Breastfeeding Practices in the United Arab Emirates: Prenatal Intentions and Postnatal Outcomes
Abstract
:1. Introduction
2. Materials and Methods
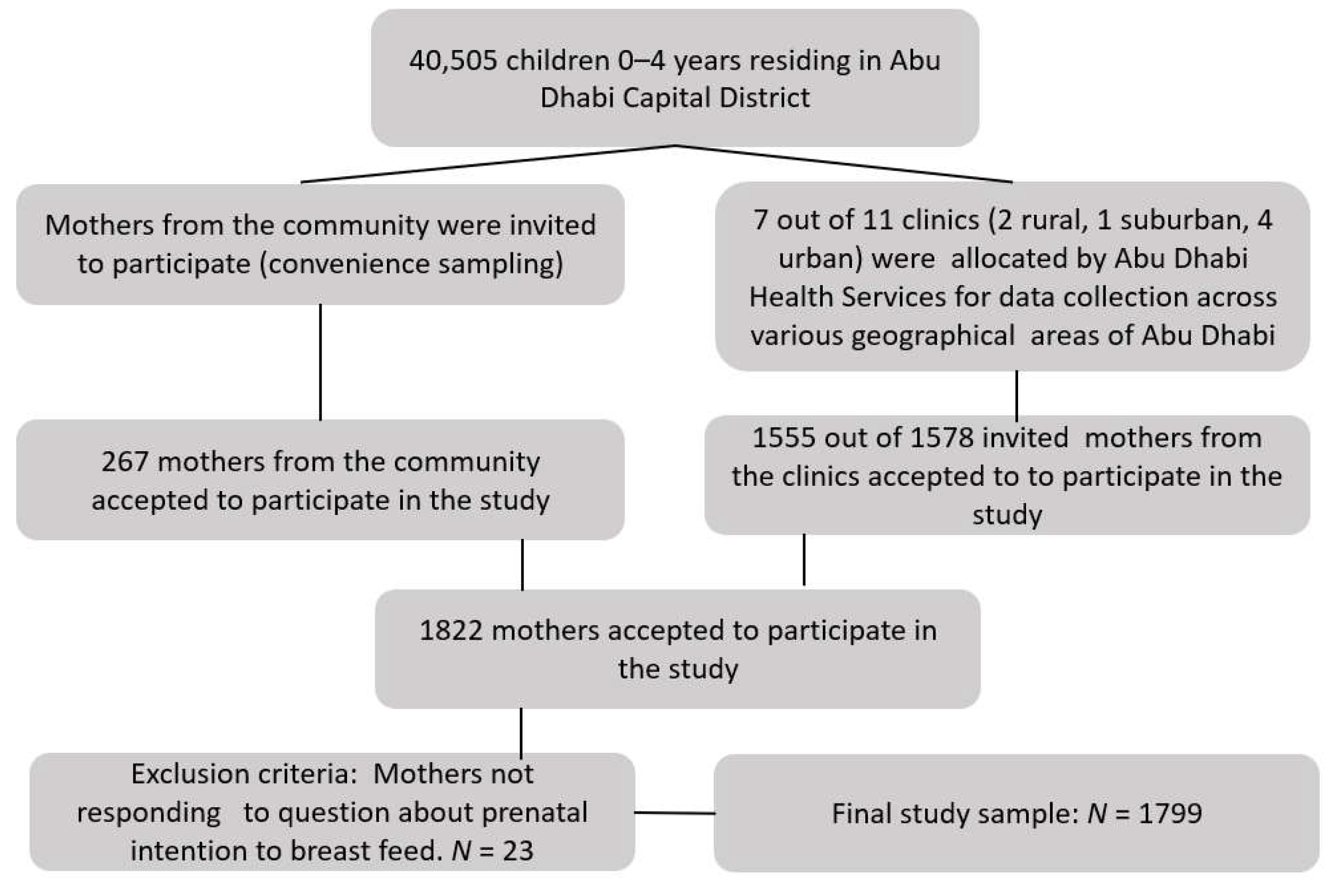
2.1. Participants and Data Collection
2.2. Study Instrument
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| aOR | Adjusted Odds Ratio |
| CI | Confidence Interval |
| EBF | Exclusive breastfeeding |
| SD | Standard Deviation |
| UAE | United Arab Emirates |
| WHO | World Health Organization |
| UK | United Kingdom |
References
- Leung, A.K.; Sauve, R.S. Breast is best for babies. J. Natl. Med. Assoc. 2005, 97, 1010. [Google Scholar]
- Salone, L.R.; Vann, W.F., Jr.; Dee, D.L. Breastfeeding: An overview of oral and general health benefits. J. Am. Dent. Assoc. 2013, 144, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Bahl, R.; Barros, A.J.; Franca, G.V.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef] [Green Version]
- Bai, Y.K.; Middlestadt, S.E.; Joanne Peng, C.Y.; Fly, A.D. Psychosocial factors underlying the mother’s decision to continue exclusive breastfeeding for 6 months: An elicitation study. J. Hum. Nutr. Diet. 2009, 22, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.R.; Dodds, L.; Legge, A.; Bryanton, J.; Semenic, S. Factors influencing the reasons why mothers stop breastfeeding. Can. J. Public Health 2014, 105, e179–e185. [Google Scholar] [CrossRef]
- Chambers, J.A.; McInnes, R.J.; Hoddinott, P.; Alder, E.M. A systematic review of measures assessing mothers’ knowledge, attitudes, confidence and satisfaction towards breastfeeding. Breastfeed. Rev. 2007, 15, 17–25. [Google Scholar]
- Colin, W.B.; Scott, J.A. Breastfeeding: Reasons for starting, reasons for stopping and problems along the way. Breastfeed. Rev. 2002, 10, 13–19. [Google Scholar]
- Jiang, H.; Li, M.; Yang, D.; Wen, L.M.; Hunter, C.; He, G.; Qian, X. Awareness, intention, and needs regarding breastfeeding: Findings from first-time mothers in Shanghai, China. Breastfeed. Med. 2012, 7, 526–534. [Google Scholar] [CrossRef]
- Santo, L.C.; de Oliveira, L.D.; Giugliani, E.R. Factors associated with low incidence of exclusive breastfeeding for the first 6 months. Birth 2007, 34, 212–219. [Google Scholar] [CrossRef]
- Kronborg, H.; Foverskov, E.; Væth, M.; Maimburg, R.D. The role of intention and self-efficacy on the association between breastfeeding of first and second child, a Danish cohort study. BMC Pregnancy Childbirth 2018, 18, 454. [Google Scholar] [CrossRef]
- Gila-Díaz, A.; Herranz Carrillo, G.; Arribas, S.M.; Ramiro-Cortijo, D. Healthy Habits and Emotional Balance in Women during the Postpartum Period: Differences between Term and Preterm Delivery. Children 2021, 8, 937. [Google Scholar] [CrossRef]
- Verret-Chalifour, J.; Giguere, Y.; Forest, J.-C.; Croteau, J.; Zhang, P.; Marc, I. Breastfeeding initiation: Impact of obesity in a large Canadian perinatal cohort study. PLoS ONE 2015, 10, e0117512. [Google Scholar] [CrossRef] [Green Version]
