Bone Mineral Density in Patients with Hepatic Glycogen Storage Diseases
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Data Collection
2.2.1. DXA Analysis
2.2.2. Biochemical Analysis
2.2.3. Food Diary
2.2.4. Anthropometric Measurements
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Sample
3.2. DXA
3.3. BTMs and Correlations with DXA, Metabolic Control and Biochemical Parameters
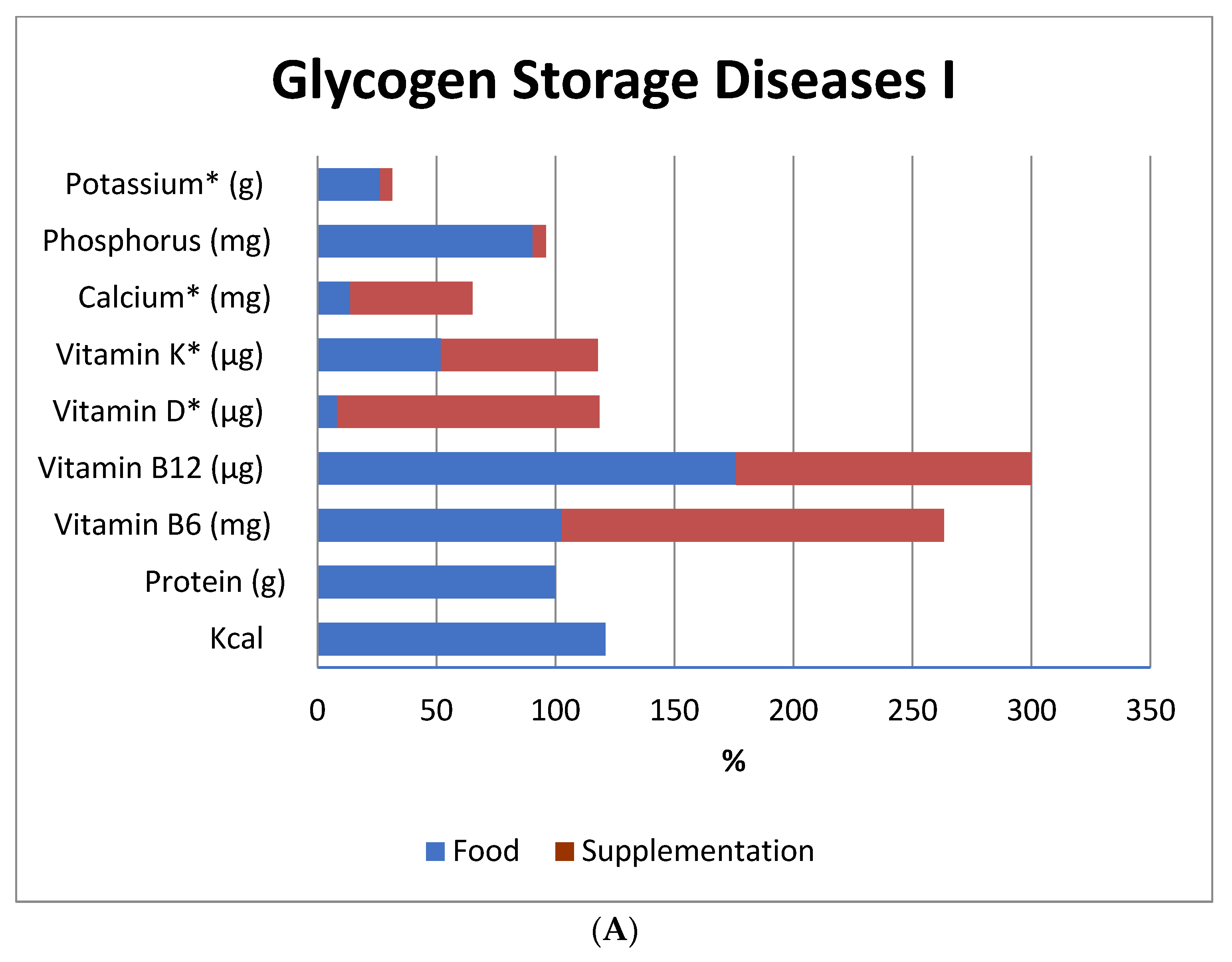
3.4. Nutritional Adequacy
3.4.1. Energy Intake
3.4.2. Protein Intake
3.4.3. Vitamin and Mineral Intake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Burda, P.; Hochuli, M. Hepatic Glycogen Storage Disorders. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 415–421. [Google Scholar] [CrossRef] [Green Version]
- Özen, H.; Bayraktar, Y. Glycogen Storage Diseases: New Perspectives Professor, Series Editor. World J. Gastroenterol. 2007, 13, 2541–2553. [Google Scholar] [CrossRef]
- Chou, J.Y.; Jun, H.S.; Mansfield, B.C. Glycogen Storage Disease Type I and G6Pase-B Deficiency: Etiology and Therapy. Nat. Rev. Endocrionl. 2010, 6, 676–688. [Google Scholar] [CrossRef]
- Kishnani, P.S.; Austin, S.L.; Abdenur, J.E.; Arn, P.; Bali, D.S.; Boney, A.; Chung, W.K.; Dagli, A.I.; Dale, D.; Koeberl, D.; et al. Diagnosis and Management of Glycogen Storage Disease Type I: A Practice Guideline of the American College of Medical Genetics and Genomics. Genet. Med. 2014, 16, e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sentner, C.P.; Hoogeveen, I.J.; Weinstein, D.A.; Santer, R.; Murphy, E.; McKiernan, P.J.; Steuerwald, U.; Beauchamp, N.J.; Taybert, J.; Laforêt, P.; et al. Glycogen Storage Disease Type III: Diagnosis, Genotype, Management, Clinical Course and Outcome. J. Inherit. Metab. Dis. 2016, 39, 697–704. [Google Scholar] [CrossRef] [Green Version]
- Kishnani, P.S.; Austin, S.L.; Arn, P.; Bali, D.S.; Boney, A.; Case, L.E.; Chung, W.K.; Desai, D.M.; El-Gharbawy, A.; Haller, R.; et al. Glycogen Storage Disease Type III Diagnosis and Management Guidelines. Genet. Med. 2010, 12, 446–463. [Google Scholar] [CrossRef] [Green Version]
- Derks, T.G.J.; van Rijn, M. Lipids in Hepatic Glycogen Storage Diseases: Pathophysiology, Monitoring of Dietary Management and Future Directions. J. Inherit. Metab. Dis. 2015, 38, 537–543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, M.A.; Weinstein, D.A. Glycogen Storage Diseases: Diagnosis, Treatment and Outcome. Transl. Sci. Rare Dis. 2014, 1, 45–72. