Colostrum Therapy for Human Gastrointestinal Health and Disease
Abstract
1. Introduction
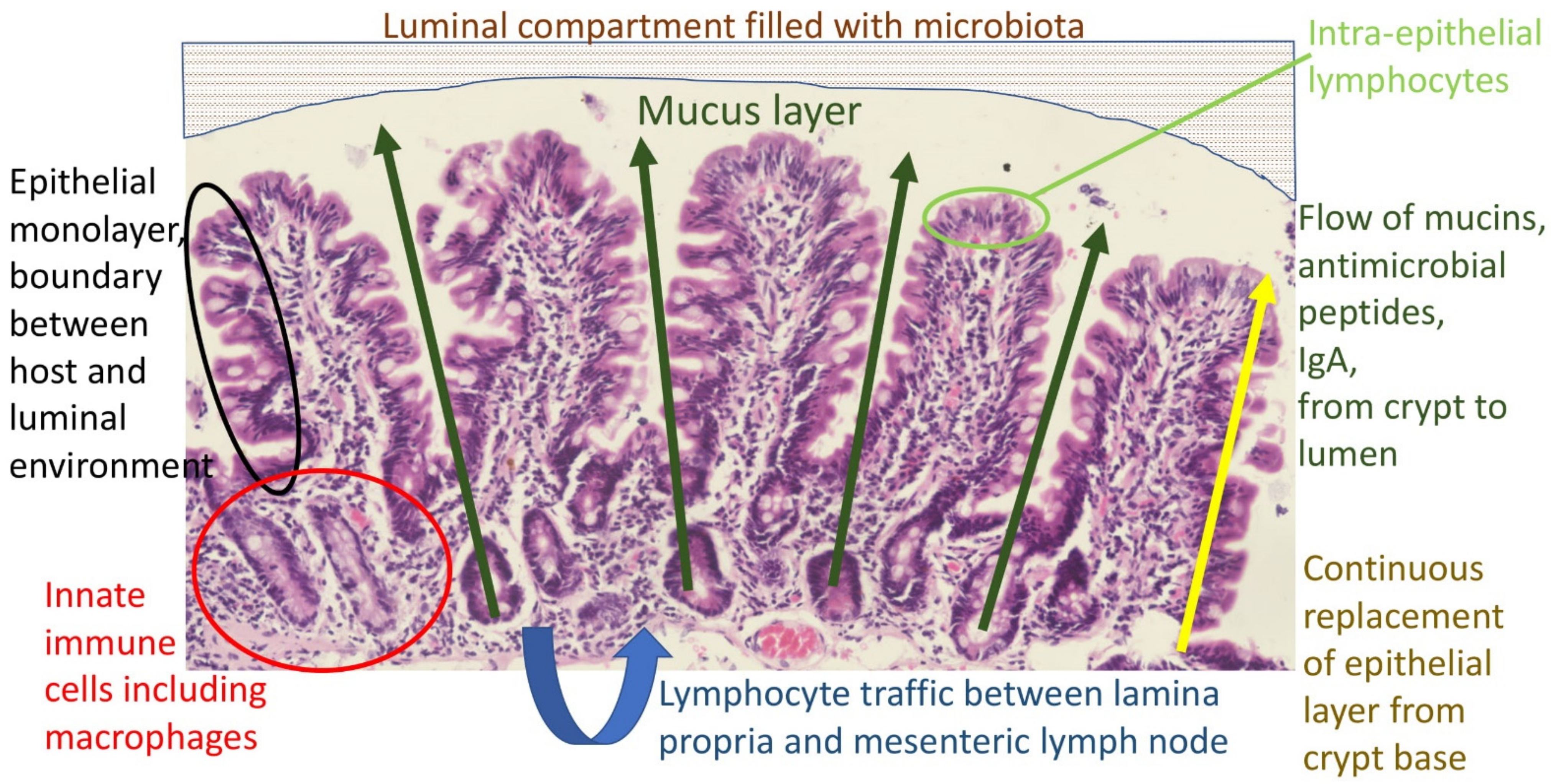
2. The Mucosal Barrier in the Gut
- The gastric acid barrier limiting access to the intestine;
- The epithelium, a single cell monolayer joined by tight junctions and other cell adhesion structures [22], and which is continuously replaced from the crypts;
- Intra-epithelial lymphocytes (IELs), a group of resident lymphocytes;
- Lymphocytes and macrophages in the lamina propria, which circulate to mesenteric lymph nodes and provide anamnestic immunity;
- Downstream, the macrophage (Kupffer cell) compartment of the liver provides a barrier against pathogens and pathogen-associated molecular patterns (PAMPs), which escape the first four elements of the barrier listed above. This will not be discussed further;
- The microbiota, which confers resistance to extraneous colonization.
