From Listing to Recovery: A Review of Nutritional Status Assessment and Management in Liver Transplant Patients
Abstract
1. Introduction
2. Data Sources and Searches
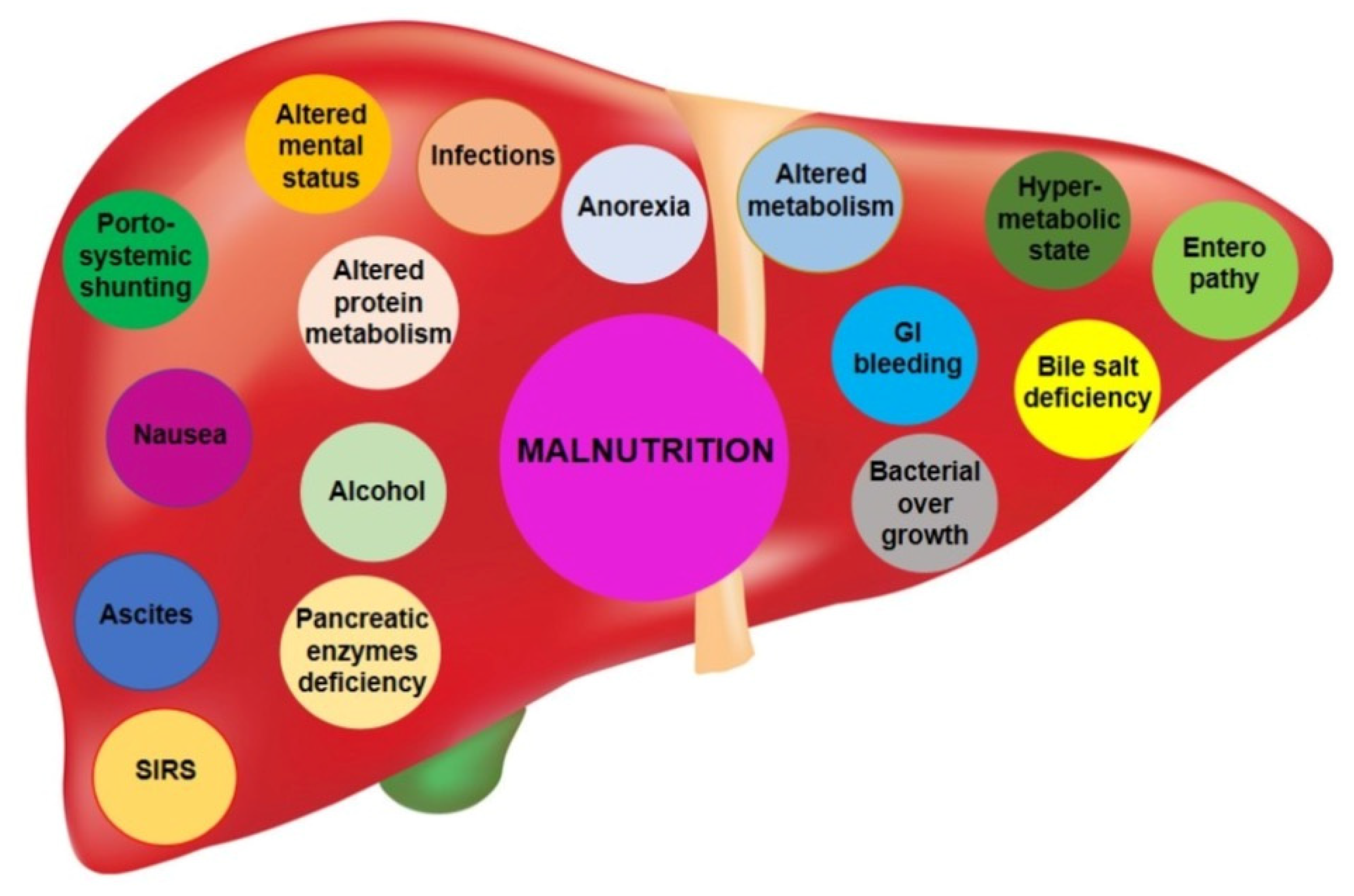
3. Malnutrition and Sarcopenia in Cirrhotic Patients
4. Nutritional Screening and Assessment in Cirrhosis
4.1. Nutritional Screening Tools
- The Mini Nutritional Assessment Short Form (MNA-SF) is a concise version of the MNA that comprises only six crucial components, with the highest level of sensitivity and specificity in comparison to the full version of the MNA and the standard nutritional assessment;
- The Malnutrition Universal Screening Test (MUST) classifies patients into malnutrition risk grades based on BMI and history of involuntary weight loss, which can also be secondary to acute illness;
- The Simplified Nutritional Appetite Questionnaire (SNAQ) is a succinct assessment comprising three inquiries pertaining to weight loss (exceeding 6 kg in the past six months or 3 kg in the past month), decreased appetite, and the necessity for nutritional supplementation within the last month;
- The Nutritional Risk Screening 2002 tool (identified by plate number 1) assesses the nutritional status and disease severity of patients over 70 years old. It has been extensively studied and validated in randomized controlled trials, proving its reliability.
- The Malnutrition Screening Tool (MST) is a quick and easy screening tool that includes questions about appetite, nutritional intake, and recent weight loss;
- The Nutrition Risk in the Critically Ill (NUTRIC Score) includes the absence of food intake, whether acute or chronic, inflammation, nutritional status, and outcomes;
- The Nutritional Risk Index (NRI) is a highly effective screening tool that was initially introduced by Buzby et al. [48] to examine the correlation between malnutrition and surgical outcomes.
| Nutritional Screening Tool | Variables Included | Pro | Cons |
|---|---|---|---|
| Mini Nutritional Assessment Short Form (MNA-SF) [49] |
|
|
|
| Malnutrition Universal Screening Test (MUST) [50] |
|
|
|
| Simplified Nutritional Appetite Questionnaire (SNAQ) [51] |
|
|
|
| Nutritional Risk Screening 2002 (NRS 2002) [52] |
|
|
|
| Malnutrition Screening Tool (MST) [53] |
|
|
|
| Nutrition Risk in the Critically Ill (NUTRIC Score) [53,54] |
|
|
|
| Nutritional Risk Index (NRI) [55] |
|
|
|
| Liver disease-tailored | |||
| The Royal Free Hospital-Nutritional Prioritizing Tool (RFH-NPT) [56] |
|
|
|
| The Liver Disease Undernutrition Screening Tool (LDUST) [57] |
|
|
|
4.2. Specific Nutritional Assessment for Liver Disease
4.3. Body Compositions and Muscle Assessments
5. Malnutrition and Sarcopenia in Orthotopic Liver Transplantation (LT) Candidates
6. Nutritional Management Strategies before LT Patients
7. Nutritional Management Strategies after LT
7.1. Nutritional Support Immediately after LT
7.2. Dietary Recommendations in Patients on Immunosuppressive Therapy
7.3. Diet and Calorie Intake in LT Patients
7.4. Long-Term Nutritional Support after LT
7.5. Eating Behaviour and Psychological Factors
7.6. Physical Activity after Liver Transplantation
8. Role of Bariatric Surgery in LT Setting
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Yasuda, S.; Nomi, T.; Hokuto, D.; Yoshikawa, T.; Matsuo, Y.; Sho, M. Liver Regeneration After Major Liver Resection for Hepatocellular Carcinoma in the Elderly. J. Investig. Surg. 2020, 33, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Merli, M.; Berzigotti, A.; Zelber-Sagi, S.; Dasarathy, S.; Montagnese, S.; Genton, L.; Plauth, M.; Parés, A. EASL Clinical Practice Guidelines on Nutrition in Chronic Liver Disease. J. Hepatol. 2019, 70, 172–193. [Google Scholar] [CrossRef] [PubMed]
- Franco, D.; Belghiti, J.; Cortesse, A.; Boucquey, B.M.; Charra, M.; Lacaine, F.; Bismuth, H. Nutritional status and immunity in alcoholic cirrhosis (author’s transl). Gastroenterol. Clin. Biol. 1981, 5, 839–846. [Google Scholar] [PubMed]
- Maharshi, S.; Sharma, B.C.; Srivastava, S. Malnutrition in Cirrhosis Increases Morbidity and Mortality: Malnutrition in Cirrhosis. J. Gastroenterol. Hepatol. 2015, 30, 1507–1513. [Google Scholar] [CrossRef]
- Merli, M.; Romiti, A.; Riggio, O.; Capocaccia, L. Optimal Nutritional Indexes in Chronic Liver Disease. JPEN J. Parenter. Enter. Nutr. 1987, 11, 130S–134S. [Google Scholar] [CrossRef]
- Merli, M. Nutritional Status in Cirrhosis. Italian Multicentre Cooperative Project on Nutrition in Liver Cirrhosis. J. Hepatol. 1994, 21, 317–325. [Google Scholar]
- McCullough, A.J.; Mullen, K.D.; Smanik, E.J.; Tabbaa, M.; Szauter, K. Nutritional Therapy and Liver Disease. Gastroenterol. Clin. N. Am. 1989, 18, 619–643. [Google Scholar] [CrossRef]
- Carvalho, L.; Parise, E.R. Evaluation of Nutritional Status of Nonhospitalized Patients with Liver Cirrhosis. Arq. Gastroenterol. 2006, 43, 269–274. [Google Scholar] [CrossRef]
- Marasco, G.; Dajti, E.; Ravaioli, F.; Brocchi, S.; Rossini, B.; Alemanni, L.V.; Peta, G.; Bartalena, L.; Golfieri, R.; Festi, D.; et al. Clinical Impact of Sarcopenia Assessment in Patients with Liver Cirrhosis. Expert Rev. Gastroenterol. Hepatol. 2021, 15, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y. Sarcopenia in the Prognosis of Cirrhosis: Going beyond the MELD Score. World J. Gastroenterol. 2015, 21, 7637. [Google Scholar] [CrossRef]
- Merli, M.; Giusto, M.; Gentili, F.; Novelli, G.; Ferretti, G.; Riggio, O.; Corradini, S.G.; Siciliano, M.; Farcomeni, A.; Attili, A.F.; et al. Nutritional Status: Its Influence on the Outcome of Patients Undergoing Liver Transplantation. Liver Int. 2010, 30, 208–214. [Google Scholar] [CrossRef]
- Marasco, G.; Dajti, E.; Serenari, M.; Alemanni, L.V.; Ravaioli, F.; Ravaioli, M.; Vestito, A.; Vara, G.; Festi, D.; Golfieri, R.; et al. Sarcopenia Predicts Major Complications after Resection for Primary Hepatocellular Carcinoma in Compensated Cirrhosis. Cancers 2022, 14, 1935. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-S.; Kao, J.-H. Sarcopenia and Chronic Liver Diseases. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 1229–1244. [Google Scholar] [CrossRef] [PubMed]
- Van Vugt, J.L.A.; Levolger, S.; de Bruin, R.W.F.; van Rosmalen, J.; Metselaar, H.J.; IJzermans, J.N.M. Systematic Review and Meta-Analysis of the Impact of Computed Tomography–Assessed Skeletal Muscle Mass on Outcome in Patients Awaiting or Undergoing Liver Transplantation. Am. J. Transplant. 2016, 16, 2277–2292. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM Criteria for the Diagnosis of Malnutrition—A Consensus Report from the Global Clinical Nutrition Community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ebadi, M.; Bhanji, R.A.; Mazurak, V.C.; Montano-Loza, A.J. Sarcopenia in Cirrhosis: From Pathogenesis to Interventions. J. Gastroenterol. 2019, 54, 845–859. [Google Scholar] [CrossRef] [PubMed]
- Dasarathy, S.; Merli, M. Sarcopenia from Mechanism to Diagnosis and Treatment in Liver Disease. J. Hepatol. 2016, 65, 1232–1244. [Google Scholar] [CrossRef]
- Wu, J.; Meng, Q.-H. Current Understanding of the Metabolism of Micronutrients in Chronic Alcoholic Liver Disease. World J. Gastroenterol. 2020, 26, 4567–4578. [Google Scholar] [CrossRef]
- Sanvisens, A.; Zuluaga, P.; Pineda, M.; Fuster, D.; Bolao, F.; Juncà, J.; Tor, J.; Muga, R. Folate Deficiency in Patients Seeking Treatment of Alcohol Use Disorder. Drug Alcohol Depend. 2017, 180, 417–422. [Google Scholar] [CrossRef]
- Ravaioli, F.; Pivetti, A.; Di Marco, L.; Chrysanthi, C.; Frassanito, G.; Pambianco, M.; Sicuro, C.; Gualandi, N.; Guasconi, T.; Pecchini, M.; et al. Role of Vitamin D in Liver Disease and Complications of Advanced Chronic Liver Disease. Int. J. Mol. Sci. 2022, 23, 9016. [Google Scholar] [CrossRef]
