A Mediterranean Diet Is Positively Associated with Bone and Muscle Health in a Non-Mediterranean Region in 25,450 Men and Women from EPIC-Norfolk
Abstract
:1. Introduction
2. Materials and Methods
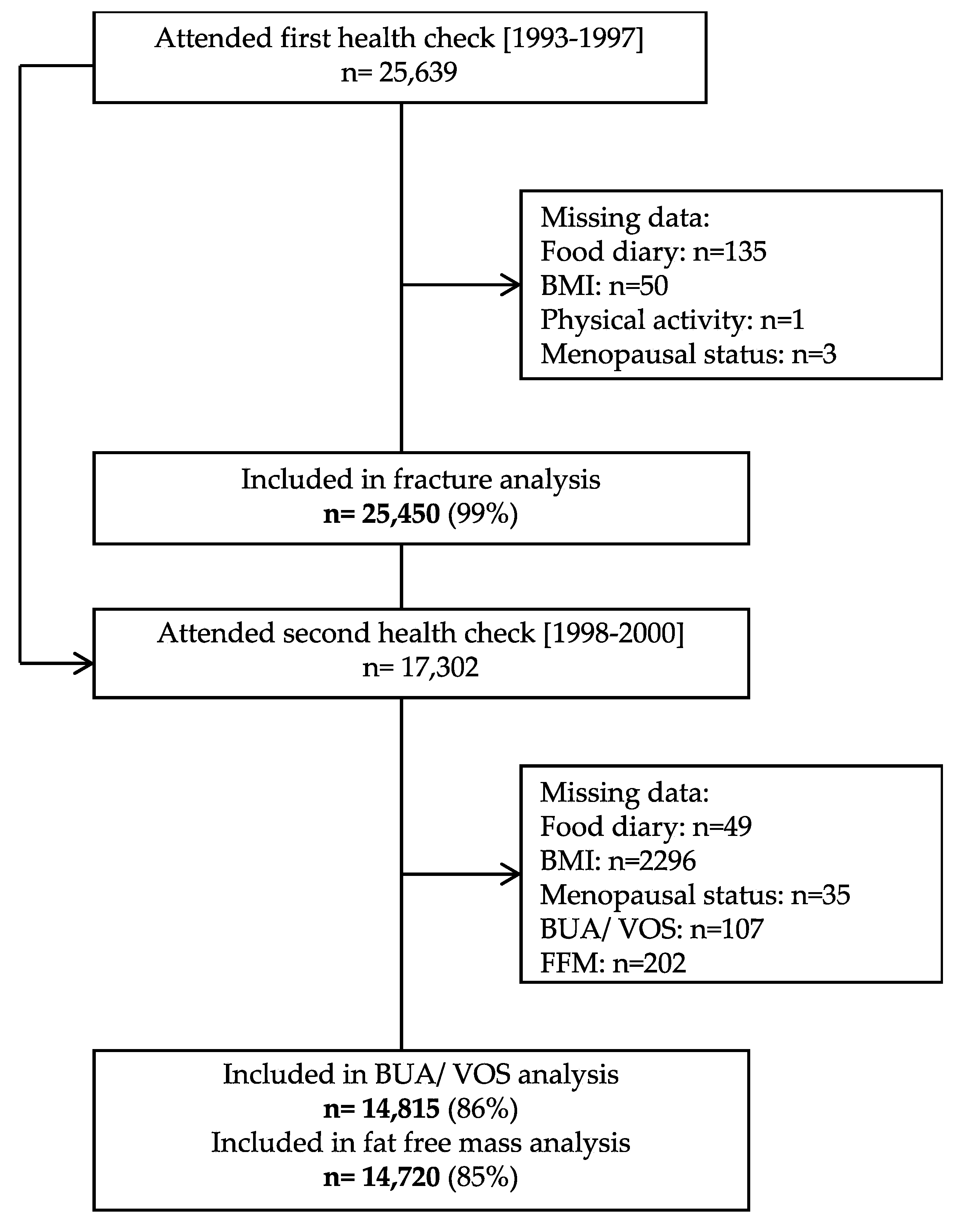
2.1. Study Population
2.2. Outcome Assessment
2.3. Assessment of Dietary Intakes
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef] [Green Version]
- Esposito, K.; Maiorino, M.I.; Ceriello, A.; Giugliano, D. Prevention and control of type 2 diabetes by Mediterranean diet: A systematic review. Diabetes Res. Clin. Pract. 2010, 89, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Jennings, A.; Cashman, K.D.; Gillings, R.; Cassidy, A.; Tang, J.; Fraser, W.; Dowling, K.G.; Hull, G.L.J.; Berendsen, A.A.M.; de Groot, L.; et al. A Mediterranean-like dietary pattern with vitamin D3 (10 microg/d) supplements reduced the rate of bone loss in older Europeans with osteoporosis at baseline: Results of a 1-y randomized controlled trial. Am. J. Clin. Nutr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Benetou, V.; Orfanos, P.; Feskanich, D.; Michaelsson, K.; Pettersson-Kymmer, U.; Byberg, L.; Eriksson, S.; Grodstein, F.; Wolk, A.; Jankovic, N.; et al. Mediterranean diet and hip fracture incidence among older adults: The CHANCES project. Osteoporos Int. 2018, 29, 1591–1599. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.V.; Bunn, D.K.; Hayhoe, R.P.; Appleyard, W.O.; Lenaghan, E.A.; Welch, A.A. Relationship between the Mediterranean dietary pattern and musculoskeletal health in children, adolescents, and adults: Systematic review and evidence map. Nutr. Rev. 2017, 75, 830–857. [Google Scholar] [CrossRef] [Green Version]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [Green Version]
- Sahni, S.; Mangano, K.M.; McLean, R.R.; Hannan, M.T.; Kiel, D.P. Dietary Approaches for Bone Health: Lessons from the Framingham Osteoporosis Study. Curr. Osteoporos. Rep. 2015, 13, 245–255. [Google Scholar] [CrossRef] [Green Version]
- Farina, E.K.; Kiel, D.P.; Roubenoff, R.; Schaefer, E.J.; Cupples, L.A.; Tucker, K.L. Protective effects of fish intake and interactive effects of long-chain polyunsaturated fatty acid intakes on hip bone mineral density in older adults: The Framingham Osteoporosis Study. Am. J. Clin. Nutr. 2011, 93, 1142–1151. [Google Scholar] [CrossRef] [Green Version]
- Roncero-Martin, R.; Aliaga Vera, I.; Moreno-Corral, L.J.; Moran, J.M.; Lavado-Garcia, J.M.; Pedrera-Zamorano, J.D.; Pedrera-Canal, M. Olive Oil Consumption and Bone Microarchitecture in Spanish Women. Nutrients 2018, 10, 968. [Google Scholar] [CrossRef] [Green Version]