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Yuan, Y.; Ma, M.; Liu, Y.; Zhang, W.; Yao, F.; Qiu, Z. Clinical and Genetic Characteristics of 17 Chinese Patients with Glycogen Storage Disease Type IXa. Gene 2017, 627, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Ross, K.M.; Ferrecchia, I.A.; Dahlberg, K.R.; Dambska, M.; Ryan, P.T.; Weinstein, D.A. Dietary Management of the Glycogen Storage Diseases: Evolution of Treatment and Ongoing Controversies. Adv. Nutr. 2020, 11, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Steunenberg, T.A.H.; Peeks, F.; Hoogeveen, I.J.; Mitchell, J.J.; Mundy, H.; de Boer, F.; Lubout, C.M.A.; de Souza, C.F.; Weinstein, D.A.; Derks, T.G.J. Safety Issues Associated with Dietary Management in Patients with Hepatic Glycogen Storage Disease. Mol. Genet. Metab. 2018, 125, 79–85. [Google Scholar] [CrossRef]
- Kishnani, P.S.; Goldstein, J.; Austin, S.L.; Arn, P.; Bachrach, B.; Bali, D.S.; Chung, W.K.; El-Gharbawy, A.; Brown, L.M.; Kahler, S.; et al. Diagnosis and Management of Glycogen Storage Diseases Type VI and IX: A Clinical Practice Resource of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 2019, 21, 772–789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Francini-pesenti, F.; Tresso, S.; Vitturi, N. Modified Atkins Ketogenic Diet Improves Heart and Skeletal Muscle Function in Glycogen Storage Disease Type III. Acta Myol. 2019, 38, 17–20. [Google Scholar] [PubMed]
- Bhattacharya, K. Investigation and Management of the Hepatic Glycogen Storage Diseases. Transl. Pediatr. 2015, 4, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Das, A.M.; Lücke, T.; Meyer, U.; Hartmann, H.; Illsinger, S. Glycogen Storage Disease Type 1: Impact of Medium-Chain Triglycerides on Metabolic Control and Growth. Ann. Nutr. Metab. 2010, 56, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Cabrera-Abreu, J.; Rabtree, N.J.C.; Lias, E.E.; Raser, W.F.; Ramb, R.C. Bone Mineral Density and Markers of Bone Turnover in Patients with Glycogen Storage Disease Types I, III and IX. J. Inherit. Metab. Dis. 2004, 27, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Minarich, L.A.; Kirpich, A.; Fiske, L.M.; Weinstein, D.A.; David, A.; Program, S.D. Bone Mineral Density in Glycogen Storage Disease Type Ia and Ib. Genet. Med. 2012, 14, 737–741. [Google Scholar] [CrossRef] [Green Version]
- Melis, D.; Rossi, A.; Pivonello, R.; Del Puente, A.; Pivonello, C.; Cangemi, G.; Negri, M.; Colao, A.; Andria, G.; Parenti, G. Reduced Bone Mineral Density in Glycogen Storage Disease Type III: Evidence for a Possible Connection between Metabolic Imbalance and Bone Homeostasis. Bone 2016, 86, 79–85. [Google Scholar] [CrossRef]
