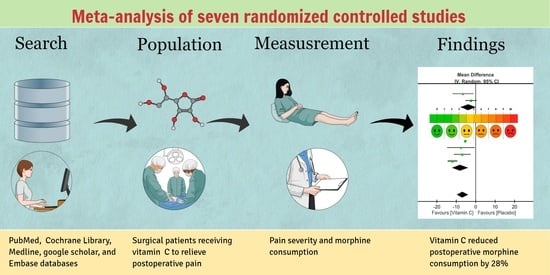
The Effect of Perioperative Vitamin C on Postoperative Analgesic Consumption: A Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection Criteria
2.3. Data Extraction
2.4. Primary Outcome, Secondary Outcomes, and Definitions
2.5. Assessment of Risk of Bias for Included Studies
2.6. Statistical Analysis
3. Results
3.1. Study Selection
3.2. Characteristics of Included Studies
3.3. Risk of Bias Assessment
3.4. Outcomes
3.4.1. Severity of Pain within 1–2 h after Surgery
3.4.2. Severity of Pain 6 h after Surgery
3.4.3. Severity of Pain at 24 h after Surgery
3.4.4. Opioid Consumption within 1–2 h after Surgery
3.4.5. Opioid Consumption within 6 h after Surgery
3.4.6. Opioid Consumption within 24 h after Surgery
3.4.7. Opioid Consumption within 48 h after Surgery
3.4.8. Perioperative Blood Loss
3.4.9. Postoperative Nausea and Vomiting
3.4.10. Postoperative Circulating Vitamin C Concentration after Vitamin C Supplementation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Apfelbaum, J.L.; Chen, C.; Mehta, S.S.; Gan, T.J. Postoperative pain experience: Results from a national survey suggest postoperative pain continues to be undermanaged. Anesth. Analg. 2003, 97, 534–540. [Google Scholar] [CrossRef] [Green Version]
- Pavlin, D.J.; Chen, C.; Penaloza, D.A.; Buckley, F.P. A survey of pain and other symptoms that affect the recovery process after discharge from an ambulatory surgery unit. J. Clin. Anesth. 2004, 16, 200–206. [Google Scholar] [CrossRef]
- Kehlet, H.; Jensen, T.S.; Woolf, C.J. Persistent postsurgical pain: Risk factors and prevention. Lancet (Lond. Engl.) 2006, 367, 1618–1625. [Google Scholar] [CrossRef]
- Chou, R.; Gordon, D.B.; de Leon-Casasola, O.A.; Rosenberg, J.M.; Bickler, S.; Brennan, T.; Carter, T.; Cassidy, C.L.; Chittenden, E.H.; Degenhardt, E. Management of Postoperative Pain: A clinical practice guideline from the American pain society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J. Pain 2016, 17, 131–157. [Google Scholar]
- Ayatollahi, V.; Dehghanpour Farashah, S.; Behdad, S.; Vaziribozorg, S.; Rabbani Anari, M. Effect of intravenous vitamin C on postoperative pain in uvulopalatopharyngoplasty with tonsillectomy. Clin. Otolaryngol. 2017, 42, 139–143. [Google Scholar] [CrossRef]
- Li, R.; Shen, L.; Yu, X.; Ma, C.; Huang, Y. Vitamin C enhances the analgesic effect of gabapentin on rats with neuropathic pain. Life Sci. 2016, 157, 25–31. [Google Scholar] [CrossRef]
- Du, J.; Cullen, J.J.; Buettner, G.R. Ascorbic acid: Chemistry, biology and the treatment of cancer. Biochim. Biophys. Acta 2012, 1826, 443–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Englard, S.; Seifter, S. The biochemical functions of ascorbic acid. Annu. Rev. Nutr 1986, 6, 365–406. [Google Scholar] [CrossRef]
- Chen, J.Y.; Chang, C.Y.; Feng, P.H.; Chu, C.C.; So, E.C.; Hu, M.L. Plasma vitamin C is lower in postherpetic neuralgia patients and administration of vitamin C reduces spontaneous pain but not brush-evoked pain. Clin. J. Pain 2009, 25, 562–569. [Google Scholar] [CrossRef]