3. Gastrointestinal Repair Mechanisms
4. Clinical Applications: Colostrum as Therapy
4.1. NSAID-Induced Gastrointestinal Injury
4.2. Inflammatory Bowel Disease (IBD)
4.3. Infectious Diarrhea
4.4. Short Bowel Syndrome; Intestinal Failure
4.5. Necrotizing Enterocolitis
4.6. Intestinal Consequences of Cancer Treatment
4.7. Use of BC in Combination with Other Nutraceuticals
4.8. Other Conditions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Williams, J.G.; Roberts, S.E.; Ali, M.F.; Cheung, W.Y.; Cohen, D.R.; Demery, G.; Edwards, A.; Greer, M.; Hellier, M.D.; Hutchings, H.A.; et al. Gastroenterology services in the UK. The burden of disease, and the organisation and delivery of services for gastrointestinal and liver disorders: A review of the evidence. Gut 2007, 56 (Suppl. 1), 1–113. [Google Scholar] [CrossRef] [PubMed]
- Peery, A.F.; Crockett, S.D.; Murphy, C.C.; Lund, J.L.; Dellon, E.S.; Williams, J.L.; Jensen, E.T.; Shaheen, N.J.; Barritt, A.S.; Lieber, S.R.; et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology 2019, 156, 254–272.e11. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Abnet, C.C.; Neale, R.E.; Vignat, J.; Giovannucci, E.L.; McGlynn, K.A.; Bray, F. Global Burden of 5 Major Types of Gastrointestinal Cancer. Gastroenterology 2020, 159, 335–349.e15. [Google Scholar] [CrossRef] [PubMed]
- Windsor, J.W.; Kaplan, G.G. Evolving Epidemiology of IBD. Curr. Gastroenterol. Rep. 2019, 21, 40. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.; Kelly, P. Inflammatory bowel disease in Africa: What is the current state of knowledge? Int. Health 2020, 12, 222–230. [Google Scholar] [CrossRef]
- Fukui, H. Increased Intestinal Permeability and Decreased Barrier Function: Does It Really Influence the Risk of Inflammation? Inflamm. Intest. Dis. 2016, 1, 135–145. [Google Scholar] [CrossRef]
- Lee, G.O.; Kosek, P.; Lima, A.A.; Singh, R.; Yori, P.P.; Olortegui, M.P.; Lamsam, J.L.; Oliveira, D.B.; Guerrant, R.L.; Kosek, M. Lactulose: Mannitol diagnostic test by HPLC and LC-MSMS platforms: Considerations for field studies of intestinal barrier function and environmental enteropathy. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 544–550. [Google Scholar] [CrossRef]
- Aldars-García, L.; Chaparro, M.; Gisbert, J. Systematic Review: The Gut Microbiome and Its Potential Clinical Application in Inflammatory Bowel Disease. Microorganisms 2021, 9, 977. [Google Scholar] [CrossRef]
- Marie, C.; Ali, A.; Chandwe, K.; Petri, W.A.; Kelly, P. Pathophysiology of environmental enteric dysfunction and its impact on oral vaccine efficacy. Mucosal Immunol. 2018, 11, 1290–1298. [Google Scholar] [CrossRef]
- Strnad, P.; Tacke, F.; Koch, A.; Trautwein, P.S.F.T.A.K.C. Liver—Guardian, modifier and target of sepsis. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 55–66. [Google Scholar] [CrossRef]
- Van Vliet, M.J.; Harmsen, H.J.; de Bont, E.S.; Tissing, W.J. The role of intestinal microbiota in the development and severity of chemotherapy-induced mucositis. PLoS Pathog. 2010, 6, e1000879. [Google Scholar] [CrossRef]
- Luján, J.A.; Rugeles, M.T.; Taborda, N.A. Contribution of the Microbiota to Intestinal Homeostasis and its Role in the Pathogenesis of HIV-1 Infection. Curr. HIV Res. 2019, 17, 13–25. [Google Scholar] [CrossRef]
- Marchetti, G.; Tincati, C.; Silvestri, G. Microbial Translocation in the Pathogenesis of HIV Infection and AIDS. Clin. Microbiol. Rev. 2013, 26, 2–18. [Google Scholar] [CrossRef]
- Micó-Carnero, M.; Rojano-Alfonso, C.; Álvarez-Mercado, A.I.; Gracia-Sancho, J.; Casillas-Ramírez, A.; Peralta, C. Effects of Gut Metabolites and Microbiota in Healthy and Marginal Livers Submitted to Surgery. Int. J. Mol. Sci. 2020, 22, 44. [Google Scholar] [CrossRef]
- Chi, X.; Pan, C.Q.; Liu, S.; Cheng, D.; Cao, Z.; Xing, H. Regulating Intestinal Microbiota in the Prevention and Treatment of Alcohol-Related Liver Disease. Can. J. Gastroenterol. Hepatol. 2020, 2020, 6629196. [Google Scholar] [CrossRef]
- Pierantonelli, I.; Svegliati-Baroni, G. Nonalcoholic Fatty Liver Disease: Basic Pathogenetic Mechanisms in the Progression From NAFLD to NASH. Transplantation 2019, 103, e1–e13. [Google Scholar] [CrossRef]
- Playford, R.; Weiser, M. Bovine Colostrum: Its Constituents and Uses. Nutrients 2021, 13, 265. [Google Scholar] [CrossRef]
- Steele, J.; Sponseller, J.; Schmidt, D.; Cohen, O.; Tzipori, S. Hyperimmune bovine colostrum for treatment of GI infections: A review and update on Clostridium difficile. Hum. Vaccin. Immunother. 2013, 9, 1565–1568. [Google Scholar] [CrossRef]
