Diet Quality Indices Used in Australian and New Zealand Adults: A Systematic Review and Critical Appraisal
Abstract
1. Introduction
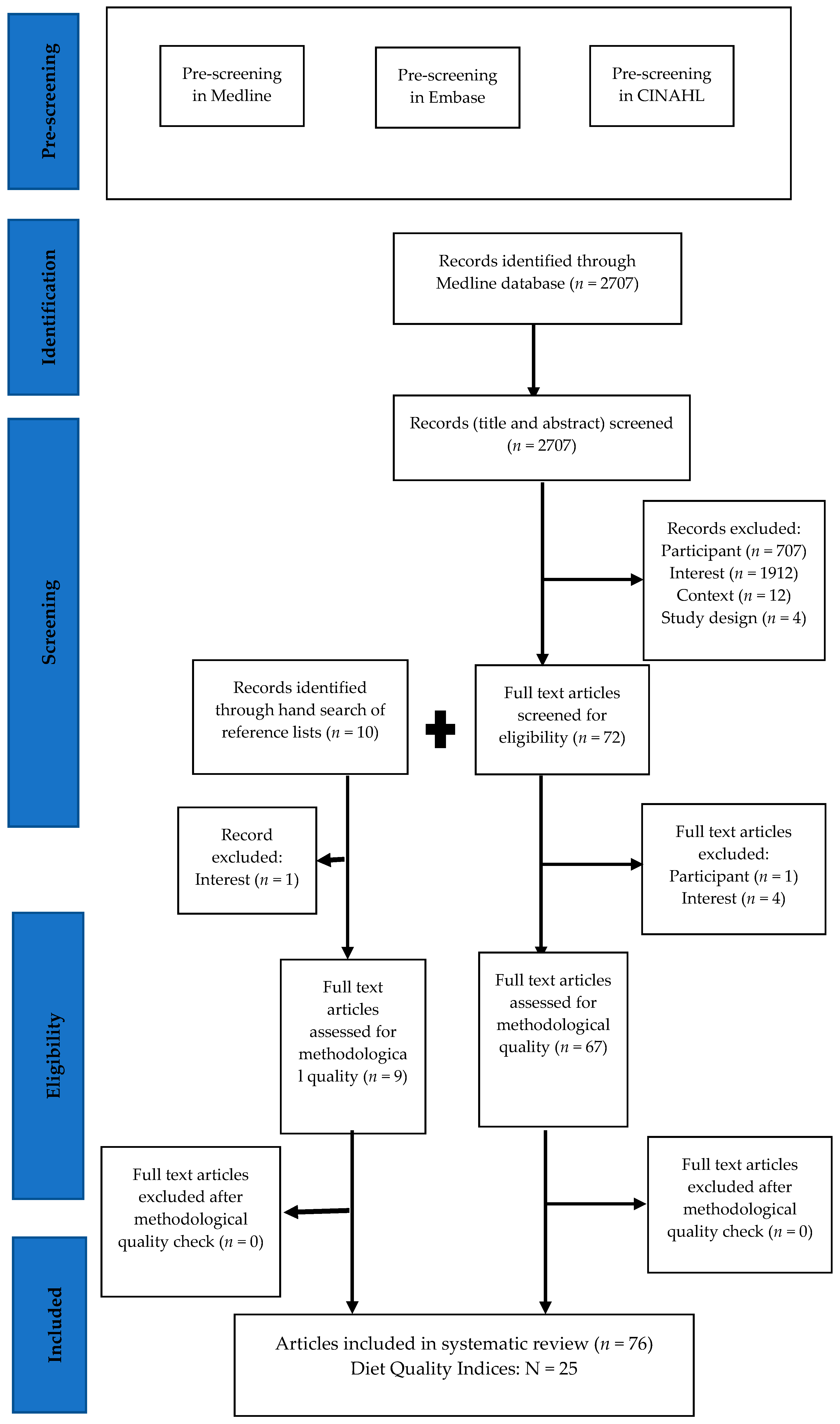
2. Materials and Methods
2.1. Developing the Search Strategy and Databases to Be Included
2.2. Inclusion/Exclusion Criteria for Eligible Studies
2.3. Screening Procedure
2.4. Quality of the Evidence
2.5. Data Extraction
3. Results
3.1. Australian and New Zealand Diet Quality Indices
| Index | Reference | Theoretical or Epidemiological Basis | Original Tool (Local or International) | Modified or Adapted Intermediate Tool | Components | Evaluation of Diet Quality Index |
|---|---|---|---|---|---|---|
| Based on Australian Dietary Guidelines | ||||||
| Australian Healthy Eating Index (Aust-HEI) | Australian Institute of Health and Welfare, 2007 [28] | Australian Guide to Healthy Eating (AGHE), 1998 [59], Dietary Guidelines for Australian Adults, 2003 [60] | - | Variety score from previous food variety score [56] and Diet Quality Index-Revised [57]; Healthy choice score from Recommended Food Score [41] | Variety; healthy choices; fruit; vegetable; low-fat milk; trim fat meat; high saturated fat, low nutrient density food | Nutrient intakes, demographic and lifestyle characteristics, general health status |
| Australian Recommended Food Score-1 (ARFS-1) | Collins et al. 2015 [42] | Australian Dietary Guidelines-2013 [61] | Recommended Food Score [55] | Australian Recommended Food Score [29], Australian Child and Adolescent Recommended Food Score [62] | Vegetable; fruit; protein foods; grains; dairy; fats; alcohol | Nutrient intakes |
| Commonwealth Scientific and Industrial Research Organization- Healthy Diet Score (CSIRO HDS) | Hendrie et al. 2017 [63] | Australian Dietary Guidelines-2013 [61] | - | Dietary Guideline Index [19] | Variety; vegetables; fruits; whole-grain cereals; meat and alternatives; dairy and alternatives; water; discretionary foods; trim fat; fats and oils; salt; sugar; alcohol | Mean dietary score component |
| Total Diet Score (TDS) | Russell et al. 2013 [33] | Australian Guide to Healthy Eating (AGHE), 1998 [59], Dietary Guidelines for Australian Adults, 2003 [60] | US 2005 Dietary Guidelines Adherence Index [58] | Australian Healthy Eating Index [28] | Vegetables, legumes and fruit; cereals/whole grains; lean meats and alternatives; dairy and alternatives; saturated fat; sodium; alcohol; sugar; extra food; physical activity | All-cause mortality |
| Aussie-Diet Quality Index (Aussie-DQI) | Zarrin et al. 2013 [18] | Australian Guide to Healthy Eating (AGHE), 1998 [59], Dietary Guidelines for Australian Adults, 2003 [60] | Australia National Health Priority Area (ANHPA) [64] | Australian Healthy Eating Index [28], Dietary Guideline Index [19] | Vegetables; fruits; dairy products; meat and alternatives; cereals; saturated fat; sugar; alcohol; processed meat; salt/sodium; variety | Sociodemographic and lifestyle characteristics, cancer mortality |
| Healthy Eating Index for Australian-2013 (HEIFA-2013) | Roy et al. 2016 [16] | Australian Dietary Guidelines-2013 [61] | - | - | Discretionary foods; vegetables; fruits; whole grains; protein foods; dairy; water; saturated fat; sodium; sugar; alcohol | Nutrient intakes |
| Australian Diet Quality Score (ADQS) | Froud et al. 2019 [30] | Recommended Daily Intake (RDI) of the Australian Dietary Guidelines (not specified) | - | - | Vegetable; fruits; whole grains; processed grains; dairy; proteins; nuts; seafood; fats ratio; extras ratio | Nil |
| Based on New Zealand Dietary Guidelines | ||||||
| Healthy Dietary Habits Index (HDHI) | Wong et al. 2017 [20] | New Zealand food and nutrition guidelines for healthy adults [43] | Healthy Dietary Habit Score for New Zealand adolescents [65] | - | Red meat; chicken; fish/shellfish; milk; spread; low-fat foods; fries; bread; fruits; vegetable; soft drinks; breakfast; fast foods; added salt; low salt food | Nutrient intakes, biomarker |
| Based on US Dietary Guidelines | ||||||
| Diet Quality Index-Revised (DQI-R) | Haines et al. 1999 [8] | 1989-Dietary recommendations from the US National Academy of Sciences and Dietary Guidelines for Americans [44], dietary reference intakes [45] | Diet Quality Index [10] | - | Total fat; saturated fat; cholesterol; fruits; vegetables; grains; calcium; iron; diversity; moderation | Nutrient intakes |
| Recommended Food Score (RFS) | Kant and Graubaud, 2000 [41] | 1989-Dietary recommendations from the US National Academy of Sciences and Dietary Guidelines for Americans [44], epidemiological evidence [46] | Developed by Kant and Graubaud [41] | - | Fruits; vegetables; whole grains; lean meat or alternatives; low-fat dairy | Mortality |
| Not Recommended Food Score (NRFS) | Michels et al. 2002 [31] | 1989-Dietary recommendations from the US National Academy of Sciences and Dietary Guidelines for Americans [44], epidemiological evidence [46] | US Dietary guidelines and results of large epidemiological studies [31] | - | Meat and its products; fried food; foods high in fat; others | Mortality |
| Specific Dietary Pattern Recommendations | ||||||
| Mediterranean Diet Scale (MDS) | Trichopoulou et al. 2005 [39] | Assessment of adherence to a Mediterranean diet developed by Trichopoulou et al. [21] | - | Grains; vegetables; nuts and legumes; fruits; fish; olive oil; dairy products; red and processed meat; alcohol | Mortality | |
| Dietary Approach to Stop Hypertension (DASH) | Fung et al. 2008 [15] | Guideline for lowering blood pressure [53] | - | Fruits; vegetables; nuts and legumes; whole grains; low-fat dairy; sodium; red and processed meat; sweetened beverage | CHD and stroke risk | |
| Alternative Healthy Eating Index-2010 (AHEI-2010) | Chiuve et al. 2012 [22] | Foods and nutrients that lowered chronic diseases based on the Mediterranean diet [48,49,50,51,52] | Healthy Eating Index [9] | Alternative Healthy Eating Index (AHEI) [23] | Vegetables; fruits; nuts and soy protein; ratio of white to red meat; cereal fiber; trans-fat; ratio of polyunsaturated to saturated fatty acids; alcohol; multivitamin use | Chronic disease risk |
| Diet Quality Tool (DQT) | O’Reilly et al. 2012 [32] | Heart Foundation’s secondary prevention nutrition guidelines [54] | - | - | Vegetable; fruits; rice, pasta or noodle; breakfast cereals; bread; spread; milk; trim fat meat; takeaway meals; discretionary foods; fish; salt use | Nutrient intakes |
| Dietary Inflammatory Index (DII) | Shivappa et al. 2014 [66] | Literature-derived, population-based dietary inflammatory index [34] | Original DII [67] | - | Nutrients, spices, whole food and other | High-sensitivity C-reactive protein |
3.2. Composition of Diet Quality Indices
3.3. Scoring of the Diet Quality Indices
3.4. Dietary Assessment Methods Used
3.5. Evaluation of Diet Quality Indices
3.6. Summary Findings of Studies Investigating Diet Quality Indices, Health Outcomes and Non-Health Related Factors
| Index | Reference | Validation Status of Diet Quality Index | Population Used in | Dietary Assessment Methods Used in Publications | Health-related Outcomes | Summary of Findings |
|---|---|---|---|---|---|---|
