Abstract
We conducted a systematic review of cohort studies comparing the risk of heart failure in people with differing metabolic health and obesity statuses. We searched three electronic databases (PubMed, Web of Science, Scopus), where the studies of the relationships of metabolic health and obesity statuses with heart failure were included. Fixed-effects or random-effects models were used to estimate the summary relative risks [RRs]. Ten cohort studies were selected. Compared with individuals with normal metabolic health and body mass, the pooled RRs (95% confidence intervals) for heart failure were 1.23 (1.17, 1.29) for metabolic healthy overweight individuals, 1.52 (1.40, 1.64) for metabolic healthy individuals with obesity, 1.56 (1.30, 1.87) for metabolically unhealthy normal-weight individuals, 1.75 (1.55, 1.98) for metabolically unhealthy overweight individuals, and 2.28 (1.96, 2.66) for metabolic unhealthy individuals with obesity. A sensitivity analysis suggested that no single study had a substantial effect on the results. The Egger’s and Begg’s tests showed no evidence of publication bias. People with overweight or obesity were at a higher risk of heart failure, even if metabolically healthy. In addition, compared with metabolically healthy normal-weight individuals; metabolically unhealthy normal-weight individuals, and those with overweight or and obesity, were at higher risk of heart failure.
1. Introduction
Heart failure has become a global public health concern, with an estimated 64.34 million people being affected [1]. Heart failure is associated with high morbidity and mortality, implying a large clinical burden and necessitating high healthcare expenditure [2,3]. Obesity is often accompanied by metabolic disorders, including diabetes, hypertension, and dyslipidemia, which play important roles in the pathogenesis and development of heart failure [4,5,6,7,8]. There is also a subset of individuals with obesity, but without metabolic disorders, who are referred to as having “metabolically healthy obesity” (MHO). However, recently, MHO has received much clinical and public health attention, because it is not considered to be a benign condition [9,10]. Individuals with MHO may be at a higher risk of developing cardiometabolic diseases than healthy lean people [11,12], and the study of MHO may also provide new perspectives regarding the mechanisms linking obesity to metabolic and cardiovascular abnormalities [11,13].
The relationships of obesity status and metabolic health status with the risk of heart failure have not been thoroughly evaluated. A cohort study by Voulgari et al. published in 2011 was the first on this topic. They reported that compared metabolically healthy normal-weight individuals, metabolically unhealthy normal-weight individuals are at a higher risk of heart failure, whereas MHO individuals are at a non-significantly lower risk [14]. However, two other cohort studies showed that the risk of heart failure is higher in people with obesity, regardless of their metabolic health status [15,16]. A meta-analysis published in 2019 summarized the results of these two studies and found that MHO or metabolically healthy overweight status is not associated with the risk of heart failure [17]. Since then, the results of several cohort studies have been published, but the results have been inconsistent. Other studies have shown that compared with metabolically healthy individuals without obesity, MHO is associated with a higher risk of heart failure [18,19,20,21,22]. However, a recent cohort study showed that compared with metabolically healthy normal-weight individuals, there is a higher risk of heart failure in metabolically unhealthy normal-weight individuals and metabolically unhealthy individuals with overweight or obesity, but not in those with MHO [23].
Given the accumulating evidence and inconsistency of the results published to date, we aimed to conduct a systematic review and meta-analysis to compare the risks of heart failure among people with differing metabolic health and obesity statuses.
2. Materials and Methods
2.1. Literature Search
We performed a meta-analysis that was designed, performed, and reported according to the Meta-analyses Of Observational Studies in Epidemiology (MOOSE) guidelines [24]. We searched three electronic databases (PubMed, Scopus, and Web of Science) for eligible studies in which the relationships of metabolic health status and obesity status with the risk of heart failure were evaluated up until August 31, 2022. The keywords were selected, with the use of appropriate Boolean operators, for the literature strategy: “metabolic health” OR “metabolically healthy” OR “metabolic syndrome” AND (“obesity” OR “overweight”) AND “heart failure” AND (“cohort study” OR “prospective study”) AND “follow-up study”. We further filtered the article types by “review”, “systematic review” or “meta-analysis”. Language and time restrictions were not applied. We only searched full-text publications; abstracts and unpublished manuscripts were not considered.
