The Association between Dietary Purine Intake and Mortality: Evidence from the CHNS Cohort Study
Abstract
:1. Introduction
2. Methods
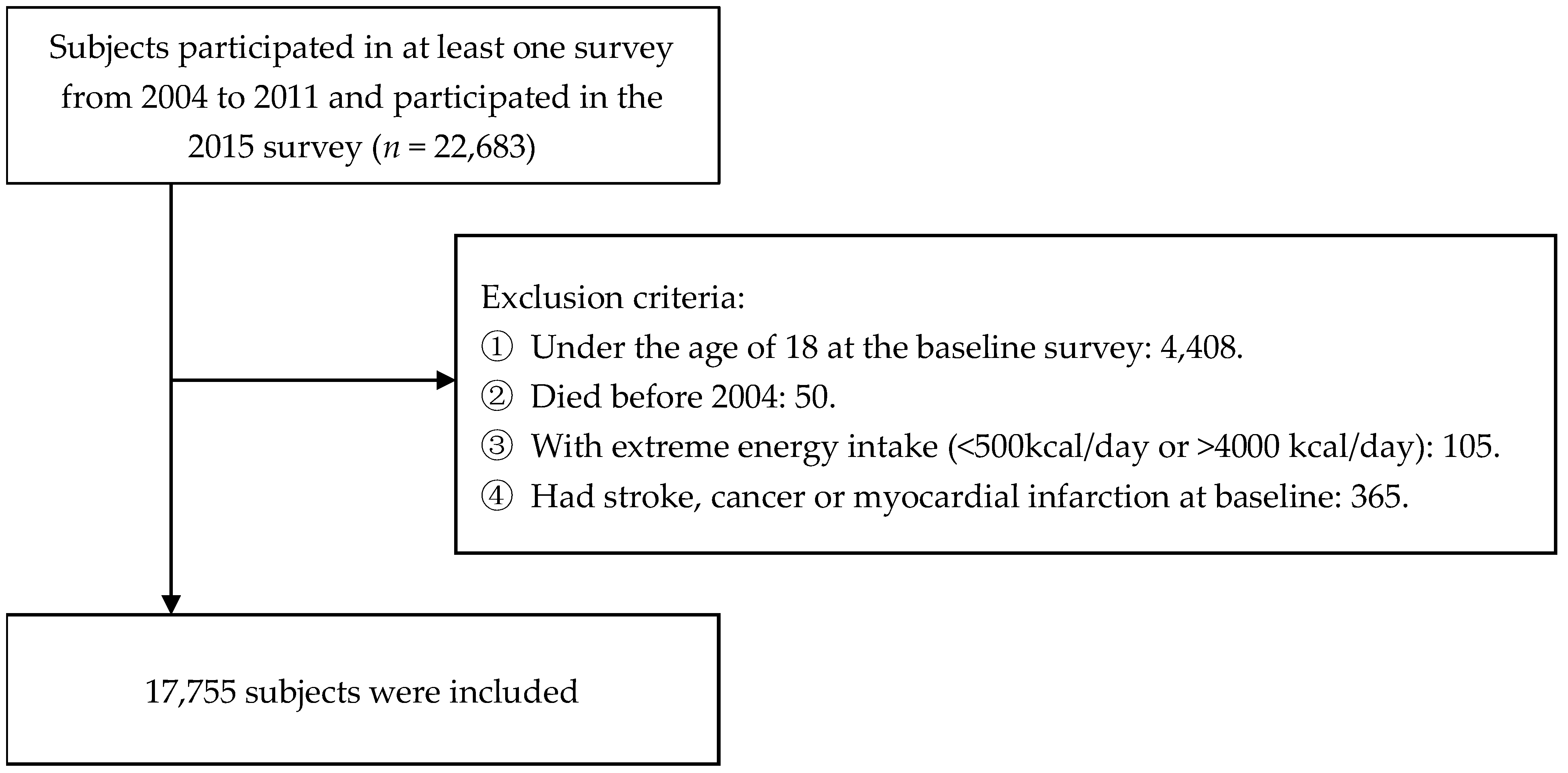
2.1. Study Design and Participants
2.2. Assessment of Purine Intake
2.3. Ascertainment of Deaths
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
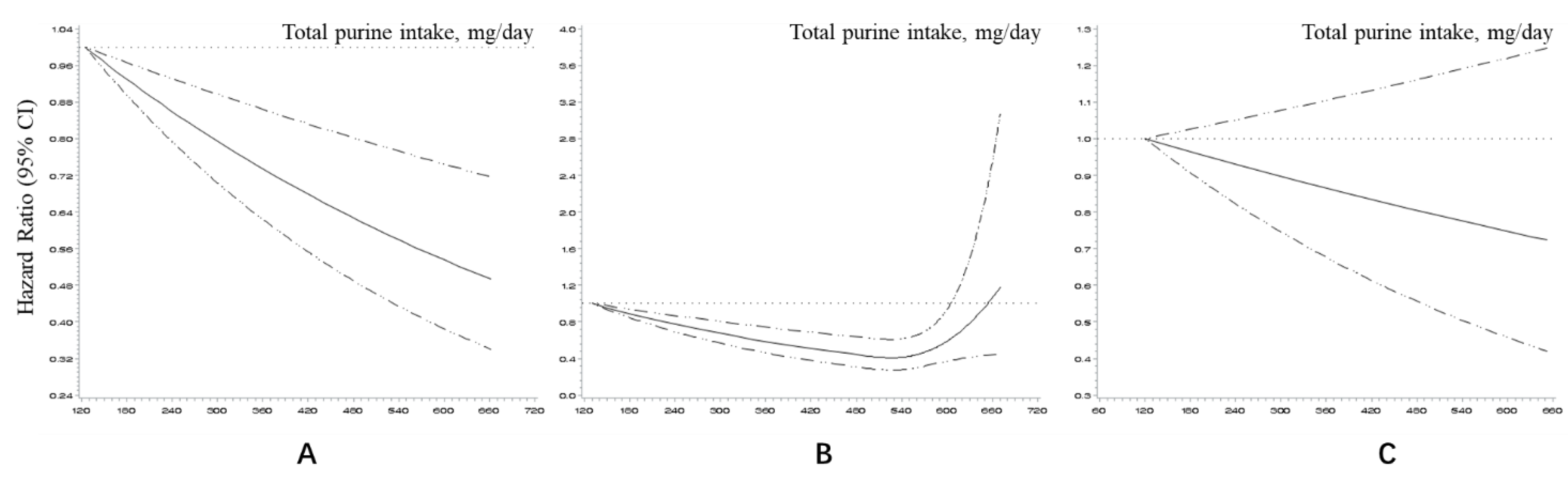
3.2. Association between Total Purine Intake and Mortality
3.3. Association between Purines from Different Food Sources and Mortality
3.4. Association between Total Purine Intake and Mortality among Different Genders
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, Z.; Xie, N.; Illes, P.; Di Virgilio, F.; Ulrich, H.; Semyanov, A.; Verkhratsky, A.; Sperlagh, B.; Yu, S.-G.; Huang, C.; et al. From purines to purinergic signalling: Molecular functions and human diseases. Signal Transduct. Target. Ther. 2021, 6, 162. [Google Scholar] [CrossRef] [PubMed]
- Richette, P.; Doherty, M.; Pascual, E.; Barskova, V.; Becce, F.; Castañeda-Sanabria, J.; Coyfish, M.; Guillo, S.; Jansen, T.L.; Janssens, H.; et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann. Rheum. Dis. 2017, 76, 29–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vedder, D.; Walrabenstein, W.; Heslinga, M.; De Vries, R.; Nurmohamed, M.; Van Schaardenburg, D.; Gerritsen, M. Dietary Interventions for Gout and Effect on Cardiovascular Risk Factors: A Systematic Review. Nutrients 2019, 11, 2955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuo, C.-F.; Grainge, M.; Zhang, W.; Doherty, M. Global epidemiology of gout: Prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 2015, 11, 649–662. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Han, C.; Wu, D.; Xia, X.; Gu, J.; Guan, H.; Shan, Z.; Teng, W. Prevalence of Hyperuricemia and Gout in Mainland China from 2000 to 2014: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2015, 2015, 762820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Y.; Pandya, B.J.; Choi, H.K. Comorbidities of Gout and Hyperuricemia in the US General Population: NHANES 2007–2008. Am. J. Med. 2012, 125, 679–687.e1. [Google Scholar] [CrossRef]
- Choi, H.K.; Curhan, G. Independent Impact of Gout on Mortality and Risk for Coronary Heart Disease. Circulation 2007, 116, 894–900. [Google Scholar] [CrossRef]
- Choi, H.K.; Atkinson, K.; Karlson, E.W.; Willett, W.; Curhan, G. Purine-Rich Foods, Dairy and Protein Intake, and the Risk of Gout in Men. N. Engl. J. Med. 2004, 350, 1093–1103. [Google Scholar] [CrossRef] [Green Version]
