Nutrition in Menopausal Women: A Narrative Review
Abstract
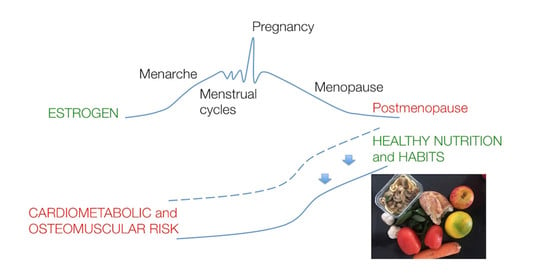
:1. Introduction
2. Dietary Intake and Clinical Endpoints in Menopausal Women
2.1. Body Composition
2.1.1. Dietary Intake and Lean Body Mass in Postmenopausal Women
Dietary Protein
Mediterranean Dietary Pattern
2.1.2. Dietary Intake and Fat Mass in Postmenopausal Women
Dietary Carbohydrate, Whole Grains, and Glycemic Index
Mediterranean Dietary Pattern
2.2. Bone Health
2.3. Cardiovascular Risk
3. Summary and Research Perspectives
- Menopausal transition has been associated with loss of BMD, LBM and increase of FM;
- RDA for protein intake may be sufficient to maintain LBM; Mediterranean diet components could be linked with better LBM;
- Low-carbohydrate-high-fat diet should not be recommended in order to reduce FM;
- In overweight or obese women, low GI diet could lead to greater decrease in FM than control diets;
- Future studies evaluating the effects of low-fat, plant-based diets on FM in postmenopausal women are needed;
- Mediterranean diet might significantly reduce the rate of BMD loss in women with osteoporosis;
- Calcium, vitamin D, vitamin K, selenium, magnesium, and beta-carotene adequate intake could be linked with better BMD in postmenopausal women;
- Diet is a major modifiable risk factor for CVD and could be a powerful intervention to reduce cardiovascular risks in postmenopausal women;
- Low-energy diet is recommended for postmenopausal women to prevent metabolic disturbance;
- Low-fat diets may lead to greater improvement in LDL cholesterol levels, whereas low-carbohydrate diets may result in greater improvement in triglyceride and HDL cholesterol levels;
- Mediterranean diet is associated with a small but significant decrease in blood pressure and reduced CVD risk of among different female cohorts, although more evidence is required for these outcomes in postmenopausal women.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davis, S.R.; Lambrinoudaki, I.; Lumsden, M.; Mishra, G.D.; Pal, L.; Rees, M.; Santoro, N.; Simoncini, T. Menopause. Nat. Rev. Dis. Primers 2015, 1, 15004. [Google Scholar] [CrossRef] [PubMed]
- El Khoudary, S.R.; Aggarwal, B.; Beckie, T.M.; Hodis, H.N.; Johnson, A.E.; Langer, R.D.; Limacher, M.C.; Manson, J.E.; Stefanick, M.L.; Allison, M.A. Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association. Circulation 2020, 142, e506–e532. [Google Scholar] [CrossRef] [PubMed]
- Nappi, R.E.; Simoncini, T. Menopause transition: A golden age to prevent cardiovascular disease. Lancet Diabetes Endocrinol. 2021, 9, 135–137. [Google Scholar] [CrossRef]
- Biglia, N.; Cagnacci, A.; Gambacciani, M.; Lello, S.; Maffei, S.; Nappi, R.E. Vasomotor symptoms in menopause: A biomarker of cardiovascular disease risk and other chronic diseases? Climacteric J. Int. Menopause Soc. 2017, 20, 306–312. [Google Scholar] [CrossRef]
- Harlow, S.D.; Gass, M.; Hall, J.E.; Lobo, R.; Maki, P.; Rebar, R.W.; Sherman, S.; Sluss, P.M.; de Villiers, T.J. Executive summary of the Stages of Reproductive Aging Workshop + 10: Addressing the unfinished agenda of staging reproductive aging. Menopause 2012, 19, 387–395. [Google Scholar] [CrossRef] [Green Version]
- Davis, S.R.; Castelo-Branco, C.; Chedraui, P.; Lumsden, M.A.; Nappi, R.E.; Shah, D.; Villaseca, P. Understanding weight gain at menopause. Climacteric J. Int. Menopause Soc. 2012, 15, 419–429. [Google Scholar] [CrossRef]
