Prognostic Effect of a Novel Simply Calculated Nutritional Index in Acute Decompensated Heart Failure
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients with TCBI ≥ 745 and TCBI < 745
3.2. Nutritional Indexes and Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Casas-Vara, A.; Santolaria, F.; Fernández-Bereciartúa, A.; González-Reimers, E.; García-Ochoa, A.; Martínez-Riera, A. The obesity paradox in elderly patients with heart failure: Analysis of nutritional status. Nutrients 2012, 28, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Takikawa, T.; Sumi, T.; Takahara, K.; Kawamura, Y.; Ohguchi, S.; Oguri, M.; Ishii, H.; Murohara, T. Prognostic Importance of Multiple Nutrition Screening Indexes for 1-Year Mortality in Hospitalized Acute Decompensated Heart Failure Patients. Circ. Rep. 2019, 1, 87–93. [Google Scholar] [CrossRef]
- Kunimura, A.; Ishii, H.; Uetani, T.; Aoki, T.; Harada, K.; Hirayama, K.; Negishi, Y.; Shibata, Y.; Sumi, T.; Kawashima, K.; et al. Impact of Geriatric Nutritional Risk Index on cardiovascular outcomes in patients with stable coronary artery disease. J. Cardiol. 2017, 69, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Wada, H.; Dohi, T.; Miyauchi, K.; Doi, S.; Naito, R.; Konishi, H.; Tsuboi, S.; Ogita, M.; Kasai, T.; Hassan, A.; et al. Prognostic Impact of the Geriatric Nutritional Risk Index on Long-Term Outcomes in Patients Who Underwent Percutaneous Coronary Intervention. Am. J. Cardiol. 2017, 119, 1740–1745. [Google Scholar] [CrossRef]
- Narumi, T.; Arimoto, T.; Funayama, A.; Kadowaki, S.; Otaki, Y.; Nishiyama, S.; Takahashi, H.; Shishido, T.; Miyashita, T.; Miyamoto, T.; et al. The prognostic importance of objective nutritional indexes in patients with chronic heart failure. J. Cardiol. 2013, 62, 307–313. [Google Scholar] [CrossRef]
- Sze, S.; Zhang, J.; Pellicori, P.; Morgan, D.; Hoye, A.; Clark, A.L. Prognostic value of simple frailty and malnutrition screening tools in patients with acute heart failure due to left ventricular systolic dysfunction. Clin. Res. Cardiol. 2017, 106, 533–541. [Google Scholar] [CrossRef]