| Australian Healthy Eating Index (Aust-HEI) | Forsyth, 2012 [120] Forsyth, 2015 [121] | Tested construct validity [28] | Adults aged ≥18 years with depression and anxiety [120,121] | Diet History Questionnaire [120,121] | Depression, Anxiety and Stress Scale (DASS) [120,121] | Mean total Aust-HEI was 42.8 (range 20–60), and Aust-HEI and DASS were negatively correlated (p < 0.001) [120]. Improved DASS in the diet and physical activity intervention group (p < 0.05) [121]. |
| Australian Recommended Food Score (ARFS) | Collins, 2008 [29] Collins, 2011 [79] Morrison, 2012 [77] Aljadani, 2013 [74] Aljadani, 2013 [75] Alhazmi, 2014 [70] Potter, 2014 [78] Petersen, 2015 [71] Aljadani, 2016 [76] Kullen, 2016 [80] Lai, 2016 [72] Lai, 2017 [73] | Tested construct validity [29] | Adults aged ≥50 years [71]; mid-aged women (50–55 years) [29,70,72,73,74,76,78,79]; young women (mean age: 27.6 ± 1.5 years and 34.2 ± 5.1 years) [75,77]; young men (mean age: 28.7 ± 8.9 years) [80] | FFQ (74-item food and 6-item alcohol) [29,70,71,72,73,74,75,76,77,78,79,80] | Diabetes [70]; Depression [72,73]; Overweight or obese [74,75,76]; Diet quality [29,71,77,78,79,80] | No association between ARFS and diabetes risk [70]. Women who maintained moderate or high ARFS scores had a low risk of depression (p = 0.045 and 0.01) [73], but no longitudinal association between ARFS and depressive symptoms [72]. Association between ARFS and overweight or obesity is not consistent [74,75,76]. Factors associated with higher ARFS were socioeconomic status, education, marital status, smoking, physical activity (all p < 0.0001) [29]; age, education, physical activity (all p < 0.001) [77]; nutrition knowledge (p = 0.009) [80]. |
| Australian Recommended Food Score-1 (ARFS-1) | Baker, 2014 [122] O’ Brien, 2014 [123] Collins, 2015 [42] Ashton, 2017 [124] Ashton, 2017 [125] Williams, 2017 [35] Ashton, 2018 [126] Harbury, 2019 [118] | Tested reproducibility, comparative validity [42]; relative validity [124] | Adults aged ≥16 years [35], ≥18 years [118,122,123,124,126], ≥30 years [42]; young men aged 18–25 years [125] | Subset of 70 items from 120-item FFQ [42,118,122,123,124,125,126]; Healthy Eating Quiz (online survey, 70 items) [35] | Plasma carotenoid [124]; Weight loss [123]; Diet quality [42,118,122,125,126]. | Significant correlation between total ARFS-1 and plasma total carotenoids (r = 0.17, p < 0.05) [124]. The intervention groups significantly lost more weight than the control group after 12-weeks (p < 0.001) [123]. Factors associated with ARFS-1 were nutrition knowledge and BMI (p < 0.001) [118]. |
| Dietary Guideline Index (DGI) | McNaughton, 2008 [19] McNaughton, 2009 [100] Arabshahi, 2011 [101] Arabshahi, 2012 [102] Thorpe, 2013 [91] Alhazmi, 2014 [70] Backholer, 2016 [103] Olstad, 2017 [104] Smith, 2017 [105] | Tested construct validity [19] | Adults aged ≥19 years [19], 18–36 years [91], ≥25 years [100,101,102,103], 26–36 years [105]; mid-aged women (50–55 years) [70], women 18–46 years [104] | FFQs: 74-item [100], FFQ (74-item food and 6-item alcohol) [70,103], 107-item [91], 151-item [101,102], items not mentioned [104]; FFQ and others: 127-item FFQ and food habit questionnaire (FHQ) [105]; 108-item FFQ, single 24-h R [19] | Diabetes [70,100] and cardiometabolic risk factors [100]; Anthropometric measurements [102,104]; Diet quality [19,91,101,103,105] | DGI was negatively associated with diabetes in men (ORQ4-Q1:0.38, 95% CI: 0.18–0.80) [100] and women (ORQ5-Q1:0.51; 95% CI: 0.35, 0.76) [70]; hypertension in both sexes (ORQ4-Q1:0.5, 95% CI: 0.31–0.81) [100]. Association between DGI and waist circumference (WC) [100,102]; body mass index (BMI) [102,104] was inconsistent. Factors associated with DGI were sex (p < 0.05) [19], age (both p < 0.05) [19,101], education (p < 0.01) [103], income (p < 0.05, <0.01) [19,103], socioeconomic status (p < 0.05, <0.01) [19,103], smoking (p < 0.05) [19], physical activity (both p < 0.05) [19,101], occupation (p < 0.05) [101], hormonal replacement therapy (p < 0.05) [101], cooking meals for oneself (p = 0.001) [91], and takeaway and convenient meal consumption (p < 0.001) [91]. |
| Modified Dietary Guideline Index (Modified DGI) | McLeod, 2011 [37] | Not tested | Women (mean age = 32.3 years) [37] | 137-item FFQ [37] | Diet quality [37] | Diet quality was significantly better in women of a high socioeconomic group as compared to those of the low socioeconomic group (p < 0.001) [37]. |
| Dietary Guideline Index-2013 (DGI-2013) | Milte et al. 2015 [89] Livingstone, 2016 [84] Thorpe, 2016 [17] Leech, 2016 [81] Leech, 2017 [82] Livingstone, 2017 [83] Martin, 2017 [86] Ribeiro, 2017 [90] Livingstone, 2018 [85] Milte, 2018 [88] Martin, 2019 [87] | Tested construct validity [17] | Adults aged ≥19 years [81,82,83,84,85], 55–68 years [17,88,89]; women aged 18–50 years [86,87]; men aged ≥74 years [90] | FFQ (74-item food and 6-item alcohol) [86,87], 111-item FFQ and food-related behavior questions [17,88,89]; two 24-h Rs [81,82,83,84,85]; diet histories questionnaire [90] | Obesity [82,84,85,90] Hypertension [84]; health related quality of life (QOL) [89]; Telomere length [88]; Diet quality [17,81,83,86,87] | Higher DGI-2013 scores were negatively associated with obesity measured by BMI (both Ptrend < 0.05) [84,85], WC (both Ptrend < 0.05) [84,85], waist–hip ratio (WHR) (p < 0.001) [90]. Men with higher DGI-2013 were less likely to be hypertensive (Ptrend < 0.05) [84]. Higher DGI-2013 scores were associated with better health-related QOL (p < 0.05) [89]. No association between DGI-2013 and relative telomere length [88]. Factors associated with DGI-2013 were sex (p < 0.001), residence (men, p < 0.001) [17], occupation (men: p = 0.02; women: p = 0.043) [17,86], income (women: p = 0.013) [86], education (p < 0.001) [17], socioeconomic status (Ptrend < 0.001) [83], smoking (p < 0.001) [17], physical activity (p < 0.001) [17], BMI (p < 0.001) [17], frequency of meals (p < 0.001) [81]. |
| RESIDential Environments (RESIDE) Dietary Guideline Index (RDGI) | Bivoltsis, 2018 [36] | Not tested | Adults aged ≥25 years [36] | 24-item questionnaire (12 from validated FFQ, 12 from validated dietary behavior questions) [36] | Diet quality [36] | Two simple RESIDE dietary guideline indices using subsets of six survey items (S-RDGI1), and nine survey items (S-RDGI2) showed reasonable agreement with RDGI (Spearman rho = 0.78, 0.84). For all indices, higher diet quality was associated with sex (all p < 0.001), age (S-RDGI1 and S-RDGI2, p < 0.001), smoking status (S-RDGI1: p = 0.001, SRDGI and S-RDGI2: p < 0.001), physical activity (RDGI: p = 0.001, S-RDGI1: p < 0.0001, S-RDGI2: p = 0.002) [36]. |
| Commonwealth Scientific and Industrial Research Organization Healthy Diet Score (CSIRO HDS) | Hendrie, 2017 [63] Hendrie, 2017 [38] Hendrie, 2018 [127] | Tested reliability and relative validity [63] | Adults aged ≥18 years [38,127], aged 19–50 years [63] | 38-item SFS [38,127]; 38-item SFS and three 24-h Rs [63] | Obesity [127]; Diet quality [38,63] | Adults having a lower score were more likely to obese (ORQ1-Q5 2.99, CI: 2.88, 3.11) [127]. Women scored higher than men (59.9 ± 12.6 vs. 56.2 ± 13.1), older adults higher than younger adults (>71yr: 63.1 ± 11.7 vs. 18–30 yr: 57.3 ± 13.2), and normal-weight adults higher than obese adults (60.5 ± 12.6 vs. 55.7 ± 13.2) [38]. |
