Protective Mechanism of Edible Food Plants against Alcoholic Liver Disease with Special Mention to Polyphenolic Compounds
Abstract
:1. ALD: Epidemiology and Risk Factors
1.1. Alcohol Metabolism
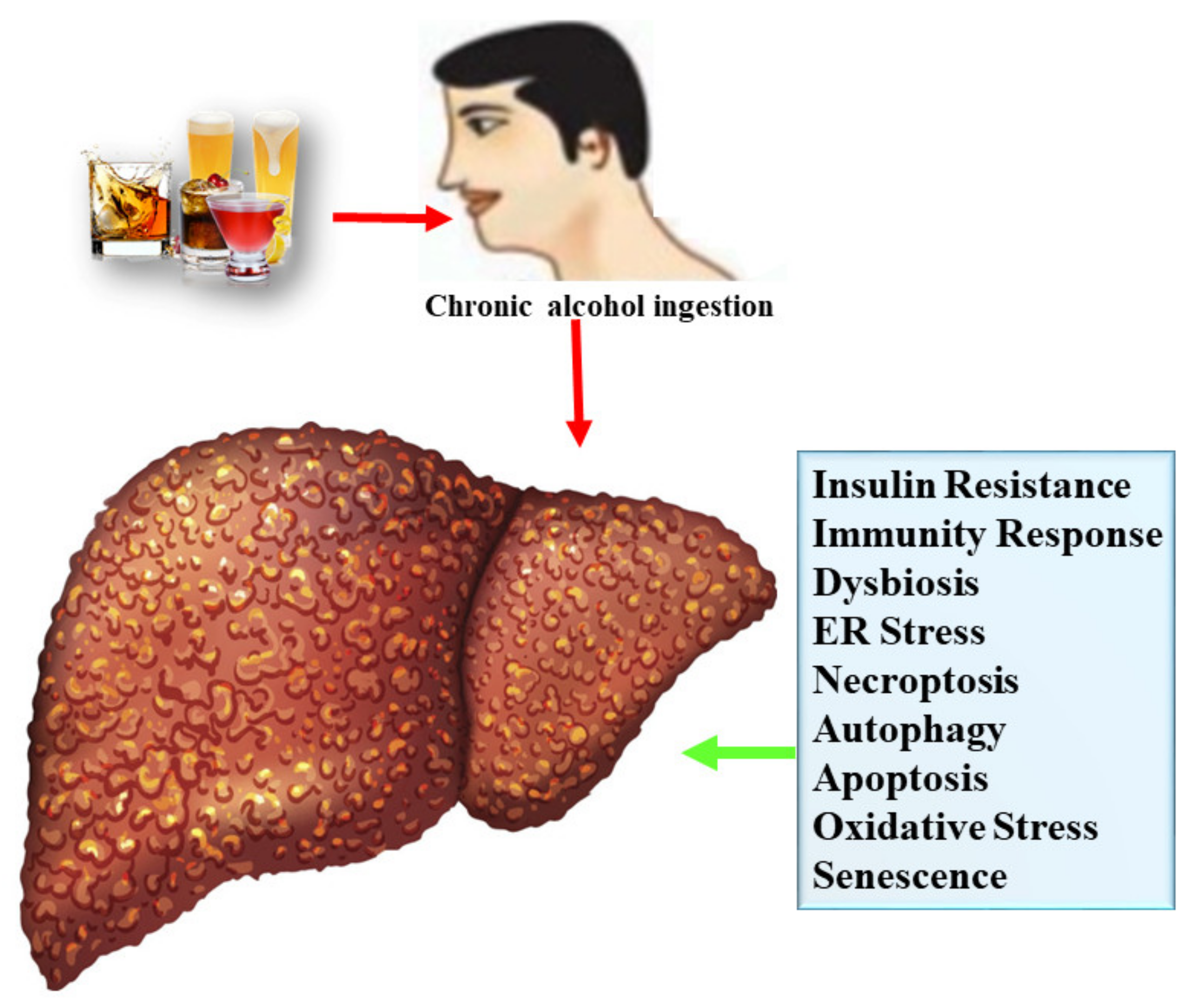
1.2. Mechanisms of Alcoholic Liver Disease
1.2.1. Lipogenesis
1.2.2. Oxidative Stress
1.2.3. Inflammatory Response
1.2.4. Gut Microflora
1.2.5. Endoplasmic Reticulum Stress
1.2.6. Apoptosis
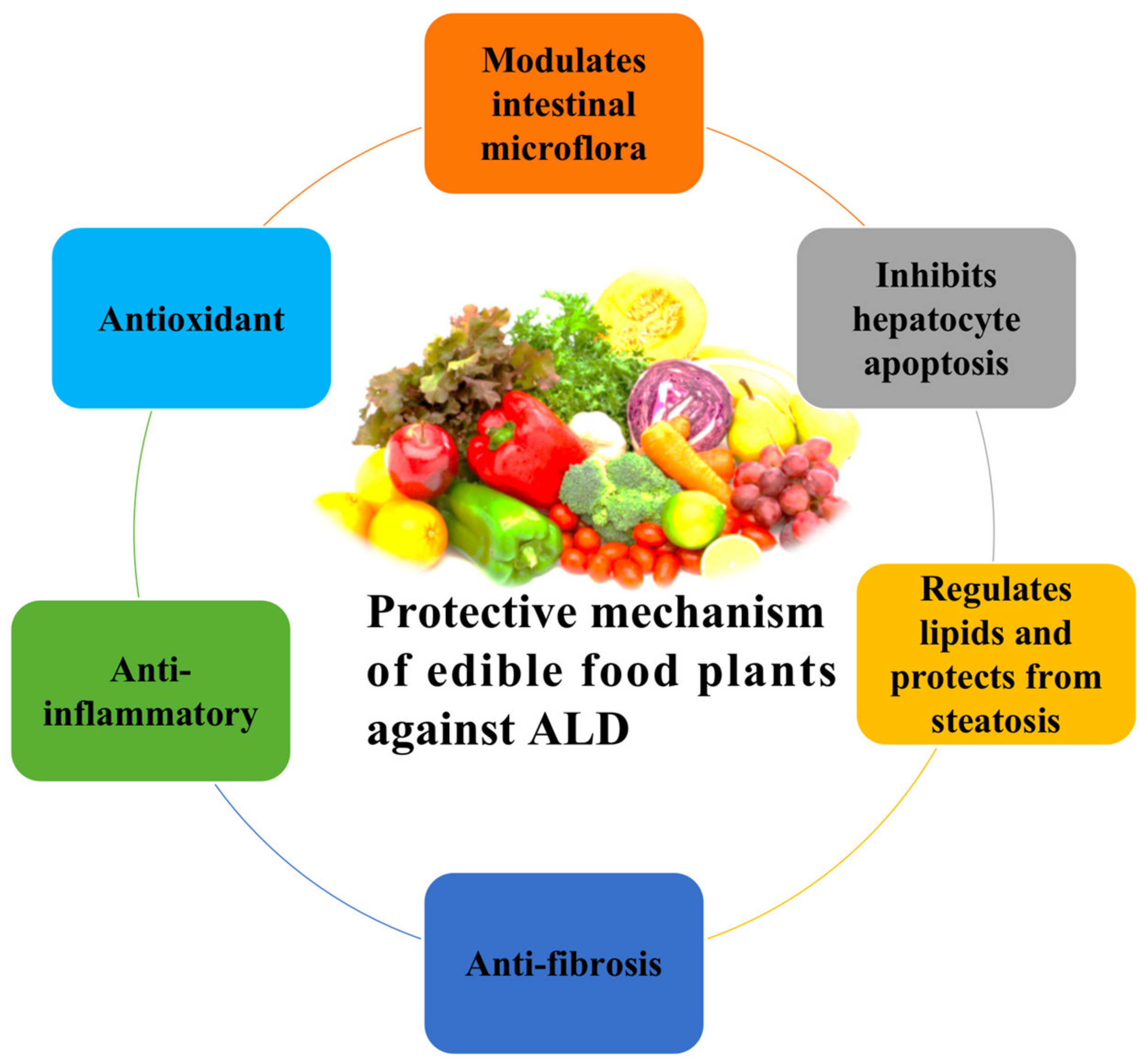
2. Bioactive Compounds Ameliorate ALD via Multiple Pathways
2.1. Flavonoids
2.1.1. Flavonols
2.1.2. Isoflavones
2.1.3. Flavones
2.1.4. Flavanones
2.1.5. Flavan-3-ols
2.1.6. Anthocyanin and Proanthocyanin
2.2. Alkaloids
2.3. Chalcone and Anthraquinone
2.4. Lignans
2.5. Saponins and Terpenoids
2.6. Stilbenes
2.7. Tannins
3. Multicomponent Food Plant Extracts against ALD
3.1. Fruits
3.2. Vegetables
3.3. Spices
3.4. Cereals and Grains
3.5. Tea and Coffee
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Bloomfield, K.; Stockwell, T.; Gmel, G.; Rehn, N. International Comparisons of Alcohol Consumption. Alcohol Res. Health 2003, 27, 95–109. [Google Scholar]
- Faiad, Y.; Khoury, B.; Daouk, S.; Maj, M.; Keeley, J.; Gureje, O.; Reed, G. Frequency of use of the international classification of diseases ICD-10 diagnostic categories for mental and behavioural disorders across world regions. Epidemiol. Psychiatr. Sci. 2018, 27, 568–576. [Google Scholar] [CrossRef]
- Probst, C.; Manthey, J.; Merey, A.; Rylett, M.; Rehm, J. Unrecorded alcohol use: A global modelling study based on nominal group assessments and survey data. Addiction 2018, 113, 1231–1241. [Google Scholar] [CrossRef] [PubMed]
- Room, R. The relation between blood alcohol content and clinically assessed intoxication: Lessons from applying the ICD-10 Y90 and Y91 codes in the emergency room. In Alcohol and Injuries: Emergency Department Studies in an International Perspective; Cherpitel, C.J., Borges, G., Hungerford, D., Peden, M., Poznyak, V., Room, R., Stockwell, T., Eds.; WHO: Geneva, Switzerland, 2009; pp. 135–146. [Google Scholar]
- World Health Organization. Global Status Report on Alcohol and Health 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/112736/9789240692763_eng.pdf?sequence=1&isAllowed=y (accessed on 6 April 2021).