- Doi, S.; Iwata, H.; Wada, H.; Funamizu, T.; Shitara, J.; Endo, H.; Naito, R.; Konishi, H.; Tsuboi, S.; Ogita, M.; et al. A novel and simply calculated nutritional index serves as a useful prognostic indicator in patients with coronary artery disease. Int. J. Cardiol. 2018, 262, 92–98. [Google Scholar] [CrossRef]
- Minami-Takano, A.; Iwata, H.; Miyosawa, K.; Kubota, K.; Kimura, A.; Osawa, S.; Shitara, M.; Okazaki, S.; Suwa, S.; Miyauchi, K.; et al. A Novel Nutritional Index Serves as A Useful Prognostic Indicator in Cardiac Critical Patients Requiring Mechanical Circulatory Support. Nutrients 2019, 11, 1420. [Google Scholar] [CrossRef]
- Lee, G.; Go, S.; Kim, D.-W.; Kim, H.; Kim, J.; An, H.J.; Jang, J.S.; Kim, B.; Hahn, S.; Heo, D.S. Geriatric Nutritional Risk Index as a prognostic marker in patients with extensive-stage disease small cell lung cancer: Results from a randomized controlled trial. Thorac. Cancer 2019, 11, 62–71. [Google Scholar] [CrossRef]
- Yamana, I.; Takeno, S.; Shimaoka, H.; Yamashita, K.; Yamada, T.; Shiwaku, H.; Hashimoto, T.; Yamashita, Y.; Hasegawa, S. Geriatric Nutritional Risk Index as a prognostic factor in patients with esophageal squamous cell carcinoma –retrospective cohort study. Int. J. Surg. 2018, 56, 44–48. [Google Scholar] [CrossRef]
- Hirose, S.; Miyazaki, S.; Yatsu, S.; Sato, A.; Ishiwata, S.; Matsumoto, H.; Shitara, J.; Murata, A.; Kato, T.; Suda, S.; et al. Impact of the Geriatric Nutritional Risk Index on In-Hospital Mortality and Length of Hospitalization in Patients with Acute Decompensated Heart Failure with Preserved or Reduced Ejection Fraction. J. Clin. Med. 2020, 9, 1169. [Google Scholar] [CrossRef] [PubMed]
- Sato, N.; Kajimoto, K.; Asai, K.; Mizuno, M.; Minami, Y.; Nagashima, M.; Murai, K.; Muanakata, R.; Yumino, D.; Meguro, T.; et al. Acute decompensated heart failure syndromes (ATTEND) registry. A prospective observational multicenter cohort study: Rationale, design, and preliminary data. Am. Heart J. 2010, 159, 949–955.e1. [Google Scholar] [CrossRef] [PubMed]
