Abstract
This web-based cross-sectional survey aimed to elucidate the differences between the two core symptoms of night eating syndrome (NES): evening hyperphagia and nocturnal ingestion in the general Japanese population aged 16–79 years. Participants who consumed at least 25% of daily calories after dinner were defined as having evening hyperphagia. Those who consumed food after sleep initiation at least twice a week were determined to have nocturnal ingestion. Of the 8348 participants, 119 (1.5%) were categorized in the evening hyperphagia group, 208 (2.6%) in the nocturnal ingestion group, and 8024 in the non-NES group. Participants with evening hyperphagia and nocturnal ingestion had significantly higher anxiety scores (p < 0.05 and p < 0.001, respectively) and depression (p < 0.001 for both) than those without NES. Multiple logistic regression analysis revealed that evening hyperphagia was significantly and independently associated with higher body mass index, shorter sleep duration, later sleep-wake schedule, and higher insomnia score, while nocturnal ingestion was significantly and independently associated with younger age, smoking habit, living alone, earlier sleep-wake schedule, and higher insomnia score. Sleep duration and sleep-wake schedule characteristics in the two groups were opposite, suggesting differences in the sleep pathophysiology mechanisms.
Keywords:
night eating syndrome; nocturnal eating; depression; anxiety; insomnia; distress; eating disorder 1. Introduction
Night eating syndrome (NES) is characterized by excessive eating just before going to bed or after waking up at night, which can result in difficulty in controlling body weight [1,2]. NES was first described by Stunkard et al. [3] in 1955 as a disease with features of morning anorexia, evening hyperphagia, and insomnia. Subsequently, nocturnal ingestion (i.e., waking during the sleep period to eat) was recognized as a symptom of NES as well [4,5]. NES has been reported to be associated with depression, distress, and sleep disorders [1,2], and it is listed as one of the “other specified feeding or eating disorders” in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition [6]. In the proposed diagnostic criteria of NES by Allison et al. [7], which was developed based on a review of previous literature, evening hyperphagia was defined as “At least 25% of the food intake is consumed after the evening meal” and nocturnal ingestion as “At least two episodes of nocturnal eating per week”.
Nocturnal ingestion shares a common pathophysiology with sleep-related eating disorder (SRED) [8,9], which is a parasomnia characterized by nocturnal eating behavior associated with total amnesia or partial unawareness of eating or drinking episodes [10,11,12,13]. Recently, we conducted a large epidemiological study in a young population using the Munich Parasomnia Screening questionnaire, a screening tool for parasomnias [14,15]. The study indicated an association between the possibility of NES and factors including female sex, smoking, use of hypnotic medications, history of sleepwalking, delayed sleep-wake schedules, and poor sleep quality [16]. However, this study had a few limitations. First, it was limited to a population of young adults. Second, even more importantly, the study only identified individuals with nocturnal ingestion and not those with evening hyperphagia [16].
A recent video polysomnography study showed that participants with nocturnal ingestion were younger and less obese than those with evening hyperphagia [17]. Additionally, in terms of eating and subsequent falling asleep behaviors, the participants in the evening hyperphagia group had significantly longer eating episodes and sleep resumption times after eating offset than those in the nocturnal ingestion group [17]. However, no studies have examined the differences in the psychological burden and lifestyle-related factors, including sleep variables, between evening hyperphagia and nocturnal ingestion. Therefore, in this study, we investigated the factors associated with evening hyperphagia and nocturnal ingestion in a large, stratified population, which covered a wide age range. Further, we compared the anxiety and depression scores between individuals with evening hyperphagia and those with nocturnal ingestion. Finally, we discuss the similarities and differences between the pathophysiology of evening hyperphagia and nocturnal ingestion with respect to sleep-wake schedules and social jet lag, after adjusting for the severity of insomnia symptoms.
2. Materials and Methods
2.1. Study Population and Outcomes
The present study was conducted as part of a comprehensive research project that investigated the sleep problems and daytime functioning in the general population [18]. This web-based cross-sectional questionnaire survey was conducted in April 2016. The participants were previously registered as research panel members of an established internet survey company and resided in all areas of Japan, stratified by age, sex, and region of residence. The study protocol was approved by the ethics committee of the Neuropsychiatric Research Institute, Tokyo, Japan. Informed consent was obtained from all participants via the survey website.
A total of 10,000 participants responded to the questionnaire. Participants were excluded based on the following criteria: out of the age range of 16–79 years (n = 3), average sleep duration out of the mean ± 2 standard deviation (SD) range (402 ± 197 min, n = 265), sleep midpoint out of the mean ± 2 SD range (3:37 AM ± 3:39, n = 240), and shift workers (n = 1144). Finally, 8348 participants (83.5%) were included in the analyses.
The following participant demographic information was obtained using the questionnaire: age, sex, body mass index (BMI), smoking status (“Do you currently smoke?”) and habitual alcohol intake (“Do you drink alcohol habitually?”), regular employment or school attendance (“Do you work or go to school regularly?”), frequency of working or going to school per week (“If yes, how many days a week do you work or go to school?”), family constitution (“Do you currently live alone or with your family?”), habitual exercise (“Do you exercise regularly: at least 30 min a day, 2 days a week, for 1 year?”) [19], and hypnotic medication use (“Do you currently take medicine to sleep?”). For evaluating the participants’ sleep habits, the following questions were included: weekday or days off bedtime (“What time do you usually go to bed on weekdays or days off?”), sleep onset latency (“How long does it usually take you to fall asleep on weekdays or days off?”), and wake-up time (“What time do you usually get up on weekdays or days off?”). The Japanese version of the Insomnia Severity Index (ISI) for assessing insomnia severity [20,21] and the Japanese version of the Hospital Anxiety and Depression Scale (HADS) for determining the severity of depression and anxiety [22,23,24] {Fulda, 2008 #117} were also included in the questionnaire.