- Shibuya, N.; Humphers, J.M.; Agarwal, M.R.; Jupiter, D.C. Efficacy and safety of high-dose vitamin C on complex regional pain syndrome in extremity trauma and surgery–systematic review and meta-analysis. J. Foot Ankle Surg. 2013, 52, 62–66. [Google Scholar] [CrossRef] [Green Version]
- Rokyta, R.; Holecek, V.; Pekárkova, I.; Krejcová, J.; Racek, J.; Trefil, L.; Yamamotová, A. Free radicals after painful stimulation are influenced by antioxidants and analgesics. Neurol. Endocrinol. Lett. 2003, 24, 304–309. [Google Scholar]
- Chen, S.; Roffey, D.M.; Dion, C.A.; Arab, A.; Wai, E.K. Effect of Perioperative Vitamin C Supplementation on Postoperative Pain and the Incidence of Chronic Regional Pain Syndrome: A Systematic Review and Meta-Analysis. Clin. J. Pain 2016, 32, 179–185. [Google Scholar] [CrossRef]
- Ma, H.; Tang, J.; White, P.F.; Zaentz, A.; Wender, R.H.; Sloninsky, A.; Naruse, R.; Kariger, R.; Quon, R.; Wood, D.; et al. Perioperative rofecoxib improves early recovery after outpatient herniorrhaphy. Anesth. Analg. 2004, 98, 970–975. [Google Scholar] [CrossRef]
- Watcha, M.F.; Issioui, T.; Klein, K.W.; White, P.F. Costs and effectiveness of rofecoxib, celecoxib, and acetaminophen for preventing pain after ambulatory otolaryngologic surgery. Anesth. Analg. 2003, 96, 987–994. [Google Scholar] [CrossRef]
- Issioui, T.; Klein, K.W.; White, P.F.; Watcha, M.F.; Coloma, M.; Skrivanek, G.D.; Jones, S.B.; Thornton, K.C.; Marple, B.F. The efficacy of premedication with celecoxib and acetaminophen in preventing pain after otolaryngologic surgery. Anesth. Analg. 2002, 94, 1188–1193. [Google Scholar] [CrossRef]
- Issioui, T.; Klein, K.W.; White, P.F.; Watcha, M.F.; Skrivanek, G.D.; Jones, S.B.; Hu, J.; Marple, B.F.; Ing, C. Cost-efficacy of rofecoxib versus acetaminophen for preventing pain after ambulatory surgery. Anesthesiology 2002, 97, 931–937. [Google Scholar] [CrossRef]
- Alishiri, A.; Mosavi, S.A. Ascorbic acid versus placebo in postoperative lid edema postphotorefractive keratectomy: A double-masked, randomized, prospective study. Oman. J. Ophthalmol. 2019, 12, 4–9. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ (Clin. Res. Ed.) 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Shaheen, P.E.; Walsh, D.; Lasheen, W.; Davis, M.P.; Lagman, R.L. Opioid equianalgesic tables: Are they all equally dangerous? J. Pain Symptom Manag. 2009, 38, 409–417. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin. Res. Ed.) 2011, 343, d5928. [Google Scholar] [CrossRef] [Green Version]
- Blaudszun, G.; Lysakowski, C.; Elia, N.; Tramèr, M.R. Effect of perioperative systemic α2 agonists on postoperative morphine consumption and pain intensity: Systematic review and meta-analysis of randomized controlled trials. Anesthesiology 2012, 116, 1312–1322. [Google Scholar] [CrossRef] [Green Version]
- Jarahzadeh, M.H.; Mousavi, B.M.H.; Abbasi, H.; Jafari, M.A.; Sheikhpouar, E. The efficacy of vitamin C infusion in reducing post-intubation sore throat. Med. časopis 2019, 53, 95–100. [Google Scholar] [CrossRef]
- Jeon, Y.; Park, J.S.; Moon, S.; Yeo, J. Effect of intravenous high dose vitamin C on postoperative pain and morphine use after laparoscopic colectomy: A randomized controlled trial. Pain Res. Manag. 2016, 2016. [Google Scholar] [CrossRef]
