The Risk of Undeclared Allergens on Food Labels for Pediatric Patients in the European Union
Abstract
:1. Introduction
2. Materials and Methods
2.1. Main Allergen Hazard
2.2. Food Category
2.3. Statistical Analysis
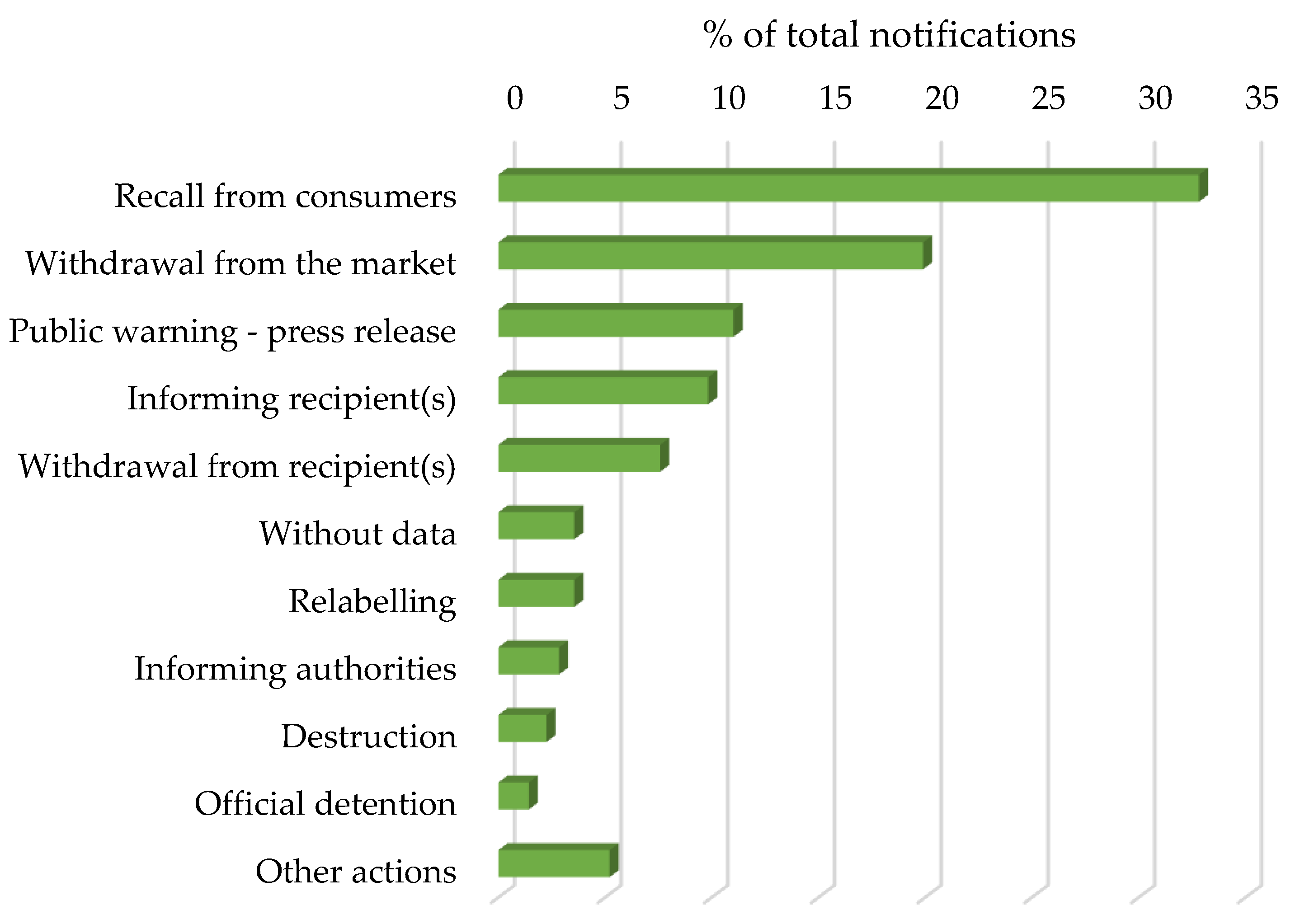
3. Results
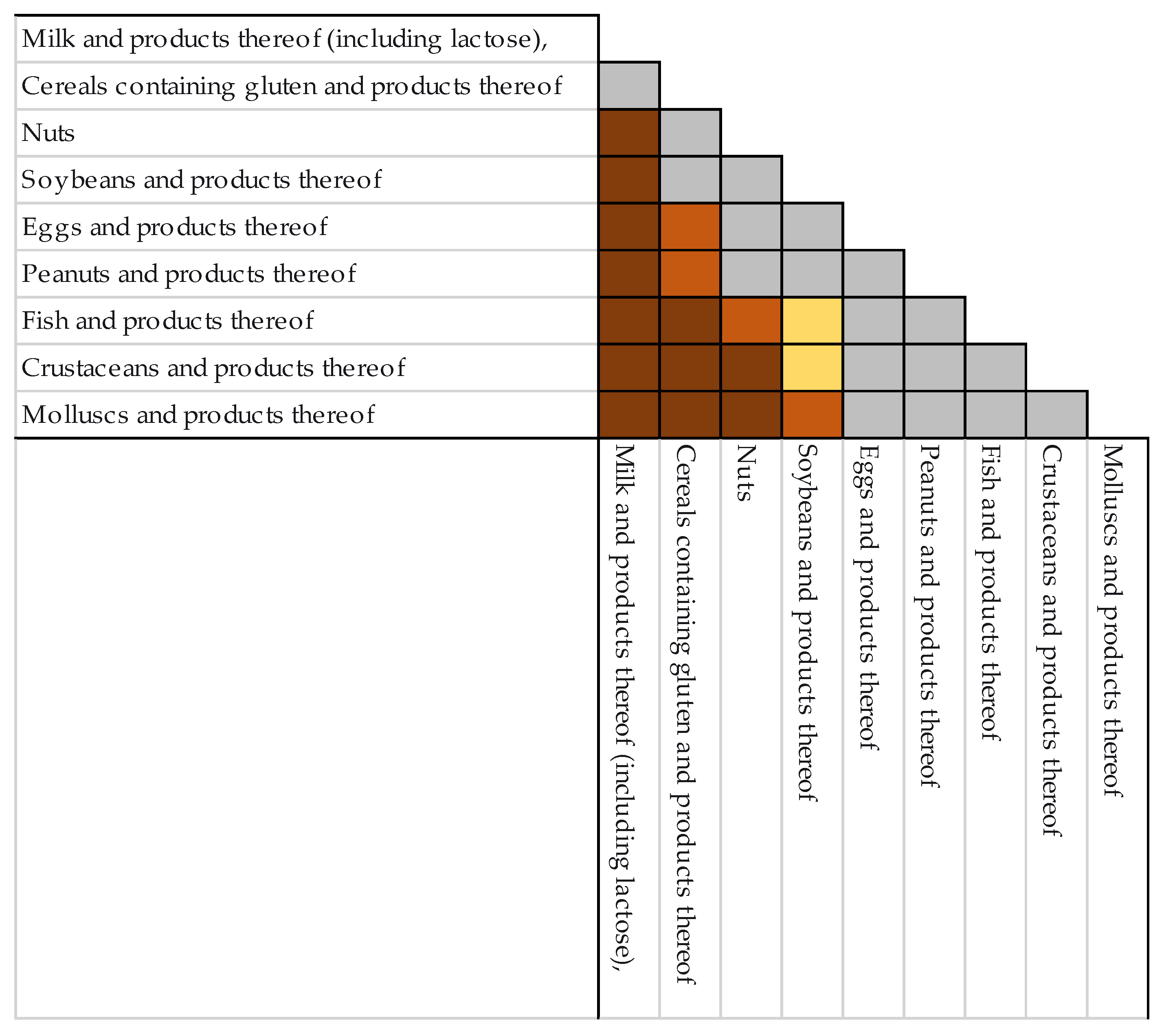
3.1. Main Allergen Hazard
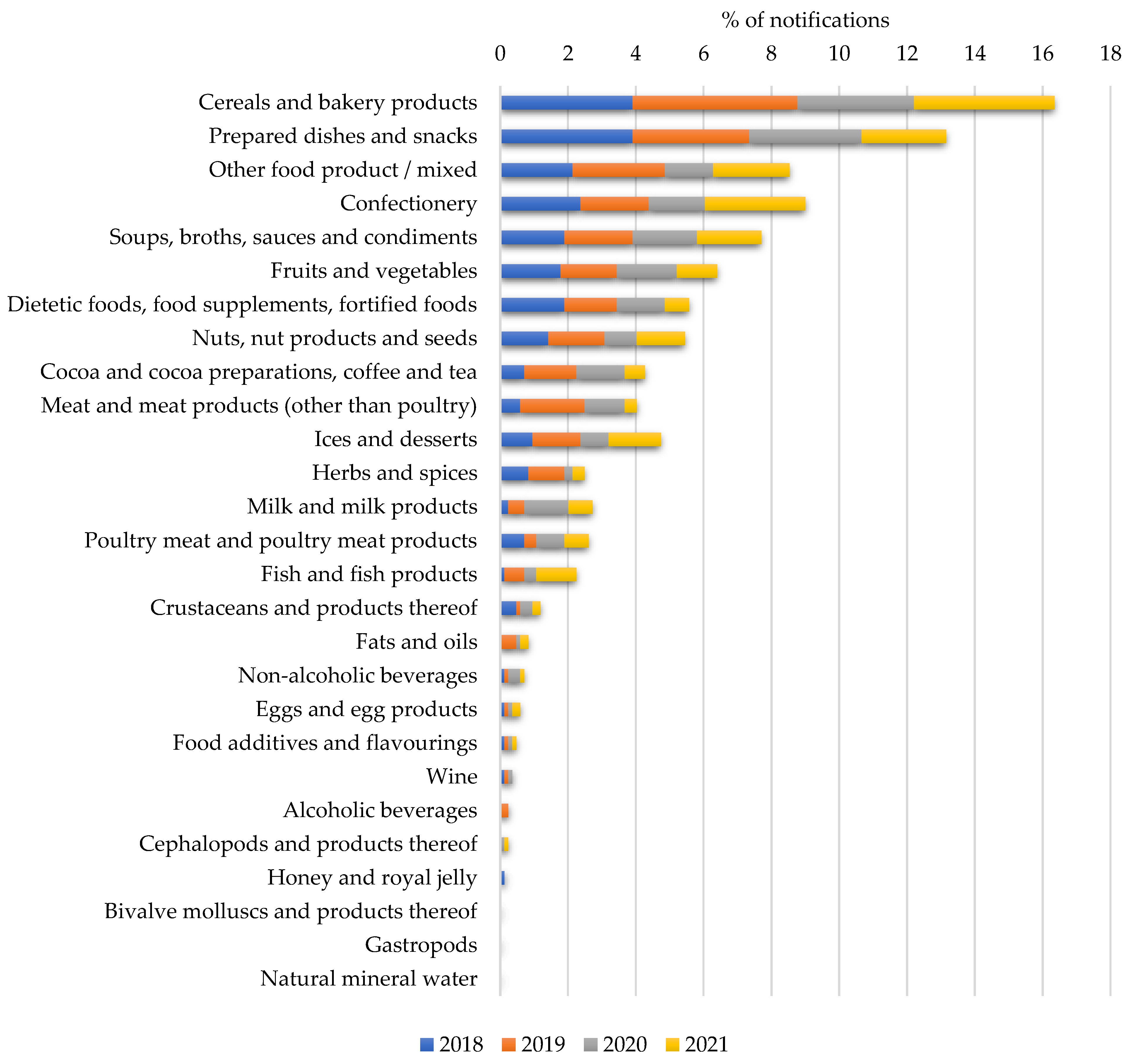
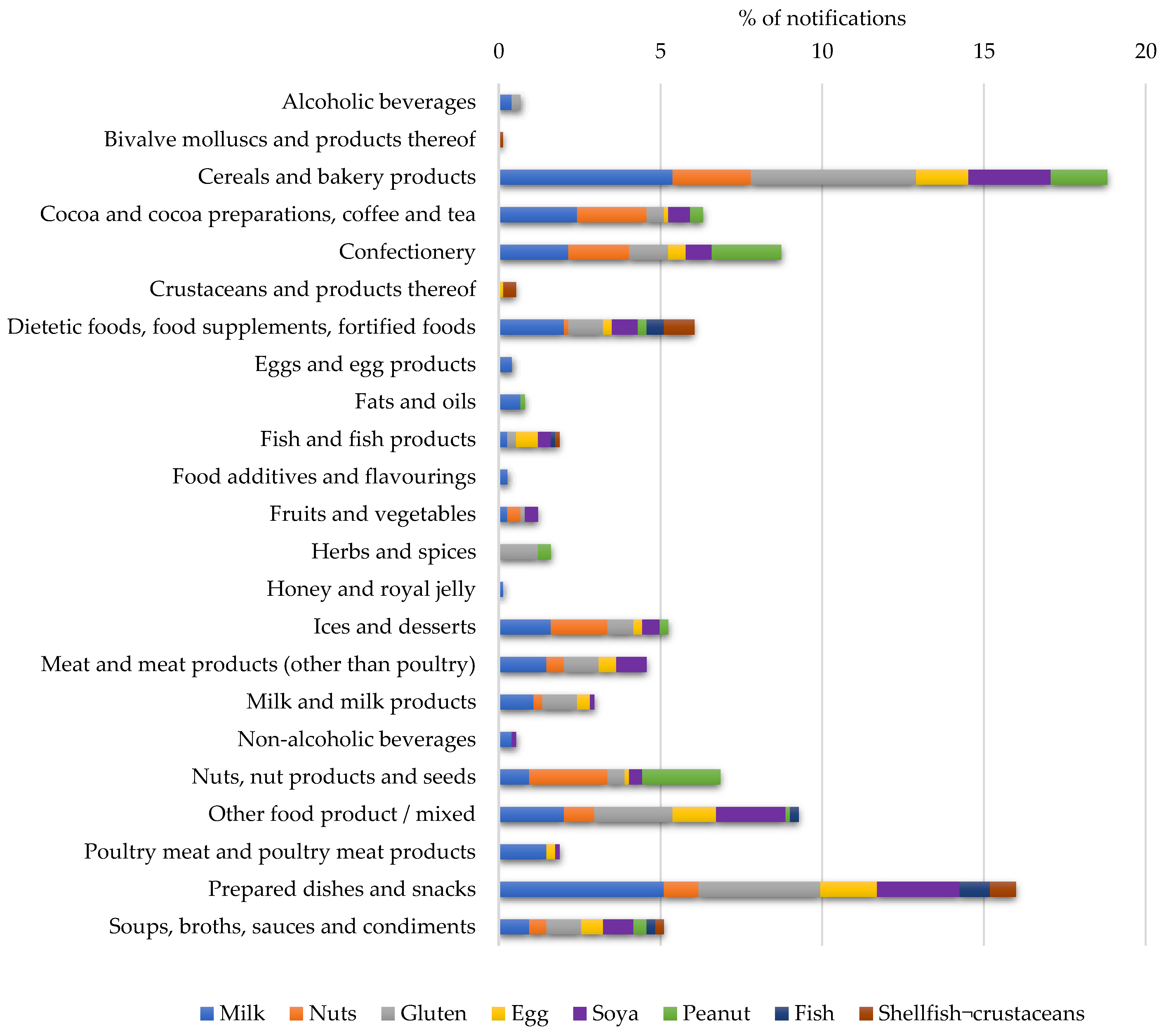
3.2. Food Categories and Related Allergens
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| Year 2018 | Year 2019 | Year 2020 | Year 2021 |
|---|---|---|---|
| Aubergines in oil | Carbonated strawberry-and-cream-flavored soft drink | Sweet and sour chicken | Canned soybeans mislabeled as spelt |
| Cake cream labelled as “lactose-free” and “milk-protein-free” | Carrot and dill hummus | Chilled, smoked-salmon salads | |
| Canned, peeled tomatoes | Chilled Hawaiian chicken salad | Frozen, organic, mung-bean nuggets | Chilled strawberries with chocolate cream |
| Chips | Frozen garlic puree | Frozen spring-roll sheets | Chilled vegan paprika slices |
| Cooked white beans | Frozen potato waffles | Frozen veggie burgers | Croutons used in Caesar salad |
| Easter-egg dye | Frozen soya product | Melba toast | Frozen beef spring rolls |
| Gluten-free bread mix | Frozen spicy burgers | Organic coconut sugar | Frozen sandwiches |
| Gluten-free-protein linseed and protein powder | Gluten-free hemp protein | Roasted vegetables | Grilled bell-pepper tapenade |
| Grilled chicken dish and tuna salad | Gluten-free hummus | Spinach noodles | Olives |
