA, 2015; pp. 118–123. [Google Scholar]
- Hofman, D.L.; van Buul, V.J.; Brouns, F.J.P.H. Nutrition, health, and regulatory aspects of digestible maltodextrins. Crit. Rev. Food Sci. Nutr. 2016, 56, 2091–2100. [Google Scholar] [CrossRef]
- Lavin, J.H.; French, S.J.; Read, N.W. Comparison of oral and gastric administration of sucrose and maltose on gastric emptying rate and appetite. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 80–86. [Google Scholar] [CrossRef]
- Murray, R.; Eddy, D.E.; Bartoli, W.P.; Paul, G.L. Gastric emptying of water and isocaloric carbohydrate solutions consumed at rest. Med. Sci. Sports Exerc. 1994, 26, 725–732. [Google Scholar] [CrossRef]
- Shankar, P.; Ahuja, S.; Sriram, K. Non-nutritive sweeteners: Review and update. Nutrition 2013, 29, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Police, S.B.; Harris, J.C.; Lodder, R.A.; Cassis, L.A. Effect of diets containing sucrose vs. D-tagatose in hypercholesterolemic mice. Obesity 2009, 17, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Chikkerur, J.; Roy, S.C.; Dhali, A.; Kolte, A.P.; Sridhar, M.; Samanta, A.K. Tagatose as a potential nutraceutical: Production, properties, biological roles, and applications. J. Food Sci. 2018, 83, 2699–2709. [Google Scholar] [CrossRef] [PubMed]
- Donner, T.W.; Wilber, J.F.; Ostrowski, D. D-tagatose, a novel hexose: Acute effects on carbohydrate tolerance in subjects with and without type 2 diabetes. Diabetes Obes. Metab. 1999, 1, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Ensor, M.; Williams, J.; Smith, R.; Banfield, A.; Lodder, R.A. Effects of three low-doses of D-tagatose on glycemic control over six months in subjects with mild type 2 diabetes mellitus under control with diet and exercise. J. Endocrinol. Diabetes Obes. 2014, 2, 1057. [Google Scholar] [PubMed]
- Lu, Y.; Levin, G.V.; Donner, T.W. Tagatose, a new antidiabetic and obesity control drug. Diabetes Obes. Metab. 2008, 10, 109–134. [Google Scholar] [CrossRef] [PubMed]
- Ensor, M.; Banfield, A.B.; Smith, R.R.; Williams, J.; Lodder, R.A. Safety and efficacy of D-tagatose in glycemic control in subjects with type 2 diabetes. J. Endocrinol. Diabetes Obes. 2015, 3, 1065. [Google Scholar]
- Little, T.J.; Gopinath, A.; Patel, E.; McGlone, A.; Lassman, D.J.; D’Amato, M.; McLaughlin, J.T.; Thompson, D.G. Gastric emptying of hexose sugars: Role of osmolality, molecular structure and the CCK(1) receptor. Neurogastroenterol. Motil. 2010, 22, 1183–1190.e314. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Zhao, B.R.; Bound, M.J.; Checklin, H.L.; Bellon, M.; Little, T.J.; Young, R.L.; Jones, K.L.; Horowitz, M.; Rayner, C.K. Effects of different sweet preloads on incretin hormone secretion, gastric emptying, and postprandial glycemia in healthy humans. Am. J. Clin. Nutr. 2012, 95, 78–83. [Google Scholar] [CrossRef]
- Hough, L. Sucrose, sweetness, and sucralose. Int. Sugar J. 1989, 91, 23–37. [Google Scholar]
- John, B.A.; Wood, S.G.; Hawkins, D.R. The pharmacokinetics and metabolism of sucralose in the mouse. Food Chem. Toxicol. 2000, 38 (Suppl. 2), S107–S110. [Google Scholar] [CrossRef]
- Wood, S.G.; John, B.A.; Hawkins, D.R. The pharmacokinetics and metabolism of sucralose in the dog. Food Chem. Toxicol. 2000, 38 (Suppl. 2), S99–S106. [Google Scholar] [CrossRef]
- Roberts, A.; Renwick, A.G.; Sims, J.; Snodin, D.J. Sucralose metabolism and pharmacokinetics in man. Food Chem. Toxicol. 2000, 38 (Suppl. 2), S31–S41. [Google Scholar] [CrossRef]
- Ma, J.; Bellon, M.; Wishart, J.M.; Young, R.; Blackshaw, L.A.; Jones, K.L.; Horowitz, M.; Rayner, C.K. Effect of the artificial sweetener, sucralose, on gastric emptying and incretin hormone release in healthy subjects. Am. J. Physiol. Gastrointest. Liver Physiol. 2009, 296, G735–G739. [Google Scholar] [CrossRef]
- Kazmi, S.A.J.; Khan, A.N.; Naqib, M.; Munir, T.A. Comparison of acute effects of sucralose, aspartame and acesulfame potassium on pulse, blood pressure, and blood glucose levels in young healthy adults. World J. Pharm. Pharm. Sci. 2017, 7, 60–69. [Google Scholar]
- Wu, T.; Bound, M.J.; Standfield, S.D.; Bellon, M.; Young, R.L.; Jones, K.L.; Horowitz, M.; Rayner, C.K. Artificial sweeteners have no effect on gastric emptying, glucagon-like peptide-1, or glycemia after oral glucose in healthy humans. Diabetes Care 2013, 36, e202–e203. [Google Scholar] [CrossRef]
- Brown, R.J.; Walter, M.; Rother, K.I. Ingestion of diet soda before a glucose load augments glucagon-like peptide-1 secretion. Diabetes Care 2009, 32, 2184–2186. [Google Scholar] [CrossRef]
- Steinert, R.E.; Frey, F.; Töpfer, A.; Drewe, J.; Beglinger, C. Effects of carbohydrate sugars and artificial sweeteners on appetite and the secretion of gastrointestinal satiety peptides. Br. J. Nutr. 2011, 105, 1320–1328. [Google Scholar] [CrossRef]
- Little, T.J.; Gupta, N.; Case, R.M.; Thompson, D.G.; McLaughlin, J.T. Sweetness and bitterness taste of meals per se does not mediate gastric emptying in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 297, R632–R639. [Google Scholar] [CrossRef]