- Yamato, M.; Muto, Y.; Yoshida, T.; Kato, M.; Moriwaki, H. Clearance Rate of Plasma Branched-Chain Amino Acids Correlates Significantly with Blood Ammonia Level in Patients with Liver Cirrhosis. Int. Hepatol. Commun. 1995, 3, 91–96. [Google Scholar] [CrossRef]
- Montanari, A.; Simoni, I.; Vallisa, D.; Trifirò, A.; Colla, R.; Abbiati, R.; Borghi, L.; Novarini, A. Free Amino Acids in Plasma and Skeletal Muscle of Patients with Liver Cirrhosis. Hepatology 1988, 8, 1034–1039. [Google Scholar] [CrossRef] [PubMed]
- Shalimar; Sheikh, M.F.; Mookerjee, R.P.; Agarwal, B.; Acharya, S.K.; Jalan, R. Prognostic Role of Ammonia in Patients with Cirrhosis. Hepatology 2019, 70, 982–994. [Google Scholar] [CrossRef]
- Dajti, E.; Renzulli, M.; Colecchia, A.; Bacchi-Reggiani, M.L.; Milandri, M.; Rossini, B.; Ravaioli, F.; Marasco, G.; Alemanni, L.V.; Ierardi, A.M.; et al. Size and Location of Spontaneous Portosystemic Shunts Predict the Risk of Decompensation in Cirrhotic Patients. Dig. Liver Dis. 2022, 54, 103–110. [Google Scholar] [CrossRef]
- Hanai, T.; Shiraki, M.; Imai, K.; Suetugu, A.; Takai, K.; Shimizu, M. Usefulness of Carnitine Supplementation for the Complications of Liver Cirrhosis. Nutrients 2020, 12, 1915. [Google Scholar] [CrossRef] [PubMed]
- Owen, O.E.; Reichle, F.A.; Mozzoli, M.A.; Kreulen, T.; Patel, M.S.; Elfenbein, I.B.; Golsorkhi, M.; Chang, K.H.; Rao, N.S.; Sue, H.S.; et al. Hepatic, Gut, and Renal Substrate Flux Rates in Patients with Hepatic Cirrhosis. J. Clin. Investig. 1981, 68, 240–252. [Google Scholar] [CrossRef]
- Owen, O.E.; Trapp, V.E.; Reichard, G.A.; Mozzoli, M.A.; Moctezuma, J.; Paul, P.; Skutches, C.L.; Boden, G. Nature and Quantity of Fuels Consumed in Patients with Alcoholic Cirrhosis. J. Clin. Investig. 1983, 72, 1821–1832. [Google Scholar] [CrossRef] [PubMed]
- Bunchorntavakul, C.; Reddy, K.R. Review Article: Malnutrition/Sarcopenia and Frailty in Patients with Cirrhosis. Aliment. Pharmacol. Ther. 2020, 51, 64–77. [Google Scholar] [CrossRef]
- Renzulli, M.; Dajti, E.; Ierardi, A.M.; Brandi, N.; Berzigotti, A.; Milandri, M.; Rossini, B.; Clemente, A.; Ravaioli, F.; Marasco, G.; et al. Validation of a Standardized CT Protocol for the Evaluation of Varices and Porto-Systemic Shunts in Cirrhotic Patients. Eur. J. Radiol. 2022, 147, 110010. [Google Scholar] [CrossRef]
- Welch, N.; Dasarathy, J.; Runkana, A.; Penumatsa, R.; Bellar, A.; Reen, J.; Rotroff, D.; McCullough, A.J.; Dasarathy, S. Continued Muscle Loss Increases Mortality in Cirrhosis: Impact of Aetiology of Liver Disease. Liver Int. 2020, 40, 1178–1188. [Google Scholar] [CrossRef] [PubMed]
- Thapaliya, S.; Runkana, A.; McMullen, M.R.; Nagy, L.E.; McDonald, C.; Prasad, S.V.N.; Dasarathy, S. Alcohol-Induced Autophagy Contributes to Loss in Skeletal Muscle Mass. Autophagy 2014, 10, 677–690. [Google Scholar] [CrossRef] [PubMed]
- Bousquet-Dubouch, M.-P.; Nguen, S.; Bouyssié, D.; Burlet-Schiltz, O.; French, S.W.; Monsarrat, B.; Bardag-Gorce, F. Chronic Ethanol Feeding Affects Proteasome-Interacting Proteins. Proteomics 2009, 9, 3609–3622. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Tandon, P.; Bernal, W.; Tapper, E.B.; Ekong, U.; Dasarathy, S.; Carey, E.J. Malnutrition, Frailty, and Sarcopenia in Patients with Cirrhosis: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2021, 74, 1611–1644. [Google Scholar] [CrossRef] [PubMed]
- Bhanji, R.A.; Narayanan, P.; Allen, A.M.; Malhi, H.; Watt, K.D. Sarcopenia in Hiding: The Risk and Consequence of Underestimating Muscle Dysfunction in Nonalcoholic Steatohepatitis. Hepatology 2017, 66, 2055–2065. [Google Scholar] [CrossRef]
- Abrigo, J.; Gonzalez, F.; Aguirre, F.; Tacchi, F.; Gonzalez, A.; Meza, M.P.; Simon, F.; Cabrera, D.; Arrese, M.; Karpen, S.; et al. Cholic Acid and Deoxycholic Acid Induce Skeletal Muscle Atrophy through a Mechanism Dependent on TGR5 Receptor. J. Cell Physiol. 2021, 236, 260–272. [Google Scholar] [CrossRef]
- Hayashi, F.; Matsumoto, Y.; Momoki, C.; Yuikawa, M.; Okada, G.; Hamakawa, E.; Kawamura, E.; Hagihara, A.; Toyama, M.; Fujii, H.; et al. Physical Inactivity and Insufficient Dietary Intake Are Associated with the Frequency of Sarcopenia in Patients with Compensated Viral Liver Cirrhosis: Sarcopenia in Compensated Liver Cirrhosis. Hepatol. Res. 2013, 43, 1264–1275. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Social Determinants of Health: Know What Affects Health. Available online: https://www.cdc.gov/socialdeterminants/index.htm (accessed on 16 August 2020).
- Reilly, J.J. Health Consequences of Obesity. Arch. Dis. Child. 2003, 88, 748–752. [Google Scholar] [CrossRef]
- Spengler, E.K.; O’Leary, J.G.; Te, H.S.; Rogal, S.; Pillai, A.A.; Al-Osaimi, A.; Desai, A.; Fleming, J.N.; Ganger, D.; Seetharam, A.; et al. Liver Transplantation in the Obese Cirrhotic Patient. Transplantation 2017, 101, 2288–2296. [Google Scholar] [CrossRef]
- Bambha, K.M.; Dodge, J.L.; Gralla, J.; Sprague, D.; Biggins, S.W. Low, Rather than High, Body Mass Index Confers Increased Risk for Post-Liver Transplant Death and Graft Loss: Risk Modulated by Model for End-Stage Liver Disease: Risk from Low Body Mass Index. Liver Transplant. 2015, 21, 1286–1294. [Google Scholar] [CrossRef]
- Choi, K.M. Sarcopenia and Sarcopenic Obesity. Korean J. Intern. Med. 2016, 31, 1054–1060. [Google Scholar] [CrossRef]
- Waters, D.L.; Baumgartner, R.N. Sarcopenia and Obesity. Clin. Geriatr. Med. 2011, 27, 401–421. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Busetto, L.; Bischoff, S.C.; Cederholm, T.; Ballesteros-Pomar, M.D.; Batsis, J.A.; Bauer, J.M.; Boirie, Y.; Cruz-Jentoft, A.J.; Dicker, D.; et al. Definition and Diagnostic Criteria for Sarcopenic Obesity: ESPEN and EASO Consensus Statement. Clin. Nutr. 2022, 41, 990–1000. [Google Scholar] [CrossRef]
- Baumgartner, R.N. Body Composition in Healthy Aging. Ann. N. Y. Acad. Sci. 2006, 904, 437–448. [Google Scholar] [CrossRef]
- Montano-Loza, A.J.; Angulo, P.; Meza-Junco, J.; Prado, C.M.M.; Sawyer, M.B.; Beaumont, C.; Esfandiari, N.; Ma, M.; Baracos, V.E. Sarcopenic Obesity and Myosteatosis Are Associated with Higher Mortality in Patients with Cirrhosis: Sarcopenic Obesity and Myosteatosis in Cirrhosis. J. Cachexia Sarcopenia Muscle 2016, 7, 126–135. [Google Scholar] [CrossRef]
- Mueller, C.; Compher, C.; Ellen, D.M.; The American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Board of Directors. A.S.P.E.N. Clinical Guidelines: Nutrition Screening, Assessment, and Intervention in Adults. J. Parenter. Enter. Nutr. 2011, 35, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Bischoff, S.C. ESPEN Guideline on Clinical Nutrition in Liver Disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef]
- Buzby, G.P.; Williford, W.O.; Peterson, O.L.; Crosby, L.O.; Page, C.P.; Reinhardt, G.F.; Mullen, J.L. A randomized clinical trial of total parenteral nutrition in malnourished surgical patients: The rationale and impact of previous clinical trials and pilot study on protocol design. Am. J. Clin. Nutr. 1988, 47, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment Short-Form (MNA(r)-SF) A Practical Tool for Identification of Nutritional Status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef]
- Gomes-Neto, A.W.; van Vliet, I.M.Y.; Osté, M.C.J.; de Jong, M.F.C.; Bakker, S.J.L.; Jager-Wittenaar, H.; Navis, G.J. Malnutrition Universal Screening Tool and Patient-Generated Subjective Global Assessment Short Form and Their Predictive Validity in Hospitalized Patients. Clin. Nutr. ESPEN 2021, 45, 252–261. [Google Scholar] [CrossRef]
