Combatting Sedentary Behaviors by Delivering Remote Physical Exercise in Children and Adolescents with Obesity in the COVID-19 Era: A Narrative Review
Abstract
1. Introduction
2. Materials and Methods
3. Obesity and Physical Activity
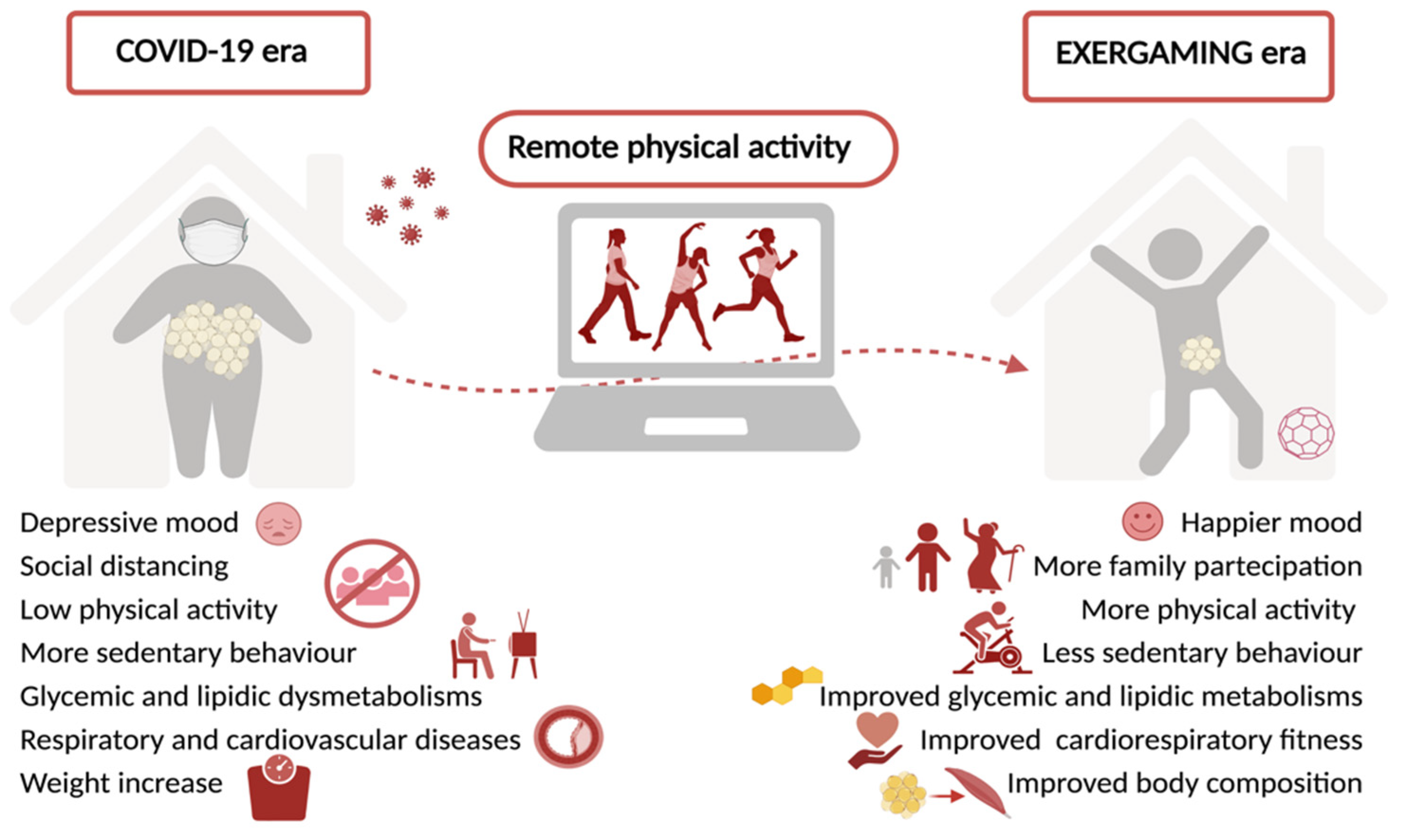
4. Changes in Exercise Practices during COVID 19 and Obesity
5. Online Exercise: Benefits and Efficacy
6. Online Exercise during COVID-19
7. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Falbe, J.; Rosner, B.; Willett, W.C.; Sonneville, K.R.; Hu, F.B.; Field, A.E. Adiposity and different types of screen time. Pediatrics 2013, 132, e1497–e1505. [Google Scholar] [CrossRef]
- Cachón-Zagalaz, J.; Sánchez-Zafra, M.; Sanabrias-Moreno, D.; González-Valero, G.; Lara-Sánchez, A.J.; Zagalaz-Sánchez, M.L. Systematic review of the literature about the effects of the COVID-19 pandemic on the lives of school children. Front. Psychol. 2020, 11, 569348. [Google Scholar] [CrossRef]
- Kakinami, L.; Barnett, T.A.; Séguin, L.; Paradis, G. Parenting style and obesity risk in children. Prev. Med. 2015, 75, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, S.; Grech, S. COVID-19: A one-way ticket to a global childhood obesity crisis? J. Diabetes Metab. Disord. 2020, 19, 2027–2030. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Vandoni, M.; Rossi, V.; di Profio, E.; Carnevale Pellino, V.; Tranfaglia, V.; Pascuzzi, M.C.; Borsani, B.; Bosetti, A.; et al. Telehealth: A useful tool for the management of nutrition and exercise programs in pediatric obesity in the COVID-19 era. Nutrients 2021, 13, 689. [Google Scholar] [CrossRef]
- Parker, K.; Uddin, R.; Ridgers, N.D.; Brown, H.; Veitch, J.; Salmon, J.; Timperio, A.; Sahlqvist, S.; Cassar, S.; Toffoletti, K.; et al. The use of digital platforms for adults’ and adolescents’ physical activity during the COVID-19 pandemic (our life at home): Survey study. J. Med. Internet Res. 2021, 23, e23389. [Google Scholar] [CrossRef]
- Stella, A.B.; Ajčević, M.; Furlanis, G.; Cillotto, T.; Menichelli, A.; Accardo, A.; Manganotti, P. Smart technology for physical activity and health assessment during COVID-19 lockdown. J. Sports Med. Phys. Fit. 2021, 61, 9. [Google Scholar]
- Liang, Y.; Lau, P.W.C.; Jiang, Y.; Maddison, R. Getting active with active video games: A quasi-experimental study. Int. J. Environ. Res. Public Health 2020, 15, 7984. [Google Scholar] [CrossRef] [PubMed]
- Zaccagni, L.; Toselli, S.; Barbieri, D. Physical activity during COVID-19 lockdown in Italy: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 6416. [Google Scholar] [CrossRef]
- Wang, Y.; Monteiro, C.; Popkin, B.M. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am. J. Clin. Nutr. 2002, 75, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Lobstein, T.; Baur, L.; Uauy, R. Obesity in children and young people: A crisis in public health. Obes. Rev. Suppl. 2004, 5, 4–85. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Katzmarzyk, P.T.; Boyce, W.F.; Vereecken, C.; Mulvihill, C.; Roberts, C.; Currie, C.; Pickett, W.; Ńemeth, Á.; Ojala, K.; et al. Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obes. Rev. 2005, 6, 123–132. [Google Scholar] [CrossRef]
- Wang, Y.; Lobstein, T. Worldwide trends in childhood overweight and obesity. Int. J. Pediatric Obes. 2006, 1, 11–25. [Google Scholar] [CrossRef]
- Arpesella, M.; Campostrini, S.; Gerzeli, S.; Lottaroli, S.; Pane, A.; Traverso, M.; Vandoni, M.; Coppola, L. obesity nutritional aspects and life style from a survey on a sample of primary school pupils in the Pavia province (northern Italy). Ital. J. Public Health 2008, 5, 12–17. [Google Scholar] [CrossRef]
- Inkpen, A.; Ramaswamy, K. Global Strategy: Creating and Sustaining Advantage across Borders; Oxford University Press: Oxford, UK, 2007; Volume 2002. [Google Scholar] [CrossRef]
- Grundy, S.M.; Brewer, H.B.; Cleeman, J.I.; Smith, S.C.; Lenfant, C. Definition of metabolic syndrome: Report of the national heart, lung, and blood institute/american heart association conference on scientific issues related to definition. Proc. Circ. 2004, 109. [Google Scholar] [CrossRef]