- Sato, N.; Kajimoto, K.; Keida, T.; Mizuno, M.; Minami, Y.; Yumino, D.; Asai, K.; Murai, K.; Muanakata, R.; Aokage, T.; et al. Clinical Features and Outcome in Hospitalized Heart Failure in Japan (From the ATTEND Registry). Circ. J. 2013, 77, 944–951. [Google Scholar] [CrossRef]
- McKee, P.A.; Castelli, W.P.; McNamara, P.M.; Kannel, W.B. The Natural History of Congestive Heart Failure: The Framingham Study. N. Engl. J. Med. 1971, 285, 1441–1446. [Google Scholar] [CrossRef]
- Matsuo, S.; Imai, E.; Horio, M.; Yasuda, Y.; Tomita, K.; Nitta, K.; Yamagata, K.; Tomino, Y.; Yokoyama, H.; Hishida, A. Revised Equations for Estimated GFR From Serum Creatinine in Japan. Am. J. Kidney Dis. 2009, 53, 982–992. [Google Scholar] [CrossRef]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.-P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef]
- Kenchaiah, S.; Sesso, H.D.; Gaziano, J.M. Response to Letter Regarding Article, “Body Mass Index and Vigorous Physical Activity and the Risk of Heart Failure Among Men”. Circulation 2009, 120. [Google Scholar] [CrossRef][Green Version]
- Rauchhaus, M.; Clark, A.L.; Doehner, W.; Davos, C.H.; Bolger, A.; Sharma, R.; Coats, A.J.; Anker, S.D. The relationship between cholesterol and survival in patients with chronic heart failure. J. Am. Coll. Cardiol. 2003, 42, 1933–1940. [Google Scholar] [CrossRef]
- Horwich, T.B.; Hernandez, A.F.; Dai, D.; Yancy, C.W.; Fonarow, G.C. Cholesterol levels and in-hospital mortality in patients with acute decompensated heart failure. Am. Heart J. 2008, 156, 1170–1176. [Google Scholar] [CrossRef]
- Zhang, Z.; Pereira, S.L.; Luo, M.; Matheson, E.M. Evaluation of Blood Biomarkers Associated with Risk of Malnutrition in Older Adults: A Systematic Review and Meta-Analysis. Nutrients 2017, 9, 829. [Google Scholar] [CrossRef]