| Mini mooncakes | Green olives in glass jars | Various frozen products | Organic, gluten-free, soy flour |
| Organic, veggie-style chicken chunks mislabeled and packed as veggie-style beef strips | Grilled artichokes in sunflower oil | Vegan pate | Organic hummus |
| Pickled pepperoni | Instant pumpkin cereal | Vegetarian, marinated fillet | Pink roses for cake decoration |
| Various foodstuffs | Mini vegetarian-burger nuggets | Spaghetti Bolognese | |
| Various halawa flavors and jams | Olive paste | Spicy peppers filled with tuna and capers | |
| Vegan, dairy-free, grated pizza topping | Organic powder preparation for fermented soy dessert | Spinach cream | |
| Vegan, stracciatella-flavored, lupin-based yogurt | Pasta salad with smoked salmon | Spreads | |
| Wafer sheets | Seitan and vegetable sausages | Various gluten-free, processed products | |
| Soy-meat products | Vegetarian burgers | ||
| Spicy carrot spread with ginger | Vegetarian sausages | ||
| Sugar-free licorice sweets | |||
| Vegetable snack | |||
| Vegetarian mince mistakenly packaged as roasted cubes | |||
| Vegetarian salami |
References
- World Health Organization; Canonica, G.W.; Holgate, S.; Lockey, R.; Pawankar, R. White Book on Allergy 2011–2012 Executive Summary; World Allergy Organization: Milwaukee, WI, USA, 2013. [Google Scholar]
- Loh, W.; Tang, M.L.K. The Epidemiology of Food Allergy in the Global Context. Int. J. Environ. Res. Public Health 2018, 15, 2043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyons, S.A.; Clausen, M.; Knulst, A.C.; Ballmer-Weber, B.K.; Fernandez-Rivas, M.; Barreales, L.; Bieli, C.; Dubakiene, R.; Fernandez-Perez, C.; Jedrzejczak-Czechowicz, M.; et al. Prevalence of Food Sensitization and Food Allergy in Children across Europe. J. Allergy Clin. Immunol. Pract. 2020, 8, 2736–2746.e9. [Google Scholar] [CrossRef] [PubMed]