- Samuel, P.; Ayoob, K.T.; Magnuson, B.A.; Wölwer-Rieck, U.; Jeppesen, P.B.; Rogers, P.J.; Rowland, I.; Mathews, R. Stevia leaf to stevia sweetener: Exploring its science, benefits, and future potential. J. Nutr. 2018, 148, 1186S–1205S. [Google Scholar] [CrossRef]
- Jorge, K. SOFT DRINKS|Chemical Composition. In Encyclopedia of Food Sciences and Nutrition, 2nd ed.; Caballero, B., Ed.; Academic Press: Oxford, NY, USA, 2003; pp. 5346–5352. [Google Scholar]
- Anton, S.D.; Martin, C.K.; Han, H.; Coulon, S.; Cefalu, W.T.; Geiselman, P.; Williamson, D.A. Effects of stevia, aspartame, and sucrose on food intake, satiety, and postprandial glucose and insulin levels. Appetite 2010, 55, 37–43. [Google Scholar] [CrossRef]
- Gregersen, S.; Jeppesen, P.B.; Holst, J.J.; Hermansen, K. Antihyperglycemic effects of stevioside in type 2 diabetic subjects. Metabolism 2004, 53, 73–76. [Google Scholar] [CrossRef]
- Pereira, R.M.; Secaf, M.; de Oliveira, R.B. Effects of different sweeteners on incretin hormone secretion, gastric emptying, intragastric distribution and postprandial glycemia in healthy humans. FASEB J. 2013, 27, 1160–1161. [Google Scholar] [CrossRef]
- Hsieh, M.H.; Chan, P.; Sue, Y.M.; Liu, J.C.; Liang, T.H.; Huang, T.Y.; Tomlinson, B.; Chow, M.S.; Kao, P.F.; Chen, Y.J. Efficacy and tolerability of oral stevioside in patients with mild essential hypertension: A two-year, randomized, placebo-controlled study. Clin. Ther. 2003, 25, 2797–2808. [Google Scholar] [CrossRef]
- Chan, P.; Tomlinson, B.; Chen, Y.J.; Liu, J.C.; Hsieh, M.H.; Cheng, J.T. A double-blind placebo-controlled study of the effectiveness and tolerability of oral stevioside in human hypertension. Br. J. Clin. Pharmacol. 2000, 50, 215–220. [Google Scholar] [CrossRef]
- Maki, K.C.; Curry, L.L.; Carakostas, M.C.; Tarka, S.M.; Reeves, M.S.; Farmer, M.V.; McKenney, J.M.; Toth, P.D.; Schwartz, S.L.; Lubin, B.C.; et al. The hemodynamic effects of rebaudioside A in healthy adults with normal and low-normal blood pressure. Food Chem. Toxicol. 2008, 46, S40–S46. [Google Scholar] [CrossRef]
- Barriocanal, L.A.; Palacios, M.; Benitez, G.; Benitez, S.; Jimenez, J.T.; Jimenez, N.; Rojas, V. Apparent lack of pharmacological effect of steviol glycosides used as sweeteners in humans. A pilot study of repeated exposures in some normotensive and hypotensive individuals and in Type 1 and Type 2 diabetics. Regul. Toxicol. Pharmacol. 2008, 51, 37–41. [Google Scholar] [CrossRef]
- O’Brien-Nabors, L. Alternative Sweeteners; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Khan, R.; Aroulmoji, V. Low calorie high-intensity sweeteners. Int. J. Adv. Sci. Eng. 2018, 5, 934–947. [Google Scholar] [CrossRef]


| Study | Year | Participant Characteristics | Study Design | Test Meal | Effects on Blood Pressure |
|---|---|---|---|---|---|
| Borg et al. [38] | 2019 | 10 diet controlled T2DM patients, 5M:5F, aged 65.6 ± 3.1 years | Randomized crossover study | ID metformin (1 g) or saline (control) 60 min before ingesting a 50 g glucose drink labelled with 150 mg 13C-acetate. | SBP and DBP decreased following oral glucose on both days. The fall in SBP was less after metformin than control. |
| Brown et al. [39] | 2008 | 15 healthy normal-weight participants, 9M:6F, aged 24 ± 1 years | Randomized crossover study | 500 mL of either water, 60 g glucose, or 60 g fructose. | Oral fructose, but not glucose, significantly increased SBP and DBP. The maximum rise in SBP after fructose was 6.2 ± 0.8 mmHg. |
| Charriere et al. [89] | 2017 | 9 young healthy men, aged 24 ± 1 years | Randomized crossover study | 500 mL of water containing 60 g of either glucose, fructose or galactose. | The increase in SBP after fructose (7–8 mmHg) was greater than after glucose (4–5 mmHg) or galactose (2–3 mmHg). DBP increased to a greater extent with fructose (~5 mmHg), compared to non-significant increases of only 2–3 mmHg after glucose or galactose. |
| Edwards et al. [51] | 1996 | 10 young (20–40 years), 9 middle-aged (41–50 years), and 10 old (61–83 years) participants | Non-randomized study | 75 g glucose in 300 mL water | SBP decrease was significant in both the older groups. A fall in SBP > 15 mmHg observed in 5 individuals; 4 aged >60 years and 1 middle aged. |
| Fagius et al. [52] | 1994 | 39 participants in 5 groups: glucose (n = 8, 4M:4F, mean age 25.8 years), fat (n = 8, 5M:3F, mean age 25.5 years), protein (n = 8, 5M:3F, mean age 25.6 years), mixed meal (n = 8, 6M:2F, mean age 26.2 years) or water (n = 7, 4M:3F, mean age 24.9 years). | Parallel study | 100 g glucose in 300 mL of water (n = 8), 50 g fat in 250 mL of water (n = 8), 100 g lean meat (40 g protein) with 250 mL water (n = 8), 300 mL water alone (n = 7) or a mixed meal (n = 8). | Small and sometimes significant increases in BP occurred during the sessions. |
| Fagius et al. [53] | 1996 | 3 groups—A: 9 young healthy, 5M:4F, aged 26.2 ± 2.8 years; B: 9 older healthy, all M, aged 73.0 ± 0.7 years; C: 9M with insulin resistance aged 72.8 ± 1.6 years | Non-randomized study | 100 g D-glucose in 300 mL | Significant fall in BP observed in groups B and C but not in group A, who demonstrated an increase in SBP. |