- Greendale, G.A.; Sternfeld, B.; Huang, M.; Han, W.; Karvonen-Gutierrez, C.; Ruppert, K.; Cauley, J.A.; Finkelstein, J.S.; Jiang, S.F.; Karlamangla, A.S. Changes in body composition and weight during the menopause transition. JCI Insight 2019, 4. [Google Scholar] [CrossRef]
- Colpani, V.; Oppermann, K.; Spritzer, P.M. Association between habitual physical activity and lower cardiovascular risk in premenopausal, perimenopausal, and postmenopausal women: A population-based study. Menopause 2013, 20, 525–531. [Google Scholar] [CrossRef]
- Cheng, C.C.; Hsu, C.Y.; Liu, J.F. Effects of dietary and exercise intervention on weight loss and body composition in obese postmenopausal women: A systematic review and meta-analysis. Menopause 2018, 25, 772–782. [Google Scholar] [CrossRef]
- Kelley, D.E.; Mandarino, L.J. Fuel selection in human skeletal muscle in insulin resistance: A reexamination. Diabetes 2000, 49, 677–683. [Google Scholar] [CrossRef] [Green Version]
- Irwin, R.W.; Yao, J.; Hamilton, R.T.; Cadenas, E.; Brinton, R.D.; Nilsen, J. Progesterone and estrogen regulate oxidative metabolism in brain mitochondria. Endocrinology 2008, 149, 3167–3175. [Google Scholar] [CrossRef] [Green Version]
- Eaton, S.A.; Sethi, J.K. Immunometabolic Links between Estrogen, Adipose Tissue and Female Reproductive Metabolism. Biology 2019, 8, 8. [Google Scholar] [CrossRef] [Green Version]
- Donato, G.B.; Fuchs, S.C.; Oppermann, K.; Bastos, C.; Spritzer, P.M. Association between menopause status and central adiposity measured at different cutoffs of waist circumference and waist-to-hip ratio. Menopause 2006, 13, 280–285. [Google Scholar] [CrossRef]
- Rolland, Y.M.; Perry, H.M., 3rd; Patrick, P.; Banks, W.A.; Morley, J.E. Loss of appendicular muscle mass and loss of muscle strength in young postmenopausal women. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2007, 62, 330–335. [Google Scholar] [CrossRef] [Green Version]
- Srikanthan, P.; Horwich, T.B.; Tseng, C.H. Relation of Muscle Mass and Fat Mass to Cardiovascular Disease Mortality. Am. J. Cardiol. 2016, 117, 1355–1360. [Google Scholar] [CrossRef]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the PROT-AGE Study Group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; Baerlocher, K.; Bauer, J.M.; Elmadfa, I.; Heseker, H.; Leschik-Bonnet, E.; Stangl, G.; Volkert, D.; Stehle, P. Revised Reference Values for the Intake of Protein. Ann. Nutr. Metab. 2019, 74, 242–250. [Google Scholar] [CrossRef]
- Francaux, M.; Demeulder, B.; Naslain, D.; Fortin, R.; Lutz, O.; Caty, G.; Deldicque, L. Aging Reduces the Activation of the mTORC1 Pathway after Resistance Exercise and Protein Intake in Human Skeletal Muscle: Potential Role of REDD1 and Impaired Anabolic Sensitivity. Nutrients 2016, 8, 47. [Google Scholar] [CrossRef] [Green Version]
- Markofski, M.M.; Dickinson, J.M.; Drummond, M.J.; Fry, C.S.; Fujita, S.; Gundermann, D.M.; Glynn, E.L.; Jennings, K.; Paddon-Jones, D.; Reidy, P.T.; et al. Effect of age on basal muscle protein synthesis and mTORC1 signaling in a large cohort of young and older men and women. Exp. Gerontol. 2015, 65, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Isanejad, M.; Mursu, J.; Sirola, J.; Kröger, H.; Rikkonen, T.; Tuppurainen, M.; Erkkilä, A.T. Dietary protein intake is associated with better physical function and muscle strength among elderly women. Br. J. Nutr. 2016, 115, 1281–1291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, X.; Zhu, K.; Devine, A.; Kerr, D.A.; Binns, C.W.; Prince, R.L. A 5-year cohort study of the effects of high protein intake on lean mass and BMC in elderly postmenopausal women. J. Bone Miner. Res. 2009, 24, 1827–1834. [Google Scholar] [CrossRef]
