Behavioral Health Risk Factors and Motivation to Change among Cardiovascular General Hospital Patients Aged 50 to 79 Years
Abstract
:1. Introduction
2. Materials and Methods
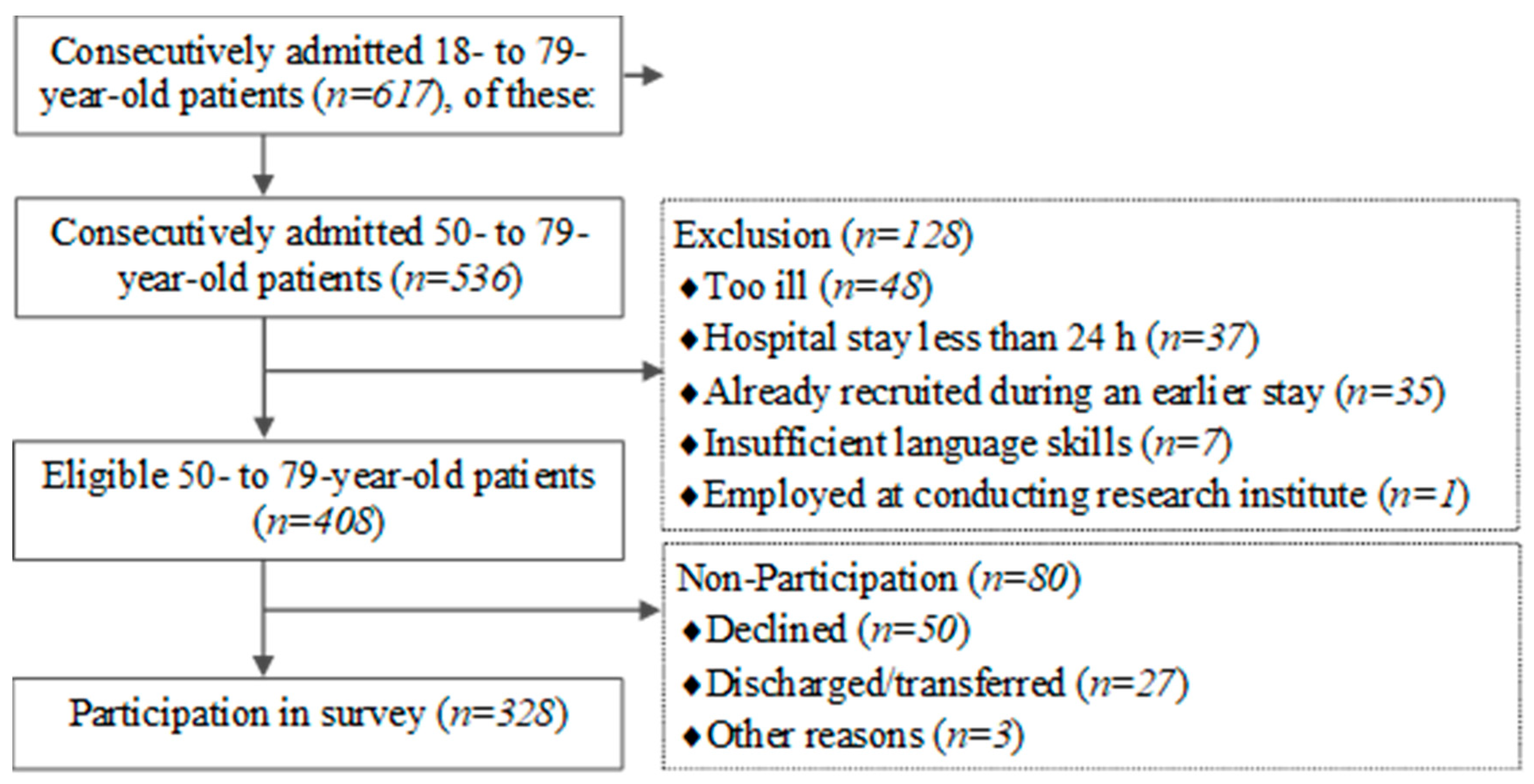
Sampling Frame and Participants
3. Measures
3.1. Behavioral Health Risk Factors
3.2. Motivation to Change Behavioral Health Risk Factors
4. Other Measures
Statistical Analysis
5. Results
5.1. Sample Characteristics
5.2. Occurrence and Co-Occurrence of Behavioral Health Risk Factors
5.3. Associations of Sociodemographic Characteristics and Number of HRFs
5.4. Motivation to Change Regarding Recommended Health Behaviors
5.5. Additional Analyses of Dietary Habits
6. Discussion
7. Strengths
8. Limitations
9. Conclusions
10. Clinical Implications
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lutz, W.; Sanderson, W.; Scherbov, S. The coming acceleration of global population ageing. Nature 2008, 451, 716–719. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Report on Ageing and Health. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=07ABF9577D09C40B02EEFF70B6A6A227?sequence=1 (accessed on 4 January 2022).
