COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review
Abstract
1. Introduction
2. Methods
3. Epidemiology and Clinical Characteristics of COVID-19 in Childhood and Adolescence
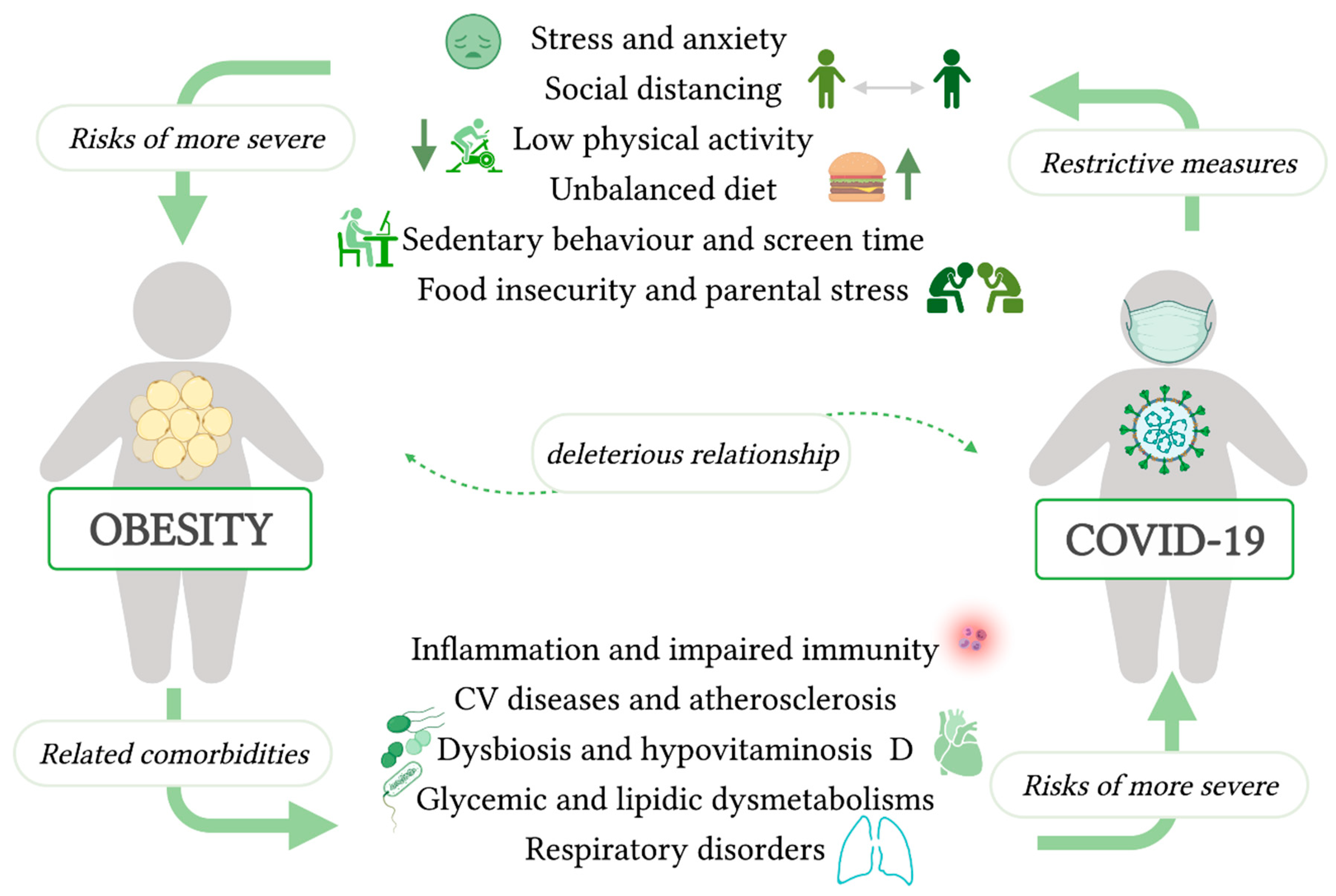
4. The Effects of COVID-19 on Weight Gain and Obesity
5. The Effects of Obesity on COVID-19
6. Interactions of Nutrition and COVID-19 Infection
7. Changes in Nutrition Behavior during COVID-19 and The Effect on Weight Gain
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khan, M.; Adil, S.F.; Alkhathlan, H.Z.; Tahir, M.N.; Saif, S.; Khan, M.; Khan, S.T. COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules 2021, 26, 39. [Google Scholar] [CrossRef]
- Tornaghi, M.; Lovecchio, N.; Vandoni, M.; Chirico, A.; Codella, R. Physical Activity Levels across COVID-19 Outbreak in Youngsters of Northwestern Lombardy. J. Sports Med. Phys. Fit. 2021, 61, 971–976. [Google Scholar] [CrossRef]
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiology of COVID-19 Among Children in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef]
- Leidman, E.; Duca, L.M.; Omura, J.D.; Proia, K.; Stephens, J.W.; Sauber-Schatz, E.K. COVID-19 Trends Among Persons Aged 0–24 Years—United States, March 1–December 12, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, N.M.; Selim, L.A. Characterisation of COVID-19 Pandemic in Paediatric Age Group: A Systematic Review and Meta-Analysis. J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol. 2020, 128, 104395. [Google Scholar] [CrossRef]
- Tai, D.B.G.; Shah, A.; Doubeni, C.A.; Sia, I.G.; Wieland, M.L. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clin. Infect. Dis. 2021, 72, 703–706. [Google Scholar] [CrossRef]
- Kara, A.A.; Böncüoğlu, E.; Kıymet, E.; Arıkan, K.Ö.; Şahinkaya, Ş.; Düzgöl, M.; Cem, E.; Çelebi, M.; Ağın, H.; Bayram, S.N.; et al. Evaluation of Predictors of Severe-moderate COVID-19 Infections at Children: A Review of 292 Children. J. Med. Virol. 2021, 93, 6634–6640. [Google Scholar] [CrossRef]
- Shekerdemian, L.S.; Mahmood, N.R.; Wolfe, K.K.; Riggs, B.J.; Ross, C.E.; McKiernan, C.A.; Heidemann, S.M.; Kleinman, L.C.; Sen, A.I.; Hall, M.W.; et al. Characteristics and Outcomes of Children with Coronavirus Disease 2019 (COVID-19) Infection Admitted to US and Canadian Pediatric Intensive Care Units. JAMA Pediatr. 2020, 174, 868. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.T.; Denniss, A.R. An Introduction to Writing Narrative and Systematic Reviews—Tasks, Tips and Traps for Aspiring Authors. Heart Lung Circ. 2018, 27, 893–898. [Google Scholar] [CrossRef]
- Garazzino, S.; Lo Vecchio, A.; Pierantoni, L.; Calò Carducci, F.I.; Marchetti, F.; Meini, A.; Castagnola, E.; Vergine, G.; Donà, D.; Bosis, S.; et al. Epidemiology, Clinical Features and Prognostic Factors of Pediatric SARS-CoV-2 Infection: Results from an Italian Multicenter Study. Front. Pediatr. 2021, 9, 649358. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.M.; Mytton, O.T.; Bonell, C.; Melendez-Torres, G.J.; Ward, J.; Hudson, L.; Waddington, C.; Thomas, J.; Russell, S.; van der Klis, F.; et al. Susceptibility to SARS-CoV-2 Infection Among Children and Adolescents Compared with Adults: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2021, 175, 143–156. [Google Scholar] [CrossRef]
- Harman, K.; Verma, A.; Cook, J.; Radia, T.; Zuckerman, M.; Deep, A.; Dhawan, A.; Gupta, A. Ethnicity and COVID-19 in Children with Comorbidities. Lancet Child Adolesc. Health 2020, 4, e24–e25. [Google Scholar] [CrossRef]
- Mackey, K.; Ayers, C.K.; Kondo, K.K.; Saha, S.; Advani, S.M.; Young, S.; Spencer, H.; Rusek, M.; Anderson, J.; Veazie, S.; et al. Racial and Ethnic Disparities in COVID-19–Related Infections, Hospitalizations, and Deaths: A Systematic Review. Ann. Intern. Med. 2021, 174, 362–373. [Google Scholar] [CrossRef]
- She, J.; Liu, L.; Liu, W. COVID-19 Epidemic: Disease Characteristics in Children. J. Med. Virol. 2020, 92, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Rinaldi, E.; Zusi, C.; Beatrice, G.; Saccomani, M.D.; Dalbeni, A. Coronavirus Disease 2019 (COVID-19) in Children and/or Adolescents: A Meta-Analysis. Pediatr. Res. 2021, 89, 733–737. [Google Scholar] [CrossRef]
- Cui, X.; Zhao, Z.; Zhang, T.; Guo, W.; Guo, W.; Zheng, J.; Zhang, J.; Dong, C.; Na, R.; Zheng, L.; et al. A Systematic Review and Meta-Analysis of Children with Coronavirus Disease 2019 (COVID-19). J. Med. Virol. 2021, 93, 1057–1069. [Google Scholar] [CrossRef]
- Yasuhara, J.; Kuno, T.; Takagi, H.; Sumitomo, N. Clinical Characteristics of COVID-19 in Children: A Systematic Review. Pediatr. Pulmonol. 2020, 55, 2565–2575. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulou, D.; Spyridis, N.; Dasoula, F.; Krepis, P.; Eleftheriou, E.; Liaska, M.; Servos, G.; Maritsi, D.; Tsolia, M. Pericarditis as the Main Clinical Manifestation of COVID-19 in Adolescents. Pediatr. Infect. Dis. J. 2021, 40, e197–e199. [Google Scholar] [CrossRef] [PubMed]
- Irfan, O.; Muttalib, F.; Tang, K.; Jiang, L.; Lassi, Z.S.; Bhutta, Z. Clinical Characteristics, Treatment and Outcomes of Paediatric COVID-19: A Systematic Review and Meta-Analysis. Arch. Dis. Child. 2021, 106, 440. [Google Scholar] [CrossRef] [PubMed]
- Chao, J.Y.; Derespina, K.R.; Herold, B.C.; Goldman, D.L.; Aldrich, M.; Weingarten, J.; Ushay, H.M.; Cabana, M.D.; Medar, S.S. Clinical Characteristics and Outcomes of Hospitalized and Critically Ill Children and Adolescents with Coronavirus Disease 2019 at a Tertiary Care Medical Center in New York City. J. Pediatr. 2020, 223, 14–19.e2. [Google Scholar] [CrossRef]
- Liguoro, I.; Pilotto, C.; Bonanni, M.; Ferrari, M.E.; Pusiol, A.; Nocerino, A.; Vidal, E.; Cogo, P. SARS-COV-2 Infection in Children and Newborns: A Systematic Review. Eur. J. Pediatr. 2020, 179, 1029–1046. [Google Scholar] [CrossRef]
- Sankar, J.; Dhochak, N.; Kabra, S.K.; Lodha, R. COVID-19 in Children: Clinical Approach and Management. Indian J. Pediatr. 2020, 87, 433–442. [Google Scholar] [CrossRef]
- Tsankov, B.K.; Allaire, J.M.; Irvine, M.A.; Lopez, A.A.; Sauvé, L.J.; Vallance, B.A.; Jacobson, K. Severe COVID-19 Infection and Pediatric Comorbidities: A Systematic Review and Meta-Analysis. Int. J. Infect. Dis. 2021, 103, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Zachariah, P.; Johnson, C.L.; Halabi, K.C.; Ahn, D.; Sen, A.I.; Fischer, A.; Banker, S.L.; Giordano, M.; Manice, C.S.; Diamond, R.; et al. Epidemiology, Clinical Features, and Disease Severity in Patients with Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA Pediatr. 2020, 174, e202430. [Google Scholar] [CrossRef]
