Impedance Analysis to Evaluate Nutritional Status in Physiological and Pathological Conditions
Abstract
:1. Introduction
- Primary care medicine: monitoring of the subject’s nutritional status, especially in conditions of obesity or overweight; detection of pathologies related to fluid variation in the body; evaluation of hydro-electrolyte changes aimed at early diagnosis of heart failure; dosage of diuretics [10].
- Sports medicine: checking body hydration and monitoring changes in FFM and fat mass (FM); detecting changes as a result of intense training or inadequate diet [11].
- Obstetrics and gynecology: monitoring weight changes and water retention in pregnancy and menopause [12].
- Geriatrics: monitoring changes in weight and dehydration with aging, with an assessment of dietary and hydration needs.
- Dietetics: monitoring changes in body compartments during specific dietary programs with an assessment of hydration status and cell mass.
- Artificial nutrition: assessment of the individual’s initial nutritional status for setting the most appropriate nutritional program, also for the intensive care and resuscitation room.
- Nephrology and dialysis: identifying the patient’s ideal dry weight to tailor the hemodialysis session; monitoring body fluids to investigate the need for dialysis; and assessing pre- and post-dialysis water status [13].
- Oncology and HIV: identification of patients with reduced cell mass or altered water balance from therapies; phase angle as a prognostic index of survival [14].
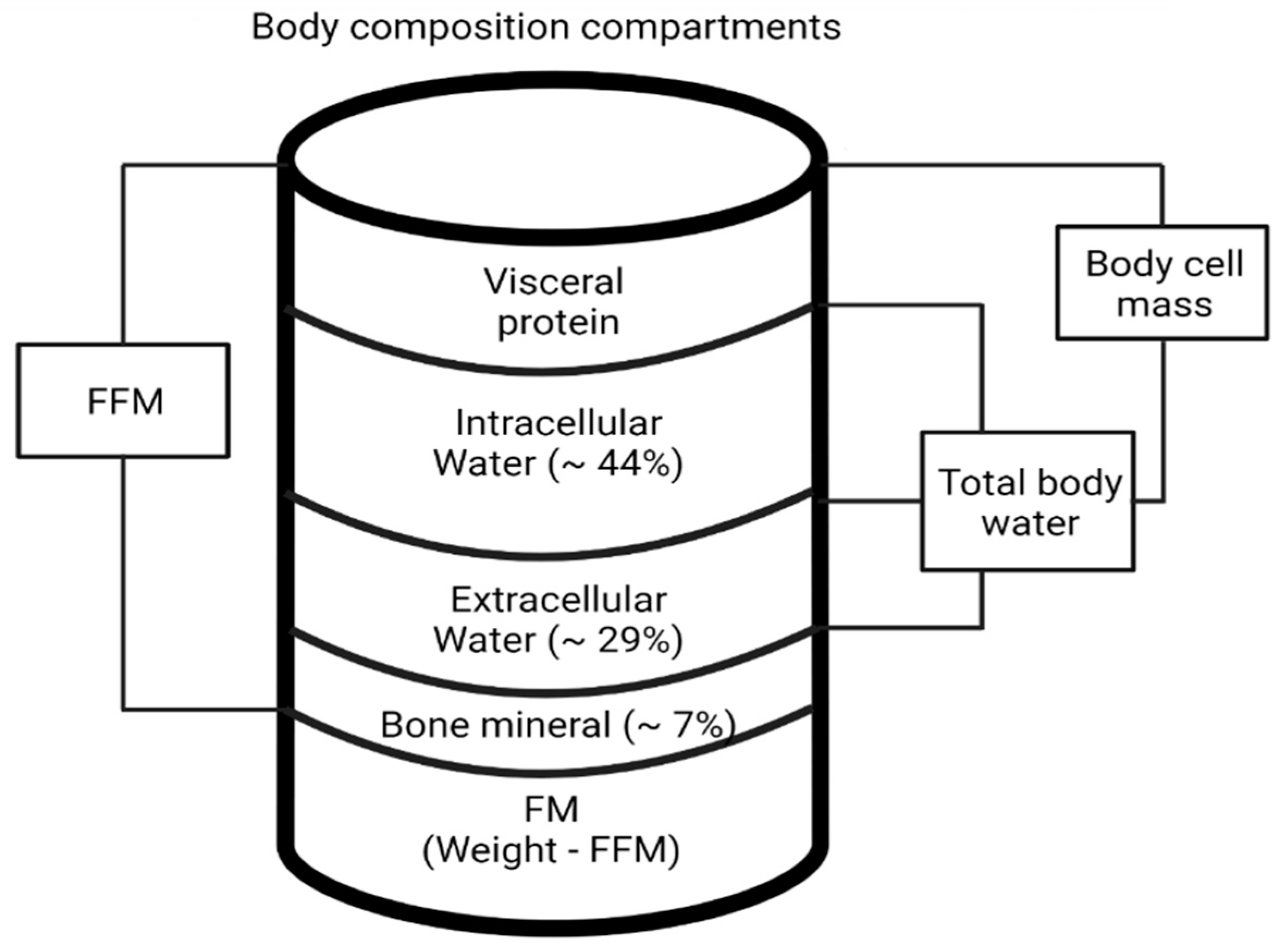
2. Body Composition
- TBW: its measurement is obtained from the ratio of stature (H) squared to R (impedance index, H2/Z or resistance index H2/R) to which other variables are added to increase the accuracy of the regression (multiple).
