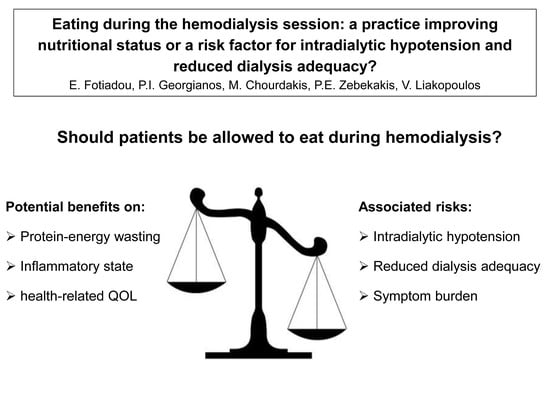
Eating during the Hemodialysis Session: A Practice Improving Nutritional Status or a Risk Factor for Intradialytic Hypotension and Reduced Dialysis Adequacy?
Abstract
:1. Introduction
2. Intradialytic Hypotension
2.1. Cross-Sectional Studies
2.2. Interventional Studies
3. Hemodialysis Adequacy
4. Malnutrition
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kistler, B.; Benner, D.; Burgess, M.; Stasios, M.; Kalantar-Zadeh, K.; Wilund, K.R. To eat or not to eat-international experiences with eating during hemodialysis treatment. J. Ren. Nutr. 2014, 24, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Benner, D.; Burgess, M.; Stasios, M.; Brosch, B.; Wilund, K.; Shen, S.; Kistler, B. In-Center Nutrition Practices of Clinics within a Large Hemodialysis Provider in the United States. Clin. J. Am. Soc. Nephrol. 2016, 11, 770–775. [Google Scholar] [CrossRef] [PubMed]
- Caglar, K.; Fedje, L.; Dimmitt, R.; Hakim, R.M.; Shyr, Y.; Ikizler, T.A. Therapeutic effects of oral nutritional supplementation during hemodialysis. Kidney Int. 2002, 62, 1054–1059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pupim, L.B.; Majchrzak, K.M.; Flakoll, P.J.; Ikizler, T.A. Intradialytic oral nutrition improves protein homeostasis in chronic hemodialysis patients with deranged nutritional status. J. Am. Soc. Nephrol. 2006, 17, 3149–3157. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Braglia, A.; Chow, J.; Kwon, O.; Kuwae, N.; Colman, S.; Cockram, D.B.; Kopple, J.D. An anti-inflammatory and antioxidant nutritional supplement for hypoalbuminemic hemodialysis patients: A pilot/feasibility study. J. Ren. Nutr. 2005, 15, 318–331. [Google Scholar] [CrossRef]
- Scott, M.K.; Shah, N.A.; Vilay, A.M.; Thomas, J., III; Kraus, M.A.; Mueller, B.A. Effects of peridialytic oral supplements on nutritional status and quality of life in chronic hemodialysis patients. J. Ren. Nutr. 2009, 19, 145–152. [Google Scholar] [CrossRef]
- Kistler, B.M.; Benner, D.; Burrowes, J.D.; Campbell, K.L.; Fouque, D.; Garibotto, G.; Kopple, J.D.; Kovesdy, C.P.; Rhee, C.M.; Steiber, A.; et al. Eating During Hemodialysis Treatment: A Consensus Statement From the International Society of Renal Nutrition and Metabolism. J. Ren. Nutr. 2018, 28, 4–12. [Google Scholar] [CrossRef] [Green Version]
- Kooman, J.; Basci, A.; Pizzarelli, F.; Canaud, B.; Haage, P.; Fouque, D.; Konner, K.; Martin-Malo, A.; Pedrini, L.; Tattersall, J.; et al. EBPG guideline on haemodynamic instability. Nephrol. Dial. Transplant. 2007, 22 (Suppl. 2), ii22–ii44. [Google Scholar] [CrossRef] [Green Version]
- Barakat, M.M.; Nawab, Z.M.; Yu, A.W.; Lau, A.H.; Ing, T.S.; Daugirdas, J.T. Hemodynamic effects of intradialytic food ingestion and the effects of caffeine. J. Am. Soc. Nephrol. 1993, 3, 1813–1818. [Google Scholar]
- Sherman, R.A.; Torres, F.; Cody, R.P. Postprandial blood pressure changes during hemodialysis. Am. J. Kidney Dis. 1988, 12, 37–39. [Google Scholar] [CrossRef]
- Zoccali, C.; Mallamaci, F.; Ciccarelli, M.; Maggiore, Q. Postprandial alterations in arterial pressure control during hemodialysis in uremic patients. Clin. Nephrol. 1989, 31, 323–326. [Google Scholar] [PubMed]