2.2. Study Selection
A study was determined as eligible for inclusion in the meta-analysis when the following criteria were all met: (1) exposure defined using metabolic health status and obesity status, (2) outcomes including heart failure, (3) cohort design, and (4) risk estimates with 95% confidence intervals (CIs) for the relationship between the defined exposure and outcome were reported. The duplicate studies presented as the published articles titles, authors, and publication year were deleted, by using Endnote software, version 9, Clarivate, Philadelphia, US. In this process, three authors (X.W., J.Y.D., and Z.D.) worked independently to screen each record. After screening, the final study selection was completed by evaluating the full text of the selected ones, and any disagreements were resolved by discussion.
2.3. Data Extraction
X.W. and J.Y.D. reviewed the selected articles independently and discussed to generate a standard form to record the following data from each included study to describe their characteristics: the family name of the first author, year of publication, characteristics of the participants (age, sex, and location), sample size, study design, number of cases, duration of follow-up, assessments of metabolic health and obesity, assessments of heart failure, risk estimates with 95% CIs, and the results of the fully adjusted statistical model.
2.4. Quality Assessment
Study quality was evaluated using the Newcastle-Ottawa Scale, which includes assessments of study sample selection, group comparability, and the assessment of exposures and outcomes. Each study could be awarded a maximum of 9 points, with ≥7 points indicating high quality and <7 points indicating low quality. Two authors (X.W. and J.Y.D.) independently conducted the quality assessment.
2.5. Statistical Analysis
We defined six groups according to the metabolic health status and obesity status of the participants: a metabolically healthy normal-weight group, a metabolically healthy overweight group, a metabolically healthy obesity group, a metabolically unhealthy normal-weight group, a metabolically unhealthy overweight group, and a metabolically unhealthy obesity group. Three studies combined individuals with overweight or obesity; we regarded those in the two Asian studies [19,20] as having overweight (mean body mass index (BMI) < 30 kg/m2) and those in the single US study [23] as having obesity (mean BMI > 30 kg/m2). The metabolically healthy normal-weight group was treated as the reference group for the analysis. Relative risks (RRs) and their 95% CIs were used as the common measures of the relationships, and hazard ratios or incidence rate ratios were converted to RRs. The heterogeneity of the RRs across the studies was tested using Cochran’s Q statistic and p < 0.10, and we also calculated the I2 statistic to estimate the degree of inconsistency across the studies [25]. According to the results of heterogeneity testing, a fixed-effects or random-effects model was used to estimate each summary RR [26]. Subgroup analyses were conducted according to the study location, study sample size, and the duration of follow up to identify possible sources of heterogeneity and their modifying effects. A sensitivity analysis was also performed to evaluate the effect of single studies on the overall risk estimate by omitting one study at a time and analyzing the remaining data [27]. We used Egger’s test and Begg’s test to assess potential publication bias [27]. Statistical analyses were performed using STATA version 12.0 (StataCorp, College Station, TX, USA).
3. Results
We initially obtained 591 records from the three databases. The majority of the records were excluded by scanning the title and abstract, mainly because the research question was not relevant or because they were duplicates. A total of 13 studies were selected for full-text review. Of these, we excluded two studies [28,29] that did not report a relationship with heart failure and one study [21] because the data were from the same source as another. Thus, data from 10 studies were included in the meta-analysis (Figure 1).
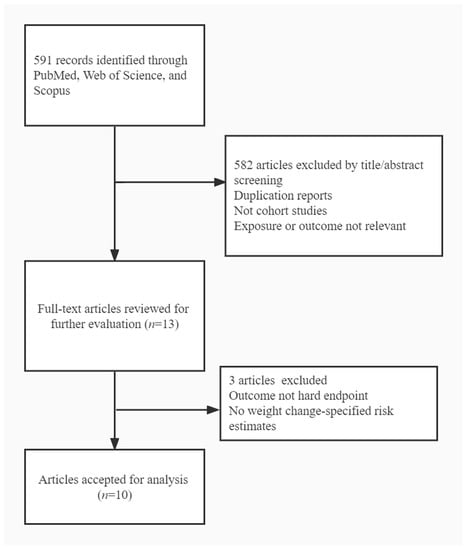
Figure 1.
Flow chart of study selection.