- ECW and ICW
- FFM
- FM
- BCM
- Muscle mass (MM)
3. BIA Application under Physiological Conditions
3.1. Sports and Muscle
- Programming proper training for a better choice of workloads and recovery times
- Nutrition programming
- Checking hydration status
- Intra- and extracellular fluid monitoring
- Evaluation of Phase angle as an index of general physical state
- Assessment of BCM to verify improvements and to avoid super-training states
- Assessment of basal metabolic rate and energy expenditure.
3.2. Pregnancy and Menopause
3.3. Aging
- Subjective Global Assessment (SGA)
- Sadness, Cholesterol, Albumin, Loss of weight, Eating problems, Shopping problems, or Inability to prepare a meal (SCALES)
- Geriatric Nutritional Risk Index (GNRI)
- Nutrition Risk Score (NRS)
- Nutrition Screening Initiative (NSI)
- Nutritional Risk Assessment Scale (NuRAS)
- Mini Nutritional Assessment (MNA)
4. BIA Application in Pathological Conditions
4.1. Overweight and Obesity
4.2. Eating Disorders: Anorexia
- Significant weight reduction
- Inability to gain body weight
- State of fasting or semi-fasting
- Associated elimination conducts (e.g., vomiting).
4.3. Type 1 and 2 Diabetes
4.4. Inflammation
4.5. Cancer
4.6. Diuretic Therapy
4.7. Bariatric Surgery
4.8. Therapeutic Fasting
5. Conclusions
- to date represents the quintessential technique for evaluation in pregnancy as it allows monitoring of hemodynamic adaptation and identification of patients at risk for the onset of hypertensive pathology [41];
- confirms its validity in menopause, in relation to the strong changes in the hydro electrolyte picture both for evaluation of fat tissue redistribution and for predisposition of hormone replacement therapy [48];
- Phase angle is a valid predictor of CRP levels, a biomarker of meta-inflammation. Thus, bioelectrical impedance parameters are extremely useful in the detection of inflammatory indices [69];
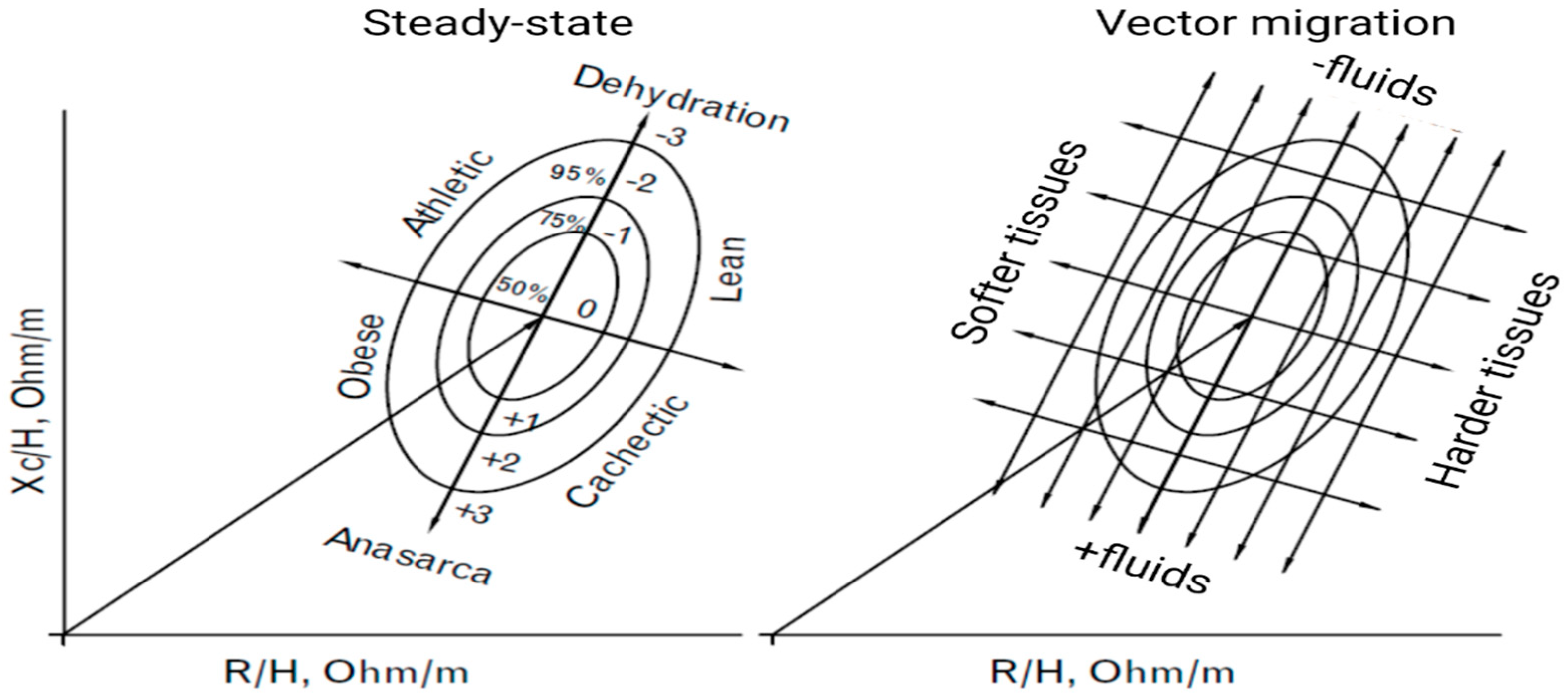
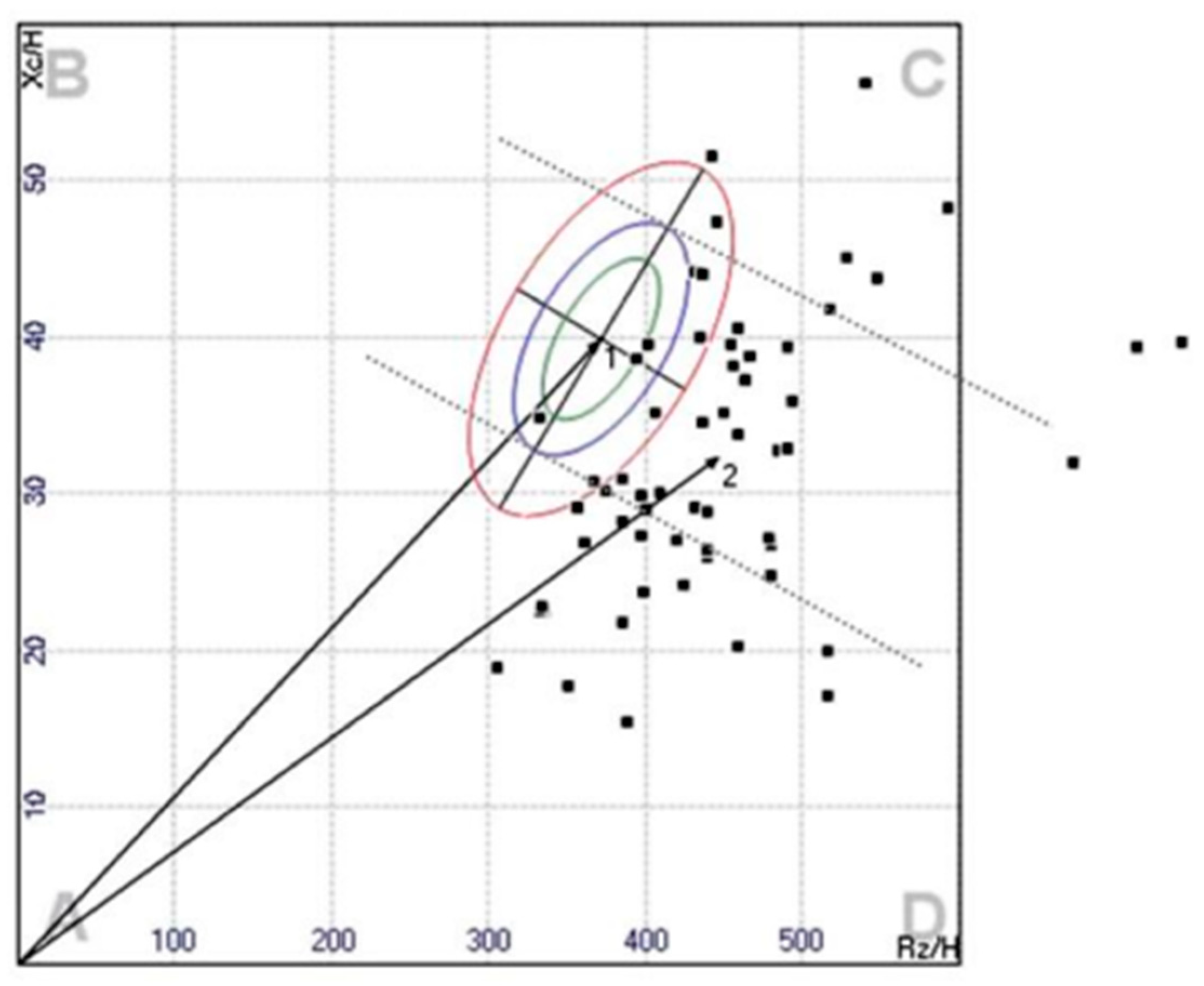
- BIVA is useful in diseases requiring diuretic therapy, for the detection of fluid overload and the identification, monitoring, and therapy planning of renal patients with impaired fluid balance. However, the greater potential of the method has been found in those patients in whom basal impedance vectors had already been measured under healthy conditions [26,75];
- In patients with average and mild obesity, BIVA was proved to be a valid method of analysis, both prognostic and therapeutic. Nonetheless, significant limitations of BIVA method in morbid obesity type III have been detected as the underestimation of body fat percentage and overestimation of FFMv [58,59,60,79]; in extreme interventions for the treatment of obesity, such as bariatric surgery, BIVA was shown to be useful in highlighting a loss of FM, as well as of FFM [78]; on the other hand, following therapeutic fasting, the aforementioned limitations were confirmed in the evaluation of subjects with severe obesity [79];