- Civra, A.; Altomare, A.; Francese, R.; Donalisio, M.; Aldini, G.; Lembo, D. Colostrum from cows immunized with a veterinary vaccine against bovine rotavirus displays enhanced in vitro anti-human rotavirus activity. J. Dairy Sci. 2019, 102, 4857–4869. [Google Scholar] [CrossRef]
- Schroeder, B.O. Fight them or feed them: How the intestinal mucus layer manages the gut microbiota. Gastroenterol. Rep. 2019, 7, 3–12. [Google Scholar] [CrossRef]
- Bevins, C.L.; Salzman, N. Paneth cells, antimicrobial peptides and maintenance of intestinal homeostasis. Nat. Rev. Genet. 2011, 9, 356–368. [Google Scholar] [CrossRef]
- Paradis, T.; Bègue, H.; Basmaciyan, L.; Dalle, F.; Bon, F. Tight Junctions as a Key for Pathogens Invasion in Intestinal Epithelial Cells. Int. J. Mol. Sci. 2021, 22, 2506. [Google Scholar] [CrossRef]
- Kelly, P. Starvation and Its Effects on the Gut. Adv. Nutr. 2020, 12, 897–903. [Google Scholar] [CrossRef]
- Brubaker, P.L. Glucagon-like Peptide-2 and the Regulation of Intestinal Growth and Function. Compr. Physiol. 2011, 8, 1185–1210. [Google Scholar] [CrossRef]
- Fesler, Z.; Mitova, E.; Brubaker, P.L. GLP-2, EGF, and the Intestinal Epithelial IGF-1 Receptor Interactions in the Regulation of Crypt Cell Proliferation. Endocrinology 2020, 161, bqaa040. [Google Scholar] [CrossRef]
- Galura, G.M.; Chavez, L.O.; Robles, A.; McCallum, R. Gastroduodenal Injury: Role of Protective Factors. Curr. Gastroenterol. Rep. 2019, 21, 34. [Google Scholar] [CrossRef]
- Goldenring, J.R. Pyloric metaplasia, pseudopyloric metaplasia, ulcer-associated cell lineage and spasmolytic polypeptide-expressing metaplasia: Reparative lineages in the gastrointestinal mucosa. J. Pathol. 2018, 245, 132–137. [Google Scholar] [CrossRef]
- Rao, J.N.; Rathor, N.; Zhuang, R.; Zou, T.; Liu, L.; Xiao, L.; Turner, D.J.; Wang, J.-Y. Polyamines regulate intestinal epithelial restitution through TRPC1-mediated Ca2+ signaling by differentially modulating STIM1 and STIM2. Am. J. Physiol. Physiol. 2012, 303, C308–C317. [Google Scholar] [CrossRef] [PubMed]
- Timmons, J.; Chang, E.T.; Wang, J.-Y.; Rao, J.N. Polyamines and Gut Mucosal Homeostasis. J. Gastrointest. Dig. Syst. 2012, 2, 1. [Google Scholar] [CrossRef]
- Chatterton, D.E.; Nguyen, D.N.; Bering, S.B.; Sangild, P.T. Anti-inflammatory mechanisms of bioactive milk proteins in the intestine of newborns. Int. J. Biochem. Cell Biol. 2013, 45, 1730–1747. [Google Scholar] [CrossRef] [PubMed]
- Blais, M.; Pouliot, Y.; Gauthier, S.; Boutin, Y.; Lessard, M. A gene expression programme induced by bovine colostrum whey promotes growth and wound-healing processes in intestinal epithelial cells. J. Nutr. Sci. 2014, 3, e57. [Google Scholar] [CrossRef][Green Version]
- Playford, R.J.; Macdonald, C.E.; Johnson, W.S. Colostrum and milk-derived peptide growth factors for the treatment of gastrointestinal disorders. Am. J. Clin. Nutr. 2000, 72, 5–14. [Google Scholar] [CrossRef]
- Asaro, J.A.; Khan, Z.; Brewer, M.; Klose, K.; Pesce, C.; Schanler, R.J.; Codipilly, C.N. Relationship Between Milk Fat Globule-Epidermal Growth Factor 8 and Intestinal Cytokines in Infants Born Preterm. J. Pediatr. 2021, 230, 71–75.e1. [Google Scholar] [CrossRef]
- Stenson, W.F.; Ciorba, M.A. Nonmicrobial Activation of TLRs Controls Intestinal Growth, Wound Repair, and Radioprotection. Front. Immunol. 2021, 11, 617510. [Google Scholar] [CrossRef]
- Jardé, T.; Chan, W.H.; Rossello, F.J.; Kahlon, T.K.; Theocharous, M.; Arackal, T.K.; Flores, T.; Giraud, M.; Richards, E.; Chan, E.; et al. Mesenchymal Niche-Derived Neuregulin-1 Drives Intestinal Stem Cell Proliferation and Regeneration of Damaged Epithelium. Cell Stem Cell 2020, 27, 646–662.e7. [Google Scholar] [CrossRef]
- Playford, R.J.; Cattell, M.; Marchbank, T. Marked variability in bioactivity between commercially available bovine colostrum for human use; implications for clinical trials. PLoS ONE 2020, 15, e0234719. [Google Scholar] [CrossRef]
- Playford, R.J.; Floyd, D.N.; Macdonald, C.E.; Calnan, D.P.; Adenekan, R.O.; Johnson, W.; Goodlad, R.A.; Marchbank, T. Bovine colostrum is a health food supplement which prevents NSAID induced gut damage. Gut 1999, 44, 653–658. [Google Scholar] [CrossRef]
- Kim, J.W.; Jeon, W.K.; Kim, E.J. Combined effects of bovine colostrum and glutamine in diclofenac-induced bacterial translocation in rat. Clin. Nutr. 2005, 24, 785–793. [Google Scholar] [CrossRef]
- Cairangzhuoma; Yamamoto, M.; Muranishi, H.; Inagaki, M.; Uchida, K.; Yamashita, K.; Saito, S.; Yabe, T.; Kanamaru, Y. Skimmed, sterilized, and concentrated bovine late colostrum promotes both prevention and recovery from intestinal tissue damage in mice. J. Dairy Sci. 2013, 96, 1347–1355. [Google Scholar] [CrossRef]