- Caussy, C.; Wallet, F.; Laville, M.; Disse, E. Obesity Is Associated with Severe Forms of COVID-19. Obesity 2020, 28, 1175. [Google Scholar] [CrossRef]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M.; et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Unamuno, X.; Gómez-Ambrosi, J.; Rodríguez, A.; Becerril, S.; Frühbeck, G.; Catalán, V. Adipokine Dysregulation and Adipose Tissue Inflammation in Human Obesity. Eur. J. Clin. Investig. 2018, 48, e12997. [Google Scholar] [CrossRef]
- Zeng, F.; Huang, Y.; Guo, Y.; Yin, M.; Chen, X.; Xiao, L.; Deng, G. Association of Inflammatory Markers with the Severity of COVID-19: A Meta-Analysis. Int. J. Infect. Dis. 2020, 96, 467–474. [Google Scholar] [CrossRef]
- Chiappetta, S.; Sharma, A.M.; Bottino, V.; Stier, C. COVID-19 and the Role of Chronic Inflammation in Patients with Obesity. Int. J. Obes. 2020, 44, 1790–1792. [Google Scholar] [CrossRef]
- Ritter, A.; Kreis, N.-N.; Louwen, F.; Yuan, J. Obesity and COVID-19: Molecular Mechanisms Linking Both Pandemics. Int. J. Mol. Sci. 2020, 21, 5793. [Google Scholar] [CrossRef] [PubMed]
- Nogueira-de-Almeida, C.A.; Del Ciampo, L.A.; Ferraz, I.S.; Del Ciampo, I.R.L.; Contini, A.A.; Ued, F.d.V. COVID-19 and Obesity in Childhood and Adolescence: A Clinical Review. J. Pediatr. (Rio J.) 2020, 96, 546–558. [Google Scholar] [CrossRef]
- Nogueira-de-Almeida, C.A. We Need to Look at the Comorbidities of Obesity during Childhood and Adolescence. Biomed. J. Sci. Tech. Res. 2017, 1, 1931–1932. [Google Scholar] [CrossRef][Green Version]
- Zhang, F.; Xiong, Y.; Wei, Y.; Hu, Y.; Wang, F.; Li, G.; Liu, K.; Du, R.; Wang, C.; Zhu, W. Obesity Predisposes to the Risk of Higher Mortality in Young COVID-19 Patients. J. Med. Virol. 2020, 92, 2536–2542. [Google Scholar] [CrossRef]
- Kass, D.A.; Duggal, P.; Cingolani, O. Obesity Could Shift Severe COVID-19 Disease to Younger Ages. Lancet 2020, 395, 1544–1545. [Google Scholar] [CrossRef]
- Williams, N.; Radia, T.; Harman, K.; Agrawal, P.; Cook, J.; Gupta, A. COVID-19 Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Children and Adolescents: A Systematic Review of Critically Unwell Children and the Association with Underlying Comorbidities. Eur. J. Pediatr. 2021, 180, 689–697. [Google Scholar] [CrossRef]
- Feldman, E.L.; Savelieff, M.G.; Hayek, S.S.; Pennathur, S.; Kretzler, M.; Pop-Busui, R. COVID-19 and Diabetes: A Collision and Collusion of Two Diseases. Diabetes 2020, 69, 2549–2565. [Google Scholar] [CrossRef]
- Kostopoulou, E.; Güemes, M.; Shah, P. COVID-19 in Children and Adolescents with EndocrineConditions. Horm. Metab. Res. 2020, 52, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Marlais, M.; Wlodkowski, T.; Vivarelli, M.; Pape, L.; Tönshoff, B.; Schaefer, F.; Tullus, K. The Severity of COVID-19 in Children on Immunosuppressive Medication. Lancet Child Adolesc. Health 2020, 4, e17–e18. [Google Scholar] [CrossRef]
- Galeotti, C.; Bayry, J. Autoimmune and Inflammatory Diseases Following COVID-19. Nat. Rev. Rheumatol. 2020, 16, 413–414. [Google Scholar] [CrossRef]
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory Shock in Children during COVID-19 Pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef]
- Nakra, N.; Blumberg, D.; Herrera-Guerra, A.; Lakshminrusimha, S. Multi-System Inflammatory Syndrome in Children (MIS-C) Following SARS-CoV-2 Infection: Review of Clinical Presentation, Hypothetical Pathogenesis, and Proposed Management. Children 2020, 7, 69. [Google Scholar] [CrossRef]
- Kaushik, S.; Aydin, S.I.; Derespina, K.R.; Bansal, P.B.; Kowalsky, S.; Trachtman, R.; Gillen, J.K.; Perez, M.M.; Soshnick, S.H.; Conway, E.E.; et al. Multisystem Inflammatory Syndrome in Children Associated with Severe Acute Respiratory Syndrome Coronavirus 2 Infection (MIS-C): A Multi-Institutional Study from New York City. J. Pediatr. 2020, 224, 24–29. [Google Scholar] [CrossRef]
- Feldstein, L.R.; Tenforde, M.W.; Friedman, K.G.; Newhams, M.; Rose, E.B.; Dapul, H.; Soma, V.L.; Maddux, A.B.; Mourani, P.M.; Bowens, C.; et al. Characteristics and Outcomes of US Children and Adolescents with Multisystem Inflammatory Syndrome in Children (MIS-C) Compared with Severe Acute COVID-19. JAMA 2021, 325, 1074. [Google Scholar] [CrossRef]
- On Behalf of the Rheumatology Study Group of the Italian Society of Pediatrics; Cattalini, M.; Taddio, A.; Bracaglia, C.; Cimaz, R.; Paolera, S.D.; Filocamo, G.; La Torre, F.; Lattanzi, B.; Marchesi, A.; et al. Childhood Multisystem Inflammatory Syndrome Associated with COVID-19 (MIS-C): A Diagnostic and Treatment Guidance from the Rheumatology Study Group of the Italian Society of Pediatrics. Ital. J. Pediatr. 2021, 47, 24. [Google Scholar] [CrossRef] [PubMed]
- Hameed, S.; Elbaaly, H.; Reid, C.E.L.; Santos, R.M.F.; Shivamurthy, V.; Wong, J.; Jogeesvaran, K.H. Spectrum of Imaging Findings at Chest Radiography, US, CT, and MRI in Multisystem Inflammatory Syndrome in Children Associated with COVID-19. Radiology 2021, 298, E1–E10. [Google Scholar] [CrossRef] [PubMed]
- Ramcharan, T.; Nolan, O.; Lai, C.Y.; Prabhu, N.; Krishnamurthy, R.; Richter, A.G.; Jyothish, D.; Kanthimathinathan, H.K.; Welch, S.B.; Hackett, S.; et al. Paediatric Inflammatory Multisystem Syndrome: Temporally Associated with SARS-CoV-2 (PIMS-TS): Cardiac Features, Management and Short-Term Outcomes at a UK Tertiary Paediatric Hospital. Pediatr. Cardiol. 2020, 41, 1391–1401. [Google Scholar] [CrossRef]
- Feldstein, L.R.; Rose, E.B.; Horwitz, S.M.; Collins, J.P.; Newhams, M.M.; Son, M.B.F.; Newburger, J.W.; Kleinman, L.C.; Heidemann, S.M.; Martin, A.A.; et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N. Engl. J. Med. 2020, 383, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Davies, P.; Evans, C.; Kanthimathinathan, H.K.; Lillie, J.; Brierley, J.; Waters, G.; Johnson, M.; Griffiths, B.; du Pré, P.; Mohammad, Z.; et al. Intensive Care Admissions of Children with Paediatric Inflammatory Multisystem Syndrome Temporally Associated with SARS-CoV-2 (PIMS-TS) in the UK: A Multicentre Observational Study. Lancet Child Adolesc. Health 2020, 4, 669–677. [Google Scholar] [CrossRef]
