Dyslipidemia Increases the Risk of Incident Kidney Stone Disease in a Large Taiwanese Population Follow-Up Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. TWB
2.3. Demographic, Laboratory, and Medical Data
2.4. Presence of KSD
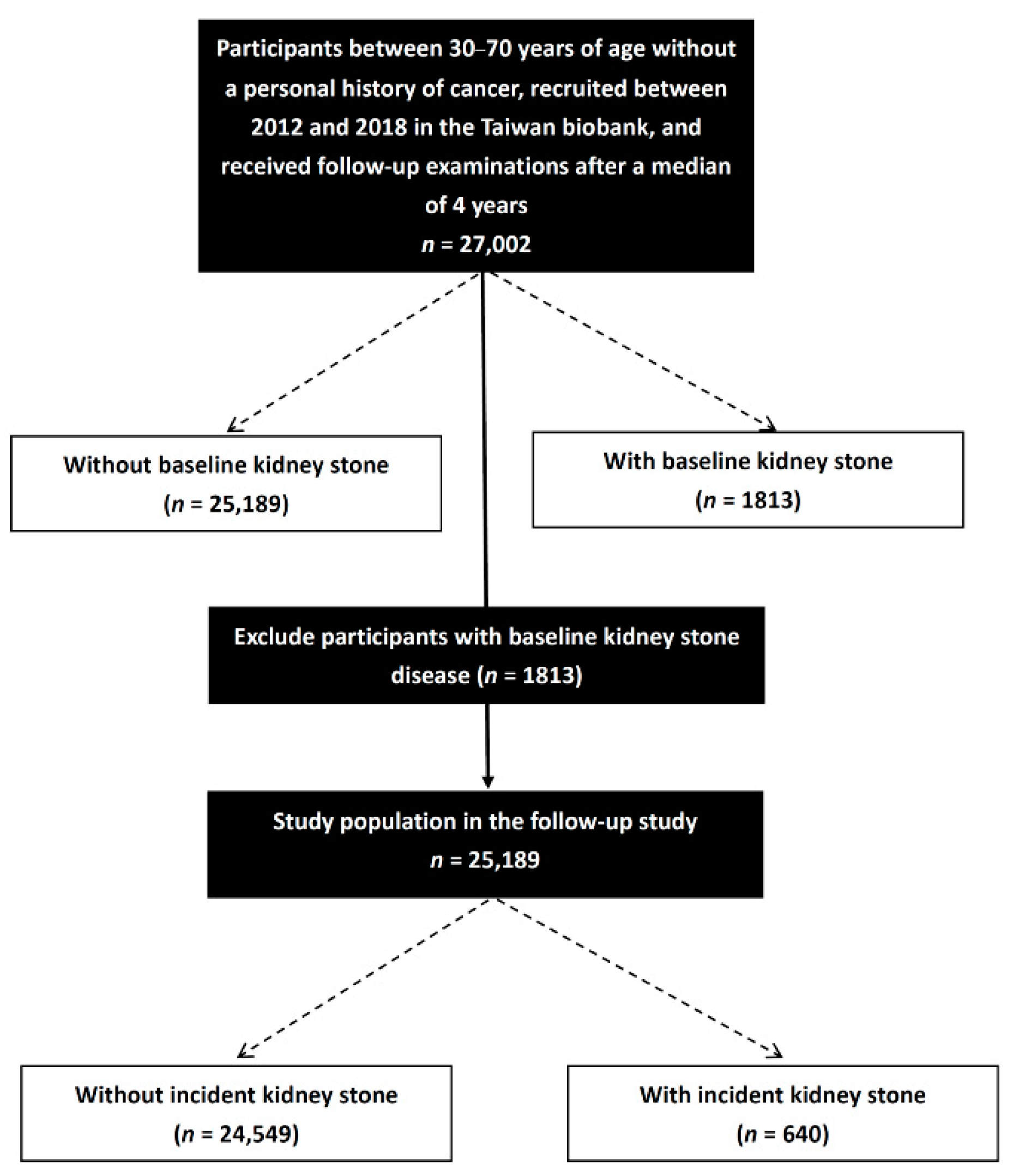
2.5. Study Participants
2.6. Statistical Analysis
3. Results
3.1. Comparison of Clinical Characteristics among Participants According to Baseline KSD
3.2. Associations among Lipid Profile Quartiles with Baseline KSD
3.3. Comparison of Clinical Characteristics among Participants According to Incident KSD
3.4. Associations among Lipid Profile Quartiles with Incident KSD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raheem, O.A.; Khandwala, Y.S.; Sur, R.L.; Ghani, K.R.; Denstedt, J.D. Burden of Urolithiasis: Trends in Prevalence, Treatments, and Costs. Eur. Urol. Focus 2017, 3, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.Y.; Chen, Y.F.; Carter, S.; Chang, H.C.; Lan, C.F.; Huang, K.H. Epidemiology of upper urinary tract stone disease in a Taiwanese population: A nationwide, population based study. J. Urol. 2013, 189, 2158–2163. [Google Scholar] [CrossRef] [PubMed]
- Moe, O.W. Kidney stones: Pathophysiology and medical management. Lancet 2006, 367, 333–344. [Google Scholar] [CrossRef]
- Alelign, T.; Petros, B. Kidney Stone Disease: An Update on Current Concepts. Adv. Urol. 2018, 2018, 3068365. [Google Scholar] [CrossRef] [PubMed]
- Jeong, I.G.; Kang, T.; Bang, J.K.; Park, J.; Kim, W.; Hwang, S.S.; Kim, H.K.; Park, H.K. Association between metabolic syndrome and the presence of kidney stones in a screened population. Am. J. Kidney Dis. 2011, 58, 383–388. [Google Scholar] [CrossRef]
- Kohjimoto, Y.; Sasaki, Y.; Iguchi, M.; Matsumura, N.; Inagaki, T.; Hara, I. Association of metabolic syndrome traits and severity of kidney stones: Results from a nationwide survey on urolithiasis in Japan. Am. J. Kidney Dis. 2013, 61, 923–929. [Google Scholar] [CrossRef]
- Rendina, D.; Mossetti, G.; De Filippo, G.; Benvenuto, D.; Vivona, C.L.; Imbroinise, A.; Zampa, G.; Ricchio, S.; Strazzullo, P. Association between metabolic syndrome and nephrolithiasis in an inpatient population in southern Italy: Role of gender, hypertension and abdominal obesity. Nephrol. Dial. Transplant. 2009, 24, 900–906. [Google Scholar] [CrossRef] [Green Version]
- Chang, I.H.; Lee, Y.T.; Lee, D.M.; Kim, T.H.; Myung, S.C.; Kim, Y.S.; Ahn, S.H. Metabolic syndrome, urine pH, and time-dependent risk of nephrolithiasis in Korean men without hypertension and diabetes. Urology 2011, 78, 753–758. [Google Scholar] [CrossRef]