- GBD Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Kamineni, A.; Carnethon, M.; Djousse, L.; Mukamal, K.J.; Siscovick, D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: The cardiovascular health study. Arch. Int. Med. 2009, 69, 798–807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ford, E.S.; Bergmann, M.M.; Kroger, J.; Schienkiewitz, A.; Weikert, C.; Boeing, H. Healthy living is the best revenge: Findings from the European Prospective Investigation Into Cancer and Nutrition-Potsdam study. Arch. Int. Med. 2009, 69, 1355–1362. [Google Scholar]
- Khaw, K.T.; Wareham, N.; Bingham, S.; Welch, A.; Luben, R.; Day, N. Combined impact of health behaviours and mortality in men and women: The EPIC-Norfolk prospective population study. PLoS Med. 2008, 5, e12. [Google Scholar]
- Loef, M.; Walach, H. The combined effects of healthy lifestyle behaviors on all cause mortality: A systematic review and meta-analysis. Prev. Med. 2012, 55, 163–170. [Google Scholar] [CrossRef]
- Manuel, D.G.; Perez, R.; Sanmartin, C.; Taljaard, M.; Hennessy, D.; Wilson, K.; Tanuseputro, P.; Manson, H.; Bennett, C.; Tuna, M.; et al. Measuring Burden of Unhealthy Behaviours Using a Multivariable Predictive Approach: Life Expectancy Lost in Canada Attributable to Smoking, Alcohol, Physical Inactivity, and Diet. PLoS Med. 2016, 13, e1002082. [Google Scholar] [CrossRef]
- Petersen, K.E.N.; Johnsen, N.F.; Olsen, A.; Albieri, V.; Olsen, L.K.H.; Dragsted, L.O.; Overvad, K.; Tjønneland, A.; Egeberg, R. The combined impact of adherence to five lifestyle factors on all-cause, cancer and cardiovascular mortality: A prospective cohort study among Danish men and women. Br. J. Nutr. 2015, 113, 849–858. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.B.; Pan, X.F.; Chen, J.; Cao, A.; Xia, L.; Zhang, Y.; Wang, J.; Li, H.; Liu, G.; Pan, A. Combined lifestyle factors, all-cause mortality and cardiovascular disease: A systematic review and meta-analysis of prospective cohort studies. J. Epidemiol. Commun. Health 2021, 75, 92–99. [Google Scholar] [CrossRef]
- Conry, M.C.; Morgan, K.; Curry, P.; McGee, H.; Harrington, J.; Ward, M.; Shelley, E. The clustering of health behaviours in Ireland and their relationship with mental health, self-rated health and quality of life. BMC Public Health 2011, 11, 692. [Google Scholar] [CrossRef] [PubMed]
- Hubert, H.B.; Bloch, D.A.; Oehlert, J.W.; Fries, J.F. Lifestyle Habits and Compression of Morbidity. J. Gerontol. Ser. A 2002, 57, M347–M351. [Google Scholar] [CrossRef] [PubMed]
- Yates, L.B.; Djoussé, L.; Kurth, T.; Buring, J.E.; Gaziano, J.M. Exceptional Longevity in Men: Modifiable Factors Associated with Survival and Function to Age 90 Years. Obstet. Gynecol. Surv. 2008, 64, 28–29. [Google Scholar] [CrossRef]
- Vita, A.J.; Terry, R.B.; Hubert, H.B.; Fries, J.F. Aging, health risks, and cumulative disability. N. Engl. J. Med. 1998, 338, 1035–1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.; Park, K.H. Health practices that predict recovery from functional limitations in older adults. Am. J. Prev. Med. 2006, 31, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.M.; Jameson, K.A.; Syddall, H.E.; Dennison, E.M.; Cooper, C.; Sayer, A.A. Hertfordshire Cohort Study Group; The Hertfordshire Cohort Study Group Clustering of lifestyle risk factors and poor physical function in older adults: The Hertfordshire cohort study. J. Am. Geriatr. Soc. 2013, 61, 1684–1691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beydoun, M.A.; Beydoun, H.A.; Gamaldo, A.A.; Teel, A.; Zonderman, A.B.; Wang, Y. Epidemiologic studies of modifiable factors associated with cognition and dementia: Systematic review and meta-analysis. BMC Public Health 2014, 14, 643. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.; Back, J.H.; Kim, J.; Kim, S.-H.; Na, D.L.; Cheong, H.-K.; Hong, C.H.; Kim, Y.G. Systematic review of health behavioral risks and cognitive health in older adults. Int. Psychogeriatr. 2010, 22, 174–187. [Google Scholar] [CrossRef]
- Elwood, P.; Galante, J.; Pickering, J.; Palmer, S.; Bayer, A.; Ben-Shlomo, Y.; Longley, M.; Gallacher, J. Healthy Lifestyles Reduce the Incidence of Chronic Diseases and Dementia: Evidence from the Caerphilly Cohort Study. PLoS ONE 2013, 8, e81877. [Google Scholar] [CrossRef]
- Czapla, M.; Karniej, P.; Juárez-Vela, R.; Łokieć, K. The Association between Nutritional Status and In-Hospital Mortality among Patients with Acute Coronary Syndrome—A Result of the Retrospective Nutritional Status Heart Study (NSHS). Nutrients 2020, 12, 3091. [Google Scholar] [CrossRef]
- Kałużna-Oleksy, M.; Krysztofiak, H.; Migaj, J.; Wleklik, M.; Dudek, M.; Uchmanowicz, I.; Lesiak, M.; Straburzyńska-Migaj, E. Relationship between Nutritional Status and Clinical and Biochemical Parameters in Hospitalized Patients with Heart Failure with Reduced Ejection Fraction, with 1-Year Follow-Up. Nutrients 2020, 12, 2330. [Google Scholar] [CrossRef] [PubMed]
- Linardakis, M.; Papadaki, A.; Smpokos, E.; Komninos, Y.; Philalithis, A. Multiple behavioral risk factors for chronic diseases in adults aged 50+: Regional differences across eleven European countries. J. Public Health 2013, 22, 101–109. [Google Scholar] [CrossRef]
- John, U.; Hanke, M.; Freyer-Adam, J. Health Risk Behavior Patterns in a National Adult Population Survey. Int. J. Environ. Res. Public Health 2018, 15, 873. [Google Scholar] [CrossRef] [Green Version]
- Noble, N.; Paul, C.; Turon, H.; Oldmeadow, C. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev. Med. 2015, 81, 16–41. [Google Scholar] [CrossRef]
- Meader, N.; King, K.; Moe-Byrne, T.; Wright, K.; Graham, H.; Petticrew, M.; Power, C.; White, M.; Sowden, A.J. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health 2016, 16, 657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saß, A.; Wurm, S.; Ziese, T. Age = Illness? Health condition and health development. In Beiträge zur Gesundheitsberichterstattung des Bundes: Gesundheit und Krankheit im Alter; Robert Koch-Institute: Berlin, Germany, 2009; pp. 31–61. [Google Scholar]
- Haveman-Nies, A.; de Groot, L.; Burema, J.; Cruz, J.A.A.; Osler, M.; Van Staveren, W.A. Dietary Quality and Lifestyle Factors in Relation to 10-Year Mortality in Older Europeans: The SENECA Study. Am. J. Epidemiol. 2002, 156, 962–968. [Google Scholar] [CrossRef]
- Tran, B.; Falster, M.O.; Douglas, K.; Blyth, F.; Jorm, L.R. Health Behaviours and Potentially Preventable Hospitalisation: A Prospective Study of Older Australian Adults. PLoS ONE 2014, 9, e93111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Syddall, H.E.; Westbury, L.D.; Simmonds, S.J.; Robinson, S.; Cooper, C.; Sayer, A.A. Understanding poor health behaviours as predictors of different types of hospital admission in older people: Findings from the Hertfordshire Cohort Study. J. Epidemiol. Commun. Health 2016, 70, 292–298. [Google Scholar] [CrossRef] [Green Version]