The characteristics of the included studies are shown in Table 1. The 10 studies were published between 2011 and 2021, with five conducted in European countries, three in Asian countries, and two in the United States. Of the 10 studies, nine had a prospective cohort design and one had a retrospective cohort design. One study was conducted in women and the others were conducted in both men and women. The median duration of follow-up in these studies ranged from 3.1 to 17.0 years. A total of 435,446 cases of heart failure cases among 8,092,751 participants were identified. The definition of metabolic health was based on the number of abnormal metabolic conditions (i.e., hypertension, diabetes, and hyperlipidemia), which varied among the studies. Overweight and obesity were defined using BMI or waist circumference. All the studies used medical records for their outcome assessments. The covariates adjusted for in multivariable models principally comprised age, sex, smoking status, alcohol consumption status, and physical activity status (Table S1).

Table 1.
Characteristics of studies evaluating the relationships of metabolic health status and obesity status with the risk of heart failure.
Figure 2 shows the results of individual studies and the pooled RRs of heart failure for the metabolically healthy overweight/obesity groups vs. the metabolically healthy normal-weight group. No significant evidence of heterogeneity was identified for the metabolically healthy overweight group (p for heterogeneity > 0.10), and a fixed-effects model was used to generate the results. In contrast, a random-effects model was used for the metabolically healthy obesity group (p for heterogeneity < 0.001). Compared with the metabolic healthy normal-weight group, the pooled RRs of heart failure were 1.23 (1.17, 1.29) for the metabolic healthy overweight group and 1.52 (1.40, 1.64) for the metabolically healthy obesity group.
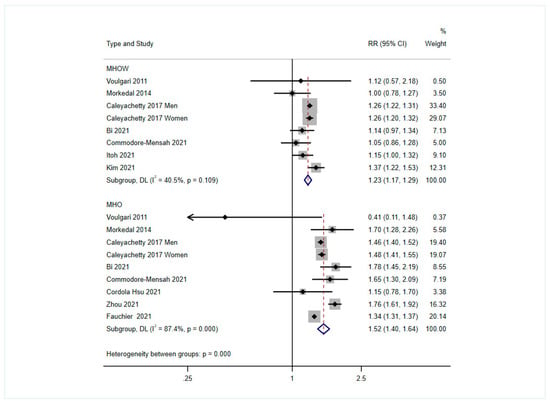
Figure 2.
Pooled results of the comparison of the risk of heart failure associated with metabolically healthy overweight or obesity, compared with that of the metabolically healthy normal-weight group [14,15,16,18,19,20,22,23,30,31]. MHOW: Metabolically healthy overweight group, MHO: Metabolically healthy obesity group.
Figure 3 shows the results of the individual studies and the pooled RRs of heart failure for the metabolically unhealthy normal-weight, overweight, and obesity groups compared with the metabolically healthy normal-weight group. For these three comparisons, the results varied across the studies (all p for heterogeneity < 0.001), and a random-effects model was used for the pooled analysis. Compared with the metabolically healthy normal-weight group, the pooled RRs of heart failure were 1.56 (1.30, 1.87) for the metabolically unhealthy normal-weight group, 1.75 (1.55, 1.98) for the metabolically unhealthy overweight group, and 2.28 (1.96, 2.66) for the metabolic unhealthy obesity group.
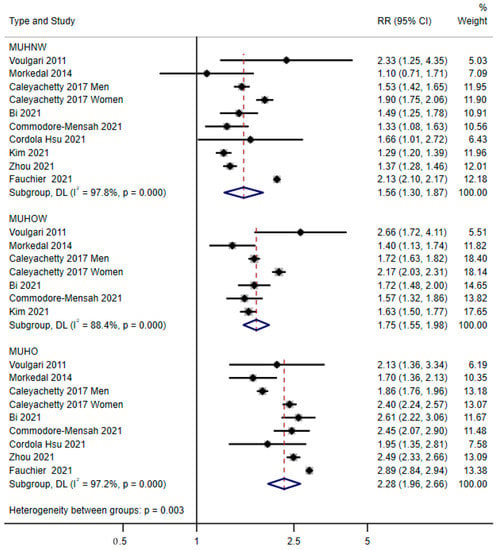
Figure 3.
Pooled results of the comparison of the risk of heart failure associated with metabolically unhealthy normal weight, overweight, or obesity, compared with that of the metabolically healthy normal-weight group [14,15,16,18,19,20,22,23,30,31]. MUHNW: Metabolically unhealthy normal-weight group, MUHOW: Metabolically unhealthy overweight group, MUHO: Metabolically unhealthy obesity group.