- Agarwal, R.; Georgianos, P. Feeding during dialysis-risks and uncertainties. Nephrol. Dial. Transplant. 2018, 33, 917–922. [Google Scholar] [CrossRef] [PubMed]
- San Juan, M.M.; Pilar, S.M.; Santos de Pablos, M.R. Reduction of Kt/V by food intake during haemodialysis. EDTNA ERCA J. 2001, 27, 150–152. [Google Scholar]
- Singri, N.; Johnstone, D.; Paparello, J.; Khosla, N.; Ahya, S.N.; Ghossein, C.; Schlueter, W.; Rosa, R.; Batlle, D.; Levin, M.L. Effect of predialysis eating on measurement of urea reduction ratio and Kt/V. Adv. Chronic Kidney Dis. 2004, 11, 398–403. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Ikizler, T.A. Let them eat during dialysis: An overlooked opportunity to improve outcomes in maintenance hemodialysis patients. J. Ren. Nutr. 2013, 23, 157–163. [Google Scholar] [CrossRef] [Green Version]
- Kalantar-Zadeh, K.; Tortorici, A.R.; Chen, J.L.; Kamgar, M.; Lau, W.L.; Moradi, H.; Rhee, C.M.; Streja, E.; Kovesdy, C.P. Dietary restrictions in dialysis patients: Is there anything left to eat? Semin. Dial. 2015, 28, 159–168. [Google Scholar] [CrossRef]
- Piccoli, G.B.; Lippi, F.; Fois, A.; Gendrot, L.; Nielsen, L.; Vigreux, J.; Chatrenet, A.; D’Alessandro, C.; Cabiddu, G.; Cupisti, A. Intradialytic Nutrition and Hemodialysis Prescriptions: A Personalized Stepwise Approach. Nutrients 2020, 12, 785. [Google Scholar] [CrossRef] [Green Version]
- Kuipers, J.; Verboom, L.M.; Ipema, K.J.R.; Paans, W.; Krijnen, W.P.; Gaillard, C.A.J.M.; Westerhuis, R.; Franssen, C.F.M. The Prevalence of Intradialytic Hypotension in Patients on Conventional Hemodialysis: A Systematic Review with Meta-Analysis. Am. J. Nephrol. 2019, 49, 497–506. [Google Scholar] [CrossRef]
- Agarwal, R. How can we prevent intradialytic hypotension? Curr. Opin. Nephrol. Hypertens. 2012, 21, 593–599. [Google Scholar] [CrossRef]
- Chang, T.I.; Paik, J.; Greene, T.; Desai, M.; Bech, F.; Cheung, A.K.; Chertow, G.M. Intradialytic hypotension and vascular access thrombosis. J. Am. Soc. Nephrol. 2011, 22, 1526–1533. [Google Scholar] [CrossRef] [Green Version]
- Shoji, T.; Tsubakihara, Y.; Fujii, M.; Imai, E. Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int. 2004, 66, 1212–1220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stefansson, B.V.; Brunelli, S.M.; Cabrera, C.; Rosenbaum, D.; Anum, E.; Ramakrishnan, K.; Jensen, D.E.; Stålhammar, N.-O. Intradialytic hypotension and risk of cardiovascular disease. Clin. J. Am. Soc. Nephrol. 2014, 9, 2124–2132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strong, J.; Burgett, M.; Buss, M.L.; Carver, M.; Kwankin, S.; Walker, D. Effects of calorie and fluid intake on adverse events during hemodialysis. J. Ren. Nutr. 2001, 11, 97–100. [Google Scholar] [CrossRef]
- Benaroia, M.; Iliescu, E.A. Oral intake during hemodialysis: Is there an association with intradialytic hypotension? Hemodial. Int. 2008, 12, 62–65. [Google Scholar] [CrossRef]
- Shibagaki, Y.; Takaichi, K. Significant reduction of the large-vessel blood volume by food intake during hemodialysis. Clin. Nephrol. 1998, 49, 49–54. [Google Scholar]
- Sivalingam, M.; Banerjee, A.; Nevett, G.; Farrington, K. Haemodynamic effects of food intake during haemodialysis. Blood Purif. 2008, 26, 157–162. [Google Scholar] [CrossRef]
