Development of the Choices 5-Level Criteria to Support Multiple Food System Actions
Abstract
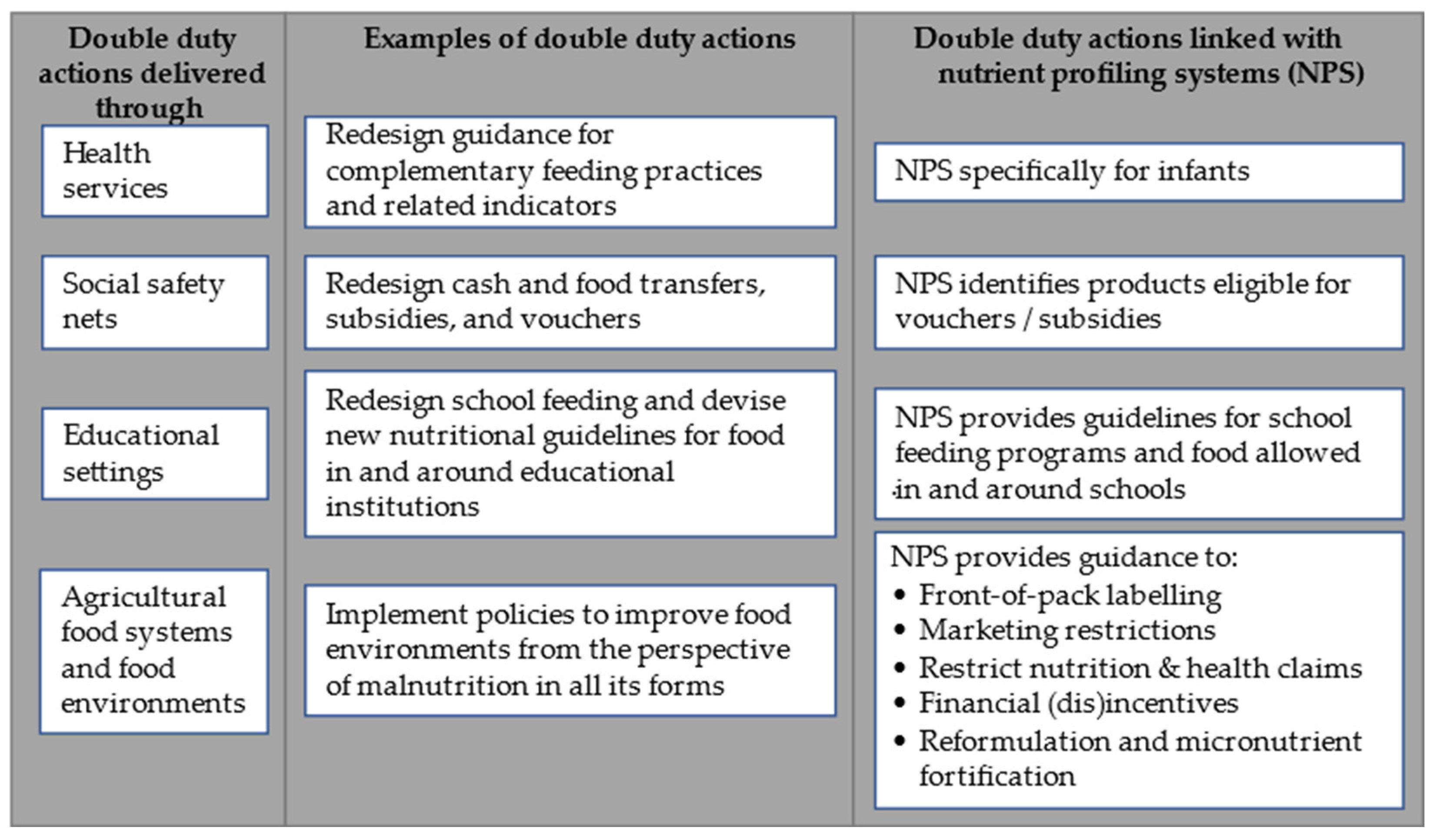
:1. Introduction
2. Materials and Methods
2.1. Development of Intermediate Five-Level Criteria
2.2. Criteria Validation
2.3. Targeted Consultation
3. Results
3.1. Intermediate Five-Level Criteria
3.2. Validation by Indicator Foods
3.3. Targeted Consultation
3.4. Finalization Five-Level Criteria
4. Discussion
4.1. Nutrient Profiling vs. Dietary Guidelines
4.2. Strengths and Limitations
5. Conclusions and Future Perspectives
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siddiqui, F.; Salam, R.A.; Lassi, Z.S.; Das, J.K. The Intertwined Relationship Between Malnutrition and Poverty. Front. Public Health 2020, 8, 453. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission Report. Lancet Lond. Engl. 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Cecchini, M.; Warin, L. Impact of Food Labelling Systems on Food Choices and Eating Behaviours: A Systematic Review and Meta-Analysis of Randomized Studies. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2016, 17, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Shangguan, S.; Afshin, A.; Shulkin, M.; Ma, W.; Marsden, D.; Smith, J.; Saheb-Kashaf, M.; Shi, P.; Micha, R.; Imamura, F.; et al. A Meta-Analysis of Food Labeling Effects on Consumer Diet Behaviors and Industry Practices. Am. J. Prev. Med. 2019, 56, 300–314. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, C.; Ruel, M.T.; Salm, L.; Sinclair, B.; Branca, F. Double-Duty Actions: Seizing Programme and Policy Opportunities to Address Malnutrition in All Its Forms. Lancet Lond. Engl. 2020, 395, 142–155. [Google Scholar] [CrossRef]
- Labonté, M.-È.; Poon, T.; Gladanac, B.; Ahmed, M.; Franco-Arellano, B.; Rayner, M.; L’Abbé, M.R. Nutrient Profile Models with Applications in Government-Led Nutrition Policies Aimed at Health Promotion and Noncommunicable Disease Prevention: A Systematic Review. Adv. Nutr. Bethesda Md. 2018, 9, 741–788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roodenburg, A.J.C.; Popkin, B.M.; Seidell, J.C. Development of International Criteria for a Front of Package Food Labelling System: The International Choices Programme. Eur. J. Clin. Nutr. 2011, 65, 1190–1200. [Google Scholar] [CrossRef]
- van den Assum, S.; Schilpzand, R.; Lissner, L.; Don, R.; Nair, K.M.; Nnam, N.; Uauy, R.; Yang, Y.; Pekcan, A.G.; Roodenburg, A.J.C. Periodic Revisions of the International Choices Criteria: Process and Results. Nutrients 2020, 12, 2774. [Google Scholar] [CrossRef] [PubMed]