The questionnaire also included four questions on the participants’ eating habits: frequency of eating dinner per week, time of last meal, frequency of nighttime food intake (“How many days per week do you eat anything between dinner and the next morning, such as a night snack or light meal?”), and percentage of nighttime food calories from the total daily calories (“Considering your total calories for the day as 100%, how many calories do you take after dinner up to the next morning?”). The questionnaire was used to identify the participants who met the two main items of the proposed diagnostic criteria of NES by Allison et al. [7]. Based on the A1 criterion (evening hyperphagia) of “At least 25% of the daily food is consumed after the evening meal,” participants who had dinner as well as snacked between dinner and the next morning and consumed at least 25% of their daily calories between dinner and bedtime every day were identified as having met the A1 criterion and defined as having evening hyperphagia. They included some participants who also met the A2 criterion [17]. According to the A2 criterion (nocturnal ingestion) of “At least two eating episodes per week occur upon awakening during the night,” participants whose last episodes of eating/drinking were later than their sleep onset time at least twice a week (both workdays and days off) were identified. The identified participants who only fulfilled the A2 criterion were defined as having nocturnal ingestion [17].
For the sleep variables, the sleep onset time was first calculated using bedtime and sleep onset latency. Next, the difference between sleep onset time and wake-up time was defined as sleep duration, while the midpoint between the sleep onset and wake-up times was defined as the sleep midpoint. Both parameters were assessed on weekdays and days off. The average sleep time was calculated using the following formula: ((sleep duration on weekdays × x + (sleep duration on days off × {7 − x}))/7, where x is the number of working days or school days in the week. Similarly, the average sleep midpoint was calculated using the following formula: ((sleep midpoint on weekdays × x) + (sleep midpoint on days off × {7 − x}))/7. Additionally, the absolute difference in sleep midpoint between weekdays and days off was calculated and defined as the absolute social jet lag [25].
2.2. Statistical Analysis
The Chi-square test (categorical variables) or Mann-Whitney’s U test and Dunn’s multiple comparison test (continuous variables) were performed for comparing the descriptive categories, including the demographic and sleep hygiene variables, ISI scores, and HADS anxiety and depression scores, among the three groups (i.e., non-NES, evening hyperphagia, and nocturnal ingestion groups). To investigate the factors associated with evening hyperphagia and nocturnal ingestion, logistic regression analysis was conducted for age (categorized; see below), sex, BMI (categorized; see below), current smoker (yes/no), habitual alcohol intake (yes/no), regular employment or school attendance (yes/no), living alone (yes/no), habitual exercise (yes/no), hypnotic medication use (yes/no), average sleep duration (categorized; see below), sleep-wake schedule (earlier/normal/later; earlier and later phases were defined by the first and third quartiles of the average sleep midpoint: earlier than 2:35 AM and later than 4:02 AM, respectively), absolute social jet lag (categorized; see below), and ISI score (categorized; see below). The aforementioned factors were categorized as follows: (1) age: 16–39, 40–59, and 60–79 years; (2) BMI: <25 and ≥25 kg/m2 [26]; (3) average sleep duration: <6 and ≥6 h (based on the cutoff for the first quartile: 357 min); (4) absolute social jet lag: <1, 1–2, and ≥2 h [18]; (5) ISI score: <8, 8–14, and 15–28 points [20,21]. Initially, all variables were examined using univariate models. The variables that showed significant correlation in the univariate analysis underwent multivariate logistic regression analysis for determining the main correlates while controlling for confounding factors. SPSS statistics version 22 (SPSS Japan, Inc., Tokyo, Japan) was used to conduct all analyses. Statistical significance was set at p < 0.05.
3. Results
Among the 8348 participants, 119 (1.5%) were categorized in the evening hyperphagia group (including four participants who met both the A1 and A2 criteria), 208 (2.6%) in the nocturnal ingestion group, and the remaining 8024 in the non-NES group. The median (range) for the continuous variables was as follows: age, 50 (16–79) years; BMI, 21.8 (12.0–49.1) kg/m2; average sleep duration, 400 (206–599) min; sleep midpoint, 3:17 (0:00–7:15) AM; absolute social jet lag, 0 (0–398) min; ISI score, 4 (0–28) points; HADS anxiety score, 4 (0–21) points, and HADS depression score, 8 (0–21) points. Descriptive information on the categorical variables of the participants is presented in Table 1.

Table 1.
Demographic, sleep schedules, and clinical data of the participants (n = 8348).