- Freyer-Adam, J.; Noetzel, F.; Baumann, S.; Aghdassi, A.A.; Siewert-Markus, U.; Gaertner, B.; John, U. Behavioral health risk factor profiles in general hospital patients: Identifying the need for screening and brief intervention. BMC Public Health 2019, 19, 1594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McBride, C.M.; Emmons, K.M.; Lipkus, I.M. Understanding the potential of teachable moments: The case of smoking cessation. Health Educ. Res. 2003, 18, 156–170. [Google Scholar] [CrossRef] [PubMed]
- Longabaugh, R.; Minugh, P.A.; Nirenberg, T.D.; Clifford, P.R.; Becker, B.; Woolard, R. Injury as a motivator to reduce drinking. Acad. Emerg. Med. 1995, 2, 817–825. [Google Scholar] [CrossRef] [PubMed]
- Steca, P.; Monzani, D.; Greco, A.; Franzelli, C.; Magrin, M.E.; Miglioretti, M.; Sarini, M.; Scrignaro, M.; Vecchio, L.; Fattirolli, F.; et al. Stability and change of lifestyle profiles in cardiovascular patients after their first acute coronary event. PLoS ONE 2017, 12, e0183905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT Alcohol Consumption Questions (AUDIT-C). An Effective Brief Screening Test for Problem Drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins-Biddle, J.C.; Babor, T.F. A review of the Alcohol Use Disorders Identification Test (AUDIT), AUDIT-C, and USAUDIT for screening in the United States: Past issues and future directions. Am. J. Drug Alcohol Abus. 2018, 44, 578–586. [Google Scholar] [CrossRef]
- Reinert, D.F.; Allen, J.P. The Alcohol Use Disorders Identification Test: An Update of Research Findings. Alcohol. Clin. Exp. Res. 2007, 31, 185–199. [Google Scholar] [CrossRef]
- National Institute on Alcohol Abuse and Alcoholism. Drinking Levels Defined. 2012. Available online: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking (accessed on 4 January 2022).
- Seitz, H.K.; Bühringer, G.; Mann, K. Grenzwerte für den Konsum alkoholischer Getränke: Empfehlungen des wissenschaftlichen Kuratoriums der DHS. In Jahrbuch Sucht; Neuland: Geesthacht, Germany, 2008; pp. 205–209. [Google Scholar]
- Deutsche Hauptstelle fur Suchtfragen. Wie Sollten Menschen mit Alkohol Umgehen, um Gesundheitsrisiken zu Verringern? Stellungnahme der Deutschen Hauptstelle für Suchtfragen e.V. 2019. Available online: https://www.dhs.de/fileadmin/user_upload/pdf/dhs-stellungnahmen/DHS_Stellungnahme_Umgang_mit_Alkohol.pdf (accessed on 4 January 2022).
- Booth, M.L. Short Last 7 Days Self-Administered Version of the IPAQ. 2002. Available online: http://youthrex.com/wp-content/uploads/2017/06/IPAQ-TM.pdf (accessed on 4 January 2022).
- World Health Organization. Guidelines on Physical Activity and Sedentary Behaviour. 2020. Available online: https://apps.who.int/iris/rest/bitstreams/1315866/retrieve (accessed on 8 March 2022).
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macrea, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081–1093. [Google Scholar] [CrossRef] [Green Version]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation (WHO Technical Report Series 894; 1999). 1999. Available online: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed on 4 January 2022).