- Lau, S.; Pek, K.; Chew, J.; Lim, J.P.; Ismail, N.H.; Ding, Y.Y.; Cesari, M.; Lim, W.S. The Simplified Nutritional Appetite Questionnaire (SNAQ) as a Screening Tool for Risk of Malnutrition: Optimal Cutoff, Factor Structure, and Validation in Healthy Community-Dwelling Older Adults. Nutrients 2020, 12, 2885. [Google Scholar] [CrossRef]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z. Nutritional Risk Screening (NRS 2002): A New Method Based on an Analysis of Controlled Clinical Trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef] [PubMed]
- Shaw, C.; Fleuret, C.; Pickard, J.M.; Mohammed, K.; Black, G.; Wedlake, L. Comparison of a Novel, Simple Nutrition Screening Tool for Adult Oncology Inpatients and the Malnutrition Screening Tool (MST) against the Patient-Generated Subjective Global Assessment (PG-SGA). Support Care Cancer 2015, 23, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Dos Reis, A.M.; Fructhenicht, A.V.G.; Moreira, L.F. NUTRIC Score Use around the World: A Systematic Review. Rev. Bras. Ter. Intensiv. 2019, 31, 379–385. [Google Scholar] [CrossRef]
- Prendergast, J.M.; Coe, R.M.; Chavez, M.N.; Romeis, J.C.; Miller, D.K.; Wolinsky, F.D. Clinical Validation of a Nutritional Risk Index. J. Community Health 1989, 14, 125–135. [Google Scholar] [CrossRef]
- Wu, Y.; Zhu, Y.; Feng, Y.; Wang, R.; Yao, N.; Zhang, M.; Liu, X.; Liu, H.; Shi, L.; Zhu, L.; et al. Royal Free Hospital-Nutritional Prioritizing Tool Improves the Prediction of Malnutrition Risk Outcomes in Liver Cirrhosis Patients Compared with Nutritional Risk Screening 2002. Br. J. Nutr. 2020, 124, 1293–1302. [Google Scholar] [CrossRef]
- McFarlane, M.; Hammond, C.; Roper, T.; Mukarati, J.; Ford, R.; Burrell, J.; Gordon, V.; Burch, N. Comparing Assessment Tools for Detecting Undernutrition in Patients with Liver Cirrhosis. Clin. Nutr. ESPEN 2018, 23, 156–161. [Google Scholar] [CrossRef]
- Serón-Arbeloa, C.; Labarta-Monzón, L.; Puzo-Foncillas, J.; Mallor-Bonet, T.; Lafita-López, A.; Bueno-Vidales, N.; Montoro-Huguet, M. Malnutrition Screening and Assessment. Nutrients 2022, 14, 2392. [Google Scholar] [CrossRef]
- Cederholm, T.; Bosaeus, I.; Barazzoni, R.; Bauer, J.; Van Gossum, A.; Klek, S.; Muscaritoli, M.; Nyulasi, I.; Ockenga, J.; Schneider, S.M.; et al. Diagnostic Criteria for Malnutrition—An ESPEN Consensus Statement. Clin. Nutr. 2015, 34, 335–340. [Google Scholar] [CrossRef]
- Tandon, P.; Raman, M.; Mourtzakis, M.; Merli, M. A Practical Approach to Nutritional Screening and Assessment in Cirrhosis. Hepatology 2017, 65, 1044–1057. [Google Scholar] [CrossRef]
- Borhofen, S.M.; Gerner, C.; Lehmann, J.; Fimmers, R.; Görtzen, J.; Hey, B.; Geiser, F.; Strassburg, C.P.; Trebicka, J. The Royal Free Hospital-Nutritional Prioritizing Tool Is an Independent Predictor of Deterioration of Liver Function and Survival in Cirrhosis. Dig. Dis. Sci. 2016, 61, 1735–1743. [Google Scholar] [CrossRef]
- Booi, A.N.; Menendez, J.; Norton, H.J.; Anderson, W.E.; Ellis, A.C. Validation of a Screening Tool to Identify Undernutrition in Ambulatory Patients with Liver Cirrhosis. Nutr. Clin. Pract. 2015, 30, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Haj Ali, S.; Abu Sneineh, A.; Hasweh, R. Nutritional Assessment in Patients with Liver Cirrhosis. World J. Hepatol. 2022, 14, 1694–1703. [Google Scholar] [CrossRef] [PubMed]
- Keyzer, W.D.; Huybrechts, I.; Vriendt, V.D.; Vandevijvere, S.; Slimani, N.; Oyen, H.V.; Henauw, S.D. Repeated 24-Hour Recalls versus Dietary Records for Estimating Nutrient Intakes in a National Food Consumption Survey. Food Nutr. Res. 2011, 55, 7307. [Google Scholar] [CrossRef] [PubMed]
- Morgan, M.Y.; Madden, A.M.; Soulsby, C.T.; Morris, R.W. Derivation and Validation of a New Global Method for Assessing Nutritional Status in Patients with Cirrhosis. Hepatology 2006, 44, 823–835. [Google Scholar] [CrossRef]
- Hasse, J.; Strong, S.; Gorman, M.A.; Liepa, G. Subjective Global Assessment: Alternative Nutrition-Assessment Technique for Liver-Transplant Candidates. Nutrition 1993, 9, 339–343. [Google Scholar]
- Ferreira, L.G.; Anastácio, L.R.; Lima, A.S.; Correia, M.I.T.D. Assessment of Nutritional Status of Patients Waiting for Liver Transplantation. Clin. Transplant. 2011, 25, 248–254. [Google Scholar] [CrossRef]
- Kalafateli, M.; Mantzoukis, K.; Choi Yau, Y.; Mohammad, A.O.; Arora, S.; Rodrigues, S.; de Vos, M.; Papadimitriou, K.; Thorburn, D.; O’Beirne, J.; et al. Malnutrition and Sarcopenia Predict Post-Liver Transplantation Outcomes Independently of the Model for End-Stage Liver Disease Score. J. Cachexia Sarcopenia Muscle 2017, 8, 113–121. [Google Scholar] [CrossRef]
- Montano–Loza, A.J.; Meza–Junco, J.; Prado, C.M.M.; Lieffers, J.R.; Baracos, V.E.; Bain, V.G.; Sawyer, M.B. Muscle Wasting Is Associated with Mortality in Patients With Cirrhosis. Clin. Gastroenterol. Hepatol. 2012, 10, 166–173.e1. [Google Scholar] [CrossRef]
- Tandon, P.; Montano-Loza, A.J.; Lai, J.C.; Dasarathy, S.; Merli, M. Sarcopenia and Frailty in Decompensated Cirrhosis. J. Hepatol. 2021, 75, S147–S162. [Google Scholar] [CrossRef]
- Carey, E.J.; Lai, J.C.; Wang, C.W.; Dasarathy, S.; Lobach, I.; Montano-Loza, A.J.; Dunn, M.A. A Multicenter Study to Define Sarcopenia in Patients with End-Stage Liver Disease. Liver Transplant. 2017, 23, 625–633. [Google Scholar] [CrossRef]
- Tandon, P.; Low, G.; Mourtzakis, M.; Zenith, L.; Myers, R.P.; Abraldes, J.G.; Shaheen, A.A.M.; Qamar, H.; Mansoor, N.; Carbonneau, M.; et al. A Model to Identify Sarcopenia in Patients With Cirrhosis. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2016, 14, 1473–1480. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.F.; Bamber, J.; Berzigotti, A.; Bota, S.; Cantisani, V.; Castera, L.; Cosgrove, D.; Ferraioli, G.; Friedrich-Rust, M.; Gilja, O.H.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall Med. 2017, 38, e16–e47. [Google Scholar] [CrossRef] [PubMed]
- Alfuraih, A.M.; Tan, A.L.; O’Connor, P.; Emery, P.; Wakefield, R.J. The Effect of Ageing on Shear Wave Elastography Muscle Stiffness in Adults. Aging Clin. Exp. Res. 2019, 31, 1755–1763. [Google Scholar] [CrossRef] [PubMed]
- Becchetti, C.; Lange, N.F.; Delgado, M.G.; Brönnimann, M.P.; Maurer, M.H.; Dufour, J.-F.; Berzigotti, A. 2D Shear Wave Elastography of the Rectus Femoris Muscle in Patients with Cirrhosis: Feasibility and Clinical Findings. A Pilot Study. Clin. Res. Hepatol. Gastroenterol. 2023, 47, 102080. [Google Scholar] [CrossRef] [PubMed]
- Strauss, B.J.G.; Gibson, P.R.; Stroud, D.B.; Borovnicar, D.J.; Xiong, D.W.; Keogh, J.; Group, T.M.L. Total Body Dual X-Ray Absorptiometry Is a Good Measure of Both Fat Mass and Fat-Free Mass in Liver Cirrhosis Compared to “Gold-Standard” Techniques. Ann. N. Y. Acad. Sci. 2000, 904, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, M.; Hoermann, R.; Peterson, A.; Testro, A.; Angus, P.W.; Hey, P.; Chapman, B.; Gow, P.J. Use of Dual X-Ray Absorptiometry in Men with Advanced Cirrhosis to Predict Sarcopenia-Associated Mortality Risk. Liver Int. 2019, 39, 1089–1097. [Google Scholar] [CrossRef]
- Ruiz-Margáin, A.; Macías-Rodríguez, R.U.; Duarte-Rojo, A.; Ríos-Torres, S.L.; Espinosa-Cuevas, Á.; Torre, A. Malnutrition Assessed through Phase Angle and Its Relation to Prognosis in Patients with Compensated Liver Cirrhosis: A Prospective Cohort Study. Dig. Liver Dis. 2015, 47, 309–314. [Google Scholar] [CrossRef]
- Alberino, F.; Gatta, A.; Amodio, P.; Merkel, C.; Di Pascoli, L.; Boffo, G.; Caregaro, L. Nutrition and Survival in Patients with Liver Cirrhosis. Nutrition 2001, 17, 445–450. [Google Scholar] [CrossRef]
- Yao, J.; Zhou, X.; Yuan, L.; Niu, L.Y.; Zhang, A.; Shi, H.; Duan, Z.; Xu, J. Prognostic Value of the Third Lumbar Skeletal Muscle Mass Index in Patients with Liver Cirrhosis and Ascites. Clin. Nutr. 2020, 39, 1908–1913. [Google Scholar] [CrossRef]
- Sarcopenia: Revised European Consensus on Definition and Diagnosis|Age and Ageing|Oxford Academic. Available online: https://academic.oup.com/ageing/article/48/1/16/5126243 (accessed on 15 January 2023).