| Total Diet Score (TDS) | Russell, 2013 [33] Gopinath, 2013 [96] Gopinath, 2013 [95] Gopinath, 2013 [97] Gopinath, 2014 [98] Gopinath, 2014 [92] Hong, 2014 [94] Gopinath, 2016 [93] Roach, 2017 [99] Russell, 2017 [68] | Tested criterion validity [33] | Adults aged ≥49 years [33,93,94], ≥50 years [95,96,97,98], ≥55 years [92], 65–85 years [68], median age-72 years [99] | 145-item FFQ [33,92,93,94,95,96,97,98], 145-item FFQ and 4-day WFRs [68], three 24 h Rs and PUFA FFQ [99] | All-cause mortality [33]; Chronic kidney disease (CKD) [96], visual impairment [94], retinal vascular change [95], quality of life (QOL) [92], aging [93] Impaired fasting glucose (IFG) and diabetes [97], dual sensory impairment (DSI) [98], Diet quality [68,99] | Those in the highest TDS quintile had reduced risk of all-cause mortality (Ptrend = 0.04) [33]. Those in highest TDS quartile had reduced risk of CKD (Ptrend = 0.005) [96], reduced risk of visual impairment (>65yrs: p = 0.05) [94], healthier retinal vessels (Ptrend < 0.05), but not associated with 5-y change in retinal vessel caliber [95], good QOL (Ptrend < 0.05) [92] and successful aging (OR: 1.58, 95% CI: 1.02, 2.46) [93]. Negative association between high TDS and risk of IFG in men (Ptrend = 0.02), but no association in women for diabetes risk [97]. No association between baseline TDS and DSI [98]. No significant mean TDS difference between results from FFQ and WFR (p = 0.63), but significant correlation between the two methods (r = 0.75, p < 0.0001) [68]. |
| Aussie-Diet Quality Index (Aussie-DQI) | Zarrin, 2013 [18] | Tested content, construct and criterion validity [18] | Adults aged ≥19 years from 1995 National Nutrition Survey (NNS); aged ≥25 from the Nambour Skin Cancer Study (NSC) [18] | 129-item FFQ and a 24-h R [18] | All-cause and cancer mortality [18] | Higher Aussie-DQI scores were associated with higher desirable nutrient intakes and inversely associated with risk of cancer mortality in men (HR: 0.3, 95% CI: 0.11, 0.83) [18]. |
| Healthy Eating Index for Australian Adults-2013 (HEIFA-2013) | Roy, 2016 [16] Roy, 2017 [119] Grech, 2017 [117] Grech, 2017 [128] | Tested criterion validity and internal consistency [16] | Adults aged 18–34 years [16,117,128], 19–24 years [119] | FFQ (74-item food and 6-item alcohol) and 5-d WFR [16], validated mobile application (e-DIA app) [119], two 24-h Rs [117,128] | Diet quality [16,117,119]; Dietary energy density [128] | Positive correlation of essential micronutrients between both FFQ and WFR HEIFA-2013 scores (Ptrend < 0.0005, Cronbach α = 0.41) [16]. Higher HEIFA-2013 was associated with reduced university campus and other takeaway foods consumption (Ptrend < 0.001), BMI (Ptrend = 0.02) and WC (Ptrend = 0.05) [119]; sociodemographic and lifestyle characteristics (p < 0.05) [117]. Higher dietary energy density was associated with lower HEIFA-2013 (p < 0.0001) [128]. |
| Australian Diet Quality Score (ADQS) | Froud, 2019 [30] | Not tested | Adults aged 18–75 years [30] | FFQ (74-item food and 6-item alcohol) [30] | Depression [30] | Lower ADQS was associated with increased depression risk (p = 0.037) [30]. |
| Healthy Dietary Habits Index (HDHI) | Wong, 2017 [20] Davison, 2017 [129] | Tested content, construct and criterion validity [20] | Adults aged ≥19 years [20], child–parent pairs (mean age of child = 10.2 years, parent = 41.6 years) [129] | Two 24-h Rs and 25-item DHQ [20], Children; 28-item FFQ and Parents; 25-item DHQ [129] | Diet quality [20,129] | Higher HDHI score was associated with sociodemographic and lifestyle characteristics; higher nutrient intakes (all p < 0.001) [20]. Parental DQI score was associated with a child’s dietary pattern score (p < 0.001) [129]. |
| Diet Quality Index-Revised (DQI-R) | Reeves et al. 2013 [116] | Tested reproducibility and validity [57] | Adults aged ≥25 years [116] | 74-item FFQ [116] | AGM- Abnormal glucose metabolism (IFG, impaired glucose tolerance, diabetes) [116] | Women with low DQI-R were more likely to have AGM (Ptrend = 0.012) [116]. |
| Recommended Food Score (RFS) | Milte et al. 2015 [89] Livingstone, 2016 [84] Milte, 2018 [88] | Not tested | Adults aged 55–68 years [88,89], ≥19 years [84] | 111-item FFQ and food-related behavior questions [88,89], two 24-h Rs [84] | Health-related QOL [89]; obesity and hypertension [84]; Telomere length [88] | Higher RFS scores were associated with better health-related QOL (Ptrend < 0.001) [89] and less likely to be hypertensive (Ptrend = 0.021) [84]. No association between RFS and telomere length [88]. |
| Not Recommended Food Score (NRFS) | Petersen, 2015 [71] | Not tested | Adults (mean age = 50 years) [71] | FFQ (74-item food and 6-item alcohol) [71] | Diet quality [71] | Mean NRFS scores for participants with diabetes and controls were not different [71]. |
| Mediterranean Diet Score (MD Score) | Petersen, 2015 [71] Dugue, 2016 [106] Hodge, 2016 [107] Hodge, 2018 [108] | Not tested | Adults (mean age = 50 years) [71], aged 27–76 years [106], mid-aged adults 40–69 years [107,108] | FFQ (74-item food and 6-item alcohol) [71], 121-item FFQ [106,107,108] | Urothelial cell carcinoma (UCC) incidence [106]; lung cancer [107]; total, cardiovascular disease (CVD), coronary heart disease (CHD) mortality [108]; Diet quality [71] | Higher MD score was inversely associated with invasive UCC (HR: 0.86; 95% CI: 0.74, 1.00) [106], lung cancer risk (HR7-9 vs. 0–3:0.64; 95% CI: 0.45, 0.90) [107] and total mortality (HRQ5-Q1:0.86; 95% CI: 0.80, 0.93) [108]. Mean MD scores for participants with diabetes and controls were not different [71]. |
| Mediterranean Diet Pattern index (MDP index) | Lai, 2016 [72] | Not tested | Mid-aged women (50–55 years) [72] | FFQ (74-item food and 6-item alcohol) [72] | Depressive symptoms [72] | Inverse association between MDP index and depressive symptoms (Ptrend = 0.007) [72]. |
| MedDiet Score | Crichton, 2013 [115] | Not tested | Adults aged 40–65 years [115] | 215-item FFQ [115] | Self-reported psychological functioning [115] | Total MedDiet score was not associated with cognitive function, but plant food intakes was beneficial for general health and mental disorders (p < 0.05) [115]. |
| Mediterranean Diet Scale (MDS) | Milte, 2015 [89] Milte, 2018 [88] | Not tested | Adults aged 55–68 years [88,89] | 111-item FFQ and food-related behavior questions [88,89] | Health-related QOL [89]; Telomere length [88] | Higher MDS scores were associated with better health-related QOL (p < 0.001) [89]. No association between MDS and relative telomere length [88]. |
| Dietary Approach to Stop Hypertension (DASH) | Petersen, 2015 [71] | Not tested | Adults (mean age = 50 years) [71] | FFQ (74-item food and 6-item alcohol) [71] | Diet quality [71] | Mean DASH scores for participants with diabetes and controls were not different [71]. |
| Alternative Healthy Eating Index (AHEI) | Petersen, 2015 [71] | Not tested | Adults (mean age = 50 years) [71] | FFQ (74-item food and 6-item alcohol) [71] | Diet quality [71] | Mean AHEI scores for participants with diabetes and controls were not different [71]. |
