Beyond Seasoning—The Role of Herbs and Spices in Rheumatic Diseases
Abstract
1. Introduction
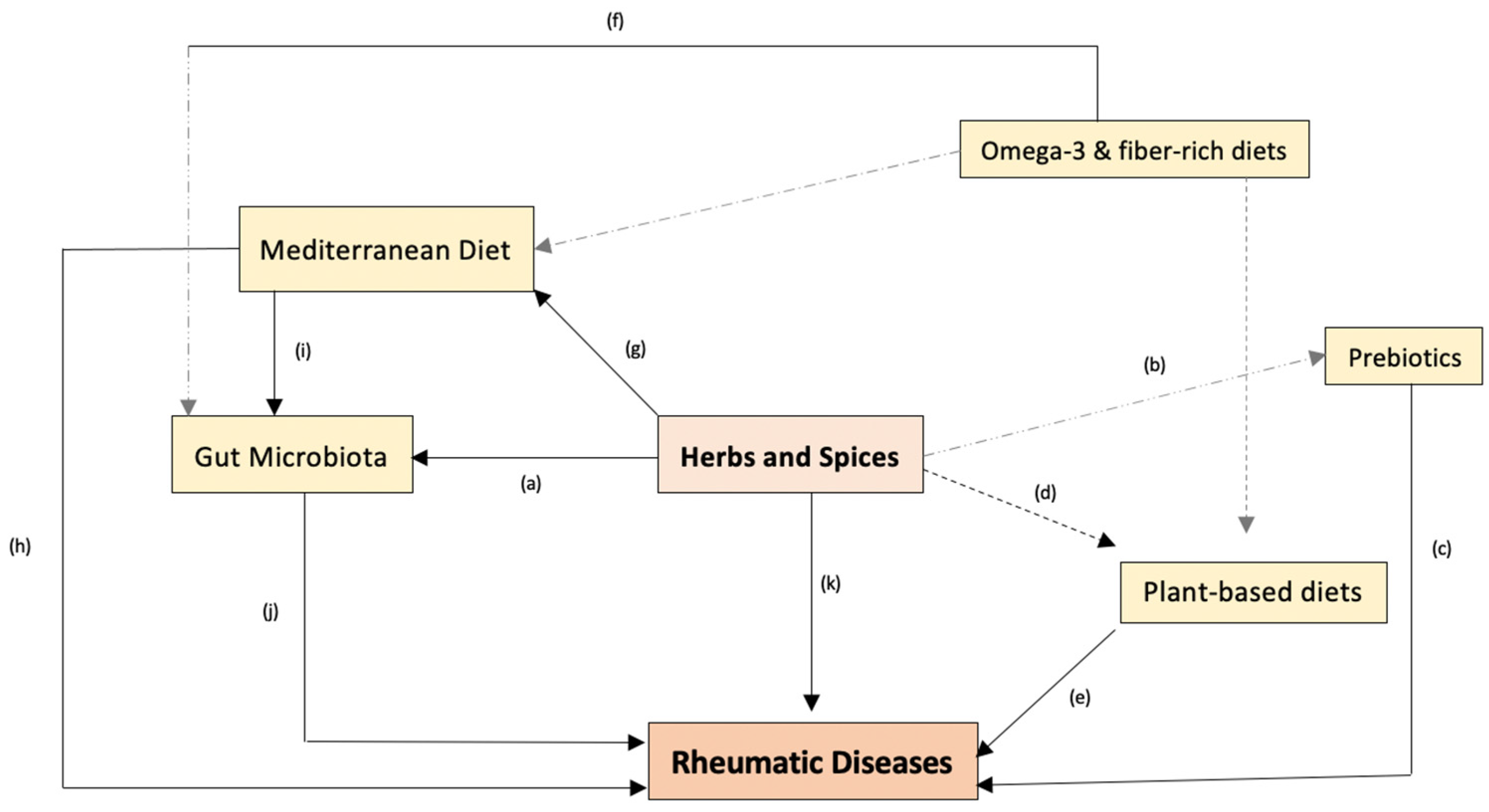
2. The Crosstalk between Diet, Gut Microbiota, and Rheumatic Diseases
3. Insights into the Bioactive Properties of Herbs and Spices and Proposed Mechanisms Whereby They May Be of Interest in Rheumatology
Gut Microbiota Modulation by Herbs and Spices
4. Experimental Evidence from Human Studies on Herbs and Spices in RDs
4.1. Rheumatoid Arthritis
| Herb/Spice | Author, Year, and Country | Study Design | Population, Sample Size (Intervention, Control) | Preparation/Dose (Intervention vs. Control) and Duration | Evaluated Parameters | Main Findings | Reported Adverse Effects (AEs) |
|---|---|---|---|---|---|---|---|
| Cinnamon | Shishehbor et al. [102], 2018, Iran | Double-Blind RCT | 36 women with active RA (18 patients/arm) | 4 capsules of either 500 mg cinnamon powder or placebo daily for 8 weeks | DAS-28, pain VAS, SJC, TJC, ESR, CRP, TNF-a | ↓DAS-28, ↓pain VAS, ↓SJC, ↓TJC, ↓CRP, ↓TNF-a | Intervention group: 1 patient reported mild gastric discomfort |
| Curcumin | Chandran et al. [103], 2012, India | Randomized single-blind pilot study | 45 RA patients (15 patients/arm) | 500 mg curcumin or 500 mg curcumin + 50 mg diclofenac sodium vs. 50 mg diclofenac sodium twice daily for 8 weeks | DAS-28, disease activity VAS, pain VAS, SJC, TJC, ESR, HAQ, CRP | ↓DAS28, ↓SJC, ↓TJC, ↓disease activity VAS, ↓pain VAS, ↓HAQ, ↓ESR | Diclofenac sodium: 3 adverse events. Curcumin + diclofenac sodium: 1 adverse event; curcumin: 2 adverse events |
| Amalraj et al. [104], 2017, India | Double-Blind RCT | 36 patients with active RA (12 patients/arm) | 250 mg or 500 mg curcumin vs. 500 mg of food-grade starch twice/day for 12 weeks | DAS28, pain VAS, TJC, SJC, ESR, CRP, RF | ↓DAS28, ↓SJC, ↓TJC, ↓pain VAS, ↓ESR, ↓CRP, ↓RF | None | |
| Javadi et al. [105], 2019, Iran | Double-blind RCT | 65 RA patients (n = 30, n = 35) | 40 mg curcumin nanomicelle vs. 500 mg wheat flour 3×/day for 12 weeks | DAS-28, TJC SJC, ESR | No significant changes were observed between groups | None | |
| Jacob et al. [106], 2019, India | Double-blind RCT | 24 patients with active RA (8 patients/arm) | 250 mg/day or 500 mg/day curcumin vs. placebo (non-described) for 12 weeks | DAS28, pain VAS, ESR, CRP, RF | ↓DAS28, ↓pain VAS, ↓ESR, ↓CRP, ↓RF | None | |
| Pourhabibi-Zarandi et al. [107], 2022, Iran | Double-blind RCT | 48 women with moderately active RA (24 patients/arm) | 500 mg/day curcumin vs. 1 capsule/day of starch flour for 8 weeks | ESR, hs-CRP, lipid profile, glycemic and anthropometric indices | ↓ESR, ↓hs-CRP | None | |
| Garlic | Moosavian et al. [108,109], 2020, Iran | Double-blind RCT | 70 women with moderate-to-severe RA (35 patients/arm) | 1000 mg/day garlic powder vs. 500 mg starch for 8 weeks | DAS28, pain VAS, SJC, TJC, HAQ, ESR, CRP, TNF-a, TAC, MDA | ↓DAS28, ↓pain VAS, ↓SJC, ↓TJC, ↓HAQ, ↓CRP, ↓TNF-a, ↑TAC, ↓MDA | Intervention: 1 patient with stomach pain |
| Ginger | Aryaeian et al. [110,111], 2019, Iran | Double-blind RCT | 66 patients with active RA (n = 33, n = 30) | 1500 mg/day ginger vs. roasted wheat flour for 12 weeks | DAS-28, hs-CRP, IL-1β, IL-2 and TNF-α, gene expression of NF-κB, PPAR-γ, FoxP3, T-bet, GATA-3, and RORγt | ↓DAS28, ↓hs-CRP, ↓IL-1β, ↑ FoxP3, ↓T-bet, ↓RORγt, | NA |
| Saffron | Hamidi et al. [112], 2019, Iran | Double-blind RCT | 66 women with active RA (33 patients/arm) | 100 mg/day saffron vs. 100 mg/day hydroxy propylmethyl cellulose for 12 weeks | DAS28, pain VAS, morning stiffness, SJC, TJC, PGA, TNF-α, IFN-γ, hs-CRP, ESR, MDA, TAC | ↓DAS28, ↓SJC, ↓TJC, ↓pain VAS | Intervention: stomach pain (n = 1) Control: stomach pain (n = 1) |
| Sahebari et al. [113], 2020, Iran | Double-blind RCT | 55 newly diagnosed RA patients (n = 28, n = 27) | 100 mg saffron (with additives: starch, lactose monohydrate, starch sodium glycolate, PVP K30) vs. pills with the mentioned additives for 12 weeks | DAS28, VAS, pain score, TJC, SJC, HAQ | No changes were observed between groups | None |
4.2. Osteoarthritis
| Herb/ Spice | Author, Year, and Country | Study Design | Population, Sample Size (Intervention, Control) | Preparation/Dose (Intervention vs. Control) and Duration | Evaluated Parameters | Main Findings | Reported Adverse Effects (AEs) |
|---|---|---|---|---|---|---|---|
| Curcumin | Kuptniratsaikul et al. [115], 2014, Thailand | Double-blind RCT | 331 patients with primary knee OA (n = 171, n = 160) | 1500 mg/day of Curcuma Domestica or 1200 mg/day of ibuprofen for 4 weeks | WOMAC *: total, pain, stiffness, and function, 6 min walk test | ↓WOMAC * (total, pain, stiffness, and physical function) in both groups | Ibuprofen group: 35.7%, C. Domestica: 29.7% |
| Srivastava et al. [116], 2016, India | Double-blind RCT | 160 with primary knee OA (n = 78, n = 82) | 500 mg Curcuma Longa or placebo 2×/day for 16 weeks, along with Diclofenac 50 mg/day (standard treatment as needed) | VAS, WOMAC * (pain, stiffness, and physical function), IL-Iβ, ROS, MDA | ↓VAS, ↓WOMAC *, ↓IL-Iβ, ↓ROS, ↓MDA | CL group: 2, placebo group: 4 | |
| Panahi et al. [118], 2016, Iran | Double-Blind RCT | 53 patients with mild–moderate knee OA (n = 27, n = 26) | 1500 mg/day of curcuminoids (combined with piperine) or placebo for 6 weeks | SOD, GSH, MDA | ↑SOD activities, ↑GSH conc., ↓MDA | NA | |
