Nutrient-Derived Beneficial for Blood Pressure Dietary Pattern Associated with Hypertension Prevention and Control: Based on China Nutrition and Health Surveillance 2015–2017
Abstract
:1. Introduction
2. Materials and Methods
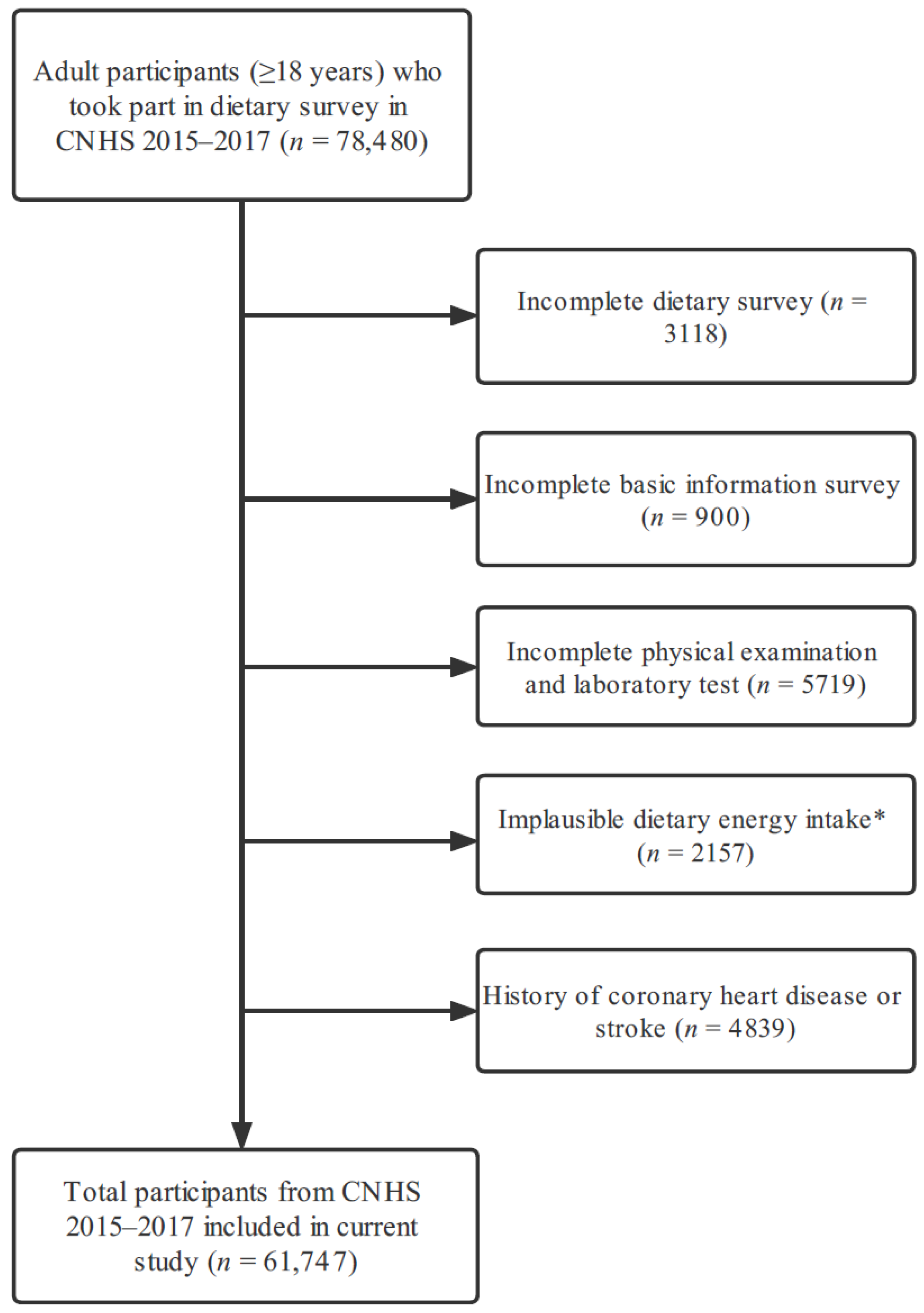
2.1. Study Population
2.2. Basic Information Interview
2.3. Medical Examination and Laboratory Test
2.4. Dietary Assessment
2.5. Definition of HTN and Other NCDs
2.6. Dietary Pattern Analysis
2.7. Covariates
2.8. Statistical Analysis
3. Results
3.1. Dietary Pattern Extracted by RRR
3.2. Characteristics of Participants in Quintile Groups
3.3. Food and Nutrients Daily Intake of Participants in Quintile Groups
3.4. Association between Dietary Scores and Risk of HTN
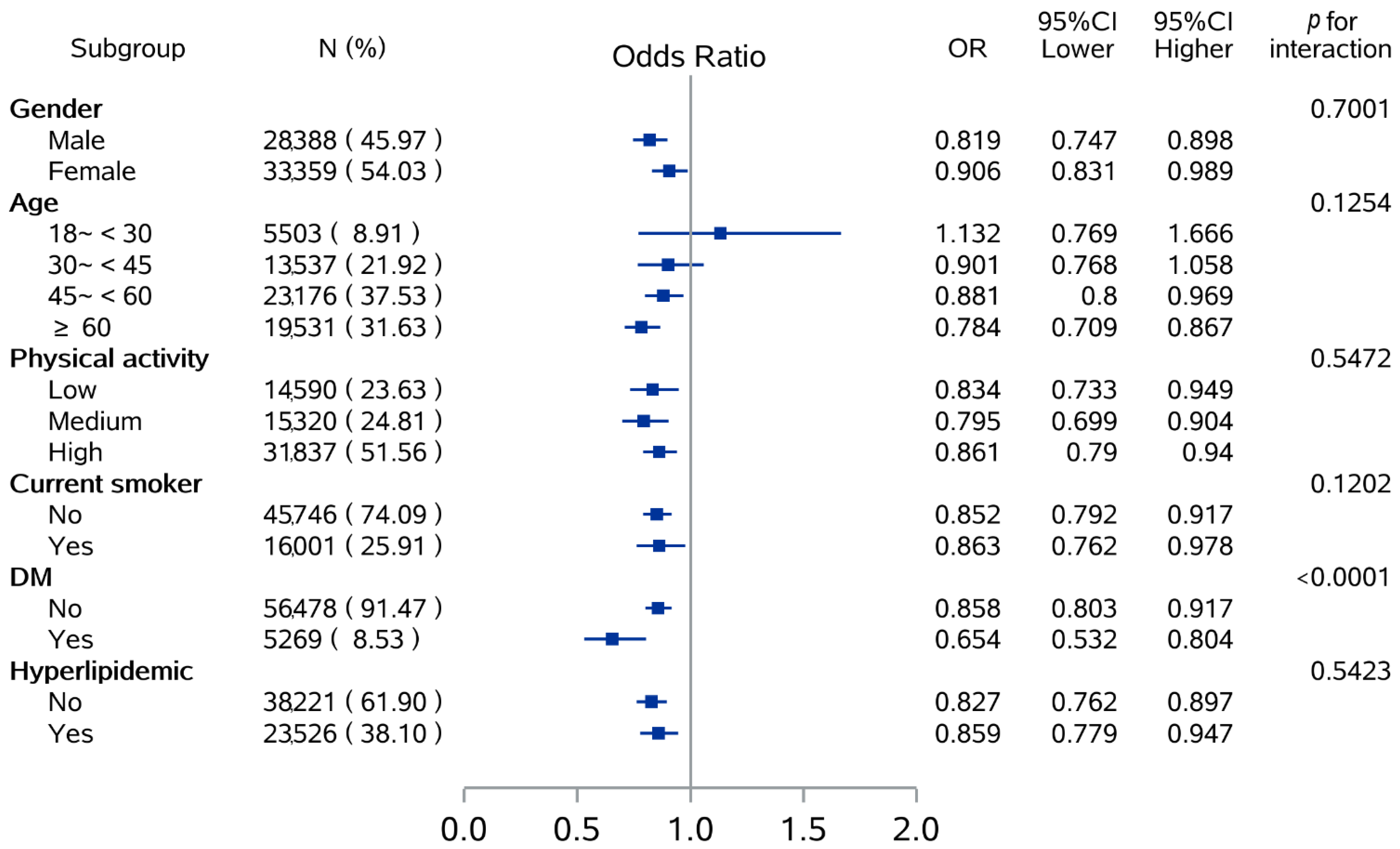
3.5. Subgroup Analysis
3.6. Sensitivity Analysis
3.7. Association between Dietary Scores and Well-Controlled HTN
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carey, R.M.; Muntner, P.; Bosworth, H.B.; Whelton, P.K. Prevention and Control of Hypertension: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1278–1293. [Google Scholar] [CrossRef] [PubMed]
- Park, J.E.; Jung, H.; Lee, J.E. Dietary pattern and hypertension in Korean adults. Public Health Nutr. 2014, 17, 597–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ettehad, D.; Emdin, C.A.; Kiran, A.; Anderson, S.G.; Callender, T.; Emberson, J.; Chalmers, J.; Rodgers, A.; Rahimi, K. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 2016, 387, 957–967. [Google Scholar] [CrossRef] [Green Version]
- Katalambula, L.K.; Meyer, D.N.; Ngoma, T.; Buza, J.; Mpolya, E.; Mtumwa, A.H.; Petrucka, P. Dietary pattern and other lifestyle factors as potential contributors to hypertension prevalence in Arusha City, Tanzania: A population-based descriptive study. BMC Public Health 2017, 17, 659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nulu, S.; Aronow, W.S.; Frishman, W.H. Hypertension in Sub-Saharan Africa: A Contextual View of Patterns of Disease, Best Management, and Systems Issues. Cardiol. Rev. 2016, 24, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Lu, Y.; Wang, X.; Li, X.; Linderman, G.C.; Wu, C.; Cheng, X.; Mu, L.; Zhang, H.; Liu, J.; et al. Prevalence, awareness, treatment, and control of hypertension in China: Data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 2017, 390, 2549–2558. [Google Scholar] [CrossRef]
- Yi, Q.; Zha, M.; Yang, Q.; Zhang, Y.; Hou, L.; Ye, X.; Chen, G.; Shao, J.; Xia, W.; Song, P. Trends in the prevalence of hypertension according to severity and phenotype in Chinese adults over two decades (1991–2015). J. Clin. Hypertens 2021, 23, 1302–1315. [Google Scholar] [CrossRef]
- Dickinson, H.O.; Mason, J.M.; Nicolson, D.J.; Campbell, F.; Beyer, F.R.; Cook, J.V.; Williams, B.; Ford, G.A. Lifestyle interventions to reduce raised blood pressure: A systematic review of randomized controlled trials. J. Hypertens 2006, 24, 215–233. [Google Scholar] [CrossRef]
- Forman, J.P.; Stampfer, M.J.; Curhan, G.C. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA 2009, 302, 401–411. [Google Scholar] [CrossRef] [Green Version]