Table 2 shows the results stratified according to study area (Western or Eastern countries). Because 5 of the 10 studies were conducted in Western countries, the results for western countries were very similar to those obtained from the overall analyses. The associations for the metabolically unhealthy normal-weight and overweight groups were weaker in Eastern countries. However, the association for the metabolically unhealthy obesity group was stronger in Eastern countries (only one Chinese study was included). The results stratified by sample size and duration of follow-up are presented in Tables S2 and S3. Overall, study sample size did not appear to modify the associations, while associations appeared to be stronger in studies with a shorter duration of follow-up (median < 10 years). Although level of heterogeneity decreased in several subgroups, it remained high in the analyses of metabolically unhealthy groups, particularly metabolically unhealthy obesity.

Table 2.
Subgroup analysis according to study location.
We next performed a sensitivity analysis by omitting one study in turn and combining the remaining data, and no single study was found to have a substantial effect on the overall results for any exposure (Table S4). In addition, the results of Egger’s and Begg’s tests showed no evidence of publication bias (all p for publication bias > 0.26).
4. Discussion
In the present meta-analysis of 8,092,751 individuals, we evaluated the relationships of metabolic health status and obesity status with the risk of heart failure. We found that people with overweight and obesity had approximately 23% and 52% higher risks of developing heart failure, even if they were metabolically healthy. Compared with the metabolically healthy normal-weight group, the metabolically unhealthy normal-weight group was associated with an approximately 56% higher risk of heart failure, and this risk increased to 75% and 128% for the metabolically unhealthy overweight and obesity groups.
There is growing interest in the relationship between MHO and cardiovascular disease (CVD). Despite the absence of metabolic abnormalities in individuals with obesity, early changes may already be present that contribute to a higher risk of occurrence of CVD. MHO was found to be associated with abnormalities in several markers of subclinical CVD, including impaired vasoreactivity, high carotid artery intima-media thickness and aortic pulse wave velocity, high left ventricular mass and impaired function, and higher prevalences of coronary and aortic calcification [32,33]. Previous cohort studies have shown positive associations of MHO with hypertension [34], myocardial infarction, ischemic heart disease [35], and stroke [36]. The findings of the present study are consistent with “healthy” obesity not being benign with respect to cardiovascular health, thereby adding to the evidence that MHO is associated with a higher risk of heart failure, because individuals with overweight or obesity were found to be at higher risk of heart failure, regardless of metabolic status.
The potential mechanisms involved in this increase in risk of heart failure include hemodynamic changes and changes in cardiac anatomy. Adipose tissue may affect the circulating blood volume, resulting in increases in cardiac output and ventricular stroke volume, thereby predisposing toward left ventricular enlargement, hypertrophy, and concentric remodeling, all of which are linked to the development of heart failure [37,38]. Thus, individuals with MHO might have worse subclinical left ventricular or systolic function [39]. When obesity induces metabolic abnormalities such as hypertension, hyperlipidemia, high fasting glucose concentration, and insulin resistance, the phenotypes of metabolically unhealthy overweight or obesity may lead to a further decline in cardiac function and the progression of heart failure [40].
We found that metabolically unhealthy individuals with normal weight were still at a higher risk of heart failure, and this group had a similar estimated risk to the MHO group (approximately 50%) in the present study. Previous prospective cohort studies have shown that the risk of CVD in metabolically unhealthy normal-weight individuals are at even higher risk than those with MHO [41,42,43]. The severity of obesity was assessed using BMI, which may not reflect body fat distribution. For example, the Women’s Health Initiative Study recently showed that both a large amount of trunk fat and small amounts of gluteofemoral or leg fat were associated with higher risks of CVD in postmenopausal women with normal BMIs [44]. Moreover, genetic studies have shown that differing metabolic and weight phenotypes are characterized by variability in genes and the genetic effects on adipocyte differentiation, lipogenesis, and lipolysis [45]. Metabolically unhealthy normal-weight individuals are more likely to have low leg fat mass and cardiorespiratory fitness, but greater fat deposition in the liver, visceral obesity, impairment in insulin secretion, insulin resistance, and carotid intima-media thickness than metabolically unhealthy individuals with obesity [45].