- Li, R.; Yu, K.; Li, C. Dietary factors and risk of gout and hyperuricemia: A meta-analysis and systematic review. Asia Pac. J. Clin. Nutr. 2018, 27, 1344–1356. [Google Scholar]
- Zgaga, L.; Theodoratou, E.; Kyle, J.; Farrington, S.M.; Agakov, F.; Tenesa, A.; Walker, M.; McNeill, G.; Wright, A.F.; Rudan, I.; et al. The Association of Dietary Intake of Purine-Rich Vegetables, Sugar-Sweetened Beverages and Dairy with Plasma Urate, in a Cross-Sectional Study. PLoS ONE 2012, 7, e38123. [Google Scholar] [CrossRef] [Green Version]
- Villegas, R.; Xiang, Y.-B.; Elasy, T.; Xu, W.; Cai, H.; Cai, Q.; Linton, M.; Fazio, S.; Zheng, W.; Shu, X.-O. Purine-rich foods, protein intake, and the prevalence of hyperuricemia: The Shanghai Men’s Health Study. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 409–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aihemaitijiang, S.; Zhang, Y.; Zhang, L.; Yang, J.; Ye, C.; Halimulati, M.; Zhang, W.; Zhang, Z. The Association between Purine-Rich Food Intake and Hyperuricemia: A Cross-Sectional Study in Chinese Adult Residents. Nutrients 2020, 12, 3835. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey—Monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2009, 39, 1435–1440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, M.-W.; Yu, H.-J.; Yuan, S.; Song, Y.; Tang, B.-W.; Cao, Z.-K.; Yang, X.-H.; Towne, S.D., Jr.; He, Q.-Q. Association between fruit and vegetable intake and the risk of hypertension among Chinese adults: A longitudinal study. Z. Ernährungswissenschaft 2018, 57, 2639–2647. [Google Scholar] [CrossRef]
- Zhou, J.; Leepromrath, S.; Tian, X.; Zhou, D. Dynamics of Chinese Diet Divergence from Chinese Food Pagoda and Its Association with Adiposity and Influential Factors: 2004–2011. Int. J. Environ. Res. Public Health 2020, 17, 507. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M.; Lu, B.; Zhai, F. Understanding the nutrition transition: Measuring rapid dietary changes in transitional countries. Public Health Nutr. 2002, 5, 947–953. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Hall, J.; Byles, J.; Shi, Z. Dietary Pattern Is Associated with Obesity in Older People in China: Data from China Health and Nutrition Survey (CHNS). Nutrients 2015, 7, 8170–8188. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y. China Food Composition Tables Standard Edition, 6th ed.; Peking University Medical Press: Beijing, China, 2018. (In Chinese) [Google Scholar]
- Wu, B.; Roseland, J.M.; Haytowitz, D.B.; Pehrsson, P.R.; Ershow, A.G. Availability and quality of published data on the purine content of foods, alcoholic beverages, and dietary supplements. J. Food Compos. Anal. 2019, 84, 103281. [Google Scholar] [CrossRef]