Descriptive and Clinical Variables
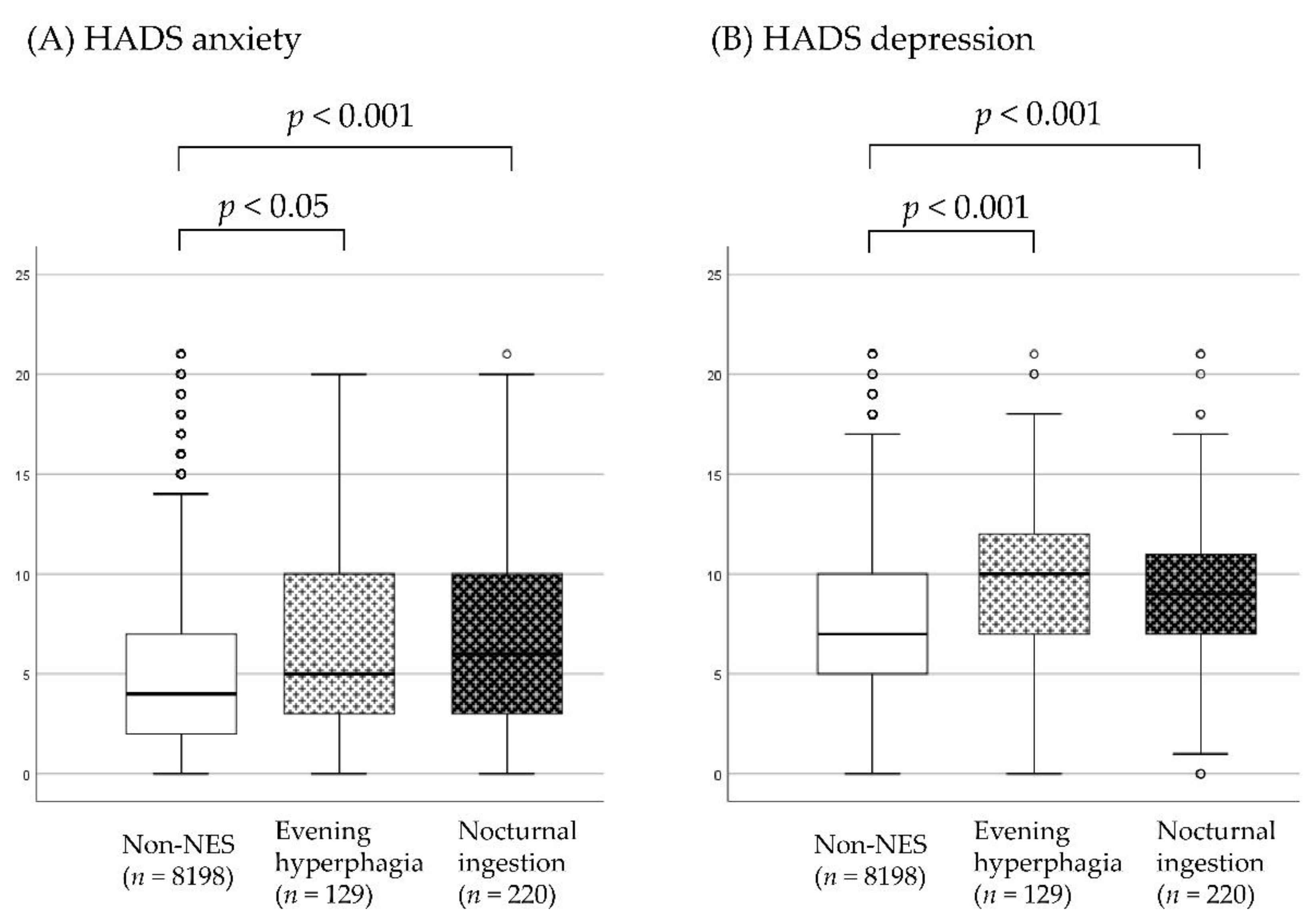
The median (interquartile range (IQR)) scores of HADS anxiety for the non-NES, evening hyperphagia, and nocturnal ingestion groups were 4 (2–7), 5 (3–10), and 6 (3–10), respectively. The HADS anxiety score was significantly different among the three groups, H (2) = 38.39, p < 0.001, η2 = 0.0046. Pairwise comparisons showed higher anxiety levels in the evening hyperphagia (p < 0.05, Cohen’s d = 0.30) and nocturnal ingestion groups than in the non-NES group (p < 0.001, Cohen’s d = 0.43). The anxiety levels were not significantly different between the participants with evening hyperphagia and those with nocturnal ingestion (p = 0.374, Cohen’s d = 0.11). The median (IQR) scores of HADS depression for the non-NES, evening hyperphagia, and nocturnal ingestion groups were 7 (5–10), 10 (7–12), and 9 (7–11), respectively. Participants with evening hyperphagia and nocturnal ingestion had significantly higher depression scores than the non-NES participants (p < 0.001 for both). The HADS depression score was significantly different among the three groups, H (2) = 63.25, p < 0.001, η2 = 0.0076. Pairwise comparisons showed higher depression levels in the evening hyperphagia (p < 0.001, Cohen’s d = 0.53) and nocturnal ingestion groups than in the non-NES group (p < 0.001, Cohen’s d = 0.38). The depression levels were not significantly different between the participants with evening hyperphagia and those with nocturnal ingestion (p = 0.739, Cohen’s d = 0.15) (Figure 1).
Figure 1.
Box-and-whisker plot showing the Hospital Anxiety and Depression Scale (HADS) scores of the non-night eating syndrome (non-NES), evening hyperphagia, and nocturnal ingestion groups. HADs anxiety and depression scores are shown in (A,B), respectively. Comparisons were made using the Mann-Whitney U test.
In the evening hyperphagia group, seven items were significantly associated in the univariate logistic regression analysis: age category of 60–79 years (odds ratio (OR) = 0.541, 95% confidence interval (CI): 0.330–0.887, p < 0.05), BMI of ≥ 25 kg/m2 (OR = 1.639, 95% CI: 1.089–2.468, p < 0.05), living alone (OR = 1.730, 95% CI: 1.134–2.640, p < 0.05), average sleep duration of < 6 h (OR = 2.345, 95% CI: 1.628–3.378, p < 0.001), later sleep-wake schedule (OR = 2.723, 95% CI: 1.834–44.044, p < 0.001), ISI score of 8–14 points (OR = 1.613, 95% CI: 1.066–2.441, p < 0.05), and ISI score of 15–28 points (OR = 3.538, 95% CI: 2.104–5.949, p < 0.001). Furthermore, in the multiple logistic regression analysis, significant associations were found for the following four items: BMI of ≥ 25 kg/m2 (OR = 1.525, 95% CI: 1.005–2.313, p < 0.05), average sleep duration of < 6 h (OR = 1.687, 95% CI: 1.152–2.472, p < 0.01), later sleep-wake schedule (OR = 2.196, 95% CI: 1.450–3.326, p < 0.001), and ISI score of 15–28 points (OR = 2.653, 95% CI: 1.558–4.515, p < 0.001) (Table 2).

Table 2.
Factors associated with evening hyperphagia (n = 119).