- Playford, R.J.; Macdonald, C.E.; Calnan, D.P.; Floyd, D.N.; Podas, T.; Johnson, W.; Wicks, A.C.; Bashir, O.; Marchbank, T. Co-administration of the health food supplement, bovine colostrum, reduces the acute non-steroidal anti-inflammatory drug-induced increase in intestinal permeability. Clin. Sci. 2001, 100, 627. [Google Scholar] [CrossRef]
- Kanwar, J.; Kanwar, R.; Stathopoulos, S.; Haggarty, N.; MacGibbon, A.; Palmano, K.; Roy, K.; Rowan, A.; Krissansen, G. Comparative activities of milk components in reversing chronic colitis. J. Dairy Sci. 2016, 99, 2488–2501. [Google Scholar] [CrossRef] [PubMed]
- Filipescu, I.E.; Leonardi, L.; Menchetti, L.; Guelfi, G.; Traina, G.; Casagrande-Proietti, P.; Piro, F.; Quattrone, A.; Barbato, O.; Brecchia, G. Preventive effects of bovine colostrum supplementation in TNBS-induced colitis in mice. PLoS ONE 2018, 13, e0202929. [Google Scholar] [CrossRef] [PubMed]
- Spalinger, M.R.; Atrott, K.; Baebler, K.; Schwarzfischer, M.; Melhem, H.; Peres, D.R.; Lalazar, G.; Rogler, G.; Scharl, M.; Frey-Wagner, I. Administration of the Hyper-immune Bovine Colostrum Extract IMM-124E Ameliorates Experimental Murine Colitis. J. Crohns Colitis 2018, 13, 785–797. [Google Scholar] [CrossRef] [PubMed]
- Playford, R.J.; Garbowsky, M.; Marchbank, T. Pasteurized Chicken Egg Powder Stimulates Proliferation and Migration of AGS, RIE1, and Caco-2 Cells and Reduces NSAID-Induced Injury in Mice and Colitis in Rats. J. Nutr. 2020, 150, 1434–1442. [Google Scholar] [CrossRef]
- Menchetti, L.; Curone, G.; Filipescu, I.E.; Barbato, O.; Leonardi, L.; Guelfi, G.; Traina, G.; Casagrande-Proietti, P.; Riva, F.; Casano, A.B.; et al. The Prophylactic Use of Bovine Colostrum in a Murine Model of TNBS-Induced Colitis. Animals 2020, 10, 492. [Google Scholar] [CrossRef]
- Khan, Z.; Macdonald, C.; Wicks, A.C.; Holt, M.P.; Floyd, D.; Ghosh, S.; Wright, N.A.; Playford, R.J. Use of the ‘nutriceutical’, bovine colostrum, for the treatment of distal colitis: Results from an initial study. Aliment. Pharmacol. Ther. 2002, 16, 1917–1922. [Google Scholar] [CrossRef]
- Choudhry, N.; Scott, F.; Edgar, M.; Sanger, G.J.; Kelly, P. Reversal of Pathogen-Induced Barrier Defects in Intestinal Epithelial Cells by Contra-pathogenicity Agents. Dig. Dis. Sci. 2021, 66, 88–104. [Google Scholar] [CrossRef]
- Li, J.; Xu, Y.-W.; Jiang, J.-J.; Song, Q.-K. Bovine colostrum and product intervention associated with relief of childhood infectious diarrhea. Sci. Rep. 2019, 9, 3093. [Google Scholar] [CrossRef]
- Barakat, S.H.; Meheissen, M.A.; Omar, O.M.; Elbana, D.A. Bovine Colostrum in the Treatment of Acute Diarrhea in Children: A Double-Blinded Randomized Controlled Trial. J. Trop. Pediatr. 2019, 66, 46–55. [Google Scholar] [CrossRef]
- Gaensbauer, J.T.; Melgar, M.A.; Calvimontes, D.M.; Lamb, M.M.; Asturias, E.J.; Contreras-Roldan, I.L.; Dominguez, S.R.; Robinson, C.C.; Berman, S. Efficacy of a bovine colostrum and egg-based intervention in acute childhood diarrhoea in Guatemala: A randomised, double-blind, placebo-controlled trial. BMJ Glob. Health 2017, 2, e000452. [Google Scholar] [CrossRef]
- Saad, K.; Abo-Elela, M.G.M.; El-Baseer, K.A.A.; Ahmed, A.E.; Ahmad, F.-A.; Tawfeek, M.S.K.; Houfey, A.A.E.-; Aboul_Khair, M.D.; Abdel-Salam, A.M.; Abo-Elgheit, A.; et al. Effects of bovine colostrum on recurrent respiratory tract infections and diarrhea in children. Medicine 2016, 95, e4560. [Google Scholar] [CrossRef]
- Otto, W.; Najnigier, B.; Stelmasiak, T.; Robins-Browne, R.M. Randomized control trials using a tablet formulation of hyperimmune bovine colostrum to prevent diarrhea caused by enterotoxigenicEscherichia coliin volunteers. Scand. J. Gastroenterol. 2011, 46, 862–868. [Google Scholar] [CrossRef]
- Kaducu, F.O.; Okia, S.A.; Upenytho, G.; Elfstrand, L.; Florén, C.-H. Effect of bovine colostrum-based food supplement in the treatment of HIV-associated diarrhea in Northern Uganda: A randomized controlled trial. Indian J. Gastroenterol. 2011, 30, 270–276. [Google Scholar] [CrossRef]
- Eslamian, G.; Ardehali, S.H.; Baghestani, A.-R.; Shariatpanahi, Z.V. Effects of early enteral bovine colostrum supplementation on intestinal permeability in critically ill patients: A randomized, double-blind, placebo-controlled study. Nutrition 2019, 60, 106–111. [Google Scholar] [CrossRef]
- Bierut, T.; Duckworth, L.; Grabowsky, M.; Ordiz, M.I.; Laury, M.L.; Callaghan-Gillespie, M.; Maleta, K.; Manary, M.J. The effect of bovine colostrum/egg supplementation compared with corn/soy flour in young Malawian children: A randomized, controlled clinical trial. Am. J. Clin. Nutr. 2021, 113, 420–427. [Google Scholar] [CrossRef]