- Kopp, W. How Western Diet And Lifestyle Drive The Pandemic Of Obesity And Civilization Diseases. Diabetes Metab. Syndr. Obes. 2019, 12, 2221–2236. [Google Scholar] [CrossRef] [Green Version]
- Song, S.; Kim, J.; Kim, J. Gender Differences in the Association between Dietary Pattern and the Incidence of Hypertension in Middle-Aged and Older Adults. Nutrients 2018, 10, 252. [Google Scholar] [CrossRef] [Green Version]
- Salehi-Abargouei, A.; Maghsoudi, Z.; Shirani, F.; Azadbakht, L. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases—Incidence: A systematic review and meta-analysis on observational prospective studies. Nutrition 2013, 29, 611–618. [Google Scholar] [CrossRef]
- Yi, S.Y.; Steffen, L.M.; Haring, B.; Rebholz, C.M.; Mosley, T.H.; Shah, A.M. Associations of the Dietary Approaches to Stop Hypertension dietary pattern with cardiac structure and function. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3345–3351. [Google Scholar] [CrossRef]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean diet, its components, and cardiovascular disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef] [Green Version]
- Grosso, G.; Stepaniak, U.; Micek, A.; Topor-Madry, R.; Stefler, D.; Szafraniec, K.; Bobak, M.; Pajak, A. A Mediterranean-type diet is associated with better metabolic profile in urban Polish adults: Results from the HAPIEE study. Metabolism 2015, 64, 738–746. [Google Scholar] [CrossRef]
- Ozemek, C.; Laddu, D.R.; Arena, R.; Lavie, C.J. The role of diet for prevention and management of hypertension. Curr. Opin. Cardiol. 2018, 33, 388–393. [Google Scholar] [CrossRef]
- Sun, J.; Buys, N.J.; Hills, A.P. Dietary pattern and its association with the prevalence of obesity, hypertension and other cardiovascular risk factors among Chinese older adults. Int. J. Environ. Res. Public Health 2014, 11, 3956–3971. [Google Scholar] [CrossRef]
- Xiao, X.; Qin, Z.; Lv, X.; Dai, Y.; Ciren, Z.; Yangla, Y.; Zeng, P.; Ma, Y.; Li, X.; Wang, L.; et al. Dietary patterns and cardiometabolic risks in diverse less-developed ethnic minority regions: Results from the China Multi-Ethnic Cohort (CMEC) Study. Lancet Reg. Health West Pac. 2021, 15, 100252. [Google Scholar] [CrossRef]
- Wang, D.; He, Y.; Li, Y.; Luan, D.; Yang, X.; Zhai, F.; Ma, G. Dietary patterns and hypertension among Chinese adults: A nationally representative cross-sectional study. BMC Public Health 2011, 11, 925. [Google Scholar] [CrossRef] [Green Version]
- Hoffmann, K.; Schulze, M.B.; Schienkiewitz, A.; Nothlings, U.; Boeing, H. Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am. J. Epidemiol. 2004, 159, 935–944. [Google Scholar] [CrossRef]
- Sun, Q.; Wen, Q.; Lyu, J.; Sun, D.; Ma, Y.; Man, S.; Yin, J.; Jin, C.; Tong, M.; Wang, B.; et al. Dietary pattern derived by reduced-rank regression and cardiovascular disease: A cross-sectional study. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 337–345. [Google Scholar] [CrossRef]
- Yu, D.; Zhao, L.; Zhang, J.; Yang, Z.; Yang, L.; Huang, J.; Fang, H.; Guo, Q.; Xu, X.; Ju, L.; et al. China Nutrition and Health Surveys (1982–2017). China CDC Wkly. 2021, 3, 193–195. [Google Scholar] [CrossRef]
- Liu, D.; He, L.; Zhang, X.; Zhai, Y.; Zhang, J.; Yang, X.; Chen, J.; Zhao, W. Establishment and application of food frequency questionnaire method among Chinese. Wei Sheng Yan Jiu 2018, 47, 744–755. [Google Scholar] [PubMed]