- Meedya, S.; Fahy, K.; Kable, A. Factors that positively influence breastfeeding duration to 6 months: A literature review. Women Birth 2010, 23, 135–145. [Google Scholar] [CrossRef] [Green Version]
- Donath, S.M.; Amir, L.H. Relationship between prenatal infant feeding intention and initiation and duration of breastfeeding: A cohort study. Acta Paediatr. 2003, 92, 352–356. [Google Scholar] [CrossRef]
- Chezem, J.; Friesen, C.; Boettcher, J. Breastfeeding knowledge, breastfeeding confidence, and infant feeding plans: Effects on actual feeding practices. J. Obstet. Gynecol. Neonatal Nurs. 2003, 32, 40–47. [Google Scholar] [CrossRef]
- Thomas, J.S.; Yu, E.A.; Tirmizi, N.; Owais, A.; Das, S.K.; Rahman, S.; Faruque, A.S.; Schwartz, B.; Stein, A.D. Maternal knowledge, attitudes and self-efficacy in relation to intention to exclusively breastfeed among pregnant women in rural Bangladesh. Matern. Child Health J. 2015, 19, 49–57. [Google Scholar] [CrossRef]
- Kornides, M.; Kitsantas, P. Evaluation of breastfeeding promotion, support, and knowledge of benefits on breastfeeding outcomes. J. Child Health Care 2013, 17, 264–273. [Google Scholar] [CrossRef] [Green Version]
- Kaunonen, M.; Hannula, L.; Tarkka, M.-T. A systematic review of peer support interventions for breastfeeding. J. Clin. Nurs. 2012, 21, 1943–1954. [Google Scholar] [CrossRef]
- Flacking, R.; Dykes, F.; Ewald, U. The influence of fathers’ socioeconomic status and paternity leave on breastfeeding duration: A population-based cohort study. Scand. J. Public Health 2010, 38, 337–343. [Google Scholar] [CrossRef]
- Rempel, L.A.; Rempel, J.K. The breastfeeding team: The role of involved fathers in the breastfeeding family. J. Hum. Lact. 2011, 27, 115–121. [Google Scholar] [CrossRef]
- Mithani, Y.; Premani, Z.S.; Kurji, Z.; Rashid, S. Exploring Fathers’ Role in Breastfeeding Practices in the Urban and Semiurban Settings of Karachi, Pakistan. J. Perinat. Educ. 2015, 24, 249–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ratnasari, D.; Paramashanti, B.A.; Hadi, H.; Yugistyowati, A.; Astiti, D.; Nurhayati, E. Family support and exclusive breastfeeding among Yogyakarta mothers in employment. Asia Pac. J. Clin. Nutr. 2017, 26, S31–S35. [Google Scholar] [CrossRef] [PubMed]
- Wouk, K.; Tully, K.P.; Labbok, M.H. Systematic Review of Evidence for Baby-Friendly Hospital Initiative Step 3. J. Hum. Lact. 2017, 33, 50–82. [Google Scholar] [CrossRef]
- Sinha, B.; Chowdhury, R.; Sankar, M.J.; Martines, J.; Taneja, S.; Mazumder, S.; Rollins, N.; Bahl, R.; Bhandari, N. Interventions to improve breastfeeding outcomes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 114–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sherriff, N.; Hall, V. Engaging and supporting fathers to promote breastfeeding: A new role for Health Visitors? Scand. J. Caring Sci. 2011, 25, 467–475. [Google Scholar] [CrossRef]