- Peacock, A.; Leung, J.; Larney, S.; Colledge, S.; Hickman, M.; Rehm, J.; Giovino, G.A.; West, R.; Hall, W.; Griffiths, P.; et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction 2018, 113, 1905–1926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, W.R.; Brown, R.S.; Terrault, N.A.; El-Serag, H. Burden of liver disease in the United States: Summary of a workshop. Hepatology 2002, 36, 227–242. [Google Scholar] [CrossRef]
- Nephew, T.M.; Williams, G.D.; Yi, H.; Hoy, A.K.; Stinson, F.S.; Dufour, M.C. Surveillance Report #59: Apparent Per Capita Alcohol Consumption: National, State, and Regional Trends, 1977–2000; NIAAA, Division of Biometry and Epidemiology, Alcohol Epidemiologic Data System: Rockville, MD, USA, 2003. [Google Scholar]
- Jiang, H.; Xiang, X.; Hao, W.; Room, R.; Zhang, X.; Wang, X. Measuring and preventing alcohol use and related harm among young people in Asian countries: A thematic review. Glob. Health Res. Policy 2018, 3, 14. [Google Scholar] [CrossRef] [Green Version]
- Kourkoumpetis, T.; Sood, G. Pathogenesis of Alcoholic Liver Disease: An Update. Clin. Liver Dis. 2019, 23, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Edenberg, H.J. The genetics of alcohol metabolism: Role of alcohol dehydrogenase and aldehyde dehydrogenase variants. Alcohol Res. Health 2007, 30, 5–13. [Google Scholar] [PubMed]
- Purohit, V.; Gao, B.; Song, B.J. Molecular mechanisms of alcoholic fatty liver. Alcohol. Clin. Exp. Res. 2009, 33, 191–205. [Google Scholar] [CrossRef] [Green Version]
- Craemer, D.D.; Pauwels, M.; Branden, C.V. Morphometric characteristics of human hepatocellular peroxisomes in alcoholic liver disease. Alcohol. Clin. Exp. Res. 1996, 20, 908–913. [Google Scholar] [CrossRef]
- You, M.; Matsumoto, M.; Pacold, C.M.; Cho, W.K.; Crabb, D.W. The role of AMP-activated protein kinase in the action of ethanol in the liver. Gastroenterology 2004, 127, 1798–1808. [Google Scholar] [CrossRef]
- Israel, Y.; Videla, L.; Fernandez Videla, V.; Bernstein, J. Effects of chronic ethanol treatment and thyroxine administration on ethanol metabolism and liver oxidative capacity. J. Pharmacol. Exp. Ther. 1975, 192, 565–574. [Google Scholar] [PubMed]
- Amet, Y.; Lucas, D.; Zhang-Gouillon, Z.Q.; French, S.W. P-450-dependent metabolism of lauric acid in alcoholic liver disease: Comparison between rat liver and kidney microsomes. Alcohol. Clin. Exp. Res. 1998, 22, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Watkins, P.B. Role of cytochromes P450 in drug metabolism and hepatotoxicity. Semin. Liver Dis. 1990, 10, 235–250. [Google Scholar] [CrossRef]
- McKillop, I.H.; Schrum, L.W.; Thompson, K.J. Role of alcohol in the development and progression of hepatocellular carcinoma. Hepatic Oncol. 2016, 3, 29–43. [Google Scholar] [CrossRef]
- Teschke, R. Alcoholic steatohepatitis (ASH) and alcoholic hepatitis (AH): Cascade of events, clinical aspects, and pharmacotherapy options. Expert Opin. Pharmacother. 2018, 19, 779–793. [Google Scholar] [CrossRef] [PubMed]
- Baraona, E.; Lieber, C.S. Effects of ethanol on lipid metabolism. J. Lipid Res. 1979, 20, 289–315. [Google Scholar] [CrossRef]
- You, M.; Fischer, M.; Deeg, M.A.; Crabb, D.W. Ethanol induces fatty acid synthesis pathways by activation of sterol regulatory element-binding protein (SREBP). J. Biol. Chem. 2002, 277, 29342–29347. [Google Scholar] [CrossRef] [Green Version]
- Galli, A.; Pinaire, J.; Fischer, M.; Dorris, R.; Crabb, D.W. The transcriptional and DNA binding activity of peroxisome proliferator-activated receptor α is inhibited by ethanol metabolism. A novel mechanism for the development of ethanol-induced fatty liver. J. Biol. Chem. 2001, 276, 68–75. [Google Scholar] [CrossRef] [Green Version]
- Parker, R.; Kim, S.J.; Gao, B. Alcohol, adipose tissue and liver disease: Mechanistic links and clinical considerations. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 50–59. [Google Scholar] [CrossRef]
- Gao, B.; Bataller, R. Alcoholic liver disease: Pathogenesis and new therapeutic targets. Gastroenterology 2011, 141, 1572–1585. [Google Scholar] [CrossRef] [Green Version]
- Lackner, C.; Tiniakos, D. Fibrosis and alcohol-related liver disease. J. Hepatol. 2019, 70, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Sancho-Bru, P.; Altamirano, J.; Rodrigo-Torres, D.; Coll, M.; Millán, C.; José Lozano, J.; Miquel, R.; Arroyo, V.; Caballería, J.; Ginès, P.; et al. Liver progenitor cell markers correlate with liver damage and predict short-term mortality in patients with alcoholic hepatitis. Hepatology 2012, 55, 1931–1941. [Google Scholar] [CrossRef]
- IARC (WHO). A review of human carcinogens. IARC Monogr. Eval. Carcinog. Risks Hum. 2012, 100, 377–503. [Google Scholar]
- Testino, G. Alcoholic hepatitis. J. Med. Life 2013, 6, 161–167. [Google Scholar]
- Gudowska, M.; Wojtowicz, E.; Cylwik, B.; Gruszewska, E.; Chrostek, L. The distribution of liver steatosis, fibrosis, steatohepatitis and inflammation activity in alcoholics according to FibroMax test. Adv. Clin. Exp. Med. 2015, 24, 823–827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osna, N.A.; Donohue, T.M.; Kharbanda, K.K. Alcoholic Liver Disease: Pathogenesis and Current Management. Alcohol Res. 2017, 38, 147–161. [Google Scholar]
- Fischer, M.; You, M.; Matsumoto, M.; Crabb, D.W. Peroxisome proliferator activated receptor alpha (PPARalpha) agonist treatment reverses PPARalpha dysfunction and abnormalities in hepatic lipid metabolism in ethanol-fed mice. J. Biol. Chem. 2003, 278, 27997–28004. [Google Scholar] [CrossRef] [Green Version]
- Albano, E.; Clot, P.; Morimoto, M.; Tomasi, A.; Ingelman-Sundberg, M.; French, S.W. Role of cytochrome P4502E1-dependent formation of hydroxyethyl free radical in the development of liver damage in rats intragastrically fed with ethanol. Hepatology 1996, 23, 155–163. [Google Scholar] [CrossRef]
- Mueller, S.; Peccerella, T.; Qin, H.; Glassen, K.; Waldherr, R.; Flechtenmacher, C.; Straub, B.K.; Millonig, G.; Stickel, F.; Bruckner, T.; et al. Carcinogenic Etheno DNA Adducts in Alcoholic Liver Disease: Correlation with Cytochrome P-4502E1 and Fibrosis. Alcohol. Clin. Exp. Res. 2018, 42, 252–259. [Google Scholar] [CrossRef]
- Linhart, K.; Bartsch, H.; Seitz, H.K. The role of reactive oxygen species (ROS) and cytochrome P-450 2E1 in the generation of carcinogenic etheno-DNA adducts. Redox Biol. 2014, 3, 56–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, T.M.; Nieto, N. CYP2E1 and oxidant stress in alcoholic and non-alcoholic fatty liver disease. J. Hepatol. 2013, 58, 395–398. [Google Scholar] [CrossRef] [Green Version]
- Bailey, S.M.; Cunningham, C.C. Contribution of mitochondria to oxidative stress associated with alcoholic liver disease. Free Radic. Biol. Med. 2002, 32, 11–16. [Google Scholar] [CrossRef]
- García-Ruiz, C.; Colell, A.; París, R.; Fernández-Checa, J.C. Direct interaction of GD3 ganglioside with mitochondria generates reactive oxygen species followed by mitochondrial permeability transition, cytochrome c release, and caspase activation. FASEB J. 2000, 14, 847–858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chamulitrat, W.; Spitzer, J.J. Nitric oxide and liver injury in alcohol-fed rats after lipopolysaccharide administration. Alcohol. Clin. Exp. Res. 1996, 20, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Lieber, C.S.; Cao, Q.; Decarli, L.M.; Leo, M.A.; Mak, K.M.; Ponomarenko, A.; Ren, C.; Wang, X. Role of medium-chain triglycerides in the alcohol-mediated cytochrome P450 2E1 induction of mitochondria. Alcohol. Clin. Exp. Res. 2007, 31, 1660–1668. [Google Scholar] [CrossRef] [PubMed]
- Harrison-Findik, D.D.; Schafer, D.; Klein, E.; Timchenko, N.A.; Kulaksiz, H.; Clemens, D.; Fein, E.; Andriopoulos, B.; Pantopoulos, K.; Gollan, J. Alcohol metabolism-mediated oxidative stress down-regulates hepcidin transcription and leads to increased duodenal iron transporter expression. J. Biol. Chem. 2006, 281, 22974–22982. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.J.; Gao, B.; Zakhari, S.; Nagy, L.E. Inflammation in alcoholic liver disease. Annu. Rev. Nutr. 2012, 32, 343–368. [Google Scholar] [CrossRef] [Green Version]
- Pritchard, M.T.; Mcmullen, M.R.; Stavitsky, A.B.; Cohen, J.I.; Lin, F.; Medof, M.E.; Nagy, L.E. Differential contributions of C3, C5, and decay-accelerating factor to ethanol-induced fatty liver in mice. Gastroenterology 2007, 132, 1117–1126. [Google Scholar] [CrossRef] [Green Version]
- Maltby, J.; Wright, S.; Bird, G.; Sheron, N. Chemokine levels in human liver homogenates: Associations between GRO α and histopathological evidence of alcoholic hepatitis. Hepatology 1996, 24, 1156–1160. [Google Scholar]
- Petrasek, J.; Mandrekar, P.; Szabo, G. Toll-like receptors in the pathogenesis of alcoholic liver disease. Gastroent. Res. Pract. 2010, 2010, 710381. [Google Scholar] [CrossRef]
- Lawrence, T.; Bebien, M.; Liu, G.Y.; Nizet, V.; Karin, M. IKKα limits macrophage NF-κB activation and contributes to the resolution of inflammation. Nature 2005, 434, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Park, C.M.; Youn, H.J.; Chang, H.K.; Song, Y.S. TOP1 and 2, polysaccharides from Taraxacum officinale, attenuate CCl4-induced hepatic damage through the modulation of NF-κB and its regulatory mediators. Food Chem. Toxicol. 2010, 48, 1255–1261. [Google Scholar] [CrossRef] [PubMed]
- Bukong, T.N.; Iracheta-Vellve, A.; Gyongyosi, B.; Ambade, A.; Catalano, D.; Kodys, K.; Szabo, G. Therapeutic Benefits of Spleen Tyrosine Kinase Inhibitor Administration on Binge Drinking-Induced Alcoholic Liver Injury, Steatosis, and Inflammation in Mice. Alcohol. Clin. Exp. Res. 2016, 40, 1524–1530. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.E.; Ha, J.S.; Park, H.Y.; Lee, E. Alteration of gut microbiota composition by short-term low-dose alcohol intake is restored by fermented rice liquor in mice. Food Res. Int. 2020, 128, 108800. [Google Scholar] [CrossRef]
- Meroni, M.; Longo, M.; Dongiovanni, P. Alcohol or Gut Microbiota: Who Is the Guilty? Int. J. Mol. Sci. 2019, 20, 4568. [Google Scholar] [CrossRef] [Green Version]
- Bjorkhaug, S.T.; Aanes, H.; Neupane, S.P.; Bramness, J.G.; Malvik, S.; Henriksen, C.; Skar, V.; Medhus, A.W.; Valeur, J. Characterization of gut microbiota composition and functions in patients with chronic alcohol overconsumption. Gut Microbes 2019, 10, 663–675. [Google Scholar] [CrossRef] [Green Version]
- Guerra Ruiz, A.; Casafont, F.; Crespo, J.; Cayón, A.; Mayorga, M.; Estebanez, A.; Fernadez-Escalante, J.C.; Pons-Romero, F. Lipopolysaccharide-binding protein plasma levels and liver TNF-alpha gene expression in obese patients: Evidence for the potential role of endotoxin in the pathogenesis of non-alcoholic steatohepatitis. Obes. Surg. 2007, 17, 1374–1380. [Google Scholar] [CrossRef]
- Yang, S.Q.; Lin, H.Z.; Lane, M.D.; Clemens, M.; Diehl, A.M. Obesity increases sensitivity to endotoxin liver injury: Implications for the pathogenesis of steatohepatitis. Proc. Natl. Acad. Sci. USA 1997, 94, 2557–2562. [Google Scholar] [CrossRef] [Green Version]
- Staun-Olsen, P.; Bjorneboe, M.; Prytz, H.; Thomsen, A.C.; Orskov, F. Escherichia coli antibodies in alcoholic liver disease. Correlation to alcohol consumption, alcoholic hepatitis, and serum IgA. Scand. J. Gastroenterol. 1983, 18, 889–896. [Google Scholar] [CrossRef]