| Gentilcore et al. [74] | 2006 | 8 healthy older participants, 3M;5F, aged 65–78 years | Randomized crossover study | 50 g glucose in either 300 mL (16.7%), 600 mL (8.3%), or 1200 mL (4.1%) or saline (0.9%) at a similar rate of 3 kcal/min | SBP and DBP decreased, and HR increased, on all days following the glucose infusions with no difference between them. |
| Gentilcore et al. [83] | 2007 | 10 healthy older participants, 5M:5F, aged 65–76 years | Randomized crossover study | Granisetron (10 mcg/kg) or control (saline) at t = −25 min; ID glucose infusion (3 kcal/min) for 60 min, followed by ID saline for a further 60 min. | There were falls in SBP and DBP and a rise in HR during ID glucose; granisetron had no effect on these responses. |
| Gentilcore et al. [14] | 2008 | 8 healthy older participants, 4M:4F, aged 68–79 years | Randomized crossover study | ID glucose (64 g), fat (10% oil emulsion), protein (72 g whey), or saline (0.9%) infusion at a rate of 2.7 mL/min for 90 min, followed by ID saline for 30 min | The maximum falls in SBP during the glucose (11.7 ± 2.8 mmHg), fat (11.7 ± 4.8 mmHg), and protein (11.0 ± 1.5 mmHg) infusion did not differ significantly. The fall occurred significantly earlier during the glucose (18 ± 3 min) than during the fat (46 ± 11 min) and protein (33 ± 7 min) infusion. |
| Gentilcore et al. [75] | 2008 | 8 healthy older participants, 5M:3F, aged 65–76 years | Randomized crossover study | (1) ID glucose (50 g) or (2) ID glucose (50 g) with intragastric infusion of 500 mL water or (3) ID saline (0.9%) with intragastric infusion of 500 mL water. | The fall in SBP and DBP greater during (1) and (2) when compared with (3) and (1) compared with (2). Gastric distension attenuated the fall in BP. |
| Gentilcore et al. [54] | 2009 | 8 healthy participants, 5M:3F, aged 66–75 years | Randomized crossover study | Day 1: ingestion of 75 g glucose in 300 mL. Gastric emptying rate (kcal/min) quantified by 3D ultrasound between t = 0–120 min. Day 2: ID glucose infused at the same rate as day 1. | SBP was greater less after oral, compared with ID glucose. |
| Grasser et al. [40] | 2014 | 12 healthy young adults, 7M:5F, aged 22.0 ± 0.4 years | Randomized crossover study | 500 mL drink of either 60 g sucrose, 60 g glucose, 60 g fructose or 30 g fructose. | Ingestion of fructose (60 or 30 g) elevated SBP, DBP and mean arterial pressure (MAP). Ingestion of glucose elevated SBP. Ingestion of sucrose showed no BP changes. The increases in DBP and MAP were significantly higher for fructose (60 or 30 g) than for either glucose or sucrose. The increase in SBP was significantly higher for fructose than for sucrose. |
| Heseltine et al. [55] | 1991 | 20 older adults, 10M:10F, aged 84 ± 5 years | Randomized crossover study | 400 kcal glucose drink with either caffeinated coffee or decaffeinated coffee | Maximal postprandial fall in sitting SBP was attenuated by caffeine. Four participants developed symptomatic PPH after placebo which was prevented by caffeine. |
| Hirayama et al. [56] | 1993 | 10 patients with MSA, 9M:1F, aged 57 ± 7 years, 3 patients with peripheral autonomic neuropathy, 2M,1F, aged 35–57 years and 16 controls, 14M:2F, aged 38 ± 11 years. | Non-randomized study | 75 g glucose in 225 mL water | In MSA, ingestion of glucose resulted in a rapid and significant fall of SBP and DBP. In peripheral autonomic neuropathy, BP decreased within 15 min of oral glucose ingestion, but soon recovered. BP in the controls remained unchanged. |
| Hirayama et al. [56] | 1993 | 5 patients with MSA, 3M:2F, aged 50–71 years, 2 patients with pure autonomic failure, 2M: 54–78 years and 1 71-year-old F patient with autonomic failure and Parkinson’s disease. All with PPH and OH | Crossover study | Denopamine and midodrine administered 30 min before 75 g glucose drink on one day versus no drug a few days prior. | PPH was prevented by denopamine and midodrine. |
| Hoeldtke et al. [58] | 1989 | 6 MSA patients, 4M:2F, aged 53–73 years, 5 progressive autonomic failure patients, 3M:2F, aged 41–84 years) and 14 controls, 9M:2F, aged 36–89 years. | Crossover study | SMS-201–995 (0.8 mcg/kg) or placebo injection sc before consuming a 50 g glucose drink. | In patients with progressive autonomic failure and MSA, glucose ingestion caused a decrease in BP which was attenuated by SMS-201–995. |
| Jansen et al. [41] | 1987 | 10 young normotensive people, aged 28 ± 1 years (YN), 10 young hypertensive patients, aged 44 ± 2 years (YH), 10 elderly normotensive people aged 75 ± 2 years (EN), 10 elderly hypertensive patients aged 75 ± 1 years (EH). | Randomized crossover study | 300 mL drink of either 75 g glucose or 75 g fructose. | Glucose decreased MAP significantly in the EH, EN and YH group. After fructose, BP remained unchanged in 4 groups. |
| Jansen et al. [59] | 1988 | Hypertensive patients: randomised to nitrendipine: 4M:5F, aged 70–78 years—or hydrochlorothiazide: 3M:10F, aged 70–84 years | Randomized parallel study | 75 g glucose drink before and after treatment with 20 mg nitrendipine once daily or 50 mg hydrochlorothiazide once daily for 12 weeks. | After 12 weeks of treatment, nitrendipine reduced the fall in MAP after oral glucose (6%, p < 0.01) but this was not significant for hydrochlorothiazide (4%, NS). |
