Does Iodine Intake Modify the Effect of Maternal Dysglycemia on Birth Weight in Mild-to-Moderate Iodine-Deficient Populations? A Mother–Newborn Prospective Cohort Study
Abstract
:1. Introduction
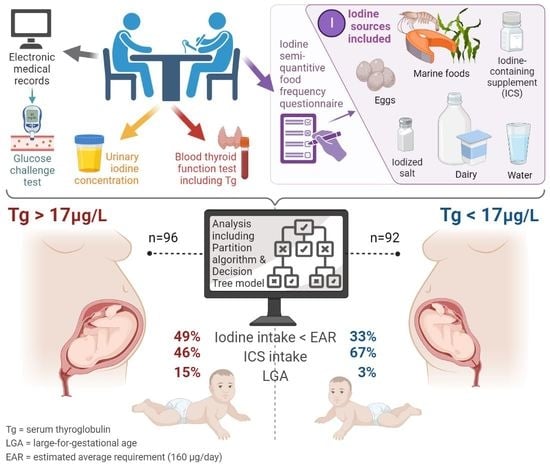
2. Materials and Methods
2.1. Design, Participants, Setting, and Ethics
2.2. Data Collection and Considerations
2.3. Assessment of Maternal Iodine Intake, Status, and Thyroid Function
2.4. Neonatal Birth Data and Antheropometrics
2.5. Statistical Analysis
3. Results
3.1. Study Population
3.2. Maternal Nutritional, Hormonal, and Clinical Characteristics
3.3. Maternal Characteristics, Pregnancy Outcomes, and Newborn Weight
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thompson, C.; Syddall, H.; Rodin, I.; Osmond, C.; Barker, D.J. Birth weight and the risk of depressive disorder in late life. Br. J. Psychiatry 2001, 179, 450–455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koller-Smith, L.I.; Shah, P.S.; Ye, X.Y.; Sjörs, G.; Wang, Y.A.; Chow, S.S.W.; Darlow, B.A.; Lee, S.K.; Håkanson, S.; Lui, K. Australian and New Zealand Neonatal Network; Canadian Neonatal Network; Swedish Neonatal Quality Register. Comparing very low birth weight versus very low gestation cohort methods for outcome analysis of high risk preterm infants. BMC Pediatr. 2017, 17, 166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barker, D.J. The developmental origins of chronic adult disease. Acta Paediatr. Suppl. 2004, 93, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; An, H.; Jin, M.; Li, Z.; Zhang, Y.; Zhang, L.; Liu, J.; Ye, R. Association of Infants Small for Gestational Age with Anemia under Five Years Old in Two Large Longitudinal Chinese Birth Cohorts. Nutrients 2022, 14, 1006. [Google Scholar] [CrossRef]
- Scifres, C.M. Short- and Long-Term Outcomes Associated with Large for Gestational Age Birth Weight. Obstet. Gynecol. Clin. N. Am. 2021, 48, 325–337. [Google Scholar] [CrossRef]
- Johnsson, I.W.; Haglund, B.; Ahlsson, F.; Gustafsson, J. A high birth weight is associated with increased risk of type 2 diabetes and obesity. Pediatr. Obes. 2015, 10, 77–83. [Google Scholar] [CrossRef]
- HAPO Study Cooperative Research Group; Metzger, B.E.; Lowe, L.P.; Dyer, A.R.; Trimble, E.R.; Chaovarindr, U.; Coustan, D.R.; Hadden, D.R.; McCance, D.R.; Hod, M.; et al. Hyperglycemia and adverse pregnancy outcomes. N. Engl. J. Med. 2008, 358, 1991–2002. [Google Scholar] [CrossRef] [Green Version]
- Beksac, M.S.; Tanacan, A.; Hakli, D.A.; Ozyuncu, O. Use of the 50-g glucose challenge test to predict excess delivery weight. Int. J. Gynaecol. Obstet. 2018, 142, 61–65. [Google Scholar] [CrossRef]
- Eastman, C.J.; Ma, G.; Li, M. Optimal Assessment and Quantification of Iodine Nutrition in Pregnancy and Lactation: Laboratory and Clinical Methods, Controversies and Future Directions. Nutrients 2019, 11, 2378. [Google Scholar] [CrossRef] [Green Version]
- Shields, B.M.; Knight, B.A.; Hill, A.; Hattersley, A.T.; Vaidya, B. Fetal thyroid hormone level at birth is associated with fetal growth. J. Clin. Endocrinol. Metab. 2011, 96, E934–E938. [Google Scholar] [CrossRef] [Green Version]
- Korevaar, T.I.; Chaker, L.; Jaddoe, V.W.; Visser, T.J.; Medici, M.; Peeters, R.P. Maternal and Birth Characteristics Are Determinants of Offspring Thyroid Function. J. Clin. Endocrinol. Metab. 2016, 101, 206–213. [Google Scholar] [CrossRef]
