Iron Deficiency Anemia in Celiac Disease
Abstract
:1. Introduction
2. Pathogenesis
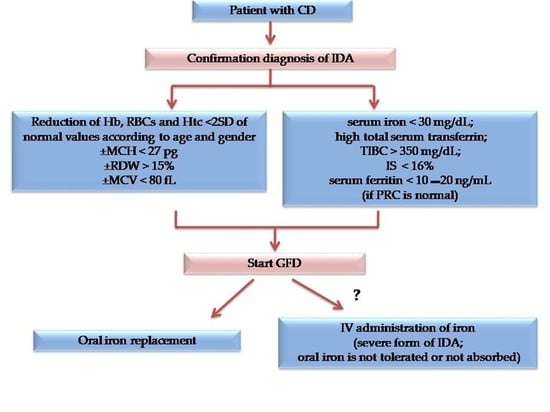
3. Diagnostic Workup for IDA Diagnosis in CD Patients
4. Prevention
5. Treatment
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- De Franceschi, L.; Iolascon, A.; Taherd, A.; Cappellini, M.D. Clinical management of iron deficiency anemia in adults: Sistemic review on advances in diagnosis and treatment. Eur. J. Intern. Med. 2017, 42, 16–23. [Google Scholar] [CrossRef]
- Lerner, N.B.; Sills, R. Iron deficiency anemia. In Nelson Text of Pediatrics, 20th ed.; Kliegman, R.M., Stanton, B.F., Schor, N.F., St. Gemelli, G.V., Behrman, R.E., Eds.; Elseviere: Amsterdam, The Netherlands, 2016; pp. 2322–2326. [Google Scholar]
- Camaschella, C. Iron deficiency. Blood 2019, 133, 30–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levi, M.; Simonetti, M.; Marconi, E.; Brignoli, O.; Cancian, M.; Masotti, A.; Pegoraro, V.; Heiman, F.; Cricelli, C.; Lapi, F. Gender differences in determinants of iron-deficiency anemia: A population-based study conducted in four European countries. Ann. Hematol. 2019, 98, 1573–1582. [Google Scholar] [CrossRef] [PubMed]
- Shahriari, M.; Honar, N.; Yousefi, A.; Javaherizadeh, H. Association of potential celiac disease and refractory iron deficiency anemia in children and adolescents. Arq. Gastroenterol. 2018, 55, 78–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mittal, S.K.; Bhattacharya, M. Celiac Disease and Anemia. Indian Pediatr. 2018, 24, 23–24. [Google Scholar] [CrossRef] [Green Version]
- Kreutz, J.M.; Adriaanse, M.P.M.; vander Ploeg, E.M.C.; Vreugdenhil, A.C.E. Narrative Review: Nutrient Deficiencies in Adults and Children with Treated and Untreated Celiac Disease. Nutrients 2020, 12, 500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freeman, H.J. Iron deficiency anemia in celiac disease. World J. Gastroenterol. 2015, 21, 9233–9238. [Google Scholar] [CrossRef] [PubMed]
- Therrien, A.; Kelly, C.P.; Silvester, J.A. Celiac Disease Extraintestinal Manifestations and Associated Conditions. J. Clin. Gastroenterol. 2020, 54, 8–21. [Google Scholar] [CrossRef]
- Abdallaa, A.; Saifullahb, S.M.; Osmana, M.; Baniyaa, R.; Sidahmedc, S.; LaChanced, J.; Bachuwaa, G. Prevalence of occult celiac disease in females with iron deficiency in the United States: An NHANES analysis. J. Community Hosp. Intern. Med. Perspect. 2017, 7, 347–350. [Google Scholar] [CrossRef] [Green Version]
- Jericho, H.; Sansotta, N.; Guandalini, S. Extraintestinal Manifestations of Celiac Disease. JPGN 2017, 65, 75–79. [Google Scholar] [CrossRef]
- Nardecchia, S.; Auricchio, R.; Discepolo, V.; Troncone, R. Extra-Intestinal Manifestations of Coeliac Disease in Children: Clinical Features and Mechanisms. Front. Pediatr. 2019, 7, 56. [Google Scholar] [CrossRef] [Green Version]
- Kolho, K.L.; Färkkilä, M.A.; Savilahti, E. Undiagnosed celiac disease is commonin Finnish adults. Scand. J. Gastroenterol. 1998, 33, 1280–1283. [Google Scholar] [PubMed]