| Jansen et al. [60] | 1989 | 10 hypertensive participants, 3M:7F, aged 74 ± 4 years; and 10 normotensive participants, 4M:6F, aged 74 ± 4 years | Randomized crossover study | Octreotide (50 mcg sc) or placebo (154 mmol/L NaCl) before oral 75 g glucose in 300 mL water | Octreotide attenuated the fall in MAP (15 ± 1 mmHg in the 10 hypertensive participants and 7 ± 2 mmHg in the 10 normotensive participants) induced by oral glucose. |
| Jansen et al. [61] | 1989 | 10 hypertensive participants, 7M:3F, aged 73 ± 3 years | Randomized crossover study | Octreotide (50 mcg sc) at t = −30 min followed by placebo or insulin (0.3 U/kg) sc at t = −10 min and oral glucose (75 g in 300 mL water) at t = 0 min | The fall in MAP after oral glucose was attenuated by octreotide with no difference between the insulin and placebo study days. |
| Jansen et al. [62] | 1989 | 15 older hypertensives (EH), 7M:8F, age 73 ± 3 years, 15 older normotensives (EN), 6M:6F, age 76 ± 4 years and 10 young normotensives (YN), 5M:5F, age 26 ± 4 years. | Non-randomized study | 75 g glucose in 300 mL water | In both elderly groups MAP decreased significantly after the glucose load, whereas no change was observed in the YN. Glucose load did not influence baroreflex sensitivity. |
| Jones et al. [11] | 1998 | 16 T2DM patients, 11M:5F, aged 39–79 years; 10 young healthy participants, 9M:9F, aged 19–26 years; 9 older healthy participants, 6M:3F, aged 40–68 years old. | Non-randomized study | 75 g glucose in 350 mL water | The fall in MAP was significantly greater in the T2DM than in older healthy participants with no change in young healthy participants. The magnitude of the fall in BP was related to the rate of gastric emptying. |
| Jones et al. [11] | 2005 | 10 healthy participants, 6M:6F, aged 73.9 ± 1.2 years | Randomized crossover study | 25 g glucose in 200 mL (12.5%), 75 g glucose in 200 mL (37.5%), 25 g glucose in 600 mL (4%), and 75 g glucose in 600 mL (12.5%) | Increased drink volume attenuates the fall in BP with no effect of glucose concentration. |
| Jones et al. [63] | 2001 | 10 healthy participants, 5M:5F, aged 67–78 years | Randomized crossover study | 300 mL water containing 50 g glucose with 30 mL lemon juice made up to 300 mL with or without 9 g guar gum | SBP, DBP and MAP fell on both days. The magnitude of the falls in SBP, DBP, and MAP were less, after guar. |
| Jones et al. [64] | 2019 | 15 healthy participants, 9M:6F, aged 67.2 ± 2.3 years and 15 T2DM patients, 9M:6F, aged 61.9 ± 2.3 years) | Randomized crossover study | Lixisenatide (10 mcg) or placebo sc 30 min before 75 g glucose drink on two separate days. | Lixisenatide attenuated the decrease in SBP and DBP compared to placebo in healthy participants and those with T2DM |
| Marathe et al. [76] | 2016 | 9 patients with T2DM, all M, aged 62 ± 2.4 years | Randomized crossover study | ID glucose (25 g/100 mL) infused at 2 kcal/min or 4 kcal/min | SBP and DBP fell at 30 min with 4 kcal/min, but not 2 kcal/min infusions. The fall in SBP was greater after the 4 kcal/min infusion. |
| Maruta et al. [76] | 2006 | 28 neurologic patients (11 with PD, 4M:7F, aged 61–86 years; 6 with MSA, 4M:2F, aged 53–76 years; 11 with T2DM, 8M:3F, aged 62–85 years) and 20 healthy controls (13 older participants, 5M:8F, aged 62–80 years; 7 young participants, 4M:3F, aged 34–59 years). | Crossover study | 75 g glucose with or without 200 mcg voglibose. All participants were studied on the day without voglibose. 11 of them (4 with PD, 5 with MSA, 1 with T2DM, 1 older control), who had PPH, were studied on the day with voglibose. | The fall in BP was less (without voglibose: 41.5 ± 13.2 mmHg, with voglibose: 21.0 ± 13.0 mmHg) and the duration of PPH was shorter (without voglibose: 52.3 ± 28.0 min, with voglibose: 17.3 ± 22.5 min) after voglibose. |
| Masuo et al. [66] | 1996 | 12 young normotensive (NT) participants, aged 47.8 ± 2.6 years; 21 elderly NT, aged 77.9 ± 1.5 years; 17 young hypertensive (EH) patients, aged 49.0 ± 1.9 years and 32 elderly EH. 1M:1F in each group. | Non-randomized study | 75 g glucose in 225 mL water | Postprandial BP reduction, defined as 10% or more decline in MAP was recognized in 3/12 (25%) young NT, 9/21 (43%) elderly NT, 5/17 (29%) young EH, and 20/32 (63%) elderly EH. The frequency of postprandial BP reduction was significantly greater in elderly hypertensives compared to elderly normotensives and was greater in young hypertensives compared to young normotensives. |
| Mathias et al. [43] | 1989 | 6 patients with chronic autonomic failure (CAF), 4M:2F, aged 42–68 years, 6 age-matched participants without CAF, aged 45–70 years; and 8 normal participants, all M, aged 28–35 years. | Randomized parallel study | An iso-osmotic solution of glucose (1 g/kg body weight) or xylose (0.83 g/kg body weight) in 250 mL water. 6 patients with CAF attended 2 on both glucose and xylose days. 6 age-matched participants and 8 male normal participants attended only on the glucose day. | Xylose caused a lower and more transient fall in BP than glucose in patients with CAF (15 ± 6% vs. 34 ± 7%). After glucose, there was a substantial fall in 6 age-matched participants but a minimal change in 8 male normal participants. |