- Stringhini, S.; Carmeli, C.; Jokela, M.; Avendano, M.; Muennig, P.; Guida, F.; Ricceri, F.; D’Errico, A.; Barros, H.; Bochud, M.; et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: A multicohort study and meta-analysis of 1·7 million men and women. Lancet 2017, 389, 1229–1237. [Google Scholar] [CrossRef] [Green Version]
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef] [Green Version]
- GBD 2016 Risk Factors Collaborators. Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef] [Green Version]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R., Jr.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities: A Second Update of Codes and MET Values. Med. Sci. Sport. Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willett, W.; Willett, W.C.; Willett, W.; Stampfer, M.J. Nutrition Epidemiology; Oxford University Press: Oxford, UK, 1998. [Google Scholar]
- Buuren, S.V. Multiple Imputation of Discrete and Continuous Data by Fully Conditional Specification. Stat. Methods Med. Res. 2007, 16, 219–242. [Google Scholar] [CrossRef] [PubMed]
- Cox, P.; Gupta, S.; Zhao, S.S.; Hughes, D.M. The incidence and prevalence of cardiovascular diseases in gout: A systematic review and meta-analysis. Rheumatol. Int. 2021, 41, 1209–1219. [Google Scholar] [CrossRef] [PubMed]
- Feig, D.I.; Kang, D.H.; Johnson, R.J. Uric acid and cardiovascular risk. N. Engl. J. Med. 2008, 359, 1811–1821. [Google Scholar] [CrossRef]
- Ragab, G.; Elshahaly, M.; Bardin, T. Gout: An old disease in new perspective—A review. J. Adv. Res. 2017, 8, 495–511. [Google Scholar] [CrossRef]
- Shahin, L.; Patel, K.M.; Heydari, M.K.; Kesselman, M.M. Hyperuricemia and Cardiovascular Risk. Cureus 2021, 13, e14855. [Google Scholar] [CrossRef]
- Rai, S.K.; Fung, T.T.; Lu, N.; Keller, S.F.; Curhan, G.C.; Choi, H.K. The Dietary Approaches to Stop Hypertension (DASH) diet, Western diet, and risk of gout in men: Prospective cohort study. BMJ 2017, 357, j1794. [Google Scholar] [CrossRef] [Green Version]
- Teng, G.G.; Pan, A.; Yuan, J.-M.; Koh, W.-P. Food Sources of Protein and Risk of Incident Gout in the Singapore Chinese Health Study. Arthritis Rheumatol. 2015, 67, 1933–1942. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Chen, C.; Choi, H.; Chaisson, C.; Hunter, D.J.; Niu, J.; Neogi, T. Purine-rich foods intake and recurrent gout attacks. Ann. Rheum. Dis. 2012, 71, 1448–1453. [Google Scholar] [CrossRef] [Green Version]