- Prochaska, J.O.; Velicer, W.F. The Transtheoretical Model of Health Behavior Change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef]
- Lippke, S.; Ziegelmann, J.P.; Schwarzer, R.; Velicer, W.F. Validity of stage assessment in the adoption and maintenance of physical activity and fruit and vegetable consumption. Health Psychol. 2009, 28, 183–193. [Google Scholar] [CrossRef] [Green Version]
- DiClemente, C.C.; Prochaska, J.O.; Fairhurst, S.K.; Velicer, W.F.; Velasquez, M.M.; Rossi, J.S. The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. J. Consult. Clin. Psychol. 1991, 59, 295–304. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-Item Mediterranean Diet Assessment Tool and Obesity Indexes among High-Risk Subjects: The PREDIMED Trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richter, A.; Schienkiewitz, A.; Starker, A.; Krug, A.; Domanska, O.; Kuhnert, R.; Loss, J.; Mensink, G.B.M. Health-promoting behaviour among adults in Germany—Results from GEDA 2019/2020-EHIS. J. Health Monit. 2021, 6, 26–44. [Google Scholar]
- Linardakis, M.; Smpokos, E.; Papadaki, A.; Komninos, I.D.; Tzanakis, N.; Philalithis, A. Prevalence of multiple behavioral risk factors for chronic diseases in adults aged 50+, from eleven European countries—The SHARE study (2004). Prev. Med. 2013, 57, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Chair, S.Y.; Lee, S.F.; Lopez, V.; Ling, E.M. Risk factors of Hong Kong Chinese patients with coronary heart disease. J. Clin. Nurs. 2007, 16, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Haynes, C.L. Health promotion services for lifestyle development within a UK hospital—Patients’ experiences and views. BMC Public Health 2008, 8, 284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doyle, B.; Fitzsimons, D.; McKeown, P.; McAloon, T. Understanding dietary decision-making in patients attending a secondary prevention clinic following myocardial infarction. J. Clin. Nurs. 2012, 21, 32–41. [Google Scholar] [CrossRef]
- Volkert, D.; Bollwein, J.; Diekmann, R.; Sieber, C. Die Rolle der Ernährung bei der Entstehung von Sarkopenie und Frailty. Ernähr. Umsch. 2011, 9, 486–493. [Google Scholar]
- Prochaska, J.J.; Spring, B.; Nigg, C.R. Multiple health behavior change research: An introduction and overview. Prev. Med. 2008, 46, 181–188. [Google Scholar] [CrossRef] [Green Version]
- Schneider, S.; Huy, C.; Schuessler, M.; Diehl, K.; Schwarz, S. Optimising lifestyle interventions: Identification of health behaviour patterns by cluster analysis in a German 50+ survey. Eur. J. Public Health 2009, 19, 271–277. [Google Scholar] [CrossRef] [Green Version]
- Stuck, A.E.; Moser, A.; Morf, U.; Wirz, U.; Wyser, J.; Gillmann, G.; Born, S.; Zwahlen, M.; Iliffe, S.; Harari, D.; et al. Effect of Health Risk Assessment and Counselling on Health Behaviour and Survival in Older People: A Pragmatic Randomised Trial. PLoS Med. 2015, 12, e1001889. [Google Scholar] [CrossRef] [Green Version]