- Sicherer, S.H.; Sampson, H.A. Food Allergy: Epidemiology, Pathogenesis, Diagnosis, and Treatment. J. Allergy Clin. Immunol. 2013, 133, 291–307.e5. [Google Scholar] [CrossRef] [PubMed]
- Nwaru, B.I.; Hickstein, L.; Panesar, S.S.; Roberts, G.; Muraro, A.; Sheikh, A. Prevalence of Common Food Allergies in Europe: A Systematic Review and Meta-Analysis. Allergy 2014, 69, 992–1007. [Google Scholar] [CrossRef] [PubMed]
- Agache, I. EAACI White Paper on Research, Innovation and Quality Care; European Academy of Allergy and Clinical Immunology: Zurich, Switzerland, 2018. [Google Scholar]
- The European Parliament and the Council of the European Union. Regulation (EU) No 1169/2011 of the European Parliament and of the Council of 25 October 2011 on the Provision of Food Information to Consumers, Amending Regulations (EC) No 1924/2006 and (EC) No 1925/2006 of the European Parliament and of the Council, and Repealing Commission Directive 87/250/EEC, Council Directive 90/496/EEC, Commission Directive 1999/10/EC, Directive 2000/13/EC of the European Parliament and of the Council, Commission Directives 2002/67/EC and 2008/5/EC and Commission Regulation (EC) No 608/2004 Text with EEA Relevance. Off. J. Eur. Union 2011, 304, 1–65. [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies). Scientific Opinion on the Evaluation of Allergenic Foods and Food Ingredients for Labelling Purposes. EFSA J. 2014, 12, 3894. [Google Scholar]
