An Attempt to Assess the Impact of Pandemic Restrictions on the Lifestyle, Diet, and Body Mass Index of Children with Endocrine Diseases—Preliminary Results
Abstract
:1. Introduction
- The pandemic has a negative impact on physical activity, eating habits, play, sedentary behaviors, leisure screen time, and sleep in school-aged children and youth with chronic endocrine disorders.
- The pandemic has a negative impact on body weight and BMI in school-aged children and youth with chronic endocrine disorders.
2. Materials and Methods
2.1. Study Design
- Consent to participate in the study.
- Availability of documented measurements of body weight and height.
- Lack of consent to participate in the study.
- Lack of documented measurements of body weight and height.
2.2. Participants
2.3. Procedures
Anthropometric Measurements
2.4. Ethics
2.5. Statistics
3. Results
3.1. Descriptive Analysis
3.2. Anthropometric Data
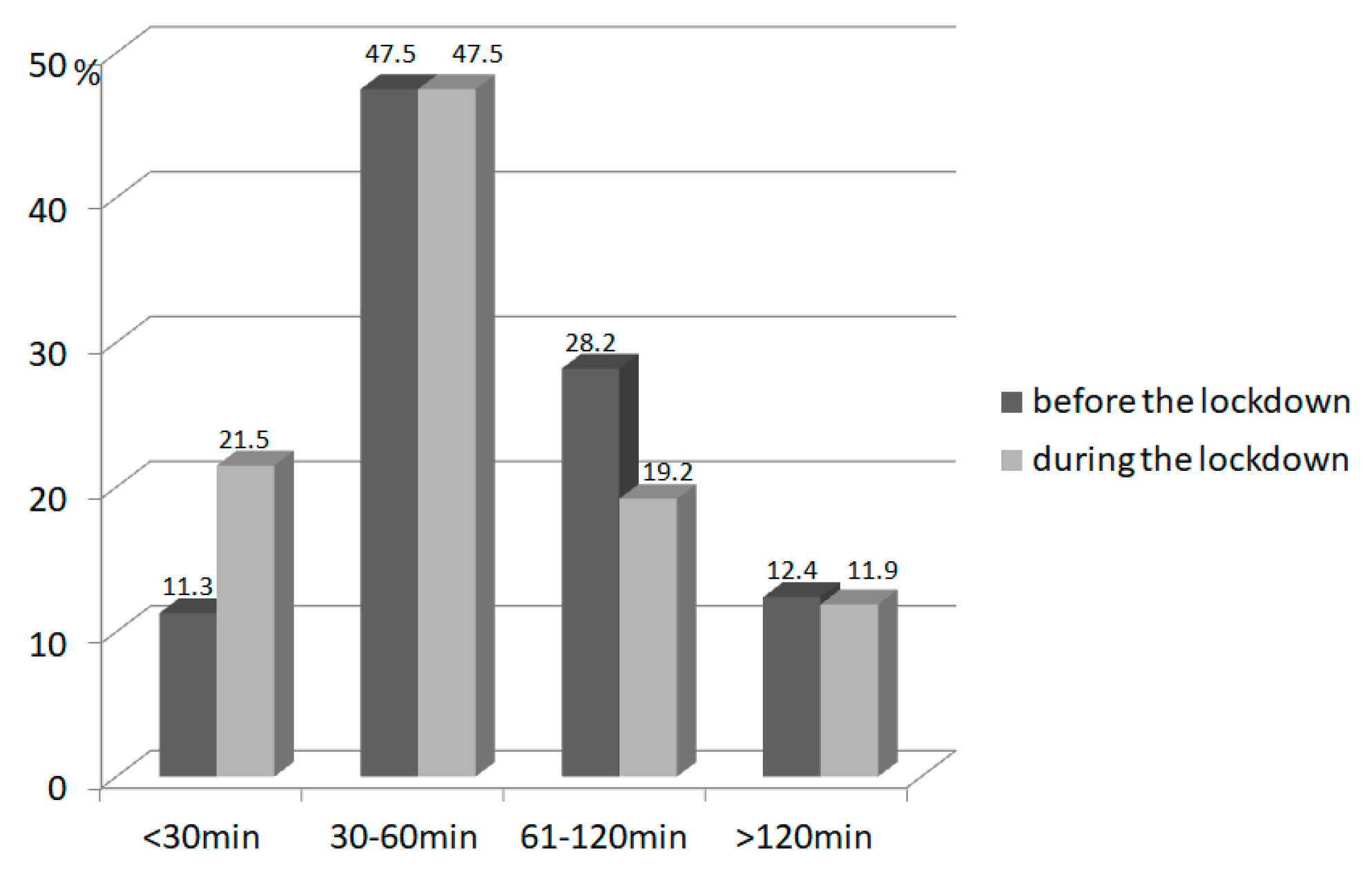
3.3. Physical Activity
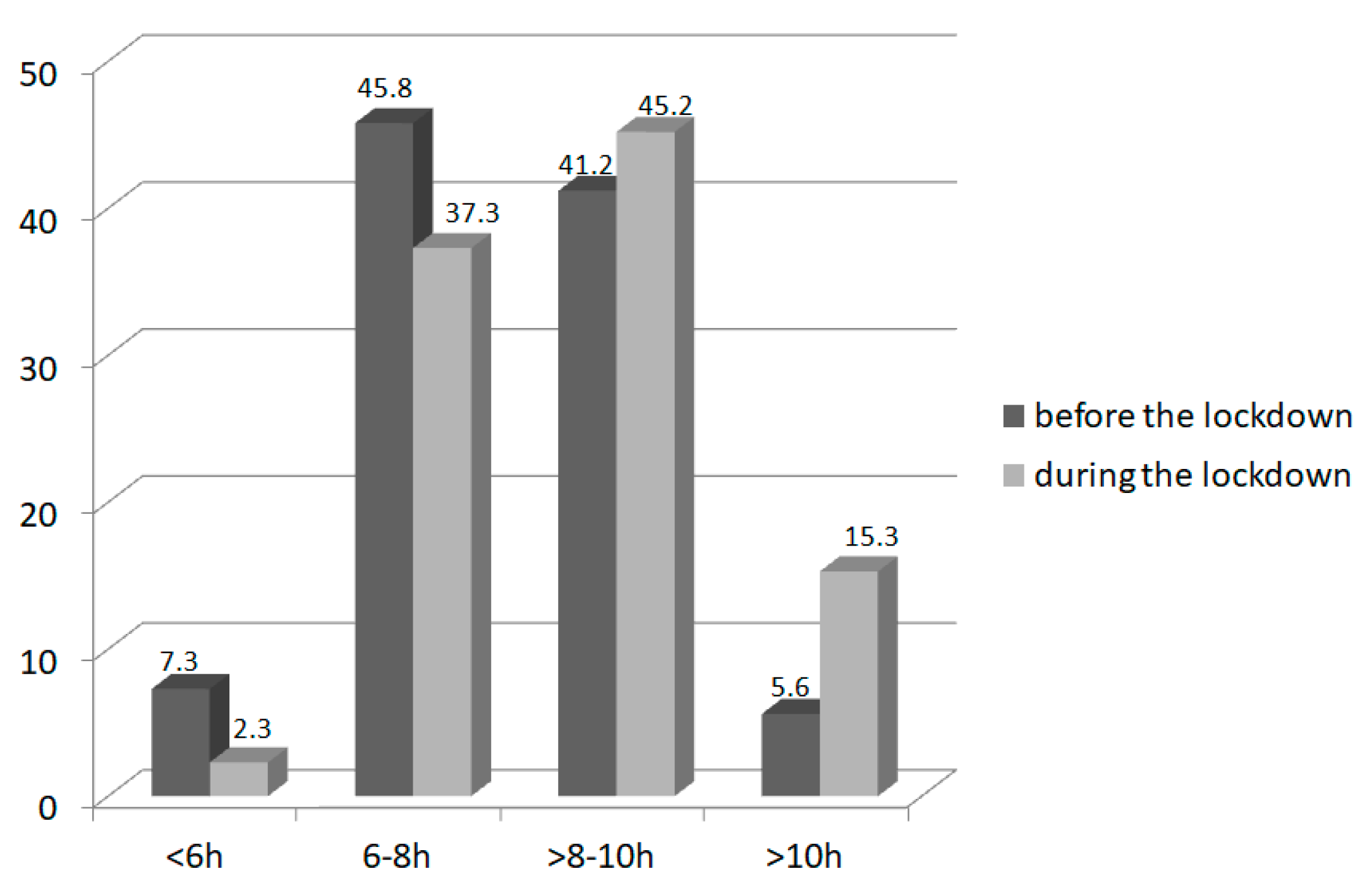
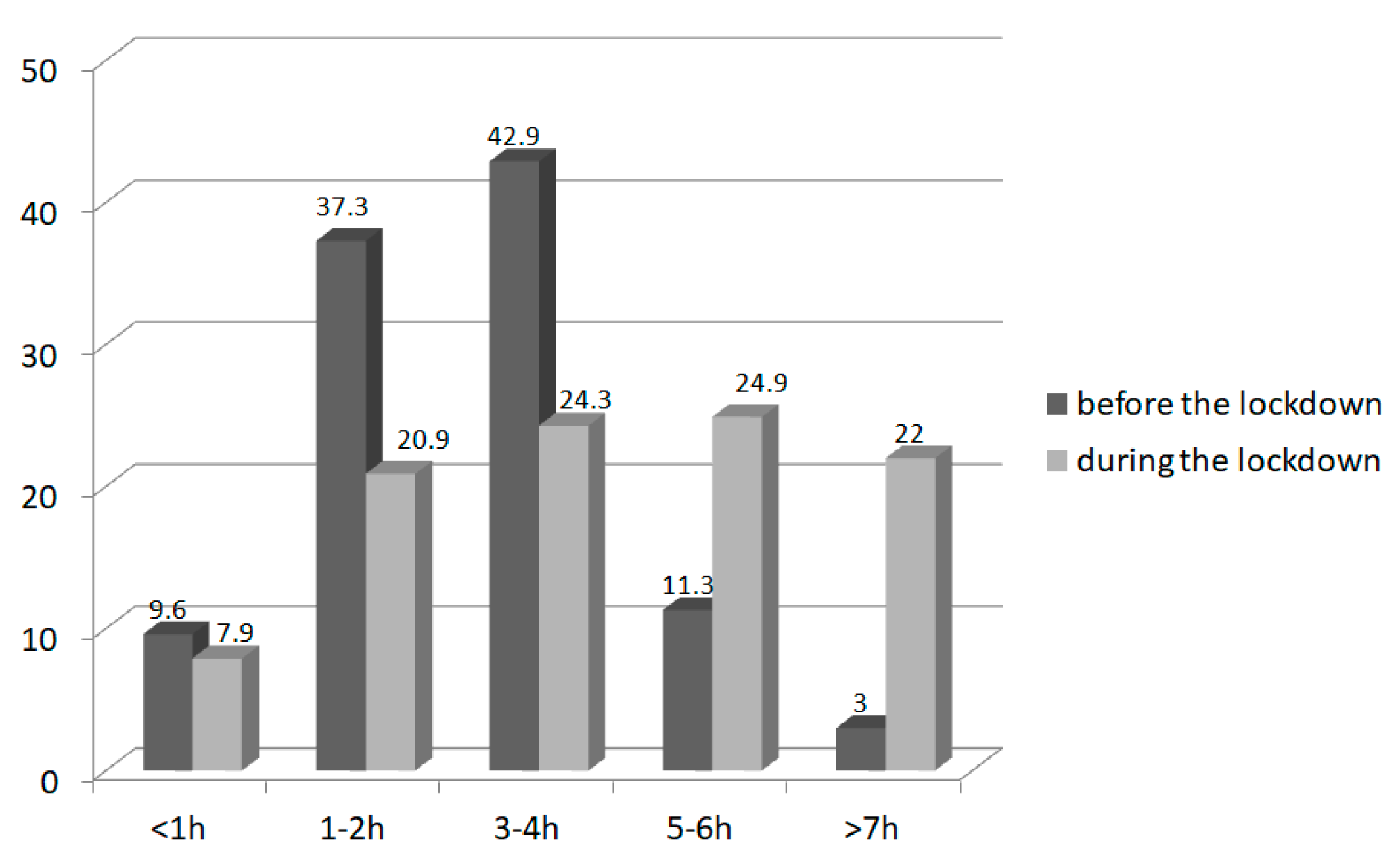
3.4. Sleep and Screen Time
3.5. Eating Habits
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Patient’s code | DoB | Sex |
| Physical activity (at and outside school) | ||||||
| Low physical activity during the day (walk, cycle) | Less than 30 min | 30–60 min | 61–120 min | More than 120 min | ||
| High physical activity (run, playing game, training) | Less than 30 min | 30–60 min | 61–120 min | More than 120 min | ||
| Sleep | ||||||
| Hours per day | Less than 6 | 6–8 | 8–10 | More than 10 | ||
| Meals | ||||||
| Number per day | 1 | 2 | 3 | 4 | 5 and more | |