- Domazetovic, V.; Marcucci, G.; Iantomasi, T.; Brandi, M.L.; Vincenzini, M.T. Oxidative stress in bone remodeling: Role of antioxidants. Clin. Cases Miner. Bone Metab. Off. J. Ital. Soc. Osteoporos. Miner. Metab. Skelet. Dis. 2017, 14, 209–216. [Google Scholar] [CrossRef]
- Longo, A.B.; Ward, W.E. PUFAs, Bone Mineral Density, and Fragility Fracture: Findings from Human Studies. Adv. Nutr. 2016, 7, 299–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobs, D.R., Jr.; Steffen, L.M. Nutrients, foods, and dietary patterns as exposures in research: A framework for food synergy. Am. J. Clin. Nutr. 2003, 78, 508s–513s. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.H.; Liu, C.; You, L.; Simmons, C.A. Boning up on Wolff’s Law: Mechanical regulation of the cells that make and maintain bone. J. Biomech. 2010, 43, 108–118. [Google Scholar] [CrossRef] [PubMed]
- Hamrick, M.W. A role for myokines in muscle-bone interactions. Exerc. Sport Sci. Rev. 2011, 39, 43–47. [Google Scholar] [CrossRef] [Green Version]
- Haring, B.; Crandall, C.J.; Wu, C.; LeBlanc, E.S.; Shikany, J.M.; Carbone, L.; Orchard, T.; Thomas, F.; Wactawaski-Wende, J.; Li, W.; et al. Dietary Patterns and Fractures in Postmenopausal Women: Results From the Women’s Health Initiative. JAMA Intern. Med. 2016, 176, 645–652. [Google Scholar] [CrossRef]
- Kelaiditi, E.; Jennings, A.; Steves, C.J.; Skinner, J.; Cassidy, A.; MacGregor, A.J.; Welch, A.A. Measurements of skeletal muscle mass and power are positively related to a Mediterranean dietary pattern in women. Osteoporos. Int. 2016, 27, 3251–3260. [Google Scholar] [CrossRef]
- Chen, G.-D.; Dong, X.-W.; Zhu, Y.-Y.; Tian, H.-Y.; He, J.; Chen, Y.-M. Adherence to the Mediterranean diet is associated with a higher BMD in middle-aged and elderly Chinese. Sci. Rep. 2016, 6, 25662. [Google Scholar] [CrossRef] [Green Version]
- Day, N.; Oakes, S.; Luben, R.; Khaw, K.T.; Bingham, S.; Welch, A.; Wareham, N. EPIC-Norfolk: Study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br. J. Cancer 1999, 80 (Suppl. 1), 95–103. [Google Scholar]
- Khaw, K.T.; Reeve, J.; Luben, R.; Bingham, S.; Welch, A.; Wareham, N.; Oakes, S.; Day, N. Prediction of total and hip fracture risk in men and women by quantitative ultrasound of the calcaneus: EPIC-Norfolk prospective population study. Lancet 2004, 363, 197–202. [Google Scholar] [CrossRef]