- Choi, H.K.; Liu, S.; Curhan, G. Intake of purine-rich foods, protein, and dairy products and relationship to serum levels of uric acid: The Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2005, 52, 283–289. [Google Scholar] [CrossRef] [PubMed]
- You, H.; Chen, K.; Han, P.; Yue, C.; Zhao, X. U-Shaped Relationship Between Cardiovascular Mortality and Serum Uric Acid May Be Attributed to Stroke- and Heart-Specific Mortality, Respectively, Among Hypertensive Patients: A Nationally Representative Cohort Study. Med Sci. Monit. 2020, 27, e928937-1. [Google Scholar] [CrossRef] [PubMed]
- Konta, T.; Ichikawa, K.; Kawasaki, R.; Fujimoto, S.; Iseki, K.; Moriyama, T.; Yamagata, K.; Tsuruya, K.; Narita, I.; Kondo, M.; et al. Association between serum uric acid levels and mortality: A nationwide community-based cohort study. Sci. Rep. 2020, 10, 6066. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.; Go, S.; Son, H.E.; Ryu, J.Y.; Lee, H.; Heo, N.J.; Chin, H.J.; Park, J.H. Association between Serum Uric Acid Level and ESRD or Death in a Korean Population. J. Korean Med Sci. 2020, 35, e254. [Google Scholar] [CrossRef]
- Odden, M.C.; Amadu, A.-R.; Smit, E.; Lo, L.; Peralta, C.A. Uric Acid Levels, Kidney Function, and Cardiovascular Mortality in US Adults: National Health and Nutrition Examination Survey (NHANES) 1988–1994 and 1999–2002. Am. J. Kidney Dis. 2014, 64, 550–557. [Google Scholar] [CrossRef] [Green Version]
- Mozaffarian, D.; Hao, T.; Rimm, E.B.; Willett, W.C.; Hu, F.B. Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and Men. N. Engl. J. Med. 2011, 364, 2392–2404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shin, S.-A.; Joo, B.J.; Lee, J.; Ryu, G.; Han, M.; Kim, W.-Y.; Park, H.H.; Lee, J.; Lee, C.S. Phytochemicals as Anti-Inflammatory Agents in Animal Models of Prevalent Inflammatory Diseases. Molecules 2020, 25, 5932. [Google Scholar] [CrossRef]
- Jakše, B.; Pajek, M. Uric Acid and Plant-Based Nutrition. Nutrients 2019, 11, 1736. [Google Scholar] [CrossRef] [Green Version]
- Evans, P.L.; Prior, J.A.; Belcher, J.; Hay, C.A.; Mallen, C.; Roddy, E. Gender-specific risk factors for gout: A systematic review of cohort studies. Adv. Rheumatol. 2019, 59, 24. [Google Scholar] [CrossRef]
- Dalbeth, N.; Merriman, T.R.; Stamp, L.K. Gout. Lancet 2016, 388, 2039–2052. [Google Scholar] [CrossRef]
- Liu, B.; Wang, T.; Zhao, H.N.; Yue, W.W.; Yu, H.P.; Liu, C.X.; Yin, J.; Jia, R.Y.; Nie, H.W. The prevalence of hyperuricemia in China: A meta-analysis. BMC Public Health 2011, 11, 832. [Google Scholar] [CrossRef] [Green Version]