| How often does your child eat: A—never/less than once a week B—1–3 times per week C—4–6 times per week D—1–2 times a day E—3 or more times a day F—do not know | ||||||
| Snacks/sweets | A | B | C | D | E | F |
| Soda/juice | A | B | C | D | E | F |
| Vegetables | A | B | C | D | E | F |
| Fruits | A | B | C | D | E | F |
| Fast-food restaurant | A | B | C | D | E | F |
| Screen time (hours a day) | Less than 1 h | 1–2 h | 3–4 h | 5–6 h | More than 7 h | |
| Physical activity (at and outside school) | ||||||
| Low physical activity during the day (walk, cycle) | Less than 30 min | 30–60 min | 61–120 min | More than 120 min | ||
| High physical activity (run, playing game, training) | Less than 30 min | 30–60 min | 61–120 min | More than 120 min | ||
| Sleep | ||||||
| Hours per day | Less than 6 | 6–8 | 8–10 | More than 10 | ||
| Meals | ||||||
| Number per day | 1 | 2 | 3 | 4 | 5 and more | |
| How often does your child eat: A—never/less than once a week B—1–3 times per week C—4–6 times per week D—1–2 times a day E—3 or more times a day F—do not know | ||||||
| Snacks/sweets | A | B | C | D | E | F |
| Soda/juice | A | B | C | D | E | F |
| Vegetables | A | B | C | D | E | F |
| Fruits | A | B | C | D | E | F |
| Fast-food restaurant | A | B | C | D | E | F |
| Screen time (hours a day) | Less than 1 h | 1–2 h | 3–4 h | 5–6 h | More than 7 h | |
| The physical activity of your child | decreased | did not change | increased | do not know |
| Screen time of your child | decreased | did not change | increased | do not know |
| Sleep duration of your child | decreased | did not change | increased | do not know |
| The diet of your child is | more healthy | the same | less healthy | do not know |
| Your physical activity | decreased | did not change | increased | do not know |