- Moayyeri, A.; Kaptoge, S.; Dalzell, N.; Bingham, S.; Luben, R.N.; Wareham, N.J.; Reeve, J.; Khaw, K.T. Is QUS or DXA better for predicting the 10-year absolute risk of fracture? J. Bone Miner. Res. 2009, 24, 1319–1325. [Google Scholar] [CrossRef]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M.; et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 547–558. [Google Scholar] [CrossRef]
- Beeson, W.L.; Batech, M.; Schultz, E.; Salto, L.; Firek, A.; Deleon, M.; Balcazar, H.; Cordero-Macintyre, Z. Comparison of body composition by bioelectrical impedance analysis and dual-energy X-ray absorptiometry in Hispanic diabetics. Int. J. Body Compos. Res. 2010, 8, 45–50. [Google Scholar] [PubMed]
- Lentjes, M.A.; McTaggart, A.; Mulligan, A.A.; Powell, N.A.; Parry-Smith, D.; Luben, R.N.; Bhaniani, A.; Welch, A.A.; Khaw, K.T. Dietary intake measurement using 7 d diet diaries in British men and women in the European Prospective Investigation into Cancer-Norfolk study: A focus on methodological issues. Br. J. Nutr. 2014, 111, 516–526. [Google Scholar] [CrossRef]
- Welch, A.A.; McTaggart, A.; Mulligan, A.A.; Luben, R.; Walker, N.; Khaw, K.T.; Day, N.E.; Bingham, S.A. DINER (Data Into Nutrients for Epidemiological Research)-a new data-entry program for nutritional analysis in the EPIC-Norfolk cohort and the 7-day diary method. Public Health Nutr. 2001, 4, 1253–1265. [Google Scholar] [CrossRef] [Green Version]
- Fung, T.T.; McCullough, M.L.; Newby, P.K.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef]
- Wareham, N.J.; Jakes, R.W.; Rennie, K.L.; Schuit, J.; Mitchell, J.; Hennings, S.; Day, N.E. Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2003, 6, 407–413. [Google Scholar] [CrossRef] [Green Version]
- Institute of Medicine of the National Academies. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids; National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Benetou, V.; Orfanos, P.; Pettersson-Kymmer, U.; Bergstrom, U.; Svensson, O.; Johansson, I.; Berrino, F.; Tumino, R.; Borch, K.B.; Lund, E.; et al. Mediterranean diet and incidence of hip fractures in a European cohort. Osteoporos. Int. 2013, 24, 1587–1598. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; Meyer, H.E.; Willett, W.C.; Feskanich, D. Association between Diet Quality Scores and Risk of Hip Fracture in Postmenopausal Women and Men Aged 50 Years and Older. J. Acad. Nutr. Diet. 2018, 118, 2269–2279.e2264. [Google Scholar] [CrossRef]
- Finck, H.; Hart, A.R.; Lentjes, M.A.; Jennings, A.; Luben, R.N.; Khaw, K.T.; Welch, A.A. Cross-sectional and prospective associations between dietary and plasma vitamin C, heel bone ultrasound, and fracture risk in men and women in the European Prospective Investigation into Cancer in Norfolk cohort. Am. J. Clin. Nutr. 2015, 102, 1416–1424. [Google Scholar] [CrossRef] [Green Version]
