Long-Term Effects of Vitamin D Supplementation in Obese Children During Integrated Weight–Loss Programme—A Double Blind Randomized Placebo–Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
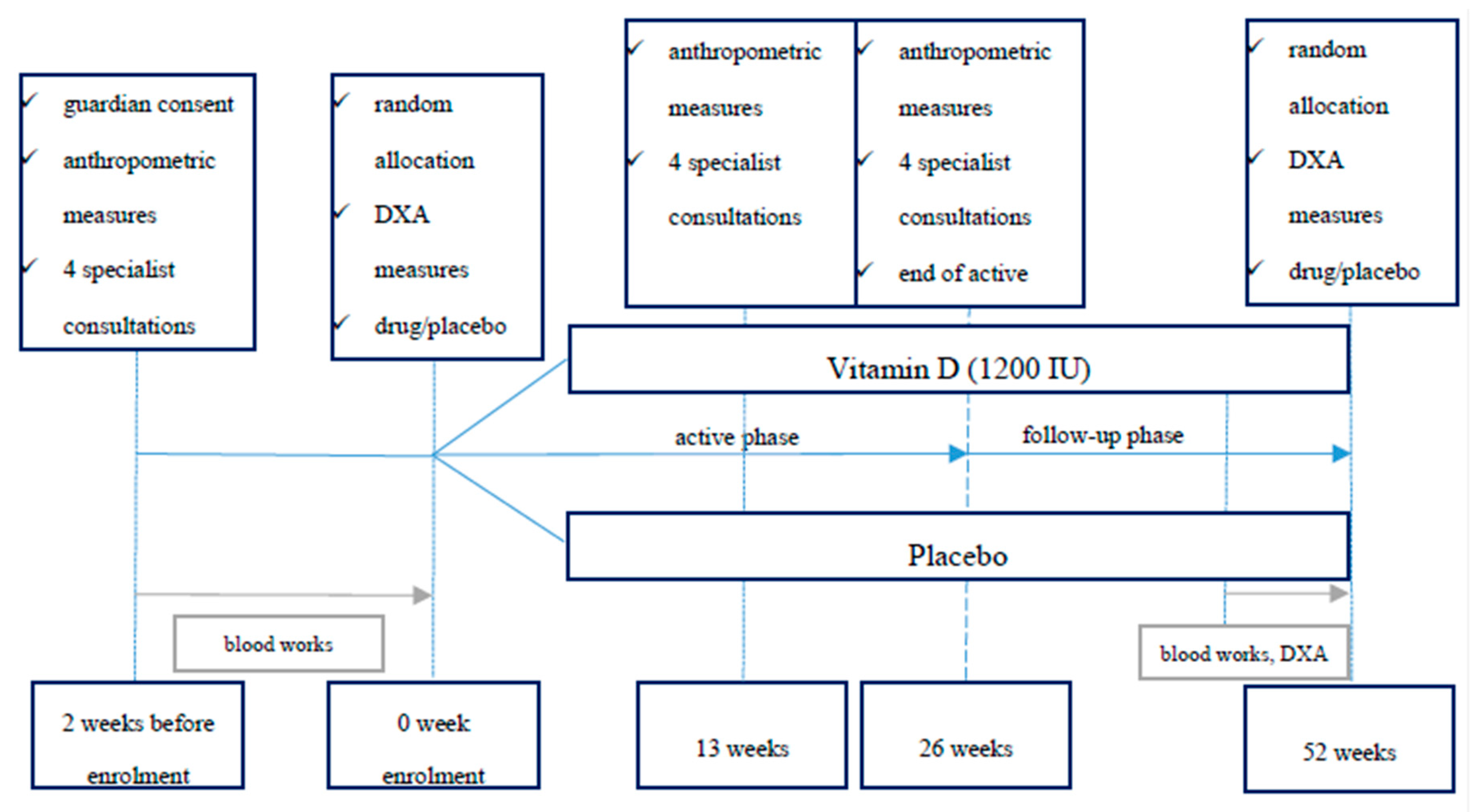
2.1. Trial Design
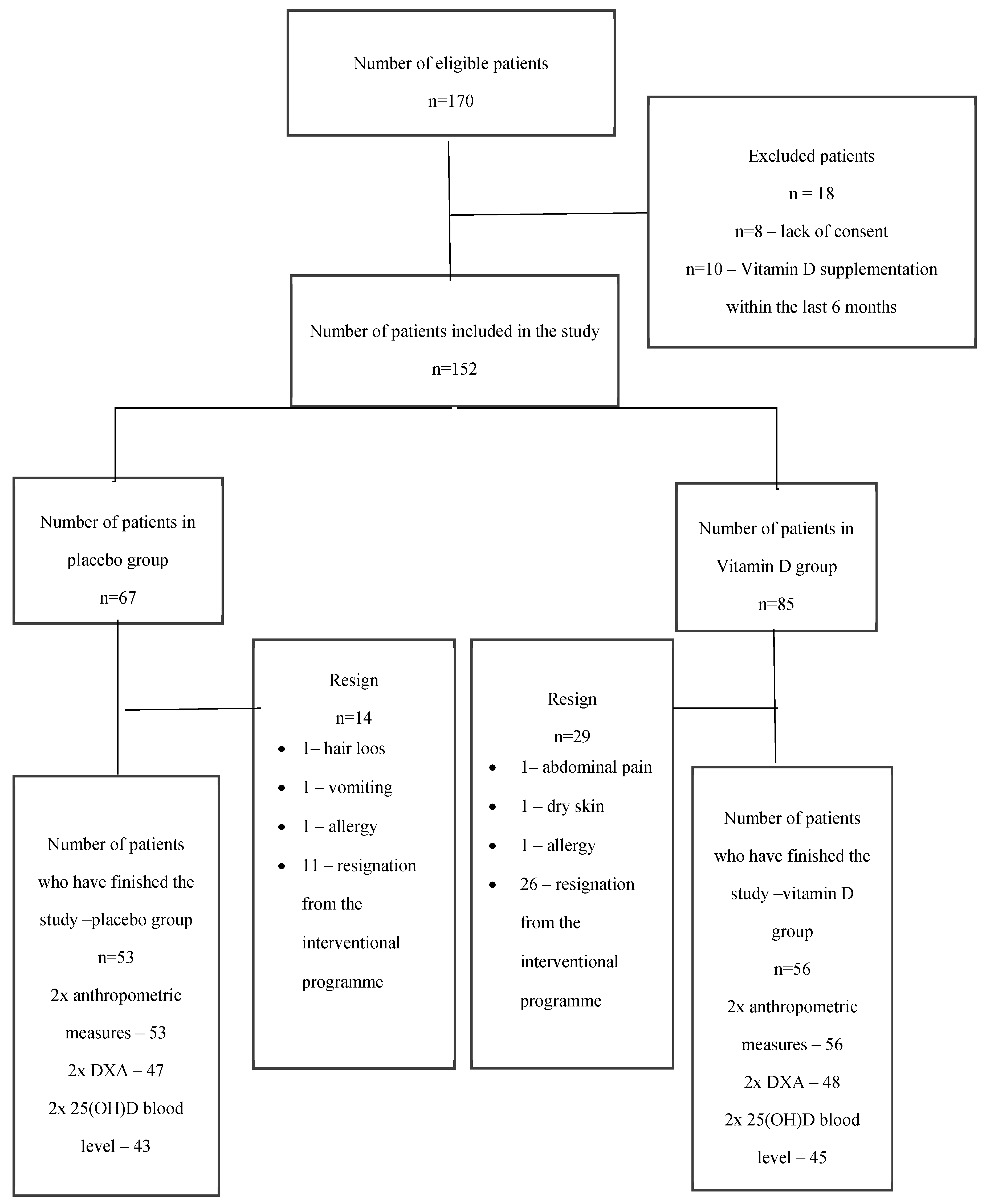
2.2. Participants
2.3. Ethics Approval and Consent to Participate
2.4. Study Procedure
- GROUP I (Vitamin D group): medical intervention, intervention of dietician, psychologist and physical education specialist, parental education + oral administration of vitamin D3 (1200 i.u. daily) for 26 weeks
- GROUP II (Placebo group): medical intervention, intervention of dietician, psychologist and physical education specialist, parental education + daily oral administration of placebo for 26 weeks.
2.5. Randomization and Blinding
2.6. Treatment Dispensing and Assessment of Compliance
2.7. Outcome Measures
2.8. Sample Size
2.9. Statistical Analysis
3. Results
4. Discussion
4.1. Effect of Vitamin D Supplementation on Body Mass Reduction
4.2. Effect of Vitamin D Supplementation on Bone Mineral Density During Weight Loss
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bentham, J.; Di Cesare, M.; Bilano, V.; Bixby, H.; Zhou, B.; Stevens, G.A.; Riley, L.M.; Taddei, C.; Hajifathalian, K.; Lu, Y.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Bann, D.; Johnson, W.; Li, L.; Kuh, D.; Hardy, R. Socioeconomic inequalities in childhood and adolescent body-mass index, weight, and height from 1953 to 2015: An analysis of four longitudinal, observational, British birth cohort studies. Lancet Public Health 2018, 3, e194–e203. [Google Scholar] [CrossRef]
- Kumar, S.; Kelly, A.S. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.S.; Barlow, S.E.; Rao, G.; Inge, T.H.; Hayman, L.L.; Steinberger, J.; Urbina, E.M.; Ewing, L.J.; Daniels, S.R. Severe obesity in children and adolescents: Identification, associated health risks, and treatment approaches: A scientific statement from the American Heart Association. Circulation 2013, 128, 1689–1712. [Google Scholar] [CrossRef] [PubMed]
- Kinlen, D.; Cody, D.; O’Shea, D. Complications of obesity. QJM An Int. J. Med. 2018, 111, 437–443. [Google Scholar] [CrossRef]
- Di Angelantonio, E.; Bhupathiraju, S.; Wormser, D.; Gao, P.; Kaptoge, S.; Berrington de Gonzalez, A.; Cairns, B.; Huxley, R.; Jackson, C.; et al.; Global BMI Mortality Collaboration Body-mass index and all-cause mortality: Individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016, 388, 776–786. [Google Scholar] [CrossRef]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 2019. [Google Scholar] [CrossRef]
- Nemet, D.; Levi, L.; Pantanowitz, M.; Eliakim, A. A combined nutritional-behavioral-physical activity intervention for the treatment of childhood obesity—A 7-year summary. J. Pediatr. Endocrinol. Metab. 2014, 27, 445–451. [Google Scholar] [CrossRef]
- Oude Luttikhuis, H.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane Database Syst. Rev. 2019, 3, CD001872. [Google Scholar] [CrossRef]