- Sinclair, M.; Chapman, B.; Hoermann, R.; Angus, P.W.; Testro, A.; Scodellaro, T.; Gow, P.J. Handgrip Strength Adds More Prognostic Value to the Model for End-Stage Liver Disease Score Than Imaging-Based Measures of Muscle Mass in Men with Cirrhosis. Liver Transplant. 2019, 25, 1480–1487. [Google Scholar] [CrossRef]
- Daphnee, D.K.; John, S.; Vaidya, A.; Khakhar, A.; Bhuvaneshwari, S.; Ramamurthy, A. Hand Grip Strength: A Reliable, Reproducible, Cost-Effective Tool to Assess the Nutritional Status and Outcomes of Cirrhotics Awaiting Liver Transplant. Clin. Nutr. ESPEN 2017, 19, 49–53. [Google Scholar] [CrossRef]
- Wang, C.W.; Feng, S.; Covinsky, K.E.; Hayssen, H.; Zhou, L.-Q.; Yeh, B.M.; Lai, J.C. A Comparison of Muscle Function, Mass, and Quality in Liver Transplant Candidates: Results from the Functional Assessment in Liver Transplantation Study. Transplantation 2016, 100, 1692. [Google Scholar] [CrossRef] [PubMed]
- Van Vugt, J.L.A.; Levolger, S.; Gharbharan, A.; Koek, M.; Niessen, W.J.; Burger, J.W.A.; Willemsen, S.P.; de Bruin, R.W.F.; IJzermans, J.N.M. A Comparative Study of Software Programmes for Cross-Sectional Skeletal Muscle and Adipose Tissue Measurements on Abdominal Computed Tomography Scans of Rectal Cancer Patients. J. Cachexia Sarcopenia Muscle 2017, 8, 285–297. [Google Scholar] [CrossRef]
- Bhanji, R.A.; Takahashi, N.; Moynagh, M.R.; Narayanan, P.; Angirekula, M.; Mara, K.C.; Dierkhising, R.A.; Watt, K.D. The Evolution and Impact of Sarcopenia Pre- and Post-Liver Transplantation. Aliment. Pharmacol. Ther. 2019, 49, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Carey, E.J.; Lai, J.C.; Sonnenday, C.; Tapper, E.B.; Tandon, P.; Duarte-Rojo, A.; Dunn, M.A.; Tsien, C.; Kallwitz, E.R.; Ng, V.; et al. A North American Expert Opinion Statement on Sarcopenia in Liver Transplantation. Hepatology 2019, 70, 1816–1829. [Google Scholar] [CrossRef]
- Durand, F.; Buyse, S.; Francoz, C.; Laouénan, C.; Bruno, O.; Belghiti, J.; Moreau, R.; Vilgrain, V.; Valla, D. Prognostic Value of Muscle Atrophy in Cirrhosis Using Psoas Muscle Thickness on Computed Tomography. J. Hepatol. 2014, 60, 1151–1157. [Google Scholar] [CrossRef]
- Baracos, V.E. Psoas as a Sentinel Muscle for Sarcopenia: A Flawed Premise. J. Cachexia Sarcopenia Muscle 2017, 8, 527–528. [Google Scholar] [CrossRef]
- Frailty Predicts Waitlist Mortality in Liver Transplant Candidates—American Journal of Transplantation. Available online: https://www.amjtransplant.org/article/S1600-6135(22)25562-2/fulltext (accessed on 15 January 2023).
- Mitnitski, A.B.; Song, X.; Rockwood, K. The Estimation of Relative Fitness and Frailty in Community-Dwelling Older Adults Using Self-Report Data. J. Gerontol. Ser. A 2004, 59, M627–M632. [Google Scholar] [CrossRef]
- Kobashigawa, J.; Dadhania, D.; Bhorade, S.; Adey, D.; Berger, J.; Bhat, G.; Budev, M.; Duarte-Rojo, A.; Dunn, M.; Hall, S.; et al. Report from the American Society of Transplantation on Frailty in Solid Organ Transplantation. Am. J. Transplant. 2019, 19, 984–994. [Google Scholar] [CrossRef]
- Kao, J.; Reid, N.; Hubbard, R.E.; Homes, R.; Hanjani, L.S.; Pearson, E.; Logan, B.; King, S.; Fox, S.; Gordon, E.H. Frailty and Solid-Organ Transplant Candidates: A Scoping Review. BMC Geriatr. 2022, 22, 864. [Google Scholar] [CrossRef]
- Lai, J.C.; Rahimi, R.S.; Verna, E.C.; Kappus, M.R.; Dunn, M.A.; McAdams-DeMarco, M.; Haugen, C.E.; Volk, M.L.; Duarte-Rojo, A.; Ganger, D.R.; et al. Frailty Associated with Waitlist Mortality Independent of Ascites and Hepatic Encephalopathy in a Multicenter Study. Gastroenterology 2019, 156, 1675–1682. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Shui, A.M.; Duarte-Rojo, A.; Ganger, D.R.; Rahimi, R.S.; Huang, C.-Y.; Yao, F.; Kappus, M.; Boyarsky, B.; McAdams-Demarco, M.; et al. Frailty, Mortality, and Health Care Utilization after Liver Transplantation: From the Multicenter Functional Assessment in Liver Transplantation (FrAILT) Study. Hepatology 2022, 75, 1471–1479. [Google Scholar] [CrossRef] [PubMed]
- Kaps, L.; Lukac, L.; Michel, M.; Kremer, W.; Hilscher, M.; Gairing, S.; Galle, P.; Schattenberg, J.; Wörns, M.-A.; Nagel, M.; et al. Liver Frailty Index for Prediction of Short-Term Rehospitalization in Patients with Liver Cirrhosis. Diagnostics 2022, 12, 1069. [Google Scholar] [CrossRef]
- Wang, S.; Whitlock, R.; Xu, C.; Taneja, S.; Singh, S.; Abraldes, J.G.; Burak, K.W.; Bailey, R.J.; Lai, J.C.; Tandon, P. Frailty Is Associated with Increased Risk of Cirrhosis Disease Progression and Death. Hepatology 2022, 75, 600–609. [Google Scholar] [CrossRef]
- Dos Santos, D.P.; Kloeckner, R.; Koch, S.; Hoppe-Lotichius, M.; Zöller, D.; Toenges, G.; Kremer, W.M.; Zimmermann, T.; Mittler, J.; Lang, H.; et al. Sarcopenia as Prognostic Factor for Survival after Orthotopic Liver Transplantation. Eur. J. Gastroenterol. Hepatol. 2020, 32, 626–634. [Google Scholar] [CrossRef]
- Kamath, P.S.; Kim, W.R.; Advanced Liver Disease Study Group. The Model for End-Stage Liver Disease (MELD). Hepatology 2007, 45, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Burra, P.; Samuel, D.; Sundaram, V.; Duvoux, C.; Petrowsky, H.; Terrault, N.; Jalan, R. Limitations of Current Liver Donor Allocation Systems and the Impact of Newer Indications for Liver Transplantation. J. Hepatol. 2021, 75, S178–S190. [Google Scholar] [CrossRef]
- Myers, R.P.; Tandon, P.; Ney, M.; Meeberg, G.; Faris, P.; Shaheen, A.A.M.; Aspinall, A.I.; Burak, K.W. Validation of the Five-Variable Model for End-Stage Liver Disease (5vMELD) for Prediction of Mortality on the Liver Transplant Waiting List. Liver Int. 2014, 34, 1176–1183. [Google Scholar] [CrossRef]
- Kim, W.R.; Mannalithara, A.; Heimbach, J.K.; Kamath, P.S.; Asrani, S.K.; Biggins, S.W.; Wood, N.L.; Gentry, S.E.; Kwong, A.J. MELD 3.0: The Model for End-Stage Liver Disease Updated for the Modern Era. Gastroenterology 2021, 161, 1887–1895.e4. [Google Scholar] [CrossRef]
- Stirnimann, G.; Ebadi, M.; Tandon, P.; Montano-Loza, A.J. Should Sarcopenia Increase Priority for Transplant or Is It a Contraindication? Curr. Gastroenterol. Rep. 2018, 20, 50. [Google Scholar] [CrossRef]
- Montano-Loza, A.J.; Duarte-Rojo, A.; Meza-Junco, J.; Baracos, V.E.; Sawyer, M.B.; Pang, J.X.Q.; Beaumont, C.; Esfandiari, N.; Myers, R.P. Inclusion of Sarcopenia Within MELD (MELD-Sarcopenia) and the Prediction of Mortality in Patients with Cirrhosis. Clin. Transl. Gastroenterol. 2015, 6, e102. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Covinsky, K.E.; Dodge, J.L.; Boscardin, W.J.; Segev, D.L.; Roberts, J.P.; Feng, S. Development of a Novel Frailty Index to Predict Mortality in Patients with End—Stage Liver Disease. Hepatology 2017, 66, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Ebadi, M.; Montano-Loza, A.J. Sarcopenia and Frailty in the Prognosis of Patients on the Liver Transplant Waiting List. Liver Transplant. 2019, 25, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Lai, Q.; Magistri, P.; Lionetti, R.; Avolio, A.W.; Lenci, I.; Giannelli, V.; Pecchi, A.; Ferri, F.; Marrone, G.; Angelico, M.; et al. Sarco-Model: A Score to Predict the Dropout Risk in the Perspective of Organ Allocation in Patients Awaiting Liver Transplantation. Liver Int. 2021, 41, 1629–1640. [Google Scholar] [CrossRef]
- Mauro, E.; Diaz, J.M.; Garcia-Olveira, L.; Spina, J.C.; Savluk, L.; Zalazar, F.; Saidman, J.; De Santibañes, M.; Pekolj, J.; De Santibañes, E.; et al. Sarcopenia HIBA Score Predicts Sarcopenia and Mortality in Patients on the Liver Transplant Waiting List. Hepatol. Commun. 2022, 6, 1699–1710. [Google Scholar] [CrossRef]
- Mauro, E.; Crespo, G.; Martinez-Garmendia, A.; Gutierrez-Acevedo, M.N.; Diaz, J.M.; Saidman, J.; Bermudez, C.; Ortiz-Patron, J.; Garcia-Olveira, L.; Zalazar, F.; et al. Cystatin C and Sarcopenia Predict Acute on Chronic Liver Failure Development and Mortality in Patients on the Liver Transplant Waiting List. Transplantation 2020, 104, e188–e198. [Google Scholar] [CrossRef] [PubMed]
- Merli, M.; Nicolini, G.; Angeloni, S.; Riggio, O. Malnutrition Is a Risk Factor in Cirrhotic Patients Undergoing Surgery. Nutrition 2002, 18, 978–986. [Google Scholar] [CrossRef]
- Englesbe, M.J.; Patel, S.P.; He, K.; Lynch, R.J.; Schaubel, D.E.; Harbaugh, C.; Holcombe, S.A.; Wang, S.C.; Segev, D.L.; Sonnenday, C.J. Sarcopenia and Mortality after Liver Transplantation. J. Am. Coll. Surg. 2010, 211, 271–278. [Google Scholar] [CrossRef]
- Di Martini, A.; Cruz, R.J.; Dew, M.A.; Myaskovsky, L.; Goodpaster, B.; Fox, K.; Kim, K.H.; Fontes, P. Muscle Mass Predicts Outcomes Following Liver Transplantation: Muscle Mass Predicts Outcomes After Transplantation. Liver Transplant. 2013, 19, 1172–1180. [Google Scholar] [CrossRef]
- Chae, M.S.; Moon, K.U.; Jung, J.-Y.; Choi, H.J.; Chung, H.S.; Park, C.S.; Lee, J.; Choi, J.H.; Hong, S.H. Perioperative Loss of Psoas Muscle Is Associated with Patient Survival in Living Donor Liver Transplantation: Chae et Al. Liver Transplant. 2018, 24, 623–633. [Google Scholar] [CrossRef]
