Predictors of Minimum Acceptable Diet among Children Aged 6–23 Months in Nepal: A Multilevel Analysis of Nepal Multiple Indicator Cluster Survey 2019
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
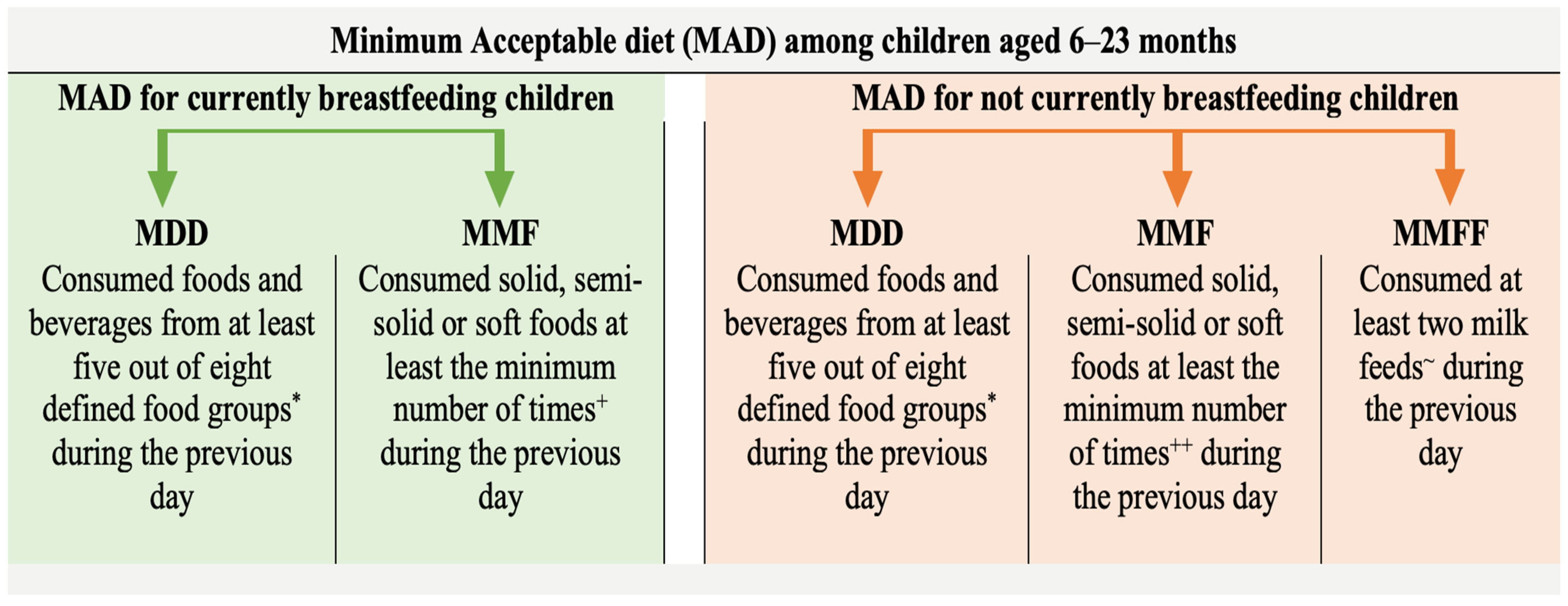
2.2. Outcome Variable
2.3. Explanatory Variables
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNICEF; WHO; World Bank Group. Levels and Trends in Child Malnutrition. 2021. Available online: https://www.who.int/publications/i/item/9789240025257 (accessed on 5 July 2022).
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-Mcgregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Chitekwe, S.; Torlesse, H.; Aguayo, V.M. Nutrition in Nepal: Three decades of commitment to children and women. Matern. Child Nutr. 2022, 18, e13229. [Google Scholar] [CrossRef] [PubMed]
- Karn, S.; Adhikari, D.P.; Paudyal, N.; Aryal, B.; Adhikari, R.K.; Steffen, M.M. Child undernutrition and feeding practices in Nepal: Trends, inequities, and determinants. DHS Furth. Anal. Rep. 2019, 122, xvi + 66. [Google Scholar]
- Cental Bureau of Statistics. Nepal Multiple Indicator Cluster Survey 2019, Survey Findings Report; Cental Bureau of Statistics: Kathmandu, Nepal, 2020.