- Bergamaschi, G.; Markopoulos, K.; Albertini, R.; Di Sabatino, A.; Biagi, F.; Ciccocioppo, R.; Arbustini, E.; Corazza, G.R. Anemia of chronic disease and defective erythropoiet in production in patients with celiac disease. Haematologica 2008, 93, 1785–1791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berry, N.; Basha, J.; Varma, N.; Varma, S.; Prasad, K.K.; Vaiphei, K.; Dhaka, N.; Sinha, S.K.; Kochhar, R. Anemia in celiac disease is multifactorial in etiology: A prospective study from India: Anemia in celiac disease. JGH Open 2018, 2, 196–200. [Google Scholar] [CrossRef]
- Binicier, O.B.; Tosun, F. Evaluation of adult celiac disease from a tertiary reference center: A retrospective analysis. Rev. Assoc. Med. Bras. 2020, 66, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Bottaro, G.; Cataldo, F.; Rotolo, N.; Spina, M.; Corazza, G.R. The clinical pattern of subclinical/silent celiac disease: Analyses is on 1026 consecutive cases. Am. J. Gastroenterol. 1999, 94, 691–696. [Google Scholar] [CrossRef]
- AbuDaya, H.; Lebwohl, B.; Lewis, S.K.; Green, P.H. Celiac disease patients presenting with anemia have more severe disea than those presenting with diarrhea. Clin. Gastroenterol. Hepatol. 2013, 11, 1472–1477. [Google Scholar] [CrossRef] [PubMed]
- Sansotta, N.; Amirikian, K.; Guandalini, S.; Jericho, H. Celiac Disease Symptom Resolution: Effectiveness of the Gluten-free Diet. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 48–52. [Google Scholar] [CrossRef]
- De Falco, L.; Tortora, R.; Imperatore, N.; Bruno, M.; Capasso, M.; Girelli, D.; Castagna, A.; Caporaso, N.; Iolascon, A.; Rispo, A. The role of TMPRSS6 and HFE variants in iron deficiency anemia in celiac disease. Am. J. Hematol. 2018, 93, 383–393. [Google Scholar] [CrossRef] [Green Version]
- Akbari, M.; Moosazadeh, M.; Tabrizi, R.; Khatibi, S.R.; Khodadost, M.; Heydari, S.T.; Tahami, A.N.; Lankarani, K.B. Estimation of iron deficiency anemia in Iranian children and adolescents: A systematic review and meta-analysis. Hematology 2017, 22, 231–239. [Google Scholar] [CrossRef] [Green Version]
- Kochhar, R.; Jain, K.; Thapa, B.R.; Rawal, P.; Khaliq, A.; Kochhar, R.; Bhadada, S.; Vaiphei, K.; Varma, S.; Dutta, U.; et al. Clinical presentation of celiac disease among pediatric compared to adolescent and adult patients. Indian J. Gastroenterol. 2012, 31, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Tolone, C.; Bellini, G.; Punzo, F.; Papparella, A.; Miele, E.; Vitale, A.; Nobili, B.; Strisciuglio, C.; Rossi, F. The DMT1 IVS4+44C>A polymorphis mand the risk of iron deficiency anemia in children with celiac disease. PLoS ONE 2017, 12, e0185822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carroccio, A.; Iannitto, E.; Cavataio, F.; Montalto, G.; Tumminello, M.; Campagna, P.; Lipari, M.G.; Notarbartolo, A.; Iacono, G. Sideropenic anemia and celiac disease: One study, two points of view. Dig. Dis. Sci. 1998, 43, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Kuloglu, Z.; Kirsaçlioglu, C.T.; Kansu, A.; Ensari, A.; Girgin, N. Celiac disease: Presentation of 109 children. Yonsei Med. J. 2009, 50, 617–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanseviero, M.T.; Mazza, G.A.; Pullano, M.N.; Oliveiro, A.C.; Altomare, F.; Pedrelli, L.; Dattilo, B.; Miniero, R.; Meloni, G.; Giancotti, L.; et al. Iron deficiency anemia in newly diagnosed celiac disease in children. Minerva Pediatr. 2016, 68, 1–4. [Google Scholar] [PubMed]