- Hayhoe, R.P.; Lentjes, M.A.; Luben, R.N.; Khaw, K.T.; Welch, A.A. Dietary magnesium and potassium intakes and circulating magnesium are associated with heel bone ultrasound attenuation and osteoporotic fracture risk in the EPIC-Norfolk cohort study. Am. J. Clin. Nutr. 2015, 102, 376–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayhoe, R.P.G.; Lentjes, M.A.H.; Mulligan, A.A.; Luben, R.N.; Khaw, K.T.; Welch, A.A. Carotenoid dietary intakes and plasma concentrations are associated with heel bone ultrasound attenuation and osteoporotic fracture risk in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk cohort. Br. J. Nutr. 2017, 117, 1439–1453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorning, T.K.; Bertram, H.C.; Bonjour, J.P.; de Groot, L.; Dupont, D.; Feeney, E.; Ipsen, R.; Lecerf, J.M.; Mackie, A.; McKinley, M.C.; et al. Whole dairy matrix or single nutrients in assessment of health effects: Current evidence and knowledge gaps. Am. J. Clin. Nutr. 2017, 105, 1033–1045. [Google Scholar] [CrossRef] [PubMed]
- Savanelli, M.C.; Barrea, L.; Macchia, P.E.; Savastano, S.; Falco, A.; Renzullo, A.; Scarano, E.; Nettore, I.C.; Colao, A.; Di Somma, C. Preliminary results demonstrating the impact of Mediterranean diet on bone health. J. Transl. Med. 2017, 15, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Štefan, L.; Čule, M.; Milinović, I.; Sporiš, G.; Juranko, D. The relationship between adherence to the Mediterranean diet and body composition in Croatian university students. Eur. J. Integr. Med. 2017, 13, 41–46. [Google Scholar] [CrossRef]
- Achamrah, N.; Colange, G.; Delay, J.; Rimbert, A.; Folope, V.; Petit, A.; Grigioni, S.; Dechelotte, P.; Coeffier, M. Comparison of body composition assessment by DXA and BIA according to the body mass index: A retrospective study on 3655 measures. PLoS ONE 2018, 13, e0200465. [Google Scholar] [CrossRef] [Green Version]
- Komar, C.; Ahmed, M.; Chen, A.; Richwine, H.; Zia, N.; Nazar, A.; Bauer, L. Advancing Methods of Assessing Bone Quality to Expand Screening for Osteoporosis. J. Am. Osteopath. Assoc. 2019, 119, 147–154. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]



| 1st Health Check (1993–1997) | 2nd Health Check (1998–2000) | |||||||
|---|---|---|---|---|---|---|---|---|
| All (n = 25,450) | Men (n = 11,511) | Women (n = 13,939) | p= | All (n = 14,815) | Men (n = 6490) | Women (n = 8325) | p= | |
| Age, years | 59.3 ± 9.3 | 59.7 ± 9.3 | 58.9 ± 9.3 | <0.01 | 62.2 ± 9.0 | 62.9 ± 9.0 | 61.6 ± 9.0 | <0.01 |