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Talluri, T. Sulle Metodiche Impedenziometriche; Akern R&D-Firenze: Firenze, Italy, 2013. [Google Scholar]
- Hermann, L. Ueber eine Wirkung galvanischer Ströme auf Muskeln und Nerven. Pflüger Arch. 1872, 5, 223–275. [Google Scholar] [CrossRef]
- Thomasset, M. Bioelectric Properties of Tissue. Impedance Measurement in Clinical Medicine. Significance of Curves Obtained. Lyon. Med. 1962, 94, 107–118. [Google Scholar] [PubMed]
- Ducrot, H.; Thomasset, A.; Joly, R.; Jungers, P.; Eyraud, C.; Lenoir, J. Determination of Extracellular Fluid Volume in Humans by Measurement of Total Body Impedance. Presse Med. 1970, 78, 2269–2272. [Google Scholar]
- Nyboer, J.; Kreider, M.M.; Hannapel, L. Electrical Impedance Plethysmography: A Physical and Physiologic Approach to Peripheral Vascular Study. Circulation 1950, 2, 811–821. [Google Scholar] [CrossRef] [PubMed]
- Hoffer, E.C.; Meador, C.K.; Simpson, D.C. Correlation of Whole-Body Impedance with Total Body Water Volume. J. Appl. Physiol. 1969, 27, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Andreoli, A.; Melchiorri, G.; De Lorenzo, A.; Caruso, I.; Sinibaldi Salimei, P.; Guerrisi, M. Bioelectrical Impedance Measures in Different Position and vs Dual-Energy X-Ray Absorptiometry (DXA). J. Sport. Med. Phys. Fit. 2002, 42, 186–189. [Google Scholar]
- Mills, W.J.; Rau, D. University of Alaska, Anchorage-Section of High Latitude Study, and the Mt. Mckinley Project (1981-82-83). Alsk. Med. 1983, 25, 21–28. [Google Scholar]
- Lukaski, H.; Johnson, P.; Bolonchuk, W.; Lykken, G. Assessment of Fat-Free Mass Using Bioelectrical Impedance Measurements of the Human Body. Am. J. Clin. Nut. R 1985, 41, 810–817. [Google Scholar] [CrossRef]
- Yu, C.-M.; Wang, L.; Chau, E.; Chan, R.H.-W.; Kong, S.-L.; Tang, M.-O.; Christensen, J.; Stadler, R.W.; Lau, C.-P. Intrathoracic Impedance Monitoring in Patients with Heart Failure. Circulation 2005, 112, 841–848. [Google Scholar] [CrossRef]
- Castizo-Olier, J.; Irurtia, A.; Jemni, M.; Carrasco-Marginet, M.; Fernández-García, R.; Rodríguez, F.A. Bioelectrical Impedance Vector Analysis (BIVA) in Sport and Exercise: Systematic Review and Future Perspectives. PLoS ONE 2018, 13, e0197957. [Google Scholar] [CrossRef]
- Moroni, A.; Vardè, C.; Giustetto, A.; Stagi, S.; Marini, E.; Micheletti Cremasco, M. Bioelectrical Impedance Vector Analysis (BIVA) for the Monitoring of Body Composition in Pregnancy. Eur. J. Clin. Nutr. 2022, 76, 604–609. [Google Scholar] [CrossRef]
- Piccoli, A. Utilità, Potenzialità e Uso Improprio Dell’analisi Di Bioimpedenza in Emodialisi. Giornale Ital. Di Nefrol. 2000, 1, 82–93. [Google Scholar]
- Earthman, C.P.; Matthie, J.R.; Reid, P.M.; Harper, I.T.; Ravussin, E.; Howell, W.H. A Comparison of Bioimpedance Methods for Detection of Body Cell Mass Change in HIV Infection. J. Appl. Physiol. 2000, 88, 944–956. [Google Scholar] [CrossRef] [PubMed]