- Silva, T.R.; Spritzer, P.M. Skeletal muscle mass is associated with higher dietary protein intake and lower body fat in postmenopausal women: A cross-sectional study. Menopause 2017, 24, 502–509. [Google Scholar] [CrossRef]
- Beasley, J.M.; LaCroix, A.Z.; Neuhouser, M.L.; Huang, Y.; Tinker, L.; Woods, N.; Michael, Y.; Curb, J.D.; Prentice, R.L. Protein intake and incident frailty in the Women’s Health Initiative observational study. J. Am. Geriatr. Soc. 2010, 58, 1063–1071. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trumbo, P.; Schlicker, S.; Yates, A.A.; Poos, M. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J. Am. Diet. Assoc. 2002, 102, 1621–1630. [Google Scholar] [CrossRef]
- Ten Haaf, D.S.M.; Nuijten, M.A.H.; Maessen, M.F.H.; Horstman, A.M.H.; Eijsvogels, T.M.H.; Hopman, M.T.E. Effects of protein supplementation on lean body mass, muscle strength, and physical performance in nonfrail community-dwelling older adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2018, 108, 1043–1059. [Google Scholar] [CrossRef] [Green Version]
- Iglay, H.B.; Apolzan, J.W.; Gerrard, D.E.; Eash, J.K.; Anderson, J.C.; Campbell, W.W. Moderately increased protein intake predominately from egg sources does not influence whole body, regional, or muscle composition responses to resistance training in older people. J. Nutr. Health Aging 2009, 13, 108–114. [Google Scholar] [CrossRef]
- Rossato, L.T.; Nahas, P.C.; de Branco, F.M.S.; Martins, F.M.; Souza, A.P.; Carneiro, M.A.S.; Orsatti, F.L.; de Oliveira, E.P. Higher Protein Intake Does Not Improve Lean Mass Gain When Compared with RDA Recommendation in Postmenopausal Women Following Resistance Exercise Protocol: A Randomized Clinical Trial. Nutrients 2017, 9, 1007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balagopal, P.; Rooyackers, O.E.; Adey, D.B.; Ades, P.A.; Nair, K.S. Effects of aging on in vivo synthesis of skeletal muscle myosin heavy-chain and sarcoplasmic protein in humans. Am. J. Physiol. 1997, 273, E790–E800. [Google Scholar] [CrossRef] [PubMed]
- Baumann, C.W.; Kwak, D.; Liu, H.M.; Thompson, L.V. Age-induced oxidative stress: How does it influence skeletal muscle quantity and quality? J. Appl. Physiol. 2016, 121, 1047–1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cruz-Jentoft, A.J.; Romero-Yuste, S.; Chamizo Carmona, E.; Nolla, J.M. Sarcopenia, immune-mediated rheumatic diseases, and nutritional interventions. Aging Clin. Exp. Res. 2021. [Google Scholar] [CrossRef]
- Daussin, F.N.; Boulanger, E.; Lancel, S. From mitochondria to sarcopenia: Role of inflammaging and RAGE-ligand axis implication. Exp. Gerontol. 2021, 146, 111247. [Google Scholar] [CrossRef]
- Isanejad, M.; Sirola, J.; Mursu, J.; Rikkonen, T.; Kröger, H.; Tuppurainen, M.; Erkkilä, A.T. Association of the Baltic Sea and Mediterranean diets with indices of sarcopenia in elderly women, OSPTRE-FPS study. Eur. J. Nutr. 2018, 57, 1435–1448. [Google Scholar] [CrossRef] [PubMed]
- Kelaiditi, E.; Jennings, A.; Steves, C.J.; Skinner, J.; Cassidy, A.; MacGregor, A.J.; Welch, A.A. Measurements of skeletal muscle mass and power are positively related to a Mediterranean dietary pattern in women. Osteoporos. Int. 2016, 27, 3251–3260. [Google Scholar] [CrossRef] [PubMed]
- Silva, T.R.D.; Martins, C.C.; Ferreira, L.L.; Spritzer, P.M. Mediterranean diet is associated with bone mineral density and muscle mass in postmenopausal women. Climacteric J. Int. Menopause Soc. 2019, 22, 162–168. [Google Scholar] [CrossRef]