- Kozdag, G.; Ertas, G.; Emre, E.; Akay, Y.; Celikyurt, U.; Sahin, T.; Gorur, G.; Karauzum, K.; Yilmaz, I.; Ural, D.; et al. Low Serum Triglyceride Levels as Predictors of Cardiac Death in Heart Failure Patients. Tex. Heart Inst. J. 2013, 40, 521–528. [Google Scholar]
- Goldwasser, P.; Feldman, J. Association of serum albumin and mortality risk. J. Clin. Epidemiol. 1997, 50, 693–703. [Google Scholar] [CrossRef]
- Horwich, T.B.; Kalantar-Zadeh, K.; MacLellan, R.W.; Fonarow, G.C. Albumin levels predict survival in patients with systolic heart failure. Am. Heart J. 2008, 155, 883–889. [Google Scholar] [CrossRef]
- Uthamalingam, S.; Kandala, J.; Daley, M.; Patvardhan, E.; Capodilupo, R.; Moore, S.A.; Januzzi, J.L. Serum albumin and mortality in acutely decompensated heart failure. Am. Heart J. 2010, 160, 1149–1155. [Google Scholar] [CrossRef]
- Yatsu, S.; Kasai, T.; Matsumoto, H.; Shitara, J.; Shimizu, M.; Murata, A.; Kato, T.; Suda, S.; Hiki, M.; Takagi, A.; et al. Relationship between Hypoalbuminemia on Admission and Long-term Mortality in Patients with Acute Decompensated Heart Failure. Intern. Med. 2019, 58, 1695–1702. [Google Scholar] [CrossRef]
- Nakayama, H.; Koyama, S.; Kuragaichi, T.; Shiba, M.; Fujiwara, H.; Takatsu, Y.; Sato, Y. Prognostic Value of Rising Serum Albumin During Hospitalization in Patients With Acute Heart Failure. Am. J. Cardiol. 2016, 117, 1305–1309. [Google Scholar] [CrossRef]
- Honda, Y.; Nagai, T.; Iwakami, N.; Sugano, Y.; Honda, S.; Okada, A.; Asaumi, Y.; Aiba, T.; Noguchi, T.; Kusano, K.; et al. Usefulness of Geriatric Nutritional Risk Index for Assessing Nutritional Status and Its Prognostic Impact in Patients Aged ≥ 65 Years With Acute Heart Failure. Am. J. Cardiol. 2016, 118, 550–555. [Google Scholar] [CrossRef]
- Nishi, I.; Seo, Y.; Hamada-Harimura, Y.; Sato, K.; Sai, S.; Yamamoto, M.; Ishizu, T.; Sugano, A.; Obara, K.; Wu, L.; et al. Nutritional screening based on the controlling nutritional status (CONUT) score at the time of admission is useful for long-term prognostic prediction in patients with heart failure requiring hospitalization. Heart Vessels 2017, 32, 1337–1349. [Google Scholar] [CrossRef] [PubMed]