| Nair et al. [67] | 2015 | 13 participants with PPH, 4M:9F, aged 76.5 ± 4 years. | Randomized crossover study | Ingestion of 50 g glucose in 200 mL on both days. On one day, participants walked at their usual pace for 30 m every 30 min for 120 min. | On the control day, there were significant falls in SBP and DBP. On the intervention day, there was no significant fall in SBP, however, DBP still fell significantly. |
| Nair et al. [68] | 2016 | 29 older participants, 18F aged 77.1 ± 5.4 years and 11M aged 74.7 ± 3.9 years | Randomized crossover study | 3 treatments: glucose (50 g in 200 mL) (G) or water (200 mL) and intermittent walking (WW) or glucose and walking (GW) | 16 participants had PPH. In PPH, there was a significant fall in SBP (26.69 ± 8.43 mmHg) on the “G” day and no change on “GW” or “WW” days. In those without PPH, there were no changes in SBP on the “G” or “GW” days, with an increase in SBP on the “WW” day. |
| Nguyen et al. [44] | 2018 | 35 older participants, 28M:7F, aged 73 ± 5 years, discharged at least 3 months from ICU | Non-randomized study | 300 mL drink containing 75 g glucose | There were significant reductions in both SBP and DBP. Ten participants (29%) had postprandial hypotension. The maximal fall in SBP and DBP were −29 ± 14 mmHg and −18 ± 7 mmHg. The maximal fall in SBP was greater in patients with PPH than in those without (−46.2 ± 10.8 mmHg vs. −22.7 ± 9.2 mmHg). |
| O’Donovan et al. [77] | 2002 | 8 healthy elderly participants, 4M:4F, aged 70.3 ± 3.4 years | Randomized crossover study | 25% glucose solution was infused intraduodenally at a rate of either 1 or 3 kcal/min for 60 min followed by 0.9% saline for a further 60 min | Between t = 0–60 min, there was a fall in SBP, DBP and MAP during the 3 kcal/min glucose infusion, but not during the 1 kcal/min infusion. |
| O’Donovan et al. [84] | 2005 | 8 healthy older participants, 4M:4F, aged 70.3 ± 3.4 years | Randomized crossover study | ID glucose infusion (3 kcal/min) with or without guar gum (4 g) for 60 min, followed by 0.9% saline intraduodenally for a further 60 min. | Between t = 0–60 min, SBP was lower during the glucose-only infusion than during the glucose and guar infusion. The maximum fall in SBP on the glucose-only study was 10 ± 4 mmHg. Between t = 0–30 min, DBP fell during the glucose-only infusion, but did not change with the glucose and guar infusion. |
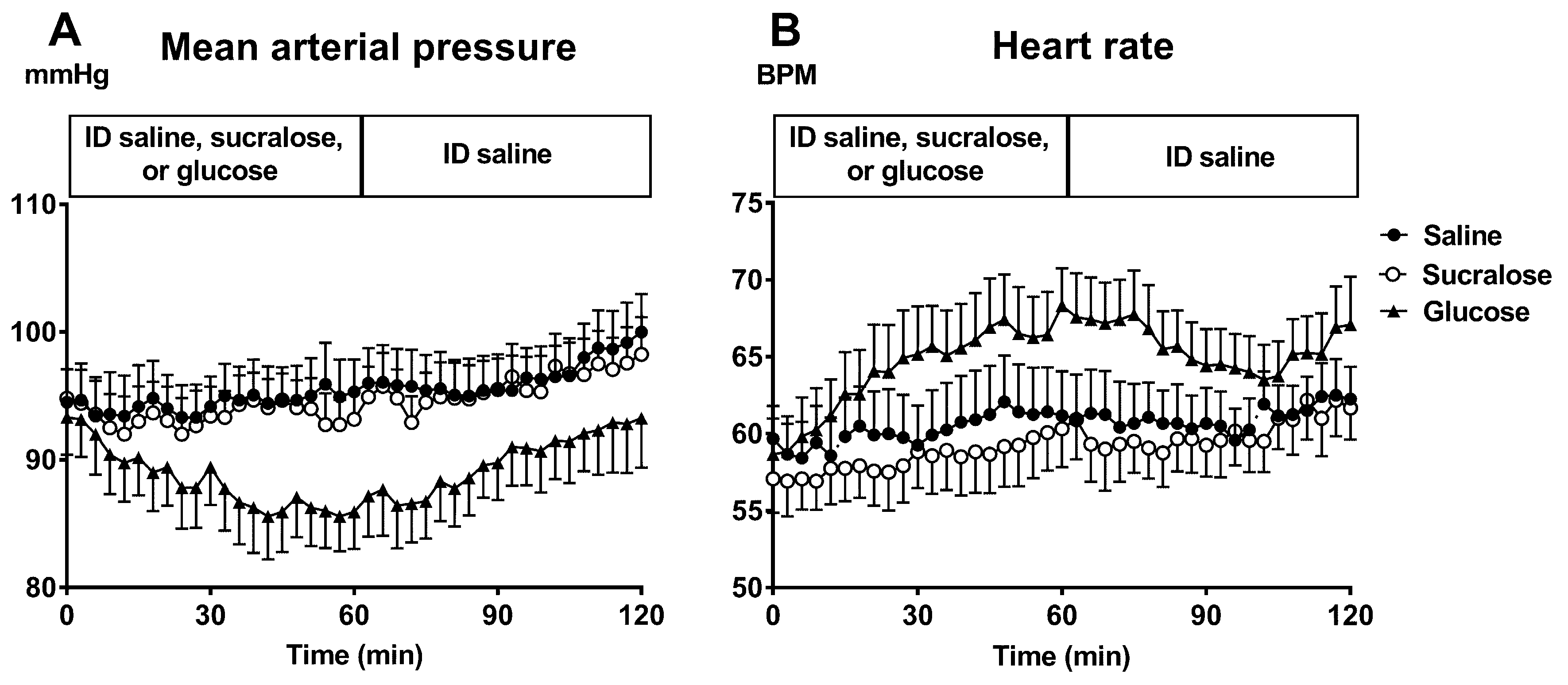
| Pham et al. [78] | 2018 | 12 healthy participants, 6M:6F, aged 73.2 ± 1.1 years | Randomized crossover study | ID infusion of either glucose (25%, ~1400 mOsmol/L), sucralose (4 mmol/L, ~300 mOsmol/L) or saline (0.9%, ~300 mOsmol/L) at a rate of 3 mL/min for 60 min followed by ID saline for a further 60 min. | MAP decreased during glucose but not during sucralose or saline. By t = 60 min, MAP was lower after glucose (85.9 ± 2.8 mmHg) than after sucralose (93.1 ± 2.2 mmHg) infusions without significant difference between sucralose and saline infusions. |
| Pham et al. [12] | 2019 | 33 healthy older participants, 16M:17F, aged 77.0 ± 0.7 years | Non-randomized study longitudinal study | 75 g glucose in 300 mL water | The prevalence of PPH doubled from 9.1% to 18.2%. There was a fall in SBP and DBP on both study days. The AUC of SBP was greater at follow-up. The maximum fall in postprandial SBP between t = 60–120 min was significantly greater at follow-up (−11.7 ± 1.4 vs. −15.2 ± 1.6 mmHg). |
| Robinson et al. [45] | 1992 | 5 participants with age-related OH, 2M:3F, aged 73–88 years), 3 participants with autonomic failure, 1M:2F, aged 72–79 years and 5 controls, 2M:3F, aged 72–86 years | Randomized crossover study | 50 g glucose or 42 g xylose in 100 mL water | In OH and autonomic failure groups, the SBP decreased comparably following glucose and xylose, DBP was lowered 60–90 min after glucose. No significant BP changes in the control group. |
| Russo et al. [13] | 2003 | 11 patients with T2DM managed by diet alone, 8M:3F, aged 61.9 ± 1.3 years | Randomized crossover study | 50 g glucose and 30 mL lemon juice, with or without 9 g guar gum in 300 mL. | There was significant fall in SBP between baseline and 30 min on the control day (143.9 ± 4.7 mmHg vs. 139.0 ± 4.2 mmHg; p < 0.01), but not after guar (145.1 ± 4.8 mmHg vs. 142.6 ± 4.5 mmHg, p = 0.6). There were significant falls in DBP and MAP between baseline and 30 min on both study days. |
| Sasaki et al. [69] | 1992 | 15 normal participants, aged 25–63 years and 35 outpatients with T2DM, aged 28–60 years | Non-randomized study | Daily meals and 75 g glucose in 300 mL water | No significant change in BP in the normal participants. The incidence of PPH in diabetics was 37% after daily meal and 20% after 75 g glucose. |
| Takamori et al. [70] | 2007 | 17 MSA patients, 9M:8F, aged 59.8 ± 7.9 years and 8 healthy controls, 7M:1F, aged 60.5 ± 8.3 years | Non-randomized study | 75 g of glucose in 225 mL of water | Of 17 MSA patients, 9 had PPH. 8 controls were PPH negative. The falls in SBP and DBP in MSA with PPH were significantly greater than in MSA without PPH or in controls. |