Metabolic health status and obesity status may change during a study. In most studies, a single baseline measurement of exposure factors was made, and we found only two studies [20,31] that evaluated the relationships of the changes in metabolic health status and obesity status with heart failure. For example, Kim et al. reported that a transition from the metabolically healthy normal-weight phenotype to the metabolically unhealthy phenotype increased the risk of incident heart failure, with hazard ratios of 1.33 (1.15, 1.54) for normal weight and 1.67 (1.21, 2.32) for obesity. Participants with metabolically unhealthy obesity lost weight (transition to the metabolically unhealthy normal-weight phenotype) or experienced a restoration of metabolic health (transition to MHO) were still associated with a higher risk of heart failure, with hazard ratios of 1.76 (1.49, 2.07) and 1.65 (1.38, 1.97), respectively. These findings are also consistent with the risk of heart failure being even greater in those who acquire metabolic abnormalities and/or maintain their obesity (e.g., transition to the metabolically unhealthy normal-weight phenotype or MHO). Thus, further longitudinal studies with repeated measures should be performed to assess the importance of changes in obesity status and metabolic health in a real-world clinical setting, because these would have important implications for the importance of weight management and metabolic health maintenance with respect to the risk of heart failure.
Several limitations of this study should be acknowledged. First, heterogeneity is a common limitation of meta-analyses. In the present study, considerable heterogeneity was identified in the analyses of the metabolically unhealthy groups. Only the studies by Caleyachetty et al. [18] and Fauchier et al. [22] showed that sex may modify the associations of metabolic health and obesity with the risk of heart failure. For instance, when comparing metabolically unhealthy normal-weight individuals to metabolically healthy normal-weight individuals, the RRs were 1.53 (1.42, 1.65) for men and 1.90 (1.75, 2.06) for women, suggesting that sex may be a possible source of the heterogeneity [18]. However, sex-specific analyses were not performed in the other cohort studies, and therefore we were unable to perform separate meta-analyses for men and women. Other factors, such as age, socioeconomic status, or different lifestyles could also explain the heterogeneity. It is of great importance to conduct future studies to explore this association for individuals with certain characteristics. Second, the inclusion criteria bias is inevitable. For example, the definition of metabolic health was based on the numbers of metabolic disorders identified in the constituent studies, which may have been another source of heterogeneity. Third, the included studies typically defined obesity using BMI, and only one study [23] used waist circumference, which has been shown to be a better means of assessing obesity. Lastly, publication bias is a threat to the validity of any meta-analysis; however, Begg’s and Egger’s tests showed little evidence of such bias in the present study.
In conclusion, the present meta-analysis of previous cohort studies showed that people with overweight or obesity are at a higher risk of heart failure, even if they are metabolically healthy. Specifically, compared with metabolically healthy normal-weight individuals, metabolically unhealthy normal-weight individuals and those with overweight or obesity were found to be at a higher risk of heart failure. Therefore, the promotion of both metabolic health and weight management may represent an important means of reducing the incidence of heart failure.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu14245223/s1, Table S1: Covariates adjusted in cohort studies, Table S2: Subgroup analysis according to sample size, Table S3: Subgroup analysis according to duration of follow-up, Table S4: Results of sensitivity analyses by omitting one study in each turn and combining the remaining studies.