- Balagopal, P.; de Ferranti, S.D.; Cook, S.; Daniels, S.R.; Gidding, S.S.; Hayman, L.L.; McCrindle, B.W.; Mietus-Snyder, M.L.; Steinberger, J. Nontraditional risk factors and biomarkers for cardiovascular disease: Mechanistic, research, and clinical considerations for youth: A scientific statement from the american heart association. Circulation 2011, 123, 2749–2769. [Google Scholar] [CrossRef]
- Steinberger, J.; Daniels, S.R.; Eckel, R.H.; Hayman, L.; Lustig, R.H.; McCrindle, B.; Mietus-Snyder, M.L. Progress and challenges in metabolic syndrome in children and adolescents. A scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the young committee of the council on cardiovascular disease in the young; council on cardiovascular nursing; and council on nutrition, physical activity, and metabolism. Circulation 2009, 119, 628–647. [Google Scholar] [PubMed]
- Calcaterra, V.; Vandoni, M.; Debarbieri, G.; Larizza, D.; Albertini, R.; Arpesella, M.; Bernardi, L. Deep breathing improves blunted baroreflex sensitivity in obese children and adolescents with insulin resistance. Int. J. Cardiol. 2013, 168, 1614–1615. [Google Scholar] [CrossRef] [PubMed]
- Vandoni, M.; Calcaterra, V.; Pellino, V.C.; de Silvestri, A.; Marin, L.; Zuccotti, G.V.; Tranfaglia, V.; Giuriato, M.; Codella, R.; Lovecchio, N. “Fitness and fatness” in children and adolescents: An Italian cross-sectional study. Children 2021, 8, 762. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Warburton, D.E.R.; Janssen, I.; Paterson, D.H.; Latimer, A.E.; Rhodes, R.E.; Kho, M.E.; Hicks, A.; LeBlanc, A.G.; Zehr, L.; et al. New Canadian physical activity guidelines. Appl. Physiol. Nutr. Metab. 2011, 36, 36–46. [Google Scholar] [CrossRef]
- Corder, K.; Ekelund, U.; Steele, R.M.; Wareham, N.J.; Brage, S. Assessment of Physical Activity in Youth. J. Appl. Physiol. 2008, 105. [Google Scholar] [CrossRef]
- US Department Of Health And Human Services. Physical Activity Guidelines Advisory Committee Scientific Report; US Department of Health And Human Services: Washington, DC, USA, 2018.
- Aubert, S. An overview of scientific-based knowledge on sedentary behaviour among the pediatric population—A conceptual model development. Rev. Interdiscip. Sci. St. Interdiscip. J. Health Sci. 2017, 7. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; Aminian, S.; et al. Sedentary Behavior Research Network (SBRN)—Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, A.; Gunnell, K.; Prince, S.; Saunders, T.; Barnes, J.; Chaput, J.-P. The ubiquity of the screen: An overview of the risks and benefits of screen time in our modern world. Transl. J. Am. Coll. Sports Med. 2017, 2, 104–113. [Google Scholar] [CrossRef]
- Gibbs, B.B.; Hergenroeder, A.L.; Katzmarzyk, P.T.; Lee, I.M.; Jakicic, J.M. Definition, Measurement, and health risks associated with sedentary behavior. Proc. Med. Sci. Sports Exerc. 2015, 47, 1295. [Google Scholar] [CrossRef]
- De Onis, M. WHO Child growth standards based on length/height, weight and age. Acta Paediatr. Int. J. Paediatr. 2006, 95, 76–85. [Google Scholar] [CrossRef]
- Corsello, P.G.; Villani, P.A.; Cerutti, P.F.; Cianfarani, P.S. Consensus su Diagnosi, Trattamento e Prevenzione dell’Obesita’ del Bambino e dell’Adolescente. Available online: http://www.siedp.it/files/Doc.ConsensusObesita__2017.pdf (accessed on 2 November 2021).
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Carson, V.; Chaput, J.P.; Connor Gorber, S.; Dinh, T.; Duggan, M.; Faulkner, G.; Gray, C.E.; Grube, R.; Janson, K.; et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 2016, 41, S311–S327. [Google Scholar] [CrossRef]
- Okely, A.D.; Ghersi, D.; Hesketh, K.D.; Santos, R.; Loughran, S.P.; Cliff, D.P.; Shilton, T.; Grant, D.; Jones, R.A.; Stanley, R.M.; et al. A Collaborative approach to adopting/adapting guidelines—The Australian 24-hour movement guidelines for the early years (birth to 5 years): An integration of physical activity, sedentary behavior, and sleep. BMC Public Health 2017, 17, 167–190. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA J. Am. Med. Assoc. 2018, 320, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Social Care. Physical Activity Guidelines: UK Chief Medical Officers’ Report; Department of Health and Social Care: London, UK, 2019. Available online: https://www.gov.uk/government/publications/physical-activity-guidelines-uk-chief-medical-officers-report (accessed on 2 November 2021).