- Masuda, T.; Shirabe, K.; Ikegami, T.; Harimoto, N.; Yoshizumi, T.; Soejima, Y.; Uchiyama, H.; Ikeda, T.; Baba, H.; Maehara, Y. Sarcopenia Is a Prognostic Factor in Living Donor Liver Transplantation: Sarcopenia Is a Prognostic Factor in LDLT. Liver Transplant. 2014, 20, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Hamaguchi, Y.; Kaido, T.; Okumura, S.; Fujimoto, Y.; Ogawa, K.; Mori, A.; Hammad, A.; Tamai, Y.; Inagaki, N.; Uemoto, S. Impact of Quality as Well as Quantity of Skeletal Muscle on Outcomes after Liver Transplantation: Impact of Imac on Liver Transplantation. Liver Transplant. 2014, 20, 1413–1419. [Google Scholar] [CrossRef] [PubMed]
- Montano-Loza, A.J.; Meza-Junco, J.; Baracos, V.E.; Prado, C.M.M.; Ma, M.; Meeberg, G.; Beaumont, C.; Tandon, P.; Esfandiari, N.; Sawyer, M.B.; et al. Severe Muscle Depletion Predicts Postoperative Length of Stay but Is Not Associated with Survival after Liver Transplantation: Sarcopenia After Liver Transplantation. Liver Transplant. 2014, 20, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, F.; Dickson, E.R.; Pasha, T.; Kasparova, P.; Therneau, T.; Malinchoc, M.; DiCecco, S.; Francisco-Ziller, N.; Charlton, M. Impact of Nutritional Status on Outcomes after Liver Transplantation1. Transplantation 2000, 70, 1347–1352. [Google Scholar] [CrossRef] [PubMed]
- Harimoto, N.; Yoshizumi, T.; Izumi, T.; Motomura, T.; Harada, N.; Itoh, S.; Ikegami, T.; Uchiyama, H.; Soejima, Y.; Nishie, A.; et al. Clinical Outcomes of Living Liver Transplantation According to the Presence of Sarcopenia as Defined by Skeletal Muscle Mass, Hand Grip, and Gait Speed. Transplant. Proc. 2017, 49, 2144–2152. [Google Scholar] [CrossRef] [PubMed]
- Kuo, S.Z.; Ahmad, M.; Dunn, M.A.; Montano-Loza, A.J.; Carey, E.J.; Lin, S.; Moghe, A.; Chen, H.-W.; Ebadi, M.; Lai, J.C. Sarcopenia Predicts Post-Transplant Mortality in Acutely Ill Men Undergoing Urgent Evaluation and Liver Transplantation. Transplantation 2019, 103, 2312–2317. [Google Scholar] [CrossRef]
- Merli, M.; Giusto, M.; Giannelli, V.; Lucidi, C.; Riggio, O. Nutritional Status and Liver Transplantation. J. Clin. Exp. Hepatol. 2011, 1, 190–198. [Google Scholar] [CrossRef]
- Sawyer, R.G.; Pelletier, S.J.; Pruett, T.L. Increased Early Morbidity and Mortality with Acceptable Long-Term Function in Severely Obese Patients Undergoing Liver Transplantation: Liver Transplantation in Obese Patients. J. Clin. Transplant. 1999, 13, 126–130. [Google Scholar] [CrossRef]
- Nair, S.; Verma, S.; Thuluvath, P.J. Obesity and Its Effect on Survival in Patients Undergoing Orthotopic Liver Transplantation in the United States: Obesity and Its Effect on Survival in Patients Undergoing Orthotopic Liver Transplantation in the United States. Hepatology 2002, 35, 105–109. [Google Scholar] [CrossRef]
- Dick, A.A.S.; Spitzer, A.L.; Seifert, C.F.; Deckert, A.; Carithers, R.L.; Reyes, J.D.; Perkins, J.D. Liver Transplantation at the Extremes of the Body Mass Index: Liver Transplantation at the Extremes of BMI. Liver Transplant. 2009, 15, 968–977. [Google Scholar] [CrossRef] [PubMed]
- Harrison, J.; McKiernan, J.; Neuberger, J.M. A Prospective Study on the Effect of Recipient Nutritional Status on Outcome in Liver Transplantation. Transpl. Int. 1997, 10, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Selberg, O.; Bottcher, J.; Tusch, G.; Pichlmayr, R.; Henkel, E.; Muller, M.J. Identification of High- and Low-Risk Patients before Liver Transplantation: A Prospective Cohort Study of Nutritional and Metabolic Parameters in 150 Patients. Hepatology 1997, 25, 652–657. [Google Scholar] [CrossRef]
- Marasco, G.; Serenari, M.; Renzulli, M.; Alemanni, L.V.; Rossini, B.; Pettinari, I.; Dajti, E.; Ravaioli, F.; Golfieri, R.; Cescon, M.; et al. Clinical Impact of Sarcopenia Assessment in Patients with Hepatocellular Carcinoma Undergoing Treatments. J. Gastroenterol. 2020, 55, 927–943. [Google Scholar] [CrossRef] [PubMed]
- Mazurak, V.C.; Tandon, P.; Montano-Loza, A.J. Nutrition and the Transplant Candidate: Mazurak et Al. Liver Transplant. 2017, 23, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- Casciola, R.; Leoni, L.; Cuffari, B.; Pecchini, M.; Menozzi, R.; Colecchia, A.; Ravaioli, F. Creatine Supplementation to Improve Sarcopenia in Chronic Liver Disease: Facts and Perspectives. Nutrients 2023, 15, 863. [Google Scholar] [CrossRef]
- Ferreira, L.G.; Ferreira Martins, A.I.; Cunha, C.E.; Anastácio, L.R.; Lima, A.S.; Correia, M.I.T.D. Negative Energy Balance Secondary to Inadequate Dietary Intake of Patients on the Waiting List for Liver Transplantation. Nutrition 2013, 29, 1252–1258. [Google Scholar] [CrossRef]
- Ney, M.; Abraldes, J.G.; Ma, M.; Belland, D.; Harvey, A.; Robbins, S.; Den Heyer, V.; Tandon, P. Insufficient Protein Intake Is Associated with Increased Mortality in 630 Patients With Cirrhosis Awaiting Liver Transplantation. Nutr. Clin. Pract. 2015, 30, 530–536. [Google Scholar] [CrossRef]
- Kaido, T.; Ogawa, K.; Fujimoto, Y.; Ogura, Y.; Hata, K.; Ito, T.; Tomiyama, K.; Yagi, S.; Mori, A.; Uemoto, S. Impact of Sarcopenia on Survival in Patients Undergoing Living Donor Liver Transplantation: Impact of Sarcopenia on Liver Transplantation. Am. J. Transplant. 2013, 13, 1549–1556. [Google Scholar] [CrossRef]
- Le Cornu, K.A.; McKiernan, F.J.; Kapadia, S.A.; Neuberger, J.M. A Prospective Randomized Study of Preoperative Nutritional Supplementation in Patients Awaiting Elective Orthotopic Liver Transplantation1. Transplantation 2000, 69, 1364–1369. [Google Scholar] [CrossRef]
- Plank, L.; Mccall, J.; Gane, E.; Rafique, M.; Gillanders, L.; Mcilroy, K.; Munn, S. Pre- and Postoperative Immunonutrition in Patients Undergoing Liver Transplantation: A Pilot Study of Safety and Efficacy. Clin. Nutr. 2005, 24, 288–296. [Google Scholar] [CrossRef]
- Plank, L.D.; Mathur, S.; Gane, E.J.; Peng, S.-L.; Gillanders, L.K.; McIlroy, K.; Chavez, C.P.; Calder, P.C.; McCall, J.L. Perioperative Immunonutrition in Patients Undergoing Liver Transplantation: A Randomized Double-Blind Trial. Hepatology 2015, 61, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Bs, Q.L.; Wang, X.; Bs, H.Z.; Bs, J.B.; Tan, S.; Li, N. Peri-Operative Immunonutrition in Patients Undergoing Liver Transplantation: A Meta-Analysis of Randomized Controlled Trials. Asia Pac. J. Clin. Nutr. 2015, 24, 583–590. [Google Scholar]
- Shirabe, K.; Yoshimatsu, M.; Motomura, T.; Takeishi, K.; Toshima, T.; Muto, J.; Matono, R.; Taketomi, A.; Uchiyama, H.; Maehara, Y. Beneficial Effects of Supplementation with Branched-Chain Amino Acids on Postoperative Bacteremia in Living Donor Liver Transplant Recipients: Branched-Chain Amino Acids in Liver Transplantation. Liver Transplant. 2011, 17, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Kaido, T.; Mori, A.; Ogura, Y.; Ogawa, K.; Hata, K.; Yoshizawa, A.; Yagi, S.; Uemoto, S. Pre- and Perioperative Factors Affecting Infection after Living Donor Liver Transplantation. Nutrition 2012, 28, 1104–1108. [Google Scholar] [CrossRef]
- Grąt, M.; Wronka, K.M.; Lewandowski, Z.; Grąt, K.; Krasnodębski, M.; Stypułkowski, J.; Hołówko, W.; Masior, Ł.; Kosińska, I.; Wasilewicz, M.; et al. Effects of Continuous Use of Probiotics before Liver Transplantation: A Randomized, Double-Blind, Placebo-Controlled Trial. Clin. Nutr. 2017, 36, 1530–1539. [Google Scholar] [CrossRef]
- Eguchi, S.; Takatsuki, M.; Hidaka, M.; Soyama, A.; Ichikawa, T.; Kanematsu, T. Perioperative Synbiotic Treatment to Prevent Infectious Complications in Patients after Elective Living Donor Liver Transplantation: A Prospective Randomized Study. Am. J. Surg. 2011, 201, 498–502. [Google Scholar] [CrossRef]
- Bischoff, S.C.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Plauth, M. ESPEN Practical Guideline: Clinical Nutrition in Liver Disease. Clin. Nutr. 2020, 39, 3533–3562. [Google Scholar] [CrossRef]
- Amodio, P.; Bemeur, C.; Butterworth, R.; Cordoba, J.; Kato, A.; Montagnese, S.; Uribe, M.; Vilstrup, H.; Morgan, M.Y. The Nutritional Management of Hepatic Encephalopathy in Patients with Cirrhosis: International Society for Hepatic Encephalopathy and Nitrogen Metabolism Consensus. Hepatology 2013, 58, 325–336. [Google Scholar] [CrossRef]
- Tsien, C.D.; McCullough, A.J.; Dasarathy, S. Late Evening Snack: Exploiting a Period of Anabolic Opportunity in Cirrhosis: Evening Snack for Cirrhotic Sarcopenia. J. Gastroenterol. Hepatol. 2012, 27, 430–441. [Google Scholar] [CrossRef]
- Plank, L.D.; Gane, E.J.; Peng, S.; Muthu, C.; Mathur, S.; Gillanders, L.; McIlroy, K.; Donaghy, A.J.; McCall, J.L. Nocturnal Nutritional Supplementation Improves Total Body Protein Status of Patients with Liver Cirrhosis: A Randomized 12-Month Trial. Hepatology 2008, 48, 557–566. [Google Scholar] [CrossRef]
- Jetten, W.D.; Hogenbirk, R.N.M.; Van Meeteren, N.L.U.; Cuperus, F.J.C.; Klaase, J.M.; De Jong, R. Physical Effects, Safety and Feasibility of Prehabilitation in Patients Awaiting Orthotopic Liver Transplantation, a Systematic Review. Transpl. Int. 2022, 35, 10330. [Google Scholar] [CrossRef] [PubMed]