- Iwakami, N.; Nagai, T.; Furukawa, T.A.; Sugano, Y.; Yasuda, S.; Okada, A.; Asaumi, Y.; Aiba, T.; Noguchi, T.; Kusano, K.; et al. Prognostic value of malnutrition assessed by Controlling Nutritional Status score for long-term mortality in patients with acute heart failure. Int. J. Cardiol. 2017, 230, 529–536. [Google Scholar] [CrossRef]
- Cheng, Y.; Sung, S.; Cheng, H.; Hsu, P.; Guo, C.; Yu, W.; Chen, C. Prognostic Nutritional Index and the Risk of Mortality in Patients With Acute Heart Failure. J. Am. Heart Assoc. 2017, 6, e004876. [Google Scholar] [CrossRef]

| TCBI < 745 n = 209 | TCBI ≥ 745 n = 208 | p | |
|---|---|---|---|
| Age, year | 74.2 ± 11.0 | 65.7 ± 14.2 | <0.001 |
| Gender (male), n (%) | 123 (58.8) | 147 (70.6) | 0.013 |
| BMI, kg/m2 | 21.2 ± 3.7 | 24.6 ± 5.4 | <0.001 |
| BW, kg | 52.7 ± 12.4 | 65.8 ± 18.5 | <0.001 |
| NYHA class II, (%) | 30 (14.3) | 43 (20.6) | 0.228 |
| III, (%) | 76 (36.3) | 68 (32.6) | |
| IV, (%) | 103 (49.2) | 97 (46.6) | |
| Ischemic heart disease, n (%) | 95 (45.4) | 91 (43.7) | 0.767 |
| History of heart failure, n (%) | 108 (56.6) | 105 (50.4) | 0.844 |
| AF, n (%) | 94 (44.9) | 91 (34.1) | 0.027 |
| Diabetes mellitus, n (%) | 61 (29.1) | 90 (43.2) | 0.003 |
| ICD, n (%) | 4 (1.9) | 4 (1.9) | 1.000 |
| CRT, n (%) | 1 (0.4) | 1 (0.4) | 1.000 |
| Mean BP, mmHg | 95.3 ± 19.1 | 101.1 ± 23.6 | 0.011 |
| Systolic BP, mmHg | 136.3 ± 29.4 | 140.8 ± 33.8 | 0.182 |
| Diastolic BP, mmHg | 74.7 ± 17.3 | 81.4 ± 21.4 | 0.001 |
| HR, rate/min | 93.1 ± 29.4 | 96.7 ± 27.7 | 0.239 |
| LVEF, % | 44.3 ± 17.9 | 40.3 ± 16.0 | 0.018 |
| Hemoglobin, g/dL | 11.8 ± 2.2 | 13.2 ± 2.4 | <0.001 |
| eGFR, mL/min/1.73 m2 | 53.9 ± 27.1 | 53.9 ± 23.3 | 0.991 |
| BUN, mg/dL | 26.1 ± 14.7 | 26.2 ± 17.0 | 0.934 |
| Sodium, mmol/L | 138.2 ± 4.4 | 139.2 ± 3.8 | 0.010 |
| Potassium, mmol/L | 4.2 ± 0.6 | 4.2 ± 0.6 | 0.269 |
| TC, mg/dl | 147 ± 31.3 | 191 ± 41.7 | <0.001 |
| TG, mg/dl | 64.2 ± 19.8 | 132.2 ± 71.6 | <0.001 |