- Royal Decree 126/2015 of 27 February 2015, which Approves the General Rule on Food Information on Foodstuffs Presented Unpackaged for Sale to the Final Consumer and to Mass Caterers, those Packaged at the Point of Sale at the Request of the Purchaser, and those Packaged by Retail Trade Operators. BOE 2015, 54, 20059–20066.
- Commission Implementing Regulation (EU) no 828/2014 of 30 July 2014 on the Requirements for the Provision of Information to Consumers on the Absence Or Reduced Presence of Gluten in Food (Text with EEA Relevance). Off. J. Eur. Union 2014, 228, 5–8.
- Commission Delegated Regulation (EU) 2016/127 of 25 September 2015 Supplementing Regulation (EU) no 609/2013 of the European Parliament and of the Council as Regards the Specific Compositional and Information Requirements for Infant Formula and Follow-on Formula and as Regards Requirements on Information Relating to Infant and Young Child Feeding (Text with EEA Relevance). Off. J. Eur. Union 2016, 25, 1–29.
- AESAN. Notice of 26 July 2019 Relating to the Conditions of use of the Terms ‘Lactose-Free’ and ‘Low Lactose’. Available online: https://www.aesan.gob.es/AECOSAN/docs/documentos/seguridad_alimentaria/interpretaciones/nutricionales/sin_lactosa.pdf (accessed on 2 April 2022).
- Soon, J.M.; Abdul Wahab, I.R. Global Food Recalls and Alerts Associated with Labelling Errors and its Contributory Factors. Trends Food Sci. Technol. 2021, 118, 791–798. [Google Scholar] [CrossRef]
- RASFF Window. Version 2.1.0. European Commission. Available online: https://webgate.ec.europa.eu/rasff-window/screen/search (accessed on 2 January 2022).