- Jung, H.S.; Chang, I.H.; Kim, K.D.; Moon, Y.T.; Kim, T.H.; Myung, S.C.; Kim, Y.S.; Lee, J.Y. Possible Relationship between Metabolic Syndrome Traits and Nephrolithiasis: Incidence for 15 Years According to Gender. Korean J. Urol. 2011, 52, 548–553. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.C.; Huang, S.P.; Juan, Y.S.; Huang, T.Y.; Liu, C.C. Impact of metabolic syndrome and its components on kidney stone in aging Taiwanese males. Aging Male 2016, 19, 197–201. [Google Scholar] [CrossRef]
- Kang, H.W.; Lee, S.K.; Kim, W.T.; Kim, Y.J.; Yun, S.J.; Lee, S.C.; Kim, W.J. Hypertriglyceridemia and low high-density lipoprotein cholesterolemia are associated with increased hazard for urolithiasis. J. Endourol. 2014, 28, 1001–1005. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.W.; Seo, S.P.; Kim, W.T.; Kim, Y.J.; Yun, S.J.; Lee, S.C.; Kim, W.J. Hypertriglyceridemia is associated with increased risk for stone recurrence in patients with urolithiasis. Urology 2014, 84, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Masterson, J.H.; Woo, J.R.; Chang, D.C.; Chi, T.; L’Esperance, J.O.; Stoller, M.L.; Sur, R.L. Dyslipidemia is associated with an increased risk of nephrolithiasis. Urolithiasis 2015, 43, 49–53. [Google Scholar] [CrossRef] [Green Version]
- Rezaee, M.E.; Ward, C.E.; Pollock, M.; Shetty, S.D. Association between multiple chronic conditions and urolithiasis. Int. Urol. Nephrol. 2017, 49, 1361–1367. [Google Scholar] [CrossRef] [PubMed]
- Ding, Q.; Ouyang, J.; Fan, B.; Cao, C.; Fan, Z.; Ding, L.; Li, F.; Tu, W.; Jin, X.; Wang, J.; et al. Association between Dyslipidemia and Nephrolithiasis Risk in a Chinese Population. Urol. Int. 2019, 103, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Kabeya, Y.; Kato, K.; Tomita, M.; Katsuki, T.; Oikawa, Y.; Shimada, A.; Atsumi, Y. Associations of insulin resistance and glycemic control with the risk of kidney stones. Intern. Med. 2012, 51, 699–705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinberg, A.E.; Patel, C.J.; Chertow, G.M.; Leppert, J.T. Diabetic severity and risk of kidney stone disease. Eur. Urol. 2014, 65, 242–247. [Google Scholar] [CrossRef] [Green Version]
- Eisner, B.H.; Porten, S.P.; Bechis, S.K.; Stoller, M.L. Hypertension is associated with increased urinary calcium excretion in patients with nephrolithiasis. J. Urol. 2010, 183, 576–579. [Google Scholar] [CrossRef]
- Kim, Y.J.; Park, M.S.; Kim, W.T.; Yun, S.J.; Kim, W.J.; Lee, S.C. Hypertension influences recurrent stone formation in nonobese stone formers. Urology 2011, 77, 1059–1063. [Google Scholar] [CrossRef]
- Whitehurst, L.; Jones, P.; Somani, B.K. Mortality from kidney stone disease (KSD) as reported in the literature over the last two decades: A systematic review. World J. Urol. 2019, 37, 759–776. [Google Scholar] [CrossRef]