- Borzou, S.R.; Mahdipour, F.; Oshvandi, K.; Salavati, M.; Alimohammadi, N. Effect of Mealtime during Hemodialysis on Patients’ Complications. J. Caring Sci. 2016, 5, 277–286. [Google Scholar] [CrossRef]
- Colson, A.; Brinkley, A.; Braconnier, P.; Ammor, N.; Burnier, M.; Pruijm, M. Impact of salt reduction in meals consumed during hemodialysis sessions on interdialytic weight gain and hemodynamic stability. Hemodial. Int. 2018, 22, 501–506. [Google Scholar] [CrossRef]
- Svinth-Johansen, C.; Reinhard, M.; Ivarsen, P. Hemodynamic Response to Glucose-Insulin Infusion and Meals during Hemodialysis. Kidney Blood Press. Res. 2020, 45, 249–262. [Google Scholar] [CrossRef]
- Georgianos, P.I.; Agarwal, R. Epidemiology, diagnosis and management of hypertension among patients on chronic dialysis. Nat. Rev. Nephrol. 2016, 12, 636–647. [Google Scholar] [CrossRef]
- Kara, B.; Acikel, C.H. The effect of intradialytic food intake on the urea reduction ratio and single-pool Kt/V values in patients followed-up at a hemodialysis center. Turk. J. Med. Sci. 2010, 40, 91–97. [Google Scholar]
- Muller-Deile, J.; Lichtinghagen, R.; Haller, H.; Schmitt, R. Online Kt/V monitoring in haemodialysis by UV absorbance: Variations during intra-dialytic meals. Blood Purif. 2014, 37, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Marcelli, D.; Usvyat, L.A.; Kotanko, P.; Bayh, I.; Canaud, B.; Etter, M.; Gatti, E.; Grassmann, A.; Wang, Y.; Marelli, C.; et al. Body composition and survival in dialysis patients: Results from an international cohort study. Clin. J. Am. Soc. Nephrol. 2015, 10, 1192–1200. [Google Scholar] [CrossRef] [PubMed]
- Burrowes, J.D.; Larive, B.; Cockram, D.B.; Dwyer, J.; Kusek, J.W.; McLeroy, S.; Poole, D.; Rocco, M.V.; Hemodialysis (HEMO) Study Group. Effects of dietary intake, appetite, and eating habits on dialysis and non-dialysis treatment days in hemodialysis patients: Cross-sectional results from the HEMO study. J. Ren. Nutr. 2003, 13, 191–198. [Google Scholar] [CrossRef]
- Kazempour-Ardebili, S.; Lecamwasam, V.L.; Dassanyake, T.; Frankel, A.H.; Tam, F.W.; Dornhorst, A.; Frost, G.; Turner, J.J.O. Assessing glycemic control in maintenance hemodialysis patients with type 2 diabetes. Diabetes Care 2009, 32, 1137–1142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riveline, J.P.; Teynie, J.; Belmouaz, S.; Franc, S.; Dardari, D.; Bauwens, M.; Caudwell, V.; Ragot, S.; Bridoux, F.; Charpentier, G.; et al. Glycaemic control in type 2 diabetic patients on chronic haemodialysis: Use of a continuous glucose monitoring system. Nephrol. Dial. Transplant. 2009, 24, 2866–2871. [Google Scholar] [CrossRef]
- Abe, M.; Kalantar-Zadeh, K. Haemodialysis-induced hypoglycaemia and glycaemic disarrays. Nat. Rev. Nephrol. 2015, 11, 302–313. [Google Scholar] [CrossRef]
- Sun, Y.; Roumelioti, M.E.; Ganta, K.; Glew, R.H.; Gibb, J.; Vigil, D.; Do, C.; Servilla, K.S.; Wagner, B.; Owen, J.; et al. Dialysis-associated hyperglycemia: Manifestations and treatment. Int. Urol. Nephrol. 2020, 52, 505–517. [Google Scholar] [CrossRef]