| Thazhath et al. [85] | 2017 | 9 patients with T2DM, managed by diet alone, 6M:3F, aged 60.7 ± 2.4 years | Randomized crossover study | Intravenous exenatide (7.5 mcg) or volume-matched saline control from −30 to 120 min + ID glucose (3 kcal /min) from 0–60 min. | During the ID glucose infusion, SBP, DBP and MAP increased with exenatide, but fell with saline control. The AUC for DBP and MAP, but not SBP, was higher with exenatide than control. |
| Trahair et al. [16] | 2015 | 14 older healthy participants, 6M:8F, aged 72.1 ± 1.1 years and 10 patients with T2DM, 6M: 4F, aged 68.7 ± 3.4 years | Randomized crossover study | Between t = −30–120 min: intravenous infusion of GLP-1 (0.9 pmol/kg/min) or saline (154 mmol/l NaCl). At t = 0 min: 75 g glucose drink in 300 mL water | After the glucose drink there were falls in SBP and DBP in both groups. The fall in DBP in older individuals; and the fall in SBP and DBP in patients with T2DM were less after GLP-1 infusion compared to control. |
| Trahair et al. [79] | 2012 | 12 healthy young participants, 6M;6F, aged 22.2 ± 2.3 years and 12 healthy older participants, 6M; 6F, aged 68.7 ± 1.0 years | Randomized crossover study | ID infusion of glucose at either 1, 2 or 3 kcal/min or 0.9% normal saline for 60 min followed by ID saline for a further 60 min. | In young participants, there were no changes in SBP and DBP during the four infusions. In older participants, there were falls in SBP and DBP during 2 kcal/min and 3 kcal/min infusions, but not during 1 kcal/min infusion. |
| Trahair et al. [18] | 2014 | 10 healthy older participants, 9M: 1F, aged 73.2 ± 1.5 years | Randomized crossover study | Between t = −30–60 min, intravenous infusion of GLP-1 (0.9 pmol/kg/min), or saline for 90. Between t = 0–60 min, ID glucose was infused at 3 kcal/min. | During ID glucose infusion, there were falls in SBP and DBP with both GLP-1 and control. The maximum fall in SBP was greater with control than GLP-1 (−13.6 ± 3.1 mmHg vs. −8.7 ± 2.3 mmHg). |
| Trahair et al. [46] | 2015 | 88 healthy older participants, 41M:47F, aged 71.0 ± 0.5 years | Non-randomized study | 75 g glucose in 300 mL water | SBP and DBP decreased significantly after the glucose drink. Eleven participants (12.8%) had PPH. |
| Trahair et al. [47] | 2016 | 21 participants with mild to moderate PD, 13M:8F, aged 64.2 ± 1.6 years | Crossover study | 75 g glucose in 300 mL water | SBP and DBP fell following the glucose drink. 8 participants (38%) had postprandial hypotension. |
| Trahair et al. [48] | 2017 | 8 healthy older participants, 4M:4F, aged 71.0 ± 1.7 years and 8 participants with PPH 1M:7F, aged 75.5 ± 1.0 years | Randomized crossover study | 75 g glucose in 300 mL water or water alone | Following the glucose, there were decreases in SBP and DBP in both groups, the maximum fall in SBP was greater in participants with PPH. Following the water, there were no changes in SBP and DBP in healthy participants, but there was a rise in SBP in participants with PPH. |
| Trahair et al. [80] | 2018 | 12 obese participants, 10M:2F, aged 36.6 ± 3.9 years, BMI: 36.1 ± 1.3 kg/m2) and 23 controls, 16M:7F, aged 27.8 ± 2.4 years, BMI: 22.4 ± 0.5 kg/m2 | Randomized crossover study | ID infusions of glucose at 1 or 3 kcal/min, or 0.9% saline, for 60 min, followed by saline for a further 60 min. | No changes in SBP in both groups during any of the conditions. There was a fall in DBP in controls during 1 kcal/min and 3 kcal/min infusions; and in obese participants during 3 kcal/min infusion. There was no difference in BP responses between the groups. |
| Umehara et al. [71] | 2014 | 37 patients with de novo PD (17 with PPH, 4M:13F, aged 76.8 ± 6.1 years; 20 without PPH, 8M:12F, aged 74.4 ± 7.5 years) and 10 healthy controls, aged 74.3 ± 4.8 years) | Non-randomized study | 75 g glucose in 300 mL water | Of the 37 patients, 17 (45.9%) had PPH, 15 (40.5%) had OH and 8 (21.6%) had both PPH and OH. 2 controls had PPH. The maximum fall in SBP after the glucose drink significantly correlated with that on head-up tilt-table testing in PD patients. |
| Umehara et al. [72] | 2016 | 64 de novo patients with PD, 22M:42F, aged 76 ± 4 years | Non-randomized study | 75 g glucose in 300 mL water | 29 patients had PPH. Patients with PPH experienced greater reductions in SBP (30 ± 11 vs. 11 ± 15 mmHg) and DBP (14 ± 9 vs. 7 ± 5 mmHg) after glucose drink compared to patients without PPH. |
| van Orshoven et al. [81] | 2008 | 8 healthy young participants (4M:4F, aged 28.8 ± 3.4 years), 8 healthy elderly (4M:4F, aged 75.3 ± 1.6 years). 2 female patients with symptomatic PPH aged 21 and 90 years | Non-randomized study | ID infusion of 25% glucose at 3 mL/min for 60 min. Saline was infused for 30 min before and after ID glucose. | ID glucose decreased SBP, in both the young and older people, but the fall in SBP was greater in the older group (−6.5 ± 1.6 vs. −17.0 ± 4.1 mmHg). 2 PPH patients had a greater fall in SBP than the two healthy groups (−21 and −98 mmHg). |