- Bode, C.; Kugler, V.; Bode, J.C. Endotoxemia in patients with alcoholic and non-alcoholic cirrhosis and in subjects with no evidence of chronic liver disease following acute alcohol excess. J. Hepatol. 1987, 4, 8–14. [Google Scholar] [CrossRef]
- Rao, R. Endotoxemia and gut barrier dysfunction in alcoholic liver disease. Hepatology 2009, 50, 638–644. [Google Scholar] [CrossRef]
- Kosnicki, K.L.; Penprase, J.C.; Cintora, P.; Torres, P.J.; Harris, G.L.; Brasser, S.M.; Kelley, S.T. Effects of moderate, voluntary ethanol consumption on the rat and human gut microbiome. Addict. Biol. 2019, 24, 617–630. [Google Scholar] [CrossRef]
- Malhi, H.; Kaufman, R.J. Endoplasmic reticulum stress in liver disease. J. Hepatol. 2011, 54, 795–809. [Google Scholar] [CrossRef] [Green Version]
- Louvet, A.; Mathurin, P. Alcoholic liver disease: Mechanisms of injury and targeted treatment. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 231–242. [Google Scholar] [CrossRef]
- Ji, C. Dissection of endoplasmic reticulum stress signaling in alcoholic and non-alcoholic liver injury. J. Gastroenterol. Hepatol. 2008, 23 (Suppl. 1), S16–S24. [Google Scholar] [CrossRef] [Green Version]
- Kaplowitz, N.; Ji, C. Unfolding new mechanisms of alcoholic liver disease in the endoplasmic reticulum. J. Gastroenterol. Hepatol. 2006, 21 (Suppl. 3), S7–S9. [Google Scholar] [CrossRef]
- Ji, C.; Chan, C.; Kaplowitz, N. Predominant role of sterol response element binding proteins (SREBP) lipogenic pathways in hepatic steatosis in the murine intragastric ethanol feeding model. J. Hepatol. 2006, 45, 717–724. [Google Scholar] [CrossRef]
- Ji, C.; Kaplowitz, N. Betaine decreases hyperhomocysteinemia, endoplasmic reticulum stress, and liver injury in alcohol-fed mice. Gastroenterology 2003, 124, 1488–1499. [Google Scholar] [CrossRef]
- Decker, R.H.; Dai, Y.; Grant, S. The cyclin-dependent kinase inhibitor flavopiridol induces apoptosis in human leukemia cells (U937) through the mitochondrial rather than the receptor-mediated pathway. Cell Death Differ. 2001, 8, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Hao, F.; Cubero, F.J.; Ramadori, P.; Liao, L.; Haas, U.; Lambertz, D.; Sonntag, R.; Bangen, J.M.; Gassler, N.; Hoss, M.; et al. Inhibition of Caspase-8 does not protect from alcohol-induced liver apoptosis but alleviates alcoholic hepatic steatosis in mice. Cell Death Dis. 2017, 8, e3152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castilla, R.; González, R.; Fouad, D.; Fraga, E.; Muntané, J. Dual effect of ethanol on death in primary culture of human and rat hepatocytes. Alcohol Alcohol. 2004, 39, 290–296. [Google Scholar] [CrossRef] [Green Version]
- Thurman, R.G.; Bradford, B.U.; Iimuro, Y.; Frankenberg, M.V.; Knecht, K.T.; Connor, H.D.; Adachi, Y.; Wall, C.; Arteel, G.E.; Raleigh, J.A.; et al. Mechanisms of alcohol-induced hepatotoxicity: Studies in rats. Front. Biosci. 1999, 4, e42–e46. [Google Scholar] [PubMed]
- Wang, K.; Wan, Z.; Ou, A.; Liang, X.; Guo, X.; Zhang, Z.; Wu, L.; Xue, X. Monofloral honey from a medical plant, Prunella Vulgaris, protected against dextran sulfate sodium-induced ulcerative colitis via modulating gut microbial populations in rats. Food Funct. 2019, 10, 3828–3838. [Google Scholar]
- Wang, K.; Jin, X.; Li, Q.; Sawaya, A.C.H.F.; Le Leu, R.K.; Conlon, M.A.; Wu, L.; Hu, F. Propolis from different geographic origins decreases intestinal inflammation and Bacteroides spp. populations in a model of DSS-Induced colitis. Mol. Nutr. Food Res. 2018, 62, 1800080. [Google Scholar]
- Zeng, H.; Guo, X.; Zhou, F.; Xiao, L.; Liu, J.; Jiang, C.; Xing, M.; Yao, P. Quercetin alleviates ethanol-induced liver steatosis associated with improvement of lipophagy. Food Chem. Toxicol. 2019, 125, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, J.; Lee, H.; Sung, J. Relative protective activities of quercetin, quercetin-3-glucoside, and rutin in alcohol-induced liver injury. J. Food Biochem. 2019, 43, e13002. [Google Scholar] [CrossRef]
- Simón, J.; Casado-Andrés, M.; Goikoetxea-Usandizaga, N.; Serrano-Maciá, M.; Martínez-Chantar, M.L. Nutraceutical Properties of Polyphenols against Liver Diseases. Nutrients 2020, 12, 3517. [Google Scholar] [CrossRef]
- Mohib, M.; Afnan, K.; Paran, T.Z.; Khan, S.; Sarker, J.; Hasan, N.; Hasan, I.; Sagor, A.T. Beneficial Role of Citrus Fruit Polyphenols Against Hepatic Dysfunctions: A Review. J. Diet. Suppl. 2018, 15, 223–250. [Google Scholar] [CrossRef]
- Vergani, L.; Vecchione, G.; Baldini, F.; Grasselli, E.; Voci, A.; Portincasa, P.; Ferrari, P.F.; Aliakbarian, B.; Casazza, A.A.; Perego, P. Polyphenolic extract attenuates fatty acid-induced steatosis and oxidative stress in hepatic and endothelial cells. Eur. J. Nutr. 2018, 57, 1793–1805. [Google Scholar] [CrossRef]
- Li, Y.; Chen, M.; Wang, J.; Guo, X.; Xiao, L.; Liu, P.; Liu, L.; Tang, Y.; Yao, P. Quercetin ameliorates autophagy in alcohol liver disease associated with lysosome through mTOR-TFEB pathway. J. Funct. Foods 2019, 52, 177–185. [Google Scholar] [CrossRef]
- Sun, Q.; Zhang, W.; Zhong, W.; Sun, X.; Zhou, Z. Dietary Fisetin Supplementation Protects Against Alcohol-Induced Liver Injury in Mice. Alcohol. Clin. Exp. Res. 2016, 40, 2076–2084. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koneru, M.; Sahu, B.D.; Kumar, J.M.; Kuncha, M.; Kadari, A.; Kilari, E.K.; Sistla, R. Fisetin protects liver from binge alcohol-induced toxicity by mechanisms including inhibition of matrix metalloproteinases (MMPs) and oxidative stress. J. Funct. Foods 2016, 22, 588–601. [Google Scholar] [CrossRef]
- Banerjee, P.; Sayantan, J.; Chakraborty, S.; Swarnakar, S. Inflammation and MMPs in Alcohol-induced Liver Diseases and Protective Action of Antioxidants. Indian J. Biochem. Biophys. 2013, 50, 377–386. [Google Scholar]
- Mishra, A.; Paul, S.; Swarnakar, S. Down regulation of matrix metalloproteinase-9 by melatonin during prevention of alcohol-induced liver injury in mice. Biochimie 2011, 93, 854–866. [Google Scholar] [CrossRef]
- Silva, J.; Yu, X.; Moradian, R.; Folk, C.; Spatz, M.H.; Kim, P.; Bhatti, A.A.; Davies, D.L.; Liang, J. Dihydromyricetin Protects the Liver via Changes in Lipid Metabolism and Enhanced Ethanol Metabolism. Alcohol. Clin. Exp. Res. 2020, 44, 1046–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhakuni, G.S.; Bedi, O.; Bariwal, J.; Kumar, P. Hepatoprotective activity of morin and its semi-synthetic derivatives against alcohol induced hepatotoxicity in rats. Indian J. Physiol. Pharmacol. 2017, 61, 175–190. [Google Scholar]
- Suzuki, T.; Tanabe, S.; Hara, H. Kaempferol enhances intestinal barrier function through the cytoskeletal association and expression of tight junction proteins in Caco-2 cells. J. Nutr. 2011, 141, 87–94. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.; Sun, J.; Jiang, Z.; Xie, W.; Zhang, X. Hepatoprotective effect of kaempferol against alcoholic liver injury in mice. Am. J. Chin. Med. 2015, 43, 241–254. [Google Scholar] [CrossRef] [Green Version]
- French, S.W. The Importance of CYP2E1 in the pathogenesis of alcoholic liver disease and drug toxicity and the role of the proteasome. Subcell Biochem. 2013, 67, 145–164. [Google Scholar]
- Chen, J.; Xuan, Y.H.; Luo, M.X.; Ni, X.G.; Ling, L.Q.; Hu, S.J.; Chen, J.Q.; Xu, J.Y.; Jiang, L.Y.; Si, W.Z.; et al. Kaempferol alleviates acute alcoholic liver injury in mice by regulating intestinal tight junction proteins and butyrate receptors and transporters. Toxicology 2020, 429, 152338. [Google Scholar] [CrossRef]
- Zhao, L.; Wang, Y.; Liu, J.; Wang, K.; Guo, X.; Ji, B.; Wu, W.; Zhou, F. Protective Effects of Genistein and Puerarin against Chronic Alcohol-Induced Liver Injury in Mice via Antioxidant, Anti-inflammatory, and Anti-apoptotic Mechanisms. J. Agric. Food Chem. 2016, 64, 7291–7297. [Google Scholar] [CrossRef]
- Leelananthakul, W.; Werawatganon, D.; Klaikeaw, N.; Maneerat Chayanupatkul, M.; Siriviriyakul, P. Protective effects of genistein alleviate alcohol-induced liver injury in rats. Pharmacogn. Mag. 2019, 15, 342–347. [Google Scholar]
- Xiong, Y.; Yang, Y.; Yang, J.; Chai, H.; Li, Y.; Yang, J.; Jia, Z.; Wang, Z. Tectoridin, an isoflavone glycoside from the flower of Pueraria lobata, prevents acute ethanol-induced liver steatosis in mice. Toxicology 2010, 276, 64–72. [Google Scholar] [CrossRef]
- Zhang, Q.Y.; Zheng, W.; Khaskheli, S.G.; Huang, W. In Vivo Evaluation of Tectoridin from Puerariae flos on anti-alcoholism Property in Rats. J. Food Nutr. Res. 2019, 7, 458–464. [Google Scholar] [CrossRef]
- Liu, G.; Zhang, Y.; Liu, C.; Xu, D.; Zhang, R.; Cheng, Y.; Pan, Y.; Huang, C.; Chen, Y. Luteolin alleviates alcoholic liver disease induced by chronic and binge ethanol feeding in mice. J. Nutr. 2014, 144, 1009–1015. [Google Scholar] [CrossRef] [Green Version]
- Li, H.D.; Chen, X.; Yang, Y.; Huang, H.M.; Zhang, L.; Zhang, X.; Zhang, L.; Huang, C.; Meng, X.M.; Li, J. Wogonin attenuates inflammation by activating PPAR-gamma in alcoholic liver disease. Int. Immunopharmacol. 2017, 50, 95–106. [Google Scholar] [CrossRef]
- Xi, Y.; Wu, M.; Li, H.; Dong, S.; Luo, E.; Gu, M.; Shen, X.; Jiang, Y.; Liu, Y.; Liu, H. Baicalin attenuates high fat diet-induced obesity and liver dysfunction: Dose-response and potential role of CaMKKβ/AMPK/ACC pathway. Cell Physiol. Biochem. 2015, 35, 2349–2359. [Google Scholar] [CrossRef]
- He, P.; Wu, Y.; Shun, J.; Liang, Y.; Cheng, M.; Wang, Y. Baicalin ameliorates liver injury induced by chronic plus binge ethanol feeding by modulating oxidative stress and inflammation via CYP2E1 and NRF2 in mice. Oxid. Med. Cell. Longev. 2017, 2017, 4820414. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, Y.; Bai, R.; Wang, M.; Du, S. Baicalin attenuates alcoholic liver injury through modulation of hepatic oxidative stress, inflammation and sonic hedgehog pathway in rats. Cell Physiol. Biochem. 2016, 39, 1129–1140. [Google Scholar] [CrossRef]
- Wang, F.; Liu, J.C.; Zhou, R.J.; Zhao, X.; Liu, M.; Ye, H.; Xie, M.L. Apigenin protects against alcohol-induced liver injury in mice by regulating hepatic CYP2E1-mediated oxidative stress and PPARα-mediated lipogenic gene expression. Chem. Biol. Interact. 2017, 275, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Tahir, M.; Sultana, S. Chrysin modulates ethanol metabolism in Wistar rats: A promising role against organ toxicities. Alcohol Alcohol. 2011, 46, 383–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, C.; Lai, Y.; Huang, P.; Xie, L.; Lin, H.; Zhou, Z.; Mo, C.; Deng, G.; Yan, W.; Gao, Z.; et al. Naringin attenuates alcoholic liver injury by reducing lipid accumulation and oxidative stress. Life Sci. 2019, 216, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Zhou, Z.; Zhong, W.; Huang, P.; Ma, N.; Zhang, Y.; Zhou, C.; Lai, Y.; Huang, S.; An, H.; et al. Naringenin inhibits alcoholic injury by improving lipid metabolism and reducing apoptosis in zebrafish larvae. Oncol. Rep. 2017, 38, 2877–2884. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhong, W.; Lin, H.; Huang, P.; Ma, N.; Zhang, Y.; Zhou, C.; Lai, Y.; Huang, S.; Huang, S.; et al. Hesperidin Protects against Acute Alcoholic Injury through Improving Lipid Metabolism and Cell Damage in Zebrafish Larvae. Evid. Based Complement. Altern. Med. 2017, 2017, 7282653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuan, G.; Gong, Z.; Zhou, X.; Zhang, P.; Sun, X.; Li, X. Epigallocatechin-3-Gallate Ameliorates Alcohol-Induced Liver Injury in Rats. Int. J. Mol. Sci. 2006, 7, 204–219. [Google Scholar] [CrossRef] [Green Version]