- The Official Portal for European Data. European Commission. Available online: https://data.europa.eu/en (accessed on 2 January 2022).
- Peters, R.L.; Krawiec, M.; Koplin, J.J.; Santos, A.F. Update on Food Allergy. Pediatr. Allergy Immunol. 2021, 32, 647. [Google Scholar] [CrossRef] [PubMed]
- Fleischer, D.M.; Perry, T.T.; Atkins, D.; Wood, R.A.; Burks, A.W.; Jones, S.M.; Henning, A.K.; Stablein, D.; Sampson, H.A.; Sicherer, S.H. Allergic Reactions to Foods in Preschool-Aged Children in a Prospective Observational Food Allergy Study. Pediatrics 2012, 130, e25–e32. [Google Scholar] [CrossRef] [Green Version]
- Turner, P.J.; Jerschow, E.; Umasunthar, T.; Lin, R.; Campbell, D.E.; Boyle, R.J. Fatal Anaphylaxis: Mortality Rate and Risk Factors. J. Allergy Clin. Immunol. Pract. 2017, 5, 1169–1178. [Google Scholar] [CrossRef] [PubMed]
- Baseggio Conrado, A.; Patel, N.; Turner, P.J. Global Patterns in Anaphylaxis due to Specific Foods: A systematic Review. J. Allergy Clin. Immunol. 2021, 148, 1515–1525.e3. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.J.; Gowland, M.H.; Sharma, V.; Ierodiakonou, D.; Harper, N.; Garcez, T.; Pumphrey, R.; Boyle, R.J. Increase in Anaphylaxis-Related Hospitalizations but no Increase in Fatalities: An Analysis of United Kingdom National Anaphylaxis Data, 1992–2012. J. Allergy Clin. Immunol. 2014, 135, 956–963.e1. [Google Scholar] [CrossRef] [Green Version]
- Kleter, G.A.; Prandini, A.; Filippi, L.; Marvin, H.J.P. Identification of Potentially Emerging Food Safety Issues by Analysis of Reports Published by the European Community’s Rapid Alert System for Food and Feed (RASFF) during a Four-Year Period. Food Chem. Toxicol. 2009, 47, 932–950. [Google Scholar] [CrossRef]
- Soon, J.M.; Brazier, A.K.M.; Wallace, C.A. Determining Common Contributory Factors in Food Safety Incidents—A Review of Global Outbreaks and Recalls 2008–2018. Trends Food Sci. Technol. 2020, 97, 76–87. [Google Scholar] [CrossRef]
- Gendel, S.M.; Jianmei, Z. Analysis of U.S. Food and Drug Administration Food Allergen Recalls After Implementation of the Food Allergen Labeling and Consumer Protection Act. J. Food Prot. 2013, 76, 1933–1938. [Google Scholar] [CrossRef]
- Bucchini, L.; Guzzon, A.; Poms, R.; Senyuva, H. Analysis and Critical Comparison of Food Allergen Recalls from the European Union, USA, Canada, Hong Kong, Australia and New Zealand. Food Addit. Contam. Part A Chem. Anal. Control Expo. Risk Assess. 2016, 33, 760–771. [Google Scholar] [CrossRef]
- Hischenhuber, C.; Crevel, R.; Jarry, B.; Maki, M.; Moneret-Vautrin, D.A.; Romano, A.; Troncone, R.; Ward, R. Review Article: Safe Amounts of Gluten for Patients with Wheat Allergy Or Coeliac Disease. Aliment Pharmacol. Ther. 2006, 23, 559–575. [Google Scholar] [CrossRef] [PubMed]
- Akobeng, A.K.; Thomas, A.G. Systematic Review: Tolerable Amount of Gluten for People with Coeliac Disease. Aliment Pharmacol. Ther. 2008, 27, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Bedford, B.; Yu, Y.; Wang, X.; Garber, E.A.E.; Jackson, L.S. A Limited Survey of Dark Chocolate Bars obtained in the United States for Undeclared Milk and Peanut Allergens. J. Food Prot. 2017, 80, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Moneret-Vautrin, D.A.; Kanny, G. Update on Threshold Doses of Food Allergens: Implications for Patients and the Food Industry. Curr. Opin. Allergy Clin. Immunol. 2004, 4, 215–219. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific Opinion on Lactose Thresholds in Lactose Intolerance and Galactosaemia. EFSA J. 2010, 8, 1777. [Google Scholar] [CrossRef]
- Gropper, S.; Weese, J.; West, P.; Gross, K. Free Galactose Content of Fresh Fruits and Strained Fruit and Vegetable Baby Foods:More Foods to Consider for the Galactose-Restricted Diet. J. Acad. Nutr. Diet. 2000, 100, 573–575. [Google Scholar]
- Protudjer, J.L.P.; Mikkelsen, A. Veganism and Paediatric Food Allergy: Two Increasingly Prevalent Dietary Issues that are Challenging when Co-Occurring. BMC Pediatr. 2020, 20, 341. [Google Scholar] [CrossRef]
- Sutter, D.O.; Bender, N. Nutrient Status and Growth in Vegan Children. Nutr. Res. 2021, 91, 13–25. [Google Scholar] [CrossRef]
- Rosenfeld, D.L.; Burrow, A.L. Vegetarian on Purpose: Understanding the Motivations of Plant-Based Dieters. Appetite 2017, 116, 456–463. [Google Scholar] [CrossRef]
- Cox, A.L.; Eigenmann, P.A.; Sicherer, S.H. Clinical Relevance of Cross-Reactivity in Food Allergy. J. Allergy Clin. Immunol. Pract. 2021, 9, 82–99. [Google Scholar] [CrossRef]