| Fracture, y | 2195 (8.6) | 610 (5.3) | 1585 (11.4) | <0.01 | - | - | - | - |
| BUA, dB/MHz | - | - | - | - | 79.9 ± 19.2 | 90.1 ± 17.5 | 72.1 ± 16.5 | <0.01 |
| VOS, m/s | - | - | - | - | 1634 ± 41.4 | 1645 ± 39.9 | 1625 ± 40.2 | <0.01 |
| BMI, kg/m2 | 26.4 ± 3.9 | 26.5 ± 3.3 | 26.2 ± 4.4 | <0.01 | 26.7 ± 4.0 | 26.9 ± 3.3 | 26.5 ± 4.4 | <0.01 |
| FFM (kg) | - | - | - | - | 49.8 ± 11.8 | 61.7 ± 6.0 | 40.6 ± 4.8 | <0.01 |
| FFMBMI (kg/(kg/m2)) | - | - | - | - | 1.9 ± 0.5 | 2.3 ± 0.3 | 1.6 ± 0.3 | <0.01 |
| Current smoking, y | 3170 (12.5) | 1472 (12.8) | 1698 (12.2) | <0.01 | 1243 (8.5) | 540 (8.4) | 703 (8.6) | <0.01 |
| Physically active, y | 4610 (18.1) | 2479 (21.5) | 2131 (15.3) | <0.01 | 2825 (19.4) | 1431 (22.4) | 1394 (17.0) | <0.01 |
| Family history of osteoporosis, y | 1117 (4.4) | 307 (2.7) | 810 (5.8) | <0.01 | 686 (4.7) | 174 (2.7) | 512 (6.3) | <0.01 |
| Vitamin D supplements, y | 6849 (26.9) | 2570 (22.3) | 4279 (30.7) | <0.01 | 4335 (29.7) | 1599 (25.0) | 2736 (33.5) | <0.01 |
| Calcium supplements, y | 911 (3.6) | 165 (1.4) | 746 (5.4) | <0.01 | 598 (4.1) | 98 (1.5) | 500 (6.1) | <0.01 |
| Corticosteroid or aspirin, y | 2687 (10.6) | 1508 (13.1) | 1179 (8.5) | <0.01 | 1667 (11.4) | 883 (13.8) | 784 (9.6) | <0.01 |
| HRT, y | - | - | 2824 (20.3) | - | - | - | 1732 (21.2) | - |
| Postmenopausal, y | - | - | 8351 (59.9) | - | - | - | 6002 (73.4) | - |
| aMED, points | 4.0 ± 1.7 | 4.0 ± 1.7 | 4.0 ± 1.7 | 0.19 | 4.1 ± 1.7 | 4.1 ± 1.7 | 4.1 ± 1.7 | 0.02 |
| MDS, points | 4.3 ± 1.6 | 4.4 ± 1.6 | 4.2 ± 1.6 | <0.01 | 4.33 ± 1.59 | 4.40 ± 1.60 | 4.28 ± 1.58 | <0.01 |
| Energy intake, kcal/d | 1941 ± 534 | 2240 ± 527 | 1694 ± 395 | <0.01 | 1974 ± 517 | 2285 ± 502 | 1731 ± 380 | <0.01 |
| Calcium intakes, mg/d | 835 ± 282 | 919 ± 297 | 766 ± 248 | <0.01 | 853 ± 275 | 942 ± 289 | 784 ± 243 | <0.01 |
| Vitamin D intakes, mg/d | 3.3 ± 2.4 | 3.7 ± 2.7 | 2.9 ± 2.1 | <0.01 | 3.4 ± 2.4 | 3.9 ± 2.8 | 3.0 ± 1.9 | <0.01 |
| Score | Component | Hazard Ratio (95% CI) | p-Value |
|---|---|---|---|
| aMED | Vegetables, g/d | 0.93 (0.86, 1.02) | 0.13 |
| Legumes, g/d | 0.91 (0.84, 1.00) | 0.04 | |
| Fruit, g/d | 0.97 (0.89, 1.06) | 0.53 | |
| Fish, g/d | 1.01 (0.93, 1.11) | 0.76 | |
| Nuts and seeds, g/d | 0.86 (0.77, 0.96) | 0.01 | |
| Wholegrains, g/d | 1.01 (0.92, 1.10) | 0.89 | |
| Red and processed meat, g/d | 0.91 (0.83, 0.99) | 0.03 | |
| Ratio MUFA: SFA | 1.03 (0.94, 1.12) | 0.57 | |
| Alcohol, g/d | 0.91 (0.83, 0.99) | 0.04 | |
| MDS | |||
| Vegetables, g/d | 0.94 (0.86, 1.02) | 0.14 | |
| Legumes, g/d | 0.92 (0.84, 1.00) | 0.06 | |