- Dietz, W.H. Reversing the Tide of obesity. Lancet 2011, 378, 744–746. [Google Scholar] [CrossRef]
- Codella, R.; Chirico, A.; Lucidi, F.; Ferrulli, A.; La Torre, A.; Luzi, L. The immune-modulatory effects of exercise should be favorably harnessed against COVID-19. J. Endocrinol. Investig. 2021, 44, 1119–1122. [Google Scholar] [CrossRef]
- Hansen, P.R.; Andersen, L.J.; Rebelo, A.N.; Brito, J.; Hornstrup, T.; Schmidt, J.F.; Jackman, S.R.; Mota, J.; Rêgo, C.; Oliveira, J.; et al. Cardiovascular effects of 3 months of football training in overweight children examined by comprehensive echocardiography: A pilot study. J. Sports Sci. 2013, 31, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Krustrup, P.; Hansen, P.R.; Nielsen, C.M.; Larsen, M.N.; Randers, M.B.; Manniche, V.; Hansen, L.; Dvorak, J.; Bangsbo, J. Structural and functional cardiac adaptations to a 10-week school-based football intervention for 9–10-year-old children. Scand. J. Med. Sci. Sports 2014, 24, 4–9. [Google Scholar] [CrossRef]
- Atkin, A.J.; Sharp, S.J.; Corder, K.; Van Sluijs, E.M.F. Prevalence and correlates of screen time in youth: An international perspective. Am. J. Prev. Med. 2014, 47, 803–807. [Google Scholar] [CrossRef]
- Seabra, A.; Katzmarzyk, P.; Carvalho, M.J.; Seabra, A.; Coelho-E-Silva, M.; Abreu, S.; Vale, S.; Póvoas, S.; Nascimento, H.; Belo, L.; et al. Effects of 6-month soccer and traditional physical activity programmes on body composition, cardiometabolic risk factors, inflammatory, oxidative stress markers and cardiorespiratory fitness in obese boys. J. Sports Sci. 2016, 34, 1822–1829. [Google Scholar] [CrossRef]
- Marshall, S.J.; Biddle, S.J.H.; Gorely, T.; Cameron, N.; Murdey, I. Relationships between media use, body fatness and physical activity in children and youth: A meta-analysis. Int. J. Obes. 2004, 28, 1238–1246. [Google Scholar] [CrossRef]
- Patrick, K.; Norman, G.J.; Calfas, K.J.; Sallis, J.F.; Zabinski, M.F.; Rupp, J.; Cella, J. Diet, physical activity, and sedentary behaviors as risk factors for overweight in adolescence. Arch. Pediatr. Adolesc. Med. 2004, 158, 385–390. [Google Scholar] [CrossRef]
- Brownson, R.C.; Boehmer, T.K.; Luke, D.A. Declining rates of physical activity in the United States: What are the contributors? Annu. Rev. Public Health 2005, 26, 421–443. [Google Scholar] [CrossRef]
- Dollman, J.; Norton, K.; Norton, L. Evidence for secular trends in children’s physical activity behaviour. Br. J. Sports Med. 2005, 39, 892–897. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Steps to Health: A European Framework to Promote Physical Activity for Health; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Della Guardia, L.; Codella, R. Exercise tolls the bell for key mediators of low-grade inflammation in dysmetabolic conditions. Cytokine Growth Factor Rev. 2021, 62, 83–93. [Google Scholar] [CrossRef]
- Rosa, J.S.; Heydari, S.; Oliver, S.R.; Flores, R.L.; Pontello, A.M.; Ibardolaza, M.; Galassetti, P.R. Inflammatory cytokine profiles during exercise in obese, diabetic, and healthy children. JCRPE J. Clin. Res. Pediatr. Endocrinol. 2011, 3, 115. [Google Scholar] [CrossRef]
- Rosa, J.S.; Oliver, S.R.; Flores, R.L.; Ngo, J.; Milne, G.L.; Zaldivar, F.P.; Galassetti, P.R. Altered inflammatory, oxidative, and metabolic responses to exercise in pediatric obesity and type 1 diabetes. Pediatr. Diabetes 2011, 12, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Simpson, R.J.; Kunz, H.; Agha, N.; Graff, R. Exercise and the Regulation of Immune Functions. In Progress in Molecular Biology and Translational Science; Elsevier: Amsterdam, The Netherlands, 2015; Volume 135, pp. 355–380. ISBN 978-0-12-803991-5. [Google Scholar]
- Timmons, B.W. Exercise and immune function in children. Am. J. Lifestyle Med. 2007, 1, 59–66. [Google Scholar] [CrossRef]
- Jedrychowski, W.; Maugeri, U.; Flak, E.; Mroz, E.; Bianchi, I. Cohort study on low physical activity level and recurrent acute respiratory infections in schoolchildren. Cent. Eur. J. Public Health 2001, 9, 126–129. [Google Scholar]
- Da Silveira, M.P.; da Silva Fagundes, K.K.; Bizuti, M.R.; Starck, É.; Rossi, R.C.; de Resende e Silva, D.T. Physical Exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature. Clin. Exp. Med. 2021, 21, 15–28. [Google Scholar] [CrossRef]
- Lai, A.; Chen, W.; Helm, K. Effects of visfatin gene polymorphism RS4730153 on exercise-induced weight loss of obese children and adolescents of Han Chinese. Int. J. Biol. Sci. 2012, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Plonka, M.; Suder, A.; Glodzik, J.; Toton-Morys, A.; Adamski, P.; Bielanski, W.; Dobrzanska, M.J.; Kaminska, A.; Piorecka, B. Association of the physical activity with leptin blood serum level, body mass indices and obesity in schoolgirls. J. Physiol. Pharmacol. 2011, 62, 647. [Google Scholar] [PubMed]
- Woo, J.; Shin, K.O.; Yoo, J.H.; Park, S.; Kang, S. The effects of detraining on blood adipokines and antioxidant enzyme in Korean overweight children. Eur. J. Pediatr. 2012, 171, 235–243. [Google Scholar] [CrossRef]
- Kim, E.S.; Kwon, Y.; Choe, Y.H.; Kim, M.J. COVID-19-related school closing aggravate obesity and glucose intolerance in pediatric patients with obesity. Sci. Rep. 2021, 11, 5494. [Google Scholar] [CrossRef] [PubMed]
- El-Karaksy, H.; El-Koofy, N.; Anwar, G.; El-Mougy, F.; El-Hennawy, A.; Fahmy, M. Predictors of non-alcoholic fatty liver disease in obese and overweight egyptian children: Single center study. Saudi J. Gastroenterol. 2011, 17, 40. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Vandoni, M.; Pellino, V.C.; Cena, H. Special attention to diet and physical activity in children and adolescents with obesity during the Coronavirus disease-2019 pandemic. Front. Pediatrics 2020, 8, 407. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Larizza, D.; Codrons, E.; de Silvestri, A.; Brambilla, P.; Abela, S.; Arpesella, M.; Vandoni, M. Improved metabolic and cardiorespiratory fitness during a recreational training program in obese children. J. Pediatr. Endocrinol. Metab. 2013, 26, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Bell, L.M.; Watts, K.; Siafarikas, A.; Thompson, A.; Ratnam, N.; Bulsara, M.; Finn, J.; O’Driscoll, G.; Green, D.J.; Jones, T.W.; et al. Exercise alone reduces insulin resistance in obese children independently of changes in body composition. J. Clin. Endocrinol. Metab. 2007, 92, 4230–4235. [Google Scholar] [CrossRef]
- Bülbül, S. Exercise in the treatment of childhood obesity. Turk Pediatri Ars. 2019, 55, 2. [Google Scholar] [CrossRef]
- Nemet, D. Childhood Obesity, Physical Activity, and Exercise. Pediatr. Exerc. Sci. 2017, 29, 60–62. [Google Scholar] [CrossRef]