- Debette-Gratien, M.; Tabouret, T.; Antonini, M.-T.; Dalmay, F.; Carrier, P.; Legros, R.; Jacques, J.; Vincent, F.; Sautereau, D.; Samuel, D.; et al. Personalized Adapted Physical Activity Before Liver Transplantation: Acceptability and Results. Transplantation 2015, 99, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Wallen, M.P.; Keating, S.E.; Hall, A.; Hickman, I.J.; Pavey, T.G.; Woodward, A.J.; Skinner, T.L.; Macdonald, G.A.; Coombes, J.S. Exercise Training Is Safe and Feasible in Patients Awaiting Liver Transplantation: A Pilot Randomized Controlled Trial. Liver Transplant. 2019, 25, 1576–1580. [Google Scholar] [CrossRef] [PubMed]
- Hammad, A.; Kaido, T.; Aliyev, V.; Mandato, C.; Uemoto, S. Nutritional Therapy in Liver Transplantation. Nutrients 2017, 9, 1126. [Google Scholar] [CrossRef] [PubMed]
- Cerreto, M.; Santopaolo, F.; Gasbarrini, A.; Pompili, M.; Ponziani, F. Bariatric Surgery and Liver Disease: General Considerations and Role of the Gut–Liver Axis. Nutrients 2021, 13, 2649. [Google Scholar] [CrossRef]
- Lata, J.; Novotný, I.; Príbramská, V.; Juránková, J.; Fric, P.; Kroupa, R.; Stibůrek, O. The Effect of Probiotics on Gut Flora, Level of Endotoxin and Child-Pugh Score in Cirrhotic Patients: Results of a Double-Blind Randomized Study. Eur. J. Gastroenterol. Hepatol. 2007, 19, 1111–1113. [Google Scholar] [CrossRef]
- Yamanaka-Okumura, H.; Nakamura, T.; Takeuchi, H.; Miyake, H.; Katayama, T.; Arai, H.; Taketani, Y.; Fujii, M.; Shimada, M.; Takeda, E. Effect of Late Evening Snack with Rice Ball on Energy Metabolism in Liver Cirrhosis. Eur. J. Clin. Nutr. 2006, 60, 1067–1072. [Google Scholar] [CrossRef]
- Schiaffonati, L.; Cairo, G.; Tacchini, L.; Pappalardo, C.; Gatti, S.; Piazzini-Albani, A.; Bernelli-Zazzera, A. Protein Synthesis and Gene Expression in Transplanted and Postischemic Livers. Transplantation 1993, 55, 977–982. [Google Scholar] [CrossRef]
- Dasarathy, S. Posttransplant Sarcopenia: An Underrecognized Early Consequence of Liver Transplantation. Dig. Dis. Sci. 2013, 58, 3103–3111. [Google Scholar] [CrossRef]
- Kaido, T.; Tamai, Y.; Hamaguchi, Y.; Okumura, S.; Kobayashi, A.; Shirai, H.; Yagi, S.; Kamo, N.; Hammad, A.; Inagaki, N.; et al. Effects of Pretransplant Sarcopenia and Sequential Changes in Sarcopenic Parameters after Living Donor Liver Transplantation. Nutrition 2017, 33, 195–198. [Google Scholar] [CrossRef]
- Bergerson, J.T.; Lee, J.-G.; Furlan, A.; Sourianarayanane, A.; Fetzer, D.T.; Tevar, A.D.; Landsittel, D.P.; DiMartini, A.F.; Dunn, M.A. Liver Transplantation Arrests and Reverses Muscle Wasting. Clin. Transpl. 2015, 29, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Tsien, C.; Garber, A.; Narayanan, A.; Shah, S.N.; Barnes, D.; Eghtesad, B.; Fung, J.; McCullough, A.J.; Dasarathy, S. Post-Liver Transplantation Sarcopenia in Cirrhosis: A Prospective Evaluation. J. Gastroenterol. Hepatol. 2014, 29, 1250–1257. [Google Scholar] [CrossRef]
- Anastácio, L.R.; Ferreira, S.C. Nutrition, Dietary Intake, and Eating Behavior after Liver Transplantation. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 381–387. [Google Scholar] [CrossRef]
- Hou, W.; Li, J.; Lu, J.; Wang, J.H.; Zhang, F.Y.; Yu, H.W.; Zhang, J.; Yao, Q.W.; Wu, J.; Shi, S.Y.; et al. Effect of a Carbohydrate-Containing Late-Evening Snack on Energy Metabolism and Fasting Substrate Utilization in Adults with Acute-on-Chronic Liver Failure Due to Hepatitis B. Eur. J. Clin. Nutr. 2013, 67, 1251–1256. [Google Scholar] [CrossRef]
- Bianchi, G.; Marzocchi, R.; Agostini, F.; Marchesini, G. Update on Nutritional Supplementation with Branched-Chain Amino Acids. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Fagiuoli, S.; Colli, A.; Bruno, R.; Craxì, A.; Gaeta, G.B.; Grossi, P.; Mondelli, M.U.; Puoti, M.; Sagnelli, E.; Stefani, S.; et al. Management of Infections Pre- and Post-Liver Transplantation: Report of an AISF Consensus Conference. J. Hepatol. 2014, 60, 1075–1089. [Google Scholar] [CrossRef] [PubMed]
- Damaskos, C.; Kaskantamis, A.; Garmpis, N.; Dimitroulis, D.; Mantas, D.; Garmpi, A.; Sakellariou, S.; Angelou, A.; Syllaios, A.; Kostakis, A.; et al. Intensive Care Unit Outcomes Following Orthotopic Liver Transplantation: Single-Center Experience and Review of the Literature. Il G. Di Chir./J. Ital. Surg. Assoc. 2019, 40, 463–480. [Google Scholar]
- Hughes, M.J.; McNally, S.; Wigmore, S.J. Enhanced Recovery Following Liver Surgery: A Systematic Review and Meta-Analysis. HPB 2014, 16, 699–706. [Google Scholar] [CrossRef]
- De la Fuente, R.A. Nutrition and Chronic Liver Disease. Clin. Drug Investig. 2022, 42, 55–61. [Google Scholar] [CrossRef]
- Chin, S.E.; Shepherd, R.W.; Cleghorn, G.J.; Patrick, M.K.; Javorsky, G.; Frangoulis, E.; Ong, T.H.; Balderson, G.; Koido, Y.; Matsunami, H. Survival, Growth and Quality of Life in Children after Orthotopic Liver Transplantation: A 5 Year Experience. J. Paediatr. Child Health 1991, 27, 380–385. [Google Scholar] [CrossRef]
- Brustia, R.; Monsel, A.; Skurzak, S.; Schiffer, E.; Carrier, F.M.; Patrono, D.; Kaba, A.; Detry, O.; Malbouisson, L.; Andraus, W.; et al. Guidelines for Perioperative Care for Liver Transplantation: Enhanced Recovery After Surgery (ERAS) Recommendations. Transplantation 2022, 106, 552–561. [Google Scholar] [CrossRef] [PubMed]
- Bayramov, N.; Mammadova, S. A Review of the Current ERAS Guidelines for Liver Resection, Liver Transplantation and Pancreatoduodenectomy. Ann. Med. Surg. 2022, 82, 104596. [Google Scholar] [CrossRef] [PubMed]
- Porayko, M.K.; DiCecco, S.; O’Keefe, S.J. Impact of Malnutrition and Its Therapy on Liver Transplantation. Semin. Liver Dis. 1991, 11, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Loyal, S.; Schwarze, M.; Lobers, J.; Selberg, O.; Ringe, B.; Pichlmayr, R. Resting Energy Expenditure and Nutritional State in Patients with Liver Cirrhosis before and after Liver Transplantation. Clin. Nutr. 1994, 13, 145–152. [Google Scholar] [CrossRef]
- Canzanello, V.J.; Schwartz, L.; Taler, S.J.; Textor, S.C.; Wiesner, R.H.; Porayko, M.K.; Krom, R.A. Evolution of Cardiovascular Risk after Liver Transplantation: A Comparison of Cyclosporine A and Tacrolimus (FK506). Liver Transplant. Surg. 1997, 3, 1–9. [Google Scholar] [CrossRef]
- Ozaki, N.; Ringe, B.; Gubernatis, G.; Takada, Y.; Yamaguchi, T.; Yamaoka, Y.; Oellerich, M.; Ozawa, K.; Pichlmayr, R. Changes in Energy Substrates in Relation to Arterial Ketone Body Ratio after Human Orthotopic Liver Transplantation. Surgery 1993, 113, 403–409. [Google Scholar]
- Kaido, T.; Ogura, Y.; Ogawa, K.; Hata, K.; Yoshizawa, A.; Yagi, S.; Uemoto, S. Effects of Post-Transplant Enteral Nutrition with an Immunomodulating Diet Containing Hydrolyzed Whey Peptide after Liver Transplantation. World J. Surg. 2012, 36, 1666–1671. [Google Scholar] [CrossRef]
- Kaido, T.; Mori, A.; Ogura, Y.; Hata, K.; Yoshizawa, A.; Iida, T.; Yagi, S.; Uemoto, S. Impact of Enteral Nutrition Using a New Immuno-Modulating Diet after Liver Transplantation. Hepatogastroenterology 2010, 57, 1522–1525. [Google Scholar]
- Senkal, M.; Zumtobel, V.; Bauer, K.H.; Marpe, B.; Wolfram, G.; Frei, A.; Eickhoff, U.; Kemen, M. Outcome and Cost-Effectiveness of Perioperative Enteral Immunonutrition in Patients Undergoing Elective Upper Gastrointestinal Tract Surgery: A Prospective Randomized Study. Arch. Surg. 1999, 134, 1309–1316. [Google Scholar] [CrossRef]
- Di Maira, T.; Little, E.C.; Berenguer, M. Immunosuppression in Liver Transplant. Best Pract. Res. Clin. Gastroenterol. 2020, 46, 101681. [Google Scholar] [CrossRef]
- Malik, S.M.; deVera, M.E.; Fontes, P.; Shaikh, O.; Ahmad, J. Outcome after Liver Transplantation for NASH Cirrhosis. Am. J. Transplant. 2009, 9, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Kume, H.; Okazaki, K.; Sasaki, H. Hepatoprotective Effects of Whey Protein on D-Galactosamine-Induced Hepatitis and Liver Fibrosis in Rats. Biosci. Biotechnol. Biochem. 2006, 70, 1281–1285. [Google Scholar] [CrossRef] [PubMed]
- Noble, J.; Terrec, F.; Malvezzi, P.; Rostaing, L. Adverse Effects of Immunosuppression after Liver Transplantation. Best Pract. Res. Clin. Gastroenterol. 2021, 54, 101762. [Google Scholar] [CrossRef] [PubMed]
- Gratreak, B.D.K.; Swanson, E.A.; Lazelle, R.A.; Jelen, S.K.; Hoenderop, J.; Bindels, R.J.; Yang, C.-L.; Ellison, D.H. Tacrolimus-Induced Hypomagnesemia and Hypercalciuria Requires FKBP12 Suggesting a Role for Calcineurin. Physiol. Rep. 2020, 8, e14316. [Google Scholar] [CrossRef] [PubMed]
- Egashira, K.; Sasaki, H.; Higuchi, S.; Ieiri, I. Food-Drug Interaction of Tacrolimus with Pomelo, Ginger, and Turmeric Juice in Rats. Drug Metab. Pharmacokinet. 2012, 27, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Richardson, R.A.; Garden, O.J.; Davidson, H.I. Reduction in Energy Expenditure after Liver Transplantation. Nutrition 2001, 17, 585–589. [Google Scholar] [CrossRef]