| Fruit and nuts, g/d | 0.97 (0.89, 1.06) | 0.54 | |
| Fish, g/d | 1.01 (0.92, 1.10) | 0.85 | |
| Cereals, g/d | 0.99 (0.90, 1.09) | 0.82 | |
| Dairy, g/d | 0.94 (0.84, 1.05) | 0.28 | |
| Meat and eggs, g/d | 0.96 (0.88, 1.05) | 0.38 | |
| Ratio MUFA: SFA | 1.01 (0.93, 1.11) | 0.76 | |
| Alcohol, g/d | 0.93 (0.85, 1.02) | 0.13 |
| Sex | Quintile | BUA (dB/MHz) | VOS (m/s) | FFMBMI (kg/(kg/m2)) | |||
|---|---|---|---|---|---|---|---|
| n = | Mean (95% CI) | n = | Mean (95% CI) | n= | Mean (95% CI) | ||
| All | Q1 | 2725 | 79.5 (78.9,80.1) | 2725 | 1632 (1631,1634) | 2711 | 1.87 (1.86,1.88) |
| Q2 | 2865 | 79.3 (78.7,79.8) | 2865 | 1632 (1631,1634) | 2848 | 1.88 (1.87,1.89) | |
| Q3 | 3240 | 80.2 (79.7,80.7) | 3240 | 1634 (1633,1636) | 3212 | 1.90 (1.89,1.91) | |
| Q4 | 2928 | 80.1 (79.5,80.7) | 2928 | 1634 (1633,1635) | 2914 | 1.90 (1.89,1.91) | |
| Q5 | 3057 | 80.6 (80.0,81.1) | 3057 | 1635 (1633,1636) | 3035 | 1.92 (1.91,1.93) | |
| Q5–Q1 | 1.04 (0.22,1.87) | 2.26 (0.27,4.24) | 0.05 (0.04,0.06) | ||||
| p = | <0.01 | 0.01 | <0.01 | ||||
| Men | Q1 | 1157 | 89.9 (88.9,90.9) | 1157 | 1644 (1642,1646) | 1155 | 2.30 (2.28,2.31) |
| Q2 | 1213 | 89.6 (88.6,90.6) | 1213 | 1644 (1642,1646) | 1208 | 2.31 (2.29,2.32) | |
| Q3 | 1442 | 90.0 (89.1,90.9) | 1442 | 1645 (1643,1648) | 1423 | 2.31 (2.30,2.33) | |
| Q4 | 1303 | 90.2 (89.3,91.2) | 1303 | 1645 (1643,1647) | 1299 | 2.33 (2.31,2.34) | |
| Q5 | 1375 | 90.5 (89.5,91.4) | 1375 | 1647 (1645,1649) | 1361 | 2.34 (2.33,2.36) | |
| Q5–Q1 | 0.58 (−0.80, 1.97) | 2.87 (−0.27, 6.01) | 0.05 (0.03, 0.07) | ||||
| p = | 0.25 | 0.06 | <0.01 | ||||
| Women | Q1 | 1568 | 71.5 (70.8,72.2) | 1568 | 1623 (1622,1625) | 1556 | 1.54 (1.53,1.55) |
| Q2 | 1652 | 71.4 (70.7,72.0) | 1652 | 1624 (1622,1625) | 1640 | 1.55 (1.54,1.57) | |
| Q3 | 1798 | 72.5 (71.9,73.2) | 1798 | 1626 (1624,1627) | 1789 | 1.57 (1.56,1.59) | |
| Q4 | 1625 | 72.1 (71.4,72.8) | 1625 | 1625 (1623,1627) | 1615 | 1.57 (1.56,1.58) | |
| Q5 | 1682 | 72.7 (72.0,73.4) | 1682 | 1625 (1623,1627) | 1674 | 1.59 (1.58,1.60) | |
| Q5–Q1 | 1.19 (0.20, 2.18) | 1.44 (−1.07, 3.94) | 0.05 (0.03, 0.07) | ||||
| p = | <0.01 | 0.14 | <0.01 | ||||
| Sex | Quintile | BUA (dB/MHz) | VOS (m/s) | FFMBMI (kg/(kg/m2)) | |||
|---|---|---|---|---|---|---|---|
| n = | Mean (95% CI) | n = | Mean (95% CI) | n = | Mean (95% CI) | ||
| All | Q1 | 1872 | 79.1 (78.4,79.8) | 1872 | 1632 (1630,1633) | 1852 | 1.88 (1.87,1.89) |
| Q2 | 2669 | 79.8 (79.2,80.4) | 2669 | 1634 (1632,1635) | 2668 | 1.89 (1.88,1.90) | |
| Q3 | 3468 | 79.9 (79.3,80.4) | 3468 | 1633 (1632,1635) | 3446 | 1.90 (1.89,1.90) | |