- World Health Organization; United Nations Children’s Fund. Indicators for Assessing Infant and Young Child Feeding Practices: Definitions and Measurement Methods; World Health Organization: Geneva, Switzerland; United Nations Children’s Fund: New York, NY, USA, 2021.
- WHO; UNICEF; USAID; AED; FANTA; UCDAVIS; IFPRI. Indicators for Assessing Infant and Young Child Feeding Practices: Conclusions of a Consensus Meeting Held 6–8 November 2007 in Washington D.C., USA; WHO: Geneva, Switzerland, 2008; Volume 8.
- Ministry of Health Nepal; New Era; ICF. Nepal Demographic and Health Survey 2016. 2017. Available online: https://dhsprogram.com/publications/publication-fr336-dhs-final-reports.cfm (accessed on 21 June 2022).
- Marriott, B.P.; White, A.; Hadden, L.; Davies, J.C.; Wallingford, J.C. World Health Organization (WHO) infant and young child feeding indicators: Associations with growth measures in 14 low-income countries. Matern. Child Nutr. 2012, 8, 354–370. [Google Scholar] [CrossRef]
- Wrottesley, S.V.; Lamper, C.; Pisa, P.T. Review of the importance of nutrition during the first 1000 days: Maternal nutritional status and its associations with fetal growth and birth, neonatal and infant outcomes among African women. J. Dev. Orig. Health Dis. 2016, 7, 144–162. [Google Scholar] [CrossRef]
- Adhikari, N.; Acharya, K.; Upadhya, D.P.; Pathak, S.; Pokharel, S.; Pradhan, P.M.S. Infant and young child feeding practices and its associated factors among mothers of under two years children in a western hilly region of Nepal. PLoS ONE 2021, 16, e0261301. [Google Scholar] [CrossRef]
- Cunningham, K.; Nagle, D.; Gupta, P.; Adhikari, R.P.; Singh, S. Associations between parents’ exposure to a multisectoral programme and infant and young child feeding practices in Nepal. Matern. Child Nutr. 2021, 17, e13143. [Google Scholar] [CrossRef]
- Na, M.; Aguayo, V.M.; Arimond, M.; Dahal, P.; Lamichhane, B.; Pokharel, R.; Chitekwe, S.; Stewart, C.P. Trends and predictors of appropriate complementary feeding practices in Nepal: An analysis of national household survey data collected between 2001 and 2014. Matern. Child Nutr. 2018, 14, e12564. [Google Scholar] [CrossRef]
- Khanal, V.; Sauer, K.; Zhao, Y. Determinants of complementary feeding practices among Nepalese children aged 6-23 months: Findings from demographic and health survey 2011. BMC Pediatr. 2013, 13, 131. [Google Scholar] [CrossRef]
- Joshi, N.; Agho, K.E.; Dibley, M.J.; Senarath, U.; Tiwari, K. Determinants of inappropriate complementary feeding practices in young children in Nepal: Secondary data analysis of Demographic and Health Survey 2006. Matern. Child Nutr. 2012, 8, 45–59. [Google Scholar] [CrossRef]
- Pradhan, R.; Shrestha, A. Ethnic and Caste Diversity: Implications for Development; Asian Development Bank: Mandaluyong, Philippines, 2005; pp. 9–11. [Google Scholar]
- United Nations Chidren’s Fund (UNICEF) Fed to Fail? The Crisis of Children’s Diets in Early Life. 2021 Child Nutrition Report. 2021. Available online: https://www.unicef.org/reports/fed-to-fail-child-nutrition (accessed on 8 June 2022).
- Tariqujjaman, M.; Hasan, M.M.; Mahfuz, M.; Ahmed, T.; Hossain, M. Between and Within-Country Variations in Infant and Young Child Feeding Practices in South Asia. Int. J. Environ. Res. Public Health 2022, 19, 4350. [Google Scholar] [CrossRef] [PubMed]
- Government of Nepal. Sustainable Development Goals Status and Roadmap: 2016–2030; Government of Nepal: Kathmandu, Nepal, 2017.
- Department of Health Services, Ministry of Health and population. Annual Report 2076/77; Department of Health Services: Kathmandu, Nepal, 2020.