| Haroyan et al. [114], 2018, Armenia | Double-blind RCT | 201 patients with OA (n = 67, n = 66, n = 68) | 500 mg Curamin or 500 mg CuraMed or 500 mg placebo 3×/day for 12 weeks | PPMs (30 s-CST, 40 m FPWT, TUG, SCT), WOMAC (total, pain, stiffness, physical function limitations), ESR, CRP | ↓all WOMAC *, ↑30 s CST repetitions, ↓TUG time, ↓SCT, ↑40 m FPWT, ⇢⇠ESR, ⇢⇠CRP | 2 in Curamin, 7 in CuraMed, 4 in placebo | |
| Lopresti et al. [119], 2022, Australia | Double-blind RCT | 101 patients with active knee OA (n = 51, n = 50) | 500 mg Curcugen or placebo 2×/day for 8 weeks | KOOS, JOA, PROMIS-29, pain, PPMs (30 s-CST, 40 m FPWT, TUG, 6-min walk test), analgesic use, AE | ↓KOOS-pain, ↓pain, ↓JOA, ↑30 s CST repetitions, ↓TUG, ↓6 min walk test (m), ⇢⇠40 m FPWT, ↓pain medication use | 5 in curcumin group and 10 in placebo group | |
| Garlic | Hussein et al. [124], 2015, Egypt | Single-blind RCT | 43 patients with knee OA (n = 15, n = 28) | Group 1: comprehensive rehabilitation; Group 2: garlic therapy (900 mg/day) + comprehensive rehabilitation for 8 weeks | Pain VAS, HAQ, 1-RM, BMI, IL-Iβ, IL6, TNF-α, selenium | ↓Pain, ↓IL-Iβ, ↓IL-6, ↓TNF-α, ↑selenium | NA |
| Salimzadeh et al. [125], 2018, Australia | Double-blind RCT | 76 post-menopausal overweight or obese women with mild–moderate knee OA (n = 39, n = 37) | 500 mg garlic tablet or placebo 2×/day for 12 weeks | WOMAC * (pain, stiffness, physical function limitation) | ↓WOMAC * (total, pain, stiffness, physical limitation, ↓pain in placebo | NA | |
| Dehghani et al. [126], 2018, Iran | Double-blind RCT | 76 post-menopausal overweight or obese women with mild–moderate knee OA (n = 39, n = 37) | 500 mg garlic tablet or placebo 2×/day for 12 weeks | Pain VAS, resistin, TNF-α, | ↓Pain VAS, ↓Resistin, ⇢⇠TNF-α | NA | |
| Hosseinzadeh-Attar et al. [127], 2020, Iran | Double-blind RCT | 48 obese women with mild–moderate knee OA (n = 23, n = 25) | 1000 mg/day garlic tablet or placebo for 12 weeks | WOMAC * (pain, stiffness, physical function limitation), pain VAS | ↓WOMAC * (total, pain, stiffness, physical limitation), ↓pain VAS | NA | |
| Ginger | Altman et al. [129], 2001, USA | Double-blind RCT | 261 patients with knee OA (n = 130, n = 131) | 255 mg ginger or placebo 2×/day for 6 weeks | Pain standing VAS, WOMAC * (total, pain, stiffness, physical function limitation), analgesic use | ↓pain standing, ↓pain walking, ↓WOMAC * (total, pain stiffness, and physical limitation), ↓analgesic use | ↑GI events in ginger group, 59% in ginger group and 37% in placebo group. No serious AEs |
| Heidari-Beni et al. [128], 2019, Iran | Double-blind RCT | 60 patients with mild–moderate knee OA (n = 30, n = 30) | Herbal formulation (30 mg curcumin, 7.5 mg gingerols, 3.75 mg piperine) or naproxen (250 mg) 2×/day for 4 weeks | PGE2 | ↓PGE2 in both groups | NA | |
| Saffron | Poursamimi et al. [123], 2019, Iran | Double-blind RCT | 35 patients with primary knee OA (n = 18, n = 17) | 15 mg/day Krocina or placebo for 16 weeks | Pain VAS, CRP, ESR, Treg-cells, Th17-cells, CD8+ T cells, CD3+ CD4+ T cells, GMFI-IL-17, GMFI-FOXP3 | ↓Pain VAS, ↓CRP, ⇢⇠ESR, ↓Th17%, ↓GMFI-IL-17, ↑Treg-cells, ↑CD4+, ⇢⇠CD8+, ⇢⇠GMFI-FOXP3, ↑Treg/Th17 ratio | NA |
4.3. Fibromyalgia
| Spice | Author, Year, and Country | Study Design | Population, Sample Size (Intervention, Control) | Preparation/Dose (Intervention vs. Control) and Duration | Evaluated Parameters | Main Findings | Reported Adverse Effects (AEs) |
|---|---|---|---|---|---|---|---|
| Saffron | Shakiba et al. [135], 2018, Iran | Double-Blind RCT | 46 patients with FM (n = 23, n = 23) | 15 mg saffron extract or duloxetine 30 mg | HRSD, FIQ, BPI, pain VAS, GFI, HADS anxiety and depression, time x treatment interaction for all parameters. | ↓HRSD, ↓FIQ, ↓BPI, ↓pain VAS, ↓GFI, ↓HADS depression, ↓HADS anxiety in both groups. No difference between the groups was observed. | 4 in saffron group, 9 in duloxetine group. |
4.4. Limitations and Implications for Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- WHO Scientific Group on Rheumatic Diseases. WHO Technical Report Series: Rheumatic Diseases. In World Health Organization—Technical Report Series; World Health Organization: Geneva, Switzerland, 1992; Volume 816. [Google Scholar]
- European League Against Rheumatism (EULAR). RheumaMap: A Research Roadmap to Transform the Lives of People with Rheumatic and Musculoskeletal Diseases; EULAR: Zürich, Switzerland, 2019. [Google Scholar]
- Moutsopoulos, H.M. Autoimmune rheumatic diseases: One or many diseases? J. Transl. Autoimmun. 2021, 4, 100129. [Google Scholar] [CrossRef]
- Van Der Heijde, D.; Daikh, D.I.; Betteridge, N.; Burmester, G.R.; Hassett, A.L.; Matteson, E.L.; Van Vollenhoven, R.; Lakhanpal, S. Common language description of the term rheumatic and musculoskeletal diseases (RMDs) for use in communication with the lay public, healthcare providers and other stakeholders endorsed by the European League Against Rheumatism (EULAR) and the College of Rheumatology (ACR). Ann. Rheum. Dis. 2018, 77, 829–832. [Google Scholar]
- Guo, Q.; Wang, Y.; Xu, D.; Nossent, J.; Pavlos, N.J.; Xu, J. Rheumatoid arthritis: Pathological mechanisms and modern pharmacologic therapies. Bone Res. 2018, 6, 15. [Google Scholar] [CrossRef] [PubMed]
- Burmester, G.R.; Bijlsma, J.W.J.; Cutolo, M.; McInnes, I.B. Managing rheumatic and musculoskeletal diseases-past, present and future. Nat. Rev. Rheumatol. 2017, 13, 443–448. [Google Scholar] [CrossRef]
- Ajeganova, S.; Huizinga, T. Sustained remission in rheumatoid arthritis: Latest evidence and clinical considerations. Adv. Musculoskelet. Dis. 2017, 9, 249–262. [Google Scholar] [CrossRef]