- Wyszyńska, J.; Ring-Dimitriou, S.; Thivel, D.; Weghuber, D.; Hadjipanayis, A.; Grossman, Z.; Ross-Russell, R.; Dereń, K.; Mazur, A. Physical activity in the prevention of childhood obesity: The position of the european childhood obesity group and the european academy of pediatrics. Front. Pediatr. 2020, 8, 535705. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Ruiz, J.R.; Hurtig-Wennlöf, A.; Vicente-Rodríguez, G.; Rizzo, N.S.; Castillo, M.J.; Sjöström, M. Cardiovascular fitness modifies the associations between physical activity and abdominal adiposity in children and adolescents: The european youth heart study. Br. J. Sports Med. 2010, 44, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K. Body mass index-independent effect of fitness and physical activity for all-cause mortality. Scand. J. Med. Sci. Sports 2007, 17, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.; Moore, J.B.; Singletary, C.R.; Skelton, J.A. Physical activity and family-based obesity treatment: A review of expert recommendations on physical activity in youth. Clin. Obes. 2018, 8, 68–79. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Miyashita, M.; Kwon, Y.C.; Park, H.T.; Kim, E.H.; Park, J.K.; Park, K.B.; Yoon, S.R.; Chung, J.W.; Nakamura, Y.; et al. A 12-week after-school physical activity programme improves endothelial cell function in overweight and obese children: A randomised controlled study. BMC Pediatr. 2012, 12, 111. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Denstel, K.D.; Beals, K.; Bolling, C.; Wright, C.; Crouter, S.E.; McKenzie, T.L.; Pate, R.R.; Saelens, B.E.; Staiano, A.E.; et al. Results from the United States of America’s 2016 Report card on physical activity for children and youth. J. Phys. Act. Health 2016, 13, S307–S313. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.M.; Mytton, O.T.; Bonell, C.; Melendez-Torres, G.J.; Ward, J.; Hudson, L.; Waddington, C.; Thomas, J.; Russell, S.; van der Klis, F.; et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: A systematic review and meta-analysis. JAMA Pediatr. 2021, 175, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Garazzino, S.; Lo Vecchio, A.; Pierantoni, L.; Calò Carducci, F.I.; Marchetti, F.; Meini, A.; Castagnola, E.; Vergine, G.; Donà, D.; Bosis, S.; et al. Epidemiology, clinical features and prognostic factors of pediatric SARS-CoV-2 infection: Results from an Italian multicenter study. Front. Pediatrics 2021, 9, 649358. [Google Scholar] [CrossRef]
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiology of COVID-19 among children in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef]
- Liguoro, I.; Pilotto, C.; Bonanni, M.; Ferrari, M.E.; Pusiol, A.; Nocerino, A.; Vidal, E.; Cogo, P. SARS-COV-2 infection in children and newborns: A systematic review. Eur. J. Pediatr. 2020, 179, 1029–1046. [Google Scholar] [CrossRef]
- Tsankov, B.K.; Allaire, J.M.; Irvine, M.A.; Lopez, A.A.; Sauvé, L.J.; Vallance, B.A.; Jacobson, K. Severe COVID-19 infection and pediatric comorbidities: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 103, 246–256. [Google Scholar] [CrossRef]
- Zachariah, P.; Johnson, C.L.; Halabi, K.C.; Ahn, D.; Sen, A.I.; Fischer, A.; Banker, S.L.; Giordano, M.; Manice, C.S.; Diamond, R.; et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children’s hospital in New York City, New York. JAMA Pediatr. 2020, 174, e202430. [Google Scholar] [CrossRef]
- Kaushik, S.; Aydin, S.I.; Derespina, K.R.; Bansal, P.B.; Kowalsky, S.; Trachtman, R.; Gillen, J.K.; Perez, M.M.; Soshnick, S.H.; Conway, E.E.; et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome Coronavirus 2 infection (MIS-C): A multi-institutional study from New York City. J. Pediatr. 2020, 224, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Nakra, N.; Blumberg, D.; Herrera-Guerra, A.; Lakshminrusimha, S. Multi-system inflammatory syndrome in children (MIS-C) Following SARS-CoV-2 infection: Review of clinical presentation, hypothetical pathogenesis, and proposed management. Children 2020, 7, 69. [Google Scholar] [CrossRef] [PubMed]
- May, T. Lockdown-type measures look effective against Covid-19. BMJ 2020, m2809. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Iafusco, D.; Carnevale Pellino, V.; Mameli, C.; Tornese, G.; Chianese, A.; Cascella, C.; Macedoni, M.; Redaelli, F.; Zuccotti, G.; et al. “CoVidentary”: An online exercise training program to reduce sedentary behaviours in children with type 1 diabetes during the COVID-19 pandemic. J. Clin. Transl. Endocrinol. 2021, 25, 100261. [Google Scholar] [CrossRef]
- Tornaghi, M.; Lovecchio, N.; Vandoni, M.; Chirico, A.; Codella, R. Physical activity levels across COVID-19 outbreak in youngsters of northwestern Lombardy. J Sports Med. Phys. Fitness 2021, 61, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 85. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Ferracuti, S.; de Giglio, O.; Caggiano, G.; Protano, C.; Valeriani, F.; Parisi, E.A.; Valerio, G.; Liguori, G.; et al. Sedentary behaviors and physical activity of italian undergraduate students during lockdown at the time of CoViD−19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6171. [Google Scholar] [CrossRef] [PubMed]
- Bronikowska, M.; Krzysztoszek, J.; Łopatka, M.; Ludwiczak, M.; Pluta, B. Comparison of physical activity levels in youths before and during a pandemic lockdown. Int. J. Environ. Res. Public Health 2021, 18, 5139. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.C.E.; Anedda, B.; Burchartz, A.; Eichsteller, A.; Kolb, S.; Nigg, C.; Niessner, C.; Oriwol, D.; Worth, A.; Woll, A. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: A natural experiment. Sci. Rep. 2020, 10, 21780. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Browne, N.T.; Snethen, J.A.; Greenberg, C.S.; Frenn, M.; Kilanowski, J.F.; Gance-Cleveland, B.; Burke, P.J.; Lewandowski, L. When pandemics collide: The impact of COVID-19 on childhood obesity. J. Pediatr. Nurs. 2021, 56, 90–98. [Google Scholar] [CrossRef]
- McManus, A.M.; Mellecker, R.R. Physical Activity and obese children. J. Sport Health Sci. 2012, 1, 141–148. [Google Scholar] [CrossRef]
- Storz, M.A. The COVID-19 Pandemic: An unprecedented tragedy in the battle against childhood obesity. Clin. Exp. Pediatr. 2020, 63, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Durá-Travé, T.; Gallinas-Victoriano, F.; Chueca-Guindulain, M.J.; Berrade-Zubiri, S. Prevalence of hypovitaminosis D and associated factors in obese spanish children. Nutr. Diabetes 2017, 7, e248. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Roso, M.B.; de Carvalho Padilha, P.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Arantes Ferreira Peres, W.; Martorell, M.; Aires, M.T.; de Oliveira Cardoso, L.; et al. Covid-19 confinement and changes of adolescent’s dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar] [CrossRef]
- Pombo, A.; Luz, C.; Rodrigues, L.P.; Ferreira, C.; Cordovil, R. Correlates of children’s physical activity during the COVID-19 confinement in Portugal. Public Health 2020, 189, 14–19. [Google Scholar] [CrossRef]
- Chambonniere, C.; Lambert, C.; Fearnbach, N.; Tardieu, M.; Fillon, A.; Genin, P.; Larras, B.; Melsens, P.; Bois, J.; Pereira, B.; et al. Effect of the COVID-19 lockdown on physical activity and sedentary behaviors in french children and adolescents: New results from the ONAPS national survey. Eur. J. Integr. Med. 2021, 43, 101308. [Google Scholar] [CrossRef]