- Joshi, B.G.; Chitekwe, S. A Nutrition Story of Change from Nepal. SUN Movement: Geneva, Switzerland. Available online: https://scalingupnutrition.org/news/a-nutrition-story-of-change-from-nepal/ (accessed on 7 March 2022).
- Senarath, U.; Agho, K.E.; Akram, D.E.S.; Godakandage, S.S.P.; Hazir, T.; Jayawickrama, H.; Joshi, N.; Kabir, I.; Khanam, M.; Patel, A.; et al. Comparisons of complementary feeding indicators and associated factors in children aged 6–23 months across five South Asian countries. Matern. Child Nutr. 2012, 8, 89–106. [Google Scholar] [CrossRef]
- Locks, L.M.; Pandey, P.R.; Osei, A.K.; Spiro, D.S.; Adhikari, D.P.; Haselow, N.J.; Quinn, V.J.; Nielsen, J.N. Using formative research to design a context-specific behaviour change strategy to improve infant and young child feeding practices and nutrition in Nepal. Matern. Child Nutr. 2015, 11, 882–896. [Google Scholar] [CrossRef] [PubMed]
- Dharel, D.; Bhattarai, A.; Paudel, Y.R.; Acharya, P.; Acharya, K. Higher rates of early initiation of breastfeeding associated with health facility delivery in Nepal. Eur. J. Public Health 2020, 30, ckaa165.1121. [Google Scholar] [CrossRef]
- Shen, X.; Lin, S.; Li, H.; Amaerjiang, N.; Shu, W.; Li, M.; Xiao, H.; Segura-Pérez, S.; Pérez-Escamilla, R.; Fan, X.; et al. Timing of Breastfeeding Initiation Mediates the Association between Delivery Mode, Source of Breastfeeding Education, and Postpartum Depression Symptoms. Nutrients 2022, 14, 2959. [Google Scholar] [CrossRef]
- Joshi, G.; Joshi, N. Determinants of household food security in the eastern region of Nepal. SAARC J. Agric. 2017, 14, 174–188. [Google Scholar] [CrossRef]
- Worku, M.G.; Alamneh, T.S.; Tesema, G.A.; Alem, A.Z.; Tessema, Z.T.; Liyew, A.M.; Yeshaw, Y.; Teshale, A.B. Minimum acceptable diet feeding practice and associated factors among children aged 6–23 months in east Africa: A multilevel binary logistic regression analysis of 2008–2018 demographic health survey data. Arch. Public Health 2022, 80, 127. [Google Scholar] [CrossRef]
- Tassew, A.A.; Tekle, D.Y.; Belachew, A.B.; Adhena, B.M. Factors affecting feeding 6–23 months age children according to minimum acceptable diet in Ethiopia: A multilevel analysis of the Ethiopian Demographic Health Survey. PLoS ONE 2019, 14, e0203098. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Etowa, J.; Ghose, B.; Tang, S.; Ji, L.; Huang, R. Association between mass media use and maternal healthcare service utilisation in malawi. J. Multidiscip. Healthc. 2021, 14, 1159–1167. [Google Scholar] [CrossRef]
- Sserwanja, Q.; Mutisya, L.M.; Musaba, M.W. Exposure to different types of mass media and timing of antenatal care initiation: Insights from the 2016 Uganda Demographic and Health Survey. BMC Women’s Health 2022, 22, 10. [Google Scholar] [CrossRef]
- Fatema, K.; Lariscy, J.T. Mass media exposure and maternal healthcare utilization in South Asia. SSM-Popul. Health 2020, 11, 100614. [Google Scholar] [CrossRef] [PubMed]
- USAID Nepal SUAAHARA II. “Good Nutrition” Program Year Two Work Plan. 2017. Available online: https://pdf.usaid.gov/pdf_docs/PA00TDB2.pdf (accessed on 1 August 2022).
- Ghimire, U.; Manandhar, J.; Gautam, A.; Tuladhar, S.; Prasai, Y.; Gebreselassie, T. Inequalities in Health Outcomes and Access to Services by Caste/Ethnicity, Province, and Wealth Quintile in Nepal; Furth. Anal. Reports No. 117; DHS Program: Rockville, MD, USA, 2019. [Google Scholar]
- National Planning Commission Government of Nepal. Multidimensional Poverty Index; National Planning Commission Government of Nepal: Kathmandu, Nepal, 2021.