- Masquio, D.C.L.; De Piano, A.; Campos, R.M.S.; Sanches, P.L.; Carnier, J.; Corgosinho, F.C.; Netto, B.D.M.; Carvalho-Ferreira, J.P.; Oyama, L.M.; Nascimento, C.M.O.; et al. The role of multicomponent therapy in the metabolic syndrome, inflammation and cardiovascular risk in obese adolescents. Br. J. Nutr. 2015, 113, 1920–1930. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, Y.A.M.; Kravchychyn, A.C.P.; Vicente, S.d.C.F.; Campos, R.M.d.S.; Tock, L.; Oyama, L.M.; Boldarine, V.T.; Masquio, D.C.L.; Thivel, D.; Shivappa, N.; et al. An interdisciplinary weight loss program improves body composition and metabolic profile in adolescents with obesity: Associations with the dietary inflammatory index. Front. Nutr. 2019, 6, 77. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T. Calculating cardiac risk in obese adolescents before and after onset of lifestyle intervention. Expert Rev. Cardiovasc. Ther. 2013, 11, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Masquio, D.C.L.; De Piano, A.; Sanches, P.L.; Corgosinho, F.C.; Campos, R.M.S.; Carnier, J.; Da Silva, P.L.; Caranti, D.A.; Tock, L.; Oyama, L.M.; et al. The effect of weight loss magnitude on pro-/anti-inflammatory adipokines and carotid intima-media thickness in obese adolescents engaged in interdisciplinary weight loss therapy. Clin. Endocrinol. 2013, 79, 55–64. [Google Scholar] [CrossRef]
- Cuda, S.E.; Censani, M. Pediatric Obesity Algorithm: A Practical Approach to Obesity Diagnosis and Management. Front. Pediatr. 2019, 6, 431. [Google Scholar] [CrossRef]
- Boland, C.L.; Harris, J.B.; Harris, K.B. Pharmacological Management of Obesity in Pediatric Patients. Ann. Pharmacother. 2015, 49, 220–232. [Google Scholar] [CrossRef]
- Domecq, J.P.; Prutsky, G.; Leppin, A.; Sonbol, M.B.; Altayar, O.; Undavalli, C.; Wang, Z.; Elraiyah, T.; Brito, J.P.; Mauck, K.F.; et al. Drugs commonly associated with weight change: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2015, 100, 363–370. [Google Scholar] [CrossRef]
- Pooyandjoo, M.; Nouhi, M.; Shab-Bidar, S.; Djafarian, K.; Olyaeemanesh, A. The effect of (L-)carnitine on weight loss in adults: A systematic review and meta-analysis of randomized controlled trials. Obes. Rev. 2016, 17, 970–976. [Google Scholar] [CrossRef]
- Huang, J.; Wang, Y.; Xie, Z.; Zhou, Y.; Zhang, Y.; Wan, X. The anti-obesity effects of green tea in human intervention and basic molecular studies. Eur. J. Clin. Nutr. 2014, 68, 1075–1087. [Google Scholar] [CrossRef]
- Kim, S.Y.; Oh, M.R.; Kim, M.G.; Chae, H.J.; Chae, S.W. Anti-obesity effects of Yerba Mate (Ilex Paraguariensis): A randomized, double-blind, placebo-controlled clinical trial. BMC Complement. Altern. Med. 2015, 15, 338. [Google Scholar] [CrossRef]
- Zalewski, B.M.; Szajewska, H. No Effect of Glucomannan on Body Weight Reduction in Children and Adolescents with Overweight and Obesity: A Randomized Controlled Trial. J. Pediatr. 2019, 211, 85–91. [Google Scholar] [CrossRef] [PubMed]
- De Luis, D.; Domingo, J.C.; Izaola, O.; Casanueva, F.F.; Bellido, D.; Sajoux, I. Effect of DHA supplementation in a very low-calorie ketogenic diet in the treatment of obesity: A randomized clinical trial. Endocrine 2016, 54, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Lerchbaum, E.; Trummer, C.; Theiler-Schwetz, V.; Kollmann, M.; Wölfler, M.; Pilz, S.; Obermayer-Pietsch, B. Effects of vitamin D supplementation on body composition and metabolic risk factors in men: A randomized controlled trial. Nutrients 2019, 11, 1894. [Google Scholar] [CrossRef] [PubMed]