- Jurak, G.; Morrison, S.A.; Kovač, M.; Leskošek, B.; Sember, V.; Strel, J.; Starc, G. A COVID-19 crisis in child physical fitness: Creating a barometric tool of public health engagement for the Republic of Slovenia. Front. Public Health 2021, 9, 644235. [Google Scholar] [CrossRef] [PubMed]
- Guerrero, M.D.; Vanderloo, L.M.; Rhodes, R.E.; Faulkner, G.; Moore, S.A.; Tremblay, M.S. Canadian children’s and youth’s adherence to the 24-h movement guidelines during the COVID-19 pandemic: A decision tree analysis. J. Sport Health Sci. 2020, 9, 313–321. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Spence, J.C.; Berry, T.; Faulkner, G.; Latimer-Cheung, A.E.; O’Reilly, N.; Tremblay, M.S.; Vanderloo, L. Parental support of the Canadian 24-hour movement guidelines for children and youth: Prevalence and correlates. BMC Public Health 2019, 19, 1385. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Lim, C. Promoting parent and child physical activity together: Elicitation of potential intervention targets and preferences. Health Educ. Behav. 2018, 45, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Larrad, A.; Mañas, A.; Labayen, I.; González-Gross, M.; Espin, A.; Aznar, S.; Serrano-Sánchez, J.A.; Vera-Garcia, F.J.; González-Lamuño, D.; Ara, I.; et al. Impact of COVID-19 confinement on physical activity and sedentary behaviour in Spanish university students: Role of gender. Int. J. Environ. Res. Public Health 2021, 18, 369. [Google Scholar] [CrossRef]
- Bates, L.; Zieff, G.; Stanford, K.; Moore, J.; Kerr, Z.; Hanson, E.; Barone Gibbs, B.; Kline, C.; Stoner, L. COVID-19 Impact on behaviors across the 24-hour day in children and adolescents: Physical activity, sedentary behavior, and sleep. Children 2020, 7, 138. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Rahman, A.M.; Chandrasekaran, B. Estimating the impact of the pandemic on children’s physical health: A scoping review. J. Sch. Health 2021, 91, 936–947. [Google Scholar] [CrossRef]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19–related school closings and risk of weight gain among children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [PubMed]
- Von Hippel, P.T.; Workman, J. From Kindergarten through second grade, u.s. children’s obesity prevalence grows only during summer vacations: Obesity grows only during summer. Obesity 2016, 24, 2296–2300. [Google Scholar] [CrossRef]
- Franckle, R.; Adler, R.; Davison, K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: A systematic review. Prev. Chronic Dis. 2014, 11, 130355. [Google Scholar] [CrossRef]
- Von Hippel, P.T.; Powell, B.; Downey, D.B.; Rowland, N.J. The effect of school on overweight in childhood: Gain in body mass index during the school year and during summer vacation. Am. J. Public Health 2007, 97, 696–702. [Google Scholar] [CrossRef]
- Smith, D.T.; Bartee, R.T.; Dorozynski, C.M.; Carr, L.J. Prevalence of overweight and influence of out-of-school seasonal periods on body mass index among american indian schoolchildren. Prev. Chronic. Dis. 2009, 6, A20. [Google Scholar] [PubMed]
- Díaz-Zavala, R.G.; Castro-Cantú, M.F.; Valencia, M.E.; Álvarez-Hernández, G.; Haby, M.M.; Esparza-Romero, J. Effect of the holiday season on weight gain: A narrative review. J. Obes. 2017, 2017, 2085136. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, P.; Pozzobon, G.; Pietrobelli, A. Physical activity as the main therapeutic tool for metabolic syndrome in childhood. Int. J. Obes. 2011, 35, 16–28. [Google Scholar] [CrossRef] [PubMed]
- An, R. Projecting the impact of the Coronavirus disease-2019 pandemic on childhood obesity in the United States: A microsimulation model. J. Sport Health Sci. 2020, 9, 302–312. [Google Scholar] [CrossRef]
- Yang, S.; Guo, B.; Ao, L.; Yang, C.; Zhang, L.; Zhou, J.; Jia, P. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin. Obes. 2020, 10, e12416. [Google Scholar] [CrossRef] [PubMed]
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Obesity in children and adolescents during COVID-19 pandemic. Children 2021, 8, 135. [Google Scholar] [CrossRef]
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: A scoping review. Front. Nutr. 2021, 8, 626432. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Brooks, C.G.; Spencer, J.R.; Sprafka, J.M.; Roehl, K.A.; Ma, J.; Londhe, A.A.; He, F.; Cheng, A.; Brown, C.A.; Page, J. Pediatric BMI changes during COVID-19 pandemic: An electronic health record-based retrospective cohort study. EClinicalMedicine 2021, 38, 101026. [Google Scholar] [CrossRef]
- Chen, F.; Zheng, D.; Liu, J.; Gong, Y.; Guan, Z.; Lou, D. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav. Immun. 2020, 88, 36–38. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef]
- Wilson, S.M.; Sato, A.F. Stress and paediatric obesity: What we know and where to go: Stress and paediatric obesity. Stress Health 2014, 30, 91–102. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Asare, M. Physical activity and mental health in children and adolescents: A review of reviews. Br. J. Sports Med. 2011, 45, 886–895. [Google Scholar] [CrossRef]
- Korczak, D.J.; Madigan, S.; Colasanto, M. Children’s physical activity and depression: A meta-analysis. Pediatrics 2017, 139, e20162266. [Google Scholar] [CrossRef]
- Rodriguez-Ayllon, M.; Cadenas-Sánchez, C.; Estévez-López, F.; Muñoz, N.E.; Mora-Gonzalez, J.; Migueles, J.H.; Molina-García, P.; Henriksson, H.; Mena-Molina, A.; Martínez-Vizcaíno, V.; et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: A systematic review and meta-analysis. Sports Med. 2019, 49, 1383–1410. [Google Scholar] [CrossRef] [PubMed]
- Wright, L.J.; Williams, S.E.; Veldhuijzen van Zanten, J.J.C.S. Physical Activity protects against the negative impact of coronavirus fear on adolescent mental health and well-being during the COVID-19 pandemic. Front. Psychol. 2021, 12, 580511. [Google Scholar] [CrossRef]
- Khan, M.; Adil, S.F.; Alkhathlan, H.Z.; Tahir, M.N.; Saif, S.; Khan, M.; Khan, S.T. COVID-19: A global challenge with old history, epidemiology and progress so far. Molecules 2021, 26, 39. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.A.; Schmidt, E.M.; Arguello, D.J.; Eyllon, M.N.; Castaneda-Sceppa, C.; Cloutier, G.; Hillman, C.H. Online preschool teacher training to promote physical activity in young children: A pilot cluster randomized controlled trial. Sch. Psychol. 2020, 35, 118–127. [Google Scholar] [CrossRef]
- Johnson, R.W.; Williams, S.A.; Gucciardi, D.F.; Bear, N.; Gibson, N. Evaluating the effectiveness of home exercise programmes using an online exercise prescription tool in children with cerebral palsy: Protocol for a randomised controlled trial. BMJ Open 2018, 8, e018316. [Google Scholar] [CrossRef]
- Houghton, K.M.; Macdonald, H.M.; McKay, H.A.; Guzman, J.; Duffy, C.; Tucker, L.; on behalf of the LEAP Study Investigators. Feasibility and safety of a 6-month exercise program to increase bone and muscle strength in children with juvenile idiopathic arthritis. Pediatr. Rheumatol. 2018, 16, 67. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Ma, Y.; Mo, D.; Zhang, S.; Xiang, M.; Zhang, Z. Methodology of an Exercise intervention program using social incentives and gamification for obese children. BMC Public Health 2019, 19, 686. [Google Scholar] [CrossRef]
