Geospatial Analysis of Food Deserts and Their Impact on Health Outcomes in Children with Cystic Fibrosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Study Design
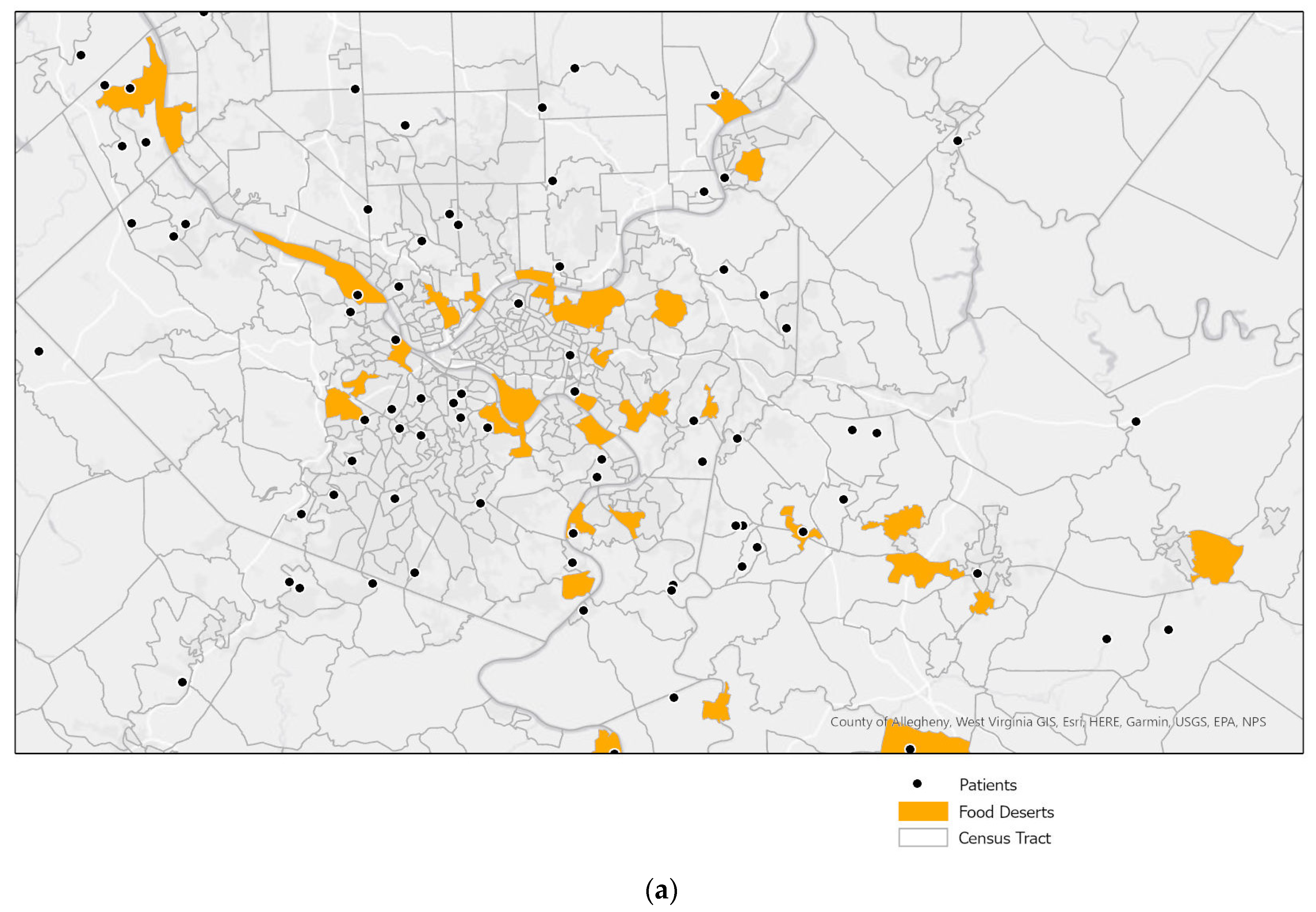
2.2. Area Resources
2.3. Outcome Variables
2.4. Statistical Analysis
3. Results
3.1. Model 1: The Individual Impact of Food Deserts and Surrounding Regions on CF Health Outcomes
3.2. Model 2: The Individual Impact of Childhood Opportunity (COI Scores) on CF Health Outcomes
3.3. Model 3: The Impact of Food Deserts and Surrounding Regions on CF Health Outcomes, Adjusting for COI Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- USDA Economic Research Service Definitions of Food Insecurity. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx (accessed on 1 April 2021).