- Keddis, M.T.; Rule, A.D. Nephrolithiasis and loss of kidney function. Curr. Opin. Nephrol. Hypertens. 2013, 22, 390–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cupisti, A. Update on nephrolithiasis: Beyond symptomatic urinary tract obstruction. J. Nephrol. 2011, 24 (Suppl. S18), S25–S29. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Giles, W.H.; Dietz, W.H. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA 2002, 287, 356–359. [Google Scholar] [CrossRef] [PubMed]
- Karr, S. Epidemiology and management of hyperlipidemia. Am. J. Manag. Care 2017, 23, S139–S148. [Google Scholar]
- Stamler, J.; Daviglus, M.L.; Garside, D.B.; Dyer, A.R.; Greenland, P.; Neaton, J.D. Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA 2000, 284, 311–318. [Google Scholar] [CrossRef]
- Yaghi, S.; Elkind, M.S. Lipids and Cerebrovascular Disease: Research and Practice. Stroke 2015, 46, 3322–3328. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.J.; Kim, C.H.; Sung, E.J.; Kim, S.R.; Shin, H.C.; Jung, W.J. Association of nephrolithiasis with metabolic syndrome and its components. Metabolism 2013, 62, 808–813. [Google Scholar] [CrossRef]
- Sur, R.L.; Masterson, J.H.; Palazzi, K.L.; L’Esperance, J.O.; Auge, B.K.; Chang, D.C.; Stoller, M.L. Impact of statins on nephrolithiasis in hyperlipidemic patients: A 10-year review of an equal access health care system. Clin. Nephrol. 2013, 79, 351–355. [Google Scholar] [CrossRef]
- Cohen, A.J.; Adamsky, M.A.; Nottingham, C.U.; Pruitt, J.; Lapin, B.; Wang, C.H.; Park, S. Impact of Statin Intake on Kidney Stone Formation. Urology 2019, 124, 57–61. [Google Scholar] [CrossRef]
- Chen, C.H.; Yang, J.H.; Chiang, C.W.K.; Hsiung, C.N.; Wu, P.E.; Chang, L.C.; Chu, H.W.; Chang, J.; Song, I.W.; Yang, S.L.; et al. Population structure of Han Chinese in the modern Taiwanese population based on 10,000 participants in the Taiwan Biobank project. Hum. Mol. Genet. 2016, 25, 5321–5331. [Google Scholar] [CrossRef] [Green Version]
- Fan, C.T.; Hung, T.H.; Yeh, C.K. Taiwan Regulation of Biobanks. J. Law Med. Ethics 2015, 43, 816–826. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Ando, R.; Nagaya, T.; Suzuki, S.; Takahashi, H.; Kawai, M.; Okada, A.; Yasui, T.; Kubota, Y.; Umemoto, Y.; Tozawa, K.; et al. Kidney stone formation is positively associated with conventional risk factors for coronary heart disease in Japanese men. J. Urol. 2013, 189, 1340–1346. [Google Scholar] [CrossRef]