- Vulsma, T.; Gons, M.H.; de Vijlder, J.J. Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. N. Engl. J. Med. 1989, 321, 13–16. [Google Scholar] [CrossRef]
- Mortimer, R.H.; Galligan, J.P.; Cannell, G.R.; Addison, R.S.; Roberts, M.S. Maternal to fetal thyroxine transmission in the human term placenta is limited by inner ring deiodination. J. Clin. Endocrinol. Metab. 1996, 81, 2247–2249. [Google Scholar] [CrossRef] [PubMed]
- Ovadia, Y.S.; Zangen, S.; Rosen, S.R.; Gefel, D.; Almashanu, S.; Benbassat, C.; Fytlovich, S.; Aharoni, D.; Anteby, E.Y.; Shenhav, S. Maternal iodine deficiency: A newborns’ overweight risk factor? A prospective study. Arch. Gynecol. Obstet. 2022, 305, 777–787. [Google Scholar] [CrossRef]
- Zhang, X.; Yuan, N.; Sun, J.; Zhao, X.; Du, J.; Nan, M.; Zhang, Q.; Ji, L. Association Between Iodine Nutritional Status and Adverse Pregnancy Outcomes in Beijing, China: A Single-Center Cohort Study. Biol. Trace Elem. Res. 2022, 200, 2620–2628. [Google Scholar] [CrossRef] [PubMed]
- Shenhav, S.; Benbassat, C.; Gefel, D.; Zangen, S.; Rosen, S.R.; Avrahami-Benyounes, Y.; Almashanu, S.; Groisman, L.; Rorman, E.; Fytlovich, S.; et al. Can Mild-to-Moderate Iodine Deficiency during Pregnancy Alter Thyroid Function? Lessons from a Mother-Newborn Cohort. Nutrients 2022, 14, 5336. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.M.; Arnegard, M.E.; Maric-Bilkan, C. Dysglycemia in Pregnancy and Maternal/Fetal Outcomes. J. Womens Health 2021, 30, 187–193. [Google Scholar] [CrossRef]
- Pregnancy at Age 35 Years or Older: ACOG Obstetric Care Consensus No. 11. Obstet Gynecol. 2022, 140, 348–366. [CrossRef]
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics. Obesity in Pregnancy: ACOG Practice Bulletin, Number 230. Obstet Gynecol. 2021, 137, e128–e144. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Andersson, M. Assessment of iodine nutrition in populations: Past, present, and future. Nutr. Rev. 2012, 70, 553–570. [Google Scholar] [CrossRef]
- IOH. Standing Committee on the Scientific Evaluation of Dietary Reference Intakes; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- CDC. Laboratory Procedure Manual: Lodine in Urine; NHANES 2003–2004 Inorganic Toxicology and Nutrition Branch, Division of Laboratory Sciences; National Center for Environmental Health: Atlanta, GA, USA, 2007. [Google Scholar]
- WHO. Assessment of iodine deficiency disorders and monitoring their elimination. In A Guide for Programmed Managers, 3rd ed.; World Health Organization: Lyon, France, 2007. [Google Scholar]
- Alexander, E.K.; Pearce, E.N.; Brent, G.A.; Brown, R.S.; Chen, H.; Dosiou, C.; Grobman, W.A.; Laurberg, P.; Lazarus, J.H.; Mandel, S.J.; et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017, 27, 315–389. [Google Scholar] [CrossRef] [Green Version]
- Ma, Z.F.; Skeaff, S.A. Thyroglobulin as a biomarker of iodine deficiency: A review. Thyroid 2014, 24, 1195–1209. [Google Scholar] [CrossRef] [Green Version]
- Dollberg, S.; Haklai, Z.; Mimouni, F.B.; Gorfein, I.; Gordon, E.S. Birth weight standards in the live-born population in Israel. Isr. Med. Assoc. J. 2005, 7, 311–314. [Google Scholar] [PubMed]
- Davidson, S.; Sokolover, N.; Erlich, A.; Litwin, A.; Linder, N.; Sirota, L. New and improved Israeli reference of birth weight, birth length, and head circumference by gestational age: A hospital-based study. Isr. Med. Assoc. J. 2008, 10, 130–134. [Google Scholar] [PubMed]