| Alternative Healthy Eating Index-2010 (AHEI-2010) | Dugue, 2016 [106] | Not tested | Adults aged 27–76 years [106] | 121-item FFQ [106] | Urothelial cell carcinoma (UCC) incidence [106] | No association between AHEI-2010 and risk of overall UCC (HR: 1.03; 95% CI: 0.92, 1.15) and invasive UCC (HR: 0.88; 95% CI: 0.75, 1.04) [106]. |
| Diet Quality Tool (DQT) | O’Reilly, 2012 [32] | Tested construct and criterion validity [32] | CVD patients (mean age = 61.2 ± 10.8 years) [32] | 13-item questionnaire from validated FFQ and 4-d food diary [32] | Diet quality [32] | Significant difference was found between mean dietary fiber (p < 0.05) and% total energy from saturated fat (p < 0.01) for those with better DQT scores (>60%) vs. poorer scores (≤60%) when compared with 4-day food diary nutrient values [32]. |
| Dietary Inflammatory Index (DII) | Wood, 2015 [114] Dugue, 2016 [106] Hodge, 2016 [107] Shivappa, 2016 [111] Vissers, 2016 [113] Vissers, 2017 [112] Hodge, 2018 [108] Mayr, 2018 [109] Nagle, 2019 [110] | Tested construct validity [66] | Adults aged ≥18 years [110,114], 27–76 years [106], mid-aged adults 40–69 years [107,108]; mid-aged women (50–55 years) [111,112,113]; mean age-61.9 years [109] | FFQ (74-item food and 6-item alcohol) [111,112,113], 121-item FFQ [106,107,108], 139-item FFQ [110], 186-item FFQ [114], 7-day food diary [109] | lung cancer [107]; total, CVD, CHD mortality [108]; ovarian cancer risk and survival [110]; hypertension [112]; CVD, CHD and cerebrovascular disease risk [113]; Asthma risk [114]; Interleukin 6 (IL-6) [109]; depression [111]; UCC incidence [106] | Higher DII score (pro-inflammatory diet) was positively associated with risk of total mortality (HRQ5-Q1:1.16; 95% CI: 1.08, 1.24) [108]; lung cancer in current smokers (HRQ4-Q1:1.70; 95% CI: 1.02, 2.82) [107]; ovarian cancer (ORQ4-Q1:1.31; 95% CI: 1.06, 1.63) [110]; hypertension (OR: 1.24; 95% CI: 1.06, 1.45) [112]; myocardial infarct (HR: 1.46; 95% CI: 1.12, 1.89) [113] and asthma (OR: 1.70; 95% CI: 1.03, 2.14) [114]. Lower DII score (anti-inflammatory diet) was negatively associated with depression (RRQ1-Q4:0.81, 95% CI: 0.69, 0.96) [111] and high sensitivity IL-6 (r = 0.34, 95% CI: 0.05, 0.56) and triglyceride (r = −0.30, 95% CI: −0.51, −0.06) [109]. No association between DII and risk of overall UCC (HR: 1.06; 95%CI: 0.96, 1.18) [106]. |
3.7. Critical Appraisal of Diet Quality Indices by Previous Suggested Recommendations
| Theoretical Framework | Dimension | Structure | Indicator Selection | Scoring Criteria | Aggregation | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dietary Guideline | Dietary Pattern | Adequacy | Moderation | Variety | Balance | Nested/ Ordered/ Not Ordered | Database | Foods & Food Groups/ Nutrients/ Both | Healthy/ Unhealthy Component | Dichotomous/ Ordinal/ Metric | Range | Cut Points | Weighted Equally by Indicators | Evaluation of DQI | |
| Aust-HEI [28] | Y | Y | Y | Y | Not ordered | FFQ (item not stated), SDQ | Foods & food groups | Y | Ordinal | [0, 60] | Y | Y | Construct Validity | ||
| ARFS [29] | Y | Y | Ordered | FFQ (74-item food and 6-item alcohol) | Foods & food groups | N | Dichotomous | [0, 74] | N | Y | Construct Validity | ||||
| ARFS-1 [42] | Y | Y | Ordered | Subset of 70 items from 120-item FFQ | Foods & food groups | N | Dichotomous | [0, 73] | N | Y | Reproducibility, comparative validity | ||||
| DGI [19] | Y | Y | Y | Y | Nested | 108-item FFQ, Single 24-h R | Foods &food groups | Y | Metric | [0, 150] | Y | Y | Construct Validity | ||
| Modified DGI [37] | Y | Y | Y | Y | Ordered | 137-item FFQ | Foods & Food groups | Y | Metric | [0, 80] | Y | Y | Not tested | ||
| DGI-2013 [17] | Y | Y | Y | Y | Nested | 111-item FFQ | Foods & food groups | Y | Metric | [0, 130] | Y | Y | Construct Validity | ||
| RDGI [36] | Y | Y | Y | Nested | 12-item FFQ, 12-item DBQ | Foods & food groups | Y | Metric | [0, 100] | Y | Y | Not tested | |||
| CSIRO HDS [63] | Y | Y | Y | Y | Ordered | 38-item SFS | Foods & food groups | Y | Metric | [0, 100] | Y | Y | Relative validity | ||
| TDS [33] | Y | Y | Y | Y | Nested | 145-item FFQ | Both | Y | Ordinal | [0, 20] | Y | Y | Relative validity | ||
| Aussie-DQI [18] | Y | Y | Y | Y | Ordered | Single 24-h R, 129-item FFQ | Both | Y | Metric | [0, 120] | Y | Y | Construct Validity, criterion validity | ||
| HEIFA-2013 [16] | Y | Y | Y | Y | Nested | Five 1-day WFR, FFQ (74-item food and 6-item alcohol) | Both | Y | Ordinal | [0, 100] | Y | Y | Internal consistency, relative validity | ||
| ADQS [30] | Y | Y | Y | Y | Not ordered | FFQ (74-item food and 6-item alcohol) | Both | Y | Metric | Maximum = RDI(−10%) | Y | Y | Not tested | ||
| HDHI [20] | Y | Y | Y | Not Ordered | Multiple-pass single 24-h R, 25-item DHQ | Foods & food groups | Y | Ordinal | [0, 60] | Y | Y | Content validity, construct validity, Relative validity | |||
| DQI-R [8] | Y | Y | Y | Y | Ordered | Two 24-h Rs | Both | Y | Metric | [0, 100] | Y | Y | Concurrent validity | ||
| RFS [41] | Y | Y | Y | Ordered | 23 items from 62-item FFQ | Foods & food groups | N | Dichotomous | [0, 23] | N | Y | Not tested | |||
| NRFS [32] | Y | Y | Not ordered | 60-item FFQ, WFRs (days not stated) | Foods & food groups | N | Dichotomous | [0, 21] | N | Y | Not tested | ||||
| MD score [11] | Y | Y | Y | Y | Not ordered | 190-item FFQ | Both | Y | Dichotomous | [0, 8] | N | Y | Not tested | ||
| MDP index [21] | Y | Y | Y | Y | Ordered | 150-item FFQ | Both | Y | Dichotomous | [0, 9] | N | Y | Not tested | ||
| MedDiet score [47] | Y | Y | Y | Ordered | 121-item FFQ | Foods & food groups | Y | Dichotomous | [0, 9] | N | Y | Not tested | |||
| MDS [39] | Y | Y | Y | Y | Ordered | FFQ (item not stated), 24–h R (days not stated) | Both | Y | Dichotomous | [0, 9] | N | Y | Not tested | ||
| DASH [15] | Y | Y | Y | Not ordered | 116-item FFQ | Both | Y | Ordinal | [8, 40] | N | Y | Not tested | |||
| AHEI [23] | Y | Y | Y | Y | Not ordered | 130-item FFQ | Both | Y | Metric | [2.5, 87.5] | Y | Y * | Not tested | ||
| AHEI-2010 [22] | Y | Y | Y | Y | Not ordered | FFQ (item not stated) | Both | Y | Metric | [0, 110] | Y | Y | Not tested | ||
| DQT [32] | Y | Y | Y | Not ordered | 4-day FD, 13-item questionnaire | Foods & food groups | Y | Ordinal | [0, 130] | Y | Y | Construct and criterion validity | |||
| DII [66] | Y | Y | Y | Y | Not ordered | 7-day dietary recalls, 24-h Rs [67] | Both | Y | Metric | [−8.87, +7.98] | N | Y | Construct validity [67] | ||
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Waijers, P.M.C.M.; Feskens, E.J.M.; Ocke’, M.C. A critical review of predefined diet quality scores. Br. J. Nutr. 2007, 97, 219–231. [Google Scholar] [CrossRef] [PubMed]
- Arvaniti, F.; Panagiotakos, D.B. Healthy Indexes in Public Health Practice and Research: A Review. Crit. Rev. Food Sci. Nutr. 2008, 48, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Wirt, A.; Collins, C.E. Diet quality—What is it and does it matter? Public Health Nutr. 2009, 12, 2473–2492. [Google Scholar] [CrossRef] [PubMed]
- Newby, P.K.; Tucker, K.L. Empirically derived eating patterns using factor or cluster analysis: A review. Nutr. Rev. 2004, 62, 177–203. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Kant, A.K. Dietary Patterns and Health Outcomes. J. Am. Diet. Assoc. 2004, 104, 615–635. [Google Scholar] [CrossRef]