- Yun, J.W.; Kim, Y.K.; Lee, B.S.; Kim, C.W.; Hyun, J.S.; Baik, J.H.; Kim, J.J.; Kim, B.H. Effect of dietary epigallocatechin-3-gallate on cytochrome P450 2E1-dependent alcoholic liver damage: Enhancement of fatty acid oxidation. Biosci. Biotechnol. Biochem. 2007, 71, 2999–3006. [Google Scholar] [CrossRef] [Green Version]
- Kaviarasan, S.; Sundarapandiyan, R.; Anuradha, C.V. Epigallocatechin gallate, a green tea phytochemical, attenuates alcohol-induced hepatic protein and lipid damage. Toxicol. Mech. Methods 2008, 18, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Rishi, P.; Arora, S.; Kaur, U.J.; Chopra, K.; Kaur, I.P. Better management of alcohol liver disease using a “microstructured synbox” system comprising L. plantarum and EGCG. PLoS ONE 2017, 12, e0168459. [Google Scholar] [CrossRef]
- Bharrhan, S.; Koul, A.; Chopra, K.; Rishi, P. Catechin suppresses an array of signalling molecules and modulates alcohol-induced endotoxin mediated liver injury in a rat model. PLoS ONE 2011, 6, e20635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, P.; Wang, F.; Wong, N.K.; Lv, Y.; Li, X.; Li, M.; Tipoe, G.L.; So, K.F.; Xu, A.; Chen, S.; et al. Divergent Roles of Kupffer Cell TLR2/3 Signaling in Alcoholic Liver Disease and the Protective Role of EGCG. Cell. Mol. Gastroenterol. Hepatol. 2020, 9, 145–160. [Google Scholar] [CrossRef]
- Hou, Z.; Qin, P.; Ren, G. Effect of anthocyanin-rich extract from black rice (Oryza sativa L. Japonica) on chronically alcohol-induced liver damage in rats. J. Agric. Food Chem. 2010, 58, 3191–3196. [Google Scholar] [CrossRef]
- Wan, T.; Wang, S.; Ye, M.; Ling, W.; Yang, L. Cyanidin-3-O-β-glucoside protects against liver fibrosis induced by alcohol via regulating energy homeostasis and AMPK/autophagy signaling pathway. J. Funct. Foods 2017, 37, 16–24. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, S.; Wan, T.; Huang, Y.; Pang, N.; Jiang, X.; Gu, Y.; Zhang, Z.; Luo, J.; Yang, L. Cyanidin-3-O-β-glucoside inactivates NLRP3 inflammasome and alleviates alcoholic steatohepatitis via SirT1/NF-κB signaling pathway. Free Radic. Biol. Med. 2020, 160, 334–341. [Google Scholar] [CrossRef]
- Yang, L.; Wan, T.; Wang, S.; Ye, M.; Pei, L.; Jiang, R.; Qiu, Y. Protective effect of anthocyanin on alcohol-induced liver fibrosis is due to the regulation on AMPK/mTOR/autophagy pathway and energy status. FASEB J. 2017, 31, 646.40. [Google Scholar]
- Choi, H.; Kim, J.; Park, J.; Noh, S.K. Beneficial effect of blueberry wine on alcoholic fatty liver in rats. FASEB J. 2013, 27, lb290. [Google Scholar]
- Zhu, J.; Ren, T.; Zhou, M.; Cheng, M. The combination of blueberry juice and probiotics reduces apoptosis of alcoholic fatty liver of mice by affecting SIRT1 pathway. Drug Des. Dev. Ther. 2016, 10, 1649–1661. [Google Scholar]
- Zuo, A.; Wang, S.; Liu, L.; Yao, Y.; Guo, J. Understanding the effect of anthocyanin extracted from Lonicera caerulea L. on alcoholic hepatosteatosis. Biomed. Pharmacother. 2019, 117, 109087. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, Y.; Zhao, X.; Liu, S.; Liu, Y.; Wang, D. Aronia melanocarpa Prevents Alcohol-Induced Chronic Liver Injury via Regulation of Nrf2 Signaling in C57BL/6 Mice. Oxid. Med. Cell Longev. 2020, 2020, 4054520. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Su, B.; Fan, S.; Fei, H.; Zhao, W. Protective effect of oligomeric proanthocyanidins against alcohol-induced liver steatosis and injury in mice. Biochem. Biophys. Res. Commun. 2015, 458, 757–762. [Google Scholar] [CrossRef]
- Zhang, P.; Ma, D.; Wang, Y.; Zhang, M.; Qiang, X.; Liao, M.; Liu, X.; Wu, H.; Zhang, Y. Berberine protects liver from ethanol-induced oxidative stress and steatosis in mice. Food Chem. Toxicol. 2014, 74, 225–232. [Google Scholar] [CrossRef]
- Li, S.; Wang, N.; Tan, H.Y.; Chueng, F.; Zhang, Z.J.; Yuen, M.F.; Feng, Y. Modulation of gut microbiota mediates berberine-induced expansion of immuno-suppressive cells to against alcoholic liver disease. Clin. Transl. Med. 2020, 10, e112. [Google Scholar] [CrossRef]
- Shu, G.; Qiu, Y.; Hao, J.; Fu, Q.; Deng, X. Nuciferine alleviates acute alcohol-induced liver injury in mice: Roles of suppressing hepatic oxidative stress and inflammation via modulating miR-144/Nrf2/HO-1 cascade. J. Funct. Foods 2019, 58, 105–113. [Google Scholar] [CrossRef]
- He, Y.; Liu, Q.; Li, Y.; Yang, X.; Wang, W.; Li, T.; Zhang, W.; Cui, Y.; Wang, C.; Lin, R. Protective effects of hydroxysafflor yellow A (HSYA) on alcohol-induced liver injury in rats. J. Physiol. Biochem. 2015, 71, 69–78. [Google Scholar] [CrossRef]
- Kong, X.; Wu, G.; Chen, S.; Zhang, L.; Li, F.; Shao, T.; Ren, L.; Chen, S.; Zhang, H.; McClain, C.; et al. Chalcone Derivative L6H21 Reduces EtOH+ LPS-Induced Liver Injury Through Inhibition of NLRP3 Inflammasome Activation. Alcohol. Clin. Exp. Res. 2019, 43, 1662–1671. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, X.; Qiu, M.; Chen, W.; Zeng, Z.; Chen, Y. Emodin ameliorates ethanol-induced fatty liver injury in mice. Pharmacology 2014, 94, 71–77. [Google Scholar] [CrossRef]
- Ferenci, P. Silymarin in the treatment of liver diseases: What is the clinical evidence? Clin. Liver Dis. 2016, 7, 8–10. [Google Scholar] [CrossRef]
- Song, Z.; Deaciuc, I.; Song, M.; Lee, D.Y.W.; Liu, Y.; Ji, X.; McClain, C. Silymarin protects against acute ethanol-induced hepatotoxicity in mice. Alcohol. Clin. Exp. Res. 2006, 30, 407–413. [Google Scholar] [CrossRef]
- Ferenci, P.; Dragosics, B.; Dittrich, H.; Frank, H.; Benda, L.; Lochs, H.; Meryn, S.; Base, W.; Schneider, B. Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver. J. Hepatol. 1989, 9, 105–113. [Google Scholar] [CrossRef]
- Lucena, M.I.; Andrade, R.J.; de la Cruz, J.P.; Rodriguez-Mendizabal, M.; Blanco, E.; Sánchez de la Cuesta, F. Effects of silymarin MZ-80 on oxidative stress in patients with alcoholic cirrhosis. Int. J. Clin. Pharmacol. Ther. 2002, 40, 2–8. [Google Scholar] [CrossRef]
- Wang, O.; Cheng, Q.; Liu, J.; Wang, Y.; Zhao, L.; Zhou, F.; Ji, B. Hepatoprotective effect of Schisandra chinensis (Turcz.) Baill. lignans and its formula with Rubus idaeus on chronic alcohol-induced liver injury in mice. Food Funct. 2014, 5, 3018–3025. [Google Scholar] [CrossRef] [PubMed]
- Su, L.; Li, P.; Lu, T.; Mao, C.; Ji, D.; Hao, M.; Huang, Z. Protective effect of Schisandra chinensis total lignans on acute alcoholic-induced liver injury related to inhibiting CYP2E1 activation and activating the Nrf2/ARE signaling pathway. Rev. Bras. Farmacogn. 2019, 29, 198–205. [Google Scholar] [CrossRef]
- Xu, J.B.; Gao, G.C.; Yuan, M.J.; Huang, X.; Zhou, H.Y.; Zhang, Y.; Zhang, Y.; Zhang, Y.; Wu, Z.; Feng, J.M.; et al. Lignans from Schisandra chinensis ameliorate alcohol induced long term liver injury and reducing hepatocellular degeneration via blocking ETBR. J. Ethnopharmacol. 2020, 258, 112813. [Google Scholar] [CrossRef]
- Yan, S.L.; Yang, H.T.; Lee, H.L.; Yin, M.C. Protective effects of maslinic acid against alcohol-induced acute liver injury in mice. Food Chem. Toxicol. 2014, 74, 149–155. [Google Scholar] [CrossRef]
- Saravanan, R.; Viswanathan, P.; Pugalendi, K.V. Protective effect of ursolic acid on ethanol-mediated experimental liver damage in rats. Life Sci. 2006, 78, 713–718. [Google Scholar] [CrossRef]
- Xu, T.; Zheng, L.; Xu, L.; Yin, L.; Qi, Y.; Xu, Y.; Han, X.; Peng, J. Protective effects of dioscin against alcohol-induced liver injury. Arch. Toxicol. 2014, 88, 739–753. [Google Scholar] [CrossRef]
- Liu, M.; Xu, Y.; Han, X.; Yin, L.; Xu, L.; Qi, Y.; Zhao, Y.; Liu, K.; Peng, J. Dioscin alleviates alcoholic liver fibrosis by attenuating hepatic stellate cell activation via the Journal Pre-proofTLR4/MyD88/NF-kappaB signaling pathway. Sci. Rep. 2015, 5, 18038. [Google Scholar] [CrossRef] [Green Version]
- Liu, F.; Bai, X.; Ding, R.B.; Hu, Y.J.; Su, H.; Wan, J.B. UPLC/Q-TOFMS-based metabolomics studies on the protective effect of Panax notoginseng saponins on alcoholic liver injury. Am. J. Chin. Med. 2015, 43, 695–714. [Google Scholar] [CrossRef]
- Ding, R.B.; Tian, K.; Cao, Y.W.; Bao, J.L.; Wang, M.; He, C.; Hu, Y.; Su, H.; Wan, J.B. Protective effect of panax notoginseng saponins on acute ethanol-induced liver injury is associated with ameliorating hepatic lipid accumulation and reducing ethanol-mediated oxidative stress. J. Agric. Food Chem. 2015, 63, 2413–2422. [Google Scholar] [CrossRef]
- Lin, C.F.; Wong, K.L.; Wu, R.S.; Huang, T.C.; Liu, C.F. Protection by hot water extract of Panax notoginseng on chronic ethanol-induced hepatotoxicity. Phytother. Res. 2003, 17, 1119–1122. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Chu, S.; Li, J.; Li, J.; Zhang, Z.; Xia, C.; Heng, Y.; Zhang, M.; Hu, J.; Wei, G.; et al. Anti-inflammatory function of ginsenoside Rg1 on alcoholic hepatitis through glucocorticoid receptor related nuclear factor-kappa B pathway. J. Ethnopharmacol. 2015, 173, 231–240. [Google Scholar] [CrossRef]
- Liu, J.; Wang, X.; Liu, R.; Liu, Y.; Zhang, T.; Fu, H.; Hai, C. Oleanolic acid co-administration alleviates ethanol-induced hepatic injury via Nrf-2 and ethanol-metabolizing modulating in rats. Chem. Biol. Interact. 2014, 221, 88–98. [Google Scholar] [CrossRef]
- Li, X.; Zhang, Y.; Jin, Q.; Xia, K.L.; Jiang, M.; Cui, B.W.; Wu, Y.L.; Song, S.Z.; Lian, L.H.; Nan, J.X. Liver kinase B1/AMP-activated protein kinase-mediated regulation by gentiopicroside ameliorates P2X7 receptor-dependent alcoholic hepatosteatosis. Br. J. Pharmacol. 2018, 175, 1451–1470. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Peng, Y.; Zeng, Y.; Hua, Y.; Xu, X. 2, 3, 4′, 5-tetrahydroxystilbene-2-0-β-d Glycoside Attenuates Age- and Diet-Associated Non-Alcoholic Steatohepatitis and Atherosclerosis in LDL Receptor Knockout Mice and Its Possible Mechanisms. Int. J. Mol. Sci. 2019, 20, 1617. [Google Scholar] [CrossRef] [Green Version]
- Peiyuan, H.; Zhiping, H.; Chengjun, S.; Chunqing, W.; Bingqing, L.; Imam, M.U. Resveratrol Ameliorates Experimental Alcoholic Liver Disease by Modulating Oxidative Stress. Evid. Based Complement. Altern. Med. 2017, 2017, 4287890. [Google Scholar] [CrossRef] [Green Version]
- Lai, Y.; Zhou, C.; Huang, P.; Dong, Z.; Mo, C.; Xie, L.; Lin, H.; Zhou, Z.; Deng, G.; Liu, Y.; et al. Polydatin alleviated alcoholic liver injury in zebrafish larvae through ameliorating lipid metabolism and oxidative stress. J. Pharmacol. Sci. 2018, 138, 46–53. [Google Scholar] [CrossRef]
- Sohn, E.H.; Koo, H.J.; Hang, D.T.T.; Jang, S.A.; Namkoong, S.; Lim, J.D.; Kang, S.C. Protective effects of ellagic acid on ethanol-induced toxicity in hepatic HepG2 cells. Mol. Cell. Toxicol. 2013, 9, 249–256. [Google Scholar] [CrossRef]
- Londhe, J.S.; Devasagayam, T.P.; Foo, L.Y.; Shastry, P.; Ghaskadbi, S.S. Geraniin and amariin, ellagitannins from Phyllanthus amarus, protect liver cells against ethanol induced cytotoxicity. Fitoterapia 2012, 83, 1562–1568. [Google Scholar] [CrossRef]
- Devipriya, N.; Srinivasan, M.; Sudheer, A.R.; Menon, V.P. Effect of ellagic acid, a natural polyphenol, on alcohol-induced prooxidant and antioxidant imbalance: A drug dose dependent study. Singap. Med. J. 2007, 48, 311–318. [Google Scholar]
- Devipriya, N.; Sudheer, A.R.; Srinivasan, M.; Menon, V.P. Effect of ellagic acid, a plant polyphenol, on fibrotic markers (MMPs and TIMPs) during alcohol-induced hepatotoxicity. Toxicol. Mech. Methods 2007, 17, 349–356. [Google Scholar] [CrossRef]