- Granic, A.; Sayer, A.A.; Robinson, S.M. Dietary Patterns, Skeletal Muscle Health, and Sarcopenia in Older Adults. Nutrients 2019, 11, 745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashimoto, Y.; Fukuda, T.; Oyabu, C.; Tanaka, M.; Asano, M.; Yamazaki, M.; Fukui, M. Impact of low-carbohydrate diet on body composition: Meta-analysis of randomized controlled studies. Obes. Rev. 2016, 17, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Valsdottir, T.D.; Øvrebø, B.; Falck, T.M.; Litleskare, S.; Johansen, E.I.; Henriksen, C.; Jensen, J. Low-Carbohydrate High-Fat Diet and Exercise: Effect of a 10-Week Intervention on Body Composition and CVD Risk Factors in Overweight and Obese Women-A Randomized Controlled Trial. Nutrients 2020, 13, 110. [Google Scholar] [CrossRef] [PubMed]
- Augustin, L.S.; Kendall, C.W.; Jenkins, D.J.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Björck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. Dis. NMCD 2015, 25, 795–815. [Google Scholar] [CrossRef] [Green Version]
- Karl, J.P.; Meydani, M.; Barnett, J.B.; Vanegas, S.M.; Goldin, B.; Kane, A.; Rasmussen, H.; Saltzman, E.; Vangay, P.; Knights, D.; et al. Substituting whole grains for refined grains in a 6-wk randomized trial favorably affects energy-balance metrics in healthy men and postmenopausal women. Am. J. Clin. Nutr. 2017, 105, 589–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pol, K.; Christensen, R.; Bartels, E.M.; Raben, A.; Tetens, I.; Kristensen, M. Whole grain and body weight changes in apparently healthy adults: A systematic review and meta-analysis of randomized controlled studies. Am. J. Clin. Nutr. 2013, 98, 872–884. [Google Scholar] [CrossRef] [Green Version]
- Ludwig, D.S. Dietary glycemic index and obesity. J. Nutr. 2000, 130, 280s–283s. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.E.; Elliott, E.J.; Baur, L. Low glycaemic index or low glycaemic load diets for overweight and obesity. Cochrane Database Syst. Rev. 2007, Cd005105. [Google Scholar] [CrossRef]
- Silva, T.R.; Lago, S.C.; Yavorivski, A.; Ferreira, L.L.; Fighera, T.M.; Spritzer, P.M. Effects of high protein, low-glycemic index diet on lean body mass, strength, and physical performance in late postmenopausal women: A randomized controlled trial. Menopause 2020, 28, 307–317. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Flor-Alemany, M.; Marín-Jiménez, N.; Nestares, T.; Borges-Cosic, M.; Aranda, P.; Aparicio, V.A. Mediterranean diet, tobacco consumption and body composition during perimenopause. The FLAMENCO project. Maturitas 2020, 137, 30–36. [Google Scholar] [CrossRef]
- Lombardo, M.; Perrone, M.A.; Guseva, E.; Aulisa, G.; Padua, E.; Bellia, C.; Della-Morte, D.; Iellamo, F.; Caprio, M.; Bellia, A. Losing Weight after Menopause with Minimal Aerobic Training and Mediterranean Diet. Nutrients 2020, 12, 2471. [Google Scholar] [CrossRef]
- Carty, C.L.; Kooperberg, C.; Neuhouser, M.L.; Tinker, L.; Howard, B.; Wactawski-Wende, J.; Beresford, S.A.; Snetselaar, L.; Vitolins, M.; Allison, M.; et al. Low-fat dietary pattern and change in body-composition traits in the Women’s Health Initiative Dietary Modification Trial. Am. J. Clin. Nutr. 2011, 93, 516–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hooper, L.; Abdelhamid, A.S.; Jimoh, O.F.; Bunn, D.; Skeaff, C.M. Effects of total fat intake on body fatness in adults. Cochrane Database Syst. Rev. 2020, 6, Cd013636. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Guo, J.; Courville, A.B.; Boring, J.; Brychta, R.; Chen, K.Y.; Darcey, V.; Forde, C.G.; Gharib, A.M.; Gallagher, I.; et al. Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat. Med. 2021, 27, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Silva, T.R.; Franz, R.; Maturana, M.A.; Spritzer, P.M. Associations between body composition and lifestyle factors with bone mineral density according to time since menopause in women from Southern Brazil: A cross-sectional study. BMC Endocr. Disord. 2015, 15, 71. [Google Scholar] [CrossRef] [Green Version]
- Sowers, M.R.; Jannausch, M.; McConnell, D.; Little, R.; Greendale, G.A.; Finkelstein, J.S.; Neer, R.M.; Johnston, J.; Ettinger, B. Hormone predictors of bone mineral density changes during the menopausal transition. J. Clin. Endocrinol. Metab. 2006, 91, 1261–1267. [Google Scholar] [CrossRef] [Green Version]
- Finkelstein, J.S.; Brockwell, S.E.; Mehta, V.; Greendale, G.A.; Sowers, M.R.; Ettinger, B.; Lo, J.C.; Johnston, J.M.; Cauley, J.A.; Danielson, M.E.; et al. Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J. Clin. Endocrinol. Metab. 2008, 93, 861–868. [Google Scholar] [CrossRef]
- Bischoff-Ferrari, H.A.; Dawson-Hughes, B.; Baron, J.A.; Burckhardt, P.; Li, R.; Spiegelman, D.; Specker, B.; Orav, J.E.; Wong, J.B.; Staehelin, H.B.; et al. Calcium intake and hip fracture risk in men and women: A meta-analysis of prospective cohort studies and randomized controlled trials. Am. J. Clin. Nutr. 2007, 86, 1780–1790. [Google Scholar] [CrossRef]
- Salmon, J. Excerpts from Dietary Reference Values for Food Energy and Nutrients for the United Kingdom: Introduction to the Guide and Summary Tables. Nutr. Rev. 1992, 50, 90–93. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. The National Academies Collection: Reports funded by National Institutes of Health. In Dietary Reference Intakes for Calcium and Vitamin D; National Academies Press (US) Copyright©, 2021; Ross, A.C., Taylor, C.L., Yaktine, A.L., Del Valle, H.B., Eds.; National Academy of Sciences: Washington, DC, USA, 2011. [Google Scholar]
- Society, N.A.M. The role of calcium in peri- and postmenopausal women: 2006 position statement of the North American Menopause Society. Menopause 2006, 13, 862–877; quiz 878–880. [Google Scholar] [CrossRef]
- Yao, P.; Bennett, D.; Mafham, M.; Lin, X.; Chen, Z.; Armitage, J.; Clarke, R. Vitamin D and Calcium for the Prevention of Fracture: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e1917789. [Google Scholar] [CrossRef]
- Chen, G.D.; Dong, X.W.; Zhu, Y.Y.; Tian, H.Y.; He, J.; Chen, Y.M. Adherence to the Mediterranean diet is associated with a higher BMD in middle-aged and elderly Chinese. Sci. Rep. 2016, 6, 25662. [Google Scholar] [CrossRef] [Green Version]
- Erkkilä, A.T.; Sadeghi, H.; Isanejad, M.; Mursu, J.; Tuppurainen, M.; Kröger, H. Associations of Baltic Sea and Mediterranean dietary patterns with bone mineral density in elderly women. Public Health Nutr. 2017, 20, 2735–2743. [Google Scholar] [CrossRef] [Green Version]
- Jennings, A.; Cashman, K.D.; Gillings, R.; Cassidy, A.; Tang, J.; Fraser, W.; Dowling, K.G.; Hull, G.L.J.; Berendsen, A.A.M.; de Groot, L.; et al. A Mediterranean-like dietary pattern with vitamin D3 (10 µg/d) supplements reduced the rate of bone loss in older Europeans with osteoporosis at baseline: Results of a 1-y randomized controlled trial. Am. J. Clin. Nutr. 2018, 108, 633–640. [Google Scholar] [CrossRef]