In the nocturnal ingestion group, nine items were significantly associated in the univariate logistic regression analysis: age category of 40–59 years (OR = 0.622, 95% CI: 0.453–0.855, p < 0.01), age category of 60–79 years (OR = 0.407, 95% CI: 0.285–0.581, p < 0.001), current smoker (OR = 1.544, 95% CI: 1.129–2.112, p < 0.01), living alone (OR = 1.618, 95% CI: 1.166–2.247, p < 0.01), hypnotic medication use (OR = 1.742, 95% CI: 1.137–2.667, p < 0.05), earlier sleep-wake schedule (OR = 1.804, 95% CI: 1.321–2.463, p < 0.001), absolute value of social jet lag of ≥2 h (OR = 1.694, 95% CI: 1.053–2.725, p < 0.05), ISI score of 8–14 points (OR = 1.705, 95% CI: 1.253–2.322, p < 0.001), and ISI score of 15–28 points (OR = 2.978, 95% CI: 1.949–4.548, p < 0.001). Furthermore, in the multiple logistic regression analysis, significant associations were found for the following seven items: age category of 40–59 years (OR = 0.532, 95% CI: 0.382–0.741, p < 0.001), age category of 60–79 years (OR = 0.355, 95% CI: 0.241–0.523, p < 0.001), current smoker (OR = 1.558, 95% CI: 1.129–2.152, p < 0.01), living alone (OR = 1.569, 95% CI: 1.121–2.196, p < 0.01), earlier sleep-wake schedule (OR = 2.153, 95% CI: 1.562–2.967, p < 0.001), ISI score of 8–14 points (OR = 1.577, 95% CI: 1.149–2.165, p < 0.01), and ISI score of 15–28 points (OR = 2.507, 95% CI: 1.571–4.001, p < 0.001) (Table 3).

Table 3.
Factors associated with nocturnal ingestion (n = 208).
4. Discussion
This is the first study to examine the prevalence of evening hyperphagia and nocturnal ingestion as well as their association with descriptive background variables, including sleep habits, in the general population across a wide age range. Here, 4.1% of the participants were suspected to have NES, out of which approximately two-thirds were categorized as having nocturnal ingestion. This prevalence was higher than that previously reported in the general population [27] but lower than that reported in individuals with obesity [28]. In the present study, both evening hyperphagia and nocturnal ingestion showed a significant association with insomnia severity. This result supports the original definition of NES by Stunkard et al. [3] and is consistent with the results of previous literature that showed an association between insomnia and NES, which was based on the definition including both evening hyperphagia and nocturnal ingestion [9,29]. This finding is also in line with the results of previous studies that indicated an association between insomnia and binge eating [30,31], suggesting a close link between insomnia and eating behavior, regardless of the time of food ingestion.
In this study, evening hyperphagia was significantly associated with shorter habitual sleep duration, independent of insomnia symptoms. A previous study indicated increased appetite due to chronic sleep deprivation [32] as one of the possible causative factors of evening overeating. In contrast, nocturnal ingestion was associated with longer average sleep duration. This is a puzzling result, considering that SREDs, another subtype of nocturnal ingestion, are more frequent in individuals with shorter sleep duration [8]. However, sleep duration in this study was calculated as the difference between sleep onset time in the night and wake-up time in the morning, and there were no data on wake time after sleep onset. A large difference between the sleep onset time and wake-up time suggests that a prolongation of time in bed due to exacerbation of sleep maintenance insomnia might lead to the occurrence of nocturnal ingestion [33]. However, a direct relationship between habitual sleep duration and evening hyperphagia or nocturnal ingestion has not been well elucidated to date, and this issue needs to be examined in future studies. One more contrasting feature observed in this study was that evening hyperphagia and nocturnal ingestion were independently associated with a later sleep-wake schedule and an earlier sleep-wake schedule, respectively. Considering the circadian rhythm perspective, the pathology of NES has been potentially linked with a delay in feeding rhythms deviating from sleep-wake rhythms [34,35]. However, because of the reports of delayed sleep-wake rhythms in patients with NES [16,36], the relationship between feeding rhythms and sleep-wake rhythms remains controversial. The inconsistencies in the sleep-wake rhythm patterns among patients with NES in previous reports were possibly attributed to the distinct association of the sleep-wake schedules between the patients with evening hyperphagia and those with nocturnal ingestion.
Among the three groups, the anxiety and depression scores were significantly higher in the evening hyperphagia and nocturnal ingestion groups than in the non-NES group. The effect sizes of Cohen’s d were small to moderate in both comparisons, indicating that these results could be applied in daily clinical practice. Although many reports suggest an association between NES and depression [1,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51], only a few reports show an association between NES and anxiety [51,52]. In the present study, both evening hyperphagia and nocturnal ingestion had similar levels of association with anxiety and depression, possibly due to the underlying covariation of anxiety and depression [53]. Administration of selective serotonin reuptake inhibitors (SSRIs) has been indicated as an effective treatment for NES [54,55,56,57]. They alleviate the eating symptoms, possibly via reduction in anxiety and depression. However, how SSRIs affect nighttime appetite and eating behavior remains unclear. Future studies should conduct detailed examinations of the relationship between the improvement of nighttime eating frequency/severity and anxiety/depression.
Consistent with the results of our previous study [16], hypnotic medication use was more common in the evening hyperphagia and nocturnal ingestion groups than in the non-NES group. However, it was not independently associated with the evening hyperphagia or nocturnal ingestion groups. The increased use of hypnotic medication might be a resultant phenomenon of the relation between evening hyperphagia and nocturnal ingestion with insomnia. However, simultaneously, it should be noted that the type and dosage of hypnotic medications were not examined in this study, and the impacts of hypnotics usage might be underestimated. Additionally, since the nocturnal ingestion group in the present study was quite young, this group might have exhibited characteristics that were common with SREDs, which are non-rapid eye movement parasomnias that commonly occur in the younger populations [13] and can be induced by hypnotic GABAA agonist medication [58,59,60,61,62,63]. Furthermore, another area of interest for future research would be the aspect of nocturnal eating with amnesia, which was not investigated in this study.
The relationship between NES and body weight remains controversial. Although NES is common in patients with obesity, many patients with NES do not present with obesity [64]. In this study, all three groups did not show a significant difference in BMI, suggesting that NES morbidity is not associated with weight gain in the general population. However, it was only evening hyperphagia and not nocturnal ingestion, that showed an independent and significant association with a higher BMI. This finding suggests that individuals with high BMI are more prone to developing evening hyperphagia, which is partly in line with a report showing that obesity is less common in individuals with nocturnal ingestion than in those with evening hyperphagia [17]. In individuals with obesity, the comorbidity of NES interferes with weight loss [65,66], but this phenomenon might be caused by evening hyperphagia and not nocturnal ingestion. Future studies should clarify the differences in the weight loss interference between evening hyperphagia and nocturnal ingestion.