- Kourlaba, G.; Panagiotakos, D.B. Dietary quality indices and human health: A review. Maturitas 2009, 62, 1–8. [Google Scholar] [CrossRef]
- Haines, P.S.; Siega-Riz, A.M.; Popkin, B.M. The Diet Quality Index Revised: A measurement instrument for populations. J. Am. Diet. Assoc. 1999, 99, 697–704. [Google Scholar] [CrossRef]
- Kennedy, T.E.; Ohls, J.; Carlson, S.; Fleming, K. The healthy eating index: Design and applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Patterson, R.E.; Haines, P.S.; Popkin, B.M. Diet quality index: Capturing a multidimensional behavior. J. Am. Diet. Assoc. 1994, 94, 57–64. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulos, D. Diet and overall survival in elderly people. BMJ 1995, 311, 1457–1460. [Google Scholar] [CrossRef] [PubMed]
- Fransen, H.P.; Ocke´, M.C. Indices of diet quality. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Trijsburg, L.; Talsma, E.F.; De Vries, J.H.; Kennedy, G.; Kuijsten, A.; Brouwer, I.D. Diet quality indices for research in low-and middle-income countries: A systematic review. Nutr. Rev. 2019, 77, 515–540. [Google Scholar] [CrossRef] [PubMed]
- Burggraf, C.; Teuber, R.; Brosig, S.; Meier, T. Review of a priori dietary quality indices in relation to their construction criteria. Nutr. Rev. 2018, 76, 747–764. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Roy, R.; Hebden, L.; Rangan, A.; Allman-Farinelli, M. The development, application, and validation of a Healthy Eating Index for Australian Adults (HEIFA-2013). Nutrition 2016, 32, 432–440. [Google Scholar] [CrossRef]
- Thorpe, M.G.; Milte, C.M.; Crawford, D.; McNaughton, S.A. A revised Australian Dietary Guideline Index and its association with key sociodemographic factors, health behaviors and body mass Index in peri-retirement aged adults. Nutrients 2016, 8, 160. [Google Scholar] [CrossRef]
- Zarrin, R.; Ibiebele, T.I.; Marks, G.C. Development and validity assessment of a diet quality index for Australians. Asia Pac. J. Clin. Nutr. 2013, 22, 177–187. [Google Scholar] [CrossRef]
- McNaughton, S.A.; Ball, K.; Crawford, D.; Mishra, G.D. An index of diet and eating patterns is a valid measure of diet quality in an Australian population. J. Nutr. 2008, 138, 86–93. [Google Scholar] [CrossRef]
- Wong, J.E.; Haszard, J.J.; Howe, A.S.; Parnell, W.R.; Skidmore, P.M.L. Development of a Healthy Dietary Habits Index for New Zealand adults. Nutrients 2017, 9, 454. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Chiuve, S.E.; Fung, T.T.; Rimm, E.B.; Hu, F.B.; McCullough, M.L.; Wang, M.; Stampfer, M.J.; Willett, W.C. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 2012, 142, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.L.; Feskanich, D.; Stampfer, M.J.; Giovannucci, E.L.; Rimm, E.B.; Hu, F.B.; Spiegelman, D.; Hunter, D.J.; Colditz, G.A.; Willett, W.C. Diet quality and major chronic disease risk in men and women: Moving toward improved dietary guidance. Am. J. Clin. Nutr. 2002, 76, 1261–1271. [Google Scholar] [CrossRef]
- Centre for Reviews and Dissemination. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care; CRD, University of York: York, UK, 2009. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Academy of Nutrition and Dietetics. Evidence Analysis Manual: Steps in the Academy Evidence Analysis Process; ADA Research and Strategic Business Development: Chicago, IL, USA, 2016. [Google Scholar]
- Sambunjak, D.; Cumpston, M.; Watts, C. Module 4: Selecting Studies and Collecting Data. In Cochrane Interactive Learning: Conducting an Intervention Review; Cochrane. Available online: https://training.cochrane.org/interactivelearning/module-4-selecting-studies-and-collecting-data (accessed on 26 May 2019).
- Australian Institute of Health and Welfare. Australian Diet Quality Index Project; Australian Institute of Health and Welfare: Canberra, Australia, 2007.
- Collins, C.E.; Young, A.F.; Hodge, A. Diet quality is associated with higher nutrient intake and self-rated health in mid-aged women. J. Am. Coll. Nutr. 2008, 27, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Froud, A.; Murphy, J.; Cribb, L.; Ng, C.H.; Sarris, J. The relationship between dietary quality, serum brain-derived neurotrophic factor (BDNF) level, and the Val66met polymorphism in predicting depression. Nutr. Neurosci. 2019, 22, 513–521. [Google Scholar] [CrossRef]
- Michels, K.B.; Wolk, A. A prospective study of variety of healthy foods and mortality in women. Int. J. Epidemiol. 2002, 31, 847–854. [Google Scholar] [CrossRef]
- O’Reilly, S.; McCann, L. Development and validation of the Diet Quality Tool for use in cardiovascular disease prevention settings. Aust. J. Prim. Health 2012, 18, 138–147. [Google Scholar] [CrossRef]
- Russell, J.; Flood, V.; Rochtchina, E.; Gopinath, B.; Allman-Farinelli, M.; Bauman, A.; Mitchell, P. Adherence to dietary guidelines and 15-year risk of all-cause mortality. Br. J. Nutr. 2013, 109, 547–555. [Google Scholar] [CrossRef]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Hébert, J.R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014, 17, 1689–1696. [Google Scholar] [CrossRef]
- Williams, R.L.; Rollo, M.E.; Schumacher, T.; Collins, C.E. Diet quality scores of Australian adults who have completed the Healthy Eating Quiz. Nutrients 2017, 9, 880. [Google Scholar] [CrossRef] [PubMed]
- Bivoltsis, A.; Trapp, G.; Knuiman, M.; Hooper, P.; Ambrosini, G. Can a simple dietary index derived from a sub-set of questionnaire items assess diet quality in a sample of Australian adults? Nutrients 2018, 10, 486. [Google Scholar] [CrossRef] [PubMed]
- McLeod, E.R.; Campbell, K.J.; Hesketh, K.D. Nutrition knowledge: A mediator between socioeconomic position and diet quality in Australian first-time mothers. J. Am. Diet. Assoc. 2011, 111, 696–704. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Baird, D.; Golley, R.K.; Noakes, M. The CSIRO Healthy Diet Score: An online survey to estimate compliance with the Australian Dietary Guidelines. Nutrients 2017, 9, 47. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Orfanos, P.; Norat, T.; Bueno-de-Mesquita, B.; Ocké, M.; Peeters, P.H.; van der Schouw, Y.T.; Boeing, H.; Hoffmann, K.; Boffetta, P.; et al. Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. BMJ 2005, 330, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Graubard, B.I. A comparison of three dietary pattern indexes for predicting biomarkers of diet and disease. J. Am. Coll. Nutr. 2005, 24, 294–303. [Google Scholar] [CrossRef]
- Kant, A.K.; Schatzkin, A.; Graubard, B.I.; Schairer, C. A prospective study of diet quality and mortality in women. JAMA 2000, 283, 2109–2115. [Google Scholar] [CrossRef]
- Collins, C.E.; Burrows, T.L.; Rollo, M.E.; Boggess, M.M.; Watson, J.F.; Guest, M.; Duncanson, K.; Pezdirc, K.; Hutchesson, M.J. The comparative validity and reproducibility of a diet quality index for adults: The Australian Recommended Food Score. Nutrients 2015, 7, 785–798. [Google Scholar] [CrossRef]
- Ministry of Health (New Zealand). New Zealand Food and Nutrition Guidelines for Healthy Adults: A Background Paper; Ministry of Health (New Zealand): Wellington, New Zealand, 2003.