| Your screen time | decreased | did not change | increased | do not know |
| Your sleep duration | decreased | did not change | increased | do not know |
| Your diet | more healthy | the same | less healthy | do not know |
| Block of flats | House with small garden space | House with big garden space | |
| Village | Small town | Average town | Big city |
References
- Guan, H.; Okely, A.D.; Aguilar-Farias, N.; Del Pozo Cruz, B.; Draper, C.E.; Hamdouchi, A.E.; Florindo, A.A.; Jáuregui, A.; Katzmarzyk, P.T.; Kontsevaya, A.; et al. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child Adolesc. Health 2020, 4, 416–418. [Google Scholar] [CrossRef]
- Chen, P.; Mao, L.; Nassis, G.P.; Harmer, P.; Ainsworth, B.E.; Li, F. Returning Chinese school-aged children and adolescents to physical activity in the wake of COVID-19: Actions and precautions. J. Sport Health Sci. 2020, 9, 322–324. [Google Scholar] [CrossRef]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Ca-nadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 85. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID 19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Poelman, M.P.; Gillebaart, M.; Schlinkert, C.; Dijkstra, S.C.; Derksen, E.; Mensink, F.; Hermans, R.C.; Aardening, P.; de Ridder, D.; de Vet, E. Eating behavior and food purchases during the COVID-19 lockdown: A cross-sectional study among adults in the Netherlands. Appetite 2021, 157, 105002. [Google Scholar] [CrossRef]
- Huizar, M.I.; Arena, R.; Laddu, D.R. “Covibesity”, a new pandemic. Obes. Med. 2020, 19, 100282. [Google Scholar]