- Benzing, G. Electrical Impedance Plethysmography, The Electrical Resistive Measure of the Blood Pulse Volume, Peripheral and Central Blood Flow, Ed 2. Arch. Pediatr. Adolesc. Med. 1970, 120, 585. [Google Scholar] [CrossRef]
- Foster, K.; Lukaski, H. Whole-Body Impedance—What Does It Measure? Am. J. Clin. Nutr. 1996, 64, 388S–396S. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.; Wang, Z.; Visser, M.; Gallagher, D.; Pierson, R. Techniques Used in the Measurement of Body Composition: An Overview with Emphasis on Bioelectrical Impedance Analysis. Am. J. Clin. Nutr. 1996, 64, 478S–484S. [Google Scholar] [CrossRef] [PubMed]
- Kushner, R.F. Bioelectrical Impedance Analysis: A Review of Principles and Applications. J. Am. Coll. Nutr. 1992, 11, 199–209. [Google Scholar] [CrossRef]
- Lukaski, H. Biological Indexes Considered in the Derivation of the Bioelectrical Impedance Analysis. Am. J. Clin. Nutr. 1996, 64, 397S–404S. [Google Scholar] [CrossRef]
- O’Brien, C.; Young, A.J.; Sawka, M.N. Bioelectrical Impedance to Estimate Changes in Hydration Status. Int. J. Sport. Med. 2002, 23, 361–366. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical Impedance Analysis—Part I: Review of Principles and Methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Manuel Gómez, J.; Lilienthal Heitmann, B.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M.; et al. Bioelectrical Impedance Analysis—Part II: Utilization in Clinical Practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef] [PubMed]
- Lukaski, H.C. Evolution of Bioimpedance: A Circuitous Journey from Estimation of Physiological Function to Assessment of Body Composition and a Return to Clinical Research. Eur. J. Clin. Nutr. 2013, 67 (Suppl. 1), S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Piccoli, A. Patterns of Bioelectrical Impedance Vector Analysis: Learning from Electrocardiography and Forgetting Electric Circuit Models. Nutrition 2002, 18, 520–521. [Google Scholar] [CrossRef] [PubMed]
- Piccoli, A. Analisi di Bioimpedenza per la Clinica; Pinelli: Milano, Italy, 2003; Volume 1, pp. 13–17. [Google Scholar]
- Piccoli, A.; Rossi, B.; Pillon, L.; Bucciante, G. A New Method for Monitoring Body Fluid Variation by Bioimpedance Analysis: The RXc Graph. Kidney Int. 1994, 46, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Scheltinga, M.R.; Jacobs, D.O.; Kimbrough, T.D.; Wilmore, D.W. Alterations in Body Fluid Content Can Be Detected by Bioelectrical Impedance Analysis. J. Surg. Res. 1991, 50, 461–468. [Google Scholar] [CrossRef]
- Mulasi, U.; Kuchnia, A.J.; Cole, A.J.; Earthman, C.P. Bioimpedance at the Bedside. Nutr. Clin. Pract. 2015, 30, 180–193. [Google Scholar] [CrossRef]
- Ward, L.C. Bioelectrical Impedance Analysis for Body Composition Assessment: Reflections on Accuracy, Clinical Utility, and Standardisation. Eur. J. Clin. Nutr. 2019, 73, 194–199. [Google Scholar] [CrossRef]