- Yang, Y.X. China Food Composition Tables; Standard Edition; Peking University Medical Press: Beijing, China, 2018. [Google Scholar]
- Yang, Y.X.; Wang, G.Y.; Pan, X.C. China Food Composition Table, 2nd ed.; Peking University Medical Press: Beijing, China, 2009. [Google Scholar]
- Chang, J.L.; Wang, Y.; Liang, X.F.; Wu, L.Y.; Ding, G.Q. Report of Chinese Residents’ Nutrition and Health Surveillance 2010–2013; Peking University Medical Press: Beijing, China, 2016. [Google Scholar]
- Yang, Y.; Piao, W.; Huang, K.; Fang, H.; Ju, L.; Zhao, L.; Yu, D.; Ma, Y. Dietary Pattern Associated with the Risk of Hyperuricemia in Chinese Elderly: Result from China Nutrition and Health Surveillance 2015–2017. Nutrients 2022, 14, 844. [Google Scholar] [CrossRef]
- Lao, X.Q.; Xu, Y.J.; Wong, M.C.; Zhang, Y.H.; Ma, W.J.; Xu, X.J.; Cai, Q.M.; Xu, H.F.; Wei, X.L.; Tang, J.L.; et al. Hypertension prevalence, awareness, treatment, control and associated factors in a developing southern Chinese population: Analysis of serial cross-sectional health survey data 2002–2010. Am. J. Hypertens 2013, 26, 1335–1345. [Google Scholar] [CrossRef] [Green Version]
- Maddock, J.; Ambrosini, G.L.; Griffin, J.L.; West, J.A.; Wong, A.; Hardy, R.; Ray, S. A dietary pattern derived using B-vitamins and its relationship with vascular markers over the life course. Clin. Nutr. 2019, 38, 1464–1473. [Google Scholar] [CrossRef] [Green Version]
- Seah, J.Y.H.; Ong, C.N.; Koh, W.P.; Yuan, J.M.; van Dam, R.M. A Dietary Pattern Derived from Reduced Rank Regression and Fatty Acid Biomarkers Is Associated with Lower Risk of Type 2 Diabetes and Coronary Artery Disease in Chinese Adults. J. Nutr. 2019, 149, 2001–2010. [Google Scholar] [CrossRef]
- Aleixandre, A.; Miguel, M. Dietary fiber and blood pressure control. Food Funct. 2016, 7, 1864–1871. [Google Scholar] [CrossRef]
- Anderson, J.W.; Baird, P.; Davis, R.H., Jr.; Ferreri, S.; Knudtson, M.; Koraym, A.; Waters, V.; Williams, C.L. Health benefits of dietary fiber. Nutr. Rev. 2009, 67, 188–205. [Google Scholar] [CrossRef]
- Cormick, G.; Ciapponi, A.; Cafferata, M.L.; Cormick, M.S.; Belizan, J.M. Calcium supplementation for prevention of primary hypertension. Cochrane Database Syst. Rev. 2021, 8, CD010037. [Google Scholar] [CrossRef]
- DiNicolantonio, J.J.; Liu, J.; O’Keefe, J.H. Thiamine and Cardiovascular Disease: A Literature Review. Prog. Cardiovasc. Dis. 2018, 61, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Duc, H.N.; Oh, H.; Yoon, I.M.; Kim, M.S. Association between levels of thiamine intake, diabetes, cardiovascular diseases and depression in Korea: A national cross-sectional study. J. Nutr. Sci. 2021, 10, e31. [Google Scholar] [CrossRef] [PubMed]
- Morelli, M.B.; Gambardella, J.; Castellanos, V.; Trimarco, V.; Santulli, G. Vitamin C and Cardiovascular Disease: An Update. Antioxidants 2020, 9, 1227. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Thakur, K.; Tomar, S.K.; Singh, A.K.; Mandal, S.; Arora, S. Riboflavin and health: A review of recent human research. Crit. Rev. Food Sci. Nutr. 2017, 57, 3650–3660. [Google Scholar] [CrossRef]