- Wolfler, A.; Mannarino, S.; Giacomet, V.; Camporesi, A.; Zuccotti, G. Acute Myocardial Injury: A Novel Clinical Pattern in Children with COVID-19. Lancet Child Adolesc. Health 2020, 4, e26–e27. [Google Scholar] [CrossRef]
- Greene, A.G.; Saleh, M.; Roseman, E.; Sinert, R. Toxic Shock-like Syndrome and COVID-19: Multisystem Inflammatory Syndrome in Children (MIS-C). Am. J. Emerg. Med. 2020, 38, 2492.e5–2492.e6. [Google Scholar] [CrossRef]
- Radia, T.; Williams, N.; Agrawal, P.; Harman, K.; Weale, J.; Cook, J.; Gupta, A. Multi-System Inflammatory Syndrome in Children & Adolescents (MIS-C): A Systematic Review of Clinical Features and Presentation. Paediatr. Respir. Rev. 2021, 38, 51–57. [Google Scholar] [CrossRef]
- Bautista-Rodriguez, C.; Sanchez-de-Toledo, J.; Clark, B.C.; Herberg, J.; Bajolle, F.; Randanne, P.C.; Salas-Mera, D.; Foldvari, S.; Chowdhury, D.; Munoz, R.; et al. Multisystem Inflammatory Syndrome in Children: An International Survey. Pediatrics 2021, 147, e2020024554. [Google Scholar] [CrossRef] [PubMed]
- Abrams, J.Y.; Oster, M.E.; Godfred-Cato, S.E.; Bryant, B.; Datta, S.D.; Campbell, A.P.; Leung, J.W.; Tsang, C.A.; Pierce, T.J.; Kennedy, J.L.; et al. Factors Linked to Severe Outcomes in Multisystem Inflammatory Syndrome in Children (MIS-C) in the USA: A Retrospective Surveillance Study. Lancet Child Adolesc. Health 2021, 5, 323–331. [Google Scholar] [CrossRef]
- Calcaterra, V.; Bosoni, P.; Dilillo, D.; Mannarino, S.; Fiori, L.; Fabiano, V.; Carlucci, P.; Di Profio, E.; Verduci, E.; Mameli, C.; et al. Impaired Glucose-Insulin Metabolism in Multisystem Inflammatory Syndrome Related to SARS-CoV-2 in Children. Children 2021, 8, 384. [Google Scholar] [CrossRef]
- Marik, P.E.; Bellomo, R. Stress Hyperglycemia: An Essential Survival Response! Crit. Care 2013, 17, 305. [Google Scholar] [CrossRef]
- Shrestha, E.; Charkviani, M.; Musurakis, C.; Kansakar, A.R.; Devkota, A.; Banjade, R.; Pudasainee, P.; Chitrakar, S.; Sharma, A.; Sous, M.; et al. Type 2 Diabetes Is Associated with Increased Risk of Critical Respiratory Illness in Patients COVID-19 in a Community Hospital. Obes. Med. 2021, 22, 100316. [Google Scholar] [CrossRef]
- Jia, X.; Gesualdo, P.; Geno Rasmussen, C.; Alkanani, A.A.; He, L.; Dong, F.; Rewers, M.J.; Michels, A.W.; Yu, L. Prevalence of SARS-CoV-2 Antibodies in Children and Adults with Type 1 Diabetes. Diabetes Technol. Ther. 2021, 23, 517–521. [Google Scholar] [CrossRef]
- Nielsen-Saines, K.; Li, E.; Olivera, A.M.; Martin-Blais, R.; Bulut, Y. Case Report: Insulin-Dependent Diabetes Mellitus and Diabetic Keto-Acidosis in a Child With COVID-19. Front. Pediatr. 2021, 9, 628810. [Google Scholar] [CrossRef]
- Hoste, L.; Van Paemel, R.; Haerynck, F. Multisystem Inflammatory Syndrome in Children Related to COVID-19: A Systematic Review. Eur. J. Pediatr. 2021, 180, 2019–2034. [Google Scholar] [CrossRef] [PubMed]
- Chams, N.; Chams, S.; Badran, R.; Shams, A.; Araji, A.; Raad, M.; Mukhopadhyay, S.; Stroberg, E.; Duval, E.J.; Barton, L.M.; et al. COVID-19: A Multidisciplinary Review. Front. Public Health 2020, 8, 383. [Google Scholar] [CrossRef]
- Azevedo, R.B.; Botelho, B.G.; de Hollanda, J.V.G.; Ferreira, L.V.L.; de Andrade, L.Z.J.; Oei, S.S.M.L.; Mello, T.d.S.; Muxfeldt, E.S. Covid-19 and the Cardiovascular System: A Comprehensive Review. J. Hum. Hypertens. 2021, 35, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Browne, N.T.; Snethen, J.A.; Greenberg, C.S.; Frenn, M.; Kilanowski, J.F.; Gance-Cleveland, B.; Burke, P.J.; Lewandowski, L. When Pandemics Collide: The Impact of COVID-19 on Childhood Obesity. J. Pediatr. Nurs. 2021, 56, 90–98. [Google Scholar] [CrossRef]
- Yang, S.; Guo, B.; Ao, L.; Yang, C.; Zhang, L.; Zhou, J.; Jia, P. Obesity and Activity Patterns before and during COVID-19 Lockdown among Youths in China. Clin. Obes. 2020, 10, e12416. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Brooks, C.G.; Spencer, J.R.; Sprafka, J.M.; Roehl, K.A.; Ma, J.; Londhe, A.A.; He, F.; Cheng, A.; Brown, C.A.; Page, J. Pediatric BMI Changes during COVID-19 Pandemic: An Electronic Health Record-Based Retrospective Cohort Study. EClinicalMedicine 2021, 38, 101026. [Google Scholar] [CrossRef] [PubMed]
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Obesity in Children and Adolescents during COVID-19 Pandemic. Children 2021, 8, 135. [Google Scholar] [CrossRef]
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The Impact of Lockdown During the COVID-19 Outbreak on Dietary Habits in Various Population Groups: A Scoping Review. Front. Nutr. 2021, 8, 626432. [Google Scholar] [CrossRef]
- Ruiz-Roso, M.B.; de Carvalho Padilha, P.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Arantes Ferreira Peres, W.; Martorell, M.; Aires, M.T.; de Oliveira Cardoso, L.; et al. Covid-19 Confinement and Changes of Adolescent’s Dietary Trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar] [CrossRef]
- Adams, E.L.; Caccavale, L.J.; Smith, D.; Bean, M.K. Food Insecurity, the Home Food Environment, and Parent Feeding Practices in the Era of COVID-19. Obesity 2020, 28, 2056–2063. [Google Scholar] [CrossRef]
- Naja, F.; Hamadeh, R. Nutrition amid the COVID-19 Pandemic: A Multi-Level Framework for Action. Eur. J. Clin. Nutr. 2020, 74, 1117–1121. [Google Scholar] [CrossRef]
- Dunton, G.F.; Do, B.; Wang, S.D. Early Effects of the COVID-19 Pandemic on Physical Activity and Sedentary Behavior in Children Living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef]
- Calcaterra, V.; Vandoni, M.; Pellino, V.C.; Cena, H. Special Attention to Diet and Physical Activity in Children and Adolescents with Obesity during the Coronavirus Disease-2019 Pandemic. Front. Pediatr. 2020, 8, 407. [Google Scholar] [CrossRef] [PubMed]
- Ruíz-Roso, M.B.; de Carvalho Padilha, P.; Matilla-Escalante, D.C.; Brun, P.; Ulloa, N.; Acevedo-Correa, D.; Arantes Ferreira Peres, W.; Martorell, M.; Rangel Bousquet Carrilho, T.; de Oliveira Cardoso, L.; et al. Changes of Physical Activity and Ultra-Processed Food Consumption in Adolescents from Different Countries during COVID-19 Pandemic: An Observational Study. Nutrients 2020, 12, 2289. [Google Scholar] [CrossRef]
- Nagata, J.M.; Abdel Magid, H.S.; Pettee Gabriel, K. Screen Time for Children and Adolescents during the Coronavirus Disease 2019 Pandemic. Obesity 2020, 28, 1582–1583. [Google Scholar] [CrossRef]