- Scharfetter, H.; Schlager, T.; Stollberger, R.; Felsberger, R.; Hutten, H.; Hinghofer-Szalkay, H. Assessing Abdominal Fatness with Local Bioimpedance Analysis: Basics and Experimental Findings. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 502–511. [Google Scholar] [CrossRef]
- Barbosa-Silva, M.C.G.; Barros, A.J. Bioelectrical Impedance Analysis in Clinical Practice: A New Perspective on Its Use beyond Body Composition Equations. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 311–317. [Google Scholar] [CrossRef]
- Piccoli, A.; Nescolarde, L.D.; Rosell, J. Conventional and Vectorial Analysis of Bioimpedance in Clinical Practice. Nefrologia 2002, 22, 228–238. [Google Scholar]
- Khalil, S.; Mohktar, M.; Ibrahim, F. The Theory and Fundamentals of Bioimpedance Analysis in Clinical Status Monitoring and Diagnosis of Diseases. Sensors 2014, 14, 10895–10928. [Google Scholar] [CrossRef] [PubMed]
- Rutkove, S.B.; Aaron, R.; Shiffman, C.A. Localized Bioimpedance Analysis in the Evaluation of Neuromuscular Disease. Muscle Nerve 2002, 25, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Campa, F.; Toselli, S. Bioimpedance Vector Analysis of Elite, Subelite, and Low-Level Male Volleyball Players. Int. J. Sport. Physiol. Perform. 2018, 13, 1250–1253. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Pirlich, M.; Sorensen, J.; Christensen, P.; Kemps, M.; Schütz, T.; Lochs, H.; Kondrup, J. Bioimpedance Vector Analysis as a Measure of Muscle Function. Clin. Nutr. 2009, 28, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Toselli, S.; Marini, E.; Maietta Latessa, P.; Benedetti, L.; Campa, F. Maturity Related Differences in Body Composition Assessed by Classic and Specific Bioimpedance Vector Analysis among Male Elite Youth Soccer Players. Int. J. Env. Res. Public Health 2020, 17, 729. [Google Scholar] [CrossRef]
- Moon, J.R. Body Composition in Athletes and Sports Nutrition: An Examination of the Bioimpedance Analysis Technique. Eur. J. Clin. Nutr. 2013, 67 (Suppl. 1), S54–S59. [Google Scholar] [CrossRef]
- Lukaski, H.C.; Siders, W.A.; Nielsen, E.J.; Hall, C.B. Total Body Water in Pregnancy: Assessment by Using Bioelectrical Impedance. Am. J. Clin. Nutr. 1994, 59, 578–585. [Google Scholar] [CrossRef]
- Pirani, B.B.; Campbell, D.M.; MacGillivray, I. Plasma Volume in Normal First Pregnancy. J. Obs. Gynaecol. Br. Commonw. 1973, 80, 884–887. [Google Scholar] [CrossRef]
- Paradisi, G.; Biaggi, A.; Savone, R.; Ianniello, F.; Tomei, C.; Caforio, L.; Caruso, A. Cardiovascular Risk Factors in Healthy Women with Previous Gestational Hypertension. J. Clin. Endocrinol. Metab. 2006, 91, 1233–1238. [Google Scholar] [CrossRef]
- Andreoli, A.; Lello, S. Composizione Corporea, Menopausa Ed Invecchiamento. Gin Endo Bullettin, Raccolta Monografie, ISGE Italy. 2007, pp. 19–31. Available online: https://bollettinoginendo.it/wp-content/uploads/2014/06/andreoli_lello_19_31.pdf (accessed on 7 May 2023).