- Wolfsdorf, J.I. Bones Benefit from Better Biochemical Control in Type 1 Glycogen Storage Disease. J. Pediatr. 2002, 141, 308–310. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, N.; Gautschi, M.; Bosanska, L.; Meienberg, F.; Baumgartner, M.R.; Spinas, G.A.; Hochuli, M. Glycemic Control and Complications in Glycogen Storage Disease Type I: Results from the Swiss Registry. Mol. Genet. Metab. 2019, 126, 355–361. [Google Scholar] [CrossRef]
- Melis, D.; Pivonello, R.; Cozzolino, M.; Della Casa, R.; Balivo, F.; Del Puente, A.; Dionisi-Vici, C.; Cotugno, G.; Zuppaldi, C.; Rigoldi, M.; et al. Impaired Bone Metabolism in Glycogen Storage Disease Type 1 Is Associated with Poor Metabolic Control in Type 1a and with Granulocyte Colony-Stimulating Factor Therapy in Type 1b. Horm. Res. Paediatr. 2014, 81, 55–62. [Google Scholar] [CrossRef]
- de Castro, M.J.; de Lamas, C.; Sánchez-Pintos, P.; González-Lamuño, D.; Couce, M.L. Bone Status in Patients with Phenylketonuria. Nutrients 2020, 12, 2154. [Google Scholar] [CrossRef]
- Daly, A.; Högler, W.; Crabtree, N.; Shaw, N.; Evans, S.; Pinto, A.; Jackson, R.; Ashmore, C.; Rocha, J.C.; Strauss, B.J.; et al. A Three-Year Longitudinal Study Comparing Bone Mass, Density, and Geometry Measured by DXA, PQCT, and Bone Turnover Markers in Children with PKU Taking L-Amino Acid or Glycomacropeptide Protein Substitutes. Nutrients 2021, 13, 2–16. [Google Scholar]
- Lorentzon, M.; Branco, J.; Brandi, M.L.; Bruyère, O.; Chapurlat, R.; Cooper, C.; Cortet, B.; Diez-Perez, A.; Ferrari, S.; Gasparik, A.; et al. Algorithm for the Use of Biochemical Markers of Bone Turnover in the Diagnosis, Assessment and Follow-Up of Treatment for Osteoporosis. Adv. Ther. 2019, 36, 2811–2824. [Google Scholar] [CrossRef] [Green Version]
- Szulc, P.; Naylor, K.; Hoyle, N.R.; Eastell, R.; Leary, E.T. Use of CTX-I and PINP as Bone Turnover Markers: National Bone Health Alliance Recommendations to Standardize Sample Handling and Patient Preparation to Reduce Pre-Analytical Variability. Osteoporos. Int. 2017, 28, 2541–2556. [Google Scholar] [CrossRef] [PubMed]
- Rake, J.P.; Visser, G.; Huismans, D.; Huitema, S.; Van Der Veer, E.; Piers, D.A.; Smit, G.P.A. Bone Mineral Density in Children, Adolescents and Adults with Glycogen Storage Disease Type Ia: A Cross-Sectional and Longitudinal Study. J. Inherit. Metab. Dis. 2003, 26, 371–384. [Google Scholar] [CrossRef]