- Park, H.K.; Kim, J.; Shim, Y.S. Association between Sleep Duration and Body Composition in Girls Ten to Eighteen Years of Age: A Population-Based Study. Child. Obes. 2020, 16, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Sunday, S.; Kabir, Z. Impact of Carers’ Smoking Status on Childhood Obesity in the Growing up in Ireland Cohort Study. Int. J. Environ. Res. Public. Health 2019, 16, 2759. [Google Scholar] [CrossRef]
- Wyszyńska, J.; Ring-Dimitriou, S.; Thivel, D.; Weghuber, D.; Hadjipanayis, A.; Grossman, Z.; Ross-Russell, R.; Dereń, K.; Mazur, A. Physical Activity in the Prevention of Childhood Obesity: The Position of the European Childhood Obesity Group and the European Academy of Pediatrics. Front. Pediatr. 2020, 8, 535705. [Google Scholar] [CrossRef] [PubMed]
- Educating the Student Body: Taking Physical Activity and Physical Education to School; National Academies Press: Washington, DC, USA, 2013; p. 18314. ISBN 978-0-309-28313-7.
- An, R. Projecting the Impact of the Coronavirus Disease-2019 Pandemic on Childhood Obesity in the United States: A Microsimulation Model. J. Sport Health Sci. 2020, 9, 302–312. [Google Scholar] [CrossRef] [PubMed]
- von Hippel, P.T.; Workman, J. From Kindergarten through Second Grade, U.S. Children’s Obesity Prevalence Grows Only during Summer Vacations: Obesity Grows Only during Summer. Obesity 2016, 24, 2296–2300. [Google Scholar] [CrossRef]
- Franckle, R.; Adler, R.; Davison, K. Accelerated Weight Gain Among Children During Summer Versus School Year and Related Racial/Ethnic Disparities: A Systematic Review. Prev. Chronic. Dis. 2014, 11, 130355. [Google Scholar] [CrossRef]
- Baranowski, T.; O’Connor, T.; Johnston, C.; Hughes, S.; Moreno, J.; Chen, T.-A.; Meltzer, L.; Baranowski, J. School Year Versus Summer Differences in Child Weight Gain: A Narrative Review. Child. Obes. 2014, 10, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19–Related School Closings and Risk of Weight Gain Among Children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [PubMed]
- Abawi, O.; Welling, M.S.; Eynde, E.; Rossum, E.F.C.; Halberstadt, J.; Akker, E.L.T.; Voorn, B. COVID-19 Related Anxiety in Children and Adolescents with Severe Obesity: A Mixed-methods Study. Clin. Obes. 2020, 10, e12412. [Google Scholar] [CrossRef]
- Wilson, S.M.; Sato, A.F. Stress and Paediatric Obesity: What We Know and Where to Go: Stress and Paediatric Obesity. Stress Health 2014, 30, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Fox, C.K.; Gross, A.C.; Rudser, K.D.; Foy, A.M.H.; Kelly, A.S. Depression, Anxiety, and Severity of Obesity in Adolescents: Is Emotional Eating the Link? Clin. Pediatr. 2016, 55, 1120–1125. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and Burden of the Coronavirus 2019 (COVID-19) Pandemic for Child and Adolescent Mental Health: A Narrative Review to Highlight Clinical and Research Needs in the Acute Phase and the Long Return to Normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef]
- Tate, E.B.; Wood, W.; Liao, Y.; Dunton, G.F. Do Stressed Mothers Have Heavier Children? A Meta-Analysis on the Relationship between Maternal Stress and Child Body Mass Index: Maternal Stress and Child Obesity. Obes. Rev. 2015, 16, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Baskind, M.J.; Taveras, E.M.; Gerber, M.W.; Fiechtner, L.; Horan, C.; Sharifi, M. Parent-Perceived Stress and Its Association with Children’s Weight and Obesity-Related Behaviors. Prev. Chronic. Dis. 2019, 16, 180368. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, S.; Christison, A.L.; Levy, E.; McGravery, J.; Tekin, A.; Bolliger, D.; Kumar, V.K.; Bansal, V.; Chiotos, K.; Gist, K.M.; et al. The Impact of Obesity on Disease Severity and Outcomes Among Hospitalized Children with COVID-19. Hosp. Pediatr. 2021, 11, e297–e316. [Google Scholar] [CrossRef]
- Busetto, L.; Bettini, S.; Fabris, R.; Serra, R.; Dal Pra, C.; Maffei, P.; Rossato, M.; Fioretto, P.; Vettor, R. Obesity and COVID-19: An Italian Snapshot. Obesity 2020, 28, 1600–1605. [Google Scholar] [CrossRef]
- Agarwal, A.; Karim, F.; Fernandez Bowman, A.; Antonetti, C.R. Obesity as a Risk Factor for Severe Illness From COVID-19 in the Pediatric Population. Cureus 2021, 13, e14825. [Google Scholar] [CrossRef] [PubMed]
- Valerio, G.; Maffeis, C.; Saggese, G.; Ambruzzi, M.A.; Balsamo, A.; Bellone, S.; Bergamini, M.; Bernasconi, S.; Bona, G.; Calcaterra, V.; et al. Diagnosis, Treatment and Prevention of Pediatric Obesity: Consensus Position Statement of the Italian Society for Pediatric Endocrinology and Diabetology and the Italian Society of Pediatrics. Ital. J. Pediatr. 2018, 44, 88. [Google Scholar] [CrossRef]
- Hajifathalian, K.; Kumar, S.; Newberry, C.; Shah, S.; Fortune, B.; Krisko, T.; Ortiz-Pujols, S.; Zhou, X.K.; Dannenberg, A.J.; Kumar, R.; et al. Obesity Is Associated with Worse Outcomes in COVID-19: Analysis of Early Data from New York City. Obesity 2020, 28, 1606–1612. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; McInnes, I.B.; McMurray, J.J.V. Obesity Is a Risk Factor for Severe COVID-19 Infection: Multiple Potential Mechanisms. Circulation 2020, 142, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Petrakis, D.; Margină, D.; Tsarouhas, K.; Tekos, F.; Stan, M.; Nikitovic, D.; Kouretas, D.; Spandidos, D.; Tsatsakis, A. Obesity—A Risk Factor for Increased COVID-19 Prevalence, Severity and Lethality (Review). Mol. Med. Rep. 2020, 22, 9–19. [Google Scholar] [CrossRef]
- Banerjee, M.; Gupta, S.; Sharma, P.; Shekhawat, J.; Gauba, K. Obesity and COVID-19: A Fatal Alliance. Indian J. Clin. Biochem. 2020, 35, 410–417. [Google Scholar] [CrossRef]
- Korakas, E.; Ikonomidis, I.; Kousathana, F.; Balampanis, K.; Kountouri, A.; Raptis, A.; Palaiodimou, L.; Kokkinos, A.; Lambadiari, V. Obesity and COVID-19: Immune and Metabolic Derangement as a Possible Link to Adverse Clinical Outcomes. Am. J. Physiol.-Endocrinol. Metab. 2020, 319, E105–E109. [Google Scholar] [CrossRef]
- Koyuncuoğlu Güngör, N. Overweight and Obesity in Children and Adolescents. J. Clin. Res. Pediatr. Endocrinol. 2014, 6, 129–143. [Google Scholar] [CrossRef]
- Erener, S. Diabetes, Infection Risk and COVID-19. Mol. Metab. 2020, 39, 101044. [Google Scholar] [CrossRef]