- Hernández-Jiménez, C.; Sarabia, R.; Paz-Zulueta, M.; Paras-Bravo, P.; Pellico, A.; Ruiz Azcona, L.; Blanco, C.; Madrazo, M.; Agudo, M.J.; Sarabia, C.; et al. Impact of active video games on body mass index in children and adolescents: Systematic review and meta-analysis evaluating the quality of primary studies. Int. J. Environ. Res. Public Health 2019, 16, 2424. [Google Scholar] [CrossRef]
- Barnett, A.; Cerin, E.; Baranowski, T. Active video games for youth: A systematic review. J. Phys. Act. Health 2011, 8, 724–737. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.B.; Pinto, R.Z.; Saraiva, B.T.C.; Tebar, W.R.; Delfino, L.D.; Franco, M.R.; Silva, C.C.M.; Christofaro, D.G.D. Effects of active video games on children and adolescents: A systematic review with meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 4–12. [Google Scholar] [CrossRef]
- Suleiman-Martos, N.; García-Lara, R.A.; Martos-Cabrera, M.B.; Albendín-García, L.; Romero-Béjar, J.L.; Cañadas-De la Fuente, G.A.; Gómez-Urquiza, J.L. Gamification for the Improvement of diet, nutritional habits, and body composition in children and adolescents: A systematic review and meta-analysis. Nutrients 2021, 13, 2478. [Google Scholar] [CrossRef]
- Santos, I.K.D.; de Medeiros, R.C.S.C.; de Medeiros, J.A.; de Almeida-Neto, P.F.; de Sena, D.C.S.; Cobucci, R.N.; Oliveira, R.S.; Cabral, B.G. de A.T.; Dantas, P.M.S. Active Video games for improving mental health and physical fitness-an alternative for children and adolescents during social isolation: An overview. Int. J. Environ. Res. Public Health 2021, 18, 1641. [Google Scholar] [CrossRef]
- Johnson, R.W.; Williams, S.A.; Gucciardi, D.F.; Bear, N.; Gibson, N. Can an online exercise prescription tool improve adherence to home exercise programmes in children with cerebral palsy and other neurodevelopmental disabilities? A randomised controlled trial. BMJ Open 2020, 10, e040108. [Google Scholar] [CrossRef]
- Gil-Cosano, J.J.; Ubago-Guisado, E.; Sánchez, M.J.; Ortega-Acosta, M.J.; Mateos, M.E.; Benito-Bernal, A.I.; Llorente-Cantarero, F.J.; Ortega, F.B.; Ruiz, J.R.; Labayen, I.; et al. The effect of an online exercise programme on bone health in paediatric cancer survivors (IboneFIT): Study protocol of a multi-centre randomized controlled trial. BMC Public Health 2020, 20, 1520. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.J. Tele-exercise as a promising tool to promote exercise in children with cystic fibrosis. Front. Public Health 2018, 6, 5. [Google Scholar] [CrossRef]
- Ambrosino, P.; Fuschillo, S.; Papa, A.; di Minno, M.N.D.; Maniscalco, M. Exergaming as a supportive tool for home-based rehabilitation in the COVID-19 pandemic era. Games Health J. 2020, 9, 311–313. [Google Scholar] [CrossRef]
- Viana, R.B.; de Lira, C.A.B. Exergames as coping strategies for anxiety disorders during the COVID-19 quarantine period. Games Health J. 2020, 9, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Sun, H. Effects of active videogame and sports, play, and active recreation for kids physical education on children’s health-related fitness and enjoyment. Games Health J. 2017, 6, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Staiano, A.E.; Abraham, A.A.; Calvert, S.L. Motivating effects of cooperative exergame play for overweight and obese adolescents. J. Diabetes Sci. Technol. 2012, 6, 812–819. [Google Scholar] [CrossRef]
- Benzing, V.; Schmidt, M. Exergaming for children and adolescents: Strengths, weaknesses, opportunities and threats. J. Clin. Med. 2018, 7, 422. [Google Scholar] [CrossRef]
- Trost, S.G.; Sundal, D.; Foster, G.D.; Lent, M.R.; Vojta, D. Effects of a pediatric weight management program with and without active video games a randomized trial. JAMA Pediatrics 2014, 168, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Lamboglia, C.M.G.F.; da Silva, V.T.B.L.; de Vasconcelos Filho, J.E.; Pinheiro, M.H.N.P.; da Munguba, M.C.S.; Silva Júnior, F.V.I.; de Paula, F.A.R.; da Silva, C.A.B. Exergaming as a strategic tool in the fight against childhood obesity: A systematic review. J. Obes. 2013, 2013, 438364. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zeng, N.; Gao, Z. Exergaming and Obesity in youth: Current perspectives. Int. J. Gen. Med. 2016, 9, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Bethea, T.C.; Berry, D.; Maloney, A.E.; Sikich, L. Pilot study of an active screen time game correlates with improved physical fitness in minority elementary school youth. Games Health J. 2012, 1, 29–36. [Google Scholar] [CrossRef]
- Murphy, M.H.; Lahart, I.; Carlin, A.; Murtagh, E. The effects of continuous compared to accumulated exercise on health: A meta-analytic review. Sports Med. 2019, 49, 1585–1607. [Google Scholar] [CrossRef]
- Daley, A.J. Can exergaming contribute to improving physical activity levels and health outcomes in children? Pediatrics 2009, 124, 763–771. [Google Scholar] [CrossRef]
- Kracht, C.L.; Joseph, E.D.; Staiano, A.E. Video games, obesity, and children. Curr. Obes. Rep. 2020, 9, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Madsen, K.A.; Yen, S.; Wlasiuk, L.; Newman, T.B.; Lustig, R. Feasibility of a dance videogame to promote weight loss among overweight children and adolescents. Arch. Pediatr. Adolesc. Med. 2007, 161, 105–107. [Google Scholar] [CrossRef]
- Ni Mhurchu, C.; Maddison, R.; Jiang, Y.; Jull, A.; Prapavessis, H.; Rodgers, A. Couch potatoes to jumping beans: A pilot study of the effect of active video games on physical activity in children. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 8. [Google Scholar] [CrossRef]
- Sinclair, J.; Hingston, P.; Masek, M.; Nosaka, K. Using a virtual body to aid in exergaming system development. IEEE Comput. Graph. Appl. 2009, 29, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Vaghetti, C.; Monteiro-Junior, R.; Finco, M.; Reategui, E.; Botelho, S. Exergames experience in physical education: A review. Phys. Cult. Sport. Stud. Res. 2018, 78, 23–32. [Google Scholar] [CrossRef]
- World Health Organization. How to Keep Your Child Safe Online While Stuck at Home during the COVID-19 Outbreak. Available online: https://www.Who.Int/News-Room/Campaigns/Connecting-the-World-to-Combat-Coronavirus/Healthyathome/Healthyathome---Physical-Activity (accessed on 11 October 2021).
- Natalucci, V.; Carnevale Pellino, V.; Barbieri, E.; Vandoni, M. Is It important to perform physical activity during coronavirus pandemic (COVID-19)? driving action for a correct exercise plan. Front. Public Health 2020, 8, 602020. [Google Scholar] [CrossRef] [PubMed]
- Italian Government. Decreto-Legge Convertito Con Modificazioni dalla L 22 Maggio 2020. n. 35 (in G.U. 23/05/2020, n. 132). 2020. Available online: www.Gazzettaufficiale.It/Eli/Id/2020/03/25/20G00035/SgC (accessed on 22 July 2020).