- World Health Organization. World Medical Association Declaration of Helsinki. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- ISCD. Official Positions Pediatric ISCD 2019. In Psychology Applied to Work: An Introduction to Industrial and Organizational Psychology, 10th ed.; Muchinsky, P., Ed.; 2019; Available online: https://iscd.org/learn/official-positions/pediatric-positions/ (accessed on 25 August 2021).
- ISCD. Official Positions Adult ISCD 2019. In Psychology Applied to Work: An Introduction to Industrial and Organizational Psychology, 10th ed.; Muchinsky, P., Ed.; 2019; Available online: https://iscd.org/learn/official-positions/adult-positions/ (accessed on 25 August 2021).
- Bayer, M. Reference Values of Osteocalcin and Procollagen Type I N-Propeptide Plasma Levels in a Healthy Central European Population Aged 0–18 Years. Osteoporos. Int. 2014, 25, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Wyness, S.P.; Roberts, W.L.; Straseski, J.A. Pediatric Reference Intervals for Four Serum Bone Markers Using Two Automated Immunoassays. Clin. Chim. Acta 2013, 415, 169–172. [Google Scholar] [CrossRef]
- Okechuku, G.O.; Shoemaker, L.R.; Dambska, M.; Brown, L.M.; Mathew, J.; Weinstein, D.A. Tight Metabolic Control plus ACE Inhibitor Therapy Improves GSD I Nephropathy. J. Inherit. Metab. Dis. 2017, 40, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Padovani, R.M.; Amaya-Farfán, J.; Colugnati, F.A.B.; Domene, S.M.Á. Dietary Reference Intakes: Application of Tables in Nutritional Studies. Rev. Nutr. 2006, 19, 741–760. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Child Growth Standards: Methods and Development: Length/Height-for-Age, Weight-for- Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- World Health Organization. Assessment of Fracture Risk and Its Application to Screening for Postmenopausal Osteoporosis: Report of a WHO Study Group; WHO: Geneva, Switzerland, 1994. [Google Scholar]
- Mundy, H.R.; Williams, J.E.; Lee, P.J.; Fewtrell, M.S. Reduction in Bone Mineral Density in Glycogenosis Type III May Be Due to a Mixed Muscle and Bone Deficit. J. Inherit. Metab. Dis. 2008, 31, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Soltani, S.; Hunter, G.R.; Kazemi, A.; Shab-Bidar, S. The Effects of Weight Loss Approaches on Bone Mineral Density in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Osteoporos. Int. 2016, 27, 2655–2671. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, J.; Koes, B.W.; Paulis, W.D.; van Middelkoop, M. Differences in Bone Mineral Density between Normal-Weight Children and Children with Overweight and Obesity: A Systematic Review and Meta-Analysis. Obes. Rev. 2017, 18, 526–546. [Google Scholar] [CrossRef]