- Weihe, P.; Weihrauch-Blüher, S. Metabolic Syndrome in Children and Adolescents: Diagnostic Criteria, Therapeutic Options and Perspectives. Curr. Obes. Rep. 2019, 8, 472–479. [Google Scholar] [CrossRef]
- Garcia, J.; Benedeti, A.C.G.S.; Caixe, S.H.; Mauad Filho, F.; Nogueira-de-Almeida, C.A. Ultrasonographic Evaluation of the Common Carotid Intima-Media Complex in Healthy and Overweight/Obese Children. J. Vasc. Bras. 2019, 18, e20190003. [Google Scholar] [CrossRef]
- Al-Shorman, A.; Al-Domi, H.; Faqih, A. Markers of Subclinical Atherosclerosis in Schoolchildren with Obesity and Metabolic Syndrome. Swiss Med. Wkly. 2017, 147, w14446. [Google Scholar] [CrossRef]
- Nägele, M.P.; Haubner, B.; Tanner, F.C.; Ruschitzka, F.; Flammer, A.J. Endothelial Dysfunction in COVID-19: Current Findings and Therapeutic Implications. Atherosclerosis 2020, 314, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Caixe, S.H.; Benedetia, A.C.G.S.; Garcia, J.; Martins, W.d.P.; Mauad Filho, F.; Del Ciampo, L.A.; Nogueira-de-Almeida, C.A. Evaluation of Echocardiography as a Marker of Cardiovascular Risk in Obese Children and Adolescents. Int. J. Clin. Pediatr. 2014, 3, 72–78. [Google Scholar] [CrossRef][Green Version]
- De, A.; Rastogi, D. Association of Pediatric Obesity and Asthma, Pulmonary Physiology, Metabolic Dysregulation, and Atopy; and the Role of Weight Management. Expert Rev. Endocrinol. Metab. 2019, 14, 335–349. [Google Scholar] [CrossRef] [PubMed]
- Köchli, S.; Endes, K.; Bartenstein, T.; Usemann, J.; Schmidt-Trucksäss, A.; Frey, U.; Zahner, L.; Hanssen, H. Lung Function, Obesity and Physical Fitness in Young Children: The EXAMIN YOUTH Study. Respir. Med. 2019, 159, 105813. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Vidal, C.; Sanjuan, G.; Moreno-García, E.; Puerta-Alcalde, P.; Garcia-Pouton, N.; Chumbita, M.; Fernandez-Pittol, M.; Pitart, C.; Inciarte, A.; Bodro, M.; et al. Incidence of Co-Infections and Superinfections in Hospitalized Patients with COVID-19: A Retrospective Cohort Study. Clin. Microbiol. Infect. 2021, 27, 83–88. [Google Scholar] [CrossRef]
- Kelishadi, R.; Roufarshbaf, M.; Soheili, S.; Payghambarzadeh, F.; Masjedi, M. Association of Childhood Obesity and the Immune System: A Systematic Review of Reviews. Child. Obes. 2017, 13, 332–346. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M.; Staiano, A. Insights on Obesity in Children and Adults: Individualizing Management. Trends Endocrinol. Metab. 2019, 30, 724–734. [Google Scholar] [CrossRef]
- Magrone, T.; Jirillo, E. Childhood Obesity: Immune Response and Nutritional Approaches. Front. Immunol. 2015, 6, 76. [Google Scholar] [CrossRef]
- Karki, R.; Sharma, B.R.; Tuladhar, S.; Williams, E.P.; Zalduondo, L.; Samir, P.; Zheng, M.; Sundaram, B.; Banoth, B.; Malireddi, R.K.S.; et al. Synergism of TNF-α and IFN-γ Triggers Inflammatory Cell Death, Tissue Damage, and Mortality in SARS-CoV-2 Infection and Cytokine Shock Syndromes. Cell 2021, 184, 149–168.e17. [Google Scholar] [CrossRef] [PubMed]
- Karakaya Molla, G.; Ünal Uzun, Ö.; Koç, N.; Özen Yeşil, B.; Bayhan, G.İ. Evaluation of Nutritional Status in Pediatric Patients Diagnosed with Covid-19 Infection. Clin. Nutr. ESPEN 2021, 44, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Vranić, L.; Mikolašević, I.; Milić, S. Vitamin D Deficiency: Consequence or Cause of Obesity? Medicina 2019, 55, 541. [Google Scholar] [CrossRef] [PubMed]
- Indiani, C.M.d.S.P.; Rizzardi, K.F.; Castelo, P.M.; Ferraz, L.F.C.; Darrieux, M.; Parisotto, T.M. Childhood Obesity and Firmicutes/Bacteroidetes Ratio in the Gut Microbiota: A Systematic Review. Child. Obes. 2018, 14, 501–509. [Google Scholar] [CrossRef]
- Abenavoli, L.; Scarpellini, E.; Colica, C.; Boccuto, L.; Salehi, B.; Sharifi-Rad, J.; Aiello, V.; Romano, B.; De Lorenzo, A.; Izzo, A.A.; et al. Gut Microbiota and Obesity: A Role for Probiotics. Nutrients 2019, 11, 2690. [Google Scholar] [CrossRef]
- Yang, Y.-J.; Ni, Y.-H. Gut Microbiota and Pediatric Obesity/Non-Alcoholic Fatty Liver Disease. J. Formos. Med. Assoc. 2019, 118, S55–S61. [Google Scholar] [CrossRef]
- Dhar, D.; Mohanty, A. Gut Microbiota and Covid-19- Possible Link and Implications. Virus Res. 2020, 285, 198018. [Google Scholar] [CrossRef]
- Díaz, E.; Rodríguez, A.; Martin-Loeches, I.; Lorente, L.; del Mar Martín, M.; Pozo, J.C.; Montejo, J.C.; Estella, A.; Arenzana, Á.; Rello, J. Impact of Obesity in Patients Infected With 2009 Influenza A(H1N1). Chest 2011, 139, 382–386. [Google Scholar] [CrossRef]
- Green, W.D.; Beck, M.A. Obesity Impairs the Adaptive Immune Response to Influenza Virus. Ann. Am. Thorac. Soc. 2017, 14, S406–S409. [Google Scholar] [CrossRef]
- Calder, P.C. Nutrition, Immunity and COVID-19. BMJ Nutr. Prev. Health 2020, 3, 74–92. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lee, I.S.; Choue, R. Obesity, Inflammation and Diet. Pediatr. Gastroenterol. Hepatol. Nutr. 2013, 16, 143. [Google Scholar] [CrossRef]
- Okubo, Y.; Nochioka, K.; Testa, M.A. The Impact of Pediatric Obesity on Hospitalized Children with Lower Respiratory Tract Infections in the United States. Clin. Respir. J. 2018, 12, 1479–1484. [Google Scholar] [CrossRef] [PubMed]
- Goossens, G.H.; Dicker, D.; Farpour-Lambert, N.J.; Frühbeck, G.; Mullerova, D.; Woodward, E.; Holm, J.-C. Obesity and COVID-19: A Perspective from the European Association for the Study of Obesity on Immunological Perturbations, Therapeutic Challenges, and Opportunities in Obesity. Obes. Facts 2020, 13, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Mui, E.; Holubar, M.K.; Deresinski, S.C. Comprehensive Guidance for Antibiotic Dosing in Obese Adults. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2017, 37, 1415–1431. [Google Scholar] [CrossRef]
- Soeroto, A.Y.; Soetedjo, N.N.; Purwiga, A.; Santoso, P.; Kulsum, I.D.; Suryadinata, H.; Ferdian, F. Effect of Increased BMI and Obesity on the Outcome of COVID-19 Adult Patients: A Systematic Review and Meta-Analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1897–1904. [Google Scholar] [CrossRef]
- Dhurandhar, N.V.; Bailey, D.; Thomas, D. Interaction of Obesity and Infections: Interaction of Obesity and Infections. Obes. Rev. 2015, 16, 1017–1029. [Google Scholar] [CrossRef]
- Dobner, J.; Kaser, S. Body Mass Index and the Risk of Infection—From Underweight to Obesity. Clin. Microbiol. Infect. 2018, 24, 24–28. [Google Scholar] [CrossRef]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for the Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef]