- Volpe, S.L. Magnesium in disease prevention and overall health. Adv. Nutr. 2013, 4, 378S–383S. [Google Scholar] [CrossRef]
- Weaver, C.M. Potassium and health. Adv. Nutr. 2013, 4, 368S–377S. [Google Scholar] [CrossRef]
- Miki, T.; Kochi, T.; Kuwahara, K.; Eguchi, M.; Kurotani, K.; Tsuruoka, H.; Ito, R.; Kabe, I.; Kawakami, N.; Mizoue, T.; et al. Dietary patterns derived by reduced rank regression (RRR) and depressive symptoms in Japanese employees: The Furukawa nutrition and health study. Psychiatry Res. 2015, 229, 214–219. [Google Scholar] [CrossRef]
- Filippou, C.D.; Tsioufis, C.P.; Thomopoulos, C.G.; Mihas, C.C.; Dimitriadis, K.S.; Sotiropoulou, L.I.; Chrysochoou, C.A.; Nihoyannopoulos, P.I.; Tousoulis, D.M. Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 1150–1160. [Google Scholar] [CrossRef]
- Xiao, M.L.; Lin, J.S.; Li, Y.H.; Liu, M.; Deng, Y.Y.; Wang, C.Y.; Chen, Y.M. Adherence to the Dietary Approaches to Stop Hypertension (DASH) diet is associated with lower presence of non-alcoholic fatty liver disease in middle-aged and elderly adults. Public Health Nutr. 2020, 23, 674–682. [Google Scholar] [CrossRef]
- Glenn, A.J.; Hernandez-Alonso, P.; Kendall, C.W.C.; Martinez-Gonzalez, M.A.; Corella, D.; Fito, M.; Martinez, J.A.; Alonso-Gomez, A.M.; Warnberg, J.; Vioque, J.; et al. Longitudinal changes in adherence to the portfolio and DASH dietary patterns and cardiometabolic risk factors in the PREDIMED-Plus study. Clin. Nutr. 2021, 40, 2825–2836. [Google Scholar] [CrossRef]
- Fan, M.; Lyu, J.; He, P. Chinese guidelines for data processing and analysis concerning the International Physical Activity Questionnaire. Zhonghua Liu Xing Bing Xue Za Zhi 2014, 35, 961–964. [Google Scholar]
- Yao, F.; Bo, Y.; Zhao, L.; Li, Y.; Ju, L.; Fang, H.; Piao, W.; Yu, D.; Lao, X. Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017. Nutrients 2021, 13, 4475. [Google Scholar] [CrossRef]
- Penney, T.L.; Jones, N.R.V.; Adams, J.; Maguire, E.R.; Burgoine, T.; Monsivais, P. Utilization of Away-From-Home Food Establishments, Dietary Approaches to Stop Hypertension Dietary Pattern, and Obesity. Am. J. Prev. Med. 2017, 53, e155–e163. [Google Scholar] [CrossRef] [Green Version]
- Cardoso, S.M.; Pereira, O.R.; Seca, A.M.; Pinto, D.C.; Silva, A.M. Seaweeds as Preventive Agents for Cardiovascular Diseases: From Nutrients to Functional Foods. Mar. Drugs 2015, 13, 6838–6865. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.H.; Yang, M.; Giovannucci, E.L.; Sun, Q.; Chavarro, J.E. Mushroom consumption, biomarkers, and risk of cardiovascular disease and type 2 diabetes: A prospective cohort study of US women and men. Am. J. Clin. Nutr. 2019, 110, 666–674. [Google Scholar] [CrossRef]
- Mohamed Yahaya, N.F.; Rahman, M.A.; Abdullah, N. Therapeutic potential of mushrooms in preventing and ameliorating hypertension. Trends Food Sci. Technol. 2014, 39, 104–115. [Google Scholar] [CrossRef]
- Ryu, B.; Kim, Y.S.; Jeon, Y.J. Seaweeds and Their Natural Products for Preventing Cardiovascular Associated Dysfunction. Mar. Drugs 2021, 19, 507. [Google Scholar] [CrossRef]
- Brown, E.S.; Allsopp, P.J.; Magee, P.J.; Gill, C.I.; Nitecki, S.; Strain, C.R.; McSorley, E.M. Seaweed and human health. Nutr. Rev. 2014, 72, 205–216. [Google Scholar] [CrossRef]