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.; Tsitsika, A. Obesity in Children and Adolescents during COVID-19 Pandemic. Children 2021, 8, 135. [Google Scholar] [CrossRef]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef]
- Pombo, A.; Luz, C.; Rodrigues, L.P.; Ferreira, C.; Cordovil, R. Correlates of children’s physical activity during the COVID-19 confinement in Portugal. Public Health 2020, 189, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Panahi, S.; Tremblay, A. Sedentariness and Health: Is Sedentary Behavior More Than Just Physical Inactivity? Front. Public Health 2018, 6, 258. [Google Scholar] [CrossRef] [Green Version]
- Ashby, N.J.S. Impact of the COVID-19 Pandemic on Unhealthy Eating in Populations with Obesity. Obesity 2020, 28, 1802–1805. [Google Scholar] [CrossRef] [PubMed]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Xiang, M.; Cheung, T.; Xiang, Y.-T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 2021, 279, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Nagata, J.M.; Magid, H.S.A.; Gabriel, K.P. Screen Time for Children and Adolescents During the Coronavirus Disease 2019 Pandemic. Obesity 2020, 28, 1582–1583. [Google Scholar] [CrossRef]
- Jia, P.; Li, M.; Xue, H.; Lu, L.; Xu, F.; Wang, Y. School environment and policies, child eating behavior and overweight/obesity in urban China: The childhood obesity study in China megacities. Int. J. Obes. 2017, 41, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Jia, P.; Liu, L.; Xie, X.; Yuan, C.; Chen, H.; Guo, B.; Zhou, J.; Yang, S. Changes in dietary patterns among youths in China during COVID-19 epidemic: The COVID-19 impact on lifestyle change survey (COINLICS). Appetite 2020, 158, 105015. [Google Scholar] [CrossRef]