- Cena, H.; Chieppa, M. Coronavirus Disease (COVID-19–SARS-CoV-2) and Nutrition: Is Infection in Italy Suggesting a Connection? Front. Immunol. 2020, 11, 944. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, Y. Potential Interventions for Novel Coronavirus in China: A Systematic Review. J. Med. Virol. 2020, 92, 479–490. [Google Scholar] [CrossRef]
- Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Krznaric, Z.; Nitzan, D.; Pirlich, M.; Singer, P. ESPEN Expert Statements and Practical Guidance for Nutritional Management of Individuals with SARS-CoV-2 Infection. Clin. Nutr. 2020, 39, 1631–1638. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, K.D.d.S.; Garcia, L.R.S.; Dametto, J.F.d.S.; Assunção, D.G.F.; Maciel, B.L.L. COVID-19 and Nutrition: The Need for Initiatives to Promote Healthy Eating and Prevent Obesity in Childhood. Child. Obes. 2020, 16, 235–237. [Google Scholar] [CrossRef] [PubMed]
- Astrup, A.; Bügel, S. Overfed but Undernourished: Recognizing Nutritional Inadequacies/Deficiencies in Patients with Overweight or Obesity. Int. J. Obes. 2019, 43, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, S.; Gangadharan, K.; Pitchumoni, C.S. Malnutrition in Obesity before and after Bariatric Surgery. Dis. Mon. 2020, 66, 100866. [Google Scholar] [CrossRef] [PubMed]
- Tagliaferri, S.; Porri, D.; De Giuseppe, R.; Manuelli, M.; Alessio, F.; Cena, H. The Controversial Role of Vitamin D as an Antioxidant: Results from Randomised Controlled Trials. Nutr. Res. Rev. 2019, 32, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Vierucci, F.; Del Pistoia, M.; Fanos, M.; Erba, P.; Saggese, G. Prevalence of Hypovitaminosis D and Predictors of Vitamin D Status in Italian Healthy Adolescents. Ital. J. Pediatr. 2014, 40, 54. [Google Scholar] [CrossRef]
- Carter, S.J.; Baranauskas, M.N.; Fly, A.D. Considerations for Obesity, Vitamin D, and Physical Activity Amid the COVID-19 Pandemic. Obesity 2020, 28, 1176–1177. [Google Scholar] [CrossRef] [PubMed]
- Durá-Travé, T.; Gallinas-Victoriano, F.; Chueca-Guindulain, M.J.; Berrade-Zubiri, S. Prevalence of Hypovitaminosis D and Associated Factors in Obese Spanish Children. Nutr. Diabetes 2017, 7, e248. [Google Scholar] [CrossRef]
- Belančić, A.; Kresović, A.; Rački, V. Potential Pathophysiological Mechanisms Leading to Increased COVID-19 Susceptibility and Severity in Obesity. Obes. Med. 2020, 19, 100259. [Google Scholar] [CrossRef]
- Ilie, P.C.; Stefanescu, S.; Smith, L. The Role of Vitamin D in the Prevention of Coronavirus Disease 2019 Infection and Mortality. Aging Clin. Exp. Res. 2020, 32, 1195–1198. [Google Scholar] [CrossRef]
- Garipağaoğlu, M.; Sahip, Y.; Budak, N.; Akdikmen, Ö.; Altan, T.; Baban, M. Food Types in the Diet and the Nutrient Intake of Obese and Non-Obese Children. J. Clin. Res. Pediatr. Endocrinol. 2011, 1, 21–29. [Google Scholar] [CrossRef]
- Huang, Z.; Liu, Y.; Qi, G.; Brand, D.; Zheng, S. Role of Vitamin A in the Immune System. J. Clin. Med. 2018, 7, 258. [Google Scholar] [CrossRef]
- Rizvi, S.; Raza, S.T.; Ahmed, F.; Ahmad, A.; Abbas, S.; Mahdi, F. The Role of Vitamin e in Human Health and Some Diseases. Sultan Qaboos Univ. Med. J. 2014, 14, e157–e165. [Google Scholar]
- Carr, A.; Maggini, S. Vitamin C and Immune Function. Nutrients 2017, 9, 1211. [Google Scholar] [CrossRef] [PubMed]
- Yoshii, K.; Hosomi, K.; Sawane, K.; Kunisawa, J. Metabolism of Dietary and Microbial Vitamin B Family in the Regulation of Host Immunity. Front. Nutr. 2019, 6, 48. [Google Scholar] [CrossRef] [PubMed]
- Beketova, N.A.; Pavlovskaya, E.V.; Kodentsova, V.M.; Vrzhesinskaya, O.A.; Kosheleva, O.A.; Sokolnikov, A.A.; Strokova, T.V. Biomarkers of vitamin status in obese school children. Vopr. Pitan. 2019, 88, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.; Halim, J.; Gow, M.; El-Haddad, N.; Marzulli, T.; Baur, L.; Cowell, C.; Garnett, S. Vitamin B12 in Obese Adolescents with Clinical Features of Insulin Resistance. Nutrients 2014, 6, 5611–5618. [Google Scholar] [CrossRef]
- Gunanti, I.R.; Marks, G.C.; Al-Mamun, A.; Long, K.Z. Low Serum Vitamin B-12 and Folate Concentrations and Low Thiamin and Riboflavin Intakes Are Inversely Associated with Greater Adiposity in Mexican American Children. J. Nutr. 2014, 144, 2027–2033. [Google Scholar] [CrossRef]
- De Giuseppe, R.; Venturelli, G.; Guez, S.; Salera, S.; De Vita, C.; Consonni, D.; Dellanoce, C.; Bamonti, F.; Chiarelli, G.; Manzoni, F.; et al. Homocysteine Metabolism in Children and Adolescents with Epidermolysis Bullosa. BMC Pediatr. 2016, 16, 173. [Google Scholar] [CrossRef]
- De Giuseppe, R.; Tomasinelli, C.E.; Vincenti, A.; Di Napoli, I.; Negro, M.; Cena, H. Sarcopenia and Homocysteine: Is There a Possible Association in the Elderly? A Narrative Review. Nutr. Res. Rev. 2021, 1–14. [Google Scholar] [CrossRef]
- Dalbeni, A.; Bevilacqua, M.; Teani, I.; Normelli, I.; Mazzaferri, F.; Chiarioni, G. Excessive Vitamin B12 and Poor Outcome in COVID-19 Pneumonia. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 774–775. [Google Scholar] [CrossRef]
- Lassi, Z.S.; Moin, A.; Bhutta, Z.A. Zinc Supplementation for the Prevention of Pneumonia in Children Aged 2 Months to 59 Months. Cochrane Database Syst. Rev. 2016, 12. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.E.; Wessling-Resnick, M. Iron Metabolism and the Innate Immune Response to Infection. Microbes Infect. 2012, 14, 207–216. [Google Scholar] [CrossRef]
- Gwamaka, M.; Kurtis, J.D.; Sorensen, B.E.; Holte, S.; Morrison, R.; Mutabingwa, T.K.; Fried, M.; Duffy, P.E. Iron Deficiency Protects Against Severe Plasmodium Falciparum Malaria and Death in Young Children. Clin. Infect. Dis. 2012, 54, 1137–1144. [Google Scholar] [CrossRef]
- Neuberger, A.; Okebe, J.; Yahav, D.; Paul, M. Oral Iron Supplements for Children in Malaria-Endemic Areas. Cochrane Database Syst. Rev. 2016, 2. [Google Scholar] [CrossRef]
- Pasricha, S.-R.; Armitage, A.E.; Prentice, A.M.; Drakesmith, H. Reducing Anaemia in Low Income Countries: Control of Infection Is Essential. BMJ 2018, 362, k3165. [Google Scholar] [CrossRef] [PubMed]
- Ganz, T.; Nemeth, E. Iron Homeostasis in Host Defence and Inflammation. Nat. Rev. Immunol. 2015, 15, 500–510. [Google Scholar] [CrossRef]