- Regu, G.M.; Kim, H.; Kim, Y.J.; Paek, J.E.; Lee, G.; Chang, N.; Kwon, O. Association between Dietary Carotenoid Intake and Bone Mineral Density in Korean Adults Aged 30–75 Years Using Data from the Fourth and Fifth Korean National Health and Nutrition Examination Surveys (2008–2011). Nutrients 2017, 9, 1025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.; Wang, N.; Gao, Y.; Zhou, Z.; Liu, W.; Pan, C.; Yin, P.; Yu, X.; Tang, M. β-Carotene suppresses osteoclastogenesis and bone resorption by suppressing NF-κB signaling pathway. Life Sci. 2017, 174, 15–20. [Google Scholar] [CrossRef]
- Atkins, G.J.; Welldon, K.J.; Wijenayaka, A.R.; Bonewald, L.F.; Findlay, D.M. Vitamin K promotes mineralization, osteoblast-to-osteocyte transition, and an anticatabolic phenotype by {gamma}-carboxylation-dependent and -independent mechanisms. Am. J. Physiol. Cell Physiol. 2009, 297, C1358–C1367. [Google Scholar] [CrossRef] [Green Version]
- Avenell, A.; Grey, A.; Gamble, G.D.; Bolland, M.J. Concerns About the Integrity of the Yamaguchi Osteoporosis Prevention Study (YOPS) Report, Am J Med. 2004;117:549-555. Am. J. Med. 2020, 133, e311–e314. [Google Scholar] [CrossRef] [PubMed]
- Rønn, S.H.; Harsløf, T.; Oei, L.; Pedersen, S.B.; Langdahl, B.L. The effect of vitamin MK-7 on bone mineral density and microarchitecture in postmenopausal women with osteopenia, a 3-year randomized, placebo-controlled clinical trial. Osteoporos. Int. 2021, 32, 185–191. [Google Scholar] [CrossRef]
- Zeng, L.F.; Luo, M.H.; Liang, G.H.; Yang, W.Y.; Xiao, X.; Wei, X.; Yu, J.; Guo, D.; Chen, H.Y.; Pan, J.K.; et al. Can Dietary Intake of Vitamin C-Oriented Foods Reduce the Risk of Osteoporosis, Fracture, and BMD Loss? Systematic Review With Meta-Analyses of Recent Studies. Front. Endocrinol. 2019, 10, 844. [Google Scholar] [CrossRef] [Green Version]
- Qu, Z.; Yang, F.; Yan, Y.; Hong, J.; Wang, W.; Li, S.; Jiang, G.; Yan, S. Relationship between Serum Nutritional Factors and Bone Mineral Density: A Mendelian Randomization Study. J. Clin. Endocrinol. Metab. 2021, 106, e2434–e2443. [Google Scholar] [CrossRef]
- Wu, F.; Wills, K.; Laslett, L.L.; Oldenburg, B.; Jones, G.; Winzenberg, T. Associations of dietary patterns with bone mass, muscle strength and balance in a cohort of Australian middle-aged women. Br. J. Nutr. 2017, 118, 598–606. [Google Scholar] [CrossRef] [Green Version]
- Maas, A.; Rosano, G.; Cifkova, R.; Chieffo, A.; van Dijken, D.; Hamoda, H.; Kunadian, V.; Laan, E.; Lambrinoudaki, I.; Maclaran, K.; et al. Cardiovascular health after menopause transition, pregnancy disorders, and other gynaecologic conditions: A consensus document from European cardiologists, gynaecologists, and endocrinologists. Eur. Heart J. 2021, 42, 967–984. [Google Scholar] [CrossRef]
- O’Keeffe, L.M.; Kuh, D.; Fraser, A.; Howe, L.D.; Lawlor, D.; Hardy, R. Age at period cessation and trajectories of cardiovascular risk factors across mid and later life. Heart 2020, 106, 499–505. [Google Scholar] [CrossRef] [Green Version]
- Oppermann, K.; Colpani, V.; Spritzer, P.M. Risk factors associated with coronary artery calcification in midlife women: A population-based study. Gynecol. Endocrinol. 2019, 35, 904–908. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Allison, M.A.; Rossouw, J.E.; Carr, J.J.; Langer, R.D.; Hsia, J.; Kuller, L.H.; Cochrane, B.B.; Hunt, J.R.; Ludlam, S.E.; et al. Estrogen therapy and coronary-artery calcification. N. Engl. J. Med. 2007, 356, 2591–2602. [Google Scholar] [CrossRef]