| Variables | Definition of Variables | Measurements |
|---|---|---|
| Child’s characteristics | ||
| Age | Age of child in completed months | 6–12 months, 13–18 months, 19–23 months |
| Sex | Sex of child | Boy, girl |
| Early initiation of breastfeeding | Child put to the breast within one hour of birth | Yes, no |
| Currently breastfeeding | Child breastfed on the previous day | Yes, no |
| Episode of diarrhea | Child had an episode of diarrhea within two weeks preceding the survey | Yes, no |
| Presence of sibling aged under five years | Child has a sibling aged under five years | Yes, no |
| Mother’s characteristics | ||
| Age | Age of mother in completed years | 15 to 49 years (Continuous numeric variable) |
| Education | Highest class attended | Grade 0–14 (0 indicates illiterate or no formal education 14 indicates Master’s degree or above) (Discrete numeric variable) |
| Media exposure | Mother listens to radio or reads newspaper or watches television at least once a week | Yes, no |
| Utilization of maternal health services | Mother had four antenatal visits and institutional delivery | Yes, no |
| Household characteristics | ||
| Raw household wealth score | A composite score generated by principal component analysis using information on the ownership of consumer goods, dwelling characteristics, water and sanitation, and other assets and durables that are related to the household’s wealth | −1.89 to 2.42 (Continuous numeric variable) |
| Ethnicity/Caste | Ethnicity/caste of household members | Relatively advantaged: Brahmin, Chhetri, Newar, Gurung, Magar and Thakali, relatively disadvantaged: Others |
| Area characteristics | ||
| Settlement | Level of urbanization | Urban (Metropolitan city, sub-metropolitan city, municipality), rural: Rural municipality |
| Province | Province where household is located | Province 1, Madhesh Province, Bagmati Province, Gandaki Province, Lumbini Province, Karnali Province, Sudoorpaschim Province |
| Characteristics | Number (n = 1930) | Percentage (%) |
|---|---|---|
| Age of child | ||
| 6–12 months | 642 | 36.4 |
| 13–18 months | 625 | 30.5 |
| 19–23 months | 663 | 33.1 |
| Sex of child | ||
| Girl | 869 | 45.8 |
| Boy | 1061 | 54.2 |
| Early initiation of breastfeeding | ||
| No | 1129 | 58.5 |
| Yes | 801 | 41.5 |
| Currently breastfeeding | ||
| No | 105 | 6.4 |
| Yes | 1825 | 93.6 |
| Diarrhea in past two weeks | ||
| Yes | 274 | 13.1 |
| No | 1656 | 86.9 |
| Has siblings aged under 5 years | ||
| Yes | 739 | 38.0 |
| No | 1191 | 62.0 |
| Mother’s media exposure | ||
| No | 740 | 37.3 |
| Yes | 1190 | 62.7 |
| Utilization of maternal health services | ||
| <4 ANC or no institutional delivery | 623 | 33.7 |
| 4 ANC and institutional delivery | 1307 | 66.3 |
| Ethnicity/caste | ||
| Relatively Advantaged | 791 | 36.8 |
| Relatively disadvantaged | 1139 | 63.2 |
| Settlement | ||
| Rural | 848 | 33.9 |
| Urban | 1082 | 66.1 |
| Province | ||
| Province 1 | 282 | 15.7 |
| Madhesh Province | 296 | 21.4 |