- Paris, M.C.; Fuller, P.J.; Carstensen, B.; Nagy, E.; Taylor, R.G.; Sourial, M.; Holst, J.J.; Hartmann, B.; Binesm, J.E. Plasma GLP-2 Levels and Intestinal Markers in the Juvenile Pig During Intestinal Adaptation: Effects of Different Diet Regimens. Dig. Dis. Sci. 2004, 49, 1688–1695. [Google Scholar] [CrossRef]
- Nagy, E.S.; Paris, M.C.; Taylor, R.G.; Fuller, P.J.; Sourial, M.; Justice, F.; Bines, J.E. Colostrum Protein Concentrate Enhances Intestinal Adaptation After Massive Small Bowel Resection in Juvenile Pigs. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 487–492. [Google Scholar] [CrossRef]
- Pereira-Fantini, P.M.; Thomas, S.L.; Taylor, R.G.; Nagy, E.; Sourial, M.; Fuller, P.J.; Bines, J.E. Colostrum Supplementation Restores Insulin-like Growth Factor -1 Levels and Alters Muscle Morphology Following Massive Small Bowel Resection. J. Parenter. Enter. Nutr. 2008, 32, 266–275. [Google Scholar] [CrossRef]
- Aunsholt, L.; Qvist, N.; Sangild, P.T.; Vegge, A.; Stoll, B.; Burrin, D.G.; Jeppesen, P.B.; Eriksen, T.; Husby, S.; Thymann, T. Minimal Enteral Nutrition to Improve Adaptation After Intestinal Resection in Piglets and Infants. JPEN J. Parenter. Enteral. Nutr. 2018, 42, 446–454. [Google Scholar] [CrossRef]
- Aunsholt, L.; Jeppesen, P.B.; Lund, P.; Sangild, P.T.; Ifaoui, I.B.; Qvist, N.; Husby, S. Bovine colostrum to children with short bowel syndrome: A randomized, double-blind, crossover pilot study. JPEN J. Parenter. Enteral. Nutr. 2014, 38, 99–106. [Google Scholar] [CrossRef]
- Lund, P.; Sangild, P.T.; Aunsholt, L.; Hartmann, B.; Holst, J.J.; Mortensen, J.; Mortensen, P.B.; Jeppesen, P.B. Randomised controlled trial of colostrum to improve intestinal function in patients with short bowel syndrome. Eur. J. Clin. Nutr. 2012, 66, 1059–1065. [Google Scholar] [CrossRef]
- Jensen, M.L.; Sangild, P.T.; Lykke, M.; Schmidt, M.; Boye, M.; Jensen, B.B.; Thymann, T. Similar efficacy of human banked milk and bovine colostrum to decrease incidence of necrotizing enterocolitis in preterm piglets. Am. J. Physiol. Integr. Comp. Physiol. 2013, 305, R4–R12. [Google Scholar] [CrossRef]
- Li, Y.; Jensen, M.L.; Chatterton, D.E.; Jensen, B.B.; Thymann, T.; Kvistgaard, A.S.; Sangild, P.T. Raw bovine milk improves gut responses to feeding relative to infant formula in preterm piglets. Am. J. Physiol. Liver Physiol. 2014, 306, G81–G90. [Google Scholar] [CrossRef] [PubMed]
- Støy, A.C.F.; Heegaard, P.M.; Thymann, T.; Bjerre, M.; Skovgaard, K.; Boye, M.; Stoll, B.; Schmidt, M.; Jensen, B.B.; Sangild, P.T. Bovine colostrum improves intestinal function following formula-induced gut inflammation in preterm pigs. Clin. Nutr. 2014, 33, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Seigel, J.K.; Smith, P.B.; Ashley, P.L.; Cotten, C.M.; Herbert, C.C.; King, B.A.; Maynor, A.R.; Neill, S.; Wynn, J.; Bidegain, M. Early Administration of Oropharyngeal Colostrum to Extremely Low Birth Weight Infants. Breastfeed. Med. 2013, 8, 491–495. [Google Scholar] [CrossRef] [PubMed]
- Balachandran, B.; Dutta, S.; Singh, R.; Prasad, R.; Kumar, P. Bovine Colostrum in Prevention of Necrotizing Enterocolitis and Sepsis in Very Low Birth Weight Neonates: A Randomized, Double-blind, Placebo-controlled Pilot Trial. J. Trop. Pediatr. 2016, 63, 10–17. [Google Scholar] [CrossRef]
- Nasuf, A.W.A.; Ojha, S.; Dorling, J. Oropharyngeal colostrum in preventing mortality and morbidity in preterm infants. Cochrane Database Syst. Rev. 2018, 9, CD011921. [Google Scholar] [CrossRef]
- ELFIN Trial Investigators Group. Enteral lactoferrin supplementation for very preterm infants: A randomised placebo-controlled trial. Lancet 2019, 393, 423–433. [Google Scholar] [CrossRef]
- Tao, J.; Mao, J.; Yang, J.; Su, Y. Effects of oropharyngeal administration of colostrum on the incidence of necrotizing enterocolitis, late-onset sepsis, and death in preterm infants: A meta-analysis of RCTs. Eur. J. Clin. Nutr. 2020, 74, 1122–1131. [Google Scholar] [CrossRef]
- Sharma, D.; Kaur, A.; Farahbakhsh, N.; Agarwal, S. Role of Oropharyngeal Administration of Colostrum in Very Low Birth Weight Infants for Reducing Necrotizing Enterocolitis: A Randomized Controlled Trial. Am. J. Perinatol. 2019, 37, 716–721. [Google Scholar] [CrossRef]
- Sadeghirad, B.; Morgan, R.L.; Zeraatkar, D.; Zea, A.M.; Couban, R.; Johnston, B.C.; Florez, I.D. Human and Bovine Colostrum for Prevention of Necrotizing Enterocolitis: A Meta-analysis. Pediatrics 2018, 142, e20180767. [Google Scholar] [CrossRef]