- Krittanawong, C.; Isath, A.; Hahn, J.; Wang, Z.; Fogg, S.E.; Bandyopadhyay, D.; Jneid, H.; Virani, S.S.; Tang, W.H.W. Mushroom Consumption and Cardiovascular Health: A Systematic Review. Am. J. Med. 2021, 134, 637–642.e632. [Google Scholar] [CrossRef]
- Rahman, M.A.; Abdullah, N.; Aminudin, N. Interpretation of mushroom as a common therapeutic agent for Alzheimer’s disease and cardiovascular diseases. Crit. Rev. Biotechnol. 2016, 36, 1131–1142. [Google Scholar] [CrossRef]
- Ma, G.; Du, H.; Hu, Q.; Yang, W.; Pei, F.; Xiao, H. Health benefits of edible mushroom polysaccharides and associated gut microbiota regulation. Crit. Rev. Food Sci. Nutr. 2021, Apr 1, 1–18. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Knuppel, S.; Iqbal, K.; Andriolo, V.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 793–803. [Google Scholar] [CrossRef]
- Drouin-Chartier, J.P.; Chen, S.; Li, Y.; Schwab, A.L.; Stampfer, M.J.; Sacks, F.M.; Rosner, B.; Willett, W.C.; Hu, F.B.; Bhupathiraju, S.N. Egg consumption and risk of cardiovascular disease: Three large prospective US cohort studies, systematic review, and updated meta-analysis. BMJ 2020, 368, m513. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.A.; Cai, H.; Yang, G.; Xu, W.H.; Zheng, W.; Li, H.; Gao, Y.T.; Xiang, Y.B.; Shu, X.O. Dietary patterns and blood pressure among middle-aged and elderly Chinese men in Shanghai. Br. J. Nutr. 2010, 104, 265–275. [Google Scholar] [CrossRef] [Green Version]
- Yu, G.; Fu, H.; Huang, W.; Zhang, N.; Deng, D.; Li, G.; Lei, H. A Dietary Pattern of Higher Fish, Egg, Milk, Nut, Vegetable and Fruit, and Lower Salt Intake Correlates With the Prevalence and Control of Hypertension. Am. J. Hypertens 2018, 31, 679–686. [Google Scholar] [CrossRef]
- Ruan, Y.; Huang, Y.; Zhang, Q.; Qin, S.; Du, X.; Sun, Y. Association between dietary patterns and hypertension among Han and multi-ethnic population in southwest China. BMC Public Health 2018, 18, 1106. [Google Scholar] [CrossRef] [Green Version]
- Shimazu, T.; Kuriyama, S.; Hozawa, A.; Ohmori, K.; Sato, Y.; Nakaya, N.; Nishino, Y.; Tsubono, Y.; Tsuji, I. Dietary patterns and cardiovascular disease mortality in Japan: A prospective cohort study. Int. J. Epidemiol. 2007, 36, 600–609. [Google Scholar] [CrossRef] [Green Version]
- Colafella, K.M.M.; Denton, K.M. Sex-specific differences in hypertension and associated cardiovascular disease. Nat. Rev. Nephrol. 2018, 14, 185–201. [Google Scholar] [CrossRef]
- Lima, R.; Wofford, M.; Reckelhoff, J.F. Hypertension in postmenopausal women. Curr. Hypertens Rep. 2012, 14, 254–260. [Google Scholar] [CrossRef] [Green Version]
- Song, J.J.; Ma, Z.; Wang, J.; Chen, L.X.; Zhong, J.C. Gender Differences in Hypertension. J. Cardiovasc. Transl. Res. 2020, 13, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Sebire, S.J.; Toumpakari, Z.; Turner, K.M.; Cooper, A.R.; Page, A.S.; Malpass, A.; Andrews, R.C. “I’ve made this my lifestyle now”: A prospective qualitative study of motivation for lifestyle change among people with newly diagnosed type two diabetes mellitus. BMC Public Health 2018, 18, 204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Danaei, G.; Finucane, M.M.; Lu, Y.; Singh, G.M.; Cowan, M.J.; Paciorek, C.J.; Lin, J.K.; Farzadfar, F.; Khang, Y.H.; Stevens, G.A.; et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011, 378, 31–40. [Google Scholar] [CrossRef]