- Biro, F.M.; Wien, M. Childhood obesity and adult morbidities. Am. J. Clin. Nutr. 2010, 91, 1499S–1505S. [Google Scholar] [CrossRef] [Green Version]
- Whitaker, R.C.; Wright, J.A.; Pepe, M.S.; Seidel, K.D.; Dietz, W.H. Predicting Obesity in Young Adulthood from Childhood and Parental Obesity. N. Engl. J. Med. 1997, 337, 869–873. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh-Taskar, P.; Nicklas, T.A.; Morales, M.; Yang, S.-J.; Zakeri, I.; Berenson, G.S. Tracking of overweight status from childhood to young adulthood: The Bogalusa Heart Study. Eur. J. Clin. Nutr. 2005, 60, 48–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jia, P.; Zhang, L.; Yu, W.; Yu, B.; Liu, M.; Zhang, D.; Yang, S. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: The COVID-19 Impact on Lifestyle Change Survey (COINLICS). Int. J. Obes. 2021, 45, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Mulugeta, W.M.; Hoqueb, L. Impact of the COVID-19 lockdown on weight status and associated factors for obesity among children in Massachusetts. Obes. Med. 2021, 22, 10032. [Google Scholar] [CrossRef]
- Wunsch, K.; Nigg, C.; Niessner, C.; Schmidt, S.C.E.; Oriwol, D.; Hanssen-Doose, A.; Burchartz, A.; Eichsteller, A.; Kolb, S.; Worth, A.; et al. The Impact of COVID-19 on the Interrelation of Physical Activity, Screen Time and Health-Related Quality of Life in Children and Adolescents in Germany: Results of the Motorik-Modul Study. Children 2021, 8, 98. [Google Scholar] [CrossRef]
- Skerritt, J.; Mulvany, L.; Almeida, I. Americans Drop Kale and Quinoa to Lock Down with Chips and Oreos. Available online: https://www.bloomberg.com/news/articles/2020-03-21/americans-drop-kale-andquinoa-to-lock-down-with-chips-and-oreos 2020 (accessed on 24 March 2020).