- Vyth, E.L.; Steenhuis, I.H.; Roodenburg, A.J.; Brug, J.; Seidell, J.C. Front-of-Pack Nutrition Label Stimulates Healthier Product Development: A Quantitative Analysis. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smed, S.; Edenbrandt, A.K.; Jansen, L. The Effects of Voluntary Front-of-Pack Nutrition Labels on Volume Shares of Products: The Case of the Dutch Choices. Public Health Nutr. 2019, 22, 2879–2890. [Google Scholar] [CrossRef]
- van der Bend, D.L.M.; Jansen, L.; van der Velde, G.; Blok, V. The Influence of a Front-of-Pack Nutrition Label on Product Reformulation: A Ten-Year Evaluation of the Dutch Choices Programme. Food Chem. X 2020, 6, 100086. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; Jewell, J. What Is the Evidence on the Policy Specifications, Development Processes and Effectiveness of Existing Front-of-Pack Food La-Belling Policies in the WHO European Region? Health Evidence Network (HEN) synthesis report 61; WHO Regional Office for Europe: Copenhagen, Denmark, 2018. [Google Scholar]
- World Health Organization. Regional Office for Europe. Manual to Develop and Implement Front-of-Pack Nutrition Labelling: Guidance for Countries on the Selection and Testing of Evidence-Informed Front-of-Pack Nutrition Labelling Systems in the WHO European Region; World Health Organisation Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- World Health Organization. Regional Office for Europe. WHO Regional Office for Europe Nutrient Profile Model; World Health Organization office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- World Health Organization, Regional office for Western Pacific Region. WHO Nutrient Profile Model for the Western Pacific Region: A Tool to Protect Children from Food Marketing; World Health Organization, Regional Office for the Western Pacific Region: Manila, Philippines, 2016. [Google Scholar]
- World Health Organization, Regional Office for South-East Asia. WHO Nutrient Profile Model for South-East Asia Region; World Health Organization, Regional Office for South-East Asia: New Delhi, India, 2016. [Google Scholar]
- World Health Organization, Regional Office for the Eastern Mediterranean. Nutrient Profile Model for the Marketing of Food and Non-Alcoholic Beverages to Children in the WHO Eastern Mediterranean Region; World Health Organization, Regional Office for the Eastern Mediterranean: Cairo, Egypt, 2017. [Google Scholar]
- World Health Organization, Regional Office for Africa. Nutrient Profile Model for the WHO African Region: A Tool for Implementing WHO Recommendations on the Marketing of Foods and Non-Alcoholic Beverages to Children; World Health Organization: Brazzaville, Republic of the Congo, 2019. [Google Scholar]