- Vargas, D.M.; Kleis, S.K.; Lehmkuhl, N.R.D.S.; de Sousa, C.A.; de Azevedo, L.C. Predictors of Bone Mineral Density in Adolescents with Excess Weight. Rev. Bras. Med. Do Esporte 2020, 26, 508–512. [Google Scholar] [CrossRef]
- Filho, E.d.A.R.; Santos, M.A.M.d.; Silva, A.T.P.d.; Farah, B.Q.; Costa, M.d.C.; Campos, F.d.A.C.e.S.; Falcão, A.P.S.T. Relation between Body Composition and Bone Mineral Density in Young Undregraduate Students with Different Nutritional Status. Einstein (Sao Paulo) 2016, 14, 12–17. [Google Scholar] [CrossRef] [Green Version]
- Nilsen, O.A.; Ahmed, L.A.; Winther, A.; Christoffersen, T.; Thrane, G.; Evensen, E.; Furberg, A.-S.; Grimnes, G.; Dennison, E.; Emaus, N. Body Weight and Body Mass Index Influence Bone Mineral Density in Late Adolescence in a Two-Year Follow-Up Study. The Tromsø Study: Fit Futures. JBMR Plus 2019, 3, e10195. [Google Scholar] [CrossRef] [Green Version]
- Rowe, P.; Koller, A.; Sharma, S.; Hospital, M.F. Physiology, Bone Remodeling. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Ferron, M.; Lacombe, J. Regulation of Energy Metabolism by the Skeleton: Osteocalcin and Beyond. Arch. Biochem. Biophys. 2014, 561, 137–146. [Google Scholar] [CrossRef]
- Lee, N.K.; Sowa, H.; Hinoi, E.; Ferron, M.; Ahn, J.D.; Confavreux, C.; Dacquin, R.; Mee, P.J.; McKee, M.D.; Jung, D.Y.; et al. Endocrine Regulation of Energy Metabolism by the Skeleton. Cell 2007, 130, 456–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laird, E.; Ward, M.; McSorley, E.; Strain, J.J.; Wallace, J. Vitamin D and Bone Health; Potential Mechanisms. Nutrients 2010, 2, 693–724. [Google Scholar] [CrossRef] [Green Version]
- Muñoz-garach, A.; García-fontana, B.; Muñoz-torres, M. Nutrients and Dietary Patterns Related to Osteoporosis. Nutrients 2020, 12, 1986. [Google Scholar] [CrossRef]
- Weinstein, D.A.; Somers, M.J.G.; Wolfsdorf, J.I. Decrease Urinary Citrate Excretion in Type 1a Glycogen Storage Disease. J. Pediatr. 2001, 138, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Y.; Gao, W.; Wang, B.; Zhao, H.; Zeng, Y.; Ji, Y.; Hao, D. Diversity Analysis of Gut Microbiota in Osteoporosis and Osteopenia Patients. PeerJ 2017, 5, e3450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weaver, C.M. Diet, Gut Microbiome, and Bone Health Gut Mirobiome-a New Frontier? HHS Public Access. Curr. Osteoporos. Rep. 2015, 13, 125–130. [Google Scholar] [CrossRef]
- Li, C.; Huang, Q.; Yang, R.; Dai, Y.; Zeng, Y.; Tao, L.; Li, X.; Zeng, J.; Wang, Q. Gut Microbiota Composition and Bone Mineral Loss—Epidemiologic Evidence from Individuals in Wuhan, China. Osteoporos. Int. 2019, 30, 1003–1013. [Google Scholar] [CrossRef]