- Guide to Measuring Household Food Security, Revised 2000. Available online: https://naldc.nal.usda.gov/download/38369/PDF (accessed on 1 April 2021).
- Centers for Disease Control and Prevention Geographic Information Systems. Available online: www.cdc.gov/gis/index.html (accessed on 1 April 2021).
- USDA Economic Research Service Mapping Food Deserts in the United States. Available online: https://www.ers.usda.gov/amber-waves/2011/december/data-feature-mapping-food-deserts-in-the-us/ (accessed on 1 April 2021).
- Addressing Food Insecurity in CF Care. Available online: https://www.cff.org/Care/Clinician-Resources/Network-News/January-2019/Addressing-Food-Insecurity-in-CF-Care/ (accessed on 1 May 2021).
- Yen, E.; Quniton, B.; Borowitz, D. Better Nutritional Status in Early Childhood is Associated with Improved Clinical Outcomes and Survival in Patients with Cystic Fibrosis. J. Pediatrics 2013, 162, 530–535. [Google Scholar] [CrossRef]
- Konstan, M.W.; Butler, S.M.; Wohl, M.E.; Stoddard, M.; Matousek, R.; Wagener, J.S.; Johnson, C.A.; Morgan, W.J. Growth and nutritional indexes in early life predict pulmonary function in cystic fibrosis. J. Pediatrics 2003, 142, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.S.; Durham, D.; Tivis, R.D.; Stamper, S.; Waldren, C.; Toevs, S.E.; Gordon, B.; Robb, T.A. Evaluation of Food Insecurity in Adults and Children with Cystic Fibrosis: Community Case Study. Front. Public Health 2018, 6, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borowitz, D.; Baker, R.D.; Stallings, V. Consensus Report on Nutrition for Pediatric Patients with Cystic Fibrosis. J. Ped Gastroenterol. Nutr. 2002, 35, 246–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Academy of Pediatrics and the Food Research & Action Center Screen and Intervenie: A Toolkit for Pediatricians to Address Food Insecurity. Available online: https://frac.org/wp-content/uploads/FRAC_AAP_Toolkit_2021.pdf (accessed on 1 May 2021).
- Banerjee, S.; Radak, T.; Khubchandani, J.; Dunn, P. Food Insecurity and Mortality in American Adults: Results From the NHANES-Linked Mortality Study. Health Promot. Pract. 2021, 22, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Clemm, C. Force Field Analysis of Food Insecurity Screening and Treatment in 15 CF Care Centers. In Proceedings of the 33rd Annual North American Cystic Fibrosis Conference, Nashville, TN, USA, 31 October–2 November 2019. Abstract Number 836. [Google Scholar]
- USDA Economic Research Service Food Access Research Atlas. Available online: https://www.ers.usda.gov/data-products/food-access-research-atlas/ (accessed on 1 March 2021).
- Noelke, C.; McArdle, N.; Baek, M.; Huntington, N.; Huber, R.; Hardy, E.; Acevedo-Garcia, D. Child Opportunity Index 2.0 Technical Documentation. Available online: http://new.diversitydatakids.org/sites/default/files/2020-01/ddk_coi2.0_technical_documentation_20200115_1.pdf (accessed on 1 April 2021).