- World Health Organization. Nutrient Profiling: Report of a WHO/IASO Technical Meeting. London, United Kingdom 4–6 October 2010; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Drewnowski, A.; Fulgoni, V. Nutrient Profiling of Foods: Creating a Nutrient-Rich Food Index. Nutr. Rev. 2008, 66, 23–39. [Google Scholar] [CrossRef]
- Drewnowski, A.; Fulgoni, V.L. Nutrient Density: Principles and Evaluation Tools. Am. J. Clin. Nutr. 2014, 99, 1223S–1228S. [Google Scholar] [CrossRef] [Green Version]
- Fulgoni, V.L.; Keast, D.R.; Drewnowski, A. Development and Validation of the Nutrient-Rich Foods Index: A Tool to Measure Nutritional Quality of Foods. J. Nutr. 2009, 139, 1549–1554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Agency for Research on Cancer, World Health Organization. IARC Monographs Evaluate Consumption of Red Meat and Processed Meat; World Health Organization: Lyon, France, 2015. [Google Scholar]
- Herforth, A.; Arimond, M.; Álvarez-Sánchez, C.; Coates, J.; Christianson, K.; Muehlhoff, E. A Global Review of Food-Based Dietary Guidelines. Adv. Nutr. 2019, 10, 590–605. [Google Scholar] [CrossRef] [Green Version]
- Montagnese, C.; Santarpia, L.; Iavarone, F.; Strangio, F.; Sangiovanni, B.; Buonifacio, M.; Caldara, A.R.; Silvestri, E.; Contaldo, F.; Pasanisi, F. Food-Based Dietary Guidelines around the World: Eastern Mediterranean and Middle Eastern Countries. Nutrients 2019, 11, 1325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lobstein, T.; Davies, S. Defining and Labelling “healthy” and “Unhealthy” Food. Public Health Nutr. 2009, 12, 331–340. [Google Scholar] [CrossRef] [Green Version]
- Sacks, G.; Rayner, M.; Stockley, L.; Scarborough, P.; Snowdon, W.; Swinburn, B. Applications of Nutrient Profiling: Potential Role in Diet-Related Chronic Disease Prevention and the Feasibility of a Core Nutrient-Profiling System. Eur. J. Clin. Nutr. 2011, 65, 298–306. [Google Scholar] [CrossRef] [Green Version]
- Rayner, M.; Scarborough, P.; Kaur, A. Nutrient Profiling and the Regulation of Marketing to Children. Possibilities and Pitfalls. Appetite 2013, 62, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A. Uses of Nutrient Profiling to Address Public Health Needs: From Regulation to Reformulation. Proc. Nutr. Soc. 2017, 76, 220–229. [Google Scholar] [CrossRef] [Green Version]
- Stewart, C.; Piernas, C.; Cook, B.; Jebb, S.A. Trends in UK Meat Consumption: Analysis of Data from Years 1–11 (2008–09 to 2018–19) of the National Diet and Nutrition Survey Rolling Programme. Lancet Planet. Health 2021, 5, e699–e708. [Google Scholar] [CrossRef]