- Heymsfield, S.B.; Gallagher, D.; Poehlman, E.T.; Wolper, C.; Nonas, K.; Nelson, D.; Wang, Z.M. Menopausal Changes in Body Composition and Energy Expenditure. Exp. Gerontol. 1994, 29, 377–389. [Google Scholar] [CrossRef]
- Poehlman, E.T.; Toth, M.J.; Gardner, A.W. Changes in Energy Balance and Body Composition at Menopause: A Controlled Longitudinal Study. Ann. Intern. Med. 1995, 123, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Tchernof, A.; Poehlman, E.T. Effects of the Menopause Transition on Body Fatness and Body Fat Distribution. Obes. Res. 1998, 6, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Matthews, K.A.; Kuller, L.H.; Meilahn, E.N.; Plantinga, P.L. Weight Gain at the Time of Menopause. Arch. Intern. Med. 1991, 151, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Folsom, A.R.; Kaye, S.A.; Sellers, T.A.; Hong, C.P.; Cerhan, J.R.; Potter, J.D.; Prineas, R.J. Body Fat Distribution and 5-Year Risk of Death in Older Women. JAMA 1993, 269, 483–487. [Google Scholar] [CrossRef]
- Meeuwsen, I.B.; Samson, M.M.; Duursma, S.A.; Verhaar, H.J. The Effect of Tibolone on Fat Mass, Fat-Free Mass, and Total Body Water in Postmenopausal Women. Endocrinology 2001, 142, 4813–4817. [Google Scholar] [CrossRef]
- Bissoli, L.; Zamboni, M.; Sergi, G.; Ferrari, E.; Bosello, O. Linee Guida per La Valutazione Della Malnutrizione Nell’anziano. Giorn. Geront 2001, 49, 4–12. [Google Scholar]
- Buffa, R.; Marini, E.; Mereu, R.M.; Putzu, P.F.; Floris, G. La Malnutrizione Proteico-Energetica Nell’anziano: Tecniche Di Analisi e Applicazioni. Antropo 2007, 14, 19–27. [Google Scholar]
- Lu, H.-K.; Lai, C.-L.; Lee, L.-W.; Chu, L.-P.; Hsieh, K.-C. Assessment of Total and Regional Bone Mineral Density Using Bioelectrical Impedance Vector Analysis in Elderly Population. Sci. Rep. 2021, 11, 21161. [Google Scholar] [CrossRef]
- Antunes, M.; Cyrino, E.S.; Silva, D.R.P.; Tomeleri, C.M.; Nabuco, H.C.G.; Cavalcante, E.F.; Cunha, P.M.; Cyrino, L.T.; dos Santos, L.; Silva, A.M.; et al. Total and Regional Bone Mineral Density are Associated with Cellular Health in Older Men and Women. Arch. Gerontol. Geriatr. 2020, 90, 104156. [Google Scholar] [CrossRef]
- Öztürk, N.; Ozturk-Isik, E.; Ülgen, Y. Screening Post-Menopausal Women for Bone Mineral Level by Bioelectrical Impedance Spectroscopy of Dominant Arm. J. Electr. Bioimpedance 2018, 9, 39–47. [Google Scholar] [CrossRef]
- Ngai, H.H.Y.; Cheung, C.-L.; Yao, T.-J.; Kung, A.W.C. Bioimpedance: Can Its Addition to Simple Clinical Criteria Enhance the Diagnosis of Osteoporosis? J. Bone Min. Metab. 2009, 27, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Branca, F.; Nikogosian, H.; Lobstein, T. The Challenge of Obesity in the WHO European Region and the Strategies for Response: Summary; World Health Organization: Geneva, Switzerland, 2007; ISBN 9289013885. [Google Scholar]
- Zhou, Y.; Chi, J.; Lv, W.; Wang, Y. Obesity and Diabetes as High-risk Factors for Severe Coronavirus Disease 2019 (COVID-19). Diabetes Metab. Res. Rev. 2021, 37, e3377. [Google Scholar] [CrossRef] [PubMed]
- Gray, D.S.; Bray, G.A.; Gemayel, N.; Kaplan, K. Effect of Obesity on Bioelectrical Impedance. Am. J. Clin. Nutr. 1989, 50, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Piccoli, A.; Brunani, A.; Savia, G.; Pillon, L.; Favaro, E.; Berselli, M.E.; Cavagnini, F. Discriminating between Body Fat and Fluid Changes in the Obese Adult Using Bioimpedance Vector Analysis. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 97–104. [Google Scholar] [CrossRef]