- Stallings, V.A.; Stark, L.J.; Robinson, K.; Feranchak, A.; Quinton, H. Evidence based practive recommendations for nutrition-related management of children and adults with cystic fibrosis and pancreatic insufficiency: Results of a systematic review. J. Am. Diet. Assoc. 2008, 108, 832–839. [Google Scholar] [CrossRef]
- Flume, P.A.; O’Sullivan, B.P.; Robinson, K.A.; Goss, C.H.; Mogayzel, P.J.; Willey-Courand, D.B.; Bujan, J.; Finder, J.; Lester, M.; Quittell, L.; et al. Cystic Fibrosis Pulmonary Guidelines: Chronic Medications for Maintenance of Lung Health. Am. J. Respir. Crit. Care Med. 2007, 176, 957–969. [Google Scholar] [CrossRef]
- Cystic Fibrosis Foundation Patient Registry 2019 Annual Data Report. Available online: https://www.cff.org/Research/Researcher-Resources/Patient-Registry/2019-Patient-Registry-Annual-Data-Report.pdf (accessed on 1 August 2021).
- Beaulac, J.; Kristjansson, E.; Cummins, S. A Systematic Review of Food Deserts, 1966–2007. Prev. Chronic Dis. 2009, 6, 1–10. [Google Scholar]
- Stronks, K.; Van De Mheen, D.; Looman, C.W.N.; Mackenbach, J. Behavioural and structural factors in the explanation of socio-economic inequalities in health: An empirical analysis. Sociol. Health Illn. 1996, 18, 653–674. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention Social Determinants of Health: Know What Affects Health. Available online: https://www.cdc.gov/socialdeterminants/index.htm (accessed on 1 July 2021).
- Berkowitz, S.A.; Basu, S.; Venkataramani, A.; Reznor, G.; Fleegler, E.W.; Atlas, S.J. Association between access to social service resources and cardiometabolic risk factors: A machine learning and multilevel modeling analysis. BMJ 2019, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Cook, J.T.; Frank, D.A.; Berkowitz, C.; Black, M.M.; Casey, P.H.; Cutts, D.B.; Meyers, A.F.; Zaldivar, N.; Skalicky, A.; Levenson, S.; et al. Food Insecurity Is Associated with Adverse Health Outcomes among Human Infants and Toddlers. J. Nutr. 2004, 134, 1432–1438. [Google Scholar] [CrossRef]
- Diez Roux, A.V. Investigating Neighborhood and Area Effects on Health. Am. J. Public Health 2001, 91, 1783–1789. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.E.; Keane, C.R.; Burke, J.G. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place 2010, 16, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Food Insecurity and Chronic Disease. Available online: https://www.ifm.org/news-insights/food-insecurity-chronic-disease/ (accessed on 1 August 2021).
- Kelli, H.M.; Hammadah, M.; Ahmed, H.; Ko, Y.A.; Topel, M.; Samman-Tahhan, A.; Awad, M.; Patel, K.; Mohammed, K.; Sperling, L.S.; et al. Association Between Living in Food Deserts and Cardiovascular Risk. Circ. Cardiovas. Qual. Outcomes 2017, 10, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Sturm, R.; Datar, A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health 2005, 119, 1059–1068. [Google Scholar] [CrossRef]
- Larson, N.I.; Story, M.T.; Nelson, M.C. Neighborhood environments: Disparities in access to healthy foods in the U.S. Am. J. Prev. Med. 2009, 36, 74–81. [Google Scholar] [CrossRef]