- Liu, Y.T.; Yang, P.Y.; Yang, Y.W.; Sun, H.Y.; Lin, I.C. The association of nephrolithiasis with metabolic syndrome and its components: A cross-sectional analysis. Ther. Clin. Risk Manag. 2017, 13, 41–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inci, M.; Demirtas, A.; Sarli, B.; Akinsal, E.; Baydilli, N. Association between body mass index, lipid profiles, and types of urinary stones. Ren. Fail. 2012, 34, 1140–1143. [Google Scholar] [CrossRef]
- Khan, S.R. Crystal-induced inflammation of the kidneys: Results from human studies, animal models, and tissue-culture studies. Clin. Exp. Nephrol. 2004, 8, 75–88. [Google Scholar] [CrossRef] [PubMed]
- Besiroglu, H.; Otunctemur, A.; Ozbek, E. The metabolic syndrome and urolithiasis: A systematic review and meta-analysis. Ren. Fail. 2015, 37, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Ozbek, E. Induction of oxidative stress in kidney. Int. J. Nephrol. 2012, 2012, 465897. [Google Scholar] [CrossRef] [Green Version]
- Naya, Y.; Ito, H.; Masai, M.; Yamaguchi, K. Association of dietary fatty acids with urinary oxalate excretion in calcium oxalate stone-formers in their fourth decade. BJU Int. 2002, 89, 842–846. [Google Scholar] [CrossRef] [Green Version]
- Meschi, T.; Nouvenne, A.; Borghi, L. Lifestyle recommendations to reduce the risk of kidney stones. Urol. Clin. N. Am. 2011, 38, 313–320. [Google Scholar] [CrossRef]
- Torricelli, F.C.; De, S.K.; Gebreselassie, S.; Li, I.; Sarkissian, C.; Monga, M. Dyslipidemia and kidney stone risk. J. Urol. 2014, 191, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.J.; Huang, H.S. Statins significantly alter urinary stone-related urine biochemistry in calcium kidney stone patients with dyslipidemia. Int. J. Urol. 2020, 27, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Hoofnagle, A.N.; Vaisar, T.; Mitra, P.; Chait, A. HDL lipids and insulin resistance. Curr. Diab. Rep. 2010, 10, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Bobulescu, I.A.; Dubree, M.; Zhang, J.; McLeroy, P.; Moe, O.W. Effect of renal lipid accumulation on proximal tubule Na+/H+ exchange and ammonium secretion. Am. J. Physiol. Ren. Physiol. 2008, 294, F1315–F1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoller, M.L.; Meng, M.V.; Abrahams, H.M.; Kane, J.P. The primary stone event: A new hypothesis involving a vascular etiology. J. Urol. 2004, 171, 1920–1924. [Google Scholar] [CrossRef]
- Lemieux, I.; Lamarche, B.; Couillard, C.; Pascot, A.; Cantin, B.; Bergeron, J.; Dagenais, G.R.; Despres, J.P. Total cholesterol/HDL cholesterol ratio vs. LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men: The Quebec Cardiovascular Study. Arch. Intern. Med. 2001, 161, 2685–2692. [Google Scholar] [CrossRef]