- Li, M.; Wu, C.; Guo, H.; Chu, C.; Hu, M.; Zhou, C. Mangiferin improves hepatic damage-associated molecular patterns, lipid metabolic disorder and mitochondrial dysfunction in alcohol hepatitis rats. Food Funct. 2019, 10, 3514–3534. [Google Scholar] [CrossRef]
- Amen, Y.; Sherif, A.E.; Shawky, N.M.; Abdelrahman, R.S.; Wink, M.; Sobeh, M. Grape-Leaf Extract Attenuates Alcohol-Induced Liver Injury via Interference with NF-κB Signaling Pathway. Biomolecules 2020, 10, 558. [Google Scholar] [CrossRef] [Green Version]
- Liang, H.W.; Yang, T.Y.; Teng, C.S.; Lee, Y.J.; Yu, M.H.; Lee, H.J.; Hsu, L.S.; Wang, C.J. Mulberry leaves extract ameliorates alcohol-induced liver damages through reduction of acetaldehyde toxicity and inhibition of apoptosis caused by oxidative stress signals. Int. J. Med. Sci. 2021, 18, 53–64. [Google Scholar] [CrossRef]
- Nam, K.S.; Kim, J.; Noh, S.K.; Park, J.H.; Sung, E.G. Effect of Sweet Persimmon Wine on Alcoholic Fatty Livers in Rats. J. Korean Soc. Food Sci. Nutr. 2011, 40, 1548–1555. [Google Scholar] [CrossRef]
- Cho, Y.E.; Song, B.J. Pomegranate prevents binge alcohol-induced gut leakiness and hepatic inflammation by suppressing oxidative and nitrative stress. Redox Biol. 2018, 18, 266–278. [Google Scholar] [CrossRef]
- Zavodnik, I.; Buko, V.; Lukivskaya, O.; Lapshina, E.; Ilyich, T.; Belonovskaya, E.; Kirko, S.; Naruta, E.; Kuzmitskaya, I.; Budryn, G.; et al. Cranberry (Vaccinium macrocarpon) peel polyphenol-rich extract attenuates rat liver mitochondria impairments in alcoholic steatohepatitis in vivo and after oxidative treatment in vitro. J. Funct. Foods 2019, 57, 83–94. [Google Scholar] [CrossRef]
- Gao, H.; Lv, Y.; Liu, Y.; Li, J.; Wang, X.; Zhou, Z.; Tipoe, G.L.; Ouyang, S.; Guo, Y.; Zhang, J.; et al. Wolfberry-Derived Zeaxanthin Dipalmitate Attenuates Ethanol-Induced Hepatic Damage. Mol. Nutr. Food Res. 2019, 63, e1801339. [Google Scholar] [CrossRef]
- Dong, M.; Li, L.; Li, G.; Song, J.; Liu, B.; Liu, X.; Wang, M. Mangiferin protects against alcoholic liver injury: Via suppression of inflammation-induced adipose hyperlipolysis. Food Funct. 2020, 11, 8837–8851. [Google Scholar] [CrossRef]
- Pari, L.; Suresh, A. Effect of grape (Vitis vinifera L.) leaf extract on alcohol induced oxidative stress in rats. Food Chem. Toxicol. 2008, 46, 1627–1634. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Zhang, R.; Huang, F.; Liu, L.; Deng, Y.; Wei, Z.; Zhang, Y.; Liu, D.; Zhang, M. The biphasic dose effect of lychee (Litchi chinensis Sonn.) pulp phenolic extract on alcoholic liver disease in mice. Food Funct. 2017, 8, 189–200. [Google Scholar] [CrossRef]
- Xiao, J.; Zhang, R.; Huang, F.; Liu, L.; Deng, Y.; Ma, Y.; Tang, X.; Zhang, Y.; Zhang, M. Lychee (Litchi chinensis Sonn.) pulp phenolic extract confers a protective activity against alcoholic liver disease in mice by alleviating mitochondrial dysfunction. J. Agric. Food Chem. 2017, 65, 5000–5009. [Google Scholar] [CrossRef]
- Xiao, J.; Zhang, R.; Zhou, Q.; Liu, L.; Huang, F.; Deng, Y.; Ma, Y.; Wei, Z.; Tang, X.; Zhang, M. Lychee (Litchi chinensis Sonn.) pulp phenolic extract provides protection against alcoholic liver injury in mice by alleviating intestinal microbiota dysbiosis, intestinal barrier dysfunction, and liver inflammation. J. Agric. Food Chem. 2017, 65, 9675–9684. [Google Scholar] [CrossRef]
- Zhuge, Q.; Zhang, Y.; Liu, B.; Wu, M. Blueberry polyphenols play a preventive effect on alcoholic fatty liver disease C57BL/6 J mice by promoting autophagy to accelerate lipolysis to eliminate excessive TG accumulation in hepatocytes. Ann. Cardiothorac. Surg. 2020, 9, 1045–1054. [Google Scholar] [CrossRef] [PubMed]
- Adedosu, O.T.; Oyedeji, A.T.; Iwaku, T.; Ehigie, A.F.; Olorunsogo, O.O. Hepatoprotective activity and inhibitory effect of flavonoid-rich extract of Brysocarpus Coccineus leaves on mitochondrial membrane permeability transition pore. Asian J. Nat. Appl. Sci. 2014, 3, 92–100. [Google Scholar]
- Park, S.; Kim, D.S.; Wu, X.; Yi, Q.J. Mulberry and dandelion water extracts prevent alcohol-induced steatosis with alleviating gut microbiome dysbiosis. Exp. Biol. Med. 2018, 243, 882–894. [Google Scholar] [CrossRef] [PubMed]
- Szachowicz-Petelska, B.; Dobrzyńska, I.; Skrzydlewska, E.; Figaszewski, Z. Protective effect of blackcurrant on liver cell membrane of rats intoxicated with ethanol. J. Membr. Biol. 2012, 245, 191–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damodara Reddy, V.; Padmavathi, P.; Gopi, S.; Paramahamsa, M.; Varadacharyulu, N.C. Protective effect of Emblica officinalis against alcohol-induced hepatic injury by ameliorating oxidative stress in rats. Indian J. Clin. Biochem. 2010, 25, 419–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, D.Y.; Kim, M.J.; Yoon, D.; Lee, Y.S.; Kim, G.S.; Choon Yoo, Y. Ginseng berry prevents alcohol-induced liver damage by improving the anti-inflammatory system damage in mice and quality control of active compounds. Int. J. Mol. Sci. Artic. 2019, 20, 3522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, J.H.; Lee, K.Y.; Kim, J.H.; Shin, H.; Lee, J.H.; Kim, Y.J. Prunus mume Sieb. et Zucc. fruit ameliorates alcoholic liver injury in mice by inhibiting apoptosis and inflammation through oxidative stress. J. Funct. Foods 2016, 25, 135–148. [Google Scholar] [CrossRef]
- Abozid, M.M.; Farid, H.E. The anti-fatty liver effects of guava leaves and pomegranate peel extracts on ethanol-exposed rats. J. Biol. Chem. Environ. Sci. 2013, 8, 83–104. [Google Scholar]
- Zhou, T.; Zhang, Y.J.; Xu, D.-P.; Wang, F.; Zhou, Y.; Zheng, J.; Li, Y.; Zhang, J.J.; Li, H.B. Protective effects of lemon juice on alcohol-induced liver injury in mice. BioMed Res. Int. 2017, 2017, 1–8. [Google Scholar] [CrossRef]
- Lee, E.Y.; Kim, S.H.; Chang, S.N.; Lee, J.H.; Hwang, B.S.; Woo, J.T.; Kang, S.C.; Lee, J.; Park, J.G. Efficacy of polymethoxylated flavonoids from citrus depressa extract on alcohol-induced liver injury in mice. Biotechnol. Bioprocess Eng. 2019, 24, 907–914. [Google Scholar] [CrossRef]
- Guo, M.; Mao, B.; Ahmed Sadiq, F.; Hao, Y.; Cui, S.; Yi, M.; Hong, Q.; Lee, Y.K.; Zhao, J. Effects of noni fruit and fermented noni juice against acute alcohol induced liver injury in mice. J. Funct. Foods 2020, 70, 103995. [Google Scholar] [CrossRef]
- Wiese, J.; McPherson, S.; Odden, M.C.; Shlipak, M.G. Effect of Opuntia ficus indica on Symptoms of the Alcohol Hangover. Arch. Intern. Med. 2004, 164, 1334–1340. [Google Scholar] [CrossRef]
- Cheng, N.; Du, B.; Wang, Y.; Gao, H.; Cao, W.; Zheng, J.; Feng, F. Antioxidant properties of jujube honey and its protective effects against chronic alcohol-induced liver damage in mice. Food Funct. 2014, 5, 900–908. [Google Scholar] [CrossRef]
- Sun, H.; Mu, T.; Liu, X.; Zhang, M.; Chen, J. Purple Sweet Potato (Ipomoea batatas L.) Anthocyanins: Preventive Effect on Acute and Subacute Alcoholic Liver Damage and Dealcoholic Effect. J. Agric. Food Chem. 2014, 62, 2364–2373. [Google Scholar] [CrossRef]
- Jiang, Z.; Chen, C.; Wang, J.; Xie, W.; Wang, M.; Li, X.; Zhang, X. Purple potato (Solanum tuberosum L.) anthocyanins attenuate alcohol-induced hepatic injury by enhancing antioxidant defense. J. Nat. Med. 2016, 70, 45–53. [Google Scholar] [CrossRef]
- Kim, J.; Seo, Y.; Park, J.H.; Noh, S.K. Protective Effect of Onion Wine on Alcoholic Fatty Liver in Rats. J. Korean Soc. Food Sci. Nutr. 2016, 45, 467–473. [Google Scholar] [CrossRef]
- Guan, M.J.; Zhao, N.; Xie, K.Q.; Zeng, T. Hepatoprotective effects of garlic against ethanol-induced liver injury: A mini-review. Food Chem. Toxicol. 2018, 111, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Zeng, T.; Guo, F.F.; Zhang, C.L.; Zhao, S.; Dou, D.D.; Gao, X.C.; Xie, K.Q. The anti-fatty liver effects of garlic oil on acute ethanol-exposed mice. Chem. Biol. Interact. 2008, 176, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Zeng, T.; Zhang, C.L.; Pan, G.B.; Zhao, S.; Dou, D.D.; Xin, X.; Xie, K.Q. The protective effects of garlic oil on acute ethanol-induced oxidative stress in the liver of mice. J. Sci. Food Agric. 2008, 88, 2238–2243. [Google Scholar] [CrossRef]
- Zeng, T.; Zhang, C.L.; Song, F.Y.; Zhao, X.L.; Xie, K.Q. Garlic oil alleviated ethanol-induced fat accumulation via modulation of SREBP-1, PPAR-α, and CYP2E1. Food Chem. Toxicol. 2012, 50, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Zeng, T.; Zhang, C.L.; Song, F.Y.; Zhao, X.L.; Yu, L.H.; Zhu, Z.P.; Xie, K.Q. The activation of HO-1/Nrf-2 contributes to the protective effects of diallyl disulfide (DADS) against ethanol-induced oxidative stress. Biochim. Biophys. Acta Gen. Subj. 2013, 1830, 4848–4859. [Google Scholar] [CrossRef] [PubMed]
- Zeng, T.; Zhang, C.L.; Zhu, Z.P.; Yu, L.H.; Zhao, X.L.; Xie, K.Q. Diallyl trisulfide (DATS) effectively attenuated oxidative stress-mediated liver injury and hepatic mitochondrial dysfunction in acute ethanol-exposed mice. Toxicology 2008, 252, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.Y.; Cui, Z.G.; Lee, S.R.; Kim, S.J.; Kang, H.K.; Lee, Y.K.; Park, D.B. Effects of Asparagus officinalis Extracts on Liver Cell Toxicity and Ethanol Metabolism. J. Food Sci. 2009, 74, H204–H208. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lu, Y.; Yang, X.; Zhao, Y. Supplementation of okra seed oil ameliorates ethanol-induced liver injury and modulates gut microbiota dysbiosis in mice. Food Funct. 2019, 10, 6385–6398. [Google Scholar] [CrossRef]
- Tang, X.; Wei, R.; Deng, A.; Lei, T. Protective Effects of Ethanolic Extracts from Artichoke, an Edible Herbal Medicine, against Acute Alcohol-Induced Liver Injury in Mice. Nutrients 2017, 9, 1000. [Google Scholar] [CrossRef] [Green Version]
- Neyrinck, A.M.; Etxeberria, U.; Taminiau, B.; Daube, G.; Van Hul, M.; Everard, A.; Cani, P.D.; Bindels, L.B.; Delzenne, N.M. Rhubarb extract prevents hepatic inflammation induced by acute alcohol intake, an effect related to the modulation of the gut microbiota. Mol. Nutr. Food Res. 2017, 61, 1500899. [Google Scholar] [CrossRef] [Green Version]
- Lu, K.H.; Tseng, H.C.; Liu, C.T.; Huang, C.J.; Chyuan, J.H.; Sheen, L.Y. Wild bitter gourd protects against alcoholic fatty liver in mice by attenuating oxidative stress and inflammatory responses. Food Funct. 2014, 5, 1027–1037. [Google Scholar] [CrossRef]
- Kanuri, G.; Weber, S.; Volynets, V.; Spruss, A.; Bischoff, S.C.; Bergheim, I. Cinnamon extract protects against acute alcohol-induced liver steatosis in mice. J. Nutr. 2009, 139, 482–487. [Google Scholar] [CrossRef] [Green Version]
- Kaviarasan, S.; Viswanathan, P.; Anuradha, C. Fenugreek seed (Trigonella foenum graecum) polyphenols inhibit ethanol-induced collagen and lipid accumulation in rat liver. Cell Biol. Toxicol. 2007, 23, 373–383. [Google Scholar] [CrossRef]
- Azizi, M.; Abbasi, N.; Mohamadpour, M.; Bakhtiyari, S.; Asadi, S.; Shirzadpour, E.; Aidy, A.; Mohamadpour, M.; Amraei, M. Investigating the effect of Crocus sativus L. petal hydroalcoholic extract on inflammatory and enzymatic indices resulting from alcohol use in kidney and liver of male rats. J. Inflamm. Res. 2019, 12, 269–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abou Seif, H.S. Ameliorative effect of parsley oil (Petroselinum crispum) against alcohol-induced hepatotoxicity and oxidative stress. Med. Res. J. 2014, 13, 100–107. [Google Scholar] [CrossRef]
- Jose, S.P.; Ratheesh, M.; Asha, S.; Krishnakumar, I.M.; Sandya, S.; Kumar, G. Hepato-protective Effect of Clove Bud Polyphenols (Syzygium aromaticum L.) (Clovinol®) by Modulating Alcohol Induced Oxidative Stress and Inflammation. J. Food Res. 2018, 7, 10–20. [Google Scholar] [CrossRef] [Green Version]