- Greenwood, D.C.; Webster, J.; Keeble, C.; Taylor, E.; Hardie, L.J. Maternal Iodine Status and Birth Outcomes: A Systematic Literature Review and Meta-Analysis. Nutrients 2023, 15, 387. [Google Scholar] [CrossRef]
- Dosiou, C.; Medici, M. Management of endocrine disease: Isolated maternal hypothyroxinemia during pregnancy: Knowns and unknowns. Eur. J. Endocrinol. 2017, 176, R21–R38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glinoer, D. Maternal and fetal impact of chronic iodine deficiency. Clin. Obstet. Gynecol. 1997, 40, 102–116. [Google Scholar] [CrossRef]
- Rousset, B.; Dupuy, C.; Miot, F.; Dumont, J. Chapter 2 Thyroid Hormone Synthesis And Secretion. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2015. [Google Scholar]
- Fernández-Real, J.M.; López-Bermejo, A.; Castro, A.; Casamitjana, R.; Ricart, W. Thyroid function is intrinsically linked to insulin sensitivity and endothelium-dependent vasodilation in healthy euthyroid subjects. J. Clin. Endocrinol. Metab. 2006, 91, 3337–3343. [Google Scholar] [CrossRef]
- Roos, A.; Bakker, S.J.; Links, T.P.; Gans, R.O.; Wolffenbuttel, B.H. Thyroid function is associated with components of the metabolic syndrome in euthyroid subjects. J. Clin. Endocrinol. Metab. 2007, 92, 491–496. [Google Scholar] [CrossRef] [Green Version]
- Fontenelle, L.C.; Feitosa, M.M.; Severo, J.S.; Freitas, T.E.C.; Morais, J.B.S.; Torres-Leal, F.L.; Henriques, G.S.; Marreiro, D.D.N. Thyroid Function in Human Obesity: Underlying Mechanisms. Horm. Metab. Res. 2016, 48, 787–794. [Google Scholar] [CrossRef] [Green Version]
- Reaven, G.M. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988, 37, 1595–1607. [Google Scholar] [CrossRef] [PubMed]
- Barbour, L.A.; McCurdy, C.E.; Hernandez, T.L.; Kirwan, J.P.; Catalano, P.M.; Friedman, J.E. Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes. Diabetes Care 2007, 30 (Suppl. S2), S112–S119, Erratum in Diabetes Care 2007, 30, 3154. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, R.; Gruppuso, P.A.; Petzold, K.; Brambilla, D.; Hiilesmaa, V.; Teramo, K.A. Hyperinsulinemia and macrosomia in the fetus of the diabetic mother. Diabetes Care 1994, 17, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Langer, O. Fetal macrosomia: Etiologic factors. Clin. Obstet. Gynecol. 2000, 43, 283–297. [Google Scholar] [CrossRef]
- Damiano, F.; Rochira, A.; Gnoni, A.; Siculella, L. Action of Thyroid Hormones, T3 and T2, on Hepatic Fatty Acids: Differences in Metabolic Effects and Molecular Mechanisms. Int. J. Mol. Sci. 2017, 18, 744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katz, L.S.; Xu, S.; Ge, K.; Scott, D.K.; Gershengorn, M.C. T3 and Glucose Coordinately Stimulate ChREBP-Mediated Ucp1 Expression in Brown Adipocytes From Male Mice. Endocrinology 2018, 159, 557–569. [Google Scholar] [CrossRef] [Green Version]
- Katz, L.S.; Argmann, C.; Lambertini, L.; Scott, D.K. T3 and glucose increase expression of phosphoenolpyruvate carboxykinase (PCK1) leading to increased β-cell proliferation. Mol. Metab. 2022, 66, 101646. [Google Scholar] [CrossRef]
- Hashimoto, K.; Ishida, E.; Matsumoto, S.; Okada, S.; Yamada, M.; Satoh, T.; Monden, T.; Mori, M. Carbohydrate Response Element Binding Protein Gene Expression Is Positively Regulated by Thyroid Hormone. Endocrinology 2009, 150, 3417–3424. [Google Scholar] [CrossRef] [Green Version]