Considering the other lifestyle-related factors, the percentage of smokers was higher in the evening hyperphagia and nocturnal ingestion groups, where smoking was independently associated with nocturnal ingestion. This was consistent with the results of our previous study [16], a report showing a high rate of nicotine dependence in patients with NES [44], and a retrospective study on NES/SRED outpatients in which nearly 40% were smokers [58]. A smoking habit is more prevalent in patients with eating disorders [67], especially in those with bulimia nervosa and binge eating disorder rather than in those with anorexia nervosa [68,69,70]. Additionally, addictive traits in smokers [71] might be associated with nocturnal ingestion. As for the other sociodemographic factors, living alone status was frequent in the evening hyperphagia and nocturnal ingestion groups, where it was independently associated with nocturnal ingestion. This may be because individuals who live alone are more likely to have disrupted lifestyles, including eating habits [72,73]. Furthermore, social jet lag, which might lead to insulin resistance via circadian disruption [74], was not significantly associated with either evening hyperphagia or nocturnal ingestion. This suggests that social jet lag, which includes weekday sleep deficits and delayed weekend sleep schedules, does not contribute to NES pathology on its own.
There are some limitations in the present study. First, the detection of NES relied only on the self-administered questionnaires and was not determined by clinical interviews. Moreover, the identification of evening hyperphagia according to the caloric intake after dinner was based on self-reports, while the definition of nocturnal ingestion, which was based on the last time of food consumption, time to go to bed, latency to fall asleep on weekdays and holidays, and frequency of eating after bedtime, was not assessed directly. In addition, the content and amount of foods ingested were not clear; thus, the possible negative effects of the diet could not be fully investigated. To address these limitations, a detailed assessment of the number of consumed calories and day-to-day variation in eating behavior should be conducted. Additionally, lack of data on wake time after sleep onset was another methodological limitation. Second, this study was conducted as an internet survey. Studies suggest that internet users tend to have shorter sleep duration and delayed sleep-wake rhythms [75,76], which might have led to a sampling bias. Additionally, this was a cross-sectional study and, therefore, a causal relationship cannot be identified between the identified factors and evening hyperphagia/nocturnal ingestion. Third, smoking and drinking habits in this study were determined by responses of “yes” or “no”; therefore, our study did not reflect the amount or timing of exposure to nicotine and alcohol. Moreover, this study did not have information on comorbidities and concomitant medications. Although comorbid sleep disorders, such as narcolepsy, obstructive sleep apnea, and periodic limb movement disorder are associated with NES [4,10], and comorbidities of certain endocrine disorders and the use of psychotropic drugs may increase appetite [77,78], information on these issues was lacking.
5. Conclusions
In the present study, we examined factors associated with the two main constituent symptoms of NES, evening hyperphagia and nocturnal ingestion. Our findings showed that participants with either of these core symptoms exhibited higher anxiety and depression scores than those without NES. Evening hyperphagia was associated with shorter habitual sleep duration and delayed sleep-wake schedules, while nocturnal ingestion was linked to longer habitual sleep duration and earlier sleep-wake schedules, suggesting different pathophysiological backgrounds between the two symptoms. These findings are important for devising therapeutic interventions for NES, such as the improvement of sleep-wake rhythms and sleep duration for severe evening hyperphagia. Moreover, the relationship between NES and sleep habits should be examined in clinical populations to confirm the significance of sleep schedule in the mechanism of NES. Furthermore, future longitudinal studies are warranted to clarify the impact of NES on physical and mental health.
Author Contributions
Conceptualization, Y.K. and Y.I.; methodology, K.M., Y.K., I.O., Y.T., K.K. and Y.I.; validation, Y.K.; formal analysis, K.M.; resources, Y.K. and Y.I.; data curation, K.M.; writing—original draft preparation, K.M.; writing—review and editing, I.O., K.K. and Y.I; visualization, K.M.; supervision, Y.K. and Y.T.; project administration, Y.K.; funding acquisition, K.M., Y.K. and I.O. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by JSPS KAKENHI Grant-in-Aid for Young Scientists (No. 16K07545, 16K04388, and 19K17098).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the ethics committee of Tokyo Medical University (No. 3307).
Informed Consent Statement
Informed consent was obtained from all participants via the survey website.