- Al-Daghri, N.M.; Amer, O.E.; Khattak, M.N.K.; Sabico, S.; Ghouse Ahmed Ansari, M.; Al-Saleh, Y.; Aljohani, N.; Alfawaz, H.; Alokail, M.S. Effects of different vitamin D supplementation strategies in reversing metabolic syndrome and its component risk factors in adolescents. J. Steroid Biochem. Mol. Biol. 2019, 191, 105378. [Google Scholar] [CrossRef] [PubMed]
- Aypak, C.; Türedi, Ö.; Yüce, A. The association of vitamin D status with cardiometabolic risk factors, obesity and puberty in children. Eur. J. Pediatr. 2014, 173, 367–373. [Google Scholar] [CrossRef]
- Lee, D.Y.; Kwon, A.R.; Ahn, J.M.; Kim, Y.J.; Chae, H.W.; Kim, D.H.; Kim, H.-S. Relationship between serum 25-hydroxyvitamin D concentration and risks of metabolic syndrome in children and adolescents from Korean National Health and Nutrition Examination survey 2008–2010. Ann. Pediatr. Endocrinol. Metab. 2015, 20, 46. [Google Scholar] [CrossRef]
- Voortman, T.; van den Hooven, E.H.; Heijboer, A.C.; Hofman, A.; Jaddoe, V.W.; Franco, O.H. Vitamin D Deficiency in School-Age Children Is Associated with Sociodemographic and Lifestyle Factors. J. Nutr. 2015, 145, 791–798. [Google Scholar] [CrossRef]
- Kamycheva, E.; Joakimsen, R.M.; Jorde, R. Intakes of Calcium and Vitamin D Predict Body Mass Index in the Population of Northern Norway. J. Nutr. 2003, 133, 102–106. [Google Scholar] [CrossRef]
- Pourshahidi, L.K. Vitamin D and obesity: Current perspectives and future directions. In Proceedings of the Nutrition Society; Cambridge University Press: Cambridge, UK, 2015; Volume 74, pp. 115–124. [Google Scholar]
- Engberg, E.; Figueiredo, R.A.O.; Rounge, T.B.; Weiderpass, E.; Viljakainen, H. Heavy screen users are the heaviest among 10,000 children. Sci. Rep. 2019, 9, 11158. [Google Scholar] [CrossRef]
- Pacifico, L.; Anania, C.; Osborn, J.F.; Ferraro, F.; Bonci, E.; Olivero, E.; Chiesa, C. Low 25(OH)D3 levels are associated with total adiposity, metabolic syndrome, and hypertension in Caucasian children and adolescents. Eur. J. Endocrinol. 2011, 165, 603–611. [Google Scholar] [CrossRef]
- Rosenstreich, S.J.; Rich, C.; Volwiler, W. Deposition in and release of vitamin D3 from body fat: Evidence for a storage site in the rat. J. Clin. Invest. 1971, 50, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Han, L.; Zhao, Y.; Li, G.; Zhu, Y.; Li, Y.; Li, M.; Gao, S.; Willi, S.M. Vitamin D levels are associated with metabolic syndrome in adolescents and young adults: The BCAMS study. Clin. Nutr. 2019, 38, 2161–2167. [Google Scholar] [CrossRef] [PubMed]
- Denova-Gutiérrez, E.; Muñoz-Aguirre, P.; López, D.; Flores, M.; Medeiros, M.; Tamborrel, N.; Clark, P. Low serum vitamin D concentrations are associated with insulin resistance in Mexican children and adolescents. Nutrients 2019, 11, 2109. [Google Scholar] [CrossRef] [PubMed]