- Rhee, C.M.; You, A.S.; Koontz, P.T.; Tortorici, A.R.; Bross, R.; St-Jules, D.E.; Jing, J.; Lee, M.L.; Benner, D.; Kovesdy, C.P.; et al. Effect of high-protein meals during hemodialysis combined with lanthanum carbonate in hypoalbuminemic dialysis patients: Findings from the FrEDI randomized controlled trial. Nephrol. Dial. Transplant. 2017, 32, 1233–1243. [Google Scholar] [CrossRef]
- Gama-Axelsson, T.; Heimburger, O.; Stenvinkel, P.; Barany, P.; Lindholm, B.; Qureshi, A.R. Serum albumin as predictor of nutritional status in patients with ESRD. Clin. J. Am. Soc. Nephrol. 2012, 7, 1446–1453. [Google Scholar] [CrossRef]
- Liu, P.J.; Ma, F.; Wang, Q.Y.; He, S.L. The effects of oral nutritional supplements in patients with maintenance dialysis therapy: A systematic review and meta-analysis of randomized clinical trials. PLoS ONE 2018, 13, e0203706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sohrabi, Z.; Eftekhari, M.H.; Eskandari, M.H.; Rezaianzadeh, A.; Sagheb, M.M. Intradialytic Oral Protein Supplementation and Nutritional and Inflammation Outcomes in Hemodialysis: A Randomized Controlled Trial. Am. J. Kidney Dis. 2016, 68, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Weiner, D.E.; Tighiouart, H.; Ladik, V.; Meyer, K.B.; Zager, P.G.; Johnson, D.S. Oral intradialytic nutritional supplement use and mortality in hemodialysis patients. Am. J. Kidney Dis. 2014, 63, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Korzets, A.; Azoulay, O.; Ori, Y.; Zevin, D.; Boaz, M.; Herman, M.; Chagnac, A.; Gafter, U. The use of intradialytic parenteral nutrition in acutely ill haemodialysed patients. J. Ren. Care 2008, 34, 14–18. [Google Scholar] [CrossRef]
- Dukkipati, R.; Kalantar-Zadeh, K.; Kopple, J.D. Is there a role for intradialytic parenteral nutrition? A review of the evidence. Am. J. Kidney Dis. 2010, 55, 352–364. [Google Scholar] [CrossRef] [Green Version]
| Study ID | Year | Patients | Intervention | Main Findings |
|---|---|---|---|---|
| Sherman et al. [10] | 1988 | 9 non-diabetic dialysis patients without autonomic neuropathy or orthostatic hypotension | Dialysis with vs. without oral food intake (62 vs. 63 sessions, respectively) | Postprandial drop in BP. Higher incidence of IDH with oral food intake. |
| Zoccali et al. [11] | 1989 | 13 stable dialysis patients | Dialysis with vs. without oral intake of a standard snack | Postprandial drop in BP. Higher incidence of IDH with oral food intake. |
| Barakat et al. [9] | 1993 | 10 stable dialysis patients | Placebo pre-dialysis and no intradialytic meal vs. placebo pre-dialysis and intradialytic mean vs. caffeine 200 mg pre-dialysis and intradialytic mean | Postprandial drop is SVRI and in BP. Administration of caffeine before dialysis did not prevent postprandial IDH. |
| Shibagaki et al. [25] | 1998 | 21 dialysis patients without evidence of orthostatic hypotension | Administration of standard meal 1 h after initiation of dialysis | Postprandial reduction in blood volume of large vessels assessed with RBV monitoring. Postprandial hypotension. |
| Sivalingam et al. [26] | 2008 | 20 stable, non-diabetic dialysis patients | Administration of standard meal 45 min after initiation of dialysis | Postprandial reduction in blood volume of large vessels assessed with RBV monitoring. Postprandial drop in mean BP. |