- Arsenault, B.J.; Boekholdt, S.M.; Kastelein, J.J. Lipid parameters for measuring risk of cardiovascular disease. Nat. Rev. Cardiol. 2011, 8, 197–206. [Google Scholar] [CrossRef]
- Ingelsson, E.; Schaefer, E.J.; Contois, J.H.; McNamara, J.R.; Sullivan, L.; Keyes, M.J.; Pencina, M.J.; Schoonmaker, C.; Wilson, P.W.; D’Agostino, R.B.; et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA 2007, 298, 776–785. [Google Scholar] [CrossRef] [Green Version]
- Cupisti, A.; Meola, M.; D’Alessandro, C.; Bernabini, G.; Pasquali, E.; Carpi, A.; Barsotti, G. Insulin resistance and low urinary citrate excretion in calcium stone formers. Biomed. Pharmacother. 2007, 61, 86–90. [Google Scholar] [CrossRef]
- Eisner, B.H.; Porten, S.P.; Bechis, S.K.; Stoller, M.L. Diabetic kidney stone formers excrete more oxalate and have lower urine pH than nondiabetic stone formers. J. Urol. 2010, 183, 2244–2248. [Google Scholar] [CrossRef]
- Abate, N.; Chandalia, M.; Cabo-Chan, A.V., Jr.; Moe, O.W.; Sakhaee, K. The metabolic syndrome and uric acid nephrolithiasis: Novel features of renal manifestation of insulin resistance. Kidney Int. 2004, 65, 386–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- West, B.; Luke, A.; Durazo-Arvizu, R.A.; Cao, G.; Shoham, D.; Kramer, H. Metabolic syndrome and self-reported history of kidney stones: The National Health and Nutrition Examination Survey (NHANES III) 1988-1994. Am. J. Kidney Dis. 2008, 51, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.S.; Lai, M.S.; Gau, S.S.; Wang, S.C.; Tsai, H.J. Concordance between patient self-reports and claims data on clinical diagnoses, medication use, and health system utilization in Taiwan. PLoS ONE 2014, 9, e112257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chou, Y.H.; Li, C.C.; Wu, W.J.; Juan, Y.S.; Huang, S.P.; Lee, Y.C.; Liu, C.C.; Li, W.M.; Huang, C.H.; Chang, A.W. Urinary stone analysis of 1,000 patients in southern Taiwan. Kaohsiung J. Med. Sci. 2007, 23, 63–66. [Google Scholar] [CrossRef] [Green Version]


| Characteristics | Baseline Kidney Stone (−) (n = 25,189) | Baseline Kidney Stone (+) (n = 1813) | p |
|---|---|---|---|
| Age (year) | 51.0 ± 10.4 | 54.1 ± 9.2 | <0.001 |
| Male gender (%) | 33.6 | 59.6 | <0.001 |
| Smoking history (%) | 23.2 | 39.1 | <0.001 |
| Alcohol history (%) | 8.2 | 11.8 | <0.001 |
| DM (%) | 5.0 | 9.4 | <0.001 |
| Hypertension (%) | 12.1 | 25.5 | <0.001 |
| Laboratory parameters | |||
| Fasting glucose (mg/dL) | 95.9 ± 20.0 | 100.3 ± 24.6 | <0.001 |
| Albumin (g/dL) | 4.55 ± 0.23 | 4.57 ± 0.23 | <0.001 |
| Triglyceride (mg/dL) | 112.9 ± 82.5 | 129.6 ± 90.4 | <0.001 |
| Total cholesterol (mg/dL) | 195.5 ± 35.4 | 194.3 ± 35.5 | 0.150 |