- Zhang, Y.Z.; Li, Y.Y. Inflammatory bowel disease: Pathogenesis. World J. Gastroenterol. 2014, 20, 91–99. [Google Scholar] [CrossRef]
- Wehkamp, J.; Götz, M.; Herrlinger, K.; Steurer, W.; Stange, E.F. Inflammatory Bowel Disease. Dtsch. Aerzteblatt Online 2016, 113, 72–82. [Google Scholar] [CrossRef]
- Guan, Q. A Comprehensive Review and Update on the Pathogenesis of Inflammatory Bowel Disease. J. Immunol. Res. 2019, 2019, 7247238. [Google Scholar] [CrossRef]
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.; Lomer, M.C.E.; Parkes, G.C.; Selinger, C.; et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019, 68 (Suppl. 3), s1–s106. [Google Scholar] [CrossRef]
- Nadpara, N.; Reichenbach, Z.W.; Ehrlich, A.C.; Friedenberg, F. Current Status of Medical Therapy for Inflammatory Bowel Disease: The Wealth of Medications. Dig. Dis. Sci. 2020, 65, 2769–2779. [Google Scholar] [CrossRef]
- Seyedian, S.S.; Nokhostin, F.; Malamir, M.D. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J. Med. Life 2019, 12, 113–122. [Google Scholar] [CrossRef]
- Hartman, C.; Berkowitz, D.; Weiss, B.; Shaoul, R.; Levine, A.; Adiv, O.E.; Shapira, R.; Fradkin, A.; Wilschanski, M.; Tamir, A.; et al. Nutritional supplementation with polymeric diet enriched with transforming growth factor-beta 2 for children with Crohn’s disease. Isr. Med. Assoc. J. 2008, 10, 503–507. [Google Scholar]
- Rubio, A.; Pigneur, B.; Garnier-Lengliné, H.; Talbotec, C.; Schmitz, J.; Canioni, D.; Goulet, O.; Ruemmele, F.M. The efficacy of exclusive nutritional therapy in paediatric Crohn’s disease, comparing fractionated oral vs. continuous enteral feeding. Aliment. Pharmacol. Ther. 2011, 33, 1332–1339. [Google Scholar] [CrossRef]
- Liu, L.; Oza, S.; Hogan, D.; Chu, Y.; Perin, J.; Zhu, J.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016, 388, 3027–3035. [Google Scholar] [CrossRef]
- De Onis, M.; Branca, F. Childhood stunting: A global perspective. Matern. Child Nutr. 2016, 12 (Suppl. 1), 12–26. [Google Scholar] [CrossRef]
- Prendergast, A.; Kelly, P. Interactions between intestinal pathogens, enteropathy and malnutrition in developing countries. Curr. Opin. Infect. Dis. 2016, 29, 229–236. [Google Scholar] [CrossRef]
- Lamberti, L.M.; Fischer Walker, C.L.; Noiman, A.; Victora, C.; Black, R.E. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health 2011, 11 (Suppl. 3), S15. [Google Scholar] [CrossRef]
- Santos, F.S.; Santos, F.C.S.; Dos Santos, L.H.; Leite, A.M.; De Mello, D.F. Breastfeeding and protection against diarrhea: An integrative review of literature. Einstein (São Paulo) 2015, 13, 435–440. [Google Scholar] [CrossRef]
- Playford, R.J.; Choudhry, N.; Kelly, P.; Marchbank, T. Effects of Bovine Colostrum with or without Egg on In Vitro Bacterial-Induced Intestinal Damage with Relevance for SIBO and Infectious Diarrhea. Nutrients 2021, 13, 1024. [Google Scholar] [CrossRef]
- Ulfman, L.H.; Leusen, J.H.W.; Savelkoul, H.F.J.; Warner, J.O.; Van Neerven, R.J.J. Effects of Bovine Immunoglobulins on Immune Function, Allergy, and Infection. Front. Nutr. 2018, 5, 52. [Google Scholar] [CrossRef]
- Billiauws, L.; Corcos, O.; Joly, F. What’s new in short bowel syndrome? Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Shakhsheer, B.A.; Warner, B.W. Short Bowel Syndrome. Curr. Treat. Options Pediatr. 2019, 5, 494–505. [Google Scholar] [CrossRef]
- Massironi, S.; Cavalcoli, F.; Rausa, E.; Invernizzi, P.; Braga, M.; Vecchi, M. Understanding short bowel syndrome: Current status and future perspectives. Dig. Liver Dis. 2020, 52, 253–261. [Google Scholar] [CrossRef]
- Byrne, T.A.; Persinger, R.L.; Young, L.S.; Ziegler, T.R.; Wilmore, D.W. A New Treatment for Patients with Short-Bowel Syndrome Growth Hormone, Glutamine, and a Modified Diet. Ann. Surg. 1995, 222, 243–255. [Google Scholar] [CrossRef]
- Carter, B.A.; Cohran, V.C.; Cole, C.R.; Corkins, M.R.; Dimmitt, R.A.; Duggan, C.; Hill, S.; Horslen, S.; Lim, J.D.; Mercer, D.F.; et al. Outcomes from a 12-Week, Open-Label, Multicenter Clinical Trial of Teduglutide in Pediatric Short Bowel Syndrome. J. Pediatr. 2017, 181, 102–111.e5. [Google Scholar] [CrossRef] [PubMed]
- Neu, J.; Walker, W.A. Necrotizing Enterocolitis. N. Engl. J. Med. 2011, 364, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Meister, A.L.; Doheny, K.K.; Travagli, R.A. Necrotizing enterocolitis: It’s not all in the gut. Exp. Biol. Med. 2020, 245, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Howard, S.C.; Pillai, A.; Vogel, P.; Naren, A.P.; Davis, S.; Ringwald-Smith, K.; Buddington, K.; Buddington, R.K. The weaned pig as a model for Doxorubicin-induced mucositis. Chemotherapy 2014, 60, 24–36. [Google Scholar] [CrossRef]