Author Contributions
Conceptualization, X.W. and J.D.; Data curation, X.W. and Z.D.; Formal analysis, J.D.; Funding acquisition, X.W.; Investigation, Z.D.; Methodology, J.D.; Supervision, J.D., Y.H. (Yonghua Hu) and Y.H. (Yuantao Hao); Validation, Y.H. (Yonghua Hu) and L.Q.; Writing—original draft, X.W.; Writing—review and editing, J.D., Z.D., J.J., Y.H. (Yonghua Hu), L.Q. and Y.H. (Yuantao Hao). All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by the National key research and development program of China (Grant No. 2022YFC3600804).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in the study are available in the included articles.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lippi, G.; Sanchis-Gomar, F. Global epidemiology and future trends of heart failure. AME Med. J. 2020, 5, 15. [Google Scholar] [CrossRef]
- Kudo, A.; Asahi, K.; Satoh, H.; Iseki, K.; Moriyama, T.; Yamagata, K.; Tsuruya, K.; Fujimoto, S.; Narita, I.; Konta, T.; et al. Fast eating is a strong risk factor for new-onset diabetes among the Japanese general population. Sci. Rep. 2019, 9, 8210. [Google Scholar] [CrossRef] [PubMed]
- Braunwald, E. The war against heart failure: The Lancet lecture. Lancet 2015, 385, 812–824. [Google Scholar] [CrossRef] [PubMed]
- Jenny-Avital, E.R. Obesity and the risk of heart failure. N. Engl. J. Med. 2002, 347, 1887–1889. [Google Scholar]
- Aune, D.; Sen, A.; Norat, T.; Janszky, I.; Romundstad, P.; Tonstad, S.; Vatten, L.J. Body Mass Index, Abdominal Fatness, and Heart Failure Incidence and Mortality: A Systematic Re-view and Dose-Response Meta-Analysis of Prospective Studies. Circulation 2016, 133, 639–649. [Google Scholar] [CrossRef]
- Lumbers, T.; Katsoulis, M.; Henry, A.; Mordi, I.; Lang, C.; Hemingway, H.; Langenberg, C.; Holmes, M.; Sattar, N. Body mass index and heart failure risk: A cohort study in 1.5 million individuals and Mendelian randomisation analysis. medRxiv 2020. [Google Scholar] [CrossRef]
- Ho, K.K.; Pinsky, J.L.; Kannel, W.B.; Levy, D. The epidemiology of heart failure: The Framingham Study. J. Am. Coll. Cardiol. 1993, 22, 6A–13A. [Google Scholar] [CrossRef]
- Ingelsson, E.; Ärnlöv, J.; Sundström, J.; Zethelius, B.; Vessby, B.; Lind, L. Novel Metabolic Risk Factors for Heart Failure. J. Am. Coll. Cardiol. 2005, 46, 2054–2060. [Google Scholar] [CrossRef]
- Rey-López, J.P.; de Rezende, L.F.; de Sá, T.H.; Stamatakis, E. Is the Metabolically Healthy Obesity Phenotype an Irrelevant Artifact for Public Health? Am. J. Epidemiol. 2015, 182, 737–741. [Google Scholar] [CrossRef]
- Blüher, M. Are metabolically healthy obese individuals really healthy? Eur. J. Endocrinol. 2014, 171, R209–R219. [Google Scholar] [CrossRef]
- Blüher, M. Metabolically Healthy Obesity. Endocr. Rev. 2020, 41, 405–420. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.B. Metabolic health in normal-weight and obese individuals. Diabetologia 2018, 62, 558–566. [Google Scholar] [CrossRef]
- Gómez-Zorita, S.; Queralt, M.; Vicente, M.A.; González, M.; Portillo, M.P. Metabolically healthy obesity and metabolically obese normal weight: A review. J. Physiol. Biochem. 2021, 77, 175–189. [Google Scholar] [CrossRef]
- Voulgari, C.; Tentolouris, N.; Dilaveris, P.; Tousoulis, D.; Katsilambros, N.; Stefanadis, C. Increased Heart Failure Risk in Normal-Weight People With Metabolic Syndrome Compared With Metabolically Healthy Obese Individuals. J. Am. Coll. Cardiol. 2011, 58, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Mørkedal, B.; Vatten, L.J.; Romundstad, P.R.; Laugsand, L.E.; Janszky, I. Risk of myocardial infarction and heart failure among metabolically healthy but obese individuals: HUNT (Nord-Trondelag Health Study), Norway. J. Am. Coll. Cardiol. 2014, 63, 1071–1078. [Google Scholar] [CrossRef]