| The Purpose of Visit in the Outpatient | Number | % |
|---|---|---|
| Obesity | 64 | 36.2 |
| Type 1 diabetes | 36 | 20.3 |
| Growth hormone deficiency | 39 | 22.0 |
| Thyroid disorders | 10 | 5.6 |
| Turner syndrome | 7 | 4.0 |
| Other endocrine disorders (growth and puberty disorders, Prader–Willi syndrome, SGA, gynecomastia) | 15 | 8.5 |
| Other lipids and carbohydrates metabolism disorders | 6 | 3.4 |
| Total (n = 177) | Males (n = 96) | Females (n = 81) | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | Range | |
| Age (y) | 12.8 ± 2.6 | 5.7–18.5 | 12.9 ± 2.3 | 5.7–16.1 | 12.6 ± 2.8 | 6.8–18.5 |
| Height (cm) | 156.2 ± 17.5 | 111.7–195.0 | 160.7 ± 16.5 | 121.0–195.0 | 150.9 ± 17.1 | 11.7–183.7 |
| Weight (kg) | 59.8 ± 25.2 | 19.0–162.0 | 64.0 ± 26.2 | 20.6–162.0 | 54.9 ± 23.1 | 19.0–114.0 |
| Garden space | Number | % | ||||
| None | 48 | 27.3 | ||||
| Small | 16 | 9.1 | ||||
| Large | 112 | 63.6 | ||||
| Place of residence | Number | % | ||||
| Village | 93 | 52.8 | ||||
| Small town | 27 | 15.3 | ||||
| Average size town | 28 | 15.9 | ||||
| Large city | 28 | 15.9 |
| BMI z-Score | Before Lockdown (Mean ± SD) | During Lockdown (Mean ± SD) | Δ (Mean ± SD) | p |
|---|---|---|---|---|
| Study group (n = 177) | 0.79 ± 1.35 | 0.86 ± 1.31 | 0.07 ± 0.34 | 0.006 |
| Females (n = 96) | 0.84 ± 1.34 | 0.89 ± 1.37 | 0.05 ± 0.32 | 0.1 |
| Males (n = 81) | 0.73 ± 1.36 | 0.82 ± 1.26 | 0.094 ± 0.36 | 0.02 |
| Obese (n = 64) | 2.02 ± 0.44 | 2.10 ± 0.38 | 0.073 ± 0.18 | 0.002 |
| Non-obese (n = 113) | 0.09 ± 1.18 | 0.16 ± 1.27 | 0.07 ± 0.40 | 0.064 |
| Variable | Before Lockdown (Mean ± SD) | During Lockdown (Mean ± SD) | Δ (Mean ± SD) | p | |
|---|---|---|---|---|---|
| Low physical activity (rated 1 to 4) | Study group (n = 177) | 2.43 ± 0.85 | 2.22 ± 0.93 | −0.20 ± 0.88 | 0.002 |
| Obese (n = 64) | 2.47 ± 0.99 | 2.09 ± 1.06 | −0.38 ± 0.97 | 0.003 | |
| Non-obese (n = 113) | 2.40 ± 0.76 | 2.29 ± 0.84 | −0.11 ± 0.82 | 0.17 | |
| High physical activity (rated 1 to 4) | Study group | 1.80 ± 0.83 | 1.43 ± 0.61 | −0.37 ± 0.95 | <0.001 |
| Obese | 1.70 ± 0.90 | 1.28 ± 0.49 | −0.42 ± 0.81 | <0.001 | |
| Non-obese | 1.85 ± 0.79 | 1.51 ± 0.66 | −0.33 ± 1.02 | <0.001 | |
| Amount of sleep (rated 1 to 4) | Study group | 2.45 ± 0.71 | 2.73 ± 0.74 | 0.28 ± 0.60 | <0.001 |
| Obese | 2.25 ± 0.64 | 2.53 ± 0.77 | 0.28 ± 0.74 | 0.004 | |
| Non-obese | 2.56 ± 0.73 | 2.85 ± 0.70 | 0.28 ± 0.49 | <0.001 | |
| Screen time (rated 1 to 5) | Study group | 2.66 ± 0.92 | 3.32 ± 1.25 | 0.66 ± 1.07 | <0.001 |