| Bagmati Province | 359 | 20.4 |
| Gandaki Province | 234 | 8.1 |
| Lumbini Province | 302 | 18.8 |
| Karnali province | 218 | 6.3 |
| Sudoorpaschim Province | 239 | 9.2 |
| Characteristics | Minimum Acceptable Diet | Crude Odds Ratio | |
|---|---|---|---|
| No (n = 1346, %) | Yes (n = 578, %) | OR (95% CI) | |
| Age of child | |||
| 6–12 months | 551 (78.6) | 150 (21.4) | Ref. |
| 13–18 months | 391 (66.5%) | 197 (33.5%) | 1.85 (1.34, 2.57) *** |
| 19–23 months | 405 (63.6%) | 232 (36.4%) | 2.1 (1.56, 2.83) *** |
| Sex of child | |||
| Female | 634 (71.9%) | 248 (28.1%) | Ref. |
| Male | 712 (68.3%) | 330 (31.7%) | 1.18 (0.95, 1.48) |
| Early initiation of breastfeeding | |||
| No | 789 (70.0%) | 338 (30.0%) | Ref. |
| Yes | 557 (69.9%) | 241 (30.1%) | 1.01 (0.79, 1.28) |
| Currently breastfeeding | |||
| No | 108 (87.0%) | 16 (13.0%) | Ref. |
| Yes | 1238 (68.8%) | 562 (31.2%) | 3.05 (1.03, 9.04) * |
| Diarrhea in past two weeks | |||
| Yes | 170 (67.2%) | 83 (32.8%) | Ref. |
| No | 1176 (70.4%) | 495 (29.6%) | 0.86 (0.63, 1.18) |
| Has siblings aged under 5 years | |||
| Yes | 564 (77.1%) | 167 (22.9%) | Ref. |
| No | 782 (65.6%) | 411 (34.4%) | 1.77(1.36, 2.30) *** |
| Age of mother [Mean (SD)] | 25.93 (5.52) | 25.51 (5.10) | 0.99 (0.96, 1.01) |
| Education of mother [Mean (SD)] | 6.62 (4.69) | 8.26 (4.12) | 1.09 (1.06, 1.12) *** |
| Mother’s media exposure | |||
| Yes | 567 (79.0%) | 150 (21.0%) | Ref. |
| No | 779 (64.5%) | 428 (35.5%) | 2.07 (1.62, 2.65) *** |
| Utilization of maternal health services | |||
| <4 ANC or no institutional delivery | 494 (76.1%) | 155 (23.9%) | Ref. |
| 4 ANC and institutional delivery | 852 (66.8%) | 423 (33.2%) | 1.58 (1.19, 2.09) *** |
| Combined household wealth score [Mean (SD)] | 0.04 (0.95) | 0.23 (0.99) | 1.23 (1.07, 1.41) *** |
| Ethnicity/caste | |||
| Relatively advantaged | 438 (61.8%) | 270 (38.2%) | Ref. |
| Relatively disadvantaged | 908 (74.7%) | 308 (25.3%) | 0.55 (0.42, 0.72) *** |
| Settlement | |||
| Urban | 898 (70.5%) | 375 (29.5%) | Ref. |
| Rural | 448 (68.8%) | 203 (31.2%) | 1.08 (0.84, 1.40) |
| Province | |||
| Province 1 | 201 (66.4%) | 102 (33.6%) | Ref. |
| Madhesh Province | 323 (78.3%) | 89 (21.7%) | 0.55 (0.35, 0.85) ** |
| Bagmati Province | 243 (61.7%) | 151 (38.3%) | 1.23 (0.82, 1.84) |
| Gandaki Province | 94 (60.2%) | 62 (39.8%) | 1.31(0.86, 1.98) |
| Lumbini Province | 266 (73.4%) | 96 (26.6%) | 0.71(0.46, 1.10) |
| Karnali Province | 94 (77.6%) | 27 (22.4%) | 0.57 (0.34, 0.96) * |
| Sudoorpaschim Province | 126 (71.3%) | 51 (28.7%) | 0.79 (0.52, 1.22) |
| Predictors | Model 0 | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | ||
| Age: 13–18 months (Ref: 6–12 months) | 2.15 *** | 1.61, 2.85 | 2.36 *** | 1.76, 3.15 | 2.37 *** | 1.77, 3.17 | |
| Age: 19–23 months (Ref: 6–12 months) | 2.34 *** | 1.77, 3.10 | 2.60 *** | 1.95, 3.46 | 2.60 *** | 1.95, 3.47 | |
| Sex of children: Male (Ref: Female) | 1.17 | 0.93, 1.47 | 1.14 | 0.90, 1.43 | 1.15 | 0.91, 1.45 | |