- Kanazi, G.E.; El-Khatib, M.F.; Yazbeck-Karam, V.G.; Hanna, J.E.; Masri, B.; Aouad, M.T. Effect of vitamin C on morphine use after laparoscopic cholecystectomy: A randomized controlled trial. Can. J. Anaesth. 2012, 59, 538–543. [Google Scholar] [CrossRef] [Green Version]
- Tunay, D.L.; Ilgınel, M.T.; Ünlügenç, H.; Tunay, M.; Karacaer, F.; Biricik, E. Comparison of the effects of preoperative melatonin or vitamin C administration on postoperative analgesia. Bosn. J. Basic Med. Sci. 2020, 20, 117. [Google Scholar] [CrossRef] [Green Version]
- Moon, S.; Lim, S.; Yun, J.; Lee, W.; Kim, M.; Cho, K.; Ki, S. Additional effect of magnesium sulfate and vitamin C in laparoscopic gynecologic surgery for postoperative pain management: A double-blind randomized controlled trial. Anesth. Pain Med. 2020, 15, 88–95. [Google Scholar] [CrossRef] [Green Version]
- Moon, S.; Lim, S.H.; Cho, K.; Kim M-h Lee, W.; Cho, Y.H. The efficacy of vitamin C on postlaparoscopic shoulder pain: A double-blind randomized controlled trial. Anesth. Pain Med. 2019, 14, 202–207. [Google Scholar] [CrossRef]
- Pourmatroud, E.; Hormozi, L.; Hemadi, M.; Golshahi, R. Intravenous ascorbic acid (vitamin C) administration in myomectomy: A prospective, randomized, clinical trial. Arch. Gynecol. Obstet. 2012, 285, 111–115. [Google Scholar] [CrossRef]
- Gan, T.J.; Habib, A.S.; Miller, T.E.; White, W.; Apfelbaum, J.L. Incidence, patient satisfaction, and perceptions of post-surgical pain: Results from a US national survey. Curr. Med. Res. Opin. 2014, 30, 149–160. [Google Scholar] [CrossRef]
- McGrath, B.; Elgendy, H.; Chung, F.; Kamming, D.; Curti, B.; King, S. Thirty percent of patients have moderate to severe pain 24 hr after ambulatory surgery: A survey of 5,703 patients. Can. J. Anaesth. 2004, 51, 886–891. [Google Scholar] [CrossRef]
- Gjeilo, K.H.; Stenseth, R.; Klepstad, P. Risk factors and early pharmacological interventions to prevent chronic postsurgical pain following cardiac surgery. Am. J. Cardiovasc. Drugs 2014, 14, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Hyllested, M.; Jones, S.; Pedersen, J.L.; Kehlet, H. Comparative effect of paracetamol, NSAIDs or their combination in postoperative pain management: A qualitative review. Br. J. Anaesth. 2002, 88, 199–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorissen, K.J.; Benning, D.; Berghmans, T.; Snoeijs, M.G.; Sosef, M.N.; Hulsewe, K.W.; Luyer, M.D. Risk of anastomotic leakage with non-steroidal anti-inflammatory drugs in colorectal surgery. Br. J. Surg. 2012, 99, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Dodwell, E.R.; Latorre, J.G.; Parisini, E.; Zwettler, E.; Chandra, D.; Mulpuri, K.; Snyder, B. NSAID exposure and risk of nonunion: A meta-analysis of case-control and cohort studies. Calcif. Tissue Int. 2010, 87, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Rivers, J.M. Safety of high-level vitamin C ingestion. Ann. N. Y. Acad. Sci. 1987, 498, 445–454. [Google Scholar] [CrossRef]
- Elia, N.; Lysakowski, C.; Tramèr, M.R. Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials. Anesthesiology 2005, 103, 1296–1304. [Google Scholar] [CrossRef]