- Gupta, R.S.; Taylor, S.L.; Baumert, J.L.; Kao, L.M.; Schuster, E.; Smith, B.M. Economic Factors Impacting Food Allergen Management: Perspectives from the Food Industry. J. Food Prot. 2017, 80, 1719. [Google Scholar] [CrossRef]
- Soon, J.M.; Manning, L. “May Contain” Allergen Statements: Facilitating Or Frustrating Consumers? J. Consum. Policy 2017, 40, 447–472. [Google Scholar] [CrossRef] [Green Version]
- Food Drink Europe. Guidance on Food Allergen Management for Food Manufacturers; Food Drink Europe: Brussels, Belgium, 2013; 88p. [Google Scholar]
- IFS Management GmbH. IFS Food Version 6.1.; IFS Management GmbH: Berlin, Germany, 2017; 158p. [Google Scholar]
- BRCGS. Gluten-Free Certification Program Global Standard (Issue 3); BRCGS: London, UK, 2019. [Google Scholar]
- Zhang, Y.; Ren, Y.; Bi, Y.; Wang, Q.; Cheng, K.; Chen, F. Review: Seafood Allergy and Potential Application of High Hydrostatic Pressure to Reduce Seafood Allergenicity. Int. J. Food Eng. 2019, 15, 20180392. [Google Scholar] [CrossRef]
- Pan, M.; Yang, J.; Liu, K.; Xie, X.; Hong, L.; Wang, S.; Wang, S. Irradiation Technology: An Effective and Promising Strategy for Eliminating Food Allergens. Food Res. Int. 2021, 148, 110578. [Google Scholar] [CrossRef] [PubMed]
- Jia, L.; Evans, S. Improving Food Allergen Management in Food Manufacturing: An Incentive-Based Approach. Food Control 2021, 129, 108246. [Google Scholar] [CrossRef]
- Groetch, M.E.; Christie, L.; Vargas, P.A.; Jones, S.M.; Sicherer, S.H. Food Allergy Educational Needs of Pediatric Dietitians: A Survey by the Consortium of Food Allergy Research. J. Nutr. Educ. Behav. 2010, 42, 259–264. [Google Scholar] [CrossRef] [Green Version]
- Collins, S.C. Practice Paper of the Academy of Nutrition and Dietetics: Role of the Registered Dietitian Nutritionist in the Diagnosis and Management of Food Allergies. J. Acad. Nutr. Diet. 2016, 116, 1621–1631. [Google Scholar] [CrossRef]
- Sicherer, S.H.; Allen, K.; Lack, G.; Taylor, S.L.; Donovan, S.M.; Oria, M. Critical Issues in Food Allergy: A National Academies Consensus Report. Pediatrics 2017, 140, e20170194. [Google Scholar] [CrossRef] [Green Version]
- Austrian Agency for Health and Food Safety (AGES). Österreichische Agentur für Gesundheit und Ernährungssicherheit GmbH. Available online: https://www.ages.at/en/human/product-warnings-product-recalls (accessed on 10 March 2022).
- AFSCA. Pour Les Consommateurs Agence Fédérale Pour La Sécurité De La Chaîne Alimentaire. Federal Agency for the Safety of the Food Chain. Available online: https://www.favv-afsca.be/consommateurs/avertissements/ (accessed on 10 March 2022).
- E-Citizens Information and Service. HRana—Food-Related Warnings. Government of the Republic of Croatia. Available online: https://gov.hr/en/hrana-food-related-warnings/1774 (accessed on 10 March 2022).
- Le Site Des Alertes De Produits Dangereux. Ministry of Agriculture and Food. France Government. Available online: https://rappel.conso.gouv.fr/categorie/ (accessed on 10 March 2022).
- Lebensmittelwarnung. Das Bundesamt für Verbraucherschutz und Lebensmittelsicherheit, BVLD; Deutschland. Available online: www.lebensmittelwarnung.de (accessed on 10 March 2022).
- Recent News. Hellenic Food Authority (EFET). Hellenic Food Authority. Available online: https://www.efet.gr/index.php/en/ (accessed on 10 March 2022).
- Latest Food Alerts. Food Safety Authority of Ireland. Available online: https://www.fsai.ie/ (accessed on 10 March 2022).
- Avvisi Di Sicurezza. Sicurezza Alimentare. Ministero della Salute. Governo Italiano. Available online: https://www.salute.gov.it/portale/news/p3_2_1_3.jsp?lingua=italiano&menu=notizie&p=avvisi (accessed on 10 March 2022).
- Alertes Alimentaires. Sécurité Aimentaire. Le Gouvernement du Gran-Duché de Luxembourg. Available online: https://securite-alimentaire.public.lu/fr.html (accessed on 10 March 2022).
- Food Alerts. Latest News. Environmental Health Directorate, Government of Malta. Available online: https://deputyprimeminister.gov.mt/en/environmental/Pages/Home-Page.aspx (accessed on 10 March 2022).
- Veiligheidswaarschuwingen. Nederlandse Voedsel- en Warenautoriteit, (NVWA). Available online: https://www.nvwa.nl/onderwerpen/veiligheidswaarschuwingen/overzicht-veiligheidswaarschuwingen (accessed on 10 March 2022).
- Rechemare/Retragere Produse Alimentare. Autoritatea Națională Sanitară Veterinară și pentru Siguranța Alimentelor, (ANSVSA); Guvernul României. Available online: http://www.ansvsa.ro/informatii-pentru-public/produse-rechemateretrase/ (accessed on 10 March 2022).