- Mitri, J.; Nelson, J.; Ruthazer, R.; Garganta, C.; Nathan, D.M.; Hu, F.B.; Dawson-Hughes, B.; Pittas, A.G. Plasma 25-hydroxyvitamin D and risk of metabolic syndrome: An ancillary analysis in the Diabetes Prevention Program. Eur. J. Clin. Nutr. 2014, 68, 376–383. [Google Scholar] [CrossRef]
- Szlagatys-Sidorkiewicz, A.; Brzeziński, M.; Jankowska, A.; Metelska, P.; Słomińska-Fraczek, M.; Socha, P. Long-term effects of vitamin D supplementation in vitamin D deficient obese children participating in an integrated weight-loss programme (a double-blind placebo-controlled study)—Rationale for the study design. BMC Pediatr. 2017, 17, 97. [Google Scholar] [CrossRef]
- Kułaga, Z.; Litwin, M.; Tkaczyk, M.; Palczewska, I.; Zaja̧czkowska, M.; Zwolińska, D.; Krynicki, T.; Wasilewska, A.; Moczulska, A.; Morawiec-Knysak, A.; et al. Polish 2010 growth references for school-aged children and adolescents. Eur. J. Pediatr. 2011, 170, 599–609. [Google Scholar] [CrossRef]
- Reyman, M.; Verrijn Stuart, A.A.; Van Summeren, M.; Rakhshandehroo, M.; Nuboer, R.; De Boer, F.K.; Van Den Ham, H.J.; Kalkhoven, E.; Prakken, B.; Schipper, H.S. Vitamin D deficiency in childhood obesity is associated with high levels of circulating inflammatory mediators, and low insulin sensitivity. Int. J. Obes. 2014, 38, 46–52. [Google Scholar] [CrossRef]
- Ganji, V.; Zhang, X.; Shaikh, N.; Tangpricha, V. Serum 25-hydroxyvitamin D concentrations are associated with prevalence of metabolic syndrome and various cardiometabolic risk factors in US children and adolescents based on assay-adjusted serum 25-hydroxyvitamin D data from NHANES 2001-2006. Am. J. Clin. Nutr. 2011, 94, 225–233. [Google Scholar] [CrossRef]
- Song, Y.; Wang, L.; Pittas, A.G.; Del Gobbo, L.C.; Zhang, C.; Manson, J.E.; Hu, F.B. Blood 25-Hydroxy Vitamin D Levels and Incident Type 2 Diabetes. Diabetes Care 2013, 36, 1422–1428. [Google Scholar] [CrossRef]
- Alemzadeh, R.; Kichler, J.; Babar, G.; Calhoun, M. Hypovitaminosis D in obese children and adolescents: Relationship with adiposity, insulin sensitivity, ethnicity, and season. Metabolism 2008, 57, 183–191. [Google Scholar] [CrossRef]
- Belenchia, A.M.; Tosh, A.K.; Hillman, L.S.; Peterson, C.A. Correcting vitamin D insufficiency improves insulin sensitivity in obese adolescents: A randomized controlled trial. Am. J. Clin. Nutr. 2013, 97, 774–781. [Google Scholar] [CrossRef] [PubMed]
- Golzarand, M.; Hollis, B.W.; Mirmiran, P.; Wagner, C.L.; Shab-Bidar, S. Vitamin D supplementation and body fat mass: A systematic review and meta-analysis. Eur. J. Clin. Nutr. 2018, 72, 1345–1357. [Google Scholar] [CrossRef]
- Bassatne, A.; Chakhtoura, M.; Saad, R.; Fuleihan, G.E.H. Vitamin D supplementation in obesity and during weight loss: A review of randomized controlled trials. Metabolism 2019, 92, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Winzenberg, T.; Powell, S.; Shaw, K.A.; Jones, G. Effects of vitamin D supplementation on bone density in healthy children: Systematic review and meta-analysis. BMJ 2011, 342, 267. [Google Scholar] [CrossRef] [PubMed]