- Mahadev, S.; Laszkowska, M.; Sundström, J.; Björkholm, M.; Lebwohl, B.; Green, P.H.R.; Ludvigsson, J.F. Prevalence of Celiac Disease in Patients with Iron Deficiency Anemia–a Systematic Review with Meta-analysis. Gastroenterology 2018, 155, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Ertekin, V.; Tozun, M.S.; Küçük, N. The prevalence of celiac disease in children with iron-deficiency anemia. Turk. J. Gastroenterol. 2013, 24, 334–338. [Google Scholar] [CrossRef]
- Karaman, K.; Akbayram, S.; Kar, S.; Demirören, K.J. Prevalence of Celiac Disease in Children with Iron Deficiency Anemia in Van Lake Region of Turkey. Pediatr. Hematol. Oncol. 2016, 38, 143–146. [Google Scholar] [CrossRef]
- Kalayci, A.G.; Kanber, Y.; Birinci, A.; Yildiz, L.; Albayrak, D. The prevalence of celiac diseaseas detected by screening in children with iron deficiency anaemia. Acta Paediatr. 2005, 94, 678–681. [Google Scholar] [CrossRef]
- Abd El Dayem, S.M.; Ahmed Aly, A.; Abd El Gafar, E.; Kamel, H. Screening for celiac disease among Egyptian children. Arch. Med. Sci. 2010, 6, 226–235. [Google Scholar] [CrossRef]
- Bansal, D.; Trehan, A.; Gupta, M.K.; Varma, N.; Marwaha, R.K. Serodiagnosis of celiac disease in children referred for evaluation of anemia: A pediatric hematology unit's experience. Indian J. Pathol. Microbiol. 2011, 54, 756–760. [Google Scholar] [PubMed]
- Dubé, C.; Rostom, A.; Sy, R.; Cranney, A.; Saloojee, N.; Garritty, C.; Sampson, M.; Zhang, L.; Yazdi, F.; Mamaladze, V.; et al. The prevalence of celiac disease in average-risk and at-risk Western European populations: A systematic review. Gastroenterology 2005, 128, S57–S67. [Google Scholar] [CrossRef]
- Hershko, C.; Patz, J. Iron in gout the mechanism of anemia in celiac disease. Haematologica 2008, 93, 1761–1765. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corazza, G.R.; Valentini, R.A.; Andreani, M.L.; D’Anchino, M.; Leva, M.T.; Ginaldi, L.; DeFeudis, L.; Quaglino, D.; Gasbarrini, G. Subclinical coeliac disease is a frequent cause of iron-deficiency anaemia. Scand. J. Gastroenterol. 1995, 30, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Annibale, B.; Severi, C.; Chistolini, A.; Antonelli, G.; Lahner, E.; Marcheggiano, A.; Iannoni, C.; Monarca, B.; DelleFave, G. Efficacy of gluten-free diet alone on recovery from iron deficiency anemia in adult celiac patients. Am. J. Gastroenterol. 2001, 96, 132–137. [Google Scholar] [CrossRef]
- Howard, M.R.; Turnbull, A.J.; Morley, P.; Hollier, P.; Webb, R.; Clarke, A. A prospective study of the prevalence of undiagnosed celiac disease in laboratory defined iron and folate deficiency. J. Clin. Pathol. 2002, 55, 754–757. [Google Scholar] [CrossRef] [Green Version]