- Mensah, K.A.; Acheampong, E.; Anokye, F.O.; Okyere, P.; Appiah-Brempong, E.; Adjei, R.O. Factors influencing the practice of exclusive breastfeeding among nursing mothers in a peri-urban district of Ghana. BMC Res. Notes 2017, 10, 466. [Google Scholar] [CrossRef]
- Zhang, K.; Tang, L.; Wang, H.; Qiu, L.; Binns, C.W.; Lee, A.H. Why do mothers of young infants choose to formula feed in China? Perceptions of mothers and hospital staff. Int. J. Environ. Res. Public Health 2015, 12, 4520–4532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Guiding Principles for Complementary Feeding of the Breastfed Child. 2003. Available online: https://pesquisa.bvsalud.org/portal/resource/pt/lis-40345 (accessed on 9 January 2022).
- Taha, Z. Trends of breastfeeding in the United Arab Emirates (UAE). Arab. J. Nutr. Exerc. (AJNE) 2017, 2, 152–159. [Google Scholar] [CrossRef]
- Taha, Z.; Garemo, M.; Nanda, J. Patterns of breastfeeding practices among infants and young children in Abu Dhabi, United Arab Emirates. Int. Breastfeed. J. 2018, 13, 48. [Google Scholar] [CrossRef] [Green Version]
- DiGirolamo, A.; Thompson, N.; Martorell, R.; Fein, S.; Grummer-Strawn, L. Intention or experience? Predictors of continued breastfeeding. Health Educ. Behav. 2005, 32, 208–226. [Google Scholar] [CrossRef]
- Sheehan, D.; Krueger, P.; Watt, S.; Sword, W.; Bridle, B. The Ontario Mother and Infant Survey: Breastfeeding outcomes. J. Hum. Lact. 2001, 17, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Kools, E.J.; Thijs, C.; Vries, H.D. The behavioral determinants of breast-feeding in The Netherlands: Predictors for the initiation of breast-feeding. Health Educ. Behav. 2005, 32, 809–824. [Google Scholar] [CrossRef] [PubMed]
- Persad, M.D.; Mensinger, J.L. Maternal breastfeeding attitudes: Association with breastfeeding intent and socio-demographics among urban primiparas. J. Community Health 2008, 33, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Perrine, C.G.; Scanlon, K.S.; Li, R.; Odom, E.; Grummer-Strawn, L.M. Baby-Friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics 2012, 130, 54–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alnasser, Y.; Almasoud, N.; Aljohni, D.; Almisned, R.; Alsuwaine, B.; Alohali, R.; Almutairi, O.; Alhezayen, R. Impact of attitude and knowledge on intention to breastfeed: Can mHealth based education influence decision to breastfeed exclusively? Ann. Med. Surg. 2018, 35, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Handayani, L.; Kosnin, A.M.; Jiar, Y.K. Breastfeeding education in term of knowledge and attitude through mother support group. J. Educ. Learn. 2012, 6, 65–72. [Google Scholar] [CrossRef] [Green Version]
- Shobo, O.G.; Umar, N.; Gana, A.; Longtoe, P.; Idogho, O.; Anyanti, J. Factors influencing the early initiation of breast feeding in public primary healthcare facilities in northeast Nigeria: A mixed-method study. BMJ Open 2020, 10, e032835. [Google Scholar] [CrossRef] [Green Version]