- Goulding, A.; Taylor, R.W.; Jones, I.E.; McAuley, K.A.; Manning, P.J.; Williams, S.M. Overweight and obese children have low bone mass and area for their weight. Int. J. Obes. 2000, 24, 627–632. [Google Scholar] [CrossRef] [PubMed]
- El Hage, R.; El Hage, Z.; Jacob, C.; Moussa, E.; Theunynck, D.; Baddoura, R. Bone Mineral Content and Density in Overweight and Control Adolescent Boys. J. Clin. Densitom. 2011, 14, 122–128. [Google Scholar] [CrossRef]
- McVey, M.K.; Geraghty, A.A.; O’Brien, E.C.; McKenna, M.J.; Kilbane, M.T.; Crowley, R.K.; Twomey, P.J.; McAuliffe, F.M. The impact of diet, body composition, and physical activity on child bone mineral density at five years of age—Findings from the ROLO Kids Study. Eur. J. Pediatr. 2020, 179, 121–131. [Google Scholar] [CrossRef]
- Rønne, M.S.; Heidemann, M.; Lylloff, L.; Schou, A.J.; Tarp, J.; Laursen, J.O.; Jørgensen, N.R.; Husby, S.; Wedderkopp, N.; Mølgaard, C. Bone Mass Development in Childhood and Its Association with Physical Activity and Vitamin D Levels. The CHAMPS-Study DK. Calcif. Tissue Int. 2019, 104, 1–13. [Google Scholar] [CrossRef]
- Kessler, J.; Koebnick, C.; Smith, N.; Adams, A. Childhood obesity is associated with increased risk of most lower extremity fractures pediatrics. Clin. Orthop. Relat. Res. 2013, 471, 1199–1207. [Google Scholar] [CrossRef]
- Cashman, K.D.; Hill, T.R.; Cotter, A.A.; Boreham, C.A.; Dubitzky, W.; Murray, L.; Strain, J.J.; Flynn, A.; Robson, P.J.; Wallace, J.M.; et al. Low vitamin D status adversely affects bone health parameters in adolescents 1-3. Am. J. Clin. Nutr. 2008, 87, 1039–1044. [Google Scholar] [CrossRef]
- Pekkinen, M.; Viljakainen, H.; Saarnio, E.; Lamberg-Allardt, C.; Mäkitie, O. Vitamin D is a major determinant of bone mineral density at school age. PLoS ONE 2012, 7, e40090. [Google Scholar] [CrossRef] [PubMed]
- Fuleihan, G.E.H.; Nabulsi, M.; Tamim, H.; Maalouf, J.; Salamoun, M.; Khalife, H.; Choucair, M.; Arabi, A.; Vieth, R. Effect of vitamin D replacement on musculoskeletal parameters in school children: A randomized controlled trial. J. Clin. Endocrinol. Metab. 2006, 91, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Lenders, C.M.; Feldman, H.A.; Von Scheven, E.; Merewood, A.; Sweeney, C.; Wilson, D.M.; Lee, P.D.K.; Abrams, S.H.; Gitelman, S.E.; Wertz, M.S.; et al. Relation of body fat indexes to vitamin D status and deficiency among obese adolescents. Am. J. Clin. Nutr. 2009, 90, 459–467. [Google Scholar] [PubMed]
- Maggio, A.B.R.; Belli, D.C.; Puigdefabregas, J.W.B.; Rizzoli, R.; Farpour-Lambert, N.J.; Beghetti, M.; McLin, V.A. High bone density in adolescents with obesity is related to fat mass and serum leptin concentrations. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 723–728. [Google Scholar] [PubMed]
- Soltani, S.; Hunter, G.R.; Kazemi, A.; Shab-Bidar, S. The effects of weight loss approaches on bone mineral density in adults: A systematic review and meta-analysis of randomized controlled trials. Osteoporos. Int. 2016, 27, 2655–2671. [Google Scholar] [CrossRef]
- Rector, R.S.; Loethen, J.; Ruebel, M.; Thomas, T.R.; Hinton, P.S. Serum markers of bone turnover are increased by modest weight loss with or without weight-bearing exercise in overweight premenopausal women. Appl. Physiol. Nutr. Metab. 2009, 34, 933–941. [Google Scholar] [CrossRef]