- Mandal, A.K.; Mehdi, I.; Munshi, S.K.; Lo, T.C. Value of routine duodenal biopsy in diagnosing celiac disease in patients with iron deficiency anaemia. Postgrad. Med. J. 2004, 80, 475–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, D.; Bardan, E.; Derazne, E.; Tzur, D.; Avidan, B. The incidence of gastrointestinal pathology and subsequent anemia in young men presenting with iron deficiency without anemia. Eur. J. Gastroenterol. Hepatol. 2016, 28, 1126–1129. [Google Scholar] [CrossRef] [PubMed]
- Lasa, J.S.; Olivera, P.; Soifer, L.; Moore, M. Iron-Deficiency anemia as asubclinical celiac disease presentation in an Argentinian population. Rev. Gastroenterol. México 2017, 82, 270–273. [Google Scholar] [CrossRef]
- Paez, M.A.; Gramel spacher, A.M.; Sinacore, J.; Winterfield, L.; Venu, M. Delay in Diagnosis of Celiac Disease in Patients Without Gastrointestinal Complaints. Am. J. Med. 2017, 130, 1318–1323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Husby, S.; Koletzko, S.; Korponay-Szabo, I.; Kurppa, K.; Mearin, M.L.; Ribes-Koninckx, C.; Shamir, R.; Troncone, R.; Auricchio, R.; Castillejo, G.; et al. European Society Paediatric Gastroenterology, Hepatology and Nutrition. Guidelines for Diagnosing Coeliac Disease. JPGN 2020, 70, 141–157. [Google Scholar]
- Ko, C.W.; Siddique, S.M.; Patel, A.; Harris, H.; Sultan, S.; Altayar, O.; Falck-Ytter, Y. AGA Clinical Practice Guidelines on th e Gastrointestinal Evaluation of Iron Deficiency Anemia. Gastroenterology 2020, 159, 1085–1094. [Google Scholar] [CrossRef]
- Goddard, A.F.; James, M.W.; Mc Intyre, A.S.; Scott, B.B. British Society of Gastroenterology. Guidelines for the management of iron –deficiency anaemia. Gut 2011, 60, 1309–1316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elli, L.; Norsa, L.; Zullo, A.; Carroccio, A.; Girelli, C.; Oliva, S.; Romano, C.; Leandro, G.; Bellini, M.; Marmo, R.; et al. Diagnosis of chronic anaemia in gastrointestinal disorders: A guideline by the Italian Association of Hospital Gastroenterologists and Endoscopists (AIGO) and the Italian Society of Paediatric Gastroenterology Hepatology and Nutrition (SIGENP). Dig. Liver Dis. 2019, 51, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Smukalla, S.; Lebwohl, B.; Mears, J.G.; Leslie, L.A.; Green, P.H. How Often Do Hematologists Consider Celiac Disease in Iron-Deficiency Anemia? Results of a National Survey. Clin. Adv. Hematol. Oncol. 2014, 12, 100–105. [Google Scholar] [PubMed]
- Nestares, T.; Martín-Masot, R.; Labella, A.; Aparicio, V.A.; Flor-Alemany, M.; López-Frías, M.; Maldonado, J. Isa Gluten-Free Diet Enough to Maintain Correct Micronutrients Status in Young Patients with Celiac Disease? Nutrients 2020, 12, 844. [Google Scholar] [CrossRef] [Green Version]
- Di Nardo, G.; Villa, M.P.; Conti, L.; Ranucci, G.; Pacchiarotti, C.; Principessa, L.; Rauci, U.; Parisei, P. Nutritional deficiencies in children with celiac disease resulting from a gluten-free diet: A systematic review. Nutrients 2019, 11, 1588. [Google Scholar] [CrossRef] [Green Version]