- Kocyigit, B.F.; Sagtaganov, Z.; Yessirkepov, M.; Akyol, A. Assessment of complementary and alternative medicine methods in the management of ankylosing spondylitis, rheumatoid arthritis, and fibromyalgia syndrome. Rheumatol. Int. 2022, 43, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Letarouilly, J.-G.; Sanchez, P.; Nguyen, Y.; Sigaux, J.; Czernichow, S.; Flipo, R.-M.; Sellam, J.; Daïen, C. Efficacy of spice supplementation in rheumatoid arthritis: A systematic literature review. Nutrients 2020, 11, 3800. [Google Scholar] [CrossRef] [PubMed]
- Kunnumakkara, A.B.; Sailo, B.L.; Banik, K.; Harsha, C.; Prasad, S.; Gupta, S.C.; Bharti, A.C.; Aggarwal, B.B. Chronic diseases, inflammation, and spices: How are they linked? J. Transl. Med. 2018, 16, 14. [Google Scholar] [CrossRef]
- Smolen, J.S.; Aletaha, D.; McInnes, I.B. Rheumatoid arthritis. Lancet 2016, 388, 2023–2038. [Google Scholar] [CrossRef]
- Smolen, J.S.; Aletaha, D.; Barton, A.; Burmester, G.R.; Emery, P.; Firestein, G.S.; Kavanaugh, A.; McInnes, I.B.; Solomon, D.H.; Strand, V.; et al. Rheumatoid arthritis. Nat. Rev. Dis. Primers 2018, 4, 18001. [Google Scholar] [CrossRef]
- Tedeschi, S.K.; Costenbader, K.H. Is There a Role for Diet in the Therapy of Rheumatoid Arthritis? Curr. Rheumatol. Rep. 2016, 18, 23. [Google Scholar] [CrossRef] [PubMed]
- Dourado, E.; Ferro, M.; Guerreiro, C.S.; Fonseca, J.E. Diet as a modulator of intestinal microbiota in rheumatoid arthritis. Nutrients. 2020, 12, 3504. [Google Scholar] [CrossRef] [PubMed]
- Guerreiro, C.S.; Calado, Â.; Sousa, J.; Fonseca, J.E. Diet, microbiota, and gut permeability-the unknown triad in rheumatoid arthritis. Front. Med. 2018, 5, 349. [Google Scholar] [CrossRef]
- Schönenberger, K.A.; Schüpfer, A.-C.; Gloy, V.L.; Hasler, P.; Stanga, Z.; Kaegi-Braun, N.; Reber, E. Effect of anti-inflammatory diets on pain in rheumatoid arthritis: A systematic review and meta-analysis. Nutrients. 2021, 13, 4221. [Google Scholar] [CrossRef] [PubMed]
- King, L.K.; March, L.; Anandacoomarasamy, A. Obesity & osteoarthritis. Indian. J. Med. Res. 2013, 63, 185–193. [Google Scholar]
- Martel-Pelletier, J.; Barr, A.J.; Cicuttini, F.M.; Conaghan, P.G.; Cooper, C.; Goldring, M.B.; Goldring, S.R.; Jones, G.; Teichtahl, A.J.; Pelletier, J.-P. Osteoarthritis. Nat. Rev. Dis. Primers 2016, 2, 16072. [Google Scholar] [CrossRef]
- Liu-Bryan, R.; Terkeltaub, R. Emerging regulators of the inflammatory process in osteoarthritis. Nat. Rev. Rheumatol. 2015, 11, 35–44. [Google Scholar] [CrossRef]
- Kapoor, M.; Martel-Pelletier, J.; Lajeunesse, D.; Pelletier, J.P.; Fahmi, H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 33–42. [Google Scholar] [CrossRef]
- Hao, X.; Shang, X.; Liu, J.; Chi, R.; Zhang, J.; Xu, T. The gut microbiota in osteoarthritis: Where do we stand and what can we do? Arthritis Res. Ther. 2021, 23, 42. [Google Scholar] [CrossRef]
- Biver, E.; Berenbaum, F.; Valdes, A.M.; de Carvalho, I.A.; Bindels, L.B.; Brandi, M.L.; Calder, P.C.; Castronovo, V.; Cavalier, E.; Cherubini, A.; et al. Gut microbiota and osteoarthritis management: An expert consensus of the European society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO). Ageing Res. Rev. 2019, 55, 100946. [Google Scholar] [CrossRef]
- Bortoluzzi, A.; Furini, F.; Scirè, C.A. Osteoarthritis and its management—Epidemiology, nutritional aspects and environmental factors. Autoimmun. Rev. 2018, 17, 1097–1104. [Google Scholar] [CrossRef]
- Morales-Ivorra, I.; Romera-Baures, M.; Roman-Viñas, B.; Serra-Majem, L. Osteoarthritis and the mediterranean diet: A systematic review. Nutrients 2018, 10, 1030. [Google Scholar] [CrossRef]
- Coskun Benlidayi, I. Role of inflammation in the pathogenesis and treatment of fibromyalgia. Rheumatol. Int. 2019, 39, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Mendieta, D.; De la Cruz-Aguilera, D.L.; Barrera-Villalpando, M.I.; Becerril-Villanueva, E.; Arreola, R.; Hernández-Ferreira, E.; Pérez-Tapia, S.M.; Pérez-Sánchez, G.; Garcés-Alvarez, M.E.; Aguirre-Cruz, L.; et al. IL-8 and IL-6 primarily mediate the inflammatory response in fibromyalgia patients. J. Neuroimmunol. 2016, 290, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Minerbi, A.; Gonzalez, E.; Brereton, N.J.B.; Anjarkouchian, A.; Dewar, K.; Fitzcharles, M.A.; Chevalier, S.; Shir, Y. Altered microbiome composition in individuals with fibromyalgia. Pain 2019, 160, 2589–2602. [Google Scholar] [CrossRef]
- Nadal-Nicolás, Y.; Miralles-Amorós, L.; Martínez-Olcina, M.; Sánchez-Ortega, M.; Mora, J.; Martínez-Rodríguez, A. Vegetarian and Vegan Diet in Fibromyalgia: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4955. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, L.C.; Hemphill, I.; Cobiac, L.; Sullivan, D.R.; Fenech, M.; Patch, C.S.; Roodenrys, S.; Keogh, J.B.; Clifton, P.M.; Williams, P.G.; et al. Health benefits of herbs and spices: The past, the present, the future. Med. J. Aust. 2006, 185, S1–S24. [Google Scholar] [CrossRef]
- Bower, A.; Marquez, S.; de Mejia, E.G. The Health Benefits of Selected Culinary Herbs and Spices Found in the Traditional Mediterranean Diet. Crit. Rev. Food Sci. Nutr. 2016, 56, 2728–2746. [Google Scholar] [CrossRef]
- Kammath, A.J.; Nair, B.; Sreelekshmi, P.; Nath, L.R. Curry versus cancer: Potential of some selected culinary spices against cancer with in vitro, in vivo, and human trials evidences. J. Food Biochem. 2021, 45, e13285. [Google Scholar] [CrossRef]
- Bi, X.; Lim, J.; Henry, C.J. Spices in the management of diabetes mellitus. Food Chem. 2017, 217, 281–293. [Google Scholar] [CrossRef]
- Vasanthi, R.H.; Parameswari, P.R. Indian Spices for Healthy Heart—An Overview. Curr. Cardiol. Rev. 2010, 6, 274–279. [Google Scholar] [CrossRef]