- Richards, J.; Gunson, B.; Johnson, J.; Neuberger, J. Weight Gain and Obesity after Liver Transplantation. Transpl. Int. 2005, 18, 461–466. [Google Scholar] [CrossRef]
- Merli, M.; Giusto, M.; Riggio, O.; Gentili, F.; Molinaro, A.; Attili, A.F.; Corradini, S.G.; Rossi, M. Improvement of Nutritional Status in Malnourished Cirrhotic Patients One Year after Liver Transplantation. E-SPEN Eur. e-J. Clin. Nutr. Metab. 2011, 6, e142–e147. [Google Scholar] [CrossRef]
- Ferreira, L.G.; Santos, L.F.; Anastácio, L.R.; Lima, A.S.; Correia, M.I.T.D. Resting Energy Expenditure, Body Composition, and Dietary Intake: A Longitudinal Study before and after Liver Transplantation. Transplantation 2013, 96, 579–585. [Google Scholar] [CrossRef]
- Lunati, M.E.; Grancini, V.; Agnelli, F.; Gatti, S.; Masserini, B.; Zimbalatti, D.; Pugliese, G.; Rossi, G.; Donato, M.F.; Colombo, M.; et al. Metabolic Syndrome after Liver Transplantation: Short-Term Prevalence and Pre- and Post-Operative Risk Factors. Dig. Liver Dis. 2013, 45, 833–839. [Google Scholar] [CrossRef]
- McCoy, S.M.; Campbell, K.L.; Lassemillante, A.-C.M.; Wallen, M.P.; Fawcett, J.; Jarrett, M.; Macdonald, G.A.; Hickman, I.J. Changes in Dietary Patterns and Body Composition within 12 Months of Liver Transplantation. Hepatobiliary Surg. Nutr. 2017, 6, 317–326. [Google Scholar] [CrossRef]
- Anastácio, L.R.; Diniz, K.G.; Ribeiro, H.S.; Ferreira, L.G.; Lima, A.S.; Correia, M.I.T.D.; Vilela, E.G. Prospective Evaluation of Metabolic Syndrome and Its Components among Long-Term Liver Recipients. Liver Int. 2014, 34, 1094–1101. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, H.S.; Anastácio, L.R.; Ferreira, L.G.; Lima, A.S.; Correia, M.I.T.D. Energy Expenditure and Balance among Long Term Liver Recipients. Clin. Nutr. 2014, 33, 1147–1152. [Google Scholar] [CrossRef] [PubMed]
- Holt, R.I.; Broide, E.; Buchanan, C.R.; Miell, J.P.; Baker, A.J.; Mowat, A.P.; Mieli-Vergani, G. Orthotopic Liver Transplantation Reverses the Adverse Nutritional Changes of End-Stage Liver Disease in Children. Am. J. Clin. Nutr. 1997, 65, 534–542. [Google Scholar] [CrossRef]
- Shanbhogue, R.L.; Bistrian, B.R.; Jenkins, R.L.; Randall, S.; Blackburn, G.L. Increased Protein Catabolism without Hypermetabolism after Human Orthotopic Liver Transplantation. Surgery 1987, 101, 146–149. [Google Scholar]
- Munoz, S.J.; Deems, R.O.; Moritz, M.J.; Martin, P.; Jarrell, B.E.; Maddrey, W.C. Hyperlipidemia and Obesity after Orthotopic Liver Transplantation. Transplant. Proc. 1991, 23, 1480–1483. [Google Scholar] [PubMed]
- Martinez-Camacho, A.; Fortune, B.E.; Gralla, J.; Bambha, K. Early Weight Changes after Liver Transplantation Significantly Impact Patient and Graft Survival. Eur. J. Gastroenterol. Hepatol. 2016, 28, 107–115. [Google Scholar] [CrossRef]
- Schütz, T.; Hudjetz, H.; Roske, A.-E.; Katzorke, C.; Kreymann, G.; Budde, K.; Fritsche, L.; Neumayer, H.-H.; Lochs, H.; Plauth, M. Weight Gain in Long-Term Survivors of Kidney or Liver Transplantation—Another Paradigm of Sarcopenic Obesity? Nutrition 2012, 28, 378–383. [Google Scholar] [CrossRef]
- Carey, E.J. Sarcopenia in Solid Organ Transplantation. Nutr. Clin. Pract. 2014, 29, 159–170. [Google Scholar] [CrossRef]
- Hammad, A.; Kaido, T.; Uemoto, S. Perioperative Nutritional Therapy in Liver Transplantation. Surg. Today 2015, 45, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.-S.; Kim, H.-C.; Park, Y.-H.; Kim, S.-K. Evaluation of Malnutrition Risk after Liver Transplantation Using the Nutritional Screening Tools. Clin. Nutr. Res. 2015, 4, 242–249. [Google Scholar] [CrossRef]
- Huang, X.; Liu, X.; Yu, Y. Depression and Chronic Liver Diseases: Are There Shared Underlying Mechanisms? Front. Mol. Neurosci. 2017, 10, 134. [Google Scholar] [CrossRef]
- Teixeira, H.R.S.; Marques, D.M.; Lopes, A.R.F.; Ziviani, L.C.; Magro, J.T.J.; Mente, Ê.D.; Castro-E-Silva, O.; Galvão, C.M.; Mendes, K.D.S. Anxiety and Stress Levels on Liver Transplantation Candidates. Transplant. Proc. 2016, 48, 2333–2337. [Google Scholar] [CrossRef]
- Schaumberg, K.; Anderson, D.A.; Anderson, L.M.; Reilly, E.E.; Gorrell, S. Dietary Restraint: What’s the Harm? A Review of the Relationship between Dietary Restraint, Weight Trajectory and the Development of Eating Pathology. Clin. Obes. 2016, 6, 89–100. [Google Scholar] [CrossRef]
- Linardon, J.; Mitchell, S. Rigid Dietary Control, Flexible Dietary Control, and Intuitive Eating: Evidence for Their Differential Relationship to Disordered Eating and Body Image Concerns. Eat. Behav. 2017, 26, 16–22. [Google Scholar] [CrossRef]
- Randler, C.; Desch, I.H.; im Kampe, V.O.; Wüst-Ackermann, P.; Wilde, M.; Prokop, P. Anxiety, Disgust and Negative Emotions Influence Food Intake in Humans. Int. J. Gastron. Food Sci. 2017, 7, 11–15. [Google Scholar] [CrossRef]
- Haynos, A.F.; Wang, S.B.; Fruzzetti, A.E. Restrictive Eating Is Associated with Emotion Regulation Difficulties in a Non-Clinical Sample. Eat. Disord. 2018, 26, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Kupeli, N.; Norton, S.; Chilcot, J.; Campbell, I.C.; Schmidt, U.H.; Troop, N.A. Affect Systems, Changes in Body Mass Index, Disordered Eating and Stress: An 18-Month Longitudinal Study in Women. Health Psychol. Behav. Med. 2017, 5, 214–228. [Google Scholar] [CrossRef] [PubMed]
- Van Strien, T.; Konttinen, H.; Homberg, J.R.; Engels, R.C.M.E.; Winkens, L.H.H. Emotional Eating as a Mediator between Depression and Weight Gain. Appetite 2016, 100, 216–224. [Google Scholar] [CrossRef]
- Lazarevich, I.; Camacho, M.E.I.; Velázquez-Alva, M.D.C.; Zepeda, M.Z. Relationship among Obesity, Depression, and Emotional Eating in Young Adults. Appetite 2016, 107, 639–644. [Google Scholar] [CrossRef]
- Ferreira, S.C.; Penaforte, F.R.O.; Cardoso, A.S.R.; da Silva, M.V.T.; Lima, A.S.; Correia, M.I.T.D.; Anastácio, L.R. Eating Behaviour Patterns Are Associated with Excessive Weight Gain after Liver Transplantation. J. Hum. Nutr. Diet. 2019, 32, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Saab, S.; Sikavi, C.; Jimenez, M.; Viramontes, M.; Allen, R.; Challita, Y.; Mai, M.; Esmailzadeh, N.; Grotts, J.; Choi, G.; et al. Clinical Food Addiction Is Not Associated with Development of Metabolic Complications in Liver Transplant Recipients. J. Clin. Transl. Hepatol. 2017, 5, 335–342. [Google Scholar] [CrossRef]
- Painter, P.; Krasnoff, J.; Paul, S.M.; Ascher, N.L. Physical Activity and Health-Related Quality of Life in Liver Transplant Recipients. Liver Transplant. 2001, 7, 213–219. [Google Scholar] [CrossRef]
- Neale, J.; Smith, A.C.; Bishop, N.C. Effects of Exercise and Sport in Solid Organ Transplant Recipients: A Review. Am. J. Phys. Med. Rehabil. 2017, 96, 273–288. [Google Scholar] [CrossRef]
- Wong, R.J.; Aguilar, M.; Cheung, R.; Perumpail, R.B.; Harrison, S.A.; Younossi, Z.M.; Ahmed, A. Nonalcoholic Steatohepatitis Is the Second Leading Etiology of Liver Disease Among Adults Awaiting Liver Transplantation in the United States. Gastroenterology 2015, 148, 547–555. [Google Scholar] [CrossRef]
- Kwong, A.; Kim, W.R.; Lake, J.R.; Smith, J.M.; Schladt, D.P.; Skeans, M.A.; Noreen, S.M.; Foutz, J.; Miller, E.; Snyder, J.J.; et al. OPTN/SRTR 2018 Annual Data Report: Liver. Am. J. Transplant. 2020, 20 (Suppl. S1), 42. [Google Scholar] [CrossRef] [PubMed]
- Chooi, Y.C.; Ding, C.; Magkos, F. The Epidemiology of Obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef]
- Leonard, J.; Heimbach, J.K.; Malinchoc, M.; Watt, K.; Charlton, M. The Impact of Obesity on Long-Term Outcomes in Liver Transplant Recipients—Results of the NIDDK Liver Transplant Database. Am. J. Transplant. 2008, 8, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Dare, A.J.; Plank, L.D.; Phillips, A.R.J.; Gane, E.J.; Harrison, B.; Orr, D.; Jiang, Y.; Bartlett, A.S.J.R. Additive Effect of Pretransplant Obesity, Diabetes, and Cardiovascular Risk Factors on Outcomes after Liver Transplantation: Obesity, Diabetes, and Cardiovascular Risk Factors. Liver Transplant. 2014, 20, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Chobanmdfacs, P.; Flancbaummdfacs, L. The Impact of Obesity on Surgical Outcomes: A Review. J. Am. Coll. Surg. 1997, 185, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Barone, M.; Viggiani, M.T.; Losurdo, G.; Principi, M.; Leandro, G.; Di Leo, A. Systematic Review with Meta-Analysis: Post-Operative Complications and Mortality Risk in Liver Transplant Candidates with Obesity. Aliment. Pharmacol. Ther. 2017, 46, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Patton, H.; Heimbach, J.; McCullough, A. AGA Clinical Practice Update on Bariatric Surgery in Cirrhosis: Expert Review. Clin. Gastroenterol. Hepatol. 2021, 19, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Eilenberg, M.; Langer, F.B.; Beer, A.; Trauner, M.; Prager, G.; Staufer, K. Significant Liver-Related Morbidity After Bariatric Surgery and Its Reversal—A Case Series. Obes. Surg. 2018, 28, 812–819. [Google Scholar] [CrossRef]