- Saukkonen, J.; Kaukinen, K.; Koivisto, A.M.; Mäki, M.; Laurila, K.; Sievänen, H.; Collin, P.; Kurppa, K. Clinical Characteristics and the Dietary Response in Celiac Disease Patients Presenting with or Without Anemia. Clin. Gastroenterol. 2017, 51, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Nurminen, S.; Kivelä, L.; Huhtala, H.; Kaukinen, K.; Kurppa, K. Extraintestinal manifestations were common in children with celiac disease and were more prevalent in patients with more severe clinical and histological presentation. Acta Paediatr. 2019, 108, 681–687. [Google Scholar] [CrossRef]
- Harper, J.W.; Holleran, S.F.; Ramakrishnan, R.; Bhagat, G.; Green, P.H. Anemia in celiac disease is multifactorial in etiology. Am. J. Hematol. 2007, 82, 996–1000. [Google Scholar] [CrossRef]
- Repo, M.; Rajalahti, T.; Hiltunen, P.; Sotka, A.; Kivelä, L.; Huhtala, H.; Kaukinen, K.; Lindfors, K.; Kurppa, K. Diagnostic findings and long-term prognosis in children with anemia undergoing GI endoscopies. Gastrointest. Endosc. 2020, 91, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Schiepatti, A.; Maimaris, S.; Nicolardi, M.L.; Alimenti, E.; Vernero, M.; Costetti, M.; Costa, S.; Biagi, F. Determinants and Trends of Adherence to a Gluten-Free Diet in Adult Celiac Patients on a Long-Term Follow-Up (2000–2020). Clin. Gastroenterol. Hepatol. 2020, S1542-3565, 31672–33174. [Google Scholar]
- Stefanelli, G.; Viscido, A.; Longo, S.; Magistroni, M.; Latella, G. Persistent Iron Deficiency Anemia in Patients with Celiac Disease Despite a Gluten-Free Diet. Nutrients 2020, 12, 2176. [Google Scholar] [CrossRef]
- Repo, M.; Hannula, M.; Taavela, J.; Hyttinen, J.; Isola, J.; Hiltunen, P.; Popp, A.; Kaukinen, K.; Kurppa, K.; Lindfors, K. Iron Transporter Protein Expressions in Children with Celiac Disease. Nutrients 2021, 13, 776. [Google Scholar] [CrossRef] [PubMed]
- Barisani, D.; Parafioriti, A.; Bardella, M.T.; Zoller, H.; Conte, D.; Armiraglio, E.; Trovato, C.; Koch, R.O.; Weiss, G. Adaptive changes of duodenal iron transport proteins in celiac disease. Physiol. Genom. 2004, 17, 316–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, M.; Singh, P.; Agnihotri, A.; Das, P.; Mishra, A.; Verma, A.K.; Ahuja, A.; Sreenivas, V.; Khadgawat, R.; Gupta, S.D.; et al. Celiac disease: A disease with varied manifestations in adults and adolescents. J. Dig. Dis. 2013, 14, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Martín-Masot, R.; Nestares, M.T.; Diaz-Castro, J.; López-Aliaga, I.; MuñozAlférez, M.J.; Moreno-Fernandez, J.; Maldonado, J. Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review. Nutrients 2019, 11, 2557. [Google Scholar] [CrossRef] [Green Version]
- Elli, L.; Poggiali, E.; Tomba, C.; Andreozzi, F.; Nava, I.; Bardella, M.T.; Campostrini, N.; Girelli, D.; Conte, D.; Cappellini, M.D. Does TMPRSS6RS855791 polymorphism contribute to iron deficiency in treated celiac disease? Am. J. Gastroenterol. 2015, 110, 200–202. [Google Scholar] [CrossRef]
- Hoppe, M.; Onning, G.; Berggren, A.; Hulthen, L. Probiotic strain Lactobacillus plantarum 299v increases iron absorption from an iron supplemented fruit drink: A double-isotope cross-over single-blind study in women of reproductive age. Br. J. Nutr. 2015, 114, 1195–1202. [Google Scholar] [CrossRef] [Green Version]