- Fifi, A.C.; Axelrod, C.H.; Chakraborty, P.; Saps, M. Herbs and spices in the treatment of functional gastrointestinal disorders: A review of clinical trials. Nutrients 2018, 10, 1075. [Google Scholar] [CrossRef]
- Iriti, M.; Vitalini, S.; Fico, G.; Faoro, F. Neuroprotective herbs and foods from different traditional medicines and diets. Molecules 2010, 15, 3517–3555. [Google Scholar] [CrossRef]
- Jiang, T.A. Health benefits of culinary herbs and spices. J. AOAC Int. 2019, 102, 395–411. [Google Scholar] [CrossRef] [PubMed]
- Yashin, A.; Yashin, Y.; Xia, X.; Nemzer, B. Antioxidant Activity of Spices and Their Impact on Human Health: A Review. Antioxidants 2017, 6, 70. [Google Scholar] [CrossRef]
- Opara, E.I.; Chohan, M. Culinary Herbs and Spices: Their Bioactive Properties, the Contribution of Polyphenols and the Challenges in Deducing Their True Health Benefits. Int. J. Mol. Sci. 2014, 15, 19183–19202. [Google Scholar] [CrossRef]
- Błaszczyk, N.; Rosiak, A.; Kałużna-Czaplińska, J. The potential role of cinnamon in human health. Forests 2021, 12, 648. [Google Scholar] [CrossRef]
- Hariri, M.; Ghiasvand, R. Cinnamon and chronic diseases. Adv. Exp. Med. Biol. 2016, 929, 1–24. [Google Scholar]
- Reddy, A.M.; Seo, J.H.; Ryu, S.Y.; Kim, Y.S.; Kim, Y.S.; Min, K.R.; Kim, Y. Cinnamaldehyde and 2-methoxycinnamaldehyde as NF-κB inhibitors from Cinnamomum cassia. Planta Med. 2004, 70, 823–827. [Google Scholar] [CrossRef] [PubMed]
- Pahan, S.; Pahan, K.; Brown, J.; Affairs, V. Can Cinnamon Spice Down Autoimmune Diseases? J. Clin. Exp. Immunol. 2020, 5, 252–258. [Google Scholar]
- Willenbacher, E.; Khan, S.Z.; Mujica, S.C.A.; Trapani, D.; Hussain, S.; Wolf, D.; Willenbacher, W.; Spizzo, G.; Seeber, A. Curcumin: New insights into an ancient ingredient against cancer. Int. J. Mol. Sci. 2019, 20, 1808. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of curcumin: Problems and promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef]
- Nasef, N.A.; Loveday, S.M.; Golding, M.; Martins, R.N.; Shah, T.M.; Clarke, M.; Coad, J.; Moughan, P.J.; Garg, M.L.; Singh, H. Food matrix and co-presence of turmeric compounds influence bioavailability of curcumin in healthy humans. Food Funct. 2019, 10, 4584–4592. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Akbar, U.; Mohan, C. Curcumin in Autoimmune and Rheumatic Diseases. Nutrients 2019, 11, 1004. [Google Scholar] [CrossRef]
- Hong, J.; Bose, M.; Ju, J.; Ryu, J.H.; Chen, X.; Sang, S.; Lee, M.-J.; Yang, C.S. Modulation of arachidonic acid metabolism by curcumin and related β-diketone derivatives: Effects on cytosolic phospholipase A2, cyclooxygenases and 5-lipoxygenase. Carcinogenesis 2004, 25, 1671–1679. [Google Scholar] [CrossRef]
- Zeng, L.; Yang, T.; Yang, K.; Yu, G.; Li, J.; Xiang, W.; Chen, H. Curcumin and Curcuma longa Extract in the Treatment of 10 Types of Autoimmune Diseases: A Systematic Review and Meta-Analysis of 31 Randomized Controlled Trials. Front. Immunol. 2022, 13, 896476. [Google Scholar] [CrossRef] [PubMed]
- Arreola, R.; Quintero-Fabián, S.; López-Roa, R.I.; Flores-Gutiérrez, E.O.; Reyes-Grajeda, J.P.; Carrera-Quintanar, L.; Ortuño-Sahagún, D. Immunomodulation and anti-inflammatory effects of garlic compounds. J. Immunol. Res. 2015, 2015, 401630. [Google Scholar] [CrossRef] [PubMed]
- You, S.; Nakanishi, E.; Kuwata, H.; Chen, J.; Nakasone, Y.; He, X.; He, J.; Liu, X.; Zhang, S.; Zhang, B.; et al. Inhibitory effects and molecular mechanisms of garlic organosulfur compounds on the production of inflammatory mediators. Mol. Nutr. Food Res. 2013, 57, 2049–2060. [Google Scholar] [CrossRef]
- Moutia, M.; Habti, N.; Badou, A. In Vitro and In Vivo Immunomodulator Activities of Allium sativum L. Evid. Based Complement. Altern. Med. 2018, 2018, 4984659. [Google Scholar] [CrossRef]
- Ho, C.Y.; Weng, C.J.; Jhang, J.J.; Cheng, Y.T.; Huang, S.M.; Yen, G.C. Diallyl sulfide as a potential dietary agent to reduce TNF-α- and histamine-induced proinflammatory responses in A7r5 cells. Mol. Nutr. Food Res. 2014, 58, 1069–1078. [Google Scholar] [CrossRef] [PubMed]
- Mofrad, M.D.; Milajerdi, A.; Koohdani, F.; Surkan, P.J.; Azadbakht, L. Garlic supplementation reduces circulating C-reactive protein, tumor necrosis factor, and interleukin-6 in Adults: A systematic review and meta-analysis of randomized controlled trials. J. Nutr. 2019, 149, 605–618. [Google Scholar]
- Liu, Y.; Liu, J.; Zhang, Y. Research Progress on Chemical Constituents of Zingiber officinale Roscoe. Biomed. Res. Int. 2019, 2019, 5370823. [Google Scholar] [CrossRef] [PubMed]
- Crichton, M.; Davidson, A.R.; Innerarity, C.; Marx, W.; Lohning, A.; Isenring, E. Orally consumed ginger and human health: An umbrella review. Am. J. Clin. Nutr. 2022, 115, 1511–1527. [Google Scholar] [CrossRef]
- Shimoda, H.; Shan, S.-J.; Tanaka, J.; Seki, A.; Seo, J.-W.; Kasajima, N.; Tamura, S.; Ke, Y.; Murakami, N. Anti-inflammatory properties of red ginger (Zingiber officinale var. Rubra) extract and suppression of nitric oxide production by its constituents. J. Med. Food 2010, 13, 156–162. [Google Scholar] [PubMed]
- Lee, T.Y.; Lee, K.C.; Chen, S.Y.; Chang, H.H. 6-Gingerol inhibits ROS and iNOS through the suppression of PKC-α and NF-κB pathways in lipopolysaccharide-stimulated mouse macrophages. Biochem. Biophys. Res. Commun. 2009, 382, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Luettig, J.; Rosenthal, R.; Lee, I.F.M.; Krug, S.M.; Schulzke, J.D. The ginger component 6-shogaol prevents TNF-α-induced barrier loss via inhibition of PI3K/Akt and NF-κB signaling. Mol. Nutr. Food Res. 2016, 60, 2576–2586. [Google Scholar] [CrossRef]