- Verhagen, N.J.E.; Gowachirapant, S.; Winichagoon, P.; Andersson, M.; Melse-Boonstra, A.; Zimmermann, M.B. Iodine Supplementation in Mildly Iodine-Deficient Pregnant Women Does Not Improve Maternal Thyroid Function or Child Development: A Secondary Analysis of a Randomized Controlled Trial. Front. Endocrinol. 2020, 11, 572984. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, Y.; Yuan, Z.; Li, Y.; Liu, S.; Zeng, X.; Qiu, X.; Ye, L.; Huang, D. The association between iron status and thyroid hormone levels during pregnancy. J. Trace Elements Med. Biol. 2022, 74, 127047. [Google Scholar] [CrossRef]
- Chu, F.C.; Shaw, S.W.; Lo, L.M.; Hsieh, T.T.; Hung, T.H. Association between maternal anemia at admission for delivery and adverse perinatal outcomes. J. Chin. Med. Assoc. 2020, 83, 402–407, Erratum in J. Chin. Med. Assoc. 2020, 83, 1054. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.; Karmisholt, J.; Pedersen, K.M.; Laurberg, P. Reliability of studies of iodine intake and recommendations for number of samples in groups and in individuals. Br. J. Nutr. 2008, 99, 813–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, J.; Wang, X.; Yuan, L.; Guo, L. Iron Deficiency, a Risk Factor of Thyroid Disorders in Reproductive-Age and Pregnant Women: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2021, 12, 629831. [Google Scholar] [CrossRef] [PubMed]



| Subgroups Segregated by Maternal Tg Values | >13 μg/L | ≤13 μg/L | p Value |
|---|---|---|---|
| Pregnant women, n | 127 | 61 | |
| Gestational age (weeks) at recruitment, mean ± SD | 31 ± 1 | 31 ± 2 | NS |
| GCT (mg/dL), mean ± SD | 118 ± 28 | 113 ± 31 | NS |
| BMI (kg/m2) | |||
| At recruitment, mean ± SD | 28 ± 5 | 28 ± 5 | NS |
| At delivery, mean ± SD | 30 ± 6 | 29 ± 4 | NS |
| Iodine Intake | |||
| Estimated dietary Iodine intake (μg/d), mean ± SD * | 181 ± 109 | 215 ± 118 | 0.06 |
| Iodized salt use, n (%) ם | 4 (5) | 5 (11) | NS |
| ICS intake, n (%) F | 68 (58) | 38 (69) | NS |
| Birthweight | |||
| Adjusted weight percentile (%), mean ± SD Do | 53 ± 28 | 51 ± 25 | NS |
| LGA L | 14 (13) | 4 (4) | 0.04 |
| Subgroups Segregated by Maternal Tg Values | >17 μg/L | ≤17 μg/L | p Value |
|---|---|---|---|
| Pregnant women, n | 96 | 92 | |
| Age (y), mean ± SD | 31 ± 6 | 32 ± 5 | NS |
| Gestational age (weeks) at recruitment, mean ± SD | 32 ± 7 | 31 ± 7 | NS |
| Israeli born, n (%) | 52 (54) | 42 (46) | NS |
| Tertiary education, n (%) | 42 (44) | 52 (56) | NS |
| Secular n (%) | 28 (30) | 35 (38) | NS |
| IVF | 6 (6) | 10 (11) | NS |
| Smoking | |||
| Current smoker | 13 (14) | 11 (12) | NS |
| Past smoker | 18 (19) | 18 (20) | NS |
| Alcohol, n (%) | 0 (0) | 0 (0) | NS |
| Post-psychological stressful event, n (%) | 14 (15) | 18 (20) | NS |
| GCT (mg/dL), mean ± SD | 119 ± 28 | 114 ± 31 | NS |
| BMI (kg/m2) | |||
| At recruitment, mean ± SD | 29 ± 5 | 28 ± 5 | NS |
| At delivery, mean ± SD | 31 ± 6 | 29 ± 4 | NS |
| Gravidity, mean ± SD * | 4 ± 2 | 3 ± 2 | 0.05 |
| Parity, mean ± SD * | 3 ± 2 | 2 ± 1 | 0.03 |
| Iodine Intake | |||
| Estimated dietary Iodine intake (μg/d), mean ± SD * | 163 ± 104 | 221 ± 114 | <0.01 |
| Iodine intake < EAR, n (%) F | 47 (49) | 30 (33) | 0.03 |
| Iodized salt use, n (%) ם | 4 (4) | 5 (5) | NS |
| ICS intake, n (%) F | 44 (46) | 62 (67) | <0.01 |