- Obvestila Za Potrošnike. Uprava za varno hrano, veterinarstvo in varstvo rastlin.; Republika Slovenija. Available online: https://www.gov.si/drzavni-organi/organi-v-sestavi/uprava-za-varno-hrano-veterinarstvo-in-varstvo-rastlin/ (accessed on 10 March 2022).
- Alertas Alimentarias De Alérgenos. Seguridad Alimentaria.Agencia Española de Seguridad Alimentaria y Nutrición. Ministerio de Consumo. Gobierno de España. Available online: https://www.aesan.gob.es/AECOSAN/web/subhomes/seguridad_alimentaria/aecosan_seguridad_alimentaria.htm (accessed on 10 March 2022).
- HRana—Food-Related Warnings. Ministry of Agriculture. Government of the Republic of Croatia. Available online: https://hrana.mps.hr/HRana/ (accessed on 10 March 2022).



| Substances or Products Causing Allergies or Intolerances | Exceptions |
|---|---|
| - Cereals containing gluten, namely wheat, rye, barley, oats, spelt, kamut, or their hybridized strains, and products thereof | - Wheat-based glucose syrups, including dextrose - Wheat-based maltodextrins - Glucose syrups based on barley - Cereals used for making alcoholic distillates, including ethyl alcohol, of agricultural origin |
| - Crustaceans and products thereof | |
| - Eggs and products thereof | |
| - Fish and products thereof | (a) Fish gelatin used as a carrier for vitamin or carotenoid preparations (b) Fish gelatin or isinglass used as a fining agent in beer and wine |
| - Peanuts and products thereof | |
| - Soybeans and products thereof | (a) Fully refined soybean oil and fat (b) Natural, mixed tocopherols (E306); natural D-alpha tocopherol; natural D-alpha tocopherol acetate; and natural D-alpha tocopherol succinate from soybean sources (c) Vegetable-oil-derived phytosterols and phytosterol esters from soybean sources (d) Plant stanol ester produced from vegetable-oil sterols from soybean sources |
| - Milk and products thereof (including lactose) | - Whey used for making alcoholic distillates, including ethyl alcohol, of agricultural origin - Lactitol |
| - Nuts, namely almonds (Amygdalus communis L.), hazelnuts (Corylus avellana), walnuts (Juglans regia), cashews (Anacardium occidentale), pecans (Carya illinoinensis (Wangenh.) K. Koch), Brazil nuts (Bertholletia excelsa), pistachio nuts (Pistacia vera), macadamia or Queensland nuts (Macadamia ternifolia), and products thereof, except for nuts used in making alcoholic distillates, including ethyl alcohol, of agricultural origin | |
| - Celery and products thereof | |
| - Mustard and products thereof | |
| - Sesame seeds and products thereof | |
| - Sulfur dioxide and sulfites at concentrations of more than 10 mg/kg or 10 mg/L in terms of the total SO2, which are to be calculated for products proposed as ready for consumption or as reconstituted according to the instructions of the manufacturers | |
| - Lupin and products thereof | |
| - Mollusks and products thereof |
| Number of Allergens Present | % of Notifications |
|---|---|
| Two undeclared allergens | 62.0 |
| Three undeclared allergens | 24.1 |
| Four undeclared allergens | 4.4 |
| Five undeclared allergens | 8.0 |
| Six undeclared allergens | 1.5 |
| Label Declaration | Total Notifications (%) | Undeclared Allergens | Examples of Notification-Related Products |
|---|---|---|---|
| “Gluten-free” | 5.9 | Gluten, lactose, milk, soy, and nuts | Organic, gluten-free, chocolate-coated, crispy cereals; gluten-free bread; and gluten-free pasta |
| “Dairy-free” | 0.6 | Milk, nuts, and soy | Chilled, dairy-free, coconut milk yogurt |
| “Lactose-free” | 0.4 | Milk, lactoprotein, lactose, and gluten | Lactose-free biscuits with buckwheat and chocolate |
| “Lactose-free and gluten-free” | 0.4 | Milk, lactoprotein, nuts, and soy | Gluten- and lactose-free chocolate spread |
| “Milk- and gluten-free” | 0.2 | Gluten, milk | Milk- and gluten-free vegan choco dessert with coconut cream |
| “Lactose-free” and “milk-protein-free” | 0.1 | Milk | Lactose- and milk-protein-free cake cream |
| Product Claimed to be “Gluten-Free” | Quantity of Undeclared Gluten (mg/Kg—ppm) | Serving Portion (g) | Estimated Gluten Intake Dose (mg/Serving Portion) |
|---|---|---|---|
| Gluten-free corn pasta | 176 | 150 | 26.4 |
| Gluten-free cream preparation with potatoes and leeks | 31.6 | 210 | 6.6 |
| Gluten-free pasta | 75.3 | 150 | 1.3 |
| Gluten-free corn chips | 265 | 30 | 8.0 |
| Gluten-free peanut butter protein bar | 853 | 40 | 34.1 |
| Gluten-free hummus | >150 | 100 | 15.0 |
| Gluten-free hemp protein | 930 | 30 | 27.9 |
| Gluten-free buckwheat and sweet potato noodles | >80 | 150 | 1.0 |
| Gluten-free yellow lentil lasagna and spaghetti | 88 | 200 | 17.6 |
| Gluten-free vegetarian nuggets | 38 | 100 | 3.8 |
| Allergen | Notified Food Category | Notified Food Examples |
|---|---|---|
| Milk (lactoproteins and lactose) | Cereal and bakery products | Organic rice pancakes with dark chocolate, biscuits, and popcorn |