- Dehlin, M.; Jacobsson, L.; Roddy, E. Global epidemiology of gout: Prevalence, incidence, treatment patterns and risk factors. Nat. Rev. Rheumatol. 2020, 16, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Miao, Z.; Li, C.; Chen, Y.; Zhao, S.; Wang, Y.; Wang, Z.; Chen, X.; Xu, F.; Wang, F.; Sun, R.; et al. Dietary and lifestyle changes associated with high prevalence of hyperuricemia and gout in the Shandong coastal cities of Eastern China. J. Rheumatol. 2008, 35, 1859–1864. [Google Scholar] [PubMed]
- Hak, A.E.; Curhan, G.C.; Grodstein, F.; Choi, H.K. Menopause, postmenopausal hormone use and risk of incident gout. Ann. Rheum. Dis. 2009, 69, 1305–1309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sumino, H.; Ichikawa, S.; Kanda, T.; Nakamura, T.; Sakamaki, T. Reduction of serum uric acid by hormone replacement therapy in postmenopausal women with hyperuricaemia. Lancet 1999, 354, 650. [Google Scholar] [CrossRef]
- Zhang, W.; Iso, H.; Murakami, Y.; Miura, K.; Nagai, M.; Sugiyama, D.; Ueshima, H.; Okamura, T.; EPOCH-JAPAN Group. Correction:Serum Uric Acid and Mortality Form Cardiovascular Disease:EPOCH-JAPAN Study. J. Atheroscler. Thromb. 2016, 23, 1365–1366. [Google Scholar] [CrossRef] [Green Version]
- Cho, S.K.; Chang, Y.; Kim, I.; Ryu, S. U-Shaped Association Between Serum Uric Acid Level and Risk of Mortality: A Cohort Study. Arthritis Rheumatol. 2018, 70, 1122–1132. [Google Scholar] [CrossRef] [Green Version]
| Quintiles of Purine Intake | p for Trend b | |||||
|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | ||
| n | 3551 | 3551 | 3551 | 3551 | 3551 | |
| Mean purine intake, mg/day | 168.75 ± 36.22 | 246.87 ± 17.80 | 308.71 ± 18.43 | 380.00 ± 24.57 | 541.39 ± 136.97 | <0.001 |
| Age, year | 51.18 ± 17.68 | 49.37 ± 16.47 | 48.60 ± 15.84 | 48.83 ± 15.28 | 48.26 ± 15.19 | <0.001 |
| Male, % | 42.6 | 47.0 | 46.4 | 48.8 | 51.8 | <0.001 |
| Urban residence, % | 31.5 | 36.2 | 39.6 | 43.9 | 50.2 | <0.001 |
| Income, CNY/year | 11,953.33 ± 16,156.92 | 14,319.05 ± 19,170.48 | 15,366.37 ± 20,335.71 | 18,131.56 ± 25,167.13 | 21,743.00 ± 33,291.38 | <0.001 |
| Education year, year | 7.16 ± 4.37 | 8.00 ± 4.19 | 8.35 ± 4.14 | 8.77 ± 4.07 | 9.10 ± 4.02 | <0.001 |
| Energy intake, kcal/day | 1915.71 ± 720.66 | 2011.52 ± 658.91 | 1988.82 ± 629.17 | 1970.03 ± 588.96 | 1872.56 ± 548.00 | 0.069 |
| Carbohydrate intake, g/day | 271.74 ± 115.78 | 284.61 ± 111.10 | 272.41 ± 105.19 | 253.47 ± 93.56 | 220.59 ± 83.02 | <0.001 |
| Protein intake, g/day | 53.69 ± 24.04 | 59.42 ± 22.03 | 63.03 ± 20.97 | 68.19 ± 21.47 | 75.81 ± 24.59 | <0.001 |
| Fat intake, g/day | 65.69 ± 40.16 | 68.15 ± 36.61 | 70.24 ± 34.02 | 74.32 ± 33.38 | 74.50 ± 32.04 | <0.001 |