Data Availability Statement
The data will be shared on reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lundgren, J.D.; Allison, K.C.; O’Reardon, J.P.; Stunkard, A.J. A descriptive study of non-obese persons with night eating syndrome and a weight-matched comparison group. Eat. Behav. 2008, 9, 343–351. [Google Scholar] [CrossRef]
- Gluck, M.E.; Geliebter, A.; Satov, T. Night eating syndrome is associated with depression, low self-esteem, reduced daytime hunger, and less weight loss in obese outpatients. Obes. Res. 2001, 9, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Stunkard, A.J.; Grace, W.J.; Wolff, H.G. The night-eating syndrome; a pattern of food intake among certain obese patients. Am. J. Med. 1955, 19, 78–86. [Google Scholar] [CrossRef]
- Spaggiari, M.C.; Granella, F.; Parrino, L.; Marchesi, C.; Melli, I.; Terzano, M.G. Nocturnal eating syndrome in adults. Sleep 1994, 17, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Birketvedt, G.S.; Florholmen, J.; Sundsfjord, J.; Osterud, B.; Dinges, D.; Bilker, W.; Stunkard, A. Behavioral and neuroendocrine characteristics of the night-eating syndrome. JAMA 1999, 282, 657–663. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Allison, K.C.; Lundgren, J.D.; O’Reardon, J.P.; Geliebter, A.; Gluck, M.E.; Vinai, P.; Mitchell, J.E.; Schenck, C.H.; Howell, M.J.; Crow, S.J.; et al. Proposed diagnostic criteria for night eating syndrome. Int. J. Eat. Disord. 2010, 43, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Inoue, Y. Sleep-related eating disorder and its associated conditions. Psychiatry Clin. Neurosci. 2015, 69, 309–320. [Google Scholar] [CrossRef]
- Vinai, P.; Ferri, R.; Ferini-Strambi, L.; Cardetti, S.; Anelli, M.; Vallauri, P.; Ferrato, N.; Zucconi, M.; Carpegna, G.; Manconi, M. Defining the borders between sleep-related eating disorder and night eating syndrome. Sleep Med. 2012, 13, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Schenck, C.H.; Mahowald, M.W. Review of nocturnal sleep-related eating disorders. Int. J. Eat. Disord. 1994, 15, 343–356. [Google Scholar] [CrossRef] [PubMed]
- Winkelman, J.W. Clinical and polysomnographic features of sleep-related eating disorder. J. Clin. Psychiatry 1998, 59, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Schenck, C.H.; Hurwitz, T.D.; O’Connor, K.A.; Mahowald, M.W. Additional categories of sleep-related eating disorders and the current status of treatment. Sleep 1993, 16, 457–466. [Google Scholar] [PubMed]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders—Third Edition (ICSD-3); American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- Fulda, S.; Hornyak, M.; Müller, K.; Cerny, L.; Beitinger, P.A.; Wetter, T.C. Development and validation of the Munich Parasomnia Screening (MUPS). Somnol.-Schlafforschung Schlafmed. 2008, 12, 56–65. [Google Scholar] [CrossRef]
- Komada, Y.; Breugelmans, R.; Fulda, S.; Nakano, S.; Watanabe, A.; Noda, C.; Nishida, S.; Inoue, Y. Japanese version of the Munich Parasomnia Screening: Translation and linguistic validation of a screening instrument for parasomnias and nocturnal behaviors. Neuropsychiatr. Dis. Treat. 2015, 11, 2953. [Google Scholar] [CrossRef] [PubMed]
- Matsui, K.; Komada, Y.; Nishimura, K.; Kuriyama, K.; Inoue, Y. Prevalence and associated factors of nocturnal eating behavior and sleep-related eating disorder-like behavior in Japanese young adults: Results of an internet survey using Munich Parasomnia Screening. J. Clin. Med. 2020, 9, 1243. [Google Scholar] [CrossRef] [PubMed]
- Loddo, G.; Zanardi, M.; Caletti, M.T.; Mignani, F.; Petroni, M.L.; Chiaro, G.; Marchesini, G.; Provini, F. Searching food during the night: The role of video-polysomnography in the characterization of the night eating syndrome. Sleep Med. 2019, 64, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Komada, Y.; Okajima, I.; Kitamura, S.; Inoue, Y. A survey on social jetlag in Japan: A nationwide, cross-sectional internet survey. Sleep Biol. Rhythm. 2019, 17, 417–422. [Google Scholar] [CrossRef]
- Satoh, A.; Arima, H.; Ohkubo, T.; Nishi, N.; Okuda, N.; Ae, R.; Inoue, M.; Kurita, S.; Murakami, K.; Kadota, A.; et al. Associations of socioeconomic status with prevalence, awareness, treatment, and control of hypertension in a general Japanese population: NIPPON DATA2010. J. Hypertens. 2017, 35, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Munezawa, T.; Morin, C.M.; Inoue, Y.; Nedate, K. Development of the Japanese version of the Insomnia Severity Index (ISI-J). Jpn. J. Psychiatr. Treat. 2009, 24, 219–225. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Hatta, H.; Higashi, A.; Yashiro, H.; Ozasa, K.; Hayashi, K.; Kiyota, K.; Inokuchi, H.; Ikeda, J.; Fujita, K.; Watanabe, Y.; et al. A Validation of the Hospital Anxiety and Dipression Scale. Jpn. J. Psychosom. Med. 1998, 38, 309–315. [Google Scholar] [CrossRef]
- Juda, M.; Vetter, C.; Roenneberg, T. Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J. Biol. Rhythm. 2013, 28, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: Executive summary. Am. J. Clin. Nutr. 1998, 68, 899–917. [Google Scholar] [CrossRef] [PubMed]
- Rand, C.S.; Macgregor, A.M.; Stunkard, A.J. The night eating syndrome in the general population and among postoperative obesity surgery patients. Int. J. Eat. Disord. 1997, 22, 65–69. [Google Scholar] [CrossRef]
- De Zwaan, M.; Marschollek, M.; Allison, K.C. The Night Eating Syndrome (NES) in bariatric surgery patients. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2015, 23, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Ceru-Bjork, C.; Andersson, I.; Rossner, S. Night eating and nocturnal eating-two different or similar syndromes among obese patients? Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 2001, 25, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Kenny, T.E.; Van Wijk, M.; Singleton, C.; Carter, J.C. An examination of the relationship between binge eating disorder and insomnia symptoms. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2018, 26, 186–196. [Google Scholar] [CrossRef] [PubMed]