- El-Newary, S.A.; Shaffie, N.M.; Omer, E.A. The protection of Thymus vulgaris leaves alcoholic extract against hepatotoxicity of alcohol in rats. Asian Pac. J. Trop. Med. 2017, 10, 361–371. [Google Scholar] [CrossRef]
- Koneru, M.; Dhar Sahu, B.; Mir, S.M.; Ravuri, H.G.; Kuncha, M.; Kumar, J.M.; Kilari, K.; Sistla, R. Capsaicin, the pungent principle of peppers, ameliorates alcohol-induced acute liver injury in mice via modulation of matrix metalloproteinases. Can. J. Physiol. Pharmacol. 2018, 96, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Zhang, R.; Wu, Y.; Wu, C.; Jia, X.; Dong, L.; Liu, L.; Chen, Y.; Bai, Y.; Zhang, M. Rice Bran Phenolic Extract Protects against Alcoholic Liver Injury in Mice by Alleviating Intestinal Microbiota Dysbiosis, Barrier Dysfunction, and Liver Inflammation Mediated by the Endotoxin-TLR4-NF-κB Pathway. J. Agric. Food Chem. 2020, 68, 1237–1247. [Google Scholar] [CrossRef]
- Xiao, J.; Wu, C.; He, Y.; Guo, M.; Peng, Z.; Liu, Y.; Liu, L.; Dong, L.; Guo, Z.; Zhang, R.; et al. Rice Bran Phenolic Extract Confers Protective Effects against Alcoholic Liver Disease in Mice by Alleviating Mitochondrial Dysfunction via the PGC-1α-TFAM Pathway Mediated by microRNA-494-3p. J. Agric. Food Chem. 2020, 68, 12284–12294. [Google Scholar] [CrossRef]
- Yang, Q.; Luo, C.; Zhang, X.; Liu, Y.; Wang, Z.; Cacciamani, P.; Shi, J.; Cui, Y.; Wang, C.; Sinha, B.; et al. Tartary buckwheat extract alleviates alcohol-induced acute and chronic liver injuries through the inhibition of oxidative stress and mitochondrial cell death pathway. Am. J. Transl. Res. 2020, 12, 70–89. [Google Scholar]
- Li, H.M.; Guo, P.; Hu, X.; Xu, L.; Zhang, X.Z. Preparation of corn (Zea mays) peptides and their protective effect against alcohol-induced acute hepatic injury in NH mice. Biotechnol. Appl. Biochem. 2007, 47, 169–174. [Google Scholar]
- Wu, Y.; Pan, X.; Zhang, S.; Wang, W.; Cai, M.; Li, Y.; Yang, F.; Guo, H. Protective effect of corn peptides against alcoholic liver injury in men with chronic alcohol consumption: A randomized double-blind placebo-controlled study. Lipids Health Dis. 2014, 13, 192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.H.; Kim, J.H.; Kim, S.H.; Oh, J.Y.; Seo, W.D.; Kim, K.M.; Jung, J.C.; Jung, Y.S. Barley sprouts extract attenuates alcoholic fatty liver injury in mice by reducing inflammatory response. Nutrients 2016, 8, 440. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Sun, Y.; Zang, Y.; Su, Y.; Zhou, H.; Wang, J.; Xie, M.; Chen, G.; Liu, L.; Mei, Q. GanMeijian ameliorates lipid accumulation and oxidative damage in alcoholic fatty liver disease in Wistar rats. Life Sci. 2020, 255, 117721. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Yu, X.H.; Gao, E.Z.; Liu, X.N.; Sun, L.J.; Li, H.L.; Wang, P.; Zhao, Y.L.; Yu, Z.G. Hepatoprotective Effect of Active Constituents Isolated from Mung Beans (Phaseolus radiatus L.) in an Alcohol-Induced Liver Injury Mouse Model. J. Food Biochem. 2014, 38, 453–459. [Google Scholar] [CrossRef]
- Yan, Z.; Zhong, Y.; Duan, Y.; Chen, Q.; Li, F. Antioxidant mechanism of tea polyphenols and its impact on health benefits. Anim. Nutr. 2020, 6, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Arteel, G.E.; Uesugi, T.; Bevan, L.N.; Gäbele, E.; Wheeler, M.D.; McKim, S.E.; Thurman, R.G. Green tea extract protects against early alcohol-induced liver injury in rats. Biol. Chem. 2002, 383, 663–670. [Google Scholar] [CrossRef]
- Chen, K.H.; Li, P.C.; Lin, W.H.; Chien, C.T.; Low, B.H. Depression by a green tea extract of alcohol-induced oxidative stress and lipogenesis in rat liver. Biosci. Biotechnol. Biochem. 2011, 75, 1668–1676. [Google Scholar] [CrossRef] [Green Version]
- Lodhi, P.; Tandan, N.; Singh, N.; Kumar, D.; Kumar, M. Camellia sinensis (L.) kuntze extract ameliorates chronic ethanol-induced hepatotoxicity in albino rats. Evidence-based Complement. Evid. Based Complement. Altern. Med. 2014, 2014, 787153. [Google Scholar] [CrossRef] [Green Version]
- Park, J.H.; Kim, Y.; Kim, S.H. Green tea extract (Camellia sinensis) fermented by lactobacillus fermentum attenuates alcohol-induced liver damage. Biosci. Biotechnol. Biochem. 2012, 76, 2294–2300. [Google Scholar] [CrossRef] [Green Version]
- Wang, R.; Xiao, R.; Yang, L.; Liu, W.; Shi, H.; Hou, Y. The Effects of Fermented Pu-erh Tea on the Dynamic Pathological Changes of the Alcoholic Liver Injury Rats. J. Yunnan Agric. Univ. 2015, 30, 408–412. [Google Scholar]
- Liu, Y.; Luo, Y.; Wang, X.; Luo, L.; Sun, K.; Zeng, L. Gut Microbiome and Metabolome Response of Pu-erh Tea on Metabolism Disorder Induced by Chronic Alcohol Consumption. J. Agric. Food Chem. 2020, 68, 6615–6627. [Google Scholar] [CrossRef] [PubMed]
- McKim, S.E.; Konno, A.; Gäbele, E.; Uesugi, T.; Froh, M.; Sies, H.; Thurman, R.G.; Arteel, G.E. Cocoa extract protects against early alcohol-induced liver injury in the rat. Arch. Biochem. Biophys. 2002, 406, 40–46. [Google Scholar] [CrossRef]
- Hu, C.M.; Cao, Q.; Lv, X.W.; Cheng, W.M.; Li, R.; Li, J. Protective effects of total flavonoids from Litsea coreana on alcoholic fatty liver in rats associated with down-regulation adipose differentiation-related protein expression. Am. J. Chin. Med. 2012, 40, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wu, Z.; Weng, P. Antioxidant and hepatoprotective effect of (-)-epigallocatechin 3- O -(3- O -Methyl) gallate (EGCG3Me) from chinese oolong tea. J. Agric. Food Chem. 2014, 62, 10046–10054. [Google Scholar] [CrossRef]


| Categories | Compound Names | Study Design | Key Findings | Ref. |
|---|---|---|---|---|
| Flavonols | Quercetin | Quercetin (100 mg/kg bw) with ethanol (28% of total calories as ethanol) were given to mice for 12 weeks | Quercetin ameliorated liver injury mediated by chronic-plus-binge ethanol by decreasing ALT and AST, decreased PLIN2 level, activated AMPK activity, and increased co-localization of liver LC3II and PLIN2 proteins. These results predict the regulatory effect of quercetin on lipophagy induced by ethanol. | [69] |
| Quercetin, quercetin-3-glucoside, and rutin | HepG2 cells were treated with quercetin, quercetin-3-glucoside, and rutin for 1 h and after that with 5% alcohol for 24 h | Quercetin, quercetin-3-glucoside, and rutin may have preventive strategies against ALD mainly by decreasing hepatic ALT, inflammatory, antioxidant response in HepG2 cells. | [70] | |
| Quercetin | C57BL/6J mice were fed with regular or ethanol-containing Lieber–DeCarli liquid diets along with quercetin (100 mg/kg bw) for 15 weeks | Quercetin ameliorated lysosomal autophagy dysfunction mediated by ethanol and also exerted autophagic flux suppression, decreased abnormal LC3II and p62 accumulation, elevated LAMP1, LAMP2, and Rab7 expression, and regulated mTOR-TFEB pathway. | [74] | |
| Fisetin | C57BL/6J mice were fed Lieber–DeCarli or ethanol diet for 4 weeks with or without fisetin (10 mg/kg/day) | Fisetin downregulated ALT, AST, and hepatic NADPH oxidase 4 levels and improved hepatic antioxidant activities. Moreover, it also attenuated alcohol-induced hepatic steatosis via p-AMPK, CYP4A, ACOX1, and MTTP. | [75] | |
| Fisetin | Fisetin (5 and 10 mg/kg) and 50% ethanol p.o. (10 mL/kg body weight) were given to animals | Fisetin protected against ALD by improving antioxidant activities and restoring mitochondrial respiratory enzymes and matrix metalloproteinase activities. | [76] | |
| Dihydromyricetin | Dihydromyricetin at dosage of 5 and 10 mg/kg; intraperitoneal injection and ethanol were given to C57BL/6J mice | Dihydromyricetin reduced liver injury markers and TG, increased activation of AMPK and downstream targets CPT-1 and ACC-1, and reduced the expression of proinflammatory cytokines and chemokines in mice and also in cell models. | [79] | |
| Morin | Morin (50 mg/kg bw) was administered along with 40% alcohol (40%, 2 mL/100 g/day, p.o.) for 21 days to rats | Morin protected from ALD by decreasing ALT, TB, SGPT, and SGOT and improved antioxidant activities in the ethanol-fed rats. | [80] | |
| Kaempferol | Mice were intragastrically administered distillate spirits (2, 4, 6, 8 g/kg, 50% alcohol, v/v) twice daily at 3-day intervals and finally 10 g/kg bw for 28 days. Kaempferol was administered at dosage of 10 and 20 mg/kg of bw for 28 days twice a day | Kaempferol treatment significantly reduced MDA, TG, and CYP2E1 and also increased GSH and SOD levels. | [82] | |
| Kaempferol | Kaempferol (25, 50, 100 mg/kg bw) and ethanol (5 g/kg) were given to ICR mice | Kaempferol may act as a prophylactic treatment against ALD by increasing the expression of butyrate receptors, transporters, and TJ proteins in the intestinal mucosa, decreasing ALT and AST levels. | [84] | |
| Isoflavones | Genistein and puerarin | Genistein and puerarin (0.3 mM/kg bw) and 50% alcohol were administered 1 h later for 5 weeks to ICR mice | Genistein and puerarin exerted protective effect against ALD by downregulating ALT, AST, hepatic lipids, and inflammation biomarkers. | [85] |
| Genistein | Genistein group received genistein (16 mg/kg/day bw dissolved in 50% alcohol) and alcohol (50%, 8 g/kg/day bw) for 4 weeks | Genistein administration decreased serum ALT and hepatic MDA, increased GSH levels, and decreased inflammatory markers (IL-18 and TNF-α). | [86] | |
| Flavones | Luteolin | Mice were fed with chronic (1–4% for 3 day and 5% for 9 day) binge ethanol (30% ethanol) and luteolin (50 mg/kg) | Luteolin treatment decreased ALT, TG, LDL-C, lipid accumulation, SREBP1C, FAS, ACC, and SCD1. Moreover, luteolin abrogated the ethanol-induced reduction of AMPK and SREBP-1c phosphorylation. | [89] |
| Wogonin | RAW264.7 cells were treated with 100 mM ethanol for 24 h or incubating with various concentrations of wogonin (1.25 to 20 µg/mL). Wogonin-treated mice at the dose of 25, 50, 100 mg/kg/day and ethanol-fed mice were fed diets containing 5% v/v ethanol for 16 days, and mice were given single binge ethanol administration (20% ethanol, 5 g/kg, bw,) on last day | Wogonin remarkably attenuated ALD by inflammatory response (TNF-α and IL-6) and suppressed PPARγ-meditated phosphorylation and activation of NF-κB p65. | [90] | |
| Baicalin | Mice were fed with ethanol Lieber–DeCarli diet for 10 days; after that, a single dose of ethanol (5 g/kg bw) and baicalin was injected i.p. (200 mg/kg/day) for 11 days. | Treatment with baicalin attenuated ethanol-induced oxidative stress, inflammation, and cell death. | [92] | |
| Baicalin | Human normal liver cell L02 were treated with 100 mM alcohol in the absence/presence of baicalin (25, 50 µM) for 24 h Rats were intragastrically administered alcohol (65% v/v, 5 mL/kg/day) for 3 days and then 10 mL/kg/day on the following days; baicalin groups intragastrically received baicalin (120 mg/kg/day) for 4 weeks | Baicalin supplementation alleviated ALD by decreasing MDA and the proinflammatory cytokines (TNF-α, IL-1β, and IL-6) expression, increasing SOD and GSH-Px. Moreover, it also modulated Shh pathway activation and upregulated expression of Ptc, Smo, Gli-1, and Shh. | [93] | |
| Apigenin | Mice were fed with 56% erguotou wine or apigenin (150–300 mg/kg) for 1 month | Apigenin reduced the expression of CYP2E1, NF-κB proteins, MDA, and TNF-α, whereas GSH and GSH-Px were increased. Furthermore, apigenin also increased the expression of PPARα and CPT1A and decreased the expression of SREBP1 and FAS. | [94] | |