- Lehtisalo, J.; Levälahti, E.; Lindström, J.; Hänninen, T.; Paajanen, T.; Peltonen, M.; Antikainen, R.; Laatikainen, T.; Strandberg, T.; Soininen, H.; et al. Dietary changes and cognition over 2 years within a multidomain intervention trial—The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Alzheimer’s Dement. 2019, 15, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levälahti, E.; Ahtiluoto, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Prince, S.A.; Adamo, K.B.; Hamel, M.E.; Hardt, J.; Gorber, S.C.; Tremblay, M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- John, U.; Hanke, M.; Grothues, J.; Thyrian, J.R. Validity of overweight and obesity in a nation based on self-report versus measurement device data. Eur. J. Clin. Nutr. 2006, 60, 372–377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newell, S.; Girgis, A.; Sanson-Fisher, R.; Savolainen, N.J. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: A critical review. Am. J. Prev. Med. 1999, 17, 211–229. [Google Scholar] [CrossRef]
| Total | Men | Women | |
|---|---|---|---|
| n (%) | 328 | 215 (65.5) | 113 (34.5) |
| Age in years | |||
| M (SD) | 66.5 (9.0) | 65.9 (9.2) | 67.7 (8.4) |
| Median (IQR) | 67.0 (59.0–75.0) | 66.0 (58.0–75.0) | 69.0 (61.0–75.0) |
| School education level * | |||
| Lower, n (%) | 214 (70.4) | 144 (72.0) | 70 (67.3) |
| Higher, n (%) | 90 (29.6) | 56 (28.0) | 34 (32.7) |
| Self-rated health | |||
| Better, n (%) | 203 (61.9) | 138 (64.2) | 65 (57.5) |
| Lower, n (%) | 125 (38.1) | 77 (35.8) | 48 (42.5) |
| Number of health risk factors ** | |||
| M (SD) | 1.6 (0.8) | 1.7 (0.9) | 1.5 (0.7) |
| Median (IQR) | 2.0 (1.0–2.0) | 2.0 (1.0–2.0) | 1.0 (1.0–2.0) |
| Overweight | Inactivity | Alcohol | Smoking | |||||
|---|---|---|---|---|---|---|---|---|
| n | n | n | n | |||||
| Total | 328 | 75.9 (71.0–80.3) | 309 | 49.5 (43.9–55.1) | 311 | 19.0 (15.0–23.7) | 311 | 16.1 (12.4–20.6) |
| Sex | ||||||||
| Men | 215 | 76.7 (70.6–81.9) | 202 | 48.0 (41.2–55.0) | 204 | 24.0 (18.6–30.4) | 204 | 18.6 (13.8–24.6) |
| Women | 113 | 74.3 (65.4–81.6) | 107 | 52.3 (42.8–61.8) | 107 | 9.3 (5.0–16.7) | 107 | 11.2 (6.4–18.9) |
| Age (years) | ||||||||
| 50–59 | 92 | 73.9 (63.8–82.0) | 85 | 43.5 (33.2–54.4) | 87 | 31.0 (22.1–41.7) | 87 | 29.9 (21.1–40.5) |
| 60–69 | 94 | 84.0 (75.0–90.2) | 91 | 52.7 (42.3–62.9) | 92 | 16.3 (10.0–25.5) | 92 | 19.6 (12.6–29.1) |
| 70–79 | 142 | 71.8 (63.8–78.7) | 133 | 51.1 (42.6–59.6) | 132 | 12.9 (8.1–19.8) | 132 | 4.5 (2.0–9.8) |
| School education level * | ||||||||
| Lower | 214 | 80.8 (75.0–85.6) | 209 | 54.5 (47.7–61.2) | 214 | 15.4 (11.1–20.9) | 214 | 19.2 (14.4–25.0) |
| Higher | 90 | 66.7 (56.1–75.8) | 89 | 37.1 (27.5–47.7) | 90 | 27.8 (19.4–38.1) | 90 | 10.0 (5.2–18.3) |
| Pattern of Health Risk Factor(s) | % | 95% CI |
|---|---|---|
| 0 health risk factors | 8.2 | 5.6–11.9 |
| Overweight | 25.9 | 21.3–31.1 |
| Inactivity | 8.5 | 5.9–12.3 |
| Alcohol | 1.0 | 0.3–3.0 |
| Smoking | 2.0 | 0.9–4.3 |
| 1 health risk factor | 37.4 | 32.1–43.0 |
| Overweight plus inactivity | 29.2 | 24.3–34.6 |
| Overweight plus alcohol | 7.5 | 5.1–11.1 |
| Overweight plus smoking | 2.6 | 1.3–5.2 |
| Inactivity plus alcohol | 1.0 | 0.3–3.0 |
| Inactivity plus smoking | 1.0 | 0.3–3.0 |
| Alcohol plus smoking | 1.0 | 0.3–3.0 |