| Vanis et al. [82] | 2011 | 12 healthy older participants, 6M:6F, aged 68.7 ± 1.0 years | Randomized crossover study | ID infusion of glucose at either 1, 2 or 3 kcal/min or 0.9% normal saline for 60 min, followed by saline for a further 60 min. | There was a fall in SBP and DBP during 2 and 3 kcal/min glucose infusions, but not during saline or 1 kcal/min glucose infusion. There was no difference in the maximum falls in SBP during 2 kcal/min (15 ± 2 mmHg) and 3 kcal/min (12 ± 2 mmHg) loads. |
| Vanis et al. [49] | 2011 | 8 healthy older participants, 6M:2F, aged 65–75 years | Randomized crossover study | 300 mL drink of water, 50 g glucose or 50 g d-xylose. | There was a fall in SBP after glucose drink and no change after xylose or water drink. |
| Vanis et al. [86] | 2010 | 8 participants, 6M:2F, aged 65–75 yeas | Randomized crossover study | The four treatments were as follows: ID glucose (3 kcal/min) + barostat (distension) (GD), ID saline + barostat (SD), ID glucose (G), and ID saline (S). | SBP and DBP fell during G, but not during S or GD; and increased during SD. The maximum changes in SBP during G, GD, S and SD were −14 ± 5, −3 ± 4, +11 ± 2, and +15 ± 3 mmHg respectively. |
| Vanis et al. [87] | 2012 | 9 participants, all M, aged 65–75 years | Randomized crossover study | ID glucose infusion (3 kcal/min) and gastric distension at a volume of (1) 0 ml (V0), (2) 100 mL (V100), (3) 300 mL (V300), or (4) 500 mL (V500). | SBP and DBP fell during V0, but did not change significantly during V100, V300, V500. |
| Visvanathan et al. [73] | 2006 | 12 elderly participants, 6M:6F, aged 72.2 ± 5.7 years | Randomized crossover study | 300 mL drink of either (1) CHO (75 g glucose and 93 g Polyjoule (CHO polymer)-653 kcal); (2) 88% fat (cream blended with milk-653 kcal) or (3) water. | SBP decreased following the CHO drink and the high-fat drink but not water; there was no difference in the magnitude of the decrease between the CHO and fat drinks. The onset of the SBP fall was slower after the fat drink (26.5 ± 17.1 min vs. 13.0 ± 11.7 min). |
| Visvanathan et al. [50] | 2005 | 10 healthy older participants, 4M; 6F, aged 72.2 ± 1.50 years | Randomized crossover study | 300 mL of either 50 g glucose, 50 g sucrose, 50 g fructose or water + 30 mL lemon juice | SBP decreased significantly following glucose (−3.96 ± 1.38 mmHg) and sucrose (−3.03 ± 1.37 mmHg) ingestion, increased non-significantly following fructose ingestion (2.59 ± 1.62 mmHg). The decrease in SBP occurred earlier after glucose than sucrose ingestion (7.33 ± 2.19 vs. 21.0 ± 4.30 min). |
| Wu et al. [88] | 2017 | Study A: 16 participants with T2DM, 11M: 5F, 65.5 ± 2.4 years. Study B: 9 participants with T2DM, all M, aged 63.8 ± 2.6 years | Randomized crossover study | Study A: vildagliptin (50 mg) or placebo was given 60 min before ID glucose infusion at 2 or 4 kcal/min (ID2 or ID4). Study B: Participants received metformin (850 mg) or placebo for 7 days. On the study day, metformin (850 mg) or placebo was given 30 min before ID2. | Study A: SBP and DBP decreased after vildagliptin, but not after placebo, without any difference between ID2 and ID4. Study B: SBP and DBP decreased on both days without any difference between metformin and placebo. |
| Study | Year | Participant Characteristics | Study Design | Sweeteners Assessed rather than Glucose | Test Meal | Effects on Blood Pressure |
|---|---|---|---|---|---|---|
| Brown et al. [39] | 2008 | 15 healthy normal-weight volunteers, 9M:6F, aged 24 ± 1 years | Randomized crossover study | Fructose | 500 mL of either water, 60 g glucose, or 60 g fructose. | Oral fructose, but not glucose, significantly increased SBP and DBP. The maximum rise in SBP after fructose was 6.2 ± 0.8 mmHg. |
| Charriere et al. [89] | 2017 | 9 young healthy men, aged 24 ± 1 years | Randomized crossover study | Galactose, fructose | 500 mL of water containing 60 g of either glucose, fructose or galactose. | The increase in SBP after fructose (7–8 mmHg) was greater than after glucose (4–5 mmHg) or galactose (2–3 mmHg). DBP increased to a greater extent with fructose (~5 mmHg), compared to non-significant increases of only 2–3 mmHg after glucose or galactose. |
| Gentilcore et al. [105] | 2005 | 8 healthy older participants, 5M:3F, aged 65–79 years | Randomized crossover study | Sucrose | 300 mL drink of 100 g sucrose and 30 mL lemon juice with or without 100 mg acarbose | There was a fall in SBP and DBP on the control day while there was an overall increase in SBP on the acarbose day. |
| Gentilcore et al. [106] | 2011 | 8 healthy older participants, 4M:4F, aged 66–77 years | Randomized crossover study | Sucrose | ID infusion of sucrose (100 g/300 mL) at ~6 kcal/min with or without acarbose (100 mg), over 60 min. | There were significant falls in SBP (maximum fall: 11.2 ± 2.0 mmHg) during control, but not after acarbose. The fall in DBP was greater after control (10.9 ± 0.9 mmHg) than after acarbose (8.1 ± 1.5 mmHg). |
| Grasser et al. [40] | 2014 | 12 healthy young adults, 7M:5F, aged 22.0 ± 0.4 years | Randomized crossover study | Fructose, sucrose | 500 mL drink of either 60 g sucrose, 60 g glucose, 60 g fructose or 30 g fructose. | Ingestion of fructose (60 or 30 g) elevated SBP, DBP and MAP. Ingestion of glucose elevated SBP. Ingestion of sucrose showed no BP changes. The increases in DBP and MAP were significantly higher for fructose (60 or 30 g) than for either glucose or sucrose. The increase in SBP was significantly higher for fructose than for sucrose. |