| Chrysin | Ethanol was given to rats (5–12 g/kg bw per week) for 4 weeks and chrysin (20 and 40 mg/kg bw) prior to ethanol administration | Chrysin-treated rats ameliorated ALD by inhibiting the activities of ADH, XO, CYP2E1, and CAT levels, respectively. | [95] | |
| Flavanones | Naringin | Zebrafish larvae were treated with 2% ethanol 32 h and naringin (6.25, 12.50, and 25 mg/L) | Naringin protected from alcohol by attenuating lipid accumulation and reducing oxidative stress and apoptosis. | [96] |
| Naringenin | Zebrafish larvae were treated with 350 mM ethanol for 32 h and naringenin (2.5, 5, and 10 mg/L) | Naringenin markedly decreased alcoholic liver morphological phenotypes and expression of alcohol and lipid metabolism (Fads2, Cyp2y3, Hmgcra, Fabp10a, Hmgcrb, Echs1, and Fasn) and attenuated hepatic apoptosis in ethanol-induced zebrafish larvae model. | [97] | |
| Hesperidin | Zebrafish larvae were treated with 350 mM ethanol 32 h and hesperidin (6.25, 12.50, 25 µg/mL) | Hesperidin inhibited alcoholic injury to liver of zebrafish larvae by reducing the hepatic morphological damage and expressions of alcohol and lipid metabolic genes (Cyp2y3, Hmgcra, Cyp3a65, Hmgcrb, Fads2, and Fasn) with comparison to ALD model. | [98] | |
| Flavan-3-ols | EGCG | Chronic ethanol administration (6 g/kg/day × 60 days) and EGCG (100 mg/kg/day) were given to rats | EGCG ameliorated protein and lipid damage mediated by ethanol. | [101] |
| EGCG | L. plantarum and EGCG combination beads were administered to rats by oral gavage for 8 weeks | EGCG and L. plantarum markedly attenuate ALD by targeting various molecular markers TNF-α, NF-kB/p50, IL12/p40, and TLR4. | [102] | |
| Catechin | Ethanol (35% (v/v) at a dose of 10 g/kg per day) for 2 weeks followed by 14 g/kg/day for 10 weeks; catechin (50 mg/kg) was co-supplemented after 4 weeks | Catechin supplementation ameliorated ALD by downregulating the endotoxin-mediated activation signaling molecule NF-κB and the downstream signaling cascade NO, ROS, and TNF-α and increased the antioxidant biomarkers. | [103] | |
| EGCG | EGCG (50 mg/kg) along with ethanol was given to mice | EGCG attenuated ALD in ethanol-fed mice. | [104] | |
| Proanthocyanin and Anthocyanin | Cyanidin-3-glucoside | LX-2 cells were treated with ethanol (50 mM) plus 0.1 mM palmitate and cyanidin-3-glucoside (2 mM) for 72 h. Mice were fed with a high-fat high-cholesterol diet plus ethanol and cyanidin-3-O-β-glucoside (200 mg/kg bw) for 12 weeks. | Cyanidin-3-glucoside supplementation reversed the liver damage induced by alcohol. Moreover, it also restored intracellular energy and increased AMPK phosphorylation and autophagy. | [106] |
| Cyanidin-3-glucoside | Cyanidin-3-glucoside (200 mg/kg bw) and ethanol were given to mice for 8 weeks | Cyanidin-3-glucoside suppressed NF-κB acetylation, NLRP3 inflammasome activation, and proinflammatory cytokines release. | [107] | |
| Oligomeric proanthocyanins | Mouse AML-12 hepatocyte cells treated with alcohol and/or OPC (50 µM) for 24 h Oligomeric proanthocyanins (50 mg/kg bw) along with ethanol were given to mice for 9 days | Oligomeric proanthocyanins significantly improved alcohol-induced dyslipidemia, alleviated liver steatosis, reduced levels of ALT, AST, TG, TC, LDL-C, and MDA, increased SOD and HDL-C levels, and decreased the expressions of lipid synthesis genes (SREBP-1, 2) and inflammation gene (TNF-α, IL-1β, and IL-6). | [113] | |
| Alkaloids | Berberine | Acute alcohol exposure model: berberine pretreated orally (200–300 mg/kg/day) for 10 days and after the last dose of ethanol (6 g/kg) at 12-h intervals to the animals Chronic ethanol exposure mouse model: mice were fed with Lieber–DeCarli liquid diets containing 0% or 36% ethanol and berberine (120 mg/kg/day) | Berberine reduced hepatic lipid peroxidation and GSH, suppressed cytochrome P4502E1, and blunted the lipid accumulation. | [114] |
| Berberine | Mice were fed with ethanol (5 g/kg body weight) by gavage at days 11, 22, and 33 and berberine-treated (10–100 mg/kg) by gavage | Berberine protected ALD via modulation of gut microbiota and expansion of immuno-suppressive cells. | [115] | |
| Nuciferine | HepG2 cells with 3 and 10 µM nuciferine for 24 h Nuciferine (3 and 10 mg/kg bw) were intraperitoneally injected once daily for 7 continuous days, and after that, mice were administered with alcohol (5 g/kg) every 12 h for a total of 3 times | Nuciferine alleviated ALD by modulating miR-144/Nrf2/HO-1 cascade. | [116] | |
| Lignans | Silymarin | Mice were fed with ethanol (5 g/kg bw) gavage every 12 h for a total of 3 doses and silymarin (200 mg/kg bw) | Silymarin protected from ALD by decreasing ALT, lipid peroxidation, and TNF-α and increasing GSH level. | [121] |
| Stilbenes, Saponins, and Terpenoids | Oleanolic acid | Rats were treated with oleanolic acid (10 mg/kg bw) and ethanol (4 g/kg bw) for 1 month | Oleanolic acid protected rats against ALD via induction of Nrf2-related antioxidant to maintain redox, inflammatory pathway, and by modulating ethanol metabolism. | [135] |
| Resveratrol | Rats were fed with alcohol 6% (v/v) and gradually increased to 20% (v/v) by the fifth week and resveratrol (250 mg/kg bw) | Resveratrol alleviated ALD via regulation of oxidative stress, inflammation, and apoptosis. | [138] | |
| Polydatin | Zebrafish larvae at 4 days post-fertilization were exposed to ethanol (350 mmol/L) for 32 h and after that treated with polydatin for 48 h | Polydatin strongly alleviated hepatic steatosis, reduced alcohol and lipid metabolism genes (Fasn, Cyp2y3, Cyp3a65, Hmgcrb, and Hmgcra), inhibited oxidative stress, and upregulated DNA damage-related genes (Chop and Gadd45aa) in zebrafish model. | [139] | |
| Tannins | Ellagic acid | HepG2 cells were treated with ethanol and ellagic acid (1, 10, and 100 µM) | Ellagic acid protected ethanol-induced toxicity in HepG2 cells. | [140] |
| Geraniin and amariin | Mouse liver slices were treated with ethanol (1.7 M) or geraniin, amariin (0.2 mM) for 2 h at 37 °C | Both ellagitannins (geraniin and amariin) effectively protected mouse liver slices from ethanol-induced cytotoxicity and apoptosis by decreasing oxidative damage and modulating Bax/Bcl-2 ratio. | [141] | |
| Ellagic acid | Rats were fed with alcohol orally (20%, 7.9 g/kg bw) for 45 days and treated with ellagic acid (30–90 mg/kg bw) via intragastric intubation | Ellagic acid effectively modulated oxidative stress, improved antioxidant status, and decreased NO, hydroperoxides PCC, and TBARS in rats. | [142,143] |
| Edible Food Plant Category | Source | Bioactive Compounds | Study Design | Major Findings | Ref. |
|---|---|---|---|---|---|
| Fruits | Blueberry | ND | Blueberry juice combined with mixed probiotics containing (Bifidobacterium, Lactobacillus bulgaricus, and Streptococcus thermophilus; blueberry juice: 1.5 mL/100 g; 20 mL/100 g probiotics) for 10 days were given to ethanol-induced mice. | Blueberry juice and probiotics increased SOD, GSH, and HDL-C levels, decreased AST, ALT, TG, TC, LDL-C, and MDA, suppressed acetylated FOXO1, FOXO1, FasL, and caspase-3, and increased the SIRT1 in ethanol-exposed mice. | [110] |
| Mango | Mangiferin | Mangiferin (50 and 100 mg/kg bw) was orally given to ethanol-exposed rats for 12 weeks. | Mangiferin effectively regulated metal elements and FFA in serum, modulated specific alcohol-hepatitis-related genes, metabolic pathways, and potential biomarkers in alcoholic hepatitis rats. | [144] | |
| Grape | Quercetin, myricetin, rosmarinic acid, catechin, b-type procyanidin trimer, caffeic acid-O-hexoside, epicatechin | Grape-leaf extract (250–500 mg/kg) was orally given to ethanol-induced rats for 12 days. | Grape leaf extract attenuated liver injury by improving antioxidant activities, suppressed NF-κB p65 and proinflammatory cytokines (TNF-α), and normalized histopathological changes in liver. | [145] | |
| Pomegranate | ND | Pomegranate (600 mg/kg bw) was orally given to ethanol-induced female Fischer wild-type rats for 10 days. | Pomegranate pretreatment markedly reduced alcohol-mediated plasma endotoxin, gut barrier dysfunction, and inflammatory biomarkers and inhibited elevated oxidative and nitrative stress marker proteins. Moreover, pomegranate also restored the levels of intestinal tight junction proteins (claundin-3, ZO-1, occludin, and claudin-1). | [148] | |
| Cranberry | Cyanidin 3-O-galactoside, peonidin 3-O-galactoside and peonidin 3-O-arabinoside, (+)-catechin, (−)-epicatechin and (−)-epicatechin 3-gallate, procyanidin oligomers, myricetin aglycone, quercetin derivatives, benzoic acid, hydroxycinnamic acid derivatives, and hydroxybenzoic acids | Male albino Wistar rats were received cranberry polyphenols daily, 4 mg/kg bw, along with 4 g/kg bw for 8 weeks | Cranberry polyphenols ameliorated alcoholic liver damage and hepatic steatosis, decreased TG, AST, and ALT activities, diminished TNF-α, TGF-β levels, and free radical generation in mitochondria during intoxication. | [149] | |
| Wolfberry | Zeaxanthin dipalmitate | BRL-3A cells were treated with ethanol (250 mM) or Wolfberry-derived zeaxanthin dipalmitate (1 µM). Wolfberry-derived zeaxanthin dipalmitate (10 mg/kg bw) was administered to ethanol-induced rats for 4 weeks. | Wolfberry-derived zeaxanthin dipalmitate attenuated hepatocyte and whole-liver injury in both ethanol-treated cells and rat model. The underlying mechanism was mainly due to Wolfberry-derived zeaxanthin dipalmitate directly targeted on cell membrane and including receptor P2 × 7 and adipoR1 which further modulate PI3K/AMP-FoXO3 pathways to restore mitochondrial autophagy. Moreover, WZD also alleviates hepatic inflammation by suppressing NLRP3 inflammasome. | [150] | |
| Mango | Mangiferin | Mangiferin (100 and 200 mg/kg bw) was orally given to ethanol-exposed rats for 11 days. | Mangiferin attenuated liver injury induced by chronic plus a single binge ethanol by restoring PDE3B stability, which further activated the AMPK/TBK1 signaling and inhibited NF-κB activation, leading to decreased FFA. | [151] | |
| Lychee | Procyanidin B2, quercetin, 3-O-rutinoside-7-O-a-L-rhamnosidase, isorhamnetin-3-O-rutinoside, (−)-epicatechin, rutin | Lychee pulp (0.4 to 0.8 g/L) was given to mice along with ethanol-containing liquid diet (4%) for 8 weeks. | Lychee pulp ameliorated ALD by decreasing TG, improved the antioxidant status, reduced Nrf2, suppressed lipid synthesis genes, elevated fatty acid β-oxidation expression, and decreased the serum endotoxin level. | [153] | |
| Lychee | Lychee pulp (0.2 and 0.4 g/kg bw) was given to mice along with ethanol-containing liquid diet for 8 weeks. | Lychee pulp supplementation decreased ALT and AST levels, inhibited serum and hepatic oxidative stress, suppressed mitochondrial 8-hydroxy-2’-deoxyguanosine level, and elevated the hepatic ATP level, mitochondrial membrane potential, activities of mitochondrial complexes I and IV, and mitochondrial DNA content. | [154] | ||
| Lychee | Lychee pulp (0.2 and 0.4 g/kg bw) was given to mice along with ethanol-containing liquid diet for 8 weeks. | Lychee pulp phenolic extract alleviated ethanol-induced liver injury in treated mice via reversed alteration of intestinal microbiota composition, downregulated inflammation markers, increased the expression of intestinal tight junction proteins, antimicrobial proteins, and mucus protecting proteins, repressed NF-κB p65, and suppressed CD14 and TLR4 expression. | [155] | ||