- Rathe, M.; De Pietri, S.; Wehner, P.S.; Frandsen, T.L.; Grell, K.; Schmiegelow, K.; Sangild, P.T.; Husby, S.; Müller, K. Bovine Colostrum Against Chemotherapy-Induced Gastrointestinal Toxicity in Children With Acute Lymphoblastic Leukemia: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Parenter. Enter. Nutr. 2020, 44, 337–347. [Google Scholar] [CrossRef]
- Playford, R.J.; Marchbank, T. Oral zinc carnosine reduces multi-organ damage caused by gut ischemia/reperfusion in mice. J. Funct. Foods 2021, 78, 104361. [Google Scholar] [CrossRef]
- Davison, G.; Marchbank, T.; March, D.S.; Thatcher, R.; Playford, R.J. Zinc carnosine works with bovine colostrum in truncating heavy exercise–induced increase in gut permeability in healthy volunteers. Am. J. Clin. Nutr. 2016, 104, 526–536. [Google Scholar] [CrossRef]
- Fischer, A.J.; Malmuthuge, N.; Guan, L.L.; Steele, M.A. Short communication: The effect of heat treatment of bovine colostrum on the concentration of oligosaccharides in colostrum and in the intestine of neonatal male Holstein calves. J. Dairy Sci. 2018, 101, 401–407. [Google Scholar] [CrossRef]
- Bitzan, M.; Gold, B.D.; Philpott, D.J.; Huesca, M.; Sherman, P.M.; Karch, H.; Lissner, R.; Lingwood, C.A.; Karmali, M.A. Inhibition of Helicobacter pylori and Helicobacter mustelae binding to lipid receptors by bovine colostrum. J. Infect. Dis. 1998, 177, 955–961. [Google Scholar] [CrossRef]
| First Author | Country | Study Population | Year | Number of Participants (Human Studies Only) | Conclusion |
|---|---|---|---|---|---|
| NSAID-Induced Gut Injury | |||||
| Playford et al. [37] | UK | Animal (Mice) | 1999 | Colostrum preparation has major beneficial effects in preventing NSAID-induced gut injury | |
| Kim et al. [38] | Korea | Animal (rats) | 2005 | BC ameliorated NSAID-induced intestinal damage and bacterial translocation, especially when combined with glutamine | |
| Cairangzhuoma et al. [39] | Japan | Animal (mice) | 2013 | Late BC aids in recovery and inhibition of NSAID-induced small intestinal injury in mouse model | |
| Playford et al. [40] | UK | RCT (cross over) | 2001 | Acute effect, 7; long-term, 22 | Compared to indomethacin alone, BC reduced the impact of indomethacin on gut permeability only in the short term |
| Inflammatory Bowel Disease | |||||
| Kanwar et al. [41] | New Zealand | Animal (mice) | 2016 | Bovine milk components attenuated the severity of DSS-induced colitis in mice with differing effectiveness against specific disease parameters | |
| Filipescu et al. [42] | Italy | Animal (mice) | 2018 | Pre-treatment of mice with BC reduces TNBS-induced intestinal damage | |
| Spalinger et al. [43] | Switzerland | Animal (mice) | 2019 | Hyperimmune BC reduces intestinal inflammation by increasing Treg cell induction while decreasing accumulation of pathogenic T cells | |
| Playford et al. [44] | UK | Animal (mice) | 2020 | Combination of BC and egg synergistically reduced indomethacin and DSS-induced gut damage | |
| Menchetti et al. [45] | Italy | Animal (mice) | 2020 | Pre-treatment with BC modulates the expression of genes and the count of microbes involved in the etiopathogenesis of colitis | |
| Khan et al. [46] | UK | RCT | 2002 | 14 | Mesalazine and BC enema improved symptoms in patients with left sided colitis compared to mesalazine with placebo |
| Infectious Diarrhea | |||||
| Choudhry et al. [47] | UK | Cell culture model of microbial translocation | 2020 | BC reduced enteropathogen-mediated damage in Caco-2 cells | |
| Li et al. [48] | China | Meta-analysis | 2019 | BC products were effective in controlling clinical symptoms and pathogenic agents in children with infectious diarrhea | |
| Barakat et al. [49] | Egypt | RCT | 2020 | 160 | BC is effective in the treatment of acute diarrhea and can be considered as adjuvant therapy in both viral and bacterial diarrhea to prevent diarrhea-related complications |
| Gaensbauer et al. [50] | Guatemala | RCT | 2017 | 301 | A BC and hen’s egg derived feed reduced acute non-bloody diarrheal duration in children in a subgroup with an identified pathogen; the primary outcome was not met |
| Saad et al. [51] | Open multicentric, noncomparative | 2016 | 160 | BC was effective in reducing the number of episodes of URTI and diarrhea in children | |
| Otto et al. [52] | Poland | RCT | 2011 | 90 | Hyperimmune BC is effective in protecting adult volunteers against diarrhea caused by ETEC |
| Kaducu et al. [53] | Uganda | RCT | 2011 | 87 | Addition of BC-based supplement is effective in treatment of HIV-associated diarrhea in adults |