| Jansen et al. [41] | 1987 | 10 young normotensive people, aged 28 ± 1 years (YN), 10 young hypertensive patients, aged 44 ± 2 years (YH), 10 elderly normotensive people aged 75 ± 2 years (EN), 10 elderly hypertensive patients aged 75 ± 1 years (EH) | Randomized crossover study | Fructose | 300 mL drink of either 75 g glucose or 75 g fructose | Glucose decreased MAP significantly in the EH, EN and YH group. After fructose, BP remained unchanged in 4 groups. |
| Mathias et al. [43] | 1989 | 6 patients with chronic autonomic failure (CAF), 4M:2F, aged 42–68 years; 6 age-matched participants without CAF, aged 45–70 years; and 8 normal participants, all M, aged 28–35 years | Randomized parallel study | Xylose | An iso-osmotic solution of glucose (1 g/kg body weight) or xylose (0.83 g/kg body weight) in 250 mL water. | Xylose caused a lower and more transient fall in BP than glucose in patients with CAF (15 ± 6% vs. 34 ± 7%). After glucose, there was a substantial fall in 6 age-matched participants but a minimal change in 8 male normal participants. |
| Robinson et al. [45] | 1992 | 5 people with age-related OH, 2M:3F, aged 73–88 years, 3 people with autonomic failure, 1M:2F, aged 72–79 years and 5 controls, 2M:3F, aged 72–86 years | Randomized crossover study | Xylose | 50 g glucose or 42 g xylose in 100 mL water | There were no significant BP changes in the control group. In OH and autonomic failure groups, the SBP decreased comparably following glucose and xylose, DBP was lowered 60–90 min after glucose. |
| Teunissen-Beekman et al. [107] | 2014 | 48 participants, 31M; 17F, aged 58 ± 1 (SEM) years | Randomized crossover study | Maltodextrin, sucrose | Test drink of 70 g either protein (pea protein isolate, milk protein isolate, egg white protein isolate or mixed protein), sucrose or maltodextrin. | DBP and MAP were significantly decreased after maltodextrin, but not after protein mix or sucrose. SBP was not significantly changed after any of the meals. |
| Vanis et al. [49] | 2011 | 8 healthy older participants, 6M:2F, aged 65–75 years | Randomized crossover study | Xylose | 300 mL drink of water, 50 g glucose or 50 g d-xylose. | There was a fall in SBP after glucose drink and no change after xylose or water drink. |
| Visvanathan et al. [50] | 2005 | 10 healthy older participants, 4M:6F, aged 72.2 ± 1.50 years | Randomized crossover study | Fructose, sucrose | 300 mL of either 50 g glucose, 50 g sucrose, 50 g fructose or water + 30 mL lemon juice | SBP decreased significantly following glucose (−3.96 ± 1.38 mmHg) and sucrose (−3.03 ± 1.37 mmHg), but not fructose, ingestion (2.59 ± 1.62 mmHg). The decrease in SBP occurred earlier after glucose than sucrose ingestion (7.33 ± 2.19 vs. 21.0 ± 4.30 min). |
| Study | Year | Participant Characteristics | Study Design | Non-Nutritive Sweeteners Assessed | Test Meal | Effects on Blood Pressure |
|---|---|---|---|---|---|---|
| Kazmi et al. [140] | 2017 | 200 students divided equally into 4 groups: A (aged 18.82 ± 0.80 years), B: (aged 18.60 ± 0.57), C (aged 18.64 ± 0.59) and D (18.64 ± 0.59) | Parallel study | Aspartame, Acesulfame-K, sucralose | Group A (control): 10 g of cellulose. Group B: 0.36 gm (5 mg/kg) sucralose. Group C: 10.8 g (150 mg/kg) aspartame. Group D: 3.24 g (45 mg/kg) Acesulfame-K. | There was no difference in BP between group A and B. SBP was lower at 60, 90 and 120 min for group C; and at 60 min for group D compared to control. |
| Pham et al. [78] | 2018 | 12 healthy participants, 6M: 6F, aged 73.2 ± 1.1 (SEM) years | Randomized crossover study | Sucralose | ID infusion of either glucose (25%, ~1400 mOsmol/L), sucralose (4 mmol/L, ~300 mOsmol/L) or saline (0.9%, ~300 mOsmol/L) at a rate of 3 mL/min for 60 min followed by ID saline for a further 60 min. | MAP decreased during glucose but not during sucralose or saline. By t = 60 min, MAP was lower after glucose (85.9 ± 2.8 mmHg) than after sucralose (93.1 ± 2.2 mmHg) infusions without significant difference between sucralose and saline infusions. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pham, H.; Phillips, L.K.; Jones, K.L. Acute Effects of Nutritive and Non-Nutritive Sweeteners on Postprandial Blood Pressure. Nutrients 2019, 11, 1717. https://doi.org/10.3390/nu11081717
Pham H, Phillips LK, Jones KL. Acute Effects of Nutritive and Non-Nutritive Sweeteners on Postprandial Blood Pressure. Nutrients. 2019; 11(8):1717. https://doi.org/10.3390/nu11081717
Chicago/Turabian StylePham, Hung, Liza K. Phillips, and Karen L. Jones. 2019. "Acute Effects of Nutritive and Non-Nutritive Sweeteners on Postprandial Blood Pressure" Nutrients 11, no. 8: 1717. https://doi.org/10.3390/nu11081717
APA StylePham, H., Phillips, L. K., & Jones, K. L. (2019). Acute Effects of Nutritive and Non-Nutritive Sweeteners on Postprandial Blood Pressure. Nutrients, 11(8), 1717. https://doi.org/10.3390/nu11081717