- Hallajzadeh, J.; Khoramdad, M.; Izadi, N.; Karamzad, N.; Almasi-Hashiani, A.; Ayubi, E.; Qorbani, M.; Pakzad, R.; Hasanzadeh, A.; Sullman, M.J.M.; et al. Metabolic syndrome and its components in premenopausal and postmenopausal women: A comprehensive systematic review and meta-analysis on observational studies. Menopause 2018, 25, 1155–1164. [Google Scholar] [CrossRef]
- Choi, Y.; Chang, Y.; Kim, B.K.; Kang, D.; Kwon, M.J.; Kim, C.W.; Jeong, C.; Ahn, Y.; Park, H.Y.; Ryu, S.; et al. Menopausal stages and serum lipid and lipoprotein abnormalities in middle-aged women. Maturitas 2015, 80, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Franz, R.; Maturana, M.A.; Magalhães, J.A.; Moraes, R.S.; Spritzer, P.M. Central adiposity and decreased heart rate variability in postmenopause: A cross-sectional study. Climacteric J. Int. Menopause Soc. 2013, 16, 576–583. [Google Scholar] [CrossRef]
- Ji, H.; Kim, A.; Ebinger, J.E.; Niiranen, T.J.; Claggett, B.L.; Bairey Merz, C.N.; Cheng, S. Sex Differences in Blood Pressure Trajectories Over the Life Course. JAMA Cardiol. 2020, 5, 19–26. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef]
- Mosca, L.; Benjamin, E.J.; Berra, K.; Bezanson, J.L.; Dolor, R.J.; Lloyd-Jones, D.M.; Newby, L.K.; Piña, I.L.; Roger, V.L.; Shaw, L.J.; et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: A guideline from the American Heart Association. J. Am. Coll. Cardiol. 2011, 57, 1404–1423. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.D.; Li, Y.; Bhupathiraju, S.N.; Rosner, B.A.; Sun, Q.; Giovannucci, E.L.; Rimm, E.B.; Manson, J.E.; Willett, W.C.; Stampfer, M.J.; et al. Fruit and Vegetable Intake and Mortality: Results From 2 Prospective Cohort Studies of US Men and Women and a Meta-Analysis of 26 Cohort Studies. Circulation 2021, 143, 1642–1654. [Google Scholar] [CrossRef]
- Wang, D.; Karvonen-Gutierrez, C.A.; Jackson, E.A.; Elliott, M.R.; Appelhans, B.M.; Barinas-Mitchell, E.; Bielak, L.F.; Huang, M.H.; Baylin, A. Western Dietary Pattern Derived by Multiple Statistical Methods Is Prospectively Associated with Subclinical Carotid Atherosclerosis in Midlife Women. J. Nutr. 2020, 150, 579–591. [Google Scholar] [CrossRef]
- Ko, S.H.; Kim, H.S. Menopause-Associated Lipid Metabolic Disorders and Foods Beneficial for Postmenopausal Women. Nutrients 2020, 12, 202. [Google Scholar] [CrossRef] [Green Version]
- Cho, Y.A.; Kim, J.; Cho, E.R.; Shin, A. Dietary patterns and the prevalence of metabolic syndrome in Korean women. Nutr. Metab. Cardiovasc. Dis. NMCD 2011, 21, 893–900. [Google Scholar] [CrossRef]
- Lovejoy, J.C.; Champagne, C.M.; de Jonge, L.; Xie, H.; Smith, S.R. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int. J. Obes. 2008, 32, 949–958. [Google Scholar] [CrossRef] [Green Version]
- Silva, T.R.; Alves, B.C.; Maturana, M.A.; Spritzer, P.M. Healthier dietary pattern and lower risk of metabolic syndrome in physically active postmenopausal women. J. Am. Coll. Nutr. 2013, 32, 287–295. [Google Scholar] [CrossRef]
- Kapoor, E.; Collazo-Clavell, M.L.; Faubion, S.S. Weight Gain in Women at Midlife: A Concise Review of the Pathophysiology and Strategies for Management. Mayo Clin. Proc. 2017, 92, 1552–1558. [Google Scholar] [CrossRef] [PubMed]
- Alves, B.C.; Silva, T.R.; Spritzer, P.M. Sedentary Lifestyle and High-Carbohydrate Intake are Associated with Low-Grade Chronic Inflammation in Post-Menopause: A Cross-sectional Study. Rev. Bras. Ginecol. Obstet. 2016, 38, 317–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 2014, 63, 2985–3023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mancini, J.G.; Filion, K.B.; Atallah, R.; Eisenberg, M.J. Systematic Review of the Mediterranean Diet for Long-Term Weight Loss. Am. J. Med. 2016, 129, 407–415.e404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thom, G.; Lean, M. Is There an Optimal Diet for Weight Management and Metabolic Health? Gastroenterology 2017, 152, 1739–1751. [Google Scholar] [CrossRef] [Green Version]