| 2 health risk factors | 42.3 | 36.8–47.9 |
| Overweight plus inactivity plus alcohol | 3.6 | 2.0–6.4 |
| Overweight plus inactivity plus smoking | 4. | 2.7–7.6 |
| Overweight plus alcohol plus smoking | 2.3 | 1.1–4.8 |
| Inactivity plus alcohol plus smoking | 1.0 | 0.3–3.0 |
| 3 health risk factors | 11.5 | 8.3–15.6 |
| Overweight plus inactivity plus alcohol plus smoking | 0.7 | 0.2–2.6 |
| Behavioral Health Risk Factor(s) | ||||
|---|---|---|---|---|
| n | ≥1 | ≥2 | ≥3 | |
| Total | 305 | 91.8 (88.1–94.4) | 54.4 (48.8–60.0) | 12.1 (8.9–16.3) |
| Sex | ||||
| Men | 199 | 91.0 (86.1–94.2) | 58.3 (51.3–65.0) | 15.1 (10.7–20.8) |
| Women | 106 | 93.4 (86.6–96.9) | 47.2 (37.7–56.8) | 6.6 (3.1–13.4) |
| Age (years) | ||||
| 50–59 | 82 | 93.9 (85.9–97.5) | 57.3 (46.2–67.7) | 20.7 (13.2–31.1) |
| 60–69 | 91 | 91.2 (83.2–95.6) | 63.7 (53.2–73.1) | 15.4 (9.2–24.5) |
| 70–79 | 132 | 90.9 (84.6–94.8) | 46.2 (37.8–54.9) | 4.5 (2.0–9.8) |
| School education level | ||||
| Lower | 209 | 95.7 (91.9–97.8) | 58.4 (51.5–64.9) | 12.0 (8.2–17.2) |
| Higher | 89 | 83.1 (73.7–89.7) | 44.9 (34.8–55.6) | 13.5 (7.7–22.5) |
| Health Risk | Recommended Behavior | Stage of Change | ||||
|---|---|---|---|---|---|---|
| Factor Present | n | Pre-Contemplation | Contemplation | Preparation | Action | |
| Overweight | 244 | Healthy diet | 18.4 (14.0–23.9) | 54.5 (48.2–60.7) | 4.5 (2.5–8.0) | 22.5 (17.7–28.3) |
| Inactivity | 152 | Sufficient physical activity | 15.1 (10.2–21.8) | 46.7 (38.8–54.7) | 17.1 (11.9–24.0) | 21.1 (15.2–28.3) |
| Alcohol | 59 | No or low-risk consumption | 6.8 (2.5–17.1) | 37.3 (25.7–50.6) | 6.8 (2.5–17.1) | 49.2 (36.4–62.1) |
| Smoking | 50 | Smoking cessation | 34.0 (21.9–48.6) | 40.0 (27.1–54.5) | 26.0 (15.4–40.3) | / |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siewert-Markus, U.; Ulbricht, S.; Gaertner, B.; Zyriax, B.-C.; Dörr, M.; Tobschall, S.; Baumann, S.; John, U.; Freyer-Adam, J. Behavioral Health Risk Factors and Motivation to Change among Cardiovascular General Hospital Patients Aged 50 to 79 Years. Nutrients 2022, 14, 1963. https://doi.org/10.3390/nu14091963
Siewert-Markus U, Ulbricht S, Gaertner B, Zyriax B-C, Dörr M, Tobschall S, Baumann S, John U, Freyer-Adam J. Behavioral Health Risk Factors and Motivation to Change among Cardiovascular General Hospital Patients Aged 50 to 79 Years. Nutrients. 2022; 14(9):1963. https://doi.org/10.3390/nu14091963
Chicago/Turabian StyleSiewert-Markus, Ulrike, Sabina Ulbricht, Beate Gaertner, Birgit-Christiane Zyriax, Marcus Dörr, Stefanie Tobschall, Sophie Baumann, Ulrich John, and Jennis Freyer-Adam. 2022. "Behavioral Health Risk Factors and Motivation to Change among Cardiovascular General Hospital Patients Aged 50 to 79 Years" Nutrients 14, no. 9: 1963. https://doi.org/10.3390/nu14091963
APA StyleSiewert-Markus, U., Ulbricht, S., Gaertner, B., Zyriax, B.-C., Dörr, M., Tobschall, S., Baumann, S., John, U., & Freyer-Adam, J. (2022). Behavioral Health Risk Factors and Motivation to Change among Cardiovascular General Hospital Patients Aged 50 to 79 Years. Nutrients, 14(9), 1963. https://doi.org/10.3390/nu14091963