| HDL-C (mg/dL) | 54.5 ± 13.2 | 50.6 ± 12.9 | <0.001 |
| LDL-C (mg/dL) | 121.6 ± 31.6 | 122.4 ± 32.0 | 0.307 |
| Chol/HDL-C ratio | 3.76 ± 1.02 | 4.03 ± 1.08 | <0.001 |
| eGFR (mL/min/1.73 m2) | 103.2 ± 23.8 | 96.3 ± 24.3 | <0.001 |
| Quartile of Lipid Profile | Univariable (Baseline Kidney Stone) | Multivariable (Baseline Kidney Stone) | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| Triglyceride | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 1.328 (1.145–1.540) | <0.001 | 1.097 (0.943–1.276) | 0.229 |
| Quartile 3 | 1.416 (1.223–1.639) | <0.001 | 1.030 (0.885–1.198) | 0.702 |
| Quartile 4 | 1.988 (1.730–2.284) | <0.001 | 1.269 (1.095–1.470) | 0.002 |
| Total cholesterol | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 0.912 (0.798–1.041) | 0.173 | 0.944 (0.823–1.082) | 0.407 |
| Quartile 3 | 0.885 (0.774–1.011) | 0.072 | 0.917 (0.798–1.053) | 0.220 |
| Quartile 4 | 0.936 (0.819–1.069) | 0.328 | 1.004 (0.872–1.155) | 0.956 |
| HDL-C | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 0.741 (0.6570.837) | <0.001 | 0.961 (0.848–1.089) | 0.532 |
| Quartile 3 | 0.549 (0.480–0.627) | <0.001 | 0.844 (0.732–0.972) | 0.019 |
| Quartile 4 | 0.452 (0.393–0.521) | <0.001 | 0.809 (0.694–0.943) | 0.003 |
| LDL-C | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 0.955 (0.833–1.094) | 0.507 | 0.948 (0.825–1.090) | 0.456 |
| Quartile 3 | 1.035 (0.904–1.183) | 0.621 | 1.006 (0.876–1.155) | 0.929 |
| Quartile 4 | 1.083 (0.948–1.236) | 0.242 | 1.045 (0.911–1.200) | 0.529 |
| Chol/HDL-C ratio | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 1.228 (1.055–1.429) | 0.008 | 1.018 (0.873–1.189) | 0.816 |
| Quartile 3 | 1.563 (1.352–1.807) | <0.001 | 1.099 (0.946–1.277) | 0.218 |
| Quartile 4 | 2.012 (1.750–2.313) | <0.001 | 1.207 (1.041–1.400) | 0.013 |
| Characteristics | Incident Kidney Stone (−) (n = 24,549) | Incident Kidney Stone (+) (n = 640) | p |
|---|---|---|---|
| Age (year) | 51.0 ± 10.4 | 52.1 ± 9.8 | 0.005 |
| Male gender (%) | 33.1 | 55.6 | <0.001 |
| Smoking history (%) | 22.9 | 37.3 | <0.001 |
| Alcohol history (%) | 8.0 | 13.0 | <0.001 |
| DM (%) | 4.9 | 6.4 | 0.093 |
| Hypertension (%) | 12.0 | 18.4 | <0.001 |
| Laboratory parameters | |||
| Fasting glucose (mg/dL) | 95.9 ± 19.9 | 98.3 ± 20.5 | 0.002 |
| Albumin (g/dL) | 4.55 ± 0.23 | 4.58 ± 0.24 | 0.002 |
| Triglyceride (mg/dL) | 112.4 ± 81.5 | 130.7 ± 111.7 | <0.001 |
| Total cholesterol (mg/dL) | 195.5 ± 35.5 | 196.7 ± 33.4 | 0.407 |
| HDL-C (mg/dL) | 54.6 ± 13.2 | 21.3 ± 13.2 | <0.001 |
| LDL-C (mg/dL) | 121.5 ± 31.6 | 124.6 ± 31.4 | 0.013 |
| Chol/HDL-C ratio | 3.75 ± 1.02 | 4.01 ± 1.03 | <0.001 |