- Tsiogkas, S.G.; Grammatikopoulou, M.G.; Gkiouras, K.; Zafiriou, E.; Bogdanos, D.P. Effect of Crocus sativus (Saffron) Intake on Top of Standard Treatment, on Disease Outcomes and Comorbidities in Patients with Rheumatic Diseases: Synthesis without Meta-Analysis (SWiM) and Level of Adherence to the CONSORT Statement for Randomized. Nutrients 2021, 13, 4274. [Google Scholar] [CrossRef]
- Boskabady, M.H.; Farkhondeh, T. Antiinflammatory, Antioxidant, and Immunomodulatory Effects of Crocus sativus L. and its Main Constituents. Phytother. Res. 2016, 30, 1072–1094. [Google Scholar] [CrossRef]
- Asbaghi, O.; Sadeghian, M.; Sadeghi, O.; Rigi, S.; Tan, S.C.; Shokri, A.; Mousavi, S.M. Effects of saffron (Crocus sativus L.) supplementation on inflammatory biomarkers: A systematic review and meta-analysis. Phytother. Res. 2021, 35, 20–32. [Google Scholar] [CrossRef]
- Chohan, M.; Forster-wilkins, G.; Opara, E.I. Determination of the Antioxidant Capacity of Culinary Herbs Subjected to Various Cooking and Storage Processes Using the ABTS * + Radical Cation Assay. Plant Foods Hum. Nut. 2008, 63, 47–52. [Google Scholar] [CrossRef]
- Khoddami, A.; Wilkes, M.A.; Roberts, T.H. Techniques for analysis of plant phenolic compounds. Molecules 2013, 18, 2328–2375. [Google Scholar] [CrossRef]
- Rao, P.V.; Gan, S.H. Cinnamon: A multifaceted medicinal plant. Evid. Based Complement. Altern. Med. 2014, 2014, 642942. [Google Scholar] [CrossRef] [PubMed]
- Jin, T.R. Curcumin and dietary polyphenol research: Beyond drug discovery. Acta Pharm. Sin. 2018, 39, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Nagella, P.; Thiruvengadam, M.; Ahmad, A.; Yoon, J.Y.; Chung, I.M. Composition of polyphenols and antioxidant activity of garlic bulbs collected from different Locations of Korea. Asian J. Chem. 2014, 26, 897–902. [Google Scholar] [CrossRef]
- Mao, Q.-Q.; Xu, X.-Y.; Cao, S.-Y.; Gan, R.-Y.; Corke, H.; Beta, T.; Li, H.-B. Bioactive compounds and bioactivities of ginger (zingiber officinale roscoe). Foods 2019, 8, 185. [Google Scholar] [CrossRef]
- Esmaeili, N.; Ebrahimzadeh, H.; Abdi, K.; Safarian, S. Determination of some phenolic compounds in Crocus sativus L. corms and its antioxidant activities study. Pharm. Mag. 2011, 7, 74–80. [Google Scholar]
- de la Rosa, L.A.; Moreno-Escamilla, J.O.; Rodrigo-García, J.; Alvarez-Parrilla, E. Chapter 12—Phenolic Compounds. In Postharvest Physiology and Biochemistry of Fruits and Vegetables; Yahia, E.M., Ed.; Woodhead Publishing: Sawston, UK, 2019; pp. 253–271. [Google Scholar]
- Kumar, N.; Goel, N. Phenolic acids: Natural versatile molecules with promising therapeutic applications. Biotechnol. Rep. 2019, 24, e00370. [Google Scholar] [CrossRef]
- Crimmin, M.R. Benzene rings broken for chemical synthesis. Nature 2021, 597, 33–34. [Google Scholar] [CrossRef]
- Speight, J.G. Chapter 1—Chemistry and Chemical Technology. In Handbook of Industrial Hydrocarbon Processes; Gulf Professional Publishing: Houston, TX, USA, 2011; pp. 1–41. ISBN 9780750686327. [Google Scholar] [CrossRef]
- Conner, E.M.; Grisham, M.B. Inflammation, free radicals, and antioxidants. Nutrition 1996, 12, 274–277. [Google Scholar] [CrossRef]
- Zeb, A. Concept, mechanism, and applications of phenolic antioxidants in foods. J. Food Biochem. 2020, 44, e13394. [Google Scholar] [CrossRef]
- Ghosh, T.; Basu, A.; Adhikari, D.; Roy, D.; Pal, A.K. Antioxidant activity and structural features of Cinnamomum zeylanicum. 3 Biotech 2015, 5, 939–947. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Chen, J.; Chen, Y.; Ma, Y.; Yang, Q.; Fan, Y.; Fu, C.; Limsila, B.; Li, R.; Liao, W. Extraction, structural characterization and antioxidant activity of turmeric polysaccharides. LWT 2022, 154, 112805. [Google Scholar] [CrossRef]
- Shang, A.; Cao, S.-Y.; Xu, X.-Y.; Gan, R.-Y.; Tang, G.-Y.; Corke, H.; Mavumengwana, V.; Li, H.-B. Bioactive compounds and biological functions of garlic (allium sativum L.). Foods 2019, 8, 246. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Shen, Y.; Cen, M.; Hong, X.; Shao, Q.; Chen, Y.; Zheng, B. Polysaccharide and crocin contents, and antioxidant activity of saffron from different origins. Ind. Crops Prod. 2019, 133, 111–117. [Google Scholar] [CrossRef]
- Gan, L.; Wang, J.; Guo, Y. Polysaccharides influence human health via microbiota-dependent and -independent pathways. Front. Nutr. 2022, 9, 1030063. [Google Scholar] [CrossRef]
- Peterson, C.T.; Rodionov, D.A.; Iablokov, S.N.; Pung, M.A.; Chopra, D.; Mills, P.J.; Peterson, S.N. Prebiotic Potential of Culinary Spices Used to Support Digestion and Bioabsorption. Evid. Based Complement. Altern. Med. 2019, 2019, 8973704. [Google Scholar] [CrossRef]
- Singh, A.K.; Cabral, C.; Kumar, R.; Ganguly, R.; Pandey, A.K. Beneficial Effects of Dietary Polyphenols on Gut Microbiota and Strategies to Improve. Nutrients 2019, 11, 2216. [Google Scholar] [CrossRef] [PubMed]
- Qi, L.; Mao, H.; Lu, X.; Shi, T.; Wang, J. Cinnamaldehyde Promotes the Intestinal Barrier Functions and Reshapes Gut Microbiome in Early Weaned Rats. Front. Nutr. 2021, 8, 748503. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.-J.; Wang, H.-J.; Ma, X.-J.; Li, Y.; Yang, H.-J.; Li, H.; Su, J.-R.; Zhang, C.-E.; Huang, L.-Q. Modulation of gut microbiota and intestinal barrier function during alleviation of antibiotic-associated diarrhea with Rhizoma: Zingiber officinale (Ginger) extract. Food Funct. 2020, 11, 10839–10851. [Google Scholar] [CrossRef]