- Rosen, G.M.; Morrissette, S.; Larson, A.; Stading, P.; Griffin, K.H.; Barnes, T.L. Use of a Probiotic to Enhance Iron Absorption in a Randomized Trial of Pediatric Patients Presenting with Iron Deficiency. J. Pediatr. 2019, 207, 192–197. [Google Scholar] [CrossRef]
- Ferus, K.; Drabinska, N.; Krupa-Kozak, U.; Jarocka-Cyrta, E. Randomized, Placebo-Controlled, Pilot Clinical Trial to Evaluate the Effect of Supplementation with Prebiotic Synergy 1 on Iron Homeostasis in Children and Adolescents with Celiac Disease Treated with a Gluten-Free Diet. Nutrients 2018, 10, 1818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrari, P. Treatment of mil non chemotherapy induced iron deficiency anemia in cancer patients: Comparison between oral ferrous bisglycinate chelate and ferrous sulfate. Biomed. Pharm. 2012, 66, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Bagna, R.; Spada, E.; Mazzone, R.; Saracco, P.; Boetti, T.; Cester, E.A.; Bertino, E.; Coscia, A. Efficacy of Supplementation with Iron Sulfate Compared to Iron Bisglycinate Chelate in Preterm Infants. Curr. Pediatr. Rev. 2018, 14, 123–129. [Google Scholar] [CrossRef] [PubMed]
- JoãoName, J.; Rodrigues Vasconcelos, A.; Valzachi Rocha Maluf, M.C. Iron Bisglycinate Chelate and Polymaltose Iron for the Treatment of Iron Deficiency Anemia: A Pilot Randomized Trial. Curr. Pediatric. Rev. 2018, 14, 261–268. [Google Scholar]
- Hacibekiroglu, T.; Akinci, S.; Basturk, A.R.; Bakanay, S.M.; Ulas, T.; Guney, T.; Dilek, I.A. Forgotten screening test for iron deficiency anemia: Oral iron absorbtion test. Clin. Ter. 2013, 164, 495–497. [Google Scholar]
- Mazza, G.A.; Pedrelli, L.; Battaglia, E.; Giancotti, L.; Miniero, R. Oral iron absorption test with ferrous bisglycinate chelate in children with celiac disease: Preliminary results. Minerva Pediatr. 2019, 10, 139–143. [Google Scholar] [CrossRef]
- Rondinelli, M.B.; Di Bartolomei, A.; De Rosa, A.; Pirelli, L. Oral Iron Absorption Test (OIAT): A forgotten screening test for iron absorption from the gastrointestinal tract. A casa series of Iron Deficiency Anemia (IDA) patients treated with FERALGINE®. J. Blood Disord. Med. 2017, 2, 1. [Google Scholar]
- Vernero, M.; Boano, V.; Ribaldone, D.G.; Pellicano, R.; Astegiano, M. Oral iron supplementation with Feralgine® in inflammatory bowel disease: A retrospective observational study. Minerva Gastroenterol. Dietol. 2019, 65, 200–203. [Google Scholar] [CrossRef]
- Giancotti, L.; Talarico, V.; Mazza, G.A.; Marrazzo, S.; Gangemi, G.; Miniero, R.; Bertini, M. FERALGINE™ a new approach for Iron Deficiency Anemia in Celiac Patients. Nutrients 2019, 11, 887. [Google Scholar] [CrossRef] [Green Version]
- Talarico, V.; Giancotti, L.; Miniero, R.; Bertini, M. Iron Deficiency Anemia Refractory to Conventional Therapy but Responsive to Feralgine® in a Young Woman with Celiac Disease. Int. Med. Case Rep. J. 2021, 14, 89–93. [Google Scholar] [CrossRef]