- Aune, D.; Keum, N.; Giovannucci, E.; Fadnes, L.T.; Boffetta, P.; Greenwood, D.C.; Tonstad, S.; Vatten, L.J.; Riboli, E.; Norat, T. Nut Consumption and Risk of Cardiovascular Disease, Total Cancer, All-Cause and Cause-Specific Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. BMC Med. 2016, 14, 207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Townsend, M.S. Where Is the Science? What Will It Take to Show That Nutrient Profiling Systems Work? Am. J. Clin. Nutr. 2010, 91, 1109S–1115S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooper, S.L.; Pelly, F.E.; Lowe, J.B. Construct and Criterion-Related Validation of Nutrient Profiling Models: A Systematic Review of the Literature. Appetite 2016, 100, 26–40. [Google Scholar] [CrossRef]
- Poon, T.; Labonté, M.-È.; Mulligan, C.; Ahmed, M.; Dickinson, K.M.; L’Abbé, M.R. Comparison of Nutrient Profiling Models for Assessing the Nutritional Quality of Foods: A Validation Study. Br. J. Nutr. 2018, 120, 567–582. [Google Scholar] [CrossRef] [PubMed]
- Deschasaux, M.; Huybrechts, I.; Julia, C.; Hercberg, S.; Egnell, M.; Srour, B.; Kesse-Guyot, E.; Latino-Martel, P.; Biessy, C.; Casagrande, C.; et al. Association between Nutritional Profiles of Foods Underlying Nutri-Score Front-of-Pack Labels and Mortality: EPIC Cohort Study in 10 European Countries. BMJ 2020, 370, m3173. [Google Scholar] [CrossRef]
- Julia, C.; Fézeu, L.K.; Ducrot, P.; Méjean, C.; Péneau, S.; Touvier, M.; Hercberg, S.; Kesse-Guyot, E. The Nutrient Profile of Foods Consumed Using the British Food Standards Agency Nutrient Profiling System Is Associated with Metabolic Syndrome in the SU.VI.MAX Cohort. J. Nutr. 2015, 145, 2355–2361. [Google Scholar] [CrossRef]
- Julia, C.; Ducrot, P.; Lassale, C.; Fézeu, L.; Méjean, C.; Péneau, S.; Touvier, M.; Hercberg, S.; Kesse-Guyot, E. Prospective Associations between a Dietary Index Based on the British Food Standard Agency Nutrient Profiling System and 13-Year Weight Gain in the SU.VI.MAX Cohort. Prev. Med. 2015, 81, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Adriouch, S.; Julia, C.; Kesse-Guyot, E.; Méjean, C.; Ducrot, P.; Péneau, S.; Donnenfeld, M.; Deschasaux, M.; Menai, M.; Hercberg, S.; et al. Prospective Association between a Dietary Quality Index Based on a Nutrient Profiling System and Cardiovascular Disease Risk. Eur. J. Prev. Cardiol. 2016, 23, 1669–1676. [Google Scholar] [CrossRef] [PubMed]
- Aguilera, J.M. The Food Matrix: Implications in Processing, Nutrition and Health. Crit. Rev. Food Sci. Nutr. 2019, 59, 3612–3629. [Google Scholar] [CrossRef] [PubMed]





| Food Group | T1 | T2 | T3 | T4 | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SAFA | iTFA | Sodium | Sugar | Fiber | Energy | SAFA | iTFA | Sodium | Sugar | Fiber | Energy | SAFA | iTFA | Sodium | Sugar | Fiber | Energy | SAFA | iTFA | Sodium | Sugar | Fiber | Energy | ||