| CRP, mg/dL | 0.9 [3.3] | 0.7 [2.9] | 0.975 |
| BNP, pg/mL | 679 [793.4] | 529.2 [698.1] | 0.176 |
| Medications at admission | |||
| Beta blocker, n (%) | 61 (29.1) | 68 (32.6) | 0.459 |
| ACE-Is/ARBs, n (%) | 74 (35.4) | 83 (39.9) | 0.364 |
| Aldosterone blocker, n (%) | 35 (16.7) | 19 (9.1) | 0.028 |
| Diuretics, n (%) | 87 (41.6) | 62 (29.8) | 0.014 |
| Statin, n (%) | 51 (24%) | 38 (18.3%) | 0.951 |
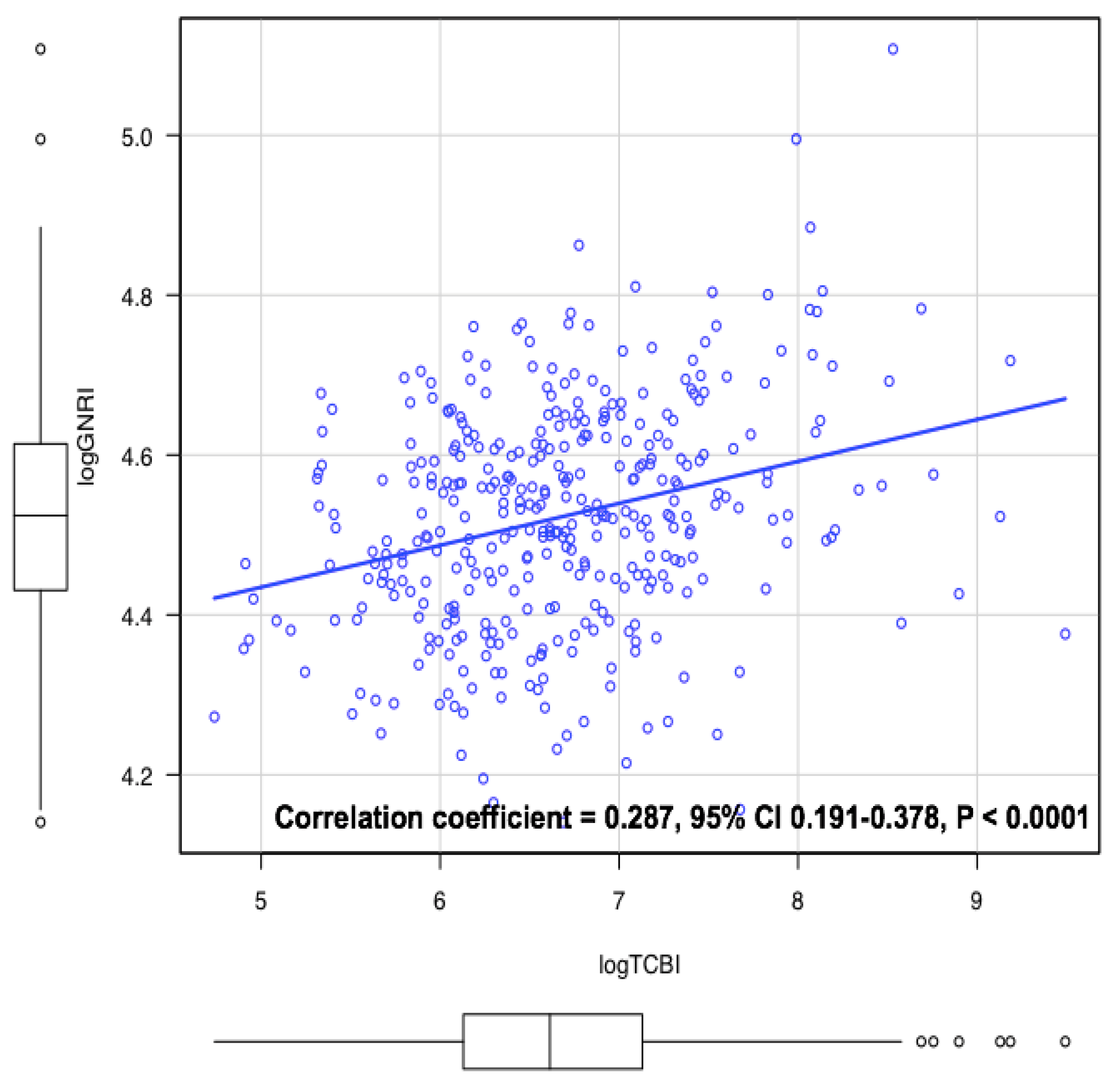
| GNRI | 89.5 [17.2] | 94.3 [17.7] | <0.001 |
| Univariable | Multivariable | ||||
|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | ||
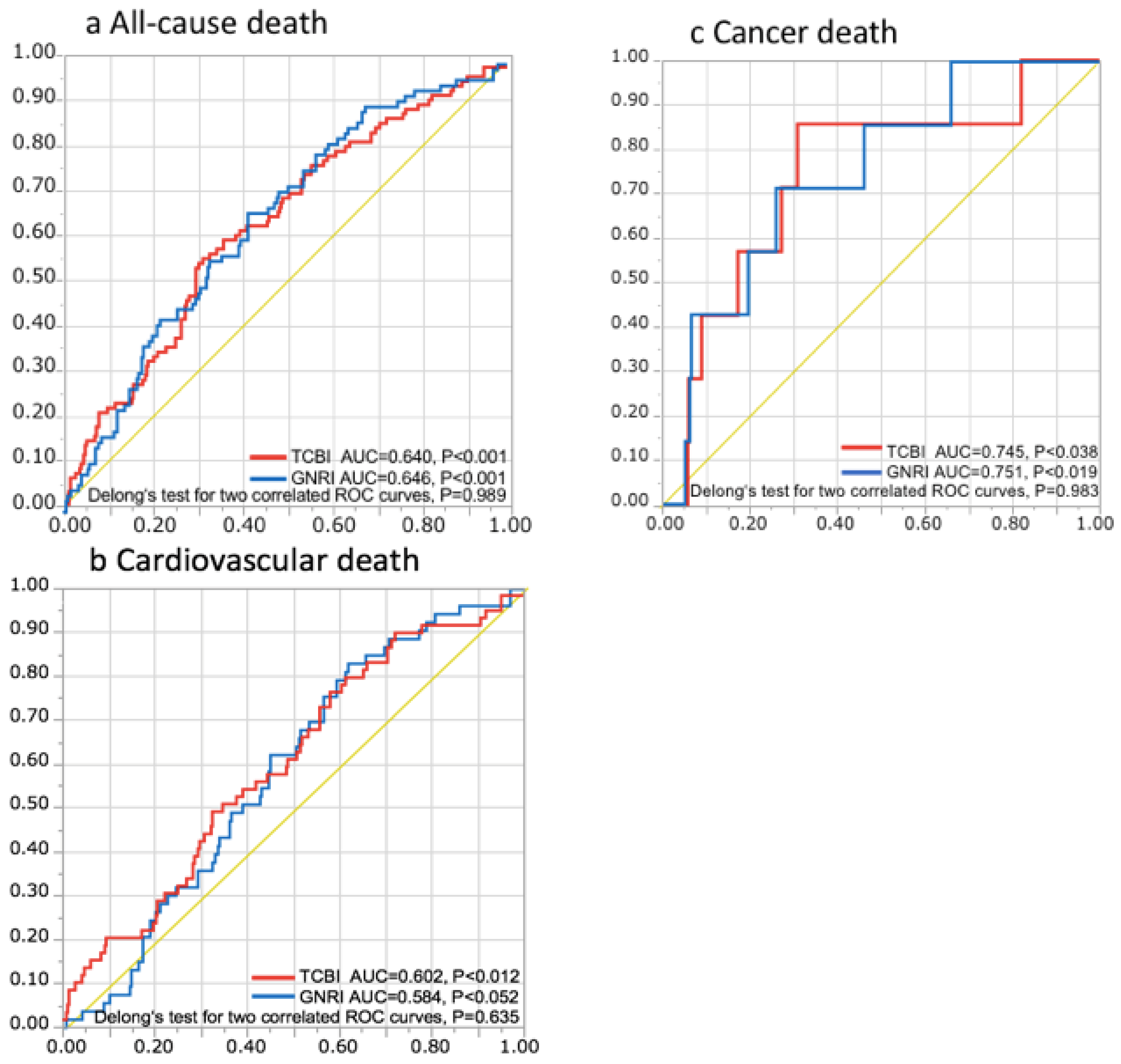
| a. All-cause deaths | Age (1 year increase) | 1.05 (1.04–1.07) | <0.001 | 1.02 (1.00–1.04) | 0.031 |
| Gender, male | 1.67 (1.11–2.51) | 0.014 | |||
| Ischemic heart disease, yes | 1.77 (1.18–2.68) | 0.006 | |||
| AF, yes | 1.49 (0.97–2.33) | 0.070 | |||
| Mean BP (1 mmHg increase) | 0.99 (0.98–1.00) | 0.017 | |||
| Hemoglobin (1 g/dL increase) | 0.73 (0.67–0.80) | <0.001 | 0.86 (0.78–0.95) | 0.004 | |
| Na (1 mmol/L increase) | 0.92 (0.88–0.96) | <0.001 | 0.91 (0.87–0.95) | <0.001 | |
| eGFR (1 mL/min/1.73 m2 increase) | 0.97 (0.97–0.99) | <0.001 | |||
| BUN (1 mg/dL increase) | 1.02 (1.01–1.03) | <0.001 | 1.02 (1.00–1.03) | 0.003 | |
| History of HF, yes | 2.30 (1.51–3.61) | <0.001 | |||
| Diuretics, yes | 2.48 (1.65–3.74) | <0.001 | 2.3 (1.45–3.72) | <0.001 | |
| Log CRP (1 increase) | 1.19 (1.05–1.35) | 0.007 | |||
| Log BNP (1 increase) | 1.39 (1.13–1.72) | 0.002 | |||
| Log GNRI (1 increase) | 0.03 (0.01–0.15) | <0.001 | |||
| Log TCBI (1 increase) | 0.51 (0.38–0.68) | <0.001 | 0.64 (0.44–0.94) | 0.024 | |
| b. Cardiovascular deaths | Age (1 year increase) | 1.05 (1.02–1.07) | <0.001 | 1.03 (1.00–1.06) | 0.019 |
| Hemoglobin (1 g/dL increase) | 0.73 (0.65–0.81) | <0.001 | 0.82 (0.72–0.93) | 0.002 | |
| Sodium (1 mmol/L increase) | 0.93 (0.88–0.99) | 0.034 | 0.93 (0.87–0.99) | 0.026 | |
| BUN (1 mg/dL increase) | 1.02 (1.01–1.03) | <0.001 | |||