| Eslamian et al. [54] | RCT | 2019 | 70 | BC supplementation may have beneficial effects on intestinal permeability and gastrointestinal complications in ICU-hospitalized patients | |
| Bierut et al. [55] | Malawi | RCT | 2021 | 267 | Addition of BC and egg to complementary feeding in Malawian infants resulted in less linear growth faltering. Episodes of diarrhea and β-diversity of the 16S configuration of fecal microbiota did not differ between the treatment group and controls |
| Short Bowel Syndrome | |||||
| Paris et al. [56] | Australia | Animal (piglets) | 2004 | A polymeric infant formula supplemented with BC given to pig model of SBS was associated with significant increase in plasma GLP-2, suggesting the role of GLP-2 in intestinal adaptation post resection | |
| Nagy et al. [57] | Animal (piglets) | 2004 | In pig model of SBS, supplementation with colostrum protein concentrate resulted in normal weight gain and features of enhanced morphologic adaptation | ||
| Pereira-Fantini et al. [58] | Australia | Animal (piglets) | 2008 | Following bowel resection, colostrum protein concentrate significantly increased circulating levels of IGF-1 and IGFBPs | |
| Aunsholt et al. [59] | Denmark | Animal (piglets) | 2018 | Parenteral nutrition (PN) with minimal enteral nutrition with BC or formula induced similar intestinal adaption after resection | |
| Aunsholt et al. [60] | Denmark | RCT (crossover) | 2012 | 9 | Inclusion of bovine colostrum to the diet did not improve intestinal function |
| Lund et al. [61] | Denmark | RCT | 2012 | 12 | BC did not significantly improve intestinal absorption, body composition, or functional tests compared with the control |
| Necrotizing Enterocolitis | |||||
| Jensen et al. [62] | Denmark | Animal (piglets) | 2013 | BC and human milk are both superior to formula in stimulating gut structure, function, and NEC resistance in preterm piglets | |
| Li et al. [63] | Denmark | Animal (piglets) | 2014 | The maturational and protective effects on the immature intestine decreased in the order BC > mature bovine milk >whole milk powder, but all three were markedly better than formula | |
| Støy et al. [64] | Animal (piglets) | 2014 | Bovine colostrum restores intestinal function after initial formula-induced inflammation in preterm pigs | ||
| Seigel et al. [65] | USA | Retrospective cohort | 2013 | 369 | Initiating oropharyngeal COL in ELBW infants in the first 2 postnatal days appears feasible and safe and may be nutritionally beneficial |
| Balachandran et al. [66] | India | RCT | 2017 | 86 | The use of prophylactic enteral BC in VLBW infants showed a trend toward increased stool IL-6 and features of NEC; there were no clinical benefits |
| Nasuf et al. [67] | Systematic review | 2018 | Limited available evidence currently suggests that oropharyngeal administration of mother’s colostrum starting within the first 48 h of life does not reduce the risk of NEC, late-onset infection, or death until discharge in preterm infants, including very preterm, VLBW infants | ||
| ELFIN trial investigators group [68] | RCT | 2019 | 2203 | Enteral supplementation with bovine lactoferrin (derived from milk) did not reduce the risk of late-onset infection in very preterm infants | |
| Tao et al. [69] | Meta-analysis of RCTs | 2020 | BC does not reduce the incidences of NEC, late onset sepsis, and death in preterm infants, but there is a trend toward a positive effect | ||
| Sharma et al. [70] | India | RCT | 2020 | 117 | There was no significant reduction in the incidence of NEC in the BC group but there was significant reduction of 7 days of hospital stay in the BC group |
| Sadeghirad et al. [71] | Meta-analysis | 2018 | Bovine or human colostrum has no effect on severe NEC, mortality, culture-proven sepsis, feed intolerance, or length of stay | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chandwe, K.; Kelly, P. Colostrum Therapy for Human Gastrointestinal Health and Disease. Nutrients 2021, 13, 1956. https://doi.org/10.3390/nu13061956
Chandwe K, Kelly P. Colostrum Therapy for Human Gastrointestinal Health and Disease. Nutrients. 2021; 13(6):1956. https://doi.org/10.3390/nu13061956
Chicago/Turabian StyleChandwe, Kanta, and Paul Kelly. 2021. "Colostrum Therapy for Human Gastrointestinal Health and Disease" Nutrients 13, no. 6: 1956. https://doi.org/10.3390/nu13061956
APA StyleChandwe, K., & Kelly, P. (2021). Colostrum Therapy for Human Gastrointestinal Health and Disease. Nutrients, 13(6), 1956. https://doi.org/10.3390/nu13061956