- Yu, X.; Chen, L.; Ding, H.; Zhao, Y.; Feng, J. Iron Transport from Ferrous Bisglycinate and Ferrous Sulfate in DMT1-Knockout Human Intestinal Caco-2 Cells. Nutrients 2019, 11, 485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liao, Z.C.; Guan, W.T.; Chen, F.; Hou, D.X.; Wang, C.X.; Lv, Y.T.; Qiao, H.Z.; Chen, J.; Han, J.H. Ferrous bisglycinate increased iron transportation through DMT1 and PepT1 in pig intestinal epithelial cells compared with ferrous sulphate. J. Anim. Feed Sci. 2014, 23, 153–159. [Google Scholar] [CrossRef] [Green Version]
- Auerbach, M.; Ballard, H. Clinical use of intravenous iron: Administration, efficacy, and safety. Hematol. Am. Soc. Hematol. Educ. Program. 2010, 2010, 338–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayraktar, U.D.; Bayraktar, S. Treatment of iron deficiency anemia associated with gastrointestinal tract disease. Word J. Gastroenterol. 2010, 16, 2720–2725. [Google Scholar] [CrossRef]
- Peyrin-Biroulet, L.; Lopez, A.; Cummings, J.R.; Dignass, A.; Detlie, T.E.; Danese, S. Review article: Treating–to –target for inflammatory bowel disease-associated anaemia. Aliment. Pharmacol. Ther. 2018, 48, 610. [Google Scholar] [CrossRef] [PubMed]
- Carman, N.; Muir, R.; Lewindon, P. Ferriccarboxymaltose in the treatment of iron deficiency in pediatric inflammatory bowel disease. Transl. Pediatr. 2019, 8, 28–34. [Google Scholar] [CrossRef] [PubMed]
| Authors | Country | No. Of Patients | % IDA | Year of the Study |
|---|---|---|---|---|
| ADULTS | ||||
| Koho, et al. [13] | Finland | 8 | 25 | 1998 |
| Bergamaschi et al. [14] | Italy | 132 | 34 | 2008 |
| Berry et al. [15] | India | 103 | 81 | 2018 |
| Binicier et al. [16] | Turkey | 195 | 53 | 2020 |
| Bottaro et al. [17] | Italy | 315 | 46 | 1999 |
| Abu Daya et al. [18] | USA | 727 | 21 | 2013 |
| Sansotta et al. [19] | USA | 327 | 48 | 2018 |
| De Falco et al. [20] | Italy | 505 | 45 | 2018 |
| Akbari et al. [21] | Iran | 27 | 52 | 2006 |
| Kockar et al. [22] | India | 434 | 84 | 2012 |
| CHILDREN | ||||
| Bottaro et al. [17] | Italy | 485 | 35 | 1999 |
| Sansotta et al. [19] | USA | 227 | 12 | 2018 |
| Tolone et al. [23] | Italy | 385 | 35 | 2017 |
| Carroccio et al. [24] | Italy | 130 | 70 | 1998 |
| Kullogu et al. [25] | Turkey | 109 | 82 | 2009 |
| Sanseviero et al. [26] | Italy | 518 | 22 | 2016 |
| (a) Red cell parameters values for diagnosis of IDA |
|
| (b) Biochemical parameters values for diagnosis of IDA |
|
| (c) Other parameters evaluable for diagnosis of IDA |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talarico, V.; Giancotti, L.; Mazza, G.A.; Miniero, R.; Bertini, M. Iron Deficiency Anemia in Celiac Disease. Nutrients 2021, 13, 1695. https://doi.org/10.3390/nu13051695
Talarico V, Giancotti L, Mazza GA, Miniero R, Bertini M. Iron Deficiency Anemia in Celiac Disease. Nutrients. 2021; 13(5):1695. https://doi.org/10.3390/nu13051695
Chicago/Turabian StyleTalarico, Valentina, Laura Giancotti, Giuseppe Antonio Mazza, Roberto Miniero, and Marco Bertini. 2021. "Iron Deficiency Anemia in Celiac Disease" Nutrients 13, no. 5: 1695. https://doi.org/10.3390/nu13051695