| Obese | 2.75 ± 0.93 | 3.36 ± 1.33 | 0.61 ± 1.23 | <0.001 | |
| Non-obese | 2.61 ± 0.92 | 3.30 ± 1.21 | 0.69 ± 0.93 | <0.001 | |
| Number of meals per day (rated 1 to 5) | Study group | 4.25 ± 0.74 | 4.29 ± 0.71 | 0.04 ± 0.63 | 0.41 |
| Obese | 4.26 ± 0.76 | 4.23 ± 0.85 | −0,03 ± 0.56 | 0.66 | |
| Non-obese | 4.25 ± 0.74 | 4.33 ± 0.62 | 0.08 ± 0.67 | 0.21 | |
| Snacks/sweets consumption (rated 1 to 6) | Study group | 2.64 ± 0.96 | 2.55 ± 1.08 | −0.09 ± 0.75 | 0.11 |
| Obese | 2.69 ± 0.99 | 2.66 ± 1.09 | −0.03 ± 0.82 | 0.76 | |
| Non-obese | 2.61 ± 0.95 | 2.49 ± 1.07 | −0.12 ± 0.71 | 0.065 | |
| Soda/juice consumption (rated 1 to 6) | Study group | 2.29 ± 1.32 | 2.21 ± 1.27 | −0.08 ± 1.0 | 0.29 |
| Obese | 2.48 ± 1.29 | 2.31 ± 1.22 | −0.17 ± 1.02 | 0.18 | |
| Non-obese | 2.18 ± 1.32 | 2.16 ± 1.30 | −0.07 ± 0.99 | 0.77 | |
| Vegetable consumption (rated 1 to 6) | Study group | 3.44 ± 1.10 | 3.34 ± 1.11 | −0.10 ± 0.87 | 0.14 |
| Obese | 3.33 ± 1.25 | 3.17 ± 1.24 | −0.16 ± 1.10 | 0.26 | |
| Non-obese | 3.50 ± 1.00 | 3.44 ± 1.02 | −0.06 ± 0.71 | 0.36 | |
| Fruit consumption (rated 1 to 6) | Study group | 3.42 ± 1.08 | 3.42 ± 1.19 | −0.006 ± 0.91 | 0.93 |
| Obese | 3.39 ± 1.20 | 3.50 ± 1.31 | 0.11 ± 1.14 | 0.18 | |
| Non-obese | 3.44 ± 1.00 | 3.37 ± 1.12 | −0.07 ± 0.75 | 0.21 | |
| Fast-food meals consumption (rated 1 to 6) | Study group | 1.41 ± 1.11 | 1.36 ± 1.07 | −0.05 ± 0.65 | 0.30 |
| Obese | 1.52 ± 1.04 | 1.39 ± 0.94 | −0.13 ± 1.06 | 0.35 | |
| Non-obese | 1.35 ± 1.14 | 1.34 ± 1.14 | −0.01 ± 0.16 | 0.57 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zachurzok, A.; Wójcik, M.; Gawlik, A.; Starzyk, J.B.; Mazur, A. An Attempt to Assess the Impact of Pandemic Restrictions on the Lifestyle, Diet, and Body Mass Index of Children with Endocrine Diseases—Preliminary Results. Nutrients 2022, 14, 156. https://doi.org/10.3390/nu14010156
Zachurzok A, Wójcik M, Gawlik A, Starzyk JB, Mazur A. An Attempt to Assess the Impact of Pandemic Restrictions on the Lifestyle, Diet, and Body Mass Index of Children with Endocrine Diseases—Preliminary Results. Nutrients. 2022; 14(1):156. https://doi.org/10.3390/nu14010156
Chicago/Turabian StyleZachurzok, Agnieszka, Małgorzata Wójcik, Aneta Gawlik, Jerzy B. Starzyk, and Artur Mazur. 2022. "An Attempt to Assess the Impact of Pandemic Restrictions on the Lifestyle, Diet, and Body Mass Index of Children with Endocrine Diseases—Preliminary Results" Nutrients 14, no. 1: 156. https://doi.org/10.3390/nu14010156