- James, P.T.; Ali, Z.; Armitage, A.E.; Bonell, A.; Cerami, C.; Drakesmith, H.; Jobe, M.; Jones, K.S.; Liew, Z.; Moore, S.E.; et al. The Role of Nutrition in COVID-19 Susceptibility and Severity of Disease: A Systematic Review. J. Nutr. 2021, 151, 1854–1878. [Google Scholar] [CrossRef]
- Frise, M.C.; Cheng, H.-Y.; Nickol, A.H.; Curtis, M.K.; Pollard, K.A.; Roberts, D.J.; Ratcliffe, P.J.; Dorrington, K.L.; Robbins, P.A. Clinical Iron Deficiency Disturbs Normal Human Responses to Hypoxia. J. Clin. Investig. 2016, 126, 2139–2150. [Google Scholar] [CrossRef] [PubMed]
- Sonnweber, T.; Pizzini, A.; Tancevski, I.; Löffler-Ragg, J.; Weiss, G. Anaemia, Iron Homeostasis and Pulmonary Hypertension: A Review. Intern. Emerg. Med. 2020, 15, 573–585. [Google Scholar] [CrossRef]
- Sadeghsoltani, F.; Mohammadzadeh, I.; Safari, M.-M.; Hassanpour, P.; Izadpanah, M.; Qujeq, D.; Moein, S.; Vaghari-Tabari, M. Zinc and Respiratory Viral Infections: Important Trace Element in Anti-Viral Response and Immune Regulation. Biol. Trace Elem. Res. 2021, 1–16. [Google Scholar] [CrossRef]
- Bellmann-Weiler, R.; Lanser, L.; Barket, R.; Rangger, L.; Schapfl, A.; Schaber, M.; Fritsche, G.; Wöll, E.; Weiss, G. Prevalence and Predictive Value of Anemia and Dysregulated Iron Homeostasis in Patients with COVID-19 Infection. J. Clin. Med. 2020, 9, 2429. [Google Scholar] [CrossRef] [PubMed]
- Salas González, M.D.; Rodríguez Rodríguez, E.; Jiménez Ortega, A.I.; González Rodríguez, L.G.; López Sobaler, A.M. Zinc and Its Relation to Insulin Resistance in Children. Nutr. Hosp. 2021, 38, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Mao, S.; Zhang, A.; Huang, S. Meta-Analysis of Zn, Cu and Fe in the Hair of Chinese Children with Recurrent Respiratory Tract Infection. Scand. J. Clin. Lab. Investig. 2014, 74, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Song, Y. Efficacy of Zinc given as an Adjunct to the Treatment of Severe Pneumonia: A Meta-Analysis of Randomized, Double-Blind and Placebo-Controlled Trials. Clin. Respir. J. 2018, 12, 857–864. [Google Scholar] [CrossRef]
- Anuk, A.T.; Polat, N.; Akdas, S.; Erol, S.A.; Tanacan, A.; Biriken, D.; Keskin, H.L.; Moraloglu Tekin, O.; Yazihan, N.; Sahin, D. The Relation Between Trace Element Status (Zinc, Copper, Magnesium) and Clinical Outcomes in COVID-19 Infection During Pregnancy. Biol. Trace Elem. Res. 2021, 199, 3608–3617. [Google Scholar] [CrossRef]
- Heller, R.A.; Sun, Q.; Hackler, J.; Seelig, J.; Seibert, L.; Cherkezov, A.; Minich, W.B.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Prediction of Survival Odds in COVID-19 by Zinc, Age and Selenoprotein P as Composite Biomarker. Redox Biol. 2021, 38, 101764. [Google Scholar] [CrossRef]
- Jothimani, D.; Kailasam, E.; Danielraj, S.; Nallathambi, B.; Ramachandran, H.; Sekar, P.; Manoharan, S.; Ramani, V.; Narasimhan, G.; Kaliamoorthy, I.; et al. COVID-19: Poor Outcomes in Patients with Zinc Deficiency. Int. J. Infect. Dis. 2020, 100, 343–349. [Google Scholar] [CrossRef]
- Sandoval, D.A.; Davis, S.N. Leptin: Metabolic Control and Regulation. J. Diabetes Complicat. 2003, 17, 108–113. [Google Scholar] [CrossRef]
- Marion-Letellier, R.; Savoye, G.; Ghosh, S. Polyunsaturated Fatty Acids and Inflammation: PUFA and Inflammation. IUBMB Life 2015, 67, 659–667. [Google Scholar] [CrossRef]
- DiNicolantonio, J.J.; O’Keefe, J.H. Importance of Maintaining a Low Omega–6/Omega–3 Ratio for Reducing Inflammation. Open Heart 2018, 5, e000946. [Google Scholar] [CrossRef]
- Simopoulos, A. An Increase in the Omega-6/Omega-3 Fatty Acid Ratio Increases the Risk for Obesity. Nutrients 2016, 8, 128. [Google Scholar] [CrossRef] [PubMed]
- Czerwonogrodzka-Senczyna, A.; Janusz, M.; Jeznach-Steinhagen, A.; Demkow, U.; Pyrzak, B. Nutrition and Immune System in Children with Simple Obesity. In Advances in Clinical Science; Pokorski, M., Ed.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2015; Volume 878, pp. 49–56. ISBN 978-3-319-21496-2. [Google Scholar]
- Bervoets, L.; Van Hoorenbeeck, K.; Kortleven, I.; Van Noten, C.; Hens, N.; Vael, C.; Goossens, H.; Desager, K.N.; Vankerckhoven, V. Differences in Gut Microbiota Composition between Obese and Lean Children: A Cross-Sectional Study. Gut Pathog. 2013, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, C.L.J.; Önnerfält, J.; Xu, J.; Molin, G.; Ahrné, S.; Thorngren-Jerneck, K. The Microbiota of the Gut in Preschool Children with Normal and Excessive Body Weight. Obesity 2012, 20, 2257–2261. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Knight, R. Dietary Effects on Human Gut Microbiome Diversity. Br. J. Nutr. 2015, 113, S1–S5. [Google Scholar] [CrossRef]
- Zhang, T.; Cui, X.; Zhao, X.; Wang, J.; Zheng, J.; Zheng, G.; Guo, W.; Cai, C.; He, S.; Xu, Y. Detectable SARS-CoV-2 Viral RNA in Feces of Three Children during Recovery Period of COVID-19 Pneumonia. J. Med. Virol. 2020, 92, 909–914. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Ramos-Campo, D.J.; Mielgo-Ayuso, J.; Dalamitros, A.A.; Nikolaidis, P.A.; Hormeño-Holgado, A.; Tornero-Aguilera, J.F. Nutrition in the Actual COVID-19 Pandemic. A Narrative Review. Nutrients 2021, 13, 1924. [Google Scholar] [CrossRef]
- Maffoni, S.; Brazzo, S.; De Giuseppe, R.; Biino, G.; Vietti, I.; Pallavicini, C.; Cena, H. Lifestyle Changes and Body Mass Index during COVID-19 Pandemic Lockdown: An Italian Online-Survey. Nutrients 2021, 13, 1117. [Google Scholar] [CrossRef]
- Fore, H.H.; Dongyu, Q.; Beasley, D.M.; Ghebreyesus, T.A. Child Malnutrition and COVID-19: The Time to Act Is Now. Lancet 2020, 396, 517–518. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating Habits and Lifestyle Changes during COVID-19 Lockdown: An Italian Survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Dragun, R.; Veček, N.N.; Marendić, M.; Pribisalić, A.; Đivić, G.; Cena, H.; Polašek, O.; Kolčić, I. Have Lifestyle Habits and Psychological Well-Being Changed among Adolescents and Medical Students Due to COVID-19 Lockdown in Croatia? Nutrients 2020, 13, 97. [Google Scholar] [CrossRef]
- iPES FOOD International Panel of Experts on Sustainable Food Systems (IPES-Food), COVID-19 and the Crisis in Food Systems: Symptoms, Causes, and Potential Solutions. Available online: Http://Www.Ipes-Food.Org/_img/Upload/Files/COVID-19_CommuniqueEN.Pdf (accessed on 7 November 2021).