- Gavhane, S.; Yadav, S.; Uday, K.; Kale, A.; Sirohi, A.; Yadav, P.; Jadhao, P. Knowledge and factors affecting initiation of breast feeding in postnatal mothers in a tertiary care center. Int. J. Res. Med. Sci. 2018, 6, 481–485. [Google Scholar] [CrossRef] [Green Version]
- Al Ketbi, M.I.; Al Noman, S.; Al Ali, A.; Darwish, E.; Al Fahim, M.; Rajah, J. Knowledge, attitudes, and practices of breastfeeding among women visiting primary healthcare clinics on the island of Abu Dhabi, United Arab Emirates. Int. Breastfeed. J. 2018, 13, 26. [Google Scholar] [CrossRef] [Green Version]
- Wen, L.M.; Baur, L.A.; Rissel, C.; Alperstein, G.; Simpson, J.M. Intention to breastfeed and awareness of health recommendations: Findings from first-time mothers in southwest Sydney, Australia. Int. Breastfeed. J. 2009, 4, 9. [Google Scholar] [CrossRef] [Green Version]
- Motee, A.; Ramasawmy, D.; Pugo-Gunsam, P.; Jeewon, R. An Assessment of the Breastfeeding Practices and Infant Feeding Pattern among Mothers in Mauritius. J. Nutr. Metab. 2013, 2013, 243852. [Google Scholar] [CrossRef] [Green Version]
- Radwan, H.; Sapsford, R. Maternal perceptions and views about breastfeeding practices among Emirati mothers. Food Nutr. Bull. 2016, 37, 73–84. [Google Scholar] [CrossRef] [Green Version]
- Thulier, D.; Mercer, J. Variables associated with breastfeeding duration. J. Obstet. Gynecol. Neonatal Nurs. 2009, 38, 259–268. [Google Scholar] [CrossRef]
- Britton, C.; McCormick, F.M.; Renfrew, M.J.; Wade, A.; King, S.E. Support for breastfeeding mothers. Cochrane Database Syst. Rev. 2007, 1, CD001141. [Google Scholar]
- Chatterji, P.; Frick, K.D. Does returning to work after childbirth affect breastfeeding practices? Rev. Econ. Househ. 2005, 3, 315–335. [Google Scholar] [CrossRef] [Green Version]
| Characteristics | Frequency | % |
|---|---|---|
| Mother’s Age (years) | ||
| 17–19 | 17 | 0.9 |
| 20–24 | 232 | 12.9 |
| 25–34 | 1153 | 64.1 |
| 35–51 | 397 | 22.1 |
| Mother’s Nationality a | ||
| Emirati | 582 | 32.4 |
| Non Emirati-Arab | 606 | 33.8 |
| Non Emirati-Non Arab | 607 | 33.8 |
| Marital Status b | ||
| Married | 1764 | 98.5 |
| Un-married | 26 | 1.5 |
| Mother’s Education c | ||
| Below High School | 76 | 4.3 |
| High School | 338 | 19 |
| University | 1364 | 76.7 |
| Father’s Education d | ||
| Below High School | 38 | 2.1 |
| High School | 202 | 11.3 |
| University | 1551 | 86.6 |
| Mother’s Employment Status | ||
| Employed | 646 | 35.9 |
| Not Employed | 1153 | 64.1 |
| Family Financial Well Being e (FFWB) | ||
| Excellent/Very Good | 1195 | 66.6 |
| Good | 480 | 26.8 |
| Fair | 106 | 5.9 |
| Poor/Very Poor | 12 | 0.7 |
| Parity | ||
| 1st child | 644 | 35.8 |
| 2nd child | 535 | 29.8 |
| 3rd child | 305 | 17.0 |
| 4th child | 312 | 17.4 |
| Pre-Delivery | Post-Delivery N (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Breastfeeding Initiation | Exclusive Breastfeeding | Any Breastfeeding | |||||||||||
| No | p-Value | <1 Month | 1–3 Months | 3–6 Months | >6 Months | p-Value | <1 Month | 1–3 Months | 3–6 Months | >6 Months | p-Value | ||