- Ceccarani, C.; Bassanini, G.; Montanari, C.; Casiraghi, M.C.; Ottaviano, E.; Morace, G.; Biasucci, G.; Paci, S.; Borghi, E.; Verduci, E. Proteobacteria Overgrowth and Butyrate-Producing Taxa Depletion in the Gut Microbiota of Glycogen Storage Disease Type 1 Patients. Metabolites 2020, 10, 133. [Google Scholar] [CrossRef] [Green Version]
- Colonetti, K.; dos Santos, B.B.; Nalin, T.; de Souza, C.F.M.; Triplett, E.W.; Dobbler, P.T.; Schwartz, I.V.D.; Roesch, L.F.W. Hepatic Glycogen Storage Diseases Are Associated to Microbial Dysbiosis. PLoS ONE 2019, 14, e0214582. [Google Scholar] [CrossRef]
- Meyer, H.E.; Willett, W.C.; Fung, T.T.; Holvik, K.; Feskanich, D. Association of High Intakes of Vitamins B6 and B12 From Food and Supplements With Risk of Hip Fracture Among Postmenopausal Women in the Nurses’ Health Study. JAMA Netw. Open 2019, 2, e193591. [Google Scholar] [CrossRef] [Green Version]
- Garcia Lopez, M.; Bønaa, K.H.; Ebbing, M.; Eriksen, E.F.; Gjesdal, C.G.; Nygård, O.; Tell, G.S.; Ueland, P.M.; Meyer, H.E. B Vitamins and Hip Fracture: Secondary Analyses and Extended Follow-Up of Two Large Randomized Controlled Trials. J. Bone Miner. Res. 2017, 32, 1981–1989. [Google Scholar] [CrossRef] [PubMed]

| Variables | Overall (n = 23) | Children (n = 12) | Adolescents (n = 5) | Adults (n = 6) | Reference Range |
|---|---|---|---|---|---|
| Sex (F/M) | 12/11 | 4/8 | 3/2 | 5/1 | - |
| GSD type (Ia/Ib/IIIa/IXα) | (13/5/2/3) | (6/3/1/2) | (3/1/1/0) | (4/1/0/1) | - |
| Weight (kg) | 56.0 (38.8–72.0) | 38.9 (28.5–46.5) | 76.0 (66.0–79.0) | 67.0 (59.3–85.0) | - |
| Age at diagnosis (years) | 1.0 (0.6–4.0) | 0.9 (0.6–2.2) | 1.0 (0.6–4.0) | 11.9 (1.1–24.3) | - |
| Height (cm) | 145.0 (132.0–154.0) | 135.0 (117.5–143.0) | 160.0 (152.0–162.0) | 152.0 (149.8–154.0) | - |
| BMI (kg/m2) | 25.1 (20.7–29.0) | 21.5 (19.2–27.0) | 29.0 (25.1–29.6) | 27.7 (24.3–35.8) | Children: ≥p3- <p85; Adults: 18.5 to 24.9. |
| Treatment duration (years) | 9.4 (5.8–15.4) | 8.5 (6.2–10.4) | 15.4 (9.5–15.5) | 12.3 (2.5–20.8) | - |
| UCCS (g/kg/day) | 6.3 (4.5–8.0) | 8.0 (4.8–10.9) | 5.3 (4.2–5.6) | 5.6 (3.2–6.7) | - |
| Serum: | |||||
| -25-OH Vitamin D (ng/mL) | 26.8 (18.1–30.5) | 26.1 (18.4–31.7) | 28.3 (26.8–40.0) | 19.9 (11.0–27.0) | Desirable: >20 |
| -Vitamin B12 (pg/mL) | 379.7 (289.1–561.7) | 416.1 (364.3–1074.5) | 263.0 (146.8–379.3) | 402.1 (160.0–561.7) | >221.4 |
| -Calcium (mmol/L) | 2.3 (2.3–2.4) | 2.4 (2.3–2.4) | 2.3 (2.2–2.4) | 2.3 (2.2–2.4) | 2.1–2.5 |