- Huggins, C.E.; Margerison, C.; Worsley, A.; Nowson, C.A. Influence of dietary modifications on the blood pressure response to antihypertensive medication. Br. J. Nutr. 2011, 105, 248–255. [Google Scholar] [CrossRef] [Green Version]
- Park, K.; Cho, S.; Bower, J.K. Changes in Adherence to Non-Pharmacological Guidelines for Hypertension. PLoS ONE 2016, 11, e0161712. [Google Scholar] [CrossRef]

| Variables | Total | Quintile | ||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | ||
| Gender * | ||||||
| Male | 28,388 (45.97%) | 6498 (52.62%) | 6307 (51.07%) | 5953 (48.21%) | 5338 (43.22%) | 4292 (34.76%) |
| Female | 33,359 (54.03%) | 5851 (47.38%) | 6043 (48.93%) | 6396 (51.79%) | 7012 (56.78%) | 8057 (65.24%) |
| Age (years) * | ||||||
| 18~<30 | 5503 (8.91%) | 834 (6.75%) | 1093 (8.85%) | 1185 (9.6%) | 1249 (10.11%) | 1142 (9.25%) |
| 30~<45 | 13,537 (21.92%) | 2468 (19.99%) | 2674 (21.65%) | 2799 (22.67%) | 2854 (23.11%) | 2742 (22.2%) |
| 45~<60 | 23,176 (37.53%) | 4813 (38.97%) | 4773 (38.65%) | 4653 (37.68%) | 4640 (37.57%) | 4297 (34.8%) |
| ≥60 | 19,531 (31.63%) | 4234 (34.29%) | 3810 (30.85%) | 3712 (30.06%) | 3607 (29.21%) | 4168 (33.75%) |
| BMI * | ||||||
| Underweight | 2487 (4.03%) | 648 (5.25%) | 553 (4.48%) | 461 (3.73%) | 452 (3.66%) | 373 (3.02%) |
| Normal | 29,434 (47.67%) | 6388 (51.73%) | 6182 (50.06%) | 5884 (47.65%) | 5689 (46.06%) | 5291 (42.85%) |
| Overweight | 21,313 (34.52%) | 3949 (31.98%) | 4089 (33.11%) | 4263 (34.52%) | 4390 (35.55%) | 4622 (37.43%) |
| Obese | 8513 (13.79%) | 1364 (11.05%) | 1526 (12.36%) | 1741 (14.1%) | 1819 (14.73%) | 2063 (16.71%) |
| Living area * | ||||||
| Urban | 25,132 (40.7%) | 3121 (25.27%) | 3838 (31.08%) | 4653 (37.68%) | 5706 (46.2%) | 7814 (63.28%) |
| Rural | 36,615 (59.3%) | 9228 (74.73%) | 8512 (68.92%) | 7696 (62.32%) | 6644 (53.8%) | 4535 (36.72%) |
| Education * | ||||||
| Primary school or below | 29,899 (48.42%) | 7785 (63.04%) | 6786 (54.95%) | 6000 (48.59%) | 5259 (42.58%) | 4069 (32.95%) |
| Junior middle school | 18,945 (30.68%) | 3301 (26.73%) | 3742 (30.3%) | 4054 (32.83%) | 4067 (32.93%) | 3781 (30.62%) |
| High school or higher | 12,903 (20.9%) | 1263 (10.23%) | 1822 (14.75%) | 2295 (18.58%) | 3024 (24.49%) | 4499 (36.43%) |
| Income * | ||||||
| Not given | 9432 (15.28%) | 2185 (17.69%) | 2146 (17.38%) | 1886 (15.27%) | 1737 (14.06%) | 1478 (11.97%) |
| Low | 16,725 (27.09%) | 4248 (34.4%) | 3665 (29.68%) | 3401 (27.54%) | 3103 (25.13%) | 2308 (18.69%) |
| Medium | 21,946 (35.54%) | 4169 (33.76%) | 4437 (35.93%) | 4627 (37.47%) | 4476 (36.24%) | 4237 (34.31%) |
| High | 13,644 (22.1%) | 1747 (14.15%) | 2102 (17.02%) | 2435 (19.72%) | 3034 (24.57%) | 4326 (35.03%) |
| Marital status * | ||||||
| Married | 56,609 (91.68%) | 11,245 (91.06%) | 11,291 (91.43%) | 11,378 (92.14%) | 11,372 (92.08%) | 11,323 (91.69%) |
| Other status | 5138 (8.32%) | 1104 (8.94%) | 1059 (8.57%) | 971 (7.86%) | 978 (7.92%) | 1026 (8.31%) |
| Current smoker * | ||||||
| No | 45,746 (74.09%) | 8335 (67.5%) | 8613 (69.74%) | 9005 (72.92%) | 9486 (76.81%) | 10,307 (83.46%) |