- Leung, C.W.; Laraia, B.A.; Kelly, M.; Nickleach, D.; Adler, N.E.; Kushi, L.H.; Yen, I.H. The influence of neighborhood food stores on change in young girls’ body mass index. Am. J. Prev. Med. 2011, 41, 43–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merchant, A.T.; Dehghan, M.; Behnke-Cook, D.; Anand, S.S. Diet, physical activity, and adiposity in children in poor and rich neighbourhoods: A cross-sectional comparison. Nutr. J. 2007, 6, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oates, G.; Rutland, S.; Juarez, L.; Friedman, A.; Schechter, M.S. The association of area deprivation and state child health with respiratory outcomes of pediatric patients with cystic fibrosis in the United States. Pediatric Pulmonol. 2021, 56, 883–890. [Google Scholar] [CrossRef]
- Schechter, M.S.; Shelton, B.J.; Margolis, P.A.; Fitzsimmons, S.C. The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am. J. Respir. Crit. Care Med. 2001, 163, 1331–1337. [Google Scholar] [CrossRef]
- Bauer, S.R.; Monuteaux, M.C.; Fleegler, E.W. Geographic Disparities in Access to Agencies Providing Income-Related Social Services. J. Urban Health 2015, 92, 853–863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berkowitz, S.A.; Karter, A.J.; Corbie-Smith, G.; Seligman, H.K.; Ackroyd, S.A.; Barnard, L.S.; Atlas, S.J.; Wexler, D.J. Food Insecurity, Food "Deserts," and Glycemic Control in Patients with Diabetes: A Longitudinal Analysis. Diabetes Care 2018, 41, 1188–1195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durfey, S.; Kind, A.; Gutman, R.; Monteiro, K.; Buckingham, W.R.; DuGoff, E.H.; Trivedi, A.N. Impact of Risk Adjustment For Socioeconomic Status On Medicare Advantage Plan Quality Rankings. Health Aff. 2018, 37, 1065–1072. [Google Scholar] [CrossRef] [PubMed]
- Incentivizing the Sale of Healthy and Local Food. Available online: http://growingfoodconnections.org/wp-content/uploads/sites/3/2015/11/GFCHealthyFoodIncentivesPlanningPolicyBrief_2016Feb-1.pdf (accessed on 15 September 2021).
- CED Healthy Food Financing Initiative FY 2016. Available online: https://www.acf.hhs.gov/archive/ocs/programs/community-economic-development/healthy-food-financing (accessed on 23 September 2021).
- Gary-Webb, T.L.; Bear, T.M.; Mendez, D.D.; Schiff, M.D.; Keenan, E.; Fabio, A. Evaluation of a Mobile Farmer’s Market Aimed at Increasing Fruit and Vegetable Consumption in Food Deserts: A Pilot Study to Determine Evaluation Feasibility. Health Equity 2018, 2, 375–383. [Google Scholar] [CrossRef]
- Mendez, D.D.; Fabio, A.; Robinson, T.; Bear, T.; Keenan, E.; Schiff, M.D.; Gary-Webb, T. Green Grocer: Using Spatial Analysis to Identify Locations for a Mobile Food Market. Prog. Community Health Partnersh. 2020, 14, 109–115. [Google Scholar] [CrossRef] [Green Version]
- The Role of the Federal Child Nutrition Programs in Improving Health and Well-Being. Available online: https://frac.org/wp-content/uploads/hunger-health-role-federal-child-nutrition-programs-improving-health-well-being.pdf (accessed on 2 November 2021).
- Understanding Food Insecurity in the City of Pittsburgh. Available online: https://apps.pittsburghpa.gov/redtail/images/11738_FeedPGH_2020.10.16.pdf (accessed on 2 November 2021).
- Baltimore Ride Share Project to Support Health Food Priority Areas. Available online: https://phnci.org/uploads/resource-files/PHNCI-Case-Study-Baltimore.pdf (accessed on 3 November 2021).
- USDA Economic Research Service Food Insecurity, Chronic Disease, and Health among Working-Age Adults. Available online: https://www.ers.usda.gov/webdocs/publications/84467/err-235.pdf?v=7518.3 (accessed on 15 June 2021).