- Coppini, L.Z.; Waitzberg, D.L.; Campos, A.C. Limitations and Validation of Bioelectrical Impedance Analysis in Morbidly Obese Patients. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 329–332. [Google Scholar] [CrossRef]
- Marra, M.; De Filippo, E.; Signorini, A.; Silvestri, E.; Pasanisi, F.; Contaldo, F.; Scalfi, L. Phase Angle Is a Predictor of Basal Metabolic Rate in Female Patients with Anorexia Nervosa. Physiol. Meas. 2005, 26, S145–S152. [Google Scholar] [CrossRef]
- Marucci, S.; Ragione, L.D.; De Iaco, G.; Mococci, T.; Vicini, M.; Guastamacchia, E.; Triggiani, V. Anorexia Nervosa and Comorbid Psychopathology. Endocr. Metab. Immune Disord. Drug Targets 2018, 18, 316–324. [Google Scholar] [CrossRef]
- Haas, V.; Riedl, A.; Hofmann, T.; Nischan, A.; Burghardt, R.; Boschmann, M.; Klapp, B. Bioimpedance and Bioimpedance Vector Analysis in Patients with Anorexia Nervosa. Eur. Eat. Disord. Rev. 2012, 20, 400–405. [Google Scholar] [CrossRef]
- Marra, M.; Caldara, A.; Montagnese, C.; De Filippo, E.; Pasanisi, F.; Contaldo, F.; Scalfi, L. Bioelectrical Impedance Phase Angle in Constitutionally Lean Females, Ballet Dancers and Patients with Anorexia Nervosa. Eur. J. Clin. Nutr. 2009, 63, 905–908. [Google Scholar] [CrossRef]
- Nakamura, F.; Kishimoto, Y.; Handa, T.; Arai, Y.; Mitani, K. Myelodysplastic Syndrome with Central Diabetes Insipidus Manifesting Hypodipsic Hypernatremia and Dehydration. Am. J. Hematol. 2004, 75, 213–216. [Google Scholar] [CrossRef]
- Di Mauro, M.; Lazzarini, D.; Fumelli, P.; Carle, F.; Kosmidis, A. Bioelectrical Impedance Analysis and Diabetes Mellitus: Which Correlation among Fructosamine, Glycosylated Haemoglobin and Exchangeable Potassium. Minerva Med. 2007, 98, 633–638. [Google Scholar] [PubMed]
- Dittmar, M.; Reber, H.; Kahaly, G.J. Bioimpedance Phase Angle Indicates Catabolism in Type 2 Diabetes. Diabet. Med. 2015, 32, 1177–1185. [Google Scholar] [CrossRef] [PubMed]
- Tajiri, Y.; Kato, T.; Nakayama, H.; Yamada, K. Reduction of Skeletal Muscle, Especially in Lower Limbs, in Japanese Type 2 Diabetic Patients with Insulin Resistance and Cardiovascular Risk Factors. Metab. Syndr. Relat. Disord. 2010, 8, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Holten, M.K.; Zacho, M.; Gaster, M.; Juel, C.; Wojtaszewski, J.F.; Dela, F. Strength Training Increases Insulin-Mediated Glucose Uptake, GLUT4 Content, and Insulin Signaling in Skeletal Muscle in Patients with Type 2 Diabetes. Diabetes 2004, 53, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Wiig, H.; Swartz, M.A. Interstitial Fluid and Lymph Formation and Transport: Physiological Regulation and Roles in Inflammation and Cancer. Physiol. Rev. 2012, 92, 1005–1060. [Google Scholar] [CrossRef]
- Badrooj, N.; Keshavarz, S.A.; Yekaninejad, M.S.; Mirzaei, K. Association between Dietary Inflammatory Index with Bioelectrical Impedance Parameters and Characteristics Health in Overweight/Obese Women: A Cross-Sectional Study. Int. J. Prev. Med. 2021, 12, 79. [Google Scholar] [CrossRef]
- Barrea, L.; Muscogiuri, G.; Pugliese, G.; Laudisio, D.; de Alteriis, G.; Graziadio, C.; Colao, A.; Savastano, S. Phase Angle as an Easy Diagnostic Tool of Meta-Inflammation for the Nutritionist. Nutrients 2021, 13, 1446. [Google Scholar] [CrossRef]
- Nwosu, A.C.; Mayland, C.R.; Mason, S.; Cox, T.F.; Varro, A.; Stanley, S.; Ellershaw, J. Bioelectrical Impedance Vector Analysis (BIVA) as a Method to Compare Body Composition Differences According to Cancer Stage and Type. Clin. Nutr. ESPEN 2019, 30, 59–66. [Google Scholar] [CrossRef]