| g/100 g | kcal/100 g | g/100 g | kcal/100 g | g/100 g | kcal/100 g | g/100 g | kcal/100 g | ||||||||||||||||||
| Basic food groups | |||||||||||||||||||||||||
| Fruits and vegetables | Fresh fruits and vegetables | All compliant | |||||||||||||||||||||||
| Processed vegetables | 0.10 | 7.0 | 1 | 0.25 | 8.5 | 0.9 | 0.40 | 10.0 | 0.8 | 0.65 | 11.0 | 0.7 | |||||||||||||
| Processed fruit | 1.1 | 11.5 | 1 | 2 | 12.5 | 0.9 | 3 | 14.0 | 0.8 | 4 | 19.0 | 0.7 | |||||||||||||
| Processed beans and legumes | 0.20 | 5.7 | 3.5 | 0.33 | 7.5 | 3.2 | 0.40 | 10.0 | 1.7 | 0.43 | 10.5 | 1.1 | |||||||||||||
| Water | Plain water, tea and coffee | 0.02 | 0.02 | ||||||||||||||||||||||
| Nuts and seeds | (Un)Processed nuts and seeds | 10.0 | 0.10 | 7.5 | 16.0 | 0.43 | 14.0 | 18.0 | 0.55 | 30.0 | 20.0 | 0.73 | 36.0 | ||||||||||||
| Sources of complex carbohydrates | Plain tubers used as staple | All compliant | |||||||||||||||||||||||
| Processed tubers used as staple | 1.1 | 0.10 | 3.0 | 2.7 | 3.0 | 0.35 | 6.5 | 2.2 | 4.0 | 0.40 | 10.0 | 1.5 | 8.0 | 1.60 | 12.0 | 0.8 | |||||||||
| Plain noodles and pasta | 0.10 | 4.0 | 6.0 | 0.20 | 4.2 | 2.8 | 0.48 | 5.0 | 1.0 | 0.80 | 6.0 | 0.5 | |||||||||||||
| Flavored noodles and pasta | 2.0 | 0.50 | 4.0 | 6.0 | 3.5 | 0.93 | 4.2 | 2.8 | 6.5 | 1.20 | 5.0 | 1.0 | 8.0 | 1.50 | 6.0 | 0.5 | |||||||||
| Grains | 1.2 | 0.10 | 4.5 | 6.0 | 1.5 | 0.23 | 6.0 | 2.8 | 1.8 | 0.48 | 10.0 | 1.0 | 4.0 | 1.40 | 12.0 | 0.5 | |||||||||
| Bread | 1.1 | 0.32 | 6.0 | 6.0 | 1.8 | 0.40 | 6.5 | 2.8 | 3.5 | 0.48 | 9.0 | 1.0 | 6.0 | 0.85 | 15.0 | 0.5 | |||||||||
| Breakfast cereals | 3.0 | 0.40 | 10.0 | 6.0 | 3.2 | 0.50 | 14.0 | 2.8 | 3.3 | 0.64 | 15.0 | 1.0 | 4.2 | 0.68 | 26.0 | 0.5 | |||||||||
| Meat, fish, poultry, and eggs | Unprocessed meat, poultry, eggs | 3.2 | 0.15 | 3.7 | 0.17 | 5.3 | 0.40 | 7.5 | 0.68 | ||||||||||||||||
| Processed meat and meat products | 5.0 | 0.45 | 6.0 | 0.60 | 8.0 | 0.68 | 10.0 | 1.30 | |||||||||||||||||
| Fresh, frozen or processed seafood | 6.0 | 0.30 | 6.5 | 0.43 | 7.0 | 0.68 | 7.5 | 1.10 | |||||||||||||||||
| Insects | 3.2 | 0.20 | 3.2 | 0.20 | |||||||||||||||||||||
| Dairy | Milk (-products) | 1.4 | 6.0 | 1.7 | 8.0 | 2.7 | 10.0 | 6.0 | 14.0 | ||||||||||||||||
| Cheese (-products) | 7.5 | 0.40 | 8.5 | 0.50 | 10.0 | 0.60 | 19.0 | 1.20 | 6.0 | ||||||||||||||||
| Oils, fats and fat containing spreads | Oils, fats, spreads | 16.0 | 0.5 | 0.10 | 30.0 | 0.5 | 0.35 | 36.0 | 0.5 | 0.52 | 55.0 | 0.5 | 0.75 | ||||||||||||