| Yes | 16,001 (25.91%) | 4014 (32.5%) | 3737 (30.26%) | 3344 (27.08%) | 2864 (23.19%) | 2042 (16.54%) |
| Second-hand smoking * | ||||||
| No | 31,815 (51.52%) | 6079 (49.23%) | 5942 (48.11%) | 6107 (49.45%) | 6487 (52.53%) | 7200 (58.3%) |
| Yes | 29,932 (48.48%) | 6270 (50.77%) | 6408 (51.89%) | 6242 (50.55%) | 5863 (47.47%) | 5149 (41.7%) |
| Excessive alcohol drinking * | ||||||
| No | 55,451 (89.8%) | 10,447 (84.6%) | 10,788 (87.35%) | 11,081 (89.73%) | 11,375 (92.11%) | 11,760 (95.23%) |
| Yes | 6296 (10.2%) | 1902 (15.4%) | 1562 (12.65%) | 1268 (10.27%) | 975 (7.89%) | 589 (4.77%) |
| Physical activity * | ||||||
| Low | 14,590 (23.63%) | 3508 (28.41%) | 3004 (24.32%) | 2875 (23.28%) | 2765 (22.39%) | 2438 (19.74%) |
| Medium | 15,320 (24.81%) | 2492 (20.18%) | 2636 (21.34%) | 2999 (24.29%) | 3271 (26.49%) | 3922 (31.76%) |
| High | 31,837 (51.56%) | 6349 (51.41%) | 6710 (54.33%) | 6475 (52.43%) | 6314 (51.13%) | 5989 (48.5%) |
| Sedentary behavior (h) * | ||||||
| <2 | 7817 (12.66%) | 1908 (15.45%) | 1584 (12.83%) | 1479 (11.98%) | 1483 (12.01%) | 1363 (11.04%) |
| 2~3 | 23,386 (37.87%) | 5036 (40.78%) | 4908 (39.74%) | 4715 (38.18%) | 4464 (36.15%) | 4263 (34.52%) |
| ≥4 | 30,544 (49.47%) | 5405 (43.77%) | 5858 (47.43%) | 6155 (49.84%) | 6403 (51.85%) | 6723 (54.44%) |
| Sleep duration (h) * | ||||||
| <7 | 12,411 (20.1%) | 2571 (20.82%) | 2389 (19.34%) | 2366 (19.16%) | 2509 (20.32%) | 2576 (20.86%) |
| 7~8 | 35,926 (58.18%) | 6650 (53.85%) | 7166 (58.02%) | 7291 (59.04%) | 7269 (58.86%) | 7550 (61.14%) |
| ≥9 | 13,410 (21.72%) | 3128 (25.33%) | 2795 (22.63%) | 2692 (21.8%) | 2572 (20.83%) | 2223 (18%) |
| Medical examination within one year * | ||||||
| No | 46,303 (74.99%) | 10,098 (81.77%) | 9812 (79.45%) | 9427 (76.34%) | 8990 (72.79%) | 7976 (64.59%) |
| Yes | 15,444 (25.01%) | 2251 (18.23%) | 2538 (20.55%) | 2922 (23.66%) | 3360 (27.21%) | 4373 (35.41%) |
| Family history of HTN * | ||||||
| No | 42,328 (68.55%) | 9447 (76.5%) | 8870 (71.82%) | 8527 (69.05%) | 8024 (64.97%) | 7460 (60.41%) |
| Yes | 19,419 (31.45%) | 2902 (23.5%) | 3480 (28.18%) | 3822 (30.95%) | 4326 (35.03%) | 4889 (39.59%) |
| HTN * | ||||||
| No | 37,482 (60.7%) | 7224 (58.5%) | 7457 (60.38%) | 7529 (60.97%) | 7700 (62.35%) | 7572 (61.32%) |
| Yes | 24,265 (39.3%) | 5125 (41.5%) | 4893 (39.62%) | 4820 (39.03%) | 4650 (37.65%) | 4777 (38.68%) |
| DM * | ||||||
| No | 56,478 (91.47%) | 11,454 (92.75%) | 11,429 (92.54%) | 11,306 (91.55%) | 11,302 (91.51%) | 10,987 (88.97%) |
| Yes | 5269 (8.53%) | 895 (7.25%) | 921 (7.46%) | 1043 (8.45%) | 1048 (8.49%) | 1362 (11.03%) |
| Hyperlipidemic * | ||||||
| No | 38,221 (61.9%) | 7864 (63.68%) | 7831 (63.41%) | 7697 (62.33%) | 7580 (61.38%) | 7249 (58.7%) |
| Yes | 23,526 (38.1%) | 4485 (36.32%) | 4519 (36.59%) | 4652 (37.67%) | 4770 (38.62%) | 5100 (41.3%) |
| DASH-score * | 24 (22, 27) | 20 (18, 22) | 23 (20, 25) | 24 (22, 26) | 26 (23, 28) | 28 (26, 31) |
| SBP * | 131.33 (119.67, 146.33) | 133 (121, 148.33) | 132 (120.33, 147) | 131 (120, 146) | 130.33 (118.67, 144.67) | 130 (118.33, 144.67) |
| DBP * | 78.33 (71.33, 86) | 79 (71.67, 86.67) | 78.67 (71.67, 86.33) | 78.67 (71.67, 86) | 78 (71, 85.33) | 77.33 (70.33, 84.67) |