- Scazzocchio, B.; Minghetti, L.; D’archivio, M. Interaction between gut microbiota and curcumin: A new key of understanding for the health effects of curcumin. Nutrients 2020, 12, 2499. [Google Scholar] [CrossRef]
- Chen, K.; Xie, K.; Liu, Z.; Nakasone, Y.; Sakao, K.; Hossain, A.; Hou, D.-X. Preventive Effects and Mechanisms of Garlic on Dyslipidemia and Gut Microbiome Dysbiosis. Nutrients 2019, 11, 1225. [Google Scholar] [CrossRef]
- Banskota, S.; Brim, H.; Kwon, Y.H.; Singh, G.; Sinha, S.R.; Wang, H.; Khan, W.I.; Ashktorab, H. Saffron pre-treatment promotes reduction in tissue inflammatory profiles and alters Microbiome composition in experimental colitis mice. Molecules 2021, 26, 3351. [Google Scholar] [CrossRef]
- Lu, Q.Y.; Rasmussen, A.M.; Yang, J.; Lee, R.P.; Huang, J.; Shao, P.; Carpenter, C.L.; Gilbuena, I.; Thames, G.; Henning, S.M.; et al. Mixed Spices at Culinary Doses Have Prebiotic Effects in Healthy Adults: A Pilot Study. Nutrients 2019, 11, 1425. [Google Scholar] [CrossRef] [PubMed]
- Khine, W.W.T.; Haldar, S.; De Loi, S.; Lee, Y.K. A single serving of mixed spices alters gut microflora composition: A dose–response randomised trial. Sci. Rep. 2021, 11, 11264. [Google Scholar] [CrossRef]
- Vieira, A.T.; Fukumori, C.; Ferreira, C.M. New insights into therapeutic strategies for gut microbiota modulation in inflammatory diseases. Clin. Transl. Immunol. 2016, 5, e87. [Google Scholar] [CrossRef]
- Dahl, S.M.; Rolfe, V.; Walton, G.E.; Gibson, G.R. Gut microbial modulation by culinary herbs and spices. Food Chem. 2023, 409, 135286. [Google Scholar] [CrossRef] [PubMed]
- Ferro, M.; Charneca, S.; Dourado, E.; Guerreiro, C.S.; Fonseca, J.E. Probiotic Supplementation for Rheumatoid Arthritis: A Promising Adjuvant Therapy in the Gut Microbiome Era. Front. Pharmacol. 2021, 12, 711788. [Google Scholar] [CrossRef]
- Alwarith, J.; Kahleova, H.; Rembert, E.; Yonas, W.; Dort, S.; Calcagno, M.; Burgess, N.; Crosby, L.; Barnard, N.D. Nutrition Interventions in Rheumatoid Arthritis: The Potential Use of Plant-Based Diets. A Review. Front. Nutr. 2019, 6, 141. [Google Scholar] [CrossRef]
- Silva, A.R.; Bernardo, A.; Costa, J.; Cardoso, A.; Santos, P.; De Mesquita, M.F.; Patto, J.V.; Moreira, P.; Silva, M.L.; Padrão, P. Dietary interventions in fibromyalgia: A systematic review. Ann. Med. 2019, 51, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Clinton, C.M.; Brien, S.O.; Law, J.; Renier, C.M.; Wendt, M.R. Whole-Foods, Plant-Based Diet Alleviates the Symptoms of Osteoarthritis. Arthritis 2015, 2015, 708152. [Google Scholar] [CrossRef]
- Fu, Y.; Wang, Y.; Gao, H.; Li, D.; Jiang, R.; Ge, L.; Tong, C.; Xu, K. Associations among Dietary Omega-3 Polyunsaturated Fatty Acids, the Gut Microbiota, and Intestinal Immunity. Mediat. Inflamm. 2021, 2021, 8879227. [Google Scholar] [CrossRef] [PubMed]
- Sköldstam, L.; Hagfors, L.; Johansson, G. An experimental study of a Mediterranean diet intervention for patients with rheumatoid arthritis. Ann. Rheum. Dis. 2003, 62, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Merra, G.; Noce, A.; Marrone, G.; Cintoni, M.; Tarsitano, M.G.; Capacci, A.; De Lorenzo, A. Influence of mediterranean diet on human gut microbiota. Nutrients 2021, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Horta-Baas, G.; Romero-Figueroa, M.D.S.; Montiel-Jarquín, A.J.; Pizano-Zárate, M.L.; García-Mena, J.; Ramírez-Durán, N. Intestinal Dysbiosis and Rheumatoid Arthritis: A Link between Gut Microbiota and the Pathogenesis of Rheumatoid Arthritis. J. Immunol. Res. 2017, 2017, 4835189. [Google Scholar] [CrossRef]
- Ramires, L.C.; Santos, G.S.; Ramires, R.P.; da Fonseca, L.F.; Jeyaraman, M.; Muthu, S.; Lana, A.V.; Azzini, G.; Smith, C.S.; Lana, J.F. The Association between Gut Microbiota and Osteoarthritis: Does the Disease Begin in the Gut? Int. J. Mol. Sci. 2022, 23, 1494. [Google Scholar] [CrossRef]
- Minerbi, A.; Fitzcharles, M.A. Gut microbiome: Pertinence in fibromyalgia. Clin. Exp. Rheumatol. 2020, 38, 99–104. [Google Scholar]
- Mousa, W.K.; Chehadeh, F.; Husband, S. Microbial dysbiosis in the gut drives systemic autoimmune diseases. Front. Immunol. 2022, 13, 906258. [Google Scholar] [CrossRef]
- Shishehbor, F.; Rezaeyan Safar, M.; Rajaei, E.; Haghighizadeh, M.H. Cinnamon Consumption Improves Clinical Symptoms and Inflammatory Markers in Women With Rheumatoid Arthritis. J. Am. Coll. Nutr. 2018, 37, 685–690. [Google Scholar] [CrossRef]
- Chandran, B.; Goel, A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother. Res. 2012, 26, 1719–1725. [Google Scholar] [CrossRef]
- Amalraj, A.; Varma, K.; Ac, K.V.; Divya, C.; Kunnumakkara, A.B.; Stohs, S.J.; Gopi, S. A Novel Highly Bioavailable Curcumin Formulation Improves Symptoms and Diagnostic Indicators in Rheumatoid Arthritis Patients: A Randomized, Double-Blind, Placebo-Controlled, Two-Dose, Three-Arm, and Parallel-Group Study. J. Med. Food. 2017, 20, 1022–1030. [Google Scholar] [CrossRef]
- Javadi, M.; Khadem Haghighian, H.; Goodarzy, S.; Abbasi, M.; Nassiri-Asl, M. Effect of curcumin nanomicelle on the clinical symptoms of patients with rheumatoid arthritis: A randomized, double-blind, controlled trial. Int. J. Rheum. Dis. 2019, 22, 1857–1862. [Google Scholar] [CrossRef]
- Jacob, J.; Amalraj, A.; Raj, K.K.J.; Divya, C.; Kunnumakkara, A.B.; Gopi, S. A novel bioavailable hydrogenated curcuminoids formulation (CuroWhiteTM) improves symptoms and diagnostic indicators in rheumatoid arthritis patients—A randomized, double blind and placebo-controlled study. J. Tradit. Complement. Med. 2019, 9, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Pourhabibi-Zarandi, F.; Rafraf, M.; Zayeni, H.; Asghari-Jafarabadi, M.; Ebrahimi, A. Effects of curcumin supplementation on metabolic parameters, inflammatory factors and obesity values in women with rheumatoid arthritis: A randomized, double-blind, placebo-controlled clinical trial. Phytother. Res. 2022, 36, 1797–1806. [Google Scholar] [CrossRef]