- National Research Council: Committee on Diet and Health. Diet and Health: Implications for Reducing Chronic Disease Risk; National Academy Press: Washington, DC, USA, 1989. [CrossRef]
- Yates, A.A.; Schlicker, S.A.; Suitor, C.W. Dietary reference intakes: The new basis for recommendations for calcium and related nutrients, B vitamins, and choline. J. Am. Diet. Assoc. 1998, 98, 699–706. [Google Scholar] [CrossRef]
- Willett, W.C. Diet and health: What should we eat? Science 1994, 264, 532–537. [Google Scholar] [CrossRef]
- Hodge, A.; English, D.; Itsiopoulos, C.; O’dea, K.; Giles, G. Does a Mediterranean diet reduce the mortality risk associated with diabetes: Evidence from the Melbourne Collaborative Cohort Study. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef] [PubMed]
- Kushi, L.H.; Lenart, E.B.; Willett, W.C. Health implications of Mediterranean diets in light of contemporary knowledge. 2. Meat, wine, fats, and oils. Am. J. Clin. Nutr. 1995, 61, 1416S–1427S. [Google Scholar] [CrossRef]
- Renaud, S.d.; de Lorgeril, M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 1992, 339, 1523–1526. [Google Scholar] [CrossRef]
- de Lorderil, M.; Renaud, S.; Mamelle, N. Mediterranean alphalinolenic acid-rich diet in secondary prevention of cardiovascular disease. Lancet 1994, 343, 1454–1459. [Google Scholar] [CrossRef]
- Kushi, L.H.; Lenart, E.B.; Willett, W.C. Health implications of Mediterranean diets in light of contemporary knowledge. 1. Plant foods and dairy products. Am. J. Clin. Nutr. 1995, 61, 1407S–1415S. [Google Scholar] [CrossRef]
- United States Department of Health and Human Services. Your Guide to Lowering Your Blood Pressure with DASH; National Institutes of Health, National Heart, Lung and Blood Institute: Bethesda, MD, USA, 2006.
- National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand. Reducing Risk in Heart Disease 2007: Guidelines for Preventing Cardiovascular Events in People with Coronary Heart Disease; National Heart Foundation of Australia: Canberra, Australia, 2008.
- Kant, A.K.; Thompson, F.E. Measures of overall diet quality from a food frequency questionnaire: National Health Interview Survey, 1992. Nutr. Res. 1997, 17, 1443–1456. [Google Scholar] [CrossRef]
- Wahlqvist, M.L.; Lo, C.S.; Myers, K.A. Food variety is associated with less macrovascular disease in those with type II diabetes and their healthy controls. J. Am. Coll. Nutr. 1989, 8, 515–523. [Google Scholar] [CrossRef]
- Newby, P.; Hu, F.B.; Rimm, E.B.; Smith-Warner, S.A.; Feskanich, D.; Sampson, L.; Willett, W.C. Reproducibility and validity of the Diet Quality Index Revised as assessed by use of a food-frequency questionnaire. Am. J. Clin. Nutr. 2003, 78, 941–949. [Google Scholar] [CrossRef]
- Fogli-Cawley, J.J.; Dwyer, J.T.; Saltzman, E.; McCullough, M.L.; Troy, L.M.; Jacques, P.F. The 2005 dietary guidelines for Americans adherence index: Development and application. J. Nutr. 2006, 136, 2908–2915. [Google Scholar] [CrossRef]
- Kellett, E.; Smith, A.; Schmerlaib, Y. Australian Guide to Healthy Eating; Commonwealth Department of Health and Family Services: Canberra, Australia, 1998. [Google Scholar]
- National Health and Medical Research Council (Australia). Dietary Guidelines for Australian Adults, 3rd ed.; National Health and Medical Research Council: Canberra, Australia, 2003.
- National Health and Medical Research Council (Australia). Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013.
- Marshall, S.; Watson, J.; Burrows, T.; Guest, M.; Collins, C.E. The development and evaluation of the Australian child and adolescent recommended food score: A cross-sectional study. Nutr. J. 2012, 11. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Rebuli, M.A.; Golley, R.K. Reliability and relative validity of a diet index score for adults derived from a self-reported short food survey. Nutr. Diet. 2017, 74, 291–297. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. National Health Priority Areas. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Products/5317BAD6B8EEE19ACA25757C001EED30?opendocument (accessed on 21 March 2020).
- Wong, J.E.; Skidmore, P.M.; Williams, S.M.; Parnell, W.R. Healthy dietary habits score as an indicator of diet quality in New Zealand adolescents. J. Nutr. 2014, 144, 937–942. [Google Scholar] [CrossRef]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Ma, Y.; Ockene, I.S.; Tabung, F.; Hébert, J.R. A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr. 2014, 17, 1825–1833. [Google Scholar] [CrossRef]
- Cavicchia, P.P.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Ma, Y.; Ockene, I.S.; Hébert, J.R. A new dietary inflammatory index predicts interval changes in serum high-sensitivity C-reactive protein. J. Nutr. 2009, 139, 2365–2372. [Google Scholar] [CrossRef]
- Russell, J.C.; Flood, V.M.; Sadeghpour, A.; Gopinath, B.; Mitchell, P. Total Diet Score as a valid method of measuring diet quality among older adults. Asia Pac. J. Clin. Nutr. 2017, 26, 212–219. [Google Scholar] [CrossRef]
- Thompson, F.E.; Subar, A.F. Dietary assessment methodology. In Nutrition in the Prevention and Treatment of Disease; Elsevier: Amsterdam, The Netherlands, 2017; pp. 5–48. [Google Scholar]
- Alhazmi, A.; Stojanovski, E.; McEvoy, M.; Brown, W.; Garg, M.L. Diet quality score is a predictor of type 2 diabetes risk in women: The Australian Longitudinal Study on Women’s Health. Br. J. Nutr. 2014, 112, 945–951. [Google Scholar] [CrossRef]
- Petersen, K.S.; Blanch, N.; Wepener, R.H.; Clifton, P.M.; Keogh, J.B. Dietary quality in people with type 1 and type 2 diabetes compared to age, sex and BMI matched controls. Diabetes Res. Clin. Pract. 2015, 107, e7–e10. [Google Scholar] [CrossRef]
- Lai, J.S.; Oldmeadow, C.; Hure, A.J.; McEvoy, M.; Byles, J.; Attia, J. Longitudinal diet quality is not associated with depressive symptoms in a cohort of middle-aged Australian women. Br. J. Nutr. 2016, 115, 842–850. [Google Scholar] [CrossRef]
- Lai, J.S.; Hure, A.J.; Oldmeadow, C.; McEvoy, M.; Byles, J.; Attia, J. Prospective study on the association between diet quality and depression in mid-aged women over 9 years. Eur. J. Nutr. 2017, 56, 273–281. [Google Scholar] [CrossRef]
- Aljadani, H.M.A.; Sibbritt, D.; Patterson, A.; Clare, C. The Australian Recommended Food Score did not predict weight gain in middle-aged Australian women during six years of follow-up. Aust. N. Z. J. Public Health 2013, 37, 322–328. [Google Scholar] [CrossRef]
- Aljadani, H.A.; Patterson, A.; Sibbritt, D.; Hutchesson, M.J.; Jensen, M.E.; Collins, C.E. Diet quality measured by fruit and vegetable intake predicts weight change in young women. J. Obes. 2013, 2013, 525161. [Google Scholar] [CrossRef]
- Aljadani, H.M.; Patterson, A.J.; Sibbritt, D.; Collins, C.E. Diet quality and 6-year risk of overweight and obesity among mid-age Australian women who were initially in the healthy weight range. Health Promot. J. Austr. 2016, 27, 29–35. [Google Scholar] [CrossRef]
- Morrison, M.; Koh, D.; Lowe, J.; Miller, Y.D.; Marshall, A.L.; Colyvas, K.; Collins, C. Postpartum diet quality in Australian women following a gestational diabetes pregnancy. Eur. J. Clin. Nutr. 2012, 66, 1160–1165. [Google Scholar] [CrossRef]
- Potter, J.; Collins, C.; Brown, L.; Hure, A. Diet quality of Australian breast cancer survivors: A cross-sectional analysis from the Australian Longitudinal Study on Women’s Health. J. Hum. Nutr. Diet. 2014, 27, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Patterson, A.; Fitzgerald, D. Higher diet quality does not predict lower Medicare costs but does predict number of claims in mid-aged Australian women. Nutrients 2011, 3, 40–48. [Google Scholar] [CrossRef]