- Pugliese, G.D.; Barrea, L.D.; Laudisio, D.D.; Aprano, S.D.; Castellucci, B.D.; Framondi, L.D.; Di Matteo, R.D.; Savastano, S.P.; Colao, A.P.; Muscogiuri, G.D. Mediterranean diet as tool to manage obesity in menopause: A narrative review. Nutrients 2020, 79–80, 110991. [Google Scholar] [CrossRef]
- Cano, A.; Marshall, S.; Zolfaroli, I.; Bitzer, J.; Ceausu, I.; Chedraui, P.; Durmusoglu, F.; Erkkola, R.; Goulis, D.G.; Hirschberg, A.L.; et al. The Mediterranean diet and menopausal health: An EMAS position statement. Maturitas 2020, 139, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.L.; Silva, T.R.; Maturana, M.A.; Spritzer, P.M. Dietary intake of isoflavones is associated with a lower prevalence of subclinical cardiovascular disease in postmenopausal women: Cross-sectional study. J. Hum. Nutr. Diet. 2019, 32, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Yoshikata, R.; Myint, K.Z.; Ohta, H.; Ishigaki, Y. Inter-relationship between diet, lifestyle habits, gut microflora, and the equol-producer phenotype: Baseline findings from a placebo-controlled intervention trial. Menopause 2019, 26, 273–285. [Google Scholar] [CrossRef] [PubMed]


| Author/Year | Country | Arms/Comparators | Duration | Participants | Interventions | LBM Analyses |
|---|---|---|---|---|---|---|
| Iglay, 2009 | USA | HP: 1.2 g/kg body weight | 12 weeks | 36 postmenopausal women and men | HP diet + resistance training vs. | LBM increased: 1.1 ± 0.2 kg |
| NP: 0.9 g/kg body weight | age = 61 ± 1 years | NP diet + resistance training | no difference between the groups | |||
| Rossato, 2017 | Brazil | HP: 1.2 g/kg body weight | 10 weeks | 23 postmenopausal women | HP diet + resistance training vs. | HP LBM: 37.1 ± 6.2 to 38.4 ± 6.5 kg |
| NP: 0.8 g/kg body weight | age = 63.2 ± 7.8 years | NP diet + resistance training | NP LBM: 37.6 ± 6.2 to 38.8 ± 6.4 kg | |||
| no difference between the groups (p = 0.572) | ||||||
| Silva, 2020 | Brazil | HP: 1.6 g/kg body weight | 6 months | 26 postmenopausal women | HP diet vs. NP diet | HP LBM: 35.6 ± 0.7 to 35.7 ± 0.7 kg |
| NP: 0.8 g/kg body weight | age = 70.8 ± 3.6 years | NP LBM: 35.3 ± 0.7 to 35.4 ± 0.7 kg | ||||
| no difference between the groups (p = 0.683) |
| Guideline | Proteins | Fats | Carbohydrates | |||
|---|---|---|---|---|---|---|
| Yes | No or Moderate | Yes | No | Yes | No | |
| EAT Lancet Commission [77] |
|
|
|
|
|
|
| American Heart Association [78] |
|
|
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, T.R.; Oppermann, K.; Reis, F.M.; Spritzer, P.M. Nutrition in Menopausal Women: A Narrative Review. Nutrients 2021, 13, 2149. https://doi.org/10.3390/nu13072149
Silva TR, Oppermann K, Reis FM, Spritzer PM. Nutrition in Menopausal Women: A Narrative Review. Nutrients. 2021; 13(7):2149. https://doi.org/10.3390/nu13072149
Chicago/Turabian StyleSilva, Thais R., Karen Oppermann, Fernando M. Reis, and Poli Mara Spritzer. 2021. "Nutrition in Menopausal Women: A Narrative Review" Nutrients 13, no. 7: 2149. https://doi.org/10.3390/nu13072149
APA StyleSilva, T. R., Oppermann, K., Reis, F. M., & Spritzer, P. M. (2021). Nutrition in Menopausal Women: A Narrative Review. Nutrients, 13(7), 2149. https://doi.org/10.3390/nu13072149