| Meals | Main meals | 2.0 | 0.24 | 5.0 | 2.4 | 190 kcal/100 g and 600 kcal/portion | 3.0 | 0.34 | 7.0 | 1.4 | 200 kcal/100 g and 600 kcal/portion | 4.0 | 0.40 | 10.0 | 1.0 | 225 | 5.0 | 0.53 | 11.0 | 0.8 | 275 | ||||
| Sandwiches and rolls | 2.0 | 0.45 | 5.0 | 2.4 | 190 kcal/100 g and 350 kcal/portion | 3.0 | 0.57 | 7.0 | 1.4 | 215 kcal/100 g and 350 kcal/portion | 4.0 | 0.62 | 10.0 | 1.0 | 225 | 5.0 | 0.80 | 11.0 | 0.8 | 275 | |||||
| Soups | 1.1 | 0.25 | 4.0 | 2.0 | 0.29 | 5.0 | 3.5 | 0.35 | 9.0 | 4.0 | 0.39 | 10.0 | |||||||||||||
| Non-basic food groups | |||||||||||||||||||||||||
| Sauces | Meal sauces | 1.1 | 0.40 | 6 | 1.3 | 0.70 | 8 | 2.5 | 2.20 | 16 | 6.0 | 4.50 | 26 | ||||||||||||
| Emulsified sauces | 3 | 0.70 | 10 | 350 | 4.5 | 1.00 | 12 | 380 | 6 | 1.20 | 17 | 550 | 8 | 1.80 | 21 | 650 | |||||||||
| Dark sauces | 3.00 | 16 | 5.50 | 20 | 6.50 | 25.5 | 7.75 | 35 | |||||||||||||||||
| Other sauces (water based) | 0.75 | 16.0 | 100 | 0.80 | 25.0 | 130 | 0.90 | 31.0 | 150 | 1.08 | 39.0 | 190 | |||||||||||||
| Snacks | Savory snacks | 4.0 | 0.4 | 0.40 | 4.0 | 500 | 7.0 | 0.5 | 0.79 | 6.5 | 535 | 9.0 | 0.5 | 0.88 | 9.0 | 540 | 13.0 | 0.5 | 1.00 | 16.0 | 570 | ||||
| Sweet snacks | 6.0 | 0.20 | 20.0 | 220 | 12.0 | 0.22 | 45.0 | 475 | 16.5 | 0.31 | 55.0 | 510 | 20.0 | 0.4 | 0.41 | 62.0 | 550 | ||||||||
| Liquids | Fruit and vegetable juices | 5.0 | 8.0 | 10.0 | 11.0 | ||||||||||||||||||||
| Non-dairy milk substitutes | 1.1 | 0.10 | 5.0 | 1.5 | 0.11 | 6.0 | 2 | 0.12 | 7.2 | 5.5 | 0.13 | 9.0 | |||||||||||||
| Beverages | 2.5 | 5.5 | 8.0 | 11.5 | |||||||||||||||||||||
| Other | All other products | 1.1 or 10 en% | 0.1 or 1 en% | 0.10 | 2.5 or 10 en% | 1.1 or 10 en% | 0.1 or 1 en% | 0.10 | 2.5 or 10 en% | ||||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tognon, G.; Beltramo, B.; Schilpzand, R.; Lissner, L.; Roodenburg, A.J.C.; Don, R.; Nair, K.M.; Nnam, N.; Hamaker, B.; Smorenburg, H. Development of the Choices 5-Level Criteria to Support Multiple Food System Actions. Nutrients 2021, 13, 4509. https://doi.org/10.3390/nu13124509
Tognon G, Beltramo B, Schilpzand R, Lissner L, Roodenburg AJC, Don R, Nair KM, Nnam N, Hamaker B, Smorenburg H. Development of the Choices 5-Level Criteria to Support Multiple Food System Actions. Nutrients. 2021; 13(12):4509. https://doi.org/10.3390/nu13124509
Chicago/Turabian StyleTognon, Gianluca, Belen Beltramo, Rutger Schilpzand, Lauren Lissner, Annet J. C. Roodenburg, Rokiah Don, Krishnapillai Madhavan Nair, Ngozi Nnam, Bruce Hamaker, and Herbert Smorenburg. 2021. "Development of the Choices 5-Level Criteria to Support Multiple Food System Actions" Nutrients 13, no. 12: 4509. https://doi.org/10.3390/nu13124509