- Kullen, C.J.; Farrugia, J.-L.; Prvan, T.; O’Connor, H.T. Relationship between general nutrition knowledge and diet quality in Australian military personnel. Br. J. Nutr. 2016, 115, 1489–1497. [Google Scholar] [CrossRef]
- Leech, R.M.; Livingstone, K.M.; Worsley, A.; Timperio, A.; McNaughton, S.A. Meal frequency but not snack frequency is associated with micronutrient intakes and overall diet quality in Australian men and women. J. Nutr. 2016, 146, 2027–2034. [Google Scholar] [CrossRef]
- Leech, R.M.; Timperio, A.; Livingstone, K.M.; Worsley, A.; McNaughton, S.A. Temporal eating patterns: Associations with nutrient intakes, diet quality, and measures of adiposity. Am. J. Clin. Nutr. 2017, 106, 1121–1130. [Google Scholar] [CrossRef]
- Livingstone, K.; Olstad, D.; Leech, R.; Ball, K.; Meertens, B.; Potter, J.; Cleanthous, X.; Reynolds, R.; McNaughton, S. Socioeconomic inequities in diet quality and nutrient intakes among Australian adults: Findings from a nationally representative cross-sectional study. Nutrients 2017, 9, 1092. [Google Scholar] [CrossRef]
- Livingstone, K.M.; McNaughton, S.A. Diet quality is associated with obesity and hypertension in Australian adults: A cross sectional study. BMC Public Health 2016, 16, 1037. [Google Scholar] [CrossRef]
- Livingstone, K.M.; McNaughton, S.A. Association between diet quality, dietary patterns and cardiometabolic health in Australian adults: A cross-sectional study. Nutr. J. 2018, 17, 19. [Google Scholar] [CrossRef]
- Martin, J.; Moran, L.; Teede, H.; Ranasinha, S.; Lombard, C.; Harrison, C. Exploring diet quality between urban and rural dwelling women of reproductive age. Nutrients 2017, 9, 586. [Google Scholar] [CrossRef]
- Martin, J.; Moran, L.; Teede, H.; Ranasinha, S.; Lombard, C.; Harrison, C. Diet quality in a weight gain prevention trial of reproductive aged women: A secondary analysis of a cluster randomized controlled trial. Nutrients 2019, 11, 49. [Google Scholar] [CrossRef]
- Milte, C.M.; Russell, A.P.; Ball, K.; Crawford, D.; Salmon, J.; McNaughton, S.A. Diet quality and telomere length in older Australian men and women. Eur. J. Nutr. 2018, 57, 363–372. [Google Scholar] [CrossRef]
- Milte, C.M.; Thorpe, M.G.; Crawford, D.; Ball, K.; McNaughton, S.A. Associations of diet quality with health-related quality of life in older Australian men and women. Exp. Gerontol. 2015, 64, 8–16. [Google Scholar] [CrossRef]
- Ribeiro, R.V.; Hirani, V.; Senior, A.M.; Gosby, A.K.; Cumming, R.G.; Blyth, F.M.; Naganathan, V.; Waite, L.M.; Handelsman, D.J.; Kendig, H. Diet quality and its implications on the cardio-metabolic, physical and general health of older men: The Concord Health and Ageing in Men Project (CHAMP). Br. J. Nutr. 2017, 118, 130–143. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, M.G.; Kestin, M.; Riddell, L.J.; Keast, R.S.; McNaughton, S.A. Diet quality in young adults and its association with food-related behaviours. Public Health Nutr. 2013, 17, 1767–1775. [Google Scholar] [CrossRef]
- Gopinath, B.; Russell, J.; Flood, V.M.; Burlutsky, G.; Mitchell, P. Adherence to dietary guidelines positively affects quality of life and functional status of older adults. J. Acad. Nutr. Diet. 2014, 114, 220–229. [Google Scholar] [CrossRef]
- Gopinath, B.; Russell, J.; Kifley, A.; Flood, V.M.; Mitchell, P. Adherence to dietary guidelines and successful aging over 10 years. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 349–355. [Google Scholar] [CrossRef]
- Hong, T.; Flood, V.; Rochtchina, E.; Mitchell, P.; Russell, J.; Wang, J.J. Adherence to dietary guidelines and the 10-year cumulative incidence of visual impairment: The Blue Mountains Eye Study. Am. J. Ophthalmol. 2014, 158, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Flood, V.M.; Wang, J.J.; Rochtchina, E.; Wong, T.Y.; Mitchell, P. Is quality of diet associated with the microvasculature? An analysis of diet quality and retinal vascular calibre in older adults. Br. J. Nutr. 2013, 110, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Harris, D.; Flood, V.; Burlutsky, G.; Mitchell, P. A better diet quality is associated with a reduced likelihood of CKD in older adults. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Rochtchina, E.; Flood, V.; Mitchell, P. Diet quality is prospectively associated with incident impaired fasting glucose in older adults. Diabet. Med. 2013, 30, 557–562. [Google Scholar] [CrossRef]
- Gopinath, B.; Schneider, J.; Flood, V.; McMahon, C.; Burlutsky, G.; Leeder, S.; Mitchell, P. Association between diet quality with concurrent vision and hearing impairment in older adults. J. Nutr. Health Aging 2014, 18, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Roach, L.A.; Lambert, K.; Holt, J.L.; Meyer, B.J. Diet quality in patients with end-stage kidney disease undergoing dialysis. J Ren Care 2017, 43, 226–234. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, S.A.; Dunstan, D.W.; Ball, K.; Shaw, J.; Crawford, D. Dietary quality Is associated with diabetes and cardio-metabolic risk factors. J. Nutr. 2009, 139, 734–742. [Google Scholar] [CrossRef]
- Arabshahi, S.; Lahmann, P.H.; Williams, G.M.; Marks, G.C.; van der Pols, J.C. Longitudinal change in diet quality in Australian adults varies by demographic, socio-economic, and lifestyle characteristics. J. Nutr. 2011, 141, 1871–1879. [Google Scholar] [CrossRef]
- Arabshahi, S.; van der Pols, J.C.; Williams, G.M.; Marks, G.C.; Lahmann, P.H. Diet quality and change in anthropometric measures: 15-year longitudinal study in Australian adults. Br. J. Nutr. 2012, 107, 1376–1385. [Google Scholar] [CrossRef]
- Backholer, K.; Spencer, E.; Gearon, E.; Magliano, D.J.; McNaughton, S.A.; Shaw, J.E.; Peeters, A. The association between socio-economic position and diet quality in Australian adults. Public Health Nutr. 2016, 19, 477–485. [Google Scholar] [CrossRef]
- Olstad, D.L.; Lamb, K.E.; Thornton, L.E.; McNaughton, S.A.; Crawford, D.A.; Minaker, L.M.; Ball, K. Prospective associations between diet quality and body mass index in disadvantaged women: The Resilience for Eating and Activity Despite Inequality (READI) study. Int. J. Epidemiol. 2017, 46, 1433–1443. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.J.; McNaughton, S.A.; Gall, S.L.; Otahal, P.; Dwyer, T.; Venn, A.J. Associations between partnering and parenting transitions and dietary habits in young adults. J. Acad. Nutr. Diet. 2017, 117, 1210–1221. [Google Scholar] [CrossRef]
- Dugué, P.A.; Hodge, A.M.; Brinkman, M.T.; Bassett, J.K.; Shivappa, N.; Hebert, J.R.; Hopper, J.L.; English, D.R.; Milne, R.L.; Giles, G.G. Association between selected dietary scores and the risk of urothelial cell carcinoma: A prospective cohort study. Int. J. Cancer 2016, 139, 1251–1260. [Google Scholar] [CrossRef] [PubMed]
- Hodge, A.; Bassett, J.; Shivappa, N.; Hébert, J.; English, D.; Giles, G.; Severi, G. Dietary inflammatory index, Mediterranean diet score, and lung cancer: A prospective study. Cancer Causes Control 2016, 27, 907–917. [Google Scholar] [CrossRef] [PubMed]