- Ministry of Health. “COVID-19 e over 65: Attività Fisica in Casa Contro i Rischi Della Sedentarietà”. Available online: https://www.Salute.Gov.It/Portale/Nuovocoronavirus/DettaglioNotizieNuovoCoronavirus.Jsp?Lingua=italiano&menu=notizie&p=dalministero&id=4388 (accessed on 2 November 2021).
- “Covid-19, Attività Fisica per Gli Adolescenti a Casa”. Available online: https://www.Salute.Gov.It/Portale/Nuovocoronavirus/DettaglioNotizieNuovoCoronavirus.Jsp?Lingua=italiano&menu=notizie&p=dalministero&id=4319 (accessed on 2 November 2021).
- Zhu, W. Should, and how can, exercise be done during a coronavirus outbreak? An interview with Dr. Jeffrey A. Woods. J. Sport Health Sci. 2020, 9, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Bian, J.; Leavitt, T.; Vincent, H.K.; Vander Zalm, L.; Teurlings, T.L.; Smith, M.D.; Modave, F. Assessing the quality of mobile exercise apps based on the american college of sports medicine guidelines: A reliable and valid scoring instrument. J. Med. Internet Res. 2017, 19, e67. [Google Scholar] [CrossRef] [PubMed]
- Lopez Martinez, J.J.; Rodríguez-Roiz, J.M.; Salcedo Cánovas, C. Musculoskeletal injuries secondary to exercise during confinement by the pandemic COVID-19. Med. Clin. 2020, 155, 221–222. [Google Scholar] [CrossRef]
- Unicef Keeping the World’s Children Learning through COVID-19. Available online: https://www.Unicef.Org/Coronavirus/Keeping-Worlds-Children-Learning-through-Covid-19 (accessed on 9 November 2021).
- Hammami, A.; Harrabi, B.; Mohr, M.; Krustrup, P. Physical activity and coronavirus disease 2019 (COVID-19): Specific recommendations for home-based physical training. Manag. Sport Leis. 2020. [Google Scholar] [CrossRef]
- Deterding, S.; Sicart, M.; Nacke, L.; O’Hara, K.; Dixon, D. Gamification: Using Game Design Elements in Non-Gaming Contexts. In Proceedings of the 2011 Annual Conference Extended Abstracts on Human Factors in Computing Systems, Vancouver, BC, Canada, 7 May 2011; Volume 66, pp. 2425–2428. [Google Scholar]
- Blok, A.C.; Valley, T.S.; Abbott, P. Gamification for family engagement in lifestyle interventions: A systematic review. Prev. Sci. 2021, 22, 831–844. [Google Scholar] [CrossRef]
- Dong, H.; Yang, F.; Lu, X.; Hao, W. Internet addiction and related psychological factors among children and adolescents in china during the coronavirus disease 2019 (COVID-19) epidemic. Front. Psychiatry 2020, 11, 00751. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Chen, I.-H.; O’Brien, K.S.; Latner, J.D.; Lin, C.-Y. Psychological distress and internet-related behaviors between schoolchildren with and without overweight during the COVID-19 outbreak. Int. J. Obes. 2021, 45, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Alimoradi, Z.; Golboni, F.; Griffiths, M.D.; Broström, A.; Lin, C.-Y.; Pakpour, A.H. Weight-related stigma and psychological distress: A systematic review and meta-analysis. Clin. Nutr. 2020, 39, 2001–2013. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.L.; Liu, D.X.; Jiang, H.; Pan, F.; Ho, C.S.; Ho, R.C. The effects of high-fat-diet combined with chronic unpredictable mild stress on depression-like behavior and leptin/leprb in male rats. Sci. Rep. 2016, 6, 35239. [Google Scholar] [CrossRef] [PubMed]
- Lucini, D.; Gandolfi, C.E.; Antonucci, C.; Cavagna, A.; Valzano, E.; Botta, E.; Chiari, M.; Mameli, L.; Nahum, M.; Brambilla, M.M.; et al. #StayHomeStayFit: UNIMI’s approach to online healthy lifestyle promotion during the COVID-19 pandemic. Acta Biomed. 2020, 91, e2020037. [Google Scholar] [CrossRef] [PubMed]
- Fanelli, C.; Pippi, R. Is physical activity a necessary element during italian coronavirus disease emergency? Yes or no debate. J. Hum. Sport Exerc. 2021, 17. [Google Scholar] [CrossRef]
- Stay Physically Active during Self-Quarantine. Available online: https://www.Euro.Who.Int/En/Health-Topics/Healthemergencies/Coronavirus-Covid-19/Technical-Guidance/Stay-Physically-Active-during-Self-Quarantine (accessed on 12 October 2021).
- NHS Inform. Coronavirus (COVID-19): PA. Available online: https://www.Nhsinform.Scot/Illnesses-Andconditions/Infections-and-Poisoning/Coronavirus-Covid-19/Healthy-Living/Coronavirus-Covid-19-Physical-Activity (accessed on 12 October 2021).
- Cdc. How to Be Physically Active While Social Distancing. Available online: https://www.Cdc.Gov/Physicalactivity/How-to-Bephysically-Active-While-Social-Distancing.Html (accessed on 12 October 2021).
- Bland, K.A.; Bigaran, A.; Campbell, K.L.; Trevaskis, M.; Zopf, E.M. Exercising in isolation? The role of telehealth in exercise oncology during the COVID-19 pandemic and beyond. Phys. Ther. 2020, 100, 1713–1716. [Google Scholar] [CrossRef] [PubMed]
- Di Blasio, A.; Morano, T.; Lancia, F.; Viscioni, G.; di Iorio, A.; Grossi, S.; Cianchetti, E.; Pippi, R.; Gobbo, S.; Bergamin, M.; et al. Effects of activity tracker-based counselling and live-web exercise on breast cancer survivors’ sleep and waking time during Italy’s COVID-19 lockdown. Home Health Care Serv. Q 2021, 1–19. [Google Scholar] [CrossRef]
- Cugusi, L.; Prosperini, L.; Mura, G. Exergaming for quality of life in persons living with chronic diseases: A systematic review and meta-analysis. PM&R 2020, 13, 756–780. [Google Scholar] [CrossRef]
- Lee, M.K.; Yun, Y.H.; Park, H.-A.; Lee, E.S.; Jung, K.H.; Noh, D.-Y. A Web-based self-management exercise and diet intervention for breast cancer survivors: Pilot randomized controlled trial. Int. J. Nurs. Stud. 2014, 51, 1557–1567. [Google Scholar] [CrossRef]
- Ariza-Garcia, A.; Lozano-Lozano, M.; Galiano-Castillo, N.; Postigo-Martin, P.; Arroyo-Morales, M.; Cantarero-Villanueva, I. A web-based exercise system (e-cuidatechemo) to counter the side effects of chemotherapy in patients with breast cancer: Randomized controlled trial. J. Med. Internet Res. 2019, 21, e14418. [Google Scholar] [CrossRef]
- Weiss, M.R.; Kipp, L.E.; Riley, A. “A piece of sanity in the midst of insane times”: Girls on the run programming to promote physical activity and psychosocial well-being during the COVID-19 pandemic. Front. Public Health 2021, 9, 729291. [Google Scholar] [CrossRef]
- American College of Sports Medicine Keeping Children Active during the Coronavirus Pandemic. Available online: https://Exerciseismedicine.Org/Wp-Content/Uploads/2021/02/EIM_Rx-for-Health_-Keeping-Children-Active-During-Coronavirus-Pandemic.Pdf (accessed on 2 November 2021).