- Toso, S.; Piccoli, A.; Gusella, M.; Menon, D.; Crepaldi, G.; Bononi, A.; Ferrazzi, E. Bioimpedance Vector Pattern in Cancer Patients without Disease versus Locally Advanced or Disseminated Disease. Nutrition 2003, 19, 510–514. [Google Scholar] [CrossRef]
- Gupta, D.; Lammersfeld, C.A.; Burrows, J.L.; Dahlk, S.L.; Vashi, P.G.; Grutsch, J.F.; Hoffman, S.; Lis, C.G. Bioelectrical Impedance Phase Angle in Clinical Practice: Implications for Prognosis in Advanced Colorectal Cancer. Am. J. Clin. Nutr. 2004, 80, 1634–1638. [Google Scholar] [CrossRef]
- Stäuber, A.; Heydenreich, M.; Wright, P.R.; Großmann, S.; Grusdat, N.; Zermann, D.H.; Schulz, H. Bioelectrical Impedance Vector Pattern and Biomarkers of Physical Functioning of Prostate Cancer Survivors in Rehabilitation. Rehabil. Process. Outcome 2021, 10, 11795727211064156. [Google Scholar] [CrossRef] [PubMed]
- Massari, F.; Iacoviello, M.; Scicchitano, P.; Mastropasqua, F.; Guida, P.; Riccioni, G.; Speziale, G.; Caldarola, P.; Ciccone, M.M.; Di Somma, S. Accuracy of Bioimpedance Vector Analysis and Brain Natriuretic Peptide in Detection of Peripheral Edema in Acute and Chronic Heart Failure. Heart Lung 2016, 45, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, R.; Weir, M.R. Dry-Weight: A Concept Revisited in an Effort to Avoid Medication-Directed Approaches for Blood Pressure Control in Hemodialysis Patients. Clin. J. Am. Soc. Nephrol. 2010, 5, 1255–1260. [Google Scholar] [CrossRef] [PubMed]
- De Freitas Junior, W.R.; Ilias, E.J.; Kassab, P.; Cordts, R.; Porto, P.G.; Martins Rodrigues, F.C.; Ali Taha, M.I.; Carrara, P.; De Carvalho Aguiar, I.; De Oliveira, L.V.; et al. Assessment of the Body Composition and the Loss of Fat-Free Mass through Bioelectric Impedance Analysis in Patients Who Underwent Open Gastric Bypass. Sci. World J. 2014, 2014, 843253. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, C.F.; Camelo, J.S., Jr.; Dos Santos, J.E.; Marchini, J.S.; Salgado, W., Jr.; Nonino, C.B. Bioelectrical Impedance Vector Analysis in Obese Women before and after Bariatric Surgery: Changes in Body Composition. Nutrition 2014, 30, 569–574. [Google Scholar] [CrossRef]
- Gray, D.S. Changes in Bioelectrical Impedance during Fasting. Am. J. Clin. Nutr. 1988, 48, 1184–1187. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catapano, A.; Trinchese, G.; Cimmino, F.; Petrella, L.; D’Angelo, M.; Di Maio, G.; Crispino, M.; Cavaliere, G.; Monda, M.; Mollica, M.P. Impedance Analysis to Evaluate Nutritional Status in Physiological and Pathological Conditions. Nutrients 2023, 15, 2264. https://doi.org/10.3390/nu15102264
Catapano A, Trinchese G, Cimmino F, Petrella L, D’Angelo M, Di Maio G, Crispino M, Cavaliere G, Monda M, Mollica MP. Impedance Analysis to Evaluate Nutritional Status in Physiological and Pathological Conditions. Nutrients. 2023; 15(10):2264. https://doi.org/10.3390/nu15102264
Chicago/Turabian StyleCatapano, Angela, Giovanna Trinchese, Fabiano Cimmino, Lidia Petrella, Margherita D’Angelo, Girolamo Di Maio, Marianna Crispino, Gina Cavaliere, Marcellino Monda, and Maria Pina Mollica. 2023. "Impedance Analysis to Evaluate Nutritional Status in Physiological and Pathological Conditions" Nutrients 15, no. 10: 2264. https://doi.org/10.3390/nu15102264
APA StyleCatapano, A., Trinchese, G., Cimmino, F., Petrella, L., D’Angelo, M., Di Maio, G., Crispino, M., Cavaliere, G., Monda, M., & Mollica, M. P. (2023). Impedance Analysis to Evaluate Nutritional Status in Physiological and Pathological Conditions. Nutrients, 15(10), 2264. https://doi.org/10.3390/nu15102264