| Diuretics, yes | 3.97 (2.33–6.98) | <0.001 | 3.39 (1.91–6.21) | <0.001 | |
| Aldosterone blocker, yes | 2.34 (1.26–4.13) | 0.009 | |||
| Beta blocker, yes | 1.79 (1.05–3.00) | 0.032 | |||
| Log BNP (1 increase) | 1.64 (1.24–2.19) | <0.001 | |||
| Log GNRI (1 increase) | 0.09 (0.01–0.66) | 0.018 | |||
| Log TCBI (1 increase) | 0.55 (0.38–0.79) | 0.001 | |||
| c. Cancer deaths | Hemoglobin (1 g/dL increase) | 0.71 (0.50–0.96) | 0.028 | ||
| LVEF (1 increase) | 1.06 (1.01–1.12) | 0.023 | 1.05 (1.0–1.12) | 0.016 | |
| Log GNRI (1 increase) | 0.01 (0.01–0.15) | 0.008 | 0.01 (0.01–0.1) | 0.006 | |
| Log TCBI (1 increase) | 0.25 (0.08–0.77) | 0.014 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishiwata, S.; Yatsu, S.; Kasai, T.; Sato, A.; Matsumoto, H.; Shitara, J.; Shimizu, M.; Murata, A.; Kato, T.; Suda, S.; et al. Prognostic Effect of a Novel Simply Calculated Nutritional Index in Acute Decompensated Heart Failure. Nutrients 2020, 12, 3311. https://doi.org/10.3390/nu12113311
Ishiwata S, Yatsu S, Kasai T, Sato A, Matsumoto H, Shitara J, Shimizu M, Murata A, Kato T, Suda S, et al. Prognostic Effect of a Novel Simply Calculated Nutritional Index in Acute Decompensated Heart Failure. Nutrients. 2020; 12(11):3311. https://doi.org/10.3390/nu12113311
Chicago/Turabian StyleIshiwata, Sayaki, Shoichiro Yatsu, Takatoshi Kasai, Akihiro Sato, Hiroki Matsumoto, Jun Shitara, Megumi Shimizu, Azusa Murata, Takao Kato, Shoko Suda, and et al. 2020. "Prognostic Effect of a Novel Simply Calculated Nutritional Index in Acute Decompensated Heart Failure" Nutrients 12, no. 11: 3311. https://doi.org/10.3390/nu12113311
APA StyleIshiwata, S., Yatsu, S., Kasai, T., Sato, A., Matsumoto, H., Shitara, J., Shimizu, M., Murata, A., Kato, T., Suda, S., Doi, S., Hiki, M., Matsue, Y., Naito, R., Iwata, H., Takagi, A., & Daida, H. (2020). Prognostic Effect of a Novel Simply Calculated Nutritional Index in Acute Decompensated Heart Failure. Nutrients, 12(11), 3311. https://doi.org/10.3390/nu12113311