- Zemrani, B.; Gehri, M.; Masserey, E.; Knob, C.; Pellaton, R. A Hidden Side of the COVID-19 Pandemic in Children: The Double Burden of Undernutrition and Overnutrition. Int. J. Equity Health 2021, 20, 44. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Kwon, Y.; Choe, Y.H.; Kim, M.J. COVID-19-Related School Closing Aggravate Obesity and Glucose Intolerance in Pediatric Patients with Obesity. Sci. Rep. 2021, 11, 5494. [Google Scholar] [CrossRef] [PubMed]
- Turel, O.; Romashkin, A.; Morrison, K.M. A Model Linking Video Gaming, Sleep Quality, Sweet Drinks Consumption and Obesity among Children and Youth: Video Gaming, Sleep, Sweet Drinks and Obesity. Clin. Obes. 2017, 7, 191–198. [Google Scholar] [CrossRef]
- Vitagliano, J.A.; Jhe, G.; Milliren, C.E.; Lin, J.A.; Spigel, R.; Freizinger, M.; Woods, E.R.; Forman, S.F.; Richmond, T.K. COVID-19 and Eating Disorder and Mental Health Concerns in Patients with Eating Disorders. J. Eat. Disord. 2021, 9, 80. [Google Scholar] [CrossRef]
- Termorshuizen, J.D.; Watson, H.J.; Thornton, L.M.; Borg, S.; Flatt, R.E.; MacDermod, C.M.; Harper, L.E.; Furth, E.F.; Peat, C.M.; Bulik, C.M. Early Impact of COVID-19 on Individuals with Self-reported Eating Disorders: A Survey of ~1,000 Individuals in the United States and the Netherlands. Int. J. Eat. Disord. 2020, 53, 1780–1790. [Google Scholar] [CrossRef]
- Marchitelli, S.; Mazza, C.; Lenzi, A.; Ricci, E.; Gnessi, L.; Roma, P. Weight Gain in a Sample of Patients Affected by Overweight/Obesity with and without a Psychiatric Diagnosis during the Covid-19 Lockdown. Nutrients 2020, 12, 3525. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, Y.; Huo, S.; Ma, Y.; Ke, Y.; Wang, P.; Zhao, A. Emotional Eating in Pregnant Women during the COVID-19 Pandemic and Its Association with Dietary Intake and Gestational Weight Gain. Nutrients 2020, 12, 2250. [Google Scholar] [CrossRef]
- Verduci, E.; Calcaterra, V.; Di Profio, E.; Fiore, G.; Rey, F.; Magenes, V.C.; Todisco, C.F.; Carelli, S.; Zuccotti, G.V. Brown Adipose Tissue: New Challenges for Prevention of Childhood Obesity. A Narrative Review. Nutrients 2021, 13, 1450. [Google Scholar] [CrossRef] [PubMed]
- Mate, A.; Reyes-Goya, C.; Santana-Garrido, Á.; Sobrevia, L.; Vázquez, C.M. Impact of Maternal Nutrition in Viral Infections during Pregnancy. Biochim. Biophys. Acta BBA—Mol. Basis Dis. 2021, 1867, 166231. [Google Scholar] [CrossRef] [PubMed]
- Butler, M.J.; Barrientos, R.M. The Impact of Nutrition on COVID-19 Susceptibility and Long-Term Consequences. Brain. Behav. Immun. 2020, 87, 53–54. [Google Scholar] [CrossRef] [PubMed]
| Centers for Disease Control and Prevention (CDC) | Royal College of Pediatrics and Child Health (RCPCH) | World Health Organization (WHO) |
|---|---|---|
| An individual aged <21 years presenting with fever, laboratory evidence of inflammation, and evidence of clinically severe illness requiring hospitalization, with multisystem (>2) organ involvement (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic, or neurologic) Fever >38.0 °C for ≥ 24 h or report of subjective fever ≥ 24 h Laboratory evidence including at least one of the following: an elevated CRP level, ESR, fibrinogen, procalcitonin, d-dimer, ferritin, lactic acid dehydrogenase, or IL-6 levels; elevated neutrophil level; reduced lymphocyte level; and low albumin level AND No alternative plausible diagnoses AND Positive for current or recent SARS-CoV-2 infection at RT-PCR assay, serology, or antigen test; or COVID-19 exposure within the 4 weeks before the onset of symptoms | A child presenting with persistent fever, inflammation (neutrophilia, elevated CRP level, and lymphopenia) with evidence of single or multiorgan dysfunction (shock, cardiac, respiratory, renal, gastrointestinal, or neurologic disorder) with additional features This may include children fulfilling full or partial criteria for Kawasaki disease Exclusion of any other microbial cause, including bacterial sepsis, staphylococcal or streptococcal shock syndromes, infections associated with myocarditis such as enterovirus SARS-CoV-2 RT-PCR testing may be positive or negative | Children and adolescents aged 0–19 years with fever ≥ 3 days AND two of the following: - Rash or bilateral nonpurulent conjunctivitis or muco-cutaneous inflammation signs (oral, hands or feet) - Hypotension or shock - Features of myocardial dysfunction: pericarditis, valvulitis, or coronary abnormalities (including echocardiographic findings or elevated troponin/NT-proBNP) - Evidence of coagulopathy (PT, PTT, elevated d-dimer level) - Acute gastrointestinal problems (diarrhea, vomiting, or abdominal pain) AND Elevated markers of inflammation (as ESR, CRP, or procalcitonin) AND No other obvious microbial cause of inflammation, including bacterial sepsis, staphylococcal or streptococcal shock syndromes AND Evidence of COVID-19 (RT-PCR assay, antigen test, or serology positive) or likely contact with patients with COVID-19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cena, H.; Fiechtner, L.; Vincenti, A.; Magenes, V.C.; De Giuseppe, R.; Manuelli, M.; Zuccotti, G.V.; Calcaterra, V. COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review. Nutrients 2021, 13, 4255. https://doi.org/10.3390/nu13124255
Cena H, Fiechtner L, Vincenti A, Magenes VC, De Giuseppe R, Manuelli M, Zuccotti GV, Calcaterra V. COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review. Nutrients. 2021; 13(12):4255. https://doi.org/10.3390/nu13124255
Chicago/Turabian StyleCena, Hellas, Lauren Fiechtner, Alessandra Vincenti, Vittoria Carlotta Magenes, Rachele De Giuseppe, Matteo Manuelli, Gian Vincenzo Zuccotti, and Valeria Calcaterra. 2021. "COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review" Nutrients 13, no. 12: 4255. https://doi.org/10.3390/nu13124255
APA StyleCena, H., Fiechtner, L., Vincenti, A., Magenes, V. C., De Giuseppe, R., Manuelli, M., Zuccotti, G. V., & Calcaterra, V. (2021). COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review. Nutrients, 13(12), 4255. https://doi.org/10.3390/nu13124255