| Q4 | 3350 | 80.1 (79.5,80.6) | 3350 | 1634 (1633,1635) | 3314 | 1.89 (1.88,1.90) | |
| Q5 | 3456 | 80.5 (79.9,81.0) | 3456 | 1634 (1633,1636) | 3440 | 1.91 (1.90,1.92) | |
| Q5–Q1 | 1.35 (0.45, 2.25) | 2.57 (0.41, 4.73) | 0.03 (0.01, 0.04) | ||||
| p = | <0.01 | 0.05 | <0.01 | ||||
| Men | Q1 | 754 | 88.9 (87.6,90.1) | 754 | 1643 (1640,1646) | 749 | 2.31 (2.29,2.33) |
| Q2 | 1122 | 90.1 (89.0,91.1) | 1122 | 1646 (1643,1648) | 1123 | 2.31 (2.29,2.32) | |
| Q3 | 1511 | 90.4 (89.5,91.2) | 1511 | 1646 (1644,1648) | 1497 | 2.32 (2.30,2.33) | |
| Q4 | 1504 | 89.6 (88.8,90.5) | 1504 | 1644 (1642,1646) | 1486 | 2.32 (2.31,2.33) | |
| Q5 | 1599 | 90.7 (89.9,91.6) | 1599 | 1647 (1645,1649) | 1591 | 2.33 (2.32,2.34) | |
| Q5–Q1 | 1.85 (0.33, 3.37) | 3.95 (0.50, 7.40) | 0.02 (0.00, 0.05) | ||||
| p = | 0.08 | 0.14 | 0.02 | ||||
| Women | Q1 | 1118 | 71.6 (70.8,72.4) | 1118 | 1623 (1621,1625) | 1103 | 1.55 (1.53,1.56) |
| Q2 | 1547 | 71.8 (71.1,72.5) | 1547 | 1625 (1623,1627) | 1545 | 1.56 (1.54,1.57) | |
| Q3 | 1957 | 71.6 (71.0,72.2) | 1957 | 1624 (1622,1625) | 1949 | 1.57 (1.56,1.58) | |
| Q4 | 1846 | 72.6 (72.0,73.3) | 1846 | 1626 (1625,1628) | 1828 | 1.56 (1.55,1.57) | |
| Q5 | 1857 | 72.5 (71.8,73.1) | 1857 | 1624 (1623,1626) | 1849 | 1.58 (1.57,1.59) | |
| Q5–Q1 | 0.87 (−0.20, 1.93) | 1.34 (−1.35, 4.04) | 0.03 (0.01, 0.05) | ||||
| p = | 0.02 | 0.21 | <0.01 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jennings, A.; Mulligan, A.A.; Khaw, K.-T.; Luben, R.N.; Welch, A.A. A Mediterranean Diet Is Positively Associated with Bone and Muscle Health in a Non-Mediterranean Region in 25,450 Men and Women from EPIC-Norfolk. Nutrients 2020, 12, 1154. https://doi.org/10.3390/nu12041154
Jennings A, Mulligan AA, Khaw K-T, Luben RN, Welch AA. A Mediterranean Diet Is Positively Associated with Bone and Muscle Health in a Non-Mediterranean Region in 25,450 Men and Women from EPIC-Norfolk. Nutrients. 2020; 12(4):1154. https://doi.org/10.3390/nu12041154
Chicago/Turabian StyleJennings, Amy, Angela A. Mulligan, Kay-Tee Khaw, Robert N. Luben, and Ailsa A. Welch. 2020. "A Mediterranean Diet Is Positively Associated with Bone and Muscle Health in a Non-Mediterranean Region in 25,450 Men and Women from EPIC-Norfolk" Nutrients 12, no. 4: 1154. https://doi.org/10.3390/nu12041154
APA StyleJennings, A., Mulligan, A. A., Khaw, K. -T., Luben, R. N., & Welch, A. A. (2020). A Mediterranean Diet Is Positively Associated with Bone and Muscle Health in a Non-Mediterranean Region in 25,450 Men and Women from EPIC-Norfolk. Nutrients, 12(4), 1154. https://doi.org/10.3390/nu12041154