- Zhou, Z.; Macpherson, J.; Gray, S.R.; Gill, J.M.R.; Welsh, P.; Celis-Morales, C.; Sattar, N.; Pell, J.P.; Ho, F.K. Are people with metabolically healthy obesity really healthy? A prospective cohort study of 381,363 UK Biobank participants. Diabetologia 2021, 64, 1963–1972. [Google Scholar] [CrossRef] [PubMed]
- Mirzababaei, A.; Djafarian, K.; Mozafari, H.; Shab-Bidar, S. The long-term prognosis of heart diseases for different metabolic phenotypes: A systematic review and meta-analysis of prospective cohort studies. Endocrine 2019, 63, 439–462. [Google Scholar] [CrossRef]
- Caleyachetty, R.; Thomas, G.N.; Toulis, K.A.; Mohammed, N.; Gokhale, K.M.; Balachandran, K.; Nirantharakumar, K. Metabolically Healthy Obese and Incident Cardiovascular Disease Events Among 3.5 Million Men and Women. J. Am. Coll. Cardiol. 2017, 70, 1429–1437. [Google Scholar] [CrossRef]
- Itoh, H.; Kaneko, H.; Kiriyama, H.; Kamon, T.; Fujiu, K.; Morita, K.; Michihata, N.; Jo, T.; Takeda, N.; Morita, H.; et al. Met-abolically Healthy Obesity and the Risk of Cardiovascular Disease in the General Population- Analysis of a Nationwide Epidemiological Database. Circ. J. 2021, 85, 914–920. [Google Scholar] [CrossRef]
- Kim, H.S.; Lee, J.; Cho, Y.K.; Park, J.-Y.; Lee, W.J.; Kim, Y.-J.; Jung, C.H. Differential Effect of Metabolic Health and Obesity on Incident Heart Failure: A Nationwide Population-Based Cohort Study. Front. Endocrinol. 2021, 12, 625083. [Google Scholar] [CrossRef]
- Lee, Y.-B.; Kim, D.H.; Kim, S.M.; Kim, N.H.; Choi, K.M.; Baik, S.H.; Park, Y.G.; Han, K.; Yoo, H.J. Hospitalization for heart failure incidence according to the transition in metabolic health and obesity status: A nationwide population-based study. Cardiovasc. Diabetol. 2020, 19, 77. [Google Scholar] [CrossRef] [PubMed]
- Fauchier, G.; Bisson, A.; Bodin, A.; Herbert, J.; Semaan, C.; Angoulvant, D.; Ducluzeau, P.H.; Lip, G.Y.H.; Fauchier, L.; Msc, J.H. Metabolically healthy obesity and cardiovascular events: A nationwide cohort study. Diabetes Obes. Metab. 2021, 23, 2492–2501. [Google Scholar] [CrossRef] [PubMed]
- Cordola Hsu, A.R.; Xie, B.; Peterson, D.V.; LaMonte, M.J.; Garcia, L.; Eaton, C.B.; Going, S.B.; Phillips, L.S.; Manson, J.E.; An-ton-Culver, H.; et al. Metabolically Healthy/Unhealthy Overweight/Obesity Associations With Incident Heart Failure in Postmenopausal Women: The Women’s Health Initiative. Circ. Heart Fail. 2021, 14, e007297. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Irwig, L.; Macaskill, P.; Berry, G.; Glasziou, P. Bias in meta-analysis detected by a simple, graphical test. Graphical test is itself biased. BMJ 1998, 316, 470–471. [Google Scholar]
- Lind, L.; Risérus, U.; Ärnlöv, J. Impact of the Definition of Metabolically Healthy Obesity on the Association with Incident Cardiovascular Disease. Metab. Syndr. Relat. Disord. 2020, 18, 302–307. [Google Scholar] [CrossRef]
- Sponholtz, T.R.; Heuvel, E.R.V.D.; Xanthakis, V.; Vasan, R.S. Association of Variability in Body Mass Index and Metabolic Health With Cardiometabolic Disease Risk. J. Am. Heart Assoc. 2019, 8, e010793. [Google Scholar] [CrossRef]
- Commodore-Mensah, Y.; Lazo, M.; Tang, O.; Echouffo-Tcheugui, J.B.; Ndumele, C.E.; Nambi, V.; Wang, D.; Ballantyne, C.; Selvin, E. High Burden of Subclinical and Cardiovascular Disease Risk in Adults With Metabolically Healthy Obesity: The Atherosclerosis Risk in Communities (ARIC) Study. Diabetes Care 2021, 44, 1657–1663. [Google Scholar] [CrossRef]
- Bi, J.; Song, L.; Wang, L.; Su, B.; Wu, M.; Li, D.; Chen, S.; Liu, Y.; Yang, Y.; Zhou, Z.; et al. Transitions in metabolic health status over time and risk of heart failure: A prospective study. Diabetes Metab. 2022, 48, 101266. [Google Scholar] [CrossRef] [PubMed]