| Dietary Pattern | Quintile | N | No. of Cases | OR (95% CI) * | ||
|---|---|---|---|---|---|---|
| Model I † | Model II ‡ | Model III § | ||||
| BBP diet | Q1 | 12,349 | 5125 | reference | reference | reference |
| Q2 | 12,350 | 4893 | 0.925 (0.879, 0.973) | 0.957 (0.904, 1.013) | 0.968 (0.913, 1.025) | |
| Q3 | 12,349 | 4820 | 0.902 (0.858, 0.949) | 0.915 (0.864, 0.969) | 0.935 (0.882, 0.992) | |
| Q4 | 12,350 | 4650 | 0.851 (0.809, 0.896) | 0.860 (0.812, 0.911) | 0.885 (0.834, 0.939) | |
| Q5 | 12,349 | 4777 | 0.889 (0.845, 0.936) | 0.791 (0.747, 0.838) | 0.842 (0.791, 0.896) | |
| p for trend | <0.0001 | <0.0001 | <0.0001 | |||
| DASH diet | Q1 | 12,298 | 4673 | reference | reference | reference |
| Q2 | 12,843 | 5023 | 1.048 (0.996, 1.103) | 1.001 (0.945, 1.060) | 1.006 (0.949, 1.067) | |
| Q3 | 13,487 | 5277 | 1.049 (0.997, 1.103) | 0.956 (0.903, 1.011) | 0.964 (0.909, 1.022) | |
| Q4 | 11,257 | 4450 | 1.067 (1.012, 1.124) | 0.981 (0.924, 1.041) | 1.005 (0.945, 1.07) | |
| Q5 | 11,862 | 4842 | 1.125 (1.069, 1.185) | 0.852 (0.803, 0.903) | 0.912 (0.854, 0.973) | |
| p for trend | <0.0001 | <0.0001 | 0.0063 | |||
| Dietary Pattern | Quintile | N | No. of Well-Controlled | OR (95% CI) * | ||
|---|---|---|---|---|---|---|
| Model I † | Model II ‡ | Model III § | ||||
| BBP diet | Q1 | 1183 | 241 | reference | reference | reference |
| Q2 | 1156 | 267 | 0.852 (0.700, 1.037) | 0.855 (0.702, 1.043) | 0.903 (0.739, 1.104) | |
| Q3 | 1276 | 306 | 0.811 (0.670, 0.982) | 0.79 (0.652, 0.958) | 0.89 (0.731, 1.084) | |
| Q4 | 1426 | 360 | 0.758 (0.630, 0.912) | 0.736 (0.611, 0.887) | 0.889 (0.732, 1.078) | |
| Q5 | 1712 | 517 | 0.591 (0.496, 0.705) | 0.548 (0.459, 0.654) | 0.762 (0.629, 0.924) | |
| p for trend | <0.0001 | <0.0001 | 0.002 | |||
| DASH diet | Q1 | 999 | 191 | reference | reference | reference |
| Q2 | 1302 | 295 | 0.807 (0.658, 0.990) | 0.782 (0.636, 0.960) | 0.829 (0.673, 1.021) | |
| Q3 | 1402 | 353 | 0.703 (0.576, 0.857) | 0.701 (0.574, 0.856) | 0.795 (0.647, 0.976) | |
| Q4 | 1336 | 345 | 0.679 (0.556, 0.829) | 0.651 (0.532, 0.796) | 0.797 (0.646, 0.983) | |
| Q5 | 1714 | 507 | 0.563 (0.466, 0.680) | 0.532 (0.440, 0.644) | 0.76 (0.616, 0.938) | |
| p for trend | <0.0001 | <0.0001 | 0.009 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; Yu, D.; Piao, W.; Huang, K.; Zhao, L. Nutrient-Derived Beneficial for Blood Pressure Dietary Pattern Associated with Hypertension Prevention and Control: Based on China Nutrition and Health Surveillance 2015–2017. Nutrients 2022, 14, 3108. https://doi.org/10.3390/nu14153108
Yang Y, Yu D, Piao W, Huang K, Zhao L. Nutrient-Derived Beneficial for Blood Pressure Dietary Pattern Associated with Hypertension Prevention and Control: Based on China Nutrition and Health Surveillance 2015–2017. Nutrients. 2022; 14(15):3108. https://doi.org/10.3390/nu14153108
Chicago/Turabian StyleYang, Yuxiang, Dongmei Yu, Wei Piao, Kun Huang, and Liyun Zhao. 2022. "Nutrient-Derived Beneficial for Blood Pressure Dietary Pattern Associated with Hypertension Prevention and Control: Based on China Nutrition and Health Surveillance 2015–2017" Nutrients 14, no. 15: 3108. https://doi.org/10.3390/nu14153108