- Lindeman, K.G.; Greenblatt, L.B.; Rourke, C.; Bouxsein, M.L.; Finkelstein, J.S.; Yu, E.W. Longitudinal 5-year evaluation of bone density and microarchitecture after Roux-en-Y gastric bypass surgery. J. Clin. Endocrinol. Metab. 2018, 103, 4104–4112. [Google Scholar] [CrossRef]
- Elaine, W.Y.; Bouxsein, M.L.; Putman, M.S.; Monis, E.L.; Roy, A.E.; Pratt, J.S.A.; Butsch, W.S.; Finkelstein, J.S. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J. Clin. Endocrinol. Metab. 2015, 100, 1452–1459. [Google Scholar]
- Kaulfers, A.M.D.; Bean, J.A.; Inge, T.H.; Dolan, L.M.; Kalkwarf, H.J. Bone loss in adolescents after bariatric surgery. Pediatrics 2011, 127, e956–e961. [Google Scholar] [CrossRef]
- Labouesse, M.A.; Gertz, E.R.; Piccolo, B.D.; Souza, E.C.; Schuster, G.U.; Witbracht, M.G.; Woodhouse, L.R.; Adams, S.H.; Keim, N.L.; Van Loan, M.D. Associations among endocrine, inflammatory, and bone markers, body composition and weight loss induced bone loss. Bone 2014, 64, 138–146. [Google Scholar] [CrossRef]
- Burt, L.A.; Billington, E.O.; Rose, M.S.; Raymond, D.A.; Hanley, D.A.; Boyd, S.K. Effect of high-dose vitamin D supplementation on volumetric bone density and bone strength: A randomized clinical trial. JAMA J. Am. Med. Assoc. 2019, 322, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Inelmen, E.M.; Toffanello, E.D.; Enzi, G.; Gasparini, G.; Miotto, F.; Sergi, G.; Busetto, L. Predictors of drop-out in overweight and obese outpatients. Int. J. Obes. 2005, 29, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Ortner Hadžiabdić, M.; Mucalo, I.; Hrabač, P.; Matić, T.; Rahelić, D.; Božikov, V. Factors predictive of drop-out and weight loss success in weight management of obese patients. J. Hum. Nutr. Diet. 2015, 28, 24–32. [Google Scholar] [CrossRef] [PubMed]
| vitamin D (n = 85) | placebo (n = 67) | ||||
|---|---|---|---|---|---|
| Mean ± SD | (95% CI) | Mean ± SD | CI (–95%) | p | |
| age (years) | 11.10 ± 2.84 | 10.49–11.72 | 10.70 ± 3.13 | 9.92–11.47 | 0.389 |
| body mass (kg) | 59.01 ± 21.04 | 54.47–63.55 | 56.89 ± 20.08 | 52.00–61.9 | 0.706 |
| height (cm) | 150.79 ± 16.69 | 147.19–154.39 | 149.31 ± 18.29 | 144.85–153.77 | 0.660 |
| BMI | 24.97 ± 4.12 | 24.08–25.86 | 24.53 ± 3.57 | 23.66–25.41 | 0.759 |
| BMI centile | 95.18 ± 3.24 | 94.49–95.88 | 95.23 ±3.43 | 94.41–96.06 | 0.812 |
| no. of girls at visit 1 | 46 | 38 | 0.827 | ||
| % of girls at visit 1 | 54.12% | 56.72% | |||
| Variable | vitamin D | placebo | |||||
|---|---|---|---|---|---|---|---|
| No | Mean ± SD | 95% CI | No | Mean ± | 95% CI | p | |
| BMI visit 1 | 85 | 24.97 ± 4.12 | 24.08–25.86 | 67 | 24.53 ± 3.58 | 23.66–25.41 | 0.759 |
| BMI visit 4 | 56 | 24.33 ± 3.97 | 23.27–25.39 | 53 | 24.68 ± 3.46 | 23.73–25.64 | 0.479 |
| ΔBMI visit 4–1 | 56 | –0.46 ± 1.80 | −0.94–0.03 | 53 | 0.11 ±1.84 | −0.40–0.61 | 0.203 |
| BMI centile 1 visit | 85 | 95.18 ± 3.22 | 94.49–95.88 | 67 | 95.23 ± 3.39 | 94.41–96.06 | 0.812 |
| BMI centile 4 visit | 56 | 90.91 ± 9.40 | 88.39–93.43 | 53 | 92.64 ± 7.53 | 90.56–94.71 | 0.303 |