- Khan, U.I.; Wang, D.; Thurston, R.C.; Sowers, M.; Sutton-Tyrrell, K.; Matthews, K.A.; Barinas-Mitchell, E.; Wildman, R.P. Burden of subclinical cardiovascular disease in “metabolically benign” and “at-risk” overweight and obese women: The Study of Women’s Health Across the Nation (SWAN). Atherosclerosis 2011, 217, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Lind, L.; Siegbahn, A.; Ingelsson, E.; Sundström, J.; Ärnlöv, J. A Detailed Cardiovascular Characterization of Obesity Without the Metabolic Syndrome. Arter. Thromb. Vasc. Biol. 2011, 31, e27–e34. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.K.; Kim, S.H.; Cho, G.-Y.; Baik, I.; Lim, H.E.; Park, C.G.; Lee, J.B.; Kim, Y.H.; Lim, S.Y.; Kim, H.; et al. Obesity phenotype and incident hypertension: A prospective community-based cohort study. J. Hypertens. 2013, 31, 145–151. [Google Scholar] [CrossRef]
- Thomsen, M.; Nordestgaard, B.G. Myocardial Infarction and Ischemic Heart Disease in Overweight and Obesity With and Without Metabolic Syndrome. JAMA Intern. Med. 2014, 174, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.-Z.; Sun, F.-R.; Wang, Z.-T.; Tan, L.; Hou, X.-H.; Ou, Y.-N.; Dong, Q.; Yu, J.-T.; Tan, L. Metabolically healthy obesity and risk of stroke: A meta-analysis of prospective cohort studies. Ann. Transl. Med. 2021, 9, 197. [Google Scholar] [CrossRef]
- Alpert, M.A.; Lavie, C.J.; Agrawal, H.; Aggarwal, K.B.; Kumar, S.A. Obesity and heart failure: Epidemiology, pathophysiology, clinical manifestations, and management. Transl. Res. 2014, 164, 345–356. [Google Scholar] [CrossRef]
- Wilner, B.; Garg, S.; Ayers, C.R.; Maroules, C.D.; McColl, R.; Matulevicius, S.A.; de Lemos, J.A.; Drazner, M.H.; Peshock, R.; Neeland, I.J. Dynamic Relation of Changes in Weight and Indices of Fat Distribution With Cardiac Structure and Function: The Dallas Heart Study. J. Am. Heart Assoc. 2017, 6, e005897. [Google Scholar] [CrossRef]
- Wang, Y.; Liang, J.; Zheng, S.; He, A.; Chen, C.; Zhao, X.; Hua, M.; Xu, J.; Zheng, Z.; Liu, M. Combined associations of obesity and metabolic health with subclinical left ventricular dysfunctions: Danyang study. ESC Heart Fail. 2021, 8, 3058–3069. [Google Scholar] [CrossRef]
- Bozkurt, B.; Aguilar, D.; Deswal, A.; Dunbar, S.B.; Francis, G.S.; Horwich, T.; Jessup, M.; Kosiborod, M.; Pritchett, A.M.; Ramasubbu, K.; et al. Contributory Risk and Management of Comorbidities of Hypertension, Obesity, Diabetes Mellitus, Hyperlipidemia, and Metabolic Syndrome in Chronic Heart Failure: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e535–e578. [Google Scholar] [CrossRef]
- Eckel, N.; Meidtner, K.; Kalle-Uhlmann, T.; Stefan, N.; Schulze, M.B. Metabolically healthy obesity and cardiovascular events: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2016, 23, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Song, Y.; Chen, Y.; Hui, R.; Zhang, W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 2013, 168, 4761–4768. [Google Scholar] [CrossRef] [PubMed]
- Eckel, N.; Li, Y.; Kuxhaus, O.; Stefan, N.; Hu, F.B.; Schulze, M.B. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90,257 women (the Nurses’ Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol. 2018, 6, 714–724. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.-C.; Arthur, R.; Iyengar, N.M.; Kamensky, V.; Xue, X.; Wassertheil-Smoller, S.; Allison, M.A.; Shadyab, A.H.; Wild, R.A.; Sun, Y.; et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur. Heart J. 2019, 40, 2849–2855. [Google Scholar] [CrossRef] [PubMed]
- Stefan, N.; Schick, F.; Häring, H.-U. Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metab. 2017, 26, 292–300. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).