- Moosavian, S.P.; Paknahad, Z.; Habibagahi, Z.; Maracy, M. The effects of garlic (Allium sativum) supplementation on inflammatory biomarkers, fatigue, and clinical symptoms in patients with active rheumatoid arthritis: A randomized, double-blind, placebo-controlled trial. Phytother. Res. 2020, 34, 2953–2962. [Google Scholar] [CrossRef] [PubMed]
- Moosavian, S.P.; Paknahad, Z.; Habibagahi, Z. A randomized, double-blind, placebo-controlled clinical trial, evaluating the garlic supplement effects on some serum biomarkers of oxidative stress, and quality of life in women with rheumatoid arthritis. Int. J. Clin. Pract. 2020, 74, e13498. [Google Scholar] [CrossRef]
- Aryaeian, N.; Shahram, F.; Mahmoudi, M.; Tavakoli, H.; Yousefi, B.; Arablou, T. The effect of ginger supplementation on some immunity and inflammation intermediate genes expression in patients with active Rheumatoid Arthritis. Gene 2019, 698, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Aryaeian, N.; Mahmoudi, M.; Shahram, F.; Poursani, S.; Jamshidi, F.; Tavakoli, H. The effect of ginger supplementation on IL2, TNFα, and IL1β cytokines gene expression levels in patients with active rheumatoid arthritis: A randomized controlled trial. Med. J. Islam. Repub. Iran. 2019, 33, 154. [Google Scholar] [CrossRef]
- Hamidi, Z.; Aryaeian, N.; Abolghasemi, J.; Shirani, F.; Hadidi, M.; Fallah, S.; Moradi, N. The effect of saffron supplement on clinical outcomes and metabolic profiles in patients with active rheumatoid arthritis: A randomized, double-blind, placebo-controlled clinical trial. Phytother. Res. 2020, 34, 1650–1658. [Google Scholar] [CrossRef]
- Sahebari, M.; Heidari, H.; Nabavi, S.; Khodashahi, M.; Rezaieyazdi, Z.; DadgarMoghaddam, M.; Hosseinzadeh, H.; Abbasi, S.; Hashemzadeh, K. A double-blind placebo-controlled randomized trial of oral saffron in the treatment of rheumatoid arthritis. Avicenna J. Phytomed. 2021, 11, 332–342. [Google Scholar]
- Haroyan, A.; Mukuchyan, V.; Mkrtchyan, N.; Minasyan, N.; Gasparyan, S.; Sargsyan, A.; Narimanyan, M.; Hovhannisyan, A. Efficacy and safety of curcumin and its combination with boswellic acid in osteoarthritis: A comparative, randomized, double-blind, placebo-controlled study. BMC Complement. Altern. Med. 2018, 18, 7. [Google Scholar] [CrossRef]
- Kuptniratsaikul, V.; Dajpratham, P.; Taechaarpornkul, W.; Buntragulpoontawee, M.; Lukkanapichonchut, P.; Chootip, C.; Saengsuwan, J.; Tantayakom, K.; Laongpech, S. Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: A multicenter study. Clin. Interv. Aging 2014, 9, 451–458. [Google Scholar] [CrossRef]
- Srivastava, S.; Saksena, A.K.; Khattri, S.; Kumar, S.; Dagur, R.S. Curcuma longa extract reduces inflammatory and oxidative stress biomarkers in osteoarthritis of knee: A four-month, double-blind, randomized, placebo-controlled trial. Inflammopharmacology 2016, 24, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Mateen, S.; Moin, S.; Khan, A.Q.; Zafar, A.; Fatima, N. Increased reactive oxygen species formation and oxidative stress in rheumatoid arthritis. PLoS ONE 2016, 11, e0152925. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Alishiri, G.H.; Parvin, S.; Sahebkar, A. Mitigation of Systemic Oxidative Stress by Curcuminoids in Osteoarthritis: Results of a Randomized Controlled Trial. J. Diet. Suppl. 2016, 13, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Lopresti, A.L.; Smith, S.J.; Jackson-michel, S.; Fairchild, T. An investigation into the effects of a curcumin extract (Curcugen®) on osteoarthritis pain of the knee: A randomised, double-blind, placebo-controlled study. Nutrients 2022, 14, 41. [Google Scholar] [CrossRef]
- Roos, E.M.; Toksvig-larsen, S. KOOS Validation and Comparison to the WOMAC in Total. Knee Replace 2003, 1, 17. [Google Scholar]
- Okuda, M.; Omokawa, S.; Tanaka, Y.; Okahashi, K.; Akahane, M. Validity and reliability of the Japanese Orthopaedic Association score for osteoarthritic knees. J. Orthop. Sci. 2012, 17, 750–756. [Google Scholar] [CrossRef]
- Bevans, M.; Ross, A.; Cella, D. Patient-Reported Outcomes Measurement Information System (PROMIS): Efficient, standardized tools to measure self-reported health and quality of life. Nurs. Outlook 2014, 62, 339–345. [Google Scholar] [CrossRef]
- Poursamimi, J.; Sarabi, Z.S.; Afshari, J.T.; Mohajeri, S.A.; Ghoryani, M.; Mohammadi, M. Immunoregulatory effects of krocina, a herbal medicine made of crocin, on osteoarthritis patients: A successful clinical trial in iran. Iran. J. Allergy Asthma Immunol. 2020, 19, 253–263. [Google Scholar] [CrossRef]
- Hussein, N.A. Effect of Combined Garlic Therapy and Comprehensive Rehabilitation Program versus Comprehensive Rehabilitation Program Alone on Control of Clinical Manifestations and Quality of Life of Knee Osteoarthritis Patients. Int. J. Phys. Med. Rehabil. 2015, 3, 2. [Google Scholar] [CrossRef]
- Salimzadeh, A.; Alipoor, E.; Dehghani, S.; Yaseri, M.; Hosseini, M.; Feinle-Bisset, C.; Hosseinzadeh-Attar, M.J. The effect of 12-week garlic supplementation on symptom relief in overweight or obese women with knee osteoarthritis. Int. J. Clin. Pract. 2018, 72, e13208. [Google Scholar] [CrossRef] [PubMed]