| Δ in BMI centiles visit 4–1 | 56 | −4.28 ± 8.43 | −6.54–−2.03 | 53 | −2.53 ± 6.10 | −4.21–−0.85 | 0.319 |
| 25 (OH) D level visit 1 | 85 | 19.35 ± 5.46 | 18.16–20.55 | 66 | 19.79 ± 5.15 | 18.52–21.06 | 0.622 * |
| 25 (OH) D level visit 4 | 45 | 24.99 ± 5.54 | 23.33–26.66 | 43 | 18.3 ± 6.70 | 16.25–20.37 | 0.000 * |
| Δ 25 (OH) level visit 4–1 | 45 | 6.06 ± 5.80 | 4.32–7.81 | 43 | −2.40 ± 5.97 | −4.24–−0.57 | 0.000 * |
| Variable | vitamin D | placebo | |||||
|---|---|---|---|---|---|---|---|
| No | Mean | CI (–95%) | No | Mean | CI (–95%) | p | |
| BI_FM (kg) visit 1 | 82 | 18.32 ± 8.01 | 16.56–20.08 | 64 | 17.80 ± 7.30 | 15.97–19.62 | 0.820 |
| BI_FM (kg) visit 4 | 55 | 18.29 ± 8.07 | 16.11–20.47 | 53 | 18.13 ± 7.18 | 16.15–20.11 | 0.907 |
| Δ BI_FM (kg) visit 4–1 | 54 | −0.11 ± 4.09 | −1.23–1.00 | 51 | 0.01 ± 4.01 | −1.11–1.14 | 0.890 |
| BI_FM (%) visit 1 | 54 | 31.15 ± 4.90 | 29.81–32.48 | 51 | 31.23 ± 5.91 | 29.57–32.89 | 0.741 |
| BI_FM (%) visit 4 | 54 | 29.57 ± 6.03 | 27.92–31.21 | 51 | 29.39 ± 6.95 | 27.44–31.35 | 0.889* |
| Δ BI_FM (%) visit 4–1 | 54 | −1.58 ± 4.04 | −2.68–0.47 | 51 | −1.83 ± 4.56 | −3.12–−0.55 | 0.951 |
| BI_MM (kg) visit 1 | 82 | 38.46 ± 14.00 | 35.39–41.54 | 64 | 37.10 ± 13.65 | 33.69–40.51 | 0.586 |
| BI_MM (kg) visit 4 | 56 | 40.12 ± 12.85 | 36.68–43.56 | 53 | 40.80 ± 12.92 | 37.24–44.36 | 0.886 |
| Δ BI_MM (kg) visit 4–1 | 55 | 2.45 ±2.57 | 1.75–3.14 | 51 | 3.33 ± 2.75 | 2.56–4.10 | 0.091 * |
| BI_MM (%) visit 1 | 82 | 65.69 ±5.39 | 64.50–66.87 | 64 | 65.48 ± 5.03 | 64.22–66.73 | 0.350 |
| BI_MM (%) visit 4 | 56 | 66.63 ±5.68 | 65.11–68.16 | 53 | 66.81 ± 6.52 | 65.01–68.61 | 0.896 |
| Δ BI_MM (%) visit 4–1 | 55 | 1.42 ±4.02 | 0.33–2.51 | 51 | 1.48 ± 3.72 | 0.43–2.53 | 0.949 |
| Vitamin D | Placebo | ||||||
|---|---|---|---|---|---|---|---|
| No | Mean | CI (–95%) | No | Mean | CI (–95%) | p | |
| Sp BMD visit 1 | 83 | 0.76 ± 0.18 | 0.72–0.80 | 67 | 0.74 ± 0.18 | 0.70–0.79 | 0.447 |
| Sp BMD visit 4 | 47 | 0.82 ± 0.19 | 0.76–0.87 | 47 | 0.80 ± 0.19 | 0.75–0.86 | 0.623 |
| Δ in Sp BMD visit 4–1 | 47 | 0.04 ± 0.04 | 0.03–0.06 | 47 | 0.06 ± 0.04 | 0.05–0.08 | 0.025 * |
| TBLH BMD visit 1 | 83 | 0.87 ± 0.14 | 0.84–0.90 | 67 | 0.86 ± 0.15 | 0.82–0.89 | 0.672 |
| TBLH BMD visit 4 | 48 | 0.91 ± 0.14 | 0.87–0.95 | 47 | 0.90 ± 0.15 | 0.86–0.94 | 0.740 |
| Δ in TBLH BMD visit 4–1 | 48 | 0.04± 0.03 | 0.04–0.05 | 47 | 0.04 ± 0.03 | 0.03–0.05 | 0.504* |
| TFM (kg) visit 1 | 83 | 25.18 ± 9.76 | 23.05–27.31 | 67 | 24.29 ± 9.08 | 22.08–26.51 | 0.652 |
| TFM (kg) visit 4 | 48 | 25.17 ± 8.72 | 22.63–27.70 | 47 | 25.07 ± 8.96 | 22.44–27.70 | 0.959* |
| Δ in TFM visit 4–1 | 48 | 0.73 ±4.55 | –0.59–2.05 | 47 | 0.68 ± 4.96 | –0.77–2.14 | 0.734 |
| TLM (kg) visit 1 | 83 | 32.52 ± 4.55 | 30.04–34.99 | 67 | 31.83 ± 10.94 | 29.16–34.50 | 0.823 |
| TLM (kg) visit 4 | 48 | 34.41 ± 10.33 | 31.41–37.42 | 47 | 34.48 ± 12.19 | 30.90–38.06 | 0.976 * |
| TFM (%) visit 1 | 48 | 43.46 ± 3.82 | 42.35–44.57 | 47 | 43.30 ± 4.42 | 42.00–44.60 | 0.847 |
| TFM (%) visit 4 | 48 | 41.89 ± 5.29 | 40.35–43.43 | 47 | 42.32 ± 5.50 | 40.71–43.94 | 0.695 |
| Δ in TFM (%) visit 4–1 | 48 | –1.57 ± 4.12 | –2.77–0.38 | 47 | –0.98 ± 3.97 | –2.14–0.19 | 0.472 * |