| Borzou et al. [27] | 2016 | 48 stable dialysis patients | Oral food intake 1 or 2 h after initiation of dialysis vs. no intradialytic meal | Postprandial drop in BP regardless of the timing of oral food intake. No difference in the incidence of nausea or vomiting. |
| Colson et al. [28] | 2018 | 40 stable dialysis patients | Intradialytic intake of a snack with high (2.4 g/session) vs. low (1.4 g/session) sodium content | Low dietary sodium intake during dialysis was associated with lower IDWG and fewer episodes of symptomatic IDH. |
| Svinth-Johansen et al. [29] | 2020 | 12 non-diabetic dialysis patients | Administration of a standard meal during a non-dialysis day vs. intradialytic intake of a standard meal. | Intradialytic reduction in BP and in AIx(75). No postprandial hemodynamic effect during the non-dialysis day. |
| Study ID | Year | Patients | Intervention | Main Findings |
|---|---|---|---|---|
| San Juan Miguelsanz et al. [13] | 2001 | 14 stable dialysis patients | Midweek dialysis with vs. without oral food intake | Lower URR and Kt/V with intradialytic food intake. No difference in intradialytic symptoms. |
| Singri et al. [14] | 2004 | 42 stable dialysis patients | Oral food intake 2 h before dialysis vs. 3-hour fasting before dialysis | No difference in URR and Kt/V. |
| Kara et al. [31] | 2010 | 25 dialysis patients without diabetic autonomic neuropathy | Midweek dialysis with vs. without oral food intake. | Lower URR and Kt/V with intradialytic food intake. |
| Müller-Deile et al. [32] | 2014 | 40 stable dialysis without symptomatic CV disease | Administration of a standard meal 2 h after the initiation of dialysis | Postprandial drop in online Kt/V assessed with UV absorbance. No change in online Kt/V with ionic dialysance method. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fotiadou, E.; Georgianos, P.I.; Chourdakis, M.; Zebekakis, P.E.; Liakopoulos, V. Eating during the Hemodialysis Session: A Practice Improving Nutritional Status or a Risk Factor for Intradialytic Hypotension and Reduced Dialysis Adequacy? Nutrients 2020, 12, 1703. https://doi.org/10.3390/nu12061703
Fotiadou E, Georgianos PI, Chourdakis M, Zebekakis PE, Liakopoulos V. Eating during the Hemodialysis Session: A Practice Improving Nutritional Status or a Risk Factor for Intradialytic Hypotension and Reduced Dialysis Adequacy? Nutrients. 2020; 12(6):1703. https://doi.org/10.3390/nu12061703
Chicago/Turabian StyleFotiadou, Eleni, Panagiotis I. Georgianos, Michail Chourdakis, Pantelis E. Zebekakis, and Vassilios Liakopoulos. 2020. "Eating during the Hemodialysis Session: A Practice Improving Nutritional Status or a Risk Factor for Intradialytic Hypotension and Reduced Dialysis Adequacy?" Nutrients 12, no. 6: 1703. https://doi.org/10.3390/nu12061703
APA StyleFotiadou, E., Georgianos, P. I., Chourdakis, M., Zebekakis, P. E., & Liakopoulos, V. (2020). Eating during the Hemodialysis Session: A Practice Improving Nutritional Status or a Risk Factor for Intradialytic Hypotension and Reduced Dialysis Adequacy? Nutrients, 12(6), 1703. https://doi.org/10.3390/nu12061703