| Intention to BF | |||||||||||||
| Yes | 1655 (97.9) | 36 (2.1) | <0.001 | 292 (22.7) | 388 (30.1) | 298 (23.2) | 309 (24.0) | 0.006 | 24 (2.4) | 110 (11.2) | 143 (14.6) | 703 (71.7) | 0.803 |
| No | 79 (73.1) | 29 (26.9) | 26 (35.6) | 19 (26.0) | 21 (28.8) | 7 (9.6) | 1 (1.8) | 8 (14.0) | 10 (17.5) | 38 (66.7) | |||
| Knowledge about BF | |||||||||||||
| 100% correct answers | 394 (96.1) | 16 (3.9) | 0.331 | 62 (19.6) | 90 (28.4) | 68 (21.5) | 97 (30.6) | 0.003 | 7 (2.7) | 26 (9.9) | 38 (14.4) | 192 (73.0) | 0.197 |
| 50% correct answers | 975 (96.9) | 31 (3.1) | 173 (23.3) | 220 (29.6) | 180 (24.2) | 170 (22.9) | 11 (2.0) | 63 (11.4) | 72 (13.0) | 407 (73.6) | |||
| 0% correct answers | 365 (95.3) | 18 (4.7) | 83 (27.7) | 97 (32.3) | 71 (23.7) | 49 (16.3) | 7 (3.2) | 29 (13.1) | 43 (19.5) | 142 (64.3) | |||
| Support from other people | |||||||||||||
| Yes | 1596 (97.7) | 38 (2.3) | <0.001 | 279 (22.6) | 369 (29,8) | 288 (23.3) | 301 (24.3) | 0.010 | 25 (2.7) | 108 (11.5) | 133 (14.1) | 676 (71.8) | 0.137 |
| No | 138 (83.6) | 27 (16.4) | 39 (31.7) | 38 (30.9) | 31 (25.2) | 15 (12.2) | 0 (0) | 10 (10.5) | 20 (21.1) | 65 (68.4) | |||
| Started Thinking About BF | Exclusive BF Duration in Months | ||||
|---|---|---|---|---|---|
| Trimester | <1 Month | 1–3 Months | 3–6 Months | >6 Months | Total |
| First | 137 (18.7) | 209 (28.5) | 188 (25.6) | 200 (27.2) | 734 |
| Second | 38 (23.8) | 50 (31.3) | 34 (21.3) | 38 (23.8) | 160 |
| Third | 71 (32.7) | 70 (32.3) | 37 (17.1) | 39 (18.0) | 217 |
| No intention to BF | 26 (35.6) | 19 (26.0) | 21 (28.8) | 7 (9.6) | 73 |
| Number of Mothers Receiving Breastfeeding Advice * | ||||
|---|---|---|---|---|
| Pre-Delivery | Post-Delivery | |||
| Encouraging N (%) | Discouraging N (%) | Encouraging N (%) | Discouraging N (%) | |
| Health professionals | 535 (29.4) | 2 (0.1) | 787 (38.4) | 8 (0.4) |
| Lactation specialists | 220 (12.1) | 2 (0.1) | 568 (27.7) | 5 (0.3) |
| Mothers | 437 (24) | 7 (0.4) | 310 (15.1) | 11 (0.6) |
| In-laws | 270 (14.9) | 7 (0.4) | 132 (6.4) | 17 (0.9) |
| Spouses | 262 (14.4) | 5 (0.3) | 165 (8) | 11 (0.6) |
| Other relatives | 61 (3.4) | 13 (0.7) | 55 (2.7) | 22 (1.2) |
| Friends/others | 33 (1.8) | 7 (0.4) | 34 (1.7) | 13 (0.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taha, Z.; Garemo, M.; El Ktaibi, F.; Nanda, J. Breastfeeding Practices in the United Arab Emirates: Prenatal Intentions and Postnatal Outcomes. Nutrients 2022, 14, 806. https://doi.org/10.3390/nu14040806
Taha Z, Garemo M, El Ktaibi F, Nanda J. Breastfeeding Practices in the United Arab Emirates: Prenatal Intentions and Postnatal Outcomes. Nutrients. 2022; 14(4):806. https://doi.org/10.3390/nu14040806
Chicago/Turabian StyleTaha, Zainab, Malin Garemo, Farid El Ktaibi, and Joy Nanda. 2022. "Breastfeeding Practices in the United Arab Emirates: Prenatal Intentions and Postnatal Outcomes" Nutrients 14, no. 4: 806. https://doi.org/10.3390/nu14040806