| eGFR (mL/min/1.73 m2) | 103.3 ± 23.8 | 99.2 ± 23.9 | <0.001 |
| Quartile of Lipid Profile | Univariable (Incident Kidney Stone) | Multivariable (Incident Kidney Stone) | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| Triglyceride | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 1.636 (1.275–2.098) | <0.001 | 1.463 (1.138–1.881) | 0.003 |
| Quartile 3 | 1.765 (1.380–2.257) | <0.001 | 1.458 (1.134–1.875) | 0.003 |
| Quartile 4 | 2.091 (1.644–2.660) | <0.001 | 1.532 (1.190–1.972) | 0.001 |
| Total cholesterol | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 1.083 (0.863–1.360) | 0.491 | 1.113 (0.885–1.399) | 0.361 |
| Quartile 3 | 1.271 (1.021–1.582) | 0.032 | 1.322 (1.059–1.651) | 0.014 |
| Quartile 4 | 1.045 (0.830–1.315) | 0.708 | 1.119 (0.883–1.417) | 0.353 |
| HDL-C | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 0.861 (0.706–1.051) | 0.141 | 1.054 (0.860–1.291) | 0.614 |
| Quartile 3 | 0.638 (0.512–0.794) | <0.001 | 0.895 (0.712–1.126) | 0.345 |
| Quartile 4 | 0.493 (0.390–0.623) | <0.001 | 0.772 (0.600–0.993) | 0.044 |
| LDL-C | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 1.153 (0.913–1.456) | 0.233 | 1.127 (0.891–1.426) | 0.317 |
| Quartile 3 | 1.424 (1.137–1.782) | 0.002 | 1.390 (1.108–1.743) | 0.004 |
| Quartile 4 | 1.307 (1.041–1.642) | 0.021 | 1.256 (0.997–1.583) | 0.054 |
| Chol/HDL-C ratio | ||||
| Quartile 1 | Reference | Reference | ||
| Quartile 2 | 1.223 (0.948–1.578) | 0.122 | 1.075 (0.832–1.391) | 0.579 |
| Quartile 3 | 1.755 (1.383–2.228) | <0.001 | 1.381 (1.082–1.763) | 0.010 |
| Quartile 4 | 2.044 (1.619–2.581) | <0.001 | 1.403 (1.097–1.793) | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, J.-A.; Li, C.-H.; Geng, J.-H.; Wu, D.-W.; Chen, S.-C. Dyslipidemia Increases the Risk of Incident Kidney Stone Disease in a Large Taiwanese Population Follow-Up Study. Nutrients 2022, 14, 1339. https://doi.org/10.3390/nu14071339
Hung J-A, Li C-H, Geng J-H, Wu D-W, Chen S-C. Dyslipidemia Increases the Risk of Incident Kidney Stone Disease in a Large Taiwanese Population Follow-Up Study. Nutrients. 2022; 14(7):1339. https://doi.org/10.3390/nu14071339
Chicago/Turabian StyleHung, Jia-An, Chien-Hsun Li, Jiun-Hung Geng, Da-Wei Wu, and Szu-Chia Chen. 2022. "Dyslipidemia Increases the Risk of Incident Kidney Stone Disease in a Large Taiwanese Population Follow-Up Study" Nutrients 14, no. 7: 1339. https://doi.org/10.3390/nu14071339
APA StyleHung, J.-A., Li, C.-H., Geng, J.-H., Wu, D.-W., & Chen, S.-C. (2022). Dyslipidemia Increases the Risk of Incident Kidney Stone Disease in a Large Taiwanese Population Follow-Up Study. Nutrients, 14(7), 1339. https://doi.org/10.3390/nu14071339