| Characteristics | Overall | Food Desert | Food Desert + 600 ft Buffer | Food Desert + 1200 ft Buffer |
|---|---|---|---|---|
| Total | 206 | 17 | 20 | 29 |
| Demographics | ||||
| Age (range 0–18 years) | 9.5 * (5.6) | 8.7 * (5.5) | 9.5 * (5.5) | 9.8 * (4.9) |
| Female, % | 47% | 47% | 45% | 52% |
| White, % | 92.7% | 94% | 95% | 93% |
| Modulator Use, % | 11.6% | 18% | 20% | 14% |
| Clinical Outcomes | ||||
| BMI/weight-for-length, percentile | 63 * (24.4) | 56.6 * (29.7) | 53.5 * (28.5) | 56.8 * (28.0) |
| ppFEV1 (>6 years old) | 95.9 * (17.1) n = 141 | 92.5 * (17.2) n = 11 | 87.2 * (18.8) n = 14 | 90 * (16.9) n = 22 |
| Pulmonary Exacerbations | 0.5 * (1.2) Range: 0–8 | 0.7 * (2.2) Range: 0–6 | 0.8 * (1.4) Range: 0–6 | 0.6 * (1.2) Range: 0–6 |
| Health Outcome | COI | Food Desert | Food Desert + | Food Desert + |
|---|---|---|---|---|
| 600 ft Buffer | 1200 ft Buffer | |||
| BMI | ||||
| Model 1 a | 1.07 (0.59, 1.94) p-value 0.832 | 2.9 (1.1, 8.21) * | 4.06 (1.54, 10.69) * | 2.65 (1.16, 6.07) * |
| OR (95% CI) | p-value 0.039 | p-value 0.005 | p-value 0.021 | |
| Model 2 b | ||||
| OR (95% CI) | ||||
| Model 3 c | 3.18 (1.01, 9.40) * | 4.41 (1.60, 12.14) * | 2.83 (1.18, 6.76) * | |
| OR (95% CI) | p-value 0.036 | p-value 0.004 | p-value 0.020 | |
| ppFEV1 (6 years and older) | ||||
| Model 1 a | 0.99 (0.49, 2.02) p-value 0.984 | 1.79 (0.51, 6.32) | 3.09 (0.99, 9.66) * | 1.90 (0.74, 4.92) |
| OR (95% CI) | p-value 0.363 | p-value 0.050 | p-value 0.184 | |
| Model 2 b | ||||
| OR (95% CI) | ||||
| Model 3 c | 1.90 (0.51, 7.14) | 3.33 (1.03, 10.84) * | 2.02 (0.75, 5.46) | |
| OR (95% CI) | p-value 0.340 | p-value 0.045 | p-value 0.166 | |
| Hospitalizations for Pulmonary Exacerbations | ||||
| Model 1 a | 1.01 (0.41, 2.53) p-value 0.976 | 2.22 (0.53, 9.25) | 2.49 (0.69, 8.95) | 1.19 (0.35, 4.05) |
| OR (95% CI) | p-value 0.273 | p-value 0.163 | p-value 0.778 | |
| Model 2 b | ||||
| OR (95% CI) | ||||
| Model 3 c | 2.42 (0.52, 11.15) | 2.63 (0.69, 10.01) | 1.20 (0.34, 4.31) | |
| OR (95% CI) | p-value 0.258 | p-value 0.156 | p-value 0.777 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corbera-Hincapie, M.A.; Kurland, K.S.; Hincapie, M.R.; Fabio, A.; Weiner, D.J.; Kim, S.C.; Kazmerski, T.M. Geospatial Analysis of Food Deserts and Their Impact on Health Outcomes in Children with Cystic Fibrosis. Nutrients 2021, 13, 3996. https://doi.org/10.3390/nu13113996
Corbera-Hincapie MA, Kurland KS, Hincapie MR, Fabio A, Weiner DJ, Kim SC, Kazmerski TM. Geospatial Analysis of Food Deserts and Their Impact on Health Outcomes in Children with Cystic Fibrosis. Nutrients. 2021; 13(11):3996. https://doi.org/10.3390/nu13113996
Chicago/Turabian StyleCorbera-Hincapie, Montserrat A., Kristen S. Kurland, Mark R. Hincapie, Anthony Fabio, Daniel J. Weiner, Sandra C. Kim, and Traci M. Kazmerski. 2021. "Geospatial Analysis of Food Deserts and Their Impact on Health Outcomes in Children with Cystic Fibrosis" Nutrients 13, no. 11: 3996. https://doi.org/10.3390/nu13113996
APA StyleCorbera-Hincapie, M. A., Kurland, K. S., Hincapie, M. R., Fabio, A., Weiner, D. J., Kim, S. C., & Kazmerski, T. M. (2021). Geospatial Analysis of Food Deserts and Their Impact on Health Outcomes in Children with Cystic Fibrosis. Nutrients, 13(11), 3996. https://doi.org/10.3390/nu13113996