| BMI, kg/m2 | 23.41 ± 4.29 | 23.27 ± 3.52 | 23.23 ± 3.72 | 23.28 ± 3.41 | 23.37 ± 3.59 | 0.819 |
| Smoke, % | 29.4 | 30.5 | 30.1 | 31.7 | 34.3 | <0.001 |
| Drink alcohol, % | 31.0 | 33.5 | 32.2 | 34.4 | 37.8 | <0.001 |
| Physical activity, MET-H/day | 21.71 ± 19.72 | 23.05 ± 19.61 | 23.35 ± 17.70 | 22.98 ± 16.69 | 23.27 ± 16.05 | <0.001 |
| Diabetes, % | 2.1 | 2.1 | 2.1 | 2.2 | 2.6 | 0.155 |
| Hypertension, % | 9.6 | 9.2 | 8.4 | 10.1 | 11.3 | 0.008 |
| Uric acid, μmol/L | 287.73 ± 95.60 | 303.95 ± 100.50 | 310.18 ± 101.35 | 313.01 ± 111.99 | 327.95 ± 119.06 | <0.001 |
| Person-year | 8.73 ± 2.96 | 8.67 ± 2.92 | 8.44 ± 3.02 | 8.16 ± 3.09 | 7.61 ± 3.20 | <0.001 |
| Death, % | 6.6 | 4.8 | 3.9 | 3.7 | 2.3 | <0.001 |
| Quintiles of Purine Intake | p for Trend b | |||||
|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | ||
| Total purine | ||||||
| Median intake, mg/day | 179.43 | 251.44 | 313.39 | 384.92 | 514.94 | |
| Deaths, cases/total | 235/3551 | 171/3551 | 137/3551 | 132/3551 | 83/3551 | |
| Model 1 c | 1.00 | 0.81 (0.67–0.99) | 0.74 (0.60–0.92) | 0.73 (0.59–0.91) | 0.49 (0.38–0.63) | <0.001 |
| Model 2 d | 1.00 | 0.90 (0.74–1.10) | 0.85 (0.68–1.05) | 0.87 (0.70–1.08) | 0.60 (0.47–0.78) | <0.001 |
| Model 3 e | 1.00 | 0.90 (0.74–1.10) | 0.84 (0.68–1.04) | 0.86 (0.70–1.07) | 0.60 (0.46–0.77) | <0.001 |
| Model 3 + protein intake | 1.00 | 0.94 (0.77–1.14) | 0.91 (0.73–1.13) | 0.98 (0.78–1.23) | 0.74 (0.56–0.99) | 0.144 |
| Animal-derived purine | ||||||
| Median intake, mg/day | 23.66 | 78.46 | 131.93 | 192.41 | 305.52 | |
| Deaths, cases/total | 268/4472 | 153/3321 | 140/3321 | 119/3321 | 78/3320 | |
| Model 1 | 1.00 | 0.86 (0.70–1.04) | 0.87 (0.71–1.07) | 0.78 (0.63–0.97) | 0.53 (0.41–0.69) | <0.001 |
| Model 2 | 1.00 | 1.02 (0.83–1.25) | 1.03 (0.84–1.27) | 1.00 (0.80–1.24) | 0.72 (0.56–0.93) | 0.067 |
| Model 3 | 1.00 | 1.03 (0.84–1.25) | 1.03 (0.84–1.27) | 0.99 (0.80–1.24) | 0.71 (0.55–0.92) | 0.052 |
| Model 3 + protein intake | 1.00 | 1.06 (0.87–1.30) | 1.11 (0.90–1.38) | 1.12 (0.89–1.41) | 0.92 (0.69–1.23) | 0.778 |
| Plant-derived purine | ||||||
| Median intake, mg/day | 112.9 | 149.98 | 178.06 | 212.2 | 280.53 | |
| Deaths, cases/total | 197/3552 | 152/3551 | 149/3550 | 148/3551 | 112/3551 | |
| Model 1 | 1.00 | 0.88 (0.71–1.09) | 0.87 (0.70–1.08) | 0.87 (0.70–1.08) | 0.67 (0.53–0.85) | 0.003 |
| Model 2 | 1.00 | 0.92 (0.74–1.14) | 0.86 (0.69–1.07) | 0.88 (0.71–1.10) | 0.64 (0.51–0.81) | 0.001 |
| Model 3 | 1.00 | 0.91 (0.73–1.13) | 0.86 (0.69–1.07) | 0.89 (0.71–1.10) | 0.64 (0.51–0.81) | 0.001 |