- Dehghani, S.; Alipoor, E.; Salimzadeh, A.; Yaseri, M.; Hosseini, M.; Feinle-Bisset, C.; Hosseinzadeh-Attar, M.J. The effect of a garlic supplement on the pro-inflammatory adipocytokines, resistin and tumor necrosis factor-alpha, and on pain severity, in overweight or obese women with knee osteoarthritis. Phytomedicine 2018, 48, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh-Attar, M.J.; Alipoor, E.; Dehghani, S.; Salimzadeh, A. Increased efficacy of a garlic supplement on knee osteoarthritis symptoms in patients with obesity. J. Herb. Med. 2020, 24, 100392. [Google Scholar] [CrossRef]
- Heidari-Beni, M.; Moravejolahkami, A.R.; Gorgian, P.; Askari, G.; Tarrahi, M.J.; Bahreini-Esfahani, N. Herbal formulation “turmeric extract, black pepper, and ginger” versus Naproxen for chronic knee osteoarthritis: A randomized, double-blind, controlled clinical trial. Phytother Res. 2020, 34, 2067–2073. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.D.; Marcussen, K.C. Effects of a ginger extract on knee pain in patients with osteoarthritis. Arthritis Rheum. 2001, 44, 2531–2538. [Google Scholar] [CrossRef]
- Srivastava, K.C.; Mustafa, T. Ginger (Zingiber officinale) in rheumatism and musculoskeletal disorders. Med. Hypotheses 1992, 39, 342–348. [Google Scholar] [CrossRef]
- Rondanelli, M.; Riva, A.; Morazzoni, P.; Allegrini, P.; Faliva, M.A.; Naso, M.; Miccono, A.; Peroni, G.; Degli Agosti, I.; Perna, S. The effect and safety of highly standardized Ginger (Zingiber officinale) and Echinacea (Echinacea angustifolia) extract supplementation on inflammation and chronic pain in NSAIDs poor responders. A pilot study in subjects with knee arthrosis. Nat. Prod. Res. 2017, 31, 1309–1313. [Google Scholar] [CrossRef]
- Amorndoljai, P.; Taneepanichskul, S.; Niempoog, S.; Nimmannit, U. A comparative of ginger extract in nanostructure lipid carrier (NLC) and 1% diclofenac gel for treatment of knee osteoarthritis (OA). J. Med. Assoc. Thail. 2017, 100, 447–456. [Google Scholar]
- Chen, P.; Zhou, J.; Ruan, A.; Zeng, L.; Liu, J.; Wang, Q. Cinnamic Aldehyde, the main monomer component of Cinnamon, exhibits anti-inflammatory property in OA synovial fibroblasts via TLR4/MyD88 pathway. J. Cell. Mol. Med. 2022, 26, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Daily, J.W.; Yang, M.; Park, S. Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J. Med. Food. 2016, 19, 717–729. [Google Scholar] [CrossRef] [PubMed]
- Shakiba, M.; Moazen-Zadeh, E.; Noorbala, A.A.; Jafarinia, M.; Divsalar, P.; Kashani, L.; Shahmansouri, N.; Tafakhori, A.; Bayat, H.; Akhondzadeh, S. Saffron (Crocus sativus) versus duloxetine for treatment of patients with fibromyalgia: A randomized double-blind clinical trial. Avicenna J. Phytomed. 2018, 8, 513–523. [Google Scholar]
- Moshiri, M.; Vahabzadeh, M.; Hosseinzadeh, H. Clinical applications of saffron (Crocus sativus) and its constituents: A review. Drug Res. 2015, 65, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Appelboom, T.; MsciBiost, C.M. Flexofytol, a Purified Curcumin Extract, in Fibromyalgia and Gout: A Retrospective Study. Open J. Rheumatol. Autoimmune Dis. 2013, 3, 104–107. [Google Scholar] [CrossRef]
- Mohabbat, A.B.; Mahapatra, S.; Jenkins, S.M.; Bauer, B.A.; Vincent, A.; Wahner-Roedler, D.L. Use of Complementary and Integrative Therapies by Fibromyalgia Patients: A 14-Year Follow-up Study. Mayo Clin. Proc. Innov. Qual. Outcomes 2019, 3, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Pagliai, G.; Giangrandi, I.; Dinu, M.; Sofi, F.; Colombini, B. Nutritional interventions in the management of fibromyalgia syndrome. Nutrients 2020, 12, 2525. [Google Scholar] [CrossRef]
- la Paz, S.; García-Gimenez, M.; Quílez, A.; Puerta, R.; Fernández-Arche, A. Ginger rhizome enhances the anti-inflammatory and anti-nociceptive effects of paracetamol in an experimental mouse model of fibromyalgia. Inflammopharmacology 2018, 26, 1093–1101. [Google Scholar] [CrossRef]
- Shen, C.L.; Schuck, A.; Tompkins, C.; Dunn, D.M.; Neugebauer, V. Bioactive Compounds for Fibromyalgia-like Symptoms: A Narrative Review and Future Perspectives. Int. J. Environ. Res. Public Health 2022, 19, 4148. [Google Scholar] [CrossRef]
- Weaver, C.M.; Miller, J.W. Challenges in conducting clinical nutrition research. Nutr. Rev. 2017, 75, 491–499. [Google Scholar] [CrossRef]
- Gibson, R.S. The role of diet- and host-related factors in nutrient bioavailability and thus in nutrient-based dietary requirement estimates. Food Nutr. Bull. 2007, 28, 77–100. [Google Scholar] [CrossRef]
- Evans, M.; Lewis, E.D.; Antony, J.M.; Crowley, D.C.; Guthrie, N.; Blumberg, J.B. Breaking new frontiers: Assessment and re-evaluation of clinical trial design for nutraceuticals. Front. Nutr. 2022, 9, 958753. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charneca, S.; Hernando, A.; Costa-Reis, P.; Guerreiro, C.S. Beyond Seasoning—The Role of Herbs and Spices in Rheumatic Diseases. Nutrients 2023, 15, 2812. https://doi.org/10.3390/nu15122812
Charneca S, Hernando A, Costa-Reis P, Guerreiro CS. Beyond Seasoning—The Role of Herbs and Spices in Rheumatic Diseases. Nutrients. 2023; 15(12):2812. https://doi.org/10.3390/nu15122812
Chicago/Turabian StyleCharneca, Sofia, Ana Hernando, Patrícia Costa-Reis, and Catarina Sousa Guerreiro. 2023. "Beyond Seasoning—The Role of Herbs and Spices in Rheumatic Diseases" Nutrients 15, no. 12: 2812. https://doi.org/10.3390/nu15122812
APA StyleCharneca, S., Hernando, A., Costa-Reis, P., & Guerreiro, C. S. (2023). Beyond Seasoning—The Role of Herbs and Spices in Rheumatic Diseases. Nutrients, 15(12), 2812. https://doi.org/10.3390/nu15122812