- Remy, C.; Marret, E.; Bonnet, F. Effects of acetaminophen on morphine side-effects and consumption after major surgery: Meta-analysis of randomized controlled trials. Br. J. Anaesth. 2005, 94, 505–513. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.K.; Park, S.K.; Zhou, J.L.; Taglialatela, G.; Chung, K.; Coggeshall, R.E.; Chung, J.M. Reactive oxygen species (ROS) play an important role in a rat model of neuropathic pain. Pain 2004, 111, 116–124. [Google Scholar] [CrossRef]
- Rebec, G.V.; Pierce, R.C. A vitamin as neuromodulator: Ascorbate release into the extracellular fluid of the brain regulates dopaminergic and glutamatergic transmission. Prog. Neurobiol. 1994, 43, 537–565. [Google Scholar] [CrossRef]
- Rosa, K.A.; Gadotti, V.M.; Rosa, A.O.; Rodrigues, A.L.; Calixto, J.B.; Santos, A.R. Evidence for the involvement of glutamatergic system in the antinociceptive effect of ascorbic acid. Neurosci. Lett. 2005, 381, 185–188. [Google Scholar] [CrossRef]
- Willis, W.D.; Westlund, K.N. Neuroanatomy of the pain system and of the pathways that modulate pain. J. Clin. Neurophysiol. 1997, 14, 2–31. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.B.; Satterlee, D.G.; Cadd, G.G. Timidity in Japanese quail: Effects of vitamin C and divergent selection for adrenocortical response. Physiol. Behav. 1999, 67, 117–120. [Google Scholar] [CrossRef]
- Harrison, F.E.; Yu, S.S.; Van Den Bossche, K.L.; Li, L.; May, J.M.; McDonald, M.P. Elevated oxidative stress and sensorimotor deficits but normal cognition in mice that cannot synthesize ascorbic acid. J. Neurochem. 2008, 106, 1198–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, M.E. Ascorbate regulation and its neuroprotective role in the brain. Trends Neurosci. 2000, 23, 209–216. [Google Scholar] [CrossRef]
- Fukushima, R.; Yamazaki, E. Vitamin C requirement in surgical patients. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 669–676. [Google Scholar] [CrossRef]
- Karanicolas, P.J.; Smith, S.E.; Kanbur, B.; Davies, E.; Guyatt, G.H. The impact of prophylactic dexamethasone on nausea and vomiting after laparoscopic cholecystectomy: A systematic review and meta-analysis. Ann. Surg. 2008, 248, 751–762. [Google Scholar] [CrossRef]
- Ghorbaninezhad, K.; Bakhsha, F.; Yousefi, Z.; Halakou, S.; Mehrbakhsh, Z. Comparison Effect of Tranexamic Acid (TA) and Tranexamic Acid Combined with Vitamin C (TXC) on Drainage Volume and Atrial Fibrillation Arrhythmia in Patients Undergoing Cardiac Bypass Surgery: Randomized Clinical Trial. Anesth. Pain Med. 2019, 9, e96096. [Google Scholar] [CrossRef] [Green Version]
- Blee, T.H.; Cogbill, T.H.; Lambert, P.J. Hemorrhage associated with vitamin C deficiency in surgical patients. Surgery 2002, 131, 408–412. [Google Scholar] [CrossRef]
- Padayatty, S.J.; Sun, H.; Wang, Y.; Riordan, H.D.; Hewitt, S.M.; Katz, A.; Wesley, R.A.; Levine, M. Vitamin C pharmacokinetics: Implications for oral and intravenous use. Ann. Intern. Med. 2004, 140, 533–537. [Google Scholar] [CrossRef]
- Jain, S.K.; Dar, M.Y.; Kumar, S.; Yadav, A.; Kearns, S.R. Role of anti-oxidant (vitamin-C) in post-operative pain relief in foot and ankle trauma surgery: A prospective randomized trial. Foot Ankle Surg. 2019, 25, 542–545. [Google Scholar] [CrossRef]