- Hodge, A.M.; Bassett, J.K.; Dugué, P.-A.; Shivappa, N.; Hébert, J.R.; Milne, R.; English, D.R.; Giles, G.G. Dietary inflammatory index or Mediterranean diet score as risk factors for total and cardiovascular mortality. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Mayr, H.L.; Itsiopoulos, C.; Tierney, A.C.; Ruiz-Canela, M.; Hebert, J.R.; Shivappa, N.; Thomas, C.J. Improvement in dietary inflammatory index score after 6-month dietary intervention is associated with reduction in interleukin-6 in patients with coronary heart disease: The AUSMED heart trial. Nutr. Res. 2018, 55, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Nagle, C.; Ibiebele, T.; Shivappa, N.; Hébert, J.; DeFazio, A.; Webb, P.; Study, A.O.C. The association between the inflammatory potential of diet and risk of developing, and survival following, a diagnosis of ovarian cancer. Eur. J. Nutr. 2019, 58, 1747–1756. [Google Scholar] [CrossRef]
- Shivappa, N.; Schoenaker, D.A.J.M.; Hebert, J.R.; Mishra, G.D. Association between inflammatory potential of diet and risk of depression in middle-aged women: The Australian Longitudinal Study on Women’s Health. Br. J. Nutr. 2016, 116, 1077–1086. [Google Scholar] [CrossRef]
- Vissers, L.E.T.; Waller, M.; van der Schouw, Y.T.; Hébert, J.R.; Shivappa, N.; Schoenaker, D.A.J.M.; Mishra, G.D. A pro-inflammatory diet is associated with increased risk of developing hypertension among middle-aged women. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 564–570. [Google Scholar] [CrossRef]
- Vissers, L.E.T.; Waller, M.A.; van der Schouw, Y.T.; Hebert, J.R.; Shivappa, N.; Schoenaker, D.A.J.M.; Mishra, G.D. The relationship between the dietary inflammatory index and risk of total cardiovascular disease, ischemic heart disease and cerebrovascular disease: Findings from an Australian population-based prospective cohort study of women. Atherosclerosis 2016, 253, 164–170. [Google Scholar] [CrossRef]
- Wood, L.G.; Shivappa, N.; Berthon, B.S.; Gibson, P.G.; Hebert, J.R. Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin. Exp. Allergy 2015, 45, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Crichton, G.E.; Bryan, J.; Hodgson, J.M.; Murphy, K.J. Mediterranean diet adherence and self-reported psychological functioning in an Australian sample. Appetite 2013, 70, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Reeves, M.M.; Healy, G.N.; Owen, N.; Shaw, J.E.; Zimmet, P.Z.; Dunstan, D.W. Joint associations of poor diet quality and prolonged television viewing time with abnormal glucose metabolism in Australian men and women. Prev. Med. 2013, 57, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Grech, A.; Sui, Z.; Siu, H.Y.; Zheng, M.; Allman-Farinelli, M.; Rangan, A. Socio-demographic determinants of diet quality in Australian adults using the validated Healthy Eating Index for Australian Adults (HEIFA-2013). Health Care (Don Mills) 2017, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Harbury, C.; Collins, C.E.; Callister, R. Diet quality is lower among adults with a BMI ≥40 kg m−2 or a history of weight loss surgery. Obes. Res. Clin. Pract. 2019, 13, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Roy, R.; Rangan, A.; Hebden, L.; Louie, J.C.Y.; Tang, L.M.; Kay, J.; Allman-Farinelli, M. Dietary contribution of foods and beverages sold within a university campus and its effect on diet quality of young adults. Nutrition 2017, 34, 118–123. [Google Scholar] [CrossRef]
- Forsyth, A.K.; Williams, P.G.; Deane, F.P. Nutrition status of primary care patients with depression and anxiety. Aust. J. Prim. Health 2012, 18, 172–176. [Google Scholar] [CrossRef]
- Forsyth, A.; Deane, F.P.; Williams, P. A lifestyle intervention for primary care patients with depression and anxiety: A randomised controlled trial. Psychiatry Res. 2015, 230, 537–544. [Google Scholar] [CrossRef]
- Baker, A.L.; Turner, A.; Kelly, P.J.; Spring, B.; Callister, R.; Collins, C.E.; Woodcock, K.L.; Kay-Lambkin, F.J.; Devir, H.; Lewin, T.J. ‘Better Health Choices’ by telephone: A feasibility trial of improving diet and physical activity in people diagnosed with psychotic disorders. Psychiatry Res. 2014, 220, 63–70. [Google Scholar] [CrossRef]
- O’Brien, K.M.; Hutchesson, M.J.; Jensen, M.; Morgan, P.; Callister, R.; Collins, C.E. Participants in an online weight loss program can improve diet quality during weight loss: A randomized controlled trial. Nutr. J. 2014, 13, 82. [Google Scholar] [CrossRef]
- Ashton, L.; Williams, R.; Wood, L.; Schumacher, T.; Burrows, T.; Rollo, M.; Pezdirc, K.; Callister, R.; Collins, C. Comparison of Australian Recommended Food Score (ARFS) and plasma carotenoid concentrations: A validation study in adults. Nutrients 2017, 9, 888. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.M.; Morgan, P.J.; Hutchesson, M.J.; Rollo, M.E.; Collins, C.E. Feasibility and preliminary efficacy of the ‘HEYMAN’healthy lifestyle program for young men: A pilot randomised controlled trial. Nutr. J. 2017, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.; Pezdirc, K.; Hutchesson, M.; Rollo, M.; Collins, C. Is skin coloration measured by reflectance spectroscopy related to intake of nutrient-dense foods? A cross-sectional evaluation in Australian young adults. Nutrients 2018, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Hendrie, G.; Golley, R.; Noakes, M. Compliance with dietary guidelines varies by weight status: A cross-sectional study of Australian adults. Nutrients 2018, 10, 197. [Google Scholar] [CrossRef] [PubMed]
- Grech, A.; Rangan, A.; Allman-Farinelli, M. Social determinants and poor diet quality of energy-dense diets of Australian young adults. Health Care (Don Mills) 2017, 5, 70. [Google Scholar] [CrossRef]
- Davison, B.; Saeedi, P.; Black, K.; Harrex, H.; Haszard, J.; Meredith-Jones, K.; Quigg, R.; Skeaff, S.; Stoner, L.; Wong, J. The association between parent diet quality and child dietary patterns in nine-to eleven-year-old children from Dunedin, New Zealand. Nutrients 2017, 9, 483. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Association of Changes in Diet Quality with Total and Cause-Specific Mortality. N. Engl. J. Med. 2017, 377, 143–153. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2015, 115, 780–800. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Bogensberger, B.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2018, 118, 74–100. [Google Scholar] [CrossRef]
- Shen, J.; Wilmot, K.A.; Ghasemzadeh, N.; Molloy, D.L.; Burkman, G.; Mekonnen, G.; Gongora, M.C.; Quyyumi, A.A.; Sperling, L.S. Mediterranean Dietary Patterns and Cardiovascular Health. Annu. Rev. Nutr. 2015, 35, 425–449. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hlaing-Hlaing, H.; Pezdirc, K.; Tavener, M.; James, E.L.; Hure, A. Diet Quality Indices Used in Australian and New Zealand Adults: A Systematic Review and Critical Appraisal. Nutrients 2020, 12, 3777. https://doi.org/10.3390/nu12123777
Hlaing-Hlaing H, Pezdirc K, Tavener M, James EL, Hure A. Diet Quality Indices Used in Australian and New Zealand Adults: A Systematic Review and Critical Appraisal. Nutrients. 2020; 12(12):3777. https://doi.org/10.3390/nu12123777
Chicago/Turabian StyleHlaing-Hlaing, Hlaing, Kristine Pezdirc, Meredith Tavener, Erica L. James, and Alexis Hure. 2020. "Diet Quality Indices Used in Australian and New Zealand Adults: A Systematic Review and Critical Appraisal" Nutrients 12, no. 12: 3777. https://doi.org/10.3390/nu12123777
APA StyleHlaing-Hlaing, H., Pezdirc, K., Tavener, M., James, E. L., & Hure, A. (2020). Diet Quality Indices Used in Australian and New Zealand Adults: A Systematic Review and Critical Appraisal. Nutrients, 12(12), 3777. https://doi.org/10.3390/nu12123777