| Early initiation of breastfeeding: Yes (Ref: No) | 1.21 | 0.95, 1.53 | 1.28 * | 1.01, 1.63 | 1.34 * | 1.05, 1.72 | |
| Currently breastfeeding: Yes (Ref: No) | 3.94 *** | 2.12, 7.29 | 4.26 *** | 2.28, 7.93 | 4.13 *** | 2.21, 7.69 | |
| Diarrhea in past two weeks: No (Ref: Yes) | 0.83 | 0.59, 1.16 | 0.79 | 0.56, 1.12 | 0.79 | 0.56, 1.11 | |
| Having siblings aged U5: No (Ref: Yes) | 1.72 *** | 1.34, 2.22 | 1.42 ** | 1.10, 1.84 | 1.33 * | 1.03, 1.73 | |
| Age of mother | 0.98 * | 0.95, 1.00 | 0.97 * | 0.95, 1.00 | |||
| Mother’s education | 1.04 * | 1.01, 1.08 | 1.04 * | 1.00, 1.08 | |||
| Media exposure: Yes (Ref: No) | 1.71 *** | 1.29, 2.28 | 1.66 *** | 1.24, 2.21 | |||
| Health service utilization: 4 ANC and institutional delivery (Ref: Otherwise) | 1.15 | 0.86, 1.54 | 1.14 | 0.85, 1.53 | |||
| Combined household wealth score | 1.07 | 0.91, 1.25 | 1.09 | 0.90, 1.32 | |||
| Ethnicity/caste: Relatively disadvantaged (Ref: Relatively advantaged) | 0.70 ** | 0.53, 0.91 | 0.71 * | 0.53, 0.94 | |||
| Settlement: Rural (Ref: Urban) | 1.45 * | 1.06, 2.00 | |||||
| Province: Province 1 (Ref: Bagmati Province) | 0.99 | 0.61, 1.59 | |||||
| Province: Madhesh Province (Ref: Bagmati) | 0.61 * | 0.37, 1.00 | |||||
| Province: Gandaki Province (Ref: Bagmati) | 1.00 | 0.59, 1.69 | |||||
| Province: Lumbini Province (Ref: Bagmati) | 0.66 | 0.41, 1.05 | |||||
| Province: Karnali Province (Ref: Bagmati) | 0.53 | 0.26, 1.05 | |||||
| Province: Sudoorpaschim Province (Ref: Bagmati) | 0.62 | 0.35, 1.11 | |||||
| Random Effects | |||||||
| Intraclass correlation (%) | 20% | 18% | 17% | 17% | |||
| Marginal R2/Conditional R2 | 0.000/0.196 | 0.133/0.286 | 0.140/0.289 | 0.159/0.300 | |||
| AIC | 2291 | 2164 | 2161 | 2159 | |||
| BIC | 2303 | 2236 | 2244 | 2281 | |||
| −2 Log Likelihood | −1144 (Ref.) | −1069 | −1065 | −1057 | |||
| Deviance | 2287 | 2138 | 2131 | 2115 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sapkota, S.; Thapa, B.; Gyawali, A.; Hu, Y. Predictors of Minimum Acceptable Diet among Children Aged 6–23 Months in Nepal: A Multilevel Analysis of Nepal Multiple Indicator Cluster Survey 2019. Nutrients 2022, 14, 3669. https://doi.org/10.3390/nu14173669
Sapkota S, Thapa B, Gyawali A, Hu Y. Predictors of Minimum Acceptable Diet among Children Aged 6–23 Months in Nepal: A Multilevel Analysis of Nepal Multiple Indicator Cluster Survey 2019. Nutrients. 2022; 14(17):3669. https://doi.org/10.3390/nu14173669
Chicago/Turabian StyleSapkota, Suman, Bipin Thapa, Amrita Gyawali, and Yifei Hu. 2022. "Predictors of Minimum Acceptable Diet among Children Aged 6–23 Months in Nepal: A Multilevel Analysis of Nepal Multiple Indicator Cluster Survey 2019" Nutrients 14, no. 17: 3669. https://doi.org/10.3390/nu14173669
APA StyleSapkota, S., Thapa, B., Gyawali, A., & Hu, Y. (2022). Predictors of Minimum Acceptable Diet among Children Aged 6–23 Months in Nepal: A Multilevel Analysis of Nepal Multiple Indicator Cluster Survey 2019. Nutrients, 14(17), 3669. https://doi.org/10.3390/nu14173669