| -Phosphorus (mmol/L) | 1.4 (1.2–1.6) | 1.6 (1.4–1.7) | 1.3 (1.2–1.5) | 1.2 (1.1–1.3) | 0.8–1.5 |
| -Glucose (mmol/L) | 4.4 (3.9–5.0) | 4.5 (3.9–5.1) | 4.0 (3.9–4.3) | 4.6 (3.8–5.4) | 4.2–5.6 |
| -Glucose (mmol/L) * | 4.6 (4.3–4.9) | 4.6 (4.4–4.9) | 4.4 (4.3–4.6) | 4.8 (4.1–5.2) | 4.2–5.6 |
| -Lactate (mmol/L) | 1.3 (1.0–2.8) | 1.3 (1.1–3.5) | 1.5 (1.0–1.6) | 1.2 (0.9–1.8) | 0.5–2.2 |
| -Lactate (mmol/L) * | 1.5 (1.3–2.3) | 1.5 (1.2–2.2) | 1.4 (1.3–1.5) | 1.9 (1.5–3.4) | 0.5–2.2 |
| -Triglycerides (mmol/L) | 2.2 (1.2–3.2) | 2.2 (1.7–3.0) | 2.9 (2.9–3.4) | 1.3 (0.9–3.2) | < 2.3 |
| -Total cholesterol (mmol/L) | 4.5 (3.6–5.2) | 4.5 (4.3–5.6) | 4.2 (3.6–4.6) | 4.6 (3.6–5.2) | <5.2 |
| -HDL | 0.9 (0.7–1.0) | 0.8 (0.8–0.9) | 0.7 (0.6–1.1) | 1.0 (0.9–1.1) | >1.0 |
| -LDL | 2.6 (1.8–2.9) | 2.7 (1.8–3.6) | 1.8 (1.7–2.7) | 2.5 (2.1–3.2) | <3.3 |
| Bone turnover biomarkers (serum) | |||||
| -CTX (ng/mL) | 0.7 (0.3–1.1) | 1.1 (0.9–1.5) | 0.5 (0.2–1.0) | 0.5 (0.2–0.7) | Table S1 |
| -OC (ng/mL) | 55.6 (31.9–102.2) | 99.9 (79.7–114.4) | 48.4 (26.6–82.6) | 30.2 (23.6–36.1) | Table S1 |
| -P1NP (µg/L) | 304.1 (75.1–420.2) | 420.2 (386.0–750.7) | 254.4 (139.9–337.1) | 62.4 (57.3–82.1) | Table S1 |
| DXA—Z-score: | |||||
| -Whole body (minus the head) | −0.1 (−0.9–0.20) | −0.1 (−1.0–0.3) | −0.2 (−0.9–0.0) | N/A | >−2.0 |
| -Proximal femur | −0.8 (−1.0–−0.5) | N/A | N/A | −0.8 (−1.0–−0.5) | >−2.0 |
| -Lumbar spine | −0.6 (−1.3–−0.2) | −0.6 (−1.3–−0.2) | −0.6 (−1.0–−0.1) | −0.7 (−1.8–−0.4) | >−2.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jacoby, J.T.; Bento dos Santos, B.; Nalin, T.; Colonetti, K.; Farret Refosco, L.; F. M. de Souza, C.; Spritzer, P.M.; Poloni, S.; Hack-Mendes, R.; Schwartz, I.V.D. Bone Mineral Density in Patients with Hepatic Glycogen Storage Diseases. Nutrients 2021, 13, 2987. https://doi.org/10.3390/nu13092987
Jacoby JT, Bento dos Santos B, Nalin T, Colonetti K, Farret Refosco L, F. M. de Souza C, Spritzer PM, Poloni S, Hack-Mendes R, Schwartz IVD. Bone Mineral Density in Patients with Hepatic Glycogen Storage Diseases. Nutrients. 2021; 13(9):2987. https://doi.org/10.3390/nu13092987
Chicago/Turabian StyleJacoby, Jésica Tamara, Bruna Bento dos Santos, Tatiele Nalin, Karina Colonetti, Lília Farret Refosco, Carolina F. M. de Souza, Poli Mara Spritzer, Soraia Poloni, Roberta Hack-Mendes, and Ida Vanessa Doederlein Schwartz. 2021. "Bone Mineral Density in Patients with Hepatic Glycogen Storage Diseases" Nutrients 13, no. 9: 2987. https://doi.org/10.3390/nu13092987