- Trace, S.E.; Thornton, L.M.; Runfola, C.D.; Lichtenstein, P.; Pedersen, N.L.; Bulik, C.M. Sleep problems are associated with binge eating in women. Int. J. Eat. Disord. 2012, 45, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, K.; Tasali, E.; Penev, P.; Van Cauter, E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann. Intern. Med. 2004, 141, 846–850. [Google Scholar] [CrossRef]
- Suzuki, M.; Furihata, R.; Konno, C.; Konno, M.; Kaneita, Y.; Ohida, T.; Gon, Y.; Uchiyama, M. Sleep disturbance is associated with not only shorter sleep duration, but also longer time in bed: A Japanese general population survey. Sleep Biol. Rhythm. 2019, 17, 407–415. [Google Scholar] [CrossRef]
- Boston, R.C.; Moate, P.J.; Allison, K.C.; Lundgren, J.D.; Stunkard, A.J. Modeling circadian rhythms of food intake by means of parametric deconvolution: Results from studies of the night eating syndrome. Am. J. Clin. Nutr. 2008, 87, 1672–1677. [Google Scholar] [CrossRef]
- Goel, N.; Stunkard, A.J.; Rogers, N.L.; Van Dongen, H.P.; Allison, K.C.; O’Reardon, J.P.; Ahima, R.S.; Cummings, D.E.; Heo, M.; Dinges, D.F. Circadian rhythm profiles in women with night eating syndrome. J. Biol. Rhythm. 2009, 24, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.F.; Thorsteinsson, E.B.; Smithson, M.; Birmingham, C.L.; Aljarallah, H.; Nolan, C. Can body temperature dysregulation explain the co-occurrence between overweight/obesity, sleep impairment, late-night eating, and a sedentary lifestyle? Eat. Weight Disord. 2017, 22, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Guentcheva, I.; Dugas, E.N.; Hanusaik, N.; Drapeau, V.; Sylvestre, M.P.; O’Loughlin, J. Depression symptoms and night eating in young adulthood. Eat. Weight Disord. 2020, 25, 1593–1600. [Google Scholar] [CrossRef] [PubMed]
- Tu, C.Y.; Meg Tseng, M.C.; Chang, C.H. Night eating syndrome in patients with eating disorders: Is night eating syndrome distinct from bulimia nervosa? J. Formos. Med. Assoc. 2019, 118, 1038–1046. [Google Scholar] [CrossRef] [PubMed]
- Geliebter, A.; McOuatt, H.; Tetreault, C.B.; Kordunova, D.; Rice, K.; Zammit, G.; Gluck, M. Is night eating syndrome associated with obstructive sleep apnea, BMI, and depressed mood in patients from a sleep laboratory study? Eat. Behav. 2016, 23, 115–119. [Google Scholar] [CrossRef]
- Dalle Grave, R.; Calugi, S.; Ruocco, A.; Marchesini, G. Night eating syndrome and weight loss outcome in obese patients. Int. J. Eat. Disord. 2011, 44, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.; Meyer, A.H.; Hermann, E.; Tuch, A.; Munsch, S. Night eating syndrome in young adults: Delineation from other eating disorders and clinical significance. Psychiatry Res. 2012, 200, 494–501. [Google Scholar] [CrossRef]
- Striegel-Moore, R.H.; Rosselli, F.; Wilson, G.T.; Perrin, N.; Harvey, K.; DeBar, L. Nocturnal eating: Association with binge eating, obesity, and psychological distress. Int. J. Eat. Disord. 2010, 43, 520–526. [Google Scholar] [CrossRef]
- Calugi, S.; Dalle Grave, R.; Marchesini, G. Night eating syndrome in class II-III obesity: Metabolic and psychopathological features. Int. J. Obes. 2009, 33, 899–904. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saraçlı, Ö.; Atasoy, N.; Akdemir, A.; Güriz, O.; Konuk, N.; Sevinçer, G.M.; Ankaralı, H.; Atik, L. The prevalence and clinical features of the night eating syndrome in psychiatric out-patient population. Compr. Psychiatry 2015, 57, 79–84. [Google Scholar] [CrossRef]
- Allison, K.C.; Wadden, T.A.; Sarwer, D.B.; Fabricatore, A.N.; Crerand, C.E.; Gibbons, L.M.; Stack, R.M.; Stunkard, A.J.; Williams, N.N. Night eating syndrome and binge eating disorder among persons seeking bariatric surgery: Prevalence and related features. Surg. Obes. Relat. Dis. Off. J. Am. Soc. Bariatr. Surg. 2006, 2, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Kim, O.S.; Kim, M.S.; Lee, J.E.; Jung, H. Night-eating syndrome and the severity of self-reported depressive symptoms from the Korea Nurses’ Health Study: Analysis of propensity score matching and ordinal regression. Public Health 2016, 141, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Striegel-Moore, R.H.; Franko, D.L.; Thompson, D.; Affenito, S.; May, A.; Kraemer, H.C. Exploring the typology of night eating syndrome. Int. J. Eat. Disord. 2008, 41, 411–418. [Google Scholar] [CrossRef]
- Rogers, N.L.; Dinges, D.F.; Allison, K.C.; Maislin, G.; Martino, N.; O’Reardon, J.P.; Stunkard, A.J. Assessment of sleep in women with night eating syndrome. Sleep 2006, 29, 814–819. [Google Scholar] [CrossRef]
- Morse, S.A.; Ciechanowski, P.S.; Katon, W.J.; Hirsch, I.B. Isn’t this just bedtime snacking? The potential adverse effects of night-eating symptoms on treatment adherence and outcomes in patients with diabetes. Diabetes Care 2006, 29, 1800–1804. [Google Scholar] [CrossRef]
- Allison, K.C.; Grilo, C.M.; Masheb, R.M.; Stunkard, A.J. Binge eating disorder and night eating syndrome: A comparative study of disordered eating. J. Consult. Clin. Psychol. 2005, 73, 1107–1115. [Google Scholar] [CrossRef]
- Kucukgoncu, S.; Tek, C.; Bestepe, E.; Musket, C.; Guloksuz, S. Clinical features of night eating syndrome among depressed patients. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2014, 22, 102–108. [Google Scholar] [CrossRef]