- Jan, A.; Narwaria, M.; Mahawar, K.K. A Systematic Review of Bariatric Surgery in Patients with Liver Cirrhosis. Obes. Surg. 2015, 25, 1518–1526. [Google Scholar] [CrossRef] [PubMed]
- McCarty, T.R.; Jirapinyo, P.; Thompson, C.C. Effect of Sleeve Gastrectomy on Ghrelin, GLP-1, PYY, and GIP Gut Hormones: A Systematic Review and Meta-Analysis. Ann. Surg. 2020, 272, 72–80. [Google Scholar] [CrossRef]
- Lavín-Alconero, L.; Fernández-Lanas, T.; Iruzubieta-Coz, P.; Arias-Loste, M.T.; Rodriguez-Duque, J.C.; Rivas, C.; Cagigal, M.L.; Montalbán, C.; Useros, A.L.; Álvarez-Cancelo, A.; et al. Efficacy and Safety of Endoscopic Sleeve Gastroplasty versus Laparoscopic Sleeve Gastrectomy in Obese Subjects with Non-Alcoholic SteatoHepatitis (NASH): Study Protocol for a Randomized Controlled Trial (TESLA-NASH Study). Trials 2021, 22, 756. [Google Scholar] [CrossRef]
- Mittal, T.; Ahuja, A.; Dey, A.; Malik, V.K.; Sheikh, M.T.M.; Bansal, N.K.; Kanuri, H. Safety and Efficacy of Laparoscopic Sleeve Gastrectomy in Patients with Portal Hypertension with Liver Function of Childs A. Surg. Endosc. 2022, 36, 2942–2948. [Google Scholar] [CrossRef]
- Tichansky, D.S.; Madan, A.K. Laparoscopic Roux-En-Y Gastric Bypass Is Safe and Feasible after Orthotopic Liver Transplantation. Obes. Surg. 2005, 15, 1481–1486. [Google Scholar] [CrossRef]
- Choudhary, N.S.; Puri, R.; Saraf, N.; Saigal, S.; Kumar, N.; Rai, R.; Rastogi, A.; Goja, S.; Bhangui, P.; Ramchandra, S.K.; et al. Intragastric Balloon as a Novel Modality for Weight Loss in Patients with Cirrhosis and Morbid Obesity Awaiting Liver Transplantation. Indian J. Gastroenterol. 2016, 35, 113–116. [Google Scholar] [CrossRef]
- Watt, K.D.; Heimbach, J.K.; Rizk, M.; Jaruvongvanich, P.; Sanchez, W.; Port, J.; Venkatesh, S.K.; Bamlet, H.; Tiedtke, K.; Malhi, H.; et al. Efficacy and Safety of Endoscopic Balloon Placement for Weight Loss in Patients with Cirrhosis Awaiting Liver Transplantation. Liver Transplant. 2021, 27, 1239–1247. [Google Scholar] [CrossRef]
- Lassailly, G.; Caiazzo, R.; Buob, D.; Pigeyre, M.; Verkindt, H.; Labreuche, J.; Raverdy, V.; Leteurtre, E.; Dharancy, S.; Louvet, A.; et al. Bariatric Surgery Reduces Features of Nonalcoholic Steatohepatitis in Morbidly Obese Patients. Gastroenterology 2015, 149, 379–388. [Google Scholar] [CrossRef]
- Diwan, T.S.; Rice, T.C.; Heimbach, J.K.; Schauer, D.P. Liver Transplantation and Bariatric Surgery: Timing and Outcomes: Liver Transplantation and Bariatric Surgery. Liver Transplant. 2018, 24, 1280–1287. [Google Scholar] [CrossRef]
- Lin, M.Y.C.; Mehdi Tavakol, M.; Sarin, A.; Amirkiai, S.M.; Rogers, S.J.; Carter, J.T.; Posselt, A.M. Laparoscopic Sleeve Gastrectomy Is Safe and Efficacious for Pretransplant Candidates. Surg. Obes. Relat. Dis. 2013, 9, 653–658. [Google Scholar] [CrossRef]
- Takata, M.C.; Campos, G.M.; Ciovica, R.; Rabl, C.; Rogers, S.J.; Cello, J.P.; Ascher, N.L.; Posselt, A.M. Laparoscopic Bariatric Surgery Improves Candidacy in Morbidly Obese Patients Awaiting Transplantation. Surg. Obes. Relat. Dis. 2008, 4, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Tariciotti, L.; D’Ugo, S.; Manzia, T.M.; Tognoni, V.; Sica, G.; Gentileschi, P.; Tisone, G. Combined Liver Transplantation and Sleeve Gastrectomy for End-Stage Liver Disease in a Bariatric Patient: First European Case-Report. Int. J. Surg. Case Rep. 2016, 28, 38–41. [Google Scholar] [CrossRef]
- Zamora-Valdes, D.; Watt, K.D.; Kellogg, T.A.; Poterucha, J.J.; Di Cecco, S.R.; Francisco-Ziller, N.M.; Taner, T.; Rosen, C.B.; Heimbach, J.K. Long-Term Outcomes of Patients Undergoing Simultaneous Liver Transplantation and Sleeve Gastrectomy. Hepatology 2018, 68, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Nesher, E.; Mor, E.; Shlomai, A.; Naftaly-Cohen, M.; Yemini, R.; Yussim, A.; Brown, M.; Keidar, A. Simultaneous Liver Transplantation and Sleeve Gastrectomy: Prohibitive Combination or a Necessity? Obes. Surg. 2017, 27, 1387–1390. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.A.; Arauz, O.; Angus, P.W.; Sinclair, M.; MacDonald, G.A.; Chelvaratnam, U.; Wigg, A.J.; Yeap, S.; Shackel, N.; Lin, L.; et al. Additive Impact of Pre-Liver Transplant Metabolic Factors on Survival Post-Liver Transplant: Pre-Liver Transplant Metabolic Factors. J. Gastroenterol. Hepatol. 2016, 31, 1016–1024. [Google Scholar] [CrossRef]
- Lin, M.Y.C.; Tavakol, M.M.; Sarin, A.; Amirkiai, S.M.; Rogers, S.J.; Carter, J.T.; Posselt, A.M. Safety and Feasibility of Sleeve Gastrectomy in Morbidly Obese Patients Following Liver Transplantation. Surg. Endosc. 2013, 27, 81–85. [Google Scholar] [CrossRef]
- Tsamalaidze, L.; Stauffer, J.A.; Arasi, L.C.; Villacreses, D.E.; Franco, J.S.S.; Bowers, S.; Elli, E.F. Laparoscopic Sleeve Gastrectomy for Morbid Obesity in Patients After Orthotopic Liver Transplant: A Matched Case-Control Study. Obes. Surg. 2018, 28, 444–450. [Google Scholar] [CrossRef]
- Diwan, T.S.; Lichvar, A.B.; Leino, A.D.; Vinks, A.A.; Christians, U.; Shields, A.R.; Cardi, M.A.; Fukuda, T.; Mizuno, T.; Kaiser, T.; et al. Pharmacokinetic and Pharmacogenetic Analysis of Immunosuppressive Agents after Laparoscopic Sleeve Gastrectomy. Clin. Transplant. 2017, 31, e12975. [Google Scholar] [CrossRef] [PubMed]
- Manzano-Nunez, R.; Rivera-Esteban, J.; Comas, M.; Angel, M.; Flores, V.; Bañares, J.; Ciudin, A.; Vilallonga, R.; Pericas, J.M. Outcomes of Patients with Severe Obesity and Cirrhosis with Portal Hypertension Undergoing Bariatric Surgery: A Systematic Review. Obes. Surg. 2023, 33, 224–233. [Google Scholar] [CrossRef] [PubMed]

| Techniques | Pro | Cons | Reference |
|---|---|---|---|
| Sleeve gastrectomy (SG) | Mechanical and hormonal weight loss. No interference with corticosteroid pharmacokinetics. Easier access in the event of gastric variceal bleeding. Maintains access to the biliary system. | Development of Gastroesophageal Reflux Disease (GERD). | Mittal et al., 2021 [220] |
| Laparoscopic adjustable gastric banding (LAGB) | Lower early complications and shorter operative time and length of stay. | Interference with corticosteroid pharmacokinetics. Not the most effective surgical procedure to reducing weight. | Tichansky et al., 2005 [221] |
| Roux-en-Y gastric bypass (RYGB) | Reduction of reflux gastritis and esophagitis. It improved glycemic control and high-density lipoprotein levels. | No access to the biliary system. Possible development of a stomal ulcer. Increased probability of cholelithiasis and Roux stasis syndrome. Interference with corticosteroid pharmacokinetics. | Tichansky et al., 2005 [221] |
| Intragastric balloon (IGB) | Non-invasive and rapid procedure. Rapid weight loss. | Upper gastrointestinal bleeding. Increase in liver fat fraction. Rapid weight loss. Not durable. | Watt et al., 2021 [223] |
| Timing | Pro | Cons | Reference |
| Before LT | Resolution of obesity-related comorbidities. | Increased costs. Two different hospitalisations. Increased patient discomfort and delayed LT. Worsening sarcopenia and malnourishment of the patient. | Diwan et al., 2018 [225] |
| During LT | Resolution of obesity-related comorbidities. Costs and patient discomfort are minimised. | The complexity of the procedure. | Tariciotti et al., 2016 [228] |
| After LT | Decrease in obesity-related comorbidities after LT. | Increased susceptibility to infections. Poor wound healing. Hostile abdominal environment after LT. | Lin et al., 2013 [232] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ravaioli, F.; De Maria, N.; Di Marco, L.; Pivetti, A.; Casciola, R.; Ceraso, C.; Frassanito, G.; Pambianco, M.; Pecchini, M.; Sicuro, C.; et al. From Listing to Recovery: A Review of Nutritional Status Assessment and Management in Liver Transplant Patients. Nutrients 2023, 15, 2778. https://doi.org/10.3390/nu15122778
Ravaioli F, De Maria N, Di Marco L, Pivetti A, Casciola R, Ceraso C, Frassanito G, Pambianco M, Pecchini M, Sicuro C, et al. From Listing to Recovery: A Review of Nutritional Status Assessment and Management in Liver Transplant Patients. Nutrients. 2023; 15(12):2778. https://doi.org/10.3390/nu15122778
Chicago/Turabian StyleRavaioli, Federico, Nicola De Maria, Lorenza Di Marco, Alessandra Pivetti, Riccardo Casciola, Carlo Ceraso, Gabriella Frassanito, Martina Pambianco, Maddalena Pecchini, Chiara Sicuro, and et al. 2023. "From Listing to Recovery: A Review of Nutritional Status Assessment and Management in Liver Transplant Patients" Nutrients 15, no. 12: 2778. https://doi.org/10.3390/nu15122778
APA StyleRavaioli, F., De Maria, N., Di Marco, L., Pivetti, A., Casciola, R., Ceraso, C., Frassanito, G., Pambianco, M., Pecchini, M., Sicuro, C., Leoni, L., Di Sandro, S., Magistri, P., Menozzi, R., Di Benedetto, F., & Colecchia, A. (2023). From Listing to Recovery: A Review of Nutritional Status Assessment and Management in Liver Transplant Patients. Nutrients, 15(12), 2778. https://doi.org/10.3390/nu15122778