| Model 3 + protein intake | 1.00 | 0.93 (0.75–1.15) | 0.90 (0.72–1.12) | 0.94 (0.75–1.17) | 0.71 (0.56–0.90) | 0.019 |
| Quintiles of Purine Intake | p for Trend b | |||||
|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | ||
| Total purine | ||||||
| Median intake, mg/day | 182.52 | 251.83 | 314.81 | 385.98 | 517.37 | |
| Deaths, cases/total | 129/1512 | 97/1670 | 74/1649 | 80/1733 | 46/1841 | |
| Model 1 c | 1.00 | 0.73 (0.56–0.95) | 0.65 (0.49–0.87) | 0.67 (0.51–0.89) | 0.40 (0.29–0.56) | <0.001 |
| Model 2 d | 1.00 | 0.78 (0.60–1.02) | 0.73 (0.55–0.98) | 0.77 (0.58–1.02) | 0.48 (0.34–0.68) | <0.001 |
| Model 3 e | 1.00 | 0.78 (0.60–1.02) | 0.73 (0.54–0.97) | 0.77 (0.58–1.02) | 0.47 (0.34–0.67) | <0.001 |
| Model 3 + protein intake | 1.00 | 0.83 (0.64–1.09) | 0.81 (0.61–1.09) | 0.94 (0.69–1.27) | 0.67 (0.46–0.97) | 0.127 |
| Animal-derived purine | ||||||
| Median intake, mg/day | 8.65 | 83.28 | 136.66 | 195.74 | 311.35 | |
| Deaths, cases/total | 153/2032 | 84/1509 | 71/1545 | 69/1610 | 49/1709 | |
| Model 1 | 1.00 | 0.81 (0.62–1.06) | 0.72 (0.54–0.95) | 0.72 (0.54–0.95) | 0.51 (0.37–0.70) | <0.001 |
| Model 2 | 1.00 | 0.97 (0.74–1.27) | 0.84 (0.63–1.12) | 0.91 (0.68–1.21) | 0.67 (0.48–0.93) | 0.024 |
| Model 3 | 1.00 | 0.97 (0.74–1.27) | 0.84 (0.63–1.12) | 0.91 (0.68–1.21) | 0.66 (0.48–0.92) | 0.022 |
| Model 3 + protein intake | 1.00 | 1.02 (0.78–1.34) | 0.94 (0.70–1.26) | 1.10 (0.81–1.49) | 0.99 (0.68–1.43) | 0.876 |
| Plant-derived purine | ||||||
| Median intake, mg/day | 107.24 | 148.35 | 185.21 | 219.1 | 290.85 | |
| Deaths, cases/total | 94/1423 | 88/1574 | 89/1731 | 90/1799 | 65/1878 | |
| Model 1 | 1.00 | 0.96 (0.72–1.28) | 0.89 (0.67–1.19) | 0.90 (0.67–1.20) | 0.63 (0.46–0.87) | 0.007 |
| Model 2 | 1.00 | 0.96 (0.71–1.28) | 0.84 (0.62–1.12) | 0.86 (0.64–1.16) | 0.58 (0.42–0.80) | 0.001 |
| Model 3 | 1.00 | 0.95 (0.71–1.27) | 0.84 (0.63–1.13) | 0.87 (0.65–1.16) | 0.58 (0.42–0.79) | 0.001 |
| Model 3 + protein intake | 1.00 | 0.98 (0.73–1.31) | 0.89 (0.66–1.20) | 0.94 (0.70–1.27) | 0.67 (0.48–0.92) | 0.027 |
| Quintiles of Purine Intake | p for Trend b | |||||
|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | ||
| Total purine | ||||||
| Median intake, mg/day | 176.76 | 251.16 | 312.09 | 384.04 | 512.74 | |
| Deaths, cases/total | 106/2039 | 74/1881 | 63/1902 | 52/1818 | 37/1710 | |
| Model 1 c | 1.00 | 0.94 (0.70–1.26) | 0.87 (0.63–1.19) | 0.82 (0.59–1.14) | 0.64 (0.44–0.94) | 0.019 |
| Model 2 d | 1.00 | 1.09 (0.81–1.47) | 1.01 (0.74–1.39) | 1.04 (0.74–1.46) | 0.83 (0.56–1.21) | 0.454 |