- Cosmic Kids. Available online: https://Cosmickids.Com (accessed on 9 November 2021).
- GoNoodle. Available online: https://www.Gonoodle.Com (accessed on 2 November 2021).
- Online Physical Education Network (OPEN). Available online: https://openphysed.org (accessed on 2 November 2021).
- School at Home with the AHA. Available online: https://www.Heart.Org/En/Professional/Educator/Coronavirus-Tips-for-Parents-and-Kids (accessed on 2 November 2021).
- Move More Together. Available online: https://www.Heart.Org/En/Healthy-Living/Fitness/Fitness-Basics/Move-More-Together (accessed on 2 November 2021).
- Yu, J.; Jee, Y. Analysis of online classes in physical education during the COVID-19 pandemic. Educ. Sci. 2021, 11, 3. [Google Scholar] [CrossRef]
- Jeong, H.-C.; So, W.-Y. Difficulties of online physical education classes in middle and high school and an efficient operation plan to address them. Int. J. Environ. Res. Public Health 2020, 17, 7279. [Google Scholar] [CrossRef] [PubMed]
- Laar, R.A.; Ashraf, M.A.; Ning, J.; Ji, P.; Fang, P.; Yu, T.; Khan, M.N. Performance, Health, and Psychological Challenges Faced by Students of Physical Education in Online Learning during COVID-19 Epidemic: A Qualitative Study in China. Healthcare 2021, 9, 1030. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, E.M.; Urtel, M.; Webster, C.A.; McMullen, J.; Culp, B. Virtual Physical Education During COVID-19: Exploring Future Directions for Equitable Online Learning Tools. Front. Sports Act. Living 2021, 3, 716566. [Google Scholar] [CrossRef]
| WHO 2006 | WHO 2006 | WHO 2007 | |
|---|---|---|---|
| Age | 0–2 years | 2–5 years | 5–18 years |
| Index | Weight-to-length ratio | BMI | BMI |
| >97th percentile | Overweight | Overweight | Obesity |
| >99th percentile | Obesity | Obesity | Severe obesity |
| Authors (Year) | Country | Population | Approach | Resources | Main Findings |
|---|---|---|---|---|---|
| Johnson et al. (2018) [131] | Australia | Children with cerebral palsy | Trial | Online individualized exercise program with supervision (16 weeks) | Ameliorated cognitive functions; increased motor function in upper limbs. |
| Chen JJ et al. (2018) [133] | USA | Children with cystic fibrosis | Trial | Online exercise training with wearable devices (16 weeks) | Increased adherence to PA practice without cross-infection risks |
| Cosano et al. (2020) [132] | Spain | Children with cancer | Study Protocol | Supervised online exercise program (12 weeks) | Improved on bone health |
| Chen H et al. (2017) [136] | USA | Children with obesity | Trial | Exergames | Reduced the sedentary behaviors; improved sport engagement and reduced risk to develop respiratory and cardiovascular pathologies. |
| Lamboglia et al. (2013) [140] | Brazil | Children with obesity | Review | Exergames | Contrasted the childhood obesity rising PA levels, energy expenditure, maximal oxygen uptake, heart rate, and decreasing waist circumference. |
| Bethea et al. (2012) [142] | USA | Children with obesity | Trial | Tele-exercise (30 weeks) | Enhanced cardiovascular fitness |
| Calcaterra et al. (2013) [60] | Italy | Children with obesity | Trial | Exergames both with supervision and without (12 weeks) | Enhanced of body composition, cardiorespiratory fitness, and metabolic profile. |
| Murphy et al. (2019) [143] | UK | Children with obesity | Review | Tele-exercise | Improved total exercise time and VO2 peak, with a reduction of body weight. |
| Daley et al. (2009) [144] | UK | Children with obesity | Review | Exergames (12 weeks) | Increased energy consumption during leisure time. |
| WHO Campaign #HealthyatHome (2020) [150] | Worldwide | Children (aged 5 to 17 years old) | Campaign | Resources posted online such as video and channels | No data available |
| Calcaterra et al. (2021) [79] | Italy | Children with type 1 diabetes (aged 5 to 17 years old | Trial | “LAMAJunior” channels with online exercise training | Reduced sedentary habits with shorter beaks of PA practice during the day |
| Weiss et al. (2021) [176] | USA | Children and young adults | Trial | “Girls on the Run” | PA online program to promote active lifestyle and psychosocial well-being |
| ACSM Campaign (2020) [177] | USA | Children and young adults | Campaign | Active gaming and other web resources | To increase active lifestyle |
| Cosmickids Campaign (2021) [178] | No available | Children | Campaign | Yoga and Mindfulness video | To help kids build their mental and physical strength and confidence |
| GoNoodle (2021) [179] | USA | Primary school children | Campaign | Online lessons | To enhance personal and community wellness and mental and physical health |
| School at Home with the AHA (2020) [181] | USA | Children and young adults | Campaign | Online advice and resources | To promote an active lifestyle |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vandoni, M.; Codella, R.; Pippi, R.; Carnevale Pellino, V.; Lovecchio, N.; Marin, L.; Silvestri, D.; Gatti, A.; Magenes, V.C.; Regalbuto, C.; et al. Combatting Sedentary Behaviors by Delivering Remote Physical Exercise in Children and Adolescents with Obesity in the COVID-19 Era: A Narrative Review. Nutrients 2021, 13, 4459. https://doi.org/10.3390/nu13124459
Vandoni M, Codella R, Pippi R, Carnevale Pellino V, Lovecchio N, Marin L, Silvestri D, Gatti A, Magenes VC, Regalbuto C, et al. Combatting Sedentary Behaviors by Delivering Remote Physical Exercise in Children and Adolescents with Obesity in the COVID-19 Era: A Narrative Review. Nutrients. 2021; 13(12):4459. https://doi.org/10.3390/nu13124459
Chicago/Turabian StyleVandoni, Matteo, Roberto Codella, Roberto Pippi, Vittoria Carnevale Pellino, Nicola Lovecchio, Luca Marin, Dario Silvestri, Alessandro Gatti, Vittoria Carlotta Magenes, Corrado Regalbuto, and et al. 2021. "Combatting Sedentary Behaviors by Delivering Remote Physical Exercise in Children and Adolescents with Obesity in the COVID-19 Era: A Narrative Review" Nutrients 13, no. 12: 4459. https://doi.org/10.3390/nu13124459
APA StyleVandoni, M., Codella, R., Pippi, R., Carnevale Pellino, V., Lovecchio, N., Marin, L., Silvestri, D., Gatti, A., Magenes, V. C., Regalbuto, C., Fabiano, V., Zuccotti, G., & Calcaterra, V. (2021). Combatting Sedentary Behaviors by Delivering Remote Physical Exercise in Children and Adolescents with Obesity in the COVID-19 Era: A Narrative Review. Nutrients, 13(12), 4459. https://doi.org/10.3390/nu13124459