- Melo, M.C.A.; de Oliveira Ribeiro, M.; de Araújo, C.F.C.; de Mesquita, L.M.F.; de Bruin, P.F.C.; de Bruin, V.M.S. Night eating in bipolar disorder. Sleep Med. 2018, 48, 49–52. [Google Scholar] [CrossRef]
- Eley, T.C.; Stevenson, J. Exploring the covariation between anxiety and depression symptoms: A genetic analysis of the effects of age and sex. J. Child Psychol. Psychiatry Allied Discip. 1999, 40, 1273–1282. [Google Scholar] [CrossRef]
- O’Reardon, J.P.; Stunkard, A.J.; Allison, K.C. Clinical trial of sertraline in the treatment of night eating syndrome. Int. J. Eat. Disord. 2004, 35, 16–26. [Google Scholar] [CrossRef] [PubMed]
- O’Reardon, J.P.; Allison, K.C.; Martino, N.S.; Lundgren, J.D.; Heo, M.; Stunkard, A.J. A randomized, placebo-controlled trial of sertraline in the treatment of night eating syndrome. Am. J. Psychiatry 2006, 163, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Vander Wal, J.S.; Gang, C.H.; Griffing, G.T.; Gadde, K.M. Escitalopram for treatment of night eating syndrome: A 12-week, randomized, placebo-controlled trial. J. Clin. Psychopharmacol. 2012, 32, 341–345. [Google Scholar] [CrossRef]
- Allison, K.C.; Studt, S.K.; Berkowitz, R.I.; Hesson, L.A.; Moore, R.H.; Dubroff, J.G.; Newberg, A.; Stunkard, A.J. An open-label efficacy trial of escitalopram for night eating syndrome. Eat. Behav. 2013, 14, 199–203. [Google Scholar] [CrossRef]
- Matsui, K.; Kuriyama, K.; Kobayashi, M.; Inada, K.; Nishimura, K.; Inoue, Y. The efficacy of add-on ramelteon and subsequent dose reduction of benzodiazepine derivatives/Z-drugs for the treatment of sleep-related eating disorder and night eating syndrome: A retrospective analysis of consecutive cases. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2021, 17, 1475–1483. [Google Scholar] [CrossRef]
- Ghosh, D.; Petrecca, A.M.; Khuhro, A.L. Sleep-Related Eating Disorder (SRED): Paradoxical effect of clonazepam. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2018, 14, 1261–1263. [Google Scholar] [CrossRef]
- Molina, S.M.; Joshi, K.G. A case of zaleplon-induced amnestic sleep-related eating disorder. J. Clin. Psychiatry 2010, 71, 210–211. [Google Scholar] [CrossRef]
- Takaesu, Y.; Ishikawa, J.; Komada, Y.; Murakoshi, A.; Futenma, K.; Nishida, S.; Inoue, Y. Prevalence of and factors associated with sleep-related eating disorder in psychiatric outpatients taking hypnotics. J. Clin. Psychiatry 2016, 77, e892–e898. [Google Scholar] [CrossRef]
- Lam, S.P.; Fong, S.Y.; Ho, C.K.; Yu, M.W.; Wing, Y.K. Parasomnia among psychiatric outpatients: A clinical, epidemiologic, cross-sectional study. J. Clin. Psychiatry 2008, 69, 1374–1382. [Google Scholar] [CrossRef]
- Ho, T.; Jimenez, A.; Sanchez, I.; Seeger, C.; Joseph, M. Sleep-related eating disorder associated with zolpidem: Cases compiled from a literature review. Sleep Med. X 2020, 2, 100019. [Google Scholar] [CrossRef] [PubMed]
- Bruzas, M.B.; Allison, K.C. A Review of the relationship between night eating syndrome and body mass index. Curr. Obes. Rep. 2019, 8, 145–155. [Google Scholar] [CrossRef]
- Gallant, A.R.; Lundgren, J.; Drapeau, V. The night-eating syndrome and obesity. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2012, 13, 528–536. [Google Scholar] [CrossRef]
- Tholin, S.; Lindroos, A.; Tynelius, P.; Akerstedt, T.; Stunkard, A.J.; Bulik, C.M.; Rasmussen, F. Prevalence of night eating in obese and nonobese twins. Obesity 2009, 17, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, C.V.; Turco, R.M.; Sunday, S.R.; Halmi, K.A. Smoking and body image concerns in adolescent girls. Int. J. Eat. Disord. 1998, 24, 429–433. [Google Scholar] [CrossRef]
- Bulik, C.M.; Epstein, L.H.; McKee, M.; Kaye, W. Drug use in women with bulimia and anorexia nervosa. NIDA Res. Monogr. 1990, 105, 462–463. [Google Scholar] [CrossRef]
- Haug, N.A.; Heinberg, L.J.; Guarda, A.S. Cigarette smoking and its relationship to other substance use among eating disordered inpatients. Eat. Weight Disord. 2001, 6, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Anzengruber, D.; Klump, K.L.; Thornton, L.; Brandt, H.; Crawford, S.; Fichter, M.M.; Halmi, K.A.; Johnson, C.; Kaplan, A.S.; LaVia, M.; et al. Smoking in eating disorders. Eat. Behav. 2006, 7, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, R.F. Addiction, cigarette smoking, and voluntary control of action: Do cigarette smokers lose their free will? Addict. Behav. Rep. 2017, 5, 67–84. [Google Scholar] [CrossRef] [PubMed]
- Hanna, K.L.; Collins, P.F. Relationship between living alone and food and nutrient intake. Nutr. Rev. 2015, 73, 594–611. [Google Scholar] [CrossRef]
- Klinenberg, E. Social isolation, loneliness, and living alone: Identifying the risks for public health. Am. J. Public Health 2016, 106, 786–787. [Google Scholar] [CrossRef] [PubMed]
- Stenvers, D.J.; Scheer, F.; Schrauwen, P.; la Fleur, S.E.; Kalsbeek, A. Circadian clocks and insulin resistance. Nat. Rev. Endocrinol. 2019, 15, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Cain, N.; Gradisar, M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010, 11, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Do, Y.K.; Shin, E.; Bautista, M.A.; Foo, K. The associations between self-reported sleep duration and adolescent health outcomes: What is the role of time spent on Internet use? Sleep Med. 2013, 14, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Warren, M.P. Endocrine manifestations of eating disorders. J. Clin. Endocrinol. Metab. 2011, 96, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Vanina, Y.; Podolskaya, A.; Sedky, K.; Shahab, H.; Siddiqui, A.; Munshi, F.; Lippmann, S. Body weight changes associated with psychopharmacology. Psychiatr. Serv. 2002, 53, 842–847. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).