| TLM (%) visit 1 | 48 | 56.54 ± 3.82 | 55.43–57.65 | 47 | 56.70 ± 4.42 | 55.40–58.00 | 0.847 |
| TLM (%) visit 4 | 48 | 58.11 ± 5.29 | 56.57–59.65 | 47 | 57.68 ± 5.50 | 56.06–59.29 | 0.695 |
| Δ in TLM (%) visit 4–1 | 48 | 1.57 ± 4.12 | 0.38–2.77 | 47 | 0.98 ± 3.97 | –0.19–2.14 | 0.472 |
| 25 (OH) D Level Visit 1 | 25 (OH) D Level Visit 4 | Δ 25 (OH) Level Visit 4–1 | |
|---|---|---|---|
| BMI centile 1 visit | –0.088910 | –0.232998 | –0.066400 |
| BMI centile 4 visit | –0.128452 | –0.297140 | –0.147392 |
| Δ in BMI centiles visit 4–1 | –0.059634 | –0.141315 | –0.138827 |
| BI_FM (%) visit 1 | –0.248164 | –0.238226 | –0.020100 |
| BI_FM (%) visit 4 | –0.213330 | –0.226632 | –0.019981 |
| Δ BI_FM (%) visit 4–1 | 0.073786 | –0.013645 | –0.058235 |
| BI_MM (%) visit 1 | 0.214256 | 0.202164 | –0.005444 |
| BI_MM (%) visit 4 | 0.204376 | 0.233062 | 0.045692 |
| Δ BI_MM (%) visit 4–1 | –0.077210 | 0.057706 | 0.107305 |
| 25 (OH) D level visit 1 | 1.000000 | 0.322476 | –0.426874 |
| 25 (OH) D level visit 4 | 0.322476 | 1.000000 | 0.692743 |
| Δ 25 (OH) level visit 4–1 | –0.426874 | 0.692743 | 1.000000 |
| TBLH BMD visit 1 | –0.357821 | –0.164349 | 0.102925 |
| TBLH BMD visit 4 | –0.377036 | –0.222562 | 0.012532 |
| Δ in TBLH BMD visit 4–1 | 0.079692 | 0.007924 | –0.047583 |
| TFM (%) visit 1 | –0.177243 | –0.206046 | –0.111781 |
| TFM (%) visit 4 | –0.035164 | –0.122583 | –0.069020 |
| Δ in TFM (%) visit 2–1 | 0.174996 | –0.008749 | –0.047612 |
| TLM (%) visit 1 | 0.177243 | 0.206046 | 0.111781 |
| TLM (%) visit 4 | 0.035164 | 0.122583 | 0.069020 |
| Δ in TLM (%) visit 4–1 | –0.174996 | 0.008749 | 0.047612 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brzeziński, M.; Jankowska, A.; Słomińska-Frączek, M.; Metelska, P.; Wiśniewski, P.; Socha, P.; Szlagatys-Sidorkiewicz, A. Long-Term Effects of Vitamin D Supplementation in Obese Children During Integrated Weight–Loss Programme—A Double Blind Randomized Placebo–Controlled Trial. Nutrients 2020, 12, 1093. https://doi.org/10.3390/nu12041093
Brzeziński M, Jankowska A, Słomińska-Frączek M, Metelska P, Wiśniewski P, Socha P, Szlagatys-Sidorkiewicz A. Long-Term Effects of Vitamin D Supplementation in Obese Children During Integrated Weight–Loss Programme—A Double Blind Randomized Placebo–Controlled Trial. Nutrients. 2020; 12(4):1093. https://doi.org/10.3390/nu12041093
Chicago/Turabian StyleBrzeziński, Michał, Agnieszka Jankowska, Magdalena Słomińska-Frączek, Paulina Metelska, Piotr Wiśniewski, Piotr Socha, and Agnieszka Szlagatys-Sidorkiewicz. 2020. "Long-Term Effects of Vitamin D Supplementation in Obese Children During Integrated Weight–Loss Programme—A Double Blind Randomized Placebo–Controlled Trial" Nutrients 12, no. 4: 1093. https://doi.org/10.3390/nu12041093
APA StyleBrzeziński, M., Jankowska, A., Słomińska-Frączek, M., Metelska, P., Wiśniewski, P., Socha, P., & Szlagatys-Sidorkiewicz, A. (2020). Long-Term Effects of Vitamin D Supplementation in Obese Children During Integrated Weight–Loss Programme—A Double Blind Randomized Placebo–Controlled Trial. Nutrients, 12(4), 1093. https://doi.org/10.3390/nu12041093