| Model 3 e | 1.00 | 1.09 (0.81–1.47) | 1.00 (0.73–1.38) | 1.03 (0.74–1.45) | 0.82 (0.56–1.20) | 0.415 |
| Model 3 + protein intake | 1.00 | 1.10 (0.81–1.49) | 1.03 (0.74–1.42) | 1.07 (0.75–1.53) | 0.88 (0.57–1.35) | 0.773 |
| Animal-derived purine | ||||||
| Median intake, mg/day | 1.12 | 68.86 | 115.99 | 170.03 | 277.6 | |
| Deaths, cases/total | 115/2440 | 69/1812 | 69/1776 | 50/1711 | 29/1611 | |
| Model 1 | 1.00 | 0.92 (0.68–1.24) | 1.09 (0.81–1.47) | 0.88 (0.63–1.22) | 0.57 (0.38–0.86) | 0.030 |
| Model 2 | 1.00 | 1.09 (0.81–1.48) | 1.31 (0.97–1.78) | 1.14 (0.81–1.60) | 0.81 (0.53–1.23) | 0.965 |
| Model 3 | 1.00 | 1.10 (0.81–1.49) | 1.32 (0.98–1.79) | 1.12 (0.80–1.58) | 0.80 (0.52–1.21) | 0.879 |
| Model 3 + protein intake | 1.00 | 1.11 (0.82–1.51) | 1.36 (1.00–1.85) | 1.17 (0.82–1.65) | 0.87 (0.55–1.37) | 0.693 |
| Plant-derived purine | ||||||
| Median intake, mg/day | 95.77 | 135.03 | 164.62 | 197.46 | 263.31 | |
| Deaths, cases/total | 103/2129 | 64/1977 | 60/1819 | 58/1752 | 47/1673 | |
| Model 1 | 1.00 | 0.80 (0.59–1.10) | 0.86 (0.62–1.18) | 0.85 (0.62–1.18) | 0.74 (0.53–1.05) | 0.140 |
| Model 2 | 1.00 | 0.88 (0.64–1.21) | 0.91 (0.66–1.26) | 0.95 (0.68–1.32) | 0.77 (0.54–1.10) | 0.257 |
| Model 3 | 1.00 | 0.87 (0.64–1.20) | 0.90 (0.65–1.25) | 0.95 (0.68–1.32) | 0.77 (0.54–1.10) | 0.275 |
| Model 3 + protein intake | 1.00 | 0.88 (0.64–1.20) | 0.91 (0.66–1.27) | 0.96 (0.69–1.35) | 0.80 (0.56–1.16) | 0.392 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, M.; Liu, Y.; Wu, L.; Liu, H.; Wang, Y.; Chen, F.; Pei, L.; Zhao, Y.; Zeng, L.; Dang, S.; et al. The Association between Dietary Purine Intake and Mortality: Evidence from the CHNS Cohort Study. Nutrients 2022, 14, 1718. https://doi.org/10.3390/nu14091718
Yan M, Liu Y, Wu L, Liu H, Wang Y, Chen F, Pei L, Zhao Y, Zeng L, Dang S, et al. The Association between Dietary Purine Intake and Mortality: Evidence from the CHNS Cohort Study. Nutrients. 2022; 14(9):1718. https://doi.org/10.3390/nu14091718
Chicago/Turabian StyleYan, Miaojia, Yezhou Liu, Lichen Wu, Huimeng Liu, Yutong Wang, Fangyao Chen, Leilei Pei, Yaling Zhao, Lingxia Zeng, Shaonong Dang, and et al. 2022. "The Association between Dietary Purine Intake and Mortality: Evidence from the CHNS Cohort Study" Nutrients 14, no. 9: 1718. https://doi.org/10.3390/nu14091718
APA StyleYan, M., Liu, Y., Wu, L., Liu, H., Wang, Y., Chen, F., Pei, L., Zhao, Y., Zeng, L., Dang, S., Yan, H., & Mi, B. (2022). The Association between Dietary Purine Intake and Mortality: Evidence from the CHNS Cohort Study. Nutrients, 14(9), 1718. https://doi.org/10.3390/nu14091718