| Estimated iodine intake from ICS (μg/d), median (IQR) K | 1 (0–150) | 150 (0–220) | <0.01 |
| Dietary goitrogens exposure, n (%) F | 20 (22) | 12 (13) | NS |
| UIC | |||
| Median UIC, μg/L (IQR) | 53 (39–86) | 65 (41–97) | NS |
| Participants with UIC <150 μg/L, n (%) | 77 (80) | 72 (86) | NS |
| Participants with UIC <50 μg/L, n (%) | 34 (35) | 30 (33) | NS |
| TSH | |||
| Mean ± SD (mIU/L), n (%) | 1.8 ± 1.0 | 1.8 ± 1.0 | NS |
| Participants with SCH, n (%) | 4 (4) | 2 (2) | NS |
| FT4 | |||
| Mean ± SD (μg/L), n (%) | 1.0 ± 0.2 | 1.0 ± 0.1 | NS |
| Participants with IHT, n (%) | 7 (7) | 8 (9) | NS |
| FT3 (pmol/L), mean ± SD | 4.1 ± 0.7 | 3.9 ± 0.7 | NS |
| TPO Ab | |||
| TPO Ab (mIU/L), median (IQR) | 13 (11–16) | 13 (11–17) | NS |
| Positive TPO Ab, n (%) | 1 (1) | 4 (4) | NS |
| Tg Ab | |||
| Tg Ab (mIU/L), median (IQR) | 10 (10–11) | 10 (10–12) | NS |
| Positive Tg Ab, n (%) | 1 (1) | 4 (5) | NS |
| Newborns at birth a, n | 85 | 84 | |
| Gestational age (days), mean ± SD | 266 ± 29 | 270 ± 13 | NS |
| Preterm birth, n (%) | 13 (15) | 11 (13) | NS |
| Gender (Female, Male) | 36, 47 | 36, 48 | NS |
| Apgar score | |||
| At 1 min after delivery, mean ± SD | 8.9 ± 0.1 | 8.9 ± 0.1 | NS |
| At 5 min after delivery, mean ± SD | 9.9 ± 0.4 | 9.9 ± 0.3 | NS |
| Birthweight | |||
| Crude weight (g), mean ± SD | 3176 ± 652 | 3029 ± 580 | NS |
| LBW | 3 (4) | 8 (10) | NS |
| Macrosomia | 6 (7) | 2 (2) | NS |
| Adjusted weight percentile (%), mean ± SD Do | 56 ± 28 | 49 ± 26 | 0.07 |
| SGA | 5 (6) | 10 (12) | NS |
| LGA F | 13 (15) | 3 (3) | 0.02 |
| Length percentile (%), mean ± SD Da | 74.4 ± 26.3 | 70.6 ± 25.9 | NS |
| Head circumference (cm) | |||
| Mean ± SD | 34.4 ± 2.1 | 34.0 ± 1.7 | NS |
| > 90th percentile Da, n (%) | 27 (28) | 17 (18) | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ovadia, Y.S.; Gefel, D.; Toledano, Y.; Rosen, S.R.; Avrahami-Benyounes, Y.; Groisman, L.; Rorman, E.; Hen, L.; Fytlovich, S.; Katz, L.S.; et al. Does Iodine Intake Modify the Effect of Maternal Dysglycemia on Birth Weight in Mild-to-Moderate Iodine-Deficient Populations? A Mother–Newborn Prospective Cohort Study. Nutrients 2023, 15, 2914. https://doi.org/10.3390/nu15132914
Ovadia YS, Gefel D, Toledano Y, Rosen SR, Avrahami-Benyounes Y, Groisman L, Rorman E, Hen L, Fytlovich S, Katz LS, et al. Does Iodine Intake Modify the Effect of Maternal Dysglycemia on Birth Weight in Mild-to-Moderate Iodine-Deficient Populations? A Mother–Newborn Prospective Cohort Study. Nutrients. 2023; 15(13):2914. https://doi.org/10.3390/nu15132914
Chicago/Turabian StyleOvadia, Yaniv S., Dov Gefel, Yoel Toledano, Shani R. Rosen, Yael Avrahami-Benyounes, Ludmila Groisman, Efrat Rorman, Lihi Hen, Shlomo Fytlovich, Liora S. Katz, and et al. 2023. "Does Iodine Intake Modify the Effect of Maternal Dysglycemia on Birth Weight in Mild-to-Moderate Iodine-Deficient Populations? A Mother–Newborn Prospective Cohort Study" Nutrients 15, no. 13: 2914. https://doi.org/10.3390/nu15132914
APA StyleOvadia, Y. S., Gefel, D., Toledano, Y., Rosen, S. R., Avrahami-Benyounes, Y., Groisman, L., Rorman, E., Hen, L., Fytlovich, S., Katz, L. S., Anteby, E. Y., & Shenhav, S. (2023). Does Iodine Intake Modify the Effect of Maternal Dysglycemia on Birth Weight in Mild-to-Moderate Iodine-Deficient Populations? A Mother–Newborn Prospective Cohort Study. Nutrients, 15(13), 2914. https://doi.org/10.3390/nu15132914