| Blueberry | ND | Blueberry polyphenols extract (100 and 200 mg/kg bw) was orally given to ethanol-exposed mice for 30 days. | Blueberry polyphenols decreased the TG lipid droplet content in liver and serum TG and TC levels and decreased lipogenic and increased lipodieretic mRNA levels. Blueberry polyphenols promoted autophagy to accelerate lipid metabolism and thus protect from ALD. | [156] | |
| Mulberry | Water extracts of mulberry (0.3 g/kg bw) were orally administered to chronic ethanol-induced rats. | Water extracts of mulberry decreased TG level and MDA contents, increased glycogen deposits, prevented the disruption of the hepatic cells and nuclei, and decreased Firmicutes to Bacteroidetes ratio. | [158] | ||
| Indian gooseberry | ND | Indian gooseberry was administered (250 mg/kg bw) to alcohol-exposed rats. | Indian gooseberry significantly reduced lipid peroxidation levels and restored antioxidant level. | [160] | |
| Ginseng berry | Ginsenoside F5, ginsenoside Rd, ginsenoside F3, and ginsenoside Re | Ginseng berry extract at the dosage of 0.5–5 mg/mouse along with ethanol was given to mice for 10 days. | Ginseng berry attenuated ALD by improving antioxidant level and reducing inflammatory mediators. | [161] | |
| Apricot | 3-caffeoylshikimic acid, 3-feruloylquinic acid, 3-hydroxy-3-methoxycarbonyl glutaric acid, 1,5-dimethyl citrate, 3,4,5-trimethoxyphenyl-β-D-glucopyranoside, prunate, methyl 3-caffeoylquinate, 3-O- caffeoylquinic acid | AML-12 cells were treated with ethanol or chlorogenic acid. Apricot extract (100 mg/kg bw) along with alcohol (1 g/kg bw) was orally given to mice for 5 days. | Chlorogenic acid derived from apricot extract ameliorated ALD in AML-12 cells by inhibiting alcohol-induced apoptosis, MAPK activation, and antioxidant activities. Apricot extract protected ALD by suppressing lipogenesis in liver tissue, inhibiting activation of SREBP-1, and suppressing hepatic apoptosis and inflammation via ROS-mediated p53 signaling pathway in mice with alcohol-induced liver injury. | [162] | |
| Lemon | ND | Lemon juice (10 mL/kg bw) was orally given to alcohol-induced C57BL/6 mice for 15 days. | Lemon juice markedly inhibited alcohol-induced increase of ALT, AST, lipid peroxidation levels, and hepatic TG, improved antioxidant capacity (SOD and CAT), and improved histopathological changes in ALD mice. | [164] | |
| Citrus depressa | 5-O-demethylnobiletin, sinensetin, tangeretin, and nobiletin | Citrus depressa extract (300 mg/kg) was orally administered to ethanol-induced mice for 8 weeks. | Citrus depressa extract remarkably decreased AST, ALT, TNF-α levels, hepatic MDA, and CYP2E1 expression, and increased glutathione in ALD mice. | [165] | |
| Noni fruit | ND | Noni fruit was orally given to ethanol-exposed mice. | Noni fruit reversed the ethanol-induced changes in mice such as ALT, AST, gamma-glutamyl transferase, LDL-C, HDL-C, TG, and TC. | [166] | |
| Vegetables | Purple potato | Petunidin-3-glucoside, Petunidin-3-rutinoside-5-glucoside, Petunidin-3-caffeoyl-rutinoside-5-glucoside | Purple potato extract was administered at the dosage of 5 and 10 mg/kg bw to ethanol-exposed mice for 5 weeks. | Purple potato extract ameliorated ALD by decreasing ALT, AST, TG, and TC, reducing MDA contents and CYP2E1 protein expression, and increasing GSH and SOD levels in ethanol-exposed mice. | [170] |
| Garlic oil | ND | Human normal cell LO2 was treated with ethanol (100 mM). Garlic oil was administered (50 to 200 mg/kg bw) to ethanol-exposed male Kunming mice. | Garlic oil decreased n-SREBP-1c and CYP2E1 and increased PPAR-α protein levels in human normal cell L02. Garlic oil decreased n-SREBP-1c and CYP2E1 and increased PPAR-α protein levels in ethanol-induced mice. Additionally, garlic oil decreased FAS and inhibited ethanol-induced hepatic mitochondrial dysfunction. | [175] | |
| Asparagus officinalis | ND | Asparagus extracts (400 mg/kg bw) were orally administered to male Wistar rats for 70 connective days. | Edible asparagus protected from toxicity mediated by alcohol by improving antioxidant status. | [178] | |
| Okra seed oil | Polyunsaturated fatty acids; ROS: reactive oxygen species; short-chain fatty acids; monounsaturated fatty acids | Okra seed oil (400 and 800 mg/kg bw) was given to mice for 8 weeks. | Okra seed oil attenuated alcohol-induced liver damage via inhibition of liver fat accumulation, decreased MDA content, decreased hepatic pro-inflammatory cytokines (IL-6, TNF-α, and IL-1), increased SOD and GSH levels, and attenuated lipid metabolic disorder. Furthermore, okra seed oil also modulated gut microbiota dysbiosis by enhancing the Bacteroidetes population and reducing the Proteobacteria proportion, Staphylococcus, and Clostridium XlVa. | [179] | |
| Artichoke | ND | Ethanolic extract of artichoke (0.4 to 1.6 g/kg) was given to ethanol-induced ICR mice for 10 days. | Artichoke remarkably attenuated ALD by preventing elevated levels of ALT, AST, TG, and TC, increased SOD and GSH, decreased MDA level, and suppressed inflammatory pathway (TLR4/NF-κB) in ethanol-induced ICR mice. | [180] | |
| Rhubarb | ND | Rhubarb extract (0.3%) was given to C57BL/6J mice for 17 days. | Rhubarb extracts protected alcohol-induced liver injury by modulating intestinal microflora, improving antioxidant level, and reducing inflammatory response. | [181] | |
| Bitter gourd | ND | Bitter gourd was administered (500 mg/kg bw) to C57BL/6 mice fed an alcohol-containing liquid diet for 30 days. | Bitter gourd supplementation reduced the steatotic alternation of liver histopathology, decreased AST, ALT, hepatic TG level, and MDA content, improved antioxidant defense system (SOD, GSH, GRd, GPx, and CAT), reduced pro-inflammatory cytokine levels (IL-6, TNF-α, and IL-1β), and suppressed ACC, CYP2E1, FAS, and SREBP-1 protein expression in alcohol-induced mice. | [182] | |
| Spices | Cinnamon | ND | Cinnamon bark extract (0.5 mL) was administered for 4 days prior to ethanol, and on 5th day, ethanol (6 g/kg bw) was administered. Murine RAW 264.7 macrophage-like cells were treated with cinnamon bark extract (4 µL). | Cinnamon bark extract protected liver from alcohol via the inhibition of MyD88 expression both in vitro and in vivo. | [183] |
| Fenugreek | ND | Fenugreek seed polyphenol extract (200 mg/kg bw) and ethanol (6 g/kg per day) were fed to rats for 30 days. | Fenugreek seed polyphenol extract inhibited lipid accumulation in ethanol-induced rats. | [184] | |
| Crocus sativus L. | Safranal, crocin, myricetin, and quercetin | Crocus sativus L. (saffron) petal extract was administered (167.5 and 335 mg/kg/day) to ethanol-induced rats for 30 days. | Saffron polyphenolic extract protected liver from ethanol by reducing inflammation in ethanol-administered rats. | [185] | |
| Parsley oil | ND | Parsley oil (50 mg/kg bw) was given to adult male albino rats for 4 weeks. | Parsley oil attenuated alcohol-induced liver injury by oxidative stress mechanism. | [186] | |
| Syzygium aromaticum L. | ND | Polyphenol-rich extract of clove buds (Clovinol) (100 mg/kg bw) was given to ethanol-induced rats for 30 days. | Clovinol decreased alcohol-associated oxidative stress and inflammatory changes in ethanol-induced rats. | [187] | |
| Thymus vulgaris | ND | Thymus vulgaris leaves were orally given (500 mg/kg bw) to ethanol-induced rats for 21 days. | Co-administration (Thymus vulgaris and ethanol) modulated several biomarkers such as ALP, AST, albumin, CAT, MDA, SOD, GST, and lipid profile. | [188] | |
| Peppers | Capsaicin | Capsaicin was given (10 and 20 mg/kg) to ethanol-induced rats. | Capsaicin ameliorated alcohol-induced liver injury by modulating matrix metalloproteinases and suppressing free radical formation and oxidative stress. | [189] | |
| Cereals | Black rice | Cyanidin-3,5-diglucoside, cyanidin-3-glucoside, cyanidin-3-rutinoside, and peonidin-3-glucoside | Alcohol (3.7 g/kg bw) and anthocyanin-rich black rice extract (125, 250, and 500 mg/kg bw) dissolved in water was administered using an intragastric tube for 45 days. | Anthocyanin-rich black rice extract attenuated ALD by decreasing serum AST, ALT, TCH, TG, and GGT levels and improving antioxidant levels. | [105] |
| Rice | Acacetin, caffeic acid, ferulic acid, sinapic acid, p-coumaric acid, quercitrin, vitexin, rutin, hesperidin, ethyl caffeate, and ethyl coumarate | Rice bran phenolic extract (0.25 or 0.50 g/L) was fed along with alcohol-containing liquid diet (4%) to mice for 8 weeks. | Anthocyanin-rich black rice extract supplementation ameliorated ALD by repressing inflammatory responses in liver, intestinal microbiota dysbiosis, and barrier dysfunction and inactivated the endotoxin-TLR4-NF-κB pathway. | [190] | |
| Rice | Acacetin, caffeic acid, ferulic acid, sinapic acid, p-coumaric acid, quercitrin, vitexin, rutin, hesperidin, ethyl caffeate, and ethyl coumarate | Rice bran phenolic extract (0.25 or 0.50 g/L) was fed along with alcohol-containing liquid diet (4%) to mice for 8 weeks. | Rice bran phenolic extract exerted protective effect against ALD in mice fed with an ethanol-containing diet via microRNAs-PGC-1α-TFAM signal pathway. | [191] | |
| Tartary buckwheat | ND | Acute liver injury model group: buckwheat ethanol extracts (8.35, 16.70 and 41.75 mL/kg bw) and ethanol (4 g/kg bw) were intragastrically administered to rats for 7 consecutive days. Chronic alcoholic liver injury: buckwheat ethanol extracts (8.35, 16.70 and 41.75 mL/kg bw) and ethanol (3 g/kg/day bw; 37.5% volume fraction) intragastrically administered to SD rats for 8–9 consecutive weeks. | Tartary buckwheat extract administration significantly decreased serum ALT, AST, and hepatic MDA and improved hepatic GSH level. | [192] | |
| Mung bean extract | Vitexin and isovitexin | Mung bean extract (containing 15 mg vitexin and 13 mg isovitexin, respectively, per kg bw) was given along with spirit (56% alcohol, 16 mL/kg bw) 2 h after the doses of mung bean extract for 14 days. | Mung bean extract decreased ALT and AST and improved antioxidant levels. | [197] | |
| Tea | Pu-erh tea | Gallocatechin, gallic acid, and caffeine | Pu-erh tea extract (1 or 4 g/L w/v added into drinking water) and ethanol solution (10% w/v) were administered by gavage for 30 days. | Pu-erh tea extract contributed to the protective effect against ALD by improving oxidative stress, reducing lipid accumulation, reducing inflammation, and modulating microbiomic and metabolomic responses. | [204] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, L.; Mehmood, A.; Yuan, D.; Usman, M.; Murtaza, M.A.; Yaqoob, S.; Wang, C. Protective Mechanism of Edible Food Plants against Alcoholic Liver Disease with Special Mention to Polyphenolic Compounds. Nutrients 2021, 13, 1612. https://doi.org/10.3390/nu13051612
Zhao L, Mehmood A, Yuan D, Usman M, Murtaza MA, Yaqoob S, Wang C. Protective Mechanism of Edible Food Plants against Alcoholic Liver Disease with Special Mention to Polyphenolic Compounds. Nutrients. 2021; 13(5):1612. https://doi.org/10.3390/nu13051612
Chicago/Turabian StyleZhao, Liang, Arshad Mehmood, Dongdong Yuan, Muhammad Usman, Mian Anjum Murtaza, Sanabil Yaqoob, and Chengtao Wang. 2021. "Protective Mechanism of Edible Food Plants against Alcoholic Liver Disease with Special Mention to Polyphenolic Compounds" Nutrients 13, no. 5: 1612. https://doi.org/10.3390/nu13051612