| Prepared dishes and snacks | Sausage rolls, grilled chips, and packed snacks | |
| Nuts | Cereal and bakery products | Pesto-and-walnut-plucked bread, chocolate pie, and energy cereal bars |
| Nuts, nut products, and seeds | Pistachio cream; fruit–nut mix; and peanut, nut, and mulberry mix | |
| Cocoa and cocoa preparations | Milk chocolate with buckwheat; chocolate; and chocolate spread | |
| Gluten | Cereal and bakery products | Rice-flour cake mix, sugar loaves, bulgur and pasta, and hot dog buns |
| Prepared dishes and snacks | Rice salad, baby food, and tortilla chips | |
| Egg | Cereal and bakery products | Donuts with cocoa coating, red velvet muffins, and bakery scones |
| Prepared dishes and snacks | Hummus and aioli, pizza, and prepared sandwiches | |
| Soya | Cereal and bakery products | Rice flour, cheese and onion bread, and butter croissants |
| Prepared dishes and snacks | Beef-flavored instant rice noodles, nacho-cheese snacks, and potato chips | |
| Peanut | Nuts, nut products, and seeds | Almond paste; nut mix; and roasted, organic, almond kernels |
| Confectionery | Baklava, wafer rolls with cream, and candies | |
| Fish | Dietetic foods, food supplements, and fortified foods | Food supplements and organic infant milk starter packs |
| Prepared dishes and snacks | Club-salad pasta, tuna and chicken, chilled tandoori chicken salad dishes, and salmon lasagna | |
| Seafood (mollusks and crustaceans) | Dietetic foods, food supplements, and fortified foods | Food supplements |
| Prepared dishes and snacks | Frozen cheese croquettes; frozen lamb and carrot dumplings; and chilled, spicy chicken salad |
| Country | Institution/ Public Organism | Website | |
|---|---|---|---|
| European Commission | RASFF consumers’ portal | https://webgate.ec.europa.eu/rasff-window/screen/consumers (accessed on 10 March 2022) | [14] |
| Austria | Austrian Agency for Health and Food Safety (AGES) | https://www.ages.at/en/human/product-warnings-product-recalls (accessed on 10 March 2022) | [46] |
| Belgium | Federal Agency for the Safety of the Food Chain (AFSCA) | https://www.favv-afsca.be/consommateurs/avertissements/ (accessed on 10 March 2022) | [47] |
| Croatia | Government of the Republic of Croatia | https://gov.hr/en/hrana-food-related-warnings/1774 (accessed on 10 March 2022) | [48] |
| France | Ministry of Agriculture and Food | https://rappel.conso.gouv.fr/categorie/1#navigation (accessed on 10 March 2022) | [49] |
| Germany | Federal Office of Consumer Protection and Food Safety | https://www.lebensmittelwarnung.de/bvl-lmwde/liste/lebensmittel/deutschlandweit/10/0 (accessed on 10 March 2022) | [50] |
| Greece | Hellenic Food Authority (EFET) | https://www.efet.gr/index.php/en/ (accessed on 10 March 2022) | [51] |
| Ireland | Food Safety Authority of Ireland | https://www.fsai.ie/ (accessed on 10 March 2022) | [52] |
| Italy | Ministry of Health | https://www.salute.gov.it/portale/news/p3_2_1_3.jsp?lingua=italiano&menu=notizie&p=avvisi (accessed on 10 March 2022) | [53] |
| Luxembourg | Food safety—Grand Duchy of Luxembourg | https://securite-alimentaire.public.lu/fr.html (accessed on 10 March 2022) | [54] |
| Malta | Environmental Health Directorate | https://deputyprimeminister.gov.mt/en/environmental/Pages/Home-Page.aspx (accessed on 10 March 2022) | [55] |
| Netherlands | Netherlands Food and Consumers Product Safety Authority | https://www.nvwa.nl/onderwerpen/veiligheidswaarschuwingen (accessed on 10 March 2022) | [56] |
| Romania | National Sanitary Veterinary and Food Safety Authority (ANSVSA) | http://www.ansvsa.ro/informatii-pentru-public/produse-rechemateretrase/ (accessed on 10 March 2022) | [57] |
| Slovenia | Republic of Slovenia | https://www.gov.si/drzavni-organi/organi-v-sestavi/uprava-za-varno-hrano-veterinarstvo-in-varstvo-rastlin/ (accessed on 10 March 2022) | [58] |
| Spain | Spanish Agency for Food Safety and Nutrition (AECOSAN) | https://www.aesan.gob.es/AECOSAN/web/subhomes/seguridad_alimentaria/aecosan_seguridad_alimentaria.htm (accessed on 10 March 2022) | [59] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Pineda, M.; Yagüe-Ruiz, C. The Risk of Undeclared Allergens on Food Labels for Pediatric Patients in the European Union. Nutrients 2022, 14, 1571. https://doi.org/10.3390/nu14081571
Martínez-Pineda M, Yagüe-Ruiz C. The Risk of Undeclared Allergens on Food Labels for Pediatric Patients in the European Union. Nutrients. 2022; 14(8):1571. https://doi.org/10.3390/nu14081571
Chicago/Turabian StyleMartínez-Pineda, Montserrat, and Cristina Yagüe-Ruiz. 2022. "The Risk of Undeclared Allergens on Food Labels for Pediatric Patients in the European Union" Nutrients 14, no. 8: 1571. https://doi.org/10.3390/nu14081571
APA StyleMartínez-Pineda, M., & Yagüe-Ruiz, C. (2022). The Risk of Undeclared Allergens on Food Labels for Pediatric Patients in the European Union. Nutrients, 14(8), 1571. https://doi.org/10.3390/nu14081571