- Dick, F.; Tevaearai, H. Significance and Limitations of the p Value. Eur. J. Vasc. Endovasc. Surg. 2015, 50, 815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.-K.; Chuang, C.-C.; Chen, J.-Y. Relief of acute herpetic pain by intravenous vitamin C: The dosage may make a difference. Ann. Dermatol. 2018, 30, 262–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]














| Author/Year | Vitamin C Dosage | Time of Administration | Route | Analgesia Methods | Surgical Procedures | Surgical Time (V vs. P) | Patient Number /Age | Follow-Up Time |
|---|---|---|---|---|---|---|---|---|
| Ayatollahi 2017 [5] | 3 g | 30 min after the BOS | i.v. | Pethidine bolus ‡ | Uvulopalatopharyngoplasty and tonsillectomy | 111.8 ± 20.8 vs. 113.7 ± 20.9 min | n = 40; 25–50 years | 24 h |
| Jarahzadeh 2019 [21] | 2 g | 30 min after the AI | i.v. | NA | Laparoscopic surgery | NA | n = 70; 20–60 years | 24 h |
| Jeon 2016 [22] | 50 mg/kg | Immediately after AI | i.v. | PCA with morphine | Laparoscopic colectomy | 160.2 ± 39.3 vs. 160.7 ± 46.0 min | n = 97; 20–75 years | 24 h |
| Kanazi 2012 [23] | 2 g | 60 min before AI | oral | PCA with morphine | Laparoscopic cholecystectomy | 98.8 ± 33.6 vs. 91.3 ± 31.3 min | n = 80; 18–75 years | 24 h |
| Tunay 2020 [24] | 2 g | 60 min before BOS | oral | PCA with morphine | Major abdominal surgery | 84.5 ± 23.9 vs. 94.5 ± 27.5 min | n = 110, 18–65 years | 24 h |
| Moon 2019 [26] | 0.5 g twice a day | The day of surgery to the third day after surgery | i.v. | PCA with fentanyl | Laparoscopic hysterectomy | 99.0 ± 30.3 vs. 96.0 ± 19.4 min | n = 60, 20–60 years | 72 h |
| Moon 2020 [25] | 50 mg/kg | Immediately prior to AI | i.v. | PCA with fentanyl | Laparoscopic gynecologic surgery | 78.4 ± 34.7 vs. 92.8 ± 30 min | n = 66, 20–60 years | 48 h |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, K.-C.; Lin, Y.-T.; Chen, K.-H.; Wang, L.-K.; Chen, J.-Y.; Chang, Y.-J.; Wu, S.-C.; Chiang, M.-H.; Sun, C.-K. The Effect of Perioperative Vitamin C on Postoperative Analgesic Consumption: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2020, 12, 3109. https://doi.org/10.3390/nu12103109
Hung K-C, Lin Y-T, Chen K-H, Wang L-K, Chen J-Y, Chang Y-J, Wu S-C, Chiang M-H, Sun C-K. The Effect of Perioperative Vitamin C on Postoperative Analgesic Consumption: A Meta-Analysis of Randomized Controlled Trials. Nutrients. 2020; 12(10):3109. https://doi.org/10.3390/nu12103109
Chicago/Turabian StyleHung, Kuo-Chuan, Yao-Tsung Lin, Kee-Hsin Chen, Li-Kai Wang, Jen-Yin Chen, Ying-Jen Chang, Shao-Chun Wu, Min-Hsien Chiang, and Cheuk-Kwan Sun. 2020. "The Effect of Perioperative Vitamin C on Postoperative Analgesic Consumption: A Meta-Analysis of Randomized Controlled Trials" Nutrients 12, no. 10: 3109. https://doi.org/10.3390/nu12103109
APA StyleHung, K.-C., Lin, Y.-T., Chen, K.-H., Wang, L.-K., Chen, J.-Y., Chang, Y.-J., Wu, S.-C., Chiang, M.-H., & Sun, C.-K. (2020). The Effect of Perioperative Vitamin C on Postoperative Analgesic Consumption: A Meta-Analysis of Randomized Controlled Trials. Nutrients, 12(10), 3109. https://doi.org/10.3390